Abstract
Purpose
Household food insecurity is related to poor mental health. This study examines whether the level of household food insecurity is associated with a gradient in the risk of reporting six adverse mental health outcomes. This study further quantifies the mental health impact if severe food insecurity, the extreme of the risk continuum, were eliminated in Canada.
Methods
Using a pooled sample of the Canadian Community Health Survey (N = 302,683), we examined the relationship between level of food insecurity, in adults 18–64 years, and reporting six adverse mental health outcomes. We conducted a probit analysis adjusted for multi-variable models, to calculate the reduction in the odds of reporting mental health outcomes that might accrue from the elimination of severe food insecurity.
Results
Controlling for various demographic and socioeconomic covariates, a food insecurity gradient was found in six mental health outcomes. We calculated that a decrease between 8.1% and 16.0% in the reporting of these mental health outcomes would accrue if those who are currently severely food insecure became food secure, after controlling for covariates.
Conclusion
Household food insecurity has a pervasive graded negative effect on a variety of mental health outcomes, in which significantly higher levels of food insecurity are associated with a higher risk of adverse mental health outcomes. Reduction of food insecurity, particularly at the severe level, is a public health concern and a modifiable structural determinant of health worthy of macro-level policy intervention.
Keywords: Food insecurity, Mental health, Chronic stress, Canadian adults
Highlights
-
•
This study uses a four-level food insecurity variable of increasing severity.
-
•
Findings show a food insecurity gradient on six adverse mental health outcomes.
-
•
Severe food insecurity is related to high odds of reporting mental health outcomes.
-
•
Eliminating severe food insecurity could reduce mental ill-health burden.
Introduction
Untreated mental health problems account for 13% of the total global burden of disease and depressive disorders are the third leading cause of disease burden worldwide (World Health Assembly, 2012). It has been estimated that by 2030 depressive disorders could represent the highest disease burden in the world (World Health Assembly, 2012). In Canada, mental health problems pose substantial direct and indirect costs on the lives of individuals and society (Deraspe, 2013). An estimated 20% of Canadians will experience a mental illness throughout the course of their lives (Smetanin et al., 2011), which can lead to short- and long-term productivity losses with serious consequences on public finances and lower government tax revenues. In addition, the costs associated with governmental financial assistance, public spending on health care and community support to address mental illness can place a major strain on the resources of the government. For example, approximately one third of hospital stays are due to mental disorders (Government of Canada, 2006) and it is estimated that the direct cost of mental ill health was $42 billion in Canada in 2011 (Smetanin et al., 2011). Therefore, strategic spending on mental illness prevention and mental health promotion will promote population health, reduce the need for hospital admissions due to mental illness, and limit productivity declines, all of which would result in cost savings and a reduction in human suffering (Roberts & Grimes, 2011).
Poverty has long been associated with poor health outcomes including mental health outcomes. In Canada, individuals in the lowest income group are three to four times more likely to report their mental health as fair or poor compared with the highest income group (Statistics Canada, 2013). In addition, many cross-national and cross-sectional studies have shown that individuals with low-income or low socioeconomic status are at increased odds of reporting major depression (Lorant et al., 2003), mood disorders, anxiety disorder and substance abuse (Fryers, Melzer & Jenkins, 2003). Recently Burns (2015), stressed the need to disaggregate poverty into specific indicators such as, “income, expenditure, assets, education, employment and food security…” (p.108), in order to examine their distinct impact on mental health outcomes. This paper contributes to the literature by examining one of these indicators in greater detail—household food insecurity (HFI).
HFI is operationally defined as the lack of access to food because of financial constraints (Tarasuk, Dachner & Loopstra, 2014) and in Canada is measured through national survey responses to the Household Food Security Survey Module (HFSSM) (Bickel et al., 2000, Health Canada, 2007). Using this metric, recent national estimates indicate that in 2012, 12.5% of Canadian households experienced some level of HFI (4.1% marginally food insecure, 5.7% moderately food insecure, and 2.7% severely food insecure) (Tarasuk, Mitchell & Dachner, 2014). The HFSSM is also the national measurement tool in the United States where the criterion for moderate food insecurity is one affirmative response more stringent, limiting direct comparability between studies using the same metric. Nevertheless, studies, which operationalize HFI using any classification system of the HFSSM by level or as a binary, have repeatedly shown that HFI has an impact on physical health and nutrition, including an increased risk of the development of chronic disease (Seligman, Laraia, & Kushel, 2010), poor self-rated health (Vozoris & Tarasuk, 2003), nutritional vulnerabilities in adolescents and adults (Kirkpatrick & Tarasuk, 2008), poor cardiovascular health (Saiz et al., 2016), diabetes (Gucciardi, Vogt, DeMelo & Stewart, 2009), oral health problems (Muirhead, Quiñonez, Figueiredo & Locker, 2009), anemia in children (Eicher-Miller, Mason, Weaver, McCabe & Boushey, 2009), and increased hospitalization (Cook et al., 2004). A growing body of evidence has also pointed to a detrimental association between HFI and mental well-being from a variety of settings and using variations on the scoring of the HFSSM (Carter et al., 2011, Davison and Kaplan, 2015, Davison et al., 2015, Fuller-Thomson and Nimigon, 2008, Heflin et al., 2005, Leung et al., 2015, Pryor et al., 2016, Siefert et al., 2004, Stuff et al., 2004, Tarasuk et al., 2013, Vozoris and Tarasuk, 2003, Muldoon et al., 2013, Whitaker et al., 2006, Wu and Schimmele, 2005). It is hypothesized that HFI impacts mental health due to the unique stresses associated with the biological and social implications of “not having enough money for food” (Health Canada, 2007, p.45), which is the common end to each HFSSM question (Hadley and Crooks, 2012, Bhattacharya et al., 2004).
The evidence presented supports the reasoning for HFI being considered one of 14 social determinants of health in Canada (Raphael & Mikkonen, 2010), or a factor apart from medical care that can shape health in a powerful way (Braveman & Gottlieb, 2014). Importantly, population health researchers emphasize that health risk does not often occur as two extremes of exposure but rather as a continuum of risk (Institute of Medicine, 2003). Therefore, population-based interventions focus on shifting the risk curve for an entire population while paying attention to the social conditions that characterize individual lives (Marmot et al., 2008, Halfon et al., 2009).
The majority of the research conducted on the association between mental health outcomes and HFI has been conducted using a binary measure of food insecurity (Carter et al., 2011, Fuller-Thomson and Nimigon, 2008, Vozoris and Tarasuk, 2003), despite the established predictive power of a three-level (food secure, moderately food insecure and severely food insecure) or four-level (food secure, marginally food insecure, moderately food insecure and severely food insecure) HFI measure on mental health outcomes (Cook et al., 2004, Tarasuk et al., 2013, Burke et al., 2016, Davison et al., 2015, Pryor et al., 2016, Muldoon et al., 2013, Whitaker et al., 2006). A binary measure treats food insecure respondents as one homogenous group and thus disguises important health outcomes associated with different severities of HFI (Burke et al., 2016, Tarasuk et al., 2015). For example, Burke and associates observed that a three-level measure of HFI severely was positively associated with mental health outcomes in children and adolescents in the United States, using a slightly more stringent criterion for moderate food insecurity compared with Canada (Burke et al., 2016). In addition, in Canada Tarasuk and colleagues showed increasing health care costs (including psychiatric care and prescription drug costs) with increasingly severe HFI, using a four-level variable (Tarasuk et al., 2015). These studies present the idea that HFI could be having a graded, or step-wise, impact on mental health outcomes. The present study contributes to the literature by analyzing the relationship between a four-level HFI variable and six adverse mental health outcomes in Canadian adults.
The objectives of this study are specifically to: 1) determine whether increasing levels of HFI are associated with higher risk of reporting adverse mental health outcomes (i.e., does an HFI gradient exist on six mental health conditions?); and 2) quantify the reduction in the reporting of mental health outcomes that could be expected if severe HFI were eliminated in Canada, i.e., if the risk curve were shifted to less severe HFI.
Methods
Data source
We pooled 4 cycles (Cycle 3.1 [2005], 2007–2008, 2009–2010, and 2011–2012) of the Canadian Community Health Survey (CCHS). The CCHS is a series of cross-sectional surveys structured to collect information on a variety of issues relating to health, including health status, health care utilization, and health determinants (Statistics Canada, 2007). The target population, sampling procedure, and sample sizes are all determined by Statistics Canada. These surveys are divided by health region and reflect estimates according to health region and province as well as the Canadian population as a whole. The CCHS collects data from any person aged 12 or older residing in a dwelling in the ten provinces and three territories. Individuals living on reserves or Crown land, in institutions, in remote regions, or who are members of the Armed Forces are not included in the survey. The CCHS data sample represents approximately 98% of the Canadian population aged 12 years or older.
Cycles were combined with the existing weights (survey weights), divided by four (the number of cycles pooled) and the pooled dataset1 was treated as one sample from a single population with a sample size of N=515,421 prior to exclusions.
The CCHS questions are designed for computer-assisted interviewing (CAI) with pre-programmed questions, content flow, and allowable responses (ranges or answers). Half of the interviews take place by telephone while the other half take place as personal interviews; participation in the CCHS is voluntary and responses are kept strictly confidential (Statistics Canada, 2007).
Exclusion criteria
The population of interest is working-age Canadian adults (18–64 years). Children aged 12–17 years were excluded from the dataset as adult members of a household will often protect children in that household from more severe food insecurity (Roshanafshar & Hawkins, 2015). As a result, the children’s level of HFI may not accurately reflect the real lived experience of food insecurity for that child, who may still feel the shame, distress and frustration related to food insecurity (Roshanafshar & Hawkins, 2015). Respondents 65 years and over were excluded because seniors in Canada receive guaranteed monthly income in the form of a seniors pension therefore they have the lowest HFI rates of the adult demographic in Canada (Emery, Fleisch & McIntyre, 2013). In addition, due to challenges of food supply related to isolated geographic areas such as Canada’s Northern Territories (Inuit Circumpolar Council, 2012), only respondents from the 10 provinces were included in the dataset.
Provincial participation in the CCHS depended on the survey cycle. In the CCHS 2007–2008 and CCHS 2011–2012, the HFI module was a core component; therefore, respondents from all ten provinces participated in the survey. The module was optional in the CCHS 3.1, and the provinces of Newfoundland and Labrador, New Brunswick, Manitoba and Saskatchewan declined participation. In the CCHS 2009–2010, Prince Edward Island and New Brunswick declined participation. Pooling four cycles (two of which include data on the provinces who declined to participate in 3.1 and 2009–2010) and bootstrapping circumvents problems related to generalizability of the results to the ten provinces. Only households that provided a response to the HFI module were included in the dataset.
Measures
Household food security survey module (HFSSM)
The exposure variable in this project was HFI as measured through the HFSSM. The HFSSM was adapted from the 18-question US Household Food Security Survey Module that had been used to monitor food insecurity in the United States since 1995 (Nord, Hooper, & Hopwood, 2008). Although the two modules are based on the same survey questions, the threshold for moderate food insecurity is one affirmation less in Canada than the US (Nord et al., 2008). The HFSSM has been validated in Canada using Rasch measurement model and has been shown to measure the same phenomenon in English and French speaking respondents (Bickel et al., 2000, Health Canada, 2007). The HFSSM assesses the food insecurity situation of adults as a group and children as a group within the household over the past 12 months. The HFSSM includes 10 questions measuring HFI in adults and 8 questions measuring HFI in children (Statistics Canada, 2007).
A four-category HFI variable was used for this study in accordance with the current literature on HFI in Canada (Tarasuk et al., 2014). The “Food Secure” group included respondents who screened negative2 or who did not answer affirmatively to any of the adult or child food situation questions in the HFSSM. The “Marginally Food Insecure” group included respondents who answered affirmatively to 1 question in the HFSSM. This group has been shown in the Canadian literature to have health implications intermediate to the food secure and moderately food insecure group (Tarasuk et al., 2015). The “Moderately Food Insecure” group included respondents who answered affirmatively to 2 to 5 adult food situation situations or 2 to 4 child food situation questions. Finally, the “Severely Food Insecure” included respondents who answered affirmatively to 6 or more adult food situation questions or 5 or more child food situation questions. Of note, this classification is identical to the US classification of the HFSSM for very low food insecurity. Those who were missing because of lack of response to the HFSSM were compared to those who responded to the HFSSM on all covariates used in this analysis. There were no statistically significant differences between the two groups, and on this basis respondents were considered missing completely at random (MCAR).
Mental health outcome variables
Six common mental health outcomes collected in the CCHS were included in the analysis: major depressive episodes in the past year, depressive thoughts in the past month, anxiety disorders, mood disorders, self-reported mental health status and suicidal thoughts in the past year. All six outcomes were self-reported, due to the nature of the survey, but respondents were asked to only respond affirmatively to the anxiety and mood disorder questions if a physician or health professional had diagnosed them with these conditions. All mental health outcomes measured in the CCHS were included in this analysis, with the exception of illicit drug use and binge drinking due to low response rate. The CCHS questions are divided into common core content and optional content. The common core content questions are asked in every province and territory whereas the optional component is tailored to the region. As a result, three of the outcome variables used in this study (suicidal thoughts, depressive thoughts and major depressive episodes) were not asked in all provinces. A detailed description of the mental health outcome variables is presented in the Appendix A.
Demographic and socioeconomic covariates
Six demographic variables (age, sex, marital status, household composition, homeownership and highest education level in household) were included as covariates and were assessed for effect modification or confounding on the relationship between HFI and adverse mental health outcomes. In addition, variables that measure respondents’ ethnicity (white, Asian, Aboriginal, or other), immigration status (immigrated less than 10 years ago, immigrated more than 10 years ago, Canadian-born), main income source (wages, Employment Insurance/Workers’ Compensation Board, social assistance, other sources), and inflation adjusted household income (low, medium-high) were also included in the analysis.
Covariates were selected based on literature citing the risk factors for HFI and its associated health effects (Chen & Chen, 2001; Tarasuk, 2001, Siefert et al., 2004; Heflin et al., 2005; Muldoon et al., 2013; Tarasuk et al., 2013; Tarasuk et al., 2014; Olabiyi & McIntyre, 2014). After reviewing the literature, referent groups were selected if they had a protective impact against HFI. Finally, a cycle variable (2005, 2007/08, 2009/10, 2011/12) was included in order to determine whether macro-level economic events, such as the 2008–2009 recession in Canada, modified the relationship between HFI and adverse mental health outcomes.
Missing values on the covariates did not account for more than 4.6% of the total sample size and the majority of the missing values accounted for less than 1% of the total sample size for each covariate. While no established cut-off for missing data exists, some authors have argued that missing data that accounts for less than 10% (Bennett, 2001), 5% (Schafer, 1999) or 1% (McKnight, McKnight, Sidani, & Figueredo, 2007) of the total sample size is inconsequential and thus can be removed.
Statistical analyses
Data analysis was conducted at the [blinded] Research Data Centre using STATA statistical software (version 14) (Statacorp, College Station, TX, 2015).
Univariate descriptive analyses of all study variables were followed by bivariate analyses to assess the proportion by level of HFI in Canadians for each mental health outcome. Crude and adjusted binary logistic regression analyses were then conducted to present the odds of reporting adverse mental health outcomes at each level of HFI (data not shown). In addition, covariates were assessed for confounding and effect modification. The covariates included in the multivariable models for each of the six mental health outcomes were determined by assessing each covariate as a potential confounder and effect modifier by comparing the crude analyses to the individually-adjusted analyses (data not shown). Significant variables and interactions were included in the all-inclusive model and non-significant variables were removed through backwards elimination using a Bonferroni adjustment for multiple testing.
Marginal effect reduction analyses were calculated to quantify the potential reduction in adverse mental health outcomes with the elimination of severe HFI in Canada compared to food secure Canadians. Marginal effects or partial effects, estimated from the probit analysis, measure the change in the conditional estimate of the outcome variable given a change in one of the regressors (e.g. HFI) (Cameron & Trivedi, 2005). We generated probit models, based on the multi-variable fully adjusted and reduced models (data not shown), to assess the probability of reporting each adverse mental health outcomes, controlling for all pertinent study covariates. The proportions were then converted to percentages and represent the percent point reduction in the odds of reporting of each adverse mental health outcome if the respondent’s variable of interest (e.g., movement from severe HFI to food security) were to be changed into the referent group of that variable of interest. While this method of analysis is typically utilized in the study of economics, there has been interest in this technique in the field of public health (Emery et al., 2012, Evans et al., 2012, McIntyre et al., 2016a, McIntyre et al., 2016b).
Analyses were conducted on sample weighted data provided by Statistics Canada, in order to account for clustering due to complex survey design, and estimates were generated using 500 bootstrap replicates. An alpha level of p < 0.05 was used to test for significance. All estimates were subjected to Statistics Canada vetting procedure for small cell sizes.
Results
Table 1 presents the demographic statistics for all respondents included in the sample. After exclusions, the proportion of Canadian adults aged 18–64 years experiencing HFI is approximately 11.8% [95% CI: 11.3–12.2], while severe HFI is reported in 1.4% [95% CI: 1.3–1.5] (Table 1). The proportion of respondents reporting one of the six adverse mental health outcomes ranges from 5.3% (95% CI: 5.2–5.4, poor/fair mental health) to 19.9% (depressive thoughts 95% CI: 19.6–20.3). Table 1 also presents the socio-demographics of food insecure Canadians.
Table 1.
Prevalence (%) and 95% Confidence Intervals of Study Variables from a Pooled Sample of Respondents from the Canadian Community Health Survey 2005–2012 (N = 302,683).
| Variable | Categories | Percent | 95% CI |
|---|---|---|---|
| Outcome | |||
| Major Depressive Episodes in the Past Year | Yes | 6.4 | 6.2–6.6 |
| Depressive Thoughts in the Past Month | Yes | 19.9 | 19.6–20.3 |
| Anxiety Disorder | Yes | 5.8 | 5.7–6.0 |
| Mood Disorder | Yes | 7.2 | 7.0–7.3 |
| Suicidal Thoughts in the Past Year | Yes | 19.7 | 18.7–20.7 |
| Mental Health Status | Fair/Poor | 5.3 | 5.2–5.4 |
| Exposure | |||
| Household Food Insecurity | Food Secure | 88.2 | 88.0–88.4 |
| Marginal Food Insecurity | 3.7 | 3.5–3.8 | |
| Moderate Food Insecurity | 6.7 | 6.5–6.9 | |
| Severe Food Insecurity | 1.4 | 1.3–1.5 | |
| Covariate | Categories | Mean | Standard Deviation |
| Age | Continuous (18–64) | 42.8 | 13.5 |
| Covariate | Categories | Percent | 95% CI |
| Sex | Male | 49.1 | 49.1–49.2 |
| Female | 50.9 | 50.8–50.9 | |
| Household | Unattached, living alone | 12.5 | 12.3–12.7 |
| Single living with others | 5.1 | 5.0–5.3 | |
| Couple, no kids | 25.3 | 25.0–25.5 | |
| Couple with kids < 25 | 45.0 | 44.7–45.3 | |
| Lone parent, kids < 25 | 6.1 | 5.9–6.3 | |
| Other/multi-family | 6.0 | 5.9–6.2 | |
| Marital Status | Married/Common Law | 65.2 | 64.9–65.4 |
| Divorced/Widowed/ | 9.2 | 9.0–9.4 | |
| Separated | 25.7 | 25.4–25.9 | |
| Single | |||
| Inflation-Adjusted Income | Lowa | 5.8 | 5.6–5.9 |
| Med-High | 94.2 | 94.1–94.4 | |
| Income Source | Wages/Salary/Self-Employment | 88.9 | 88.7–89.1 |
| EI/WCB | 1.1 | 1.0–1.1 | |
| Social Assistance b | 8.2 | 8.0–8.3 | |
| Other c | 1.8 | 1.8–1.9 | |
| Race | White | 79.2 | 78.9–79.6 |
| Asian | 11.7 | 11.4–12.0 | |
| Aboriginal | 2.6 | 2.5–2.7 | |
| Other d | 6.5 | 6.2–6.7 | |
| Education | Post-Secondary Degree | 80.5 | 80.2–80.7 |
| Some Post-Secondary | 5.4 | 5.2–5.5 | |
| High School Grad | 9.8 | 9.7–10.0 | |
| Less than High School | 4.4 | 4.2–4.5 | |
| Immigration | Immigrated > 10 years ago | 15.7 | 15.5–16.0 |
| Immigrated <10 years ago | 7.5 | 7.3–7.7 | |
| Canadian Born | 76.7 | 76.4–77.0 | |
| Homeownership | Homeowner | 73.5 | 73.1–73.8 |
| Renter | 26.5 | 26.2–26.9 | |
| Cycle of CCHS | 3.1 | 22.2 | 22.1–22.3 |
| 2007/08 | 25.5 | 25.4–25.6 | |
| 2009/10 | 25.6 | 25.6–25.7 | |
| 2011/12 | 26.6 | 26.6–26.7 | |
Derived from respondent's total household income before taxes adjusted by Canadian inflation rates for the year the respondent was surveyed (Statistics Canada, 2016). Inflation adjusted income was ranked (low-lower middle, middle, upper middle, and highest) based on the number of people in that household and national income thresholds (Canadian Institute for Health Information, 2015, Peel Public Health, 2011). Finally, the 4-level variable was dichotomized into low and medium-high income.
Includes: benefits from Canada or Quebec Pension Plan, Old Age Security and Guaranteed Income Supplement, Provincial or municipal social assistance or welfare and Child Tax Benefit.
Includes: Retirement pensions, child support, alimony and other.
Includes those who identify as: Black, Latin American, Arab, and Other (Multi-racial).
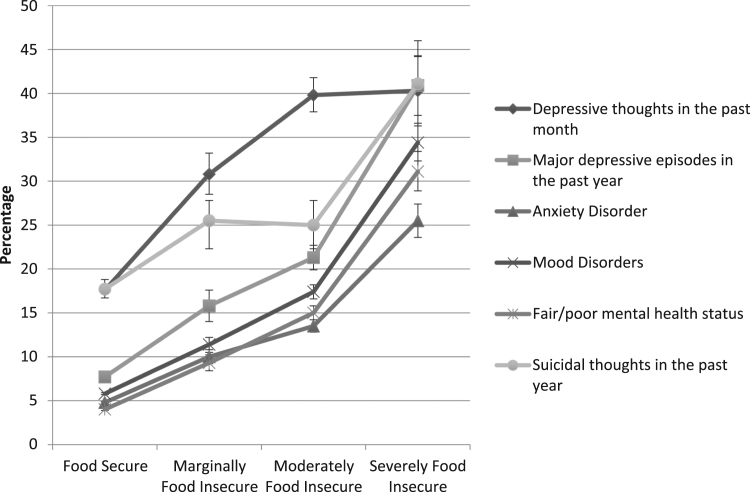
Fig. 1 presents the weighted and bootstrapped percent of Canadians reporting the six adverse mental health outcomes by each level of HFI. Overall, the percent of Canadian adults reporting six adverse mental health outcomes is positively correlated with the level of HFI. Six adverse mental health outcomes show a HFI gradient. There is nearly a two-fold difference in the burden of mental health outcomes between food secure and marginally food insecure households. Of particular concern are the extremely high percentages of adverse mental health outcomes reported among respondents in severely food insecure households, which range from 25.5% [95% CI: 23.6–36.6 anxiety disorders] to 41.1% [95% CI: 36.3–46.0, suicidal thoughts in past year].
Fig. 1.
Percent and 95% Confidence Intervals of Six Adverse Mental Health Outcomes Reported for Each Level of Household Food Insecurity (Unadjusted Prevalence).
Table 2 presents results from the marginal effect reduction analyses. In essence these results refer to the percent point reduction for the six adverse mental health outcomes if the respondent were to adopt the characteristics of the food secure referent group. Marginal effects provide insight into the impact of potential interventions that aim to reduce or remove HFI. Provided a severely food insecure households were to become food secure we can expect a 25.2% (22.4- 28.0) point reduction in the reporting of depressive thoughts in the past month as one example. Compared to all other covariates, HFI has the largest individual impact on the reporting of adverse mental health outcomes. Moreover, there is a significant reduction in mental health outcomes for all levels of HFI including marginal HFI if those households were to become food secure. For example, marginal reductions range from a percent point reduction of 3.44 [2.79–4.82] for anxiety disorders and 9.20 [7.10–11.3] for depressive thoughts in the past month.
Table 2.
Marginal Effects (in percent) and 95% Confidence Intervals of Study Variables on Six Outcomes from a Pooled Sample of Respondents from the Canadian Community Health Survey 2005–2012 (N = 302,683).
|
Marginal Effects | ||||||
|---|---|---|---|---|---|---|
| Depressive Thoughts in the Past Montha | Major Depressive Episodes in the Past Yearb | Anxiety Disordersc | Mood Disordersd | Fair/Poor Mental Health Statuse | Suicidal Thoughts in the Past Yearf | |
| Household Food Insecurity Status | ||||||
| Food Secure (referent) | 9.20*** | 3.79*** | 3.44*** | 3.95*** | 3.63*** | 7.82** |
| Marginal | (7.10–11.3) | (2.76–4.82) | (2.79–4.09) | (3.25–4.66) | (3.00–4.27) | (3.87–11.8) |
| Moderate | 14.5*** | 6.61*** | 4.63*** | 6.39*** | 5.70*** | 5.91*** |
| (12.9–16.1) | (5.87–7.34) | (4.12–5.15) | (5.84–6.94) | (5.22–6.18) | (3.12– 8.71) | |
| Severe | 25.2*** | 12.4*** | 8.01*** | 11.1*** | 9.40*** | 16.0*** |
| (22.4–28.0) | (11.3–13.6) | (7.24–11.1) | (10.3–11.9) | (8.60–10.2) | (12.1–19.9) | |
*P < 0.05, **P < 0.01, ***P < 0.001.
Adjusted by: sex, age, marital status, education, ethnicity, immigration status, income source, total household income, sense of belonging, homeownership and cycle of CCHS.
Adjusted by: sex, age, marital status, education, immigration status, income source, total household income, sense of belonging and cycle of CCHS.
Adjusted by: sex, marital status, education, ethnicity, immigration, income sources, total household income, sense of belonging, homeownership and cycle of CCHS.
Adjusted by: sex, age, marital status, household composition, ethnicity, immigration status, income source, total household income, sense of belonging, homeownership and cycle of CCHS.
Adjusted by: sex, age, marital status, household composition, education, immigration status, income source, total household income, sense of belonging, homeownership and cycle of CCHS.
Adjusted by: marital status, household composition, education, ethnicity, immigration status, income source and sense of belonging.
Discussion
We observed a HFI gradient for six adverse mental health outcomes, suggesting support for a possible dose-response relationship between HFI and adverse mental health outcomes. In general, increasingly severe HFI is associated with an increased risk of reporting six adverse mental health outcomes, with varying steepness of the gradient dependent on the mental health outcome. These relationships remained significant after adjustment for a wide range of demographic and socioeconomic covariates, including those factors typically associated with socioeconomic status such as low household income. As expected, the highest risk was among those reporting severe HFI but individuals reporting marginal HFI were also at increased risk of reporting all six adverse mental health outcomes.
We also found that marginal HFI was statistically significantly related to the risk of reporting all six adverse mental health outcomes with odds ratios, thus supporting the disaggregation of HFI into a four-level variable.
Mental illness derives from a complex interplay among genetic, biological, individual and social factors (for a review, see Public Health Agency of Canada, 2002). Current psychosocial research on the development of mental illness has emphasized the importance of stress in the pathway leading to mental illness regardless of whether the perspective is biological or sociocultural (Kessler et al., 1999, Meyer, 2003, Cohen et al., 1997, Cadoret et al., 1972). Within this complex interplay, HFI is a well-documented source of anxiety and stress among affected households (Hamelin et al., 2002, Runnels et al., 2011, Sim et al., 2011, Tarasuk, 2001) and is a modifiable factor that should not be overlooked.
The marginal effect reduction analyses offer an estimation of the substantive reductions in mental health outcomes one could expect with the removal of HFI. If those who are experiencing severe HFI were to become food secure, we could expect a percent point reduction between 8.01 and 25.2 for anxiety disorders and depressive thoughts in the past month, respectively.
In cross-sectional analyses such as this study, one cannot discern causality but our models assume that severe HFI acts as a chronic stressor leading to deleterious mental health outcomes. Recently, theorists (Melchior et al., 2009; Garg, Toy, Tripodis, Cook, Cordella, 2014; Huddleston-Casas, Charnigo, & Simmons, 2009) have begun to hypothesize a bidirectional relationship between HFI and mental health, whereby poor mental health results in a loss of productivity which can result in depletion in financial and social resources needed to buffer against HFI. This hypothesized bi-directionality of effect provides a unique opportunity to decrease the burden of both conditions (in this case HFI and adverse mental health conditions) by reducing the prevalence of one of the hypothesized stressors in the causal pathway towards the development of poor mental health. This study has shown that severe HFI, in particular, is an extremely stressful condition that has an independent impact on six adverse mental health outcomes. That being said, HFI can be modified through population health interventions.
Population health interventions aim to shift the risk curve (or reduce the gradient across levels of risk) for an entire population (Marmot et al., 2008, Halfon et al., 2009). Interventions directed at reducing HFI include income supports, income volatility protection, labour and social protections, income transfers and better access to higher education (McIntyre, 2013, Sriram and Tarasuk, 2015, Loopstra et al., 2015, McIntyre, 2011, McIntyre et al., 2016a). These interventions aim to improve the overall health of a population and reduce the steepness of the health gradient. Currently in Ontario, a basic income pilot project for working-age Canadians is being proposed, which could have important impacts on the prevalence of HFI in Canada and subsequent reductions in adverse mental health outcomes (Emery et al., 2013, McIntyre et al., 2016a, McIntyre et al., 2016b). Due to forthcoming income-based policy in Canada, hypothesizing the mental health impact of the reduction of HFI on mental health outcomes is timely and necessary.
Strengths
This study addresses an important social and political issue–HFI and mental health through analysis of a large and robust national dataset, which included a validated module for the ascertainment of HFI. The pooling of four cycles of the CCHS yielded a sample size that permitted use of a 4-level HFI variable while maintaining statistical power. The present study establishes the impact of marginal food insecurity on self-reported mental health, major depressive episodes and depressive thoughts for Canadian adults, which has been previously unreported in the literature. The study further examined the impact of HFI on mood and anxiety disorders separately, whereas the two conditions have been combined in past literature (Tarasuk et al., 2013). Previous studies have observed a HFI gradient of mental health impact on children and adolescents (Burke et al., 2016); this study contributes to the literature by examining this relationship for Canadian adults.
The advantage of the disaggregation of HFI into four categories is the ability to show a distinct increase in risk of reporting mental health outcomes with increasing HFI severity. The present study is unique in that it examines the relationship between a 4-level HFI variable and three previously unstudied mental health outcomes (self-reported mental health, major depressive episodes and depressive thoughts) in Canadian adults, as well as examining three previously studied mental health outcomes (suicidal thoughts in the past year, anxiety disorders and mood disorders) (Tarasuk et al., 2013, Davison et al., 2015).
Limitations
A longitudinal survey would have been ideal to study the temporal relationship between mental health and HFI. Given established difficulties relating to tracking and loss-to-follow-up of socially marginalized individuals (McKenzie, Tulsky, Long, & Moss, 1999), the use of cross-sectional data on the Canadian population was the best available method to answer an exploratory research question. In addition, although the CCHS does not include certain respondents, including the homeless, our results are likely an underestimation of the prevalence of HFI in Canada.
It should be noted that in quantitative research there is a fine balance between Type I and Type II error. This large sample size puts this study at risk of Type I error or the probability of rejecting a null hypothesis when it is in fact true (Oleckno, 2008). One way to avoid the probability of committing Type I error is narrowing the confidence intervals to increase the difficulty of rejecting a null hypothesis. This study employed a bootstrapping method which results in more narrow confidence intervals. In addition, while Type I error cannot be avoided, the six adverse mental health outcomes vary in terms of sample size. For example the outcome “mood disorders” has an n = 302,623 while “suicidal thoughts in the past year” has an n = 15,856. Despite the variation in sample size, HFI is statistically significantly related to both outcomes, which strengthens confidence in the validity of the findings.
When utilizing self-reported mental health variables there is always the potential for measurement error. This error could be occurring in the outcome variables “suicidal thoughts in the past year” and “depressive thoughts in the past month” where response rates were lowest. Despite this, the variable assessing Major Depressive Episodes (MDE) is a validated measure based on the CIDI-short form (with a 90% probability of caseness). In addition, two of the “self-reported” variables are physician diagnosed and would likely be an underestimation of effect due to social desirability bias rather than an overestimation. In addition, self-reported mental health status has been shown to be a valid and reliable measure of general mental health (Mawani & Gilmour, 2010). It can be speculated that the HFI variable and the mental health outcomes could be positively correlated due to their self-reported nature, which could result in measurement error if the two variables are not independent.
Many of the variables, including mental health outcomes, included in this analysis were at the individual level but the HFSSM produces a household-level variable. Therefore, it must be stated that the level of food insecurity felt by a household does not necessarily mean each individual in that household experiences the same level of food insecurity. Given that all respondents below the age of 18 were eliminated from this dataset, this study analyzed adults in the household and, therefore, it is more likely that the HFI level was related to the adult respondent’s individual food insecurity status. Again, misclassification bias would be expected to attenuate the findings.
Finally, this study utilizes the Canadian measure of HFI that uses a slightly more lenient definition of moderate food insecurity compared with the American measure. Despite evidence that the Canadian HFSSM measures the same phenomenon and when directly compared to the US measure has been shown to be reliable and valid (Health Canada, 2007; Nord & Hopwood, 2008), it is important to read these findings in a Canadian context and use care when interpreting the moderate food insecurity findings in an American context.
Conclusion
Many studies have been published on the association between HFI and poor mental health in a variety of high-income countries (Carter et al., 2011, Davison and Kaplan, 2015, Davison et al., 2015, Fuller-Thomson and Nimigon, 2008, Heflin et al., 2005, Leung et al., 2015, Pryor et al., 2016, Siefert et al., 2004, Stuff et al., 2004, Tarasuk et al., 2013, Vozoris and Tarasuk, 2003, Muldoon et al., 2013, Whitaker et al., 2006). These studies generally conclude that HFI results in, or is associated with‚ poor mental health outcomes. In this study, we extend the finding that HFI is an independent risk factor for adverse mental health outcomes through an examination of how the HFI gradient leads to increasing risk of six outcomes at each increased level of severity.
We theorize that severe HFI could be regarded as a chronic stressor with significant effects on population-level mental health. Within the complex interplay of genetics, social and biological factors hypothesized as the source of the development of adverse mental health conditions, HFI is readily modifiable through income-based interventions and its reduction. In particular the elimination of severe HFI could have a substantial quantifiable impact on the mental health of affected Canadians, or other residents of high income countries with a similar profile of HFI and mental health burden.
Conflicts of interest
We have no conflicts of interest or financial disclosures.
Acknowledgments
This study was supported by a Programmatic Grant in Health and Health Equity from the Canadian Institutes of Health Research (CIHR) (Grant no. FRN 115208) and a CIHR Graduate Student Award. We thank Dr. Cynthia Kwok for her manuscript review.
Footnotes
Pooling CCHS data requires that three assumptions be met: the same characteristics must be assessed from cycle to cycle, the same population must be targeted across cycles, and the “mode effect” (that the same method of data collection must occur across cycles) (Thomas & Wannell, 2009). All three of these assumptions were met in this analysis.
In order to be administered the HFSSM, all respondents were asked to answer a screening question referring to their household food situation. The responses on the screening question were not included in the HFSSM score.
Appendix A
See:Table A1.
Table A1.
Description of Outcome Variables Included in Study.
| Name of Variable | Level of Measurement | Survey Question | Description |
|---|---|---|---|
| Depressive Thoughts in the Past Month | Binary (Yes, No) | “During the past month, about how often did you feel sad or depressed?” | Those who responded all of the time, most of the time, some of the time were coded into the “yes” group. All other respondents were coded into the “no” group. |
| Major Depressive Episodes in the Past Year | Binary (Yes, No) | The Composite International Diagnostic Interview Short Form (CIDI-SF) measures Major Depressive Episodes (MDE). This subset of questions assesses the depressive symptoms of respondents who felt depressed or lost interest in things for 2 weeks or more in the last 12 months. Respondents are screened into the CIDI-SF based on affirmative responses to the following 2 screening questions, if a respondent answers affirmatively to the screening questions, their depression level is measured based on 7 additional questions. | The classification of depression is based on an affirmative response to the original screening question and 5 out of 9 of the depression questions. This corresponds to a 90% predictive probability of caseness, which closely aligns with the DSM-5 diagnostic guidelines for MDE in adults (American Psychiatric Association, 2013). This probability expresses the chance that the respondent would have been diagnosed as having experienced a Major Depressive Episode in the past 12 months had they completed the CIDI Long-Form (Statistics Canada, 2007). |
| Anxiety Disorder | Binary (Yes, No) | “Do you have an anxiety disorder such as phobia, obsessive-compulsive disorder or a panic disorder?” | Respondents are reminded that the question is only referring to those conditions diagnosed by a health professional in the past 6 months. |
| Mood Disorder | Binary (Yes, No) | “Do you have a mood disorder such as depression, bipolar disorder, mania or dysthymia?” | Respondents are reminded that the question only refers to those conditions diagnosed by a health professional in the past 6 months. |
| Suicidal Thoughts in the Past Year | Binary (Yes, No) | “Have you ever seriously considered committing suicide or taking your own life? Has this happened in the past 12 months?” | This variable was recoded into a dichotomous variable. In addition, those who answered “not applicable: were coded into the ”no” group, given they answered negatively to this question in an earlier prompt. |
| Self-Reported Mental Health Status | Binary (Fair/Poor, Good/Very Good/Excellent) | “In general, would you say your mental health is: excellent, very good, good, fair, or poor?” | This variable was recoded into a dichotomous variable. “Fair/poor” or “Good/very good/excellent”. This variable has been validated and is a reliable measure of general mental health (Mawani & Gilmour, 2010) |
References
- American Psychiatric Association . American Psychiatric Pub; 2013. Diagnostic and statistical manual of mental disorders (DSM-5®) [Google Scholar]
- Bennett D. How can I deal with missing data in my study? Australian and New Zealand Journal of Public Health. 2001;25(5):464–469. [PubMed] [Google Scholar]
- Bhattacharya J., Currie J., Haider S. Poverty, food insecurity, and nutritional outcomes in children and adults. Journal of Health Economics. 2004;23(4):839–862. doi: 10.1016/j.jhealeco.2003.12.008. [DOI] [PubMed] [Google Scholar]
- Bickel, G., Nord, M., Price, C., Hamilton, W., Cook, J., Guide to measuring household food security, Revised 2000. US Department of Agriculture. Alexandria VA: Food and Nutrition Service, March 2000.
- Burke M.P., Martini L.H., Çayir E., Hartline-Grafton H.L., Meade R.L. Severity of household food insecurity is positively associated with mental disorders among children and adolescents in the United States. The Journal of Nutrition. 2016:1–8. doi: 10.3945/jn.116.232298. [DOI] [PubMed] [Google Scholar]
- Burns J.K. Poverty, inequality and a political economy of mental health. Epidemiology and Psychiatric Sciences. 2015;24(24):107–113. doi: 10.1017/S2045796015000086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman P., Gottlieb L. The social determinants of health: It’s time to consider the causes of the causes. Public Health Reports. 2014;129(1):19–31. doi: 10.1177/00333549141291S206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadoret R.J., Winokur G., Dorzab J., Baker M. Depressive disease: Life events and onset of illness. Archives of General Psychiatry. 1972;26(2):133–136. doi: 10.1001/archpsyc.1972.01750200037008. [DOI] [PubMed] [Google Scholar]
- Cameron, A.C., Trivedi, P.K., Microeconometrics: methods and applications. Cambridge: Cambridge University Press, 2005.
- Canadian Institute for Health Information, Trends in income-related health inequalities in Canada: Methodology notes. Ottawa, ON: CIHI, 2015.
- Carter K.N., Kruse K., Blakely T., Collings S. The association of food security with psychological distress in New Zealand and any gender differences. Social Science Medicine. 2011;72(9):1463–1471. doi: 10.1016/j.socscimed.2011.03.009. [DOI] [PubMed] [Google Scholar]
- Chen J., Chen J. Food insecurity in Canadian households. Health Rep. 2001;12(4):11–22. [PubMed] [Google Scholar]
- Cohen S., Kessler R.C., Gordon L.U. Oxford University Press; New York, NY: 1997. Measuring stress: A guide for health and social scientists. [Google Scholar]
- Cook J.T., Frank D.A., Berkowitz C., Black M.M., Casey P.H., Cutts D.B., Nord M. Food insecurity is associated with adverse health outcomes among human infants and toddlers. The Journal of Nutrition. 2004;134(6):1432–1438. doi: 10.1093/jn/134.6.##. [DOI] [PubMed] [Google Scholar]
- Davison K., Kaplan B. Food insecurity in adults with mood disorders: Prevalence estimates and associations with nutritional and psychological health. Annals of General Psychiatry. 2015;14(21):1–7. doi: 10.1186/s12991-015-0059-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davison K.M., Marshall-Fabien G.L., Tecson A. Association of moderate and severe food insecurity with suicidal ideation in adults: National survey data from three Canadian provinces. Social Psychiatry and Psychiatric Epidemiology. 2015;50(6):963–972. doi: 10.1007/s00127-015-1018-1. [DOI] [PubMed] [Google Scholar]
- Deraspe, R., Current issues in mental health in Canada: the economic impact of mental illness (Publication No.2013-87-E).Ottawa, ON: Library of Parliament, 2013.
- Eicher-Miller H.A., Mason A.C., Weaver C.M., McCabe G.P., Boushey C.J. Food insecurity is associated with iron deficiency anemia in US. American Journal of Clinical Nutrition. 2009;90(5):1358–1371. doi: 10.3945/ajcn.2009.27886. [DOI] [PubMed] [Google Scholar]
- Emery J.C.H., Bartoo A.C., Matheson J., Ferrer A., Kirkpatrick S.I., McIntyre L. Evidence of the association between household food insecurity and heating cost inflation in Canada, 1998–2001. Canadian Public Policy. 2012;38(2):181–215. [Google Scholar]
- Emery J.C.H., Fleisch V., McIntyre L. How a guaranteed annual income could put food banks out of business. School of Public Policy Research. 2013;6(37):1–20. [Google Scholar]
- Evans W., Wolfe B., Adler N. The SES and health gradient: A brief review of the literature. In: Wolfe B., Evans W., Seeman T.E., editors. Biological consequences of socioeconomic inequalities. Russell Sage Foundation; New York: 2012. pp. 1–37. [Google Scholar]
- Fryers T., Melzer D., Jenkins R. Social inequalities and the common mental disorders. Social Psychiatry and Psychiatric Epidemiology. 2003;38(5):229–237. doi: 10.1007/s00127-003-0627-2. [DOI] [PubMed] [Google Scholar]
- Fuller-Thomson E., Nimigon J. Factors associated with depression among individuals with chronic fatigue syndrome: Findings from a nationally representative survey. Family Practice. 2008;25(6):414–422. doi: 10.1093/fampra/cmn064. [DOI] [PubMed] [Google Scholar]
- Garg A., Toy S., Tripodis Y., Cook J., Cordella N. Influence of maternal depression on household food insecurity for low-income families. Academic Pediatrics. 2014;15(3):305–310. doi: 10.1016/j.acap.2014.10.002. [DOI] [PubMed] [Google Scholar]
- Government of Canada (2006). The human face of mental health and mental illness in Canada 2006. Minister of Public Works and Government Services Canada. Retrieved from: 〈http://www.phac-aspc.gc.ca/publicat/human-humain06/pdf/human_face_e.pdf〉.
- Gucciardi E., Vogt J.A., DeMelo M., Stewart D.E. Exploration of the relationship between household food insecurity and diabetes in Canada. Diabetes Care. 2009;32(12):2218–2224. doi: 10.2337/dc09-0823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadley C., Crooks D.L. Coping and the biosocial consequences of food insecurity in the 21st century. American Journal of Physical Anthropology. 2012;149(S55):72–94. doi: 10.1002/ajpa.22161. [DOI] [PubMed] [Google Scholar]
- Halfon N., Larson K., Russ S. Why social determinants? Healthcare Quarterly. 2009;14:8–20. doi: 10.12927/hcq.2010.21979. [DOI] [PubMed] [Google Scholar]
- Hamelin A.M., Beaudry M., Habicht J.P. Characterization of household food insecurity in Quebec: Food and feelings. Social Science Medicine. 2002;54(1):119–132. doi: 10.1016/s0277-9536(01)00013-2. [DOI] [PubMed] [Google Scholar]
- Health Canada, Office of nutrition policy and promotion. canadian community health survey, Cycle 2.2, Nutrition (2004)–Income-Related Household Food Security in Canada. Ottawa: Health Canada, 2007.
- Heflin C.M., Siefert K., Williams D.R. Food insufficiency and women’s mental health: Findings from a 3-year panel of welfare recipients. Social Science Medicine. 2005;61(9):1971–1982. doi: 10.1016/j.socscimed.2005.04.014. [DOI] [PubMed] [Google Scholar]
- Huddleston-Casas C., Charnigo R., Simmons L.A. Food insecurity and maternal depression in rural, low-income families: A longitudinal investigation. Public Health Nutrition. 2009;12(8):1133–1140. doi: 10.1017/S1368980008003650. [DOI] [PubMed] [Google Scholar]
- Inuit Circumpolar Council, Food security across the arctic, 2012 Retrieved from 〈http://www.inuitcircumpolar.com/uploads/3/0/5/4/30542564/icc_food_security_across_the_arctic_may_2012.pdf〉.
- Institute of Medicine (US). 2003. Committee on assuring the health of the public in the 21st century. The future of the public's health in the 21st century. Washington, D.C: National Academy Press.
- Kessler R.C., Mickelson K.D., Williams D.R. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of Health and Social Behavior. 1999;40(3):208–230. [PubMed] [Google Scholar]
- Kirkpatrick S.I., Tarasuk V. Food insecurity is associated with nutrient inadequacies among Canadian adults and adolescents. The Journal of Nutrition. 2008;138(3):604–612. doi: 10.1093/jn/138.3.604. [DOI] [PubMed] [Google Scholar]
- Leung C.W., Epel E.S., Willett W.C., Rimm E.B., Laraia B.A. Household food insecurity is positively associated with depression among low-income supplemental nutrition assistance program participants and income-eligible nonparticipants. The Journal of Nutrition. 2015;145(3):622–627. doi: 10.3945/jn.114.199414. [DOI] [PubMed] [Google Scholar]
- Loopstra R., Dachner N., Tarasuk V. An exploration of the unprecedented decline in the prevalence of household food insecurity in Newfoundland and Labrador, 2007–2012. Canadian Public Policy. 2015;41(3):191–206. [Google Scholar]
- Lorant V., Deliège D., Eaton W., Robert A., Philippot P., Ansseau M. Socioeconomic inequalities in depression: A meta-analysis. American Journal of Epidemiology. 2003;157(2):98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Marmot M., Friel S., Bell R., Houweling T.A., Taylor S., Commission on Social Determinants of Health Closing the gap in a generation: Health equity through action on the social determinants of health. The Lancet. 2008;372(9650):1661–1669. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- Mawani F.N., Gilmour H. Validation of self-rated mental health. Health Reports. 2010;21(3):1–15. [PubMed] [Google Scholar]
- McIntyre L. Food insecurity policy is not the flipside of food security policy. Policy Options. 2011;32(7):48–51. 〈http://policyoptions.irpp.org/magazines/agri-food-policy/food-insecurity-policy-is-not-the-flipside-of-food-security-policy/〉 (Retrieved from) [Google Scholar]
- McIntyre, L., Policy framing of household food insecurity in Canada, 2013. Retrieved from 〈http://www.centrelearoback.org/assets/PDF/CLR-GCPB131212_McIntyre_PresEn.pdf〉.
- McIntyre L., Dutton D.J., Kwok C., Emery J.C.H. Reduction of food insecurity among low-income Canadian seniors as a likely impact of a guaranteed annual income. Canadian Public Policy September. 2016:274–286. doi: 10.17269/cjph.107.5372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre L., Kwok C., Emery J.C.H., Dutton D.J. Impact of a guaranteed annual income program on Canadian seniors' physical, mental and functional health. Canadian Journal of Public Health. 2016;107(2):176. doi: 10.17269/cjph.107.5372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKenzie M., Tulsky J.P., Long H.L., Moss A. Tracking and follow-up of marginalized populations: A review. Journal of Health Care for the Pool and Underserved. 1999;10(4):409–429. doi: 10.1353/hpu.2010.0697. [DOI] [PubMed] [Google Scholar]
- McKnight P.E., McKnight K.M., Sidani S., Figueredo A.J. Guilford Press; New York: 2007. Missing data: A gentle introduction. [Google Scholar]
- Melchior M., Caspi A., Howard L.M., Ambler A.P., Bolton H., Mountain N., Moffitt T.E. Mental health context of food insecurity: A representative cohort of families with young children. Pediatrics. 2009;124(4):e564–e572. doi: 10.1542/peds.2009-0583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer I.H. Prejudice as stress: Conceptual and measurement problems. American Journal of Public Health. 2003;93(2):262–265. doi: 10.2105/ajph.93.2.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muirhead V.E., Quiñonez C., Figueiredo R., Locker D. Predictors of dental care utilization among working poor Canadians. Community Dentistry and Oral Epidemiology. 2009;37(3):199–208. doi: 10.1111/j.1600-0528.2009.00471.x. [DOI] [PubMed] [Google Scholar]
- Muldoon K.A., Duff P.K., Fielden S., Anema A. Food insufficiency is associated with psychiatric morbidity in a nationally representative study of mental illness among food insecure Canadians. Social Psychiatry and Psychiatric Epidemiology. 2013;48(5):795–803. doi: 10.1007/s00127-012-0597-3. [DOI] [PubMed] [Google Scholar]
- Nord M., Hooper M.D., Hopwood H. Household-Level income-related food insecurity is less prevalent in Canada than in the United States. Journal of Hunger Environmental Nutrition. 2008;3(1):17–35. [Google Scholar]
- Olabiyi O.M., McIntyre L. Determinants of food insecurity in higher-income households in Canada. Journal of Hunger Environmental Nutrition. 2014;9(4):433–448. [Google Scholar]
- Oleckno W.A. Waveland Press; Long Grove: 2008. Epidemiology: Concepts and methods. [Google Scholar]
- Peel Public Health (2011). Health in peel: Determinants and disparities. Mississauga, ON: Region of Peel.
- Pryor L., Lioret S., van der Waerden J., Fombonne É., Falissard B., Melchior M. Food insecurity and mental health problems among a community sample of young adults. Social Psychiatry and Psychiatric Epidemiology. 2016;51(8):1073–1081. doi: 10.1007/s00127-016-1249-9. [DOI] [PubMed] [Google Scholar]
- Public Health Agency of Canada, A report of mental illness in Canada. Ottawa, ON: Public Health Agency of Canada, 2002.
- Raphael D., Mikkonen J. York University School of Health Policy and Management; Toronto, ON: 2010. Social determinants of health: The Canadian facts. [Google Scholar]
- Roberts G., Grimes K. Canadian Institute for Health Information; Ottawa, ON: 2011. Return on investment: Mental health promotion and mental illness prevention.〈http://www.cpa.ca/docs/File/Practice/roi_mental_health_report_en.pdf〉 (Retrieved from) [Google Scholar]
- Roshanafshar, S., Hawkins, E., Food insecurity in Canada. Health at a Glance, 2015. Available from: 〈http://www.statcan.gc.ca/pub/82-624-x/2015001/article/14138-eng.pdf〉.
- Runnels V.E., Kristjansson E., Calhoun M. An investigation of adults' everyday experiences and effects of food insecurity in an urban area in Canada. Canadian Journal of Community Mental Health. 2011;30(1):157–172. [Google Scholar]
- Saiz A.M., Aul A.M., Malecki K.M., Bersch A.J., Bergmans R.S., LeCaire T.J., Nieto F.J. Food insecurity and cardiovascular health: Findings from a statewide population health survey in Wisconsin. Preventive Medicine. 2016;93:1–6. doi: 10.1016/j.ypmed.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer J. Multiple imputation: A primer. Statistical Methods in Medical Research. 1999;8:3–15. doi: 10.1177/096228029900800102. [DOI] [PubMed] [Google Scholar]
- Seligman H.K., Laraia B.A., Kushel M.B. Food insecurity is associated with chronic disease among low-income NHANES participants. The Journal of Nutrition. 2010;140(2):304–310. doi: 10.3945/jn.109.112573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siefert K., Heflin C.M., Corcoran M.E., Williams D.R. Food insufficiency and physical and mental health in a longitudinal survey of welfare recipients. Journal of Health and Social Behavior. 2004;45(2):171–186. doi: 10.1177/002214650404500204. [DOI] [PubMed] [Google Scholar]
- Sim S.M., Glanville N.T., McIntyre L. Food management behaviours in food-insecure, lone mother-led families. Canadian Journal of Dietetic Practice and Research. 2011;72(3):123–129. doi: 10.3148/72.3.2011.123. [DOI] [PubMed] [Google Scholar]
- Smetanin, P., Stiff, D., Briante, C., Adair, C.E., Ahmad, S., Khan, M., The life and economic impact of major mental illnesses in Canada: 2011 to 2041. RiskAnalytica, on behalf of the Mental Health Commission of Canada, 2011. Retrieved from: 〈http://www.mentalhealthcommission.ca/sites/default/files/MHCC_Report_Base_Case_FINAL_ENG_0_0.pdf〉.
- Sriram U., Tarasuk V. Changes in household food insecurity rates in Canadian metropolitan areas from 2007 to 2012. Canadian Journal of Public Health. 2015;106(5):e322–e327. doi: 10.17269/cjph.106.4893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp, Stata Statistical Software: Release 14. College Station, TX: StataCorp LP, 2015.
- Statistics Canada, Canadian Community Health Survey–Mental Health, 2013.
- Statistics Canada . Statistics Canada; Ottawa, ON: 2016. The Consumer Price Index. [Google Scholar]
- Statistics Canada, User Guide, Public-use Microdata File, Canadian Community Health Survey. Ottawa, Ontario, 2007.
- Stuff J.E., Casey P.H., Szeto K.L., Gossett J.M., Robbins J.M., Simpson P.M., Bogle M.L. Household food insecurity is associated with adult health status. The Journal of Nutrition. 2004;134(9):2330–2335. doi: 10.1093/jn/134.9.2330. [DOI] [PubMed] [Google Scholar]
- Tarasuk, V., Discussion paper on household and individual food insecurity. Health Canada, 2001. Retrieved from: 〈http://www.hsfspark.com/sites/default/files/Tarasuk-%20Discussion%20paper%20on%20food%20security.pdf〉.
- Tarasuk V., Cheng J., de Oliveira C., Dachner N., Gundersen C., Kurdyak P. Association between household food insecurity and annual health care costs. Canadian Medical Association Journal. 2015;187(14):E429–E436. doi: 10.1503/cmaj.150234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarasuk V., Dachner N., Loopstra R. Food banks, welfare, and food insecurity in Canada. British Food Journal. 2014;116(9):1405–1417. [Google Scholar]
- Tarasuk, V., Mitchell, A., Dachner, N., Household food insecurity in Canada, 2012. 2014. Retrieved from 〈http://proof.utoronto.ca〉.
- Tarasuk V., Mitchell A., McLaren L., McIntyre L. Chronic physical and mental health conditions among adults may increase vulnerability to household food insecurity. The Journal of Nutrition. 2013;143(11):1785–1793. doi: 10.3945/jn.113.178483. [DOI] [PubMed] [Google Scholar]
- Thomas S., Wannell B. Combining cycles of the Canadian Community Health Survey. Health Reports. 2009;20(1):53–58. [PubMed] [Google Scholar]
- Vozoris N.T., Tarasuk V.S. Household food insufficiency is associated with poorer health. The Journal of Nutrition. 2003;133(1):120–126. doi: 10.1093/jn/133.1.120. [DOI] [PubMed] [Google Scholar]
- Whitaker R.C., Phillips S.M., Orzol S.M. Food insecurity and the risks of depression and anxiety in mothers and behavior problems in their preschool-aged children. Pediatrics. 2006;118(3):e859–e868. doi: 10.1542/peds.2006-0239. [DOI] [PubMed] [Google Scholar]
- World Health Assembly . World Health Organization; Geneva: 2012. Global burden of mental disorders and the need for a comprehensive, coordinated response from health and social sectors at the country level: Report by the Secretariat.〈http://apps.who.int/iris/bitstream/10665/78898/1/A65_10-en.pdf〉 (Retrieved from) [Google Scholar]
- Wu Z., Schimmele C.M. Food insufficiency and depression. Sociological Perspectives. 2005;48(4):481–504. [Google Scholar]