Abstract
There is growing interest in the relationship between socioeconomic status (SES), poverty, and mental health in low and middle-income countries (LMIC). However, it is not clear whether a gradient approach focused on a wider SES distribution or a binary poverty approach is more salient for mental health in LMIC. Yet this distinction has implications for interventions aimed at improving population health. We contribute to the literature by examining how multiple indicators of socioeconomic status, including gradient SES and binary poverty indicators, contribute to prenatal depression symptoms in a LMIC context. Prenatal depression is an important public health concern with negative sequela for the mother and her children. We use data on assets, education, food insecurity, debt, and depression symptoms from a sample of 1154 pregnant women residing in rural Pakistan. Women who screened positive for depression participated in a cluster randomized controlled trial of a perinatal depression intervention; all women were interviewed October 2015-February 2016, prior to the start of the intervention. Cluster-specific sampling weights were used to approximate a random sample of pregnant women in the area. Findings indicate that fewer assets, experiencing food insecurity, and having household debt are independently associated with worse depression symptoms. The association with assets is linear with no evidence of a threshold effect, supporting the idea of a gradient in the association between levels of SES and depression symptoms. A gradient was also initially observed with woman’s educational attainment, but this association was attenuated once other SES variables were included in the model. Together, the asset, food insecurity, and debt indicators explain 14% of the variance in depression symptoms, more than has been reported in high income country studies. These findings support the use of multiple SES indicators to better elucidate the complex relationship between socioeconomic status and mental health in LMIC.
Keywords: Socioeconomic status, Prenatal depression, Maternal depression, Poverty, LMIC, South Asia
Highlights
-
•
We compare the association between poverty, gradient measures of SES, and depression.
-
•
Above the poverty level, SES predict depression in a low income country.
-
•
Relying on simple, dichotomous, poverty measures in studies of mental health is not recommended.
Introduction
There is a growing interest in the relationship between socioeconomic status (SES), poverty, and mental health in lower and middle income countries (LMIC) (Lund et al., 2010, Lund et al., 2011; Burns, 2015). Recent reviews confirm that lower socioeconomic status is correlated with worse mental health outcomes (Lund et al., 2010, Coast et al., 2012), although the findings are not unequivocal (Das, Do, Friedman, McKenzie & Scott, 2007). For example, there is evidence that studies using domains such as education or financial stress yield more consistent results than those using income or expenditures (Araya, Lewis, Rojas & Fritsch, 2003). However, as this body of evidence grows, a distinction that is often overlooked is that between the construct of socioeconomic status, measured often as a gradient, and poverty, a binary indicator of deprivation below a demarcated threshold. Indeed, the terms SES and poverty are often used interchangeably (Lund et al., 2010). The failure to distinguish between SES and poverty may potentially explain differences in findings, and has implications for policies aimed at improving population health.
In general, SES, or socioeconomic position (SEP), refers to a person’s position in their community’s social hierarchy; it reflects a person’s access to key social and economic resources, including money, power, and social connections (Glymour, Avendano & Kawachi, 2014). SES exists on a continuum, or a gradient, and is usually understood as having multiple dimensions. Commonly used indicators of SES are occupation-based measures, income, expenditures, education, wealth/assets, as well as various composite measures (Galobardes, Shaw, Lawlor, Davey Smith & Lynch, 2006). Research from high income countries (HIC) has shown a clear gradient in the SES-health association, in that there are health benefits of belonging to every higher step on the SES ladder (Hemingway et al., 1997, Lorant et al., 2003). A discussion of poverty, on the other hand, focuses on those at the very bottom of the SES continuum. Poverty is a binary construct; the level below which “society deems it unacceptable to live”, a level of deprivation that prevents an individual from participating in normal life (Smith, 1776). Commonly used binary indicators of poverty in LMIC are living on less than $1 or $2 a day or home overcrowding, as well as qualitative indicators such as food insecurity. SES indicators can be dichotomized in a way to identify those who are most disadvantaged, i.e. poor, such as having no education vs. at least some education, or belonging to the bottom quintile of an income/expenditure distribution vs. everyone else.
The question of whether gradient indicators of SES or absolute poverty are most salient for mental health is important in that they may imply different mechanisms operating to influence health and, in turn, different potential policy solutions. If poverty is the key driver of negative health outcomes then interventions focused on the poorest in society would have the largest beneficial impact in reducing the burden of disease (i.e. the ‘high risk strategy’ (Rose, 1985)). However, if lower SES negatively impacts mental health relative to each higher step of the SES ladder, as has been found in HICs, then a broader strategy may be necessary to have the largest impact.
The majority of existing research on this topic focuses on Common Mental Disorders (CMDs) such as depression and anxiety. We extend this research by focusing our analysis on depression among women during the prenatal period, estimated to affect at least 16% of women in LMIC (Fisher et al., 2012). The majority of women who are depressed prenatally remain depressed postnatally (Rahman & Creed, 2007) and depression during this perinatal period has been linked with other health problems for the mother as well as with multiple negative developmental outcomes for her offspring (Brown and Lumley, 2000, Galler et al., 2004, Rahman et al., 2004, Gelaye et al., 2016, Maselko et al., 2016). Therefore, a better understanding of the relationship between socioeconomic status and depression during pregnancy can inform efforts to improve the mental health of mothers as well as to improve the developmental trajectories of their children.
The goal of this paper is to examine the relationship between multiple indicators of socioeconomic status, especially gradient SES and binary poverty indicators, and prenatal depression symptoms in a LMIC context. To do so, we use data from a community sample of pregnant women residing in rural Pakistan. First, we examine the association of multiple indicators of SES and poverty with prenatal depression symptoms. Finally, we conduct an exploratory analysis to see whether each SES and poverty indicator uniquely predicts depression symptoms, independent of the other indicators.
Methods
Sample
The data for the analysis come from the baseline data collection wave (during the prenatal period) of a cluster randomized controlled trial (c-RCT) of a perinatal depression intervention, the Thinking Healthy Peer Delivered Plus (THPP+) program. The study is situated in a rural area of Pakistan; sample recruitment and trial details are described elsewhere (Sikander et al., 2015, Turner et al., 2016). Briefly, all pregnant women living in 40 village clusters (half of which were randomized to the intervention and half to the control arm) were screened for depression during their third trimester of pregnancy using the Patient Health Questionnaire-9 cutoff score of 10 or greater (Kroenke, Spitzer & Williams, 2001). In order to be eligible to participate, women needed to be married, plan to reside in the study area, understand one of the study languages (Urdu, Punjabi, or Potohari), and not require immediate medical attention. All eligible women who screened positive were invited to participate in the c-RCT and an equal number of non-depressed women in each village were recruited to participate in the follow-up study. About one out of every three non-depressed women in the villages were recruited, resulting in a 1:1 ratio of women who screened positive for depression and those who did not. After the baseline prenatal interview, women in the intervention clusters began the program; and all women were interviewed during the postnatal period. The results presented in the current paper use data from the 1154 women in the baseline sample, all of whom were interviewed during third trimester of pregnancy prior to the start of the intervention.
Measures
Gradient indicators of socioeconomic status (SES)
Household assets index score
Data on assets were collected based on the Demographic and Health Survey (DHS) wealth index approach (Rutstein & Johnson, 2004). Questions cover domains such as ownership of land/home, animals, various household durable goods (TV, car, etc.), as well as items relating to type of home materials, access to water and sanitation. Asset data are considered one of the more valid and reliable indicators of SES, especially in LMIC, where data on factors such as income or expenditures are often unreliable (Kolenikov & Angeles, 2004).
As recommended in the literature, an “asset index” was generated rather than using each asset variable separately (Filmer and Pritchett, 2001, Kolenikov and Angeles, 2004, Vyas and Kumaranayake, 2006, Kolenikov and Angeles, 2009, Howe et al., 2012). To do so, categorical asset variables with more than 2 levels were transformed in to binary variables based on natural groupings agreed to by the study team (e.g. the 5 types of floor materials were combined to distinguish floors made of tiles and chips/terrazzo from all other types of flooring such as cement, bricks and mud). Using a preliminary cut of the data, items for which most (>90%) or few (<10%) owned the asset were excluded as these variables provided minimal information to distinguish between women in the study. Because the proportion of variance explained was important, the polychoric correlation principle components approach was applied to the remaining 22 binary assets using the polychoricpca command in Stata (version 14.1) (Kolenikov & Angeles, 2004). In simulations (Kolenikov & Angeles, 2009), this approach has been shown to perform better than the traditional principal components approach which uses correlations based on multivariate normality of the assets (Filmer & Pritchett, 2001). The first principal component was used as the asset index (Filmer & Pritchett, 2001); it explained 41% of the overall variability in assets. Specifically, it was used in a standardized form by subtracting the weighted mean and dividing by the weighted standard deviation (see Analysis for details of the weighting). This approach was preferred to that commonly used whereby study participants are classified in to three groups (e.g. “poor” the lowest 40%, “middle” the next 40%, and “rich” the top 20%).
Education
Each woman reported years of education completed for herself and her husband. Both values were recoded into the following categories of years to correspond to key thresholds for completion: none, primary (1–5), middle (6–8), secondary (9–10), higher secondary (11–12) and tertiary (>12). We coded the education variable categorically rather than continuously to be comparable to other studies examining education gradients in health outcomes. Additional analyses using a continuous indicator of education showed a similar pattern of results with no major thresholds in the association with depression observed (results not shown).
Binary indicators of poverty or financial stress
Food insecurity
A single question asked whether the family had sufficient money to purchase food for the family during the previous month.
Debt. A single question asked whether the household was currently in debt. As discussed more below, debt can be an indicator of financial stress in contexts with poorly functioning credit markets.
Outcome measures
Depression symptoms
The Patient Health Questionnaire (PHQ-9) was used as the main indicator of depression symptoms among the women in the study (Kroenke et al., 2001). The PHQ-9 inquires about frequency of depression symptoms in the last 2 weeks; it has been validated and used extensively in the region, including in Pakistan (Kroenke et al., 2001, Patel et al., 2008, Fraz et al., 2013, Gholizadeh et al., 2017). The score has a theoretical range of 0 to 27 and a cutoff of 10 or more is considered to be a positive screen for depression (Kroenke et al., 2001). In the current analyses, we use both the continuous score as a representation of depression symptom severity and the dichotomized score as an indicator of a positive screen and, hence, eligible for the future intervention (Sikander et al., 2015).
Other variables
Additional potential confounding variables used in the analysis include the woman’s age and number of living children (parity).
Analysis
To make the sample of 1154 women representative of the local population, we up-weighted non-depressed women to account for their sub-sampling during study sample recruitment (approximately 1 in 3) when all women were screened for depression. To do this, we created cluster-specific weights for the non-depressed (PHQ-9 score <10) women to match their sampling fraction, which varied slightly between clusters. All non-depressed women in a given cluster were weighted by the same value, the inverse of the proportion of non-depressed from the sample of women screened for depression that were subsequently enrolled in the study. This was in contrast to the depressed women who were all invited to participate in the c-RCT and therefore all received a weight of 1. All analyses and statistics computed using data from the 1154 women were weighted using the cluster-specific weights.
The SES variables, PHQ-9 scores, and demographic variables (woman’s age, parity) were summarized using means and standard deviations (SDs) for continuous variables and counts and percentages for categorical variables and were presented separately for depressed and non-depressed screened women in line with the sampling design. We then modeled the relationship between PHQ-9 total score and the SES (education and asset index) and poverty variables (debt and food insecurity) individually and in combined models using linear regression and generated figures with predicted values and 95% confidence intervals. Models with random intercepts for clusters were considered, but the random intercept covariance was estimated to be zero because the women were weighted so that the clusters were population representative and therefore the PHQ-9 score distribution was essentially the same in each cluster (i.e. there was no clustering effect on the outcome of PHQ-9 score). Therefore, linear regression was chosen. We adjusted all models for woman’s age and number of living children, and all analyses were weighted.
Results
After weighting the sample of 1154 pregnant women to make it representative of the population from which it was drawn, the women were on average 26.6 (SD=5.7; range = 18–45) years old; 32.3% were pregnant with their first child, and 39.3% already had two or more children. Among women, 12.7% had no education, 24.2% completed at least 10th grade, and 14.2% had some tertiary education. Husbands were more likely to have at least some education, with only 6.9% having no schooling at all, but were somewhat less likely to have any tertiary education with only 6.7% having gone to college. The weighted mean standardized asset index score was 0, with a standard deviation of 1 and a range of -2.6 to 1.3. For the two binary poverty indicators: 40.7% of families reported being in debt, and 10.9% responded that they did not have enough money to feed their families during the previous month.
Table 1 presents data on all measures by depression status for the sample of 1154 women. To better understand the contribution of each of the 22 individual assets to the overall asset index, Table 1 provides the “weights” applied to each level of each variable. Each individual’s asset index score is obtained by summing the relevant weight for each individual’s reported assets. Some assets were associated with a big decrease in the asset index score when absent from the household (e.g., bed with a score of -0.46 vs. 0.05 if present in the household), while others were associated with a big increase when present in the household (e.g., camera with a score of 0.36 vs. -0.07 if absent from the household). Pairwise polychoric correlations between the 22 assets indicate are presented in Supplemental Table 1. There was reasonable correlation between all five socioeconomic variables (Supplemental Table 2), with the strongest correlation between woman’s years of education and asset score (ρ= 0.56) as well as with assets and food insecurity (ρ = -0.40).
Table 1.
Participant characteristics by depression status.
| Depression Statusa |
||||||
|---|---|---|---|---|---|---|
| Depressed (N= 570) | Non-depressed (N= 584) | |||||
| Woman’s characteristics | ||||||
| PHQ-9 total score, mean (SD) | 14.7 | (3.7) | 2.8 | (2.5) | ||
| Woman’s age, mean (SD) | 27.0 | (4.8) | 26.4 | (4.3) | ||
| range | 18–45 | 18–40 | ||||
| No. of living children, n (%) | ||||||
| First Pregnancy | 137 | (24.0%) | 212 | (36.3%) | ||
| 1 to 3 | 363 | (63.7%) | 336 | (57.5%) | ||
| 4 or more | 70 | (12.3%) | 36 | (6.2%) | ||
| Binary poverty indicators | ||||||
| Food security, n (%) | ||||||
| Yes | 429 | (75.3%) | 534 | (91.4%) | ||
| No | 124 | (21.8%) | 39 | (6.7%) | ||
| Unknown | 17 | (3.0%) | 11 | (1.9%) | ||
| Family Debt, n (%) | ||||||
| Yes | 305 | (53.5%) | 206 | (35.3%) | ||
| No | 227 | (39.8%) | 331 | (56.7%) | ||
| Unknown | 38 | (6.7%) | 47 | (8.0%) | ||
| Socioeconomic indicators | ||||||
| Woman’s education, n (%) | ||||||
| None (0) | 107 | (18.8%) | 63 | (10.8%) | ||
| Primary (1–5) | 139 | (24.4%) | 87 | (14.9%) | ||
| Middle (6–8) | 107 | (18.8%) | 108 | (18.5%) | ||
| Secondary (9–10) | 126 | (22.1%) | 167 | (28.6%) | ||
| Higher secondary (11–12) | 46 | (8.1%) | 63 | (10.8%) | ||
| Tertiary (>12) | 45 | (7.9%) | 96 | (16.4%) | ||
| Husband’s education, n (%) | ||||||
| None (0) | 55 | (9.6%) | 33 | (5.7%) | ||
| Primary (1–5) | 67 | (11.8%) | 45 | (7.7%) | ||
| Middle (6–8) | 137 | (24.0%) | 105 | (18.0%) | ||
| Secondary (9–10) | 243 | (42.6%) | 286 | (49.0%) | ||
| Higher secondary (11–12) | 47 | (8.2%) | 65 | (11.1%) | ||
| Tertiary (>12) | 21 | (3.7%) | 50 | (8.6%) | ||
| Depression Status | ||||||
|---|---|---|---|---|---|---|
| Weighted asset score | Depressed (N= 570) | Non-depressed (N= 584) | ||||
| Assets | ||||||
| Standardized Asset Index, mean (SD) | -0.3 | (0.9) | 0.1 | (0.7) | ||
| Farm (own or rent) | ||||||
| Yes | 0.1065 | 281 | (49.3%) | 373 | (63.9%) | |
| No | -0.1396 | 289 | (50.7%) | 211 | (36.1%) | |
| Animals | ||||||
| Yes | 0.0545 | 302 | (53.0%) | 369 | (63.2%) | |
| No | -0.0758 | 268 | (47.0%) | 215 | (36.8%) | |
| Radio | ||||||
| Yes | 0.1725 | 98 | (17.2%) | 165 | (28.3%) | |
| No | -0.0510 | 472 | (82.8%) | 419 | (71.7%) | |
| Television | ||||||
| Yes | 0.0552 | 468 | (82.1%) | 518 | (88.7%) | |
| No | -0.3250 | 102 | (17.9%) | 66 | (11.3%) | |
| Fridge | ||||||
| Yes | 0.0936 | 420 | (73.7%) | 508 | (87.0%) | |
| No | -0.3856 | 150 | (26.3%) | 76 | (13.0%) | |
| Washing Machine | ||||||
| Yes | 0.1234 | 380 | (66.7%) | 453 | (77.6%) | |
| No | -0.3209 | 190 | (33.3%) | 131 | (22.4%) | |
| Water pump (electric) | ||||||
| Yes | 0.1332 | 308 | (54.0%) | 400 | (68.5%) | |
| No | -0.2118 | 262 | (46.0%) | 184 | (31.5%) | |
| Bed | ||||||
| Yes | 0.0488 | 496 | (87.0%) | 547 | (93.7%) | |
| No | -0.4616 | 74 | (13.0%) | 37 | (6.3%) | |
| Chair | ||||||
| Yes | 0.0451 | 487 | (85.4%) | 546 | (93.5%) | |
| No | -0.3872 | 83 | (14.6%) | 38 | (6.5%) | |
| Cabinet/cupboard | ||||||
| Yes | 0.0757 | 448 | (78.6%) | 525 | (89.9%) | |
| No | -0.4084 | 112 | (21.4%) | 59 | (10.1%) | |
| Clock | ||||||
| Yes | 0.0875 | 419 | (73.5%) | 507 | (86.8%) | |
| No | -0.3563 | 151 | (26.5%) | 77 | (13.2%) | |
| Sofa | ||||||
| Yes | 0.0933 | 426 | (74.7%) | 505 | (86.5%) | |
| No | -0.3906 | 144 | (25.3%) | 79 | (13.5%) | |
| Sewing Machine | ||||||
| Yes | 0.1334 | 326 | (57.2%) | 422 | (72.3%) | |
| No | -0.2463 | 244 | (42.8%) | 162 | (27.7%) | |
| Camera | ||||||
| Yes | 0.3644 | 64 | (11.2%) | 120 | (20.5%) | |
| No | -0.0693 | 506 | (88.8%) | 464 | (79.5%) | |
| Laptop/Computer/Tablet | ||||||
| Yes | 0.3372 | 102 | (17.9%) | 154 | (26.4%) | |
| No | -0.0964 | 468 | (82.1%) | 430 | (73.6%) | |
| Wrist-watch | ||||||
| Yes | 0.1986 | 201 | (35.3%) | 305 | (52.2%) | |
| No | -0.1553 | 369 | (64.7%) | 279 | (47.8%) | |
| Car/Truck/Tractor | ||||||
| Yes | 0.2552 | 77 | (13.5%) | 113 | (19.3%) | |
| No | -0.0504 | 493 | (86.5%) | 471 | (80.7%) | |
| Gas Cylinder | ||||||
| Yes | 0.1100 | 305 | (53.5%) | 386 | (66.1%) | |
| No | -0.1644 | 265 | (46.5%0 | 198 | (33.9%) | |
| Flush Toilet | ||||||
| Yes | 0.1149 | 299 | (52.5%) | 418 | (71.6%) | |
| No | -0.1889 | 271 | (47.5%) | 166 | (28.4%) | |
| Roof Material | ||||||
| Reinforced brick cement | 0.0829 | 342 | (60.0%) | 390 | (66.8%) | |
| Other | -0.1441 | 228 | (40.0%) | 194 | (33.2%) | |
| Wall Material | ||||||
| Baked bricks | 0.0328 | 497 | (87.2%) | 532 | (91.1%) | |
| Other | -0.2711 | 73 | (12.8%) | 52 | (8.9%) | |
| Floor Material | ||||||
| Chips or ceramix tiles | 0.1190 | 284 | (49.8%) | 353 | (60.4%) | |
| Other | -0.1469 | 286 | (50.2%) | 231 | (39.6%) | |
depression status defined as a score of 10 or more on the PHQ-9
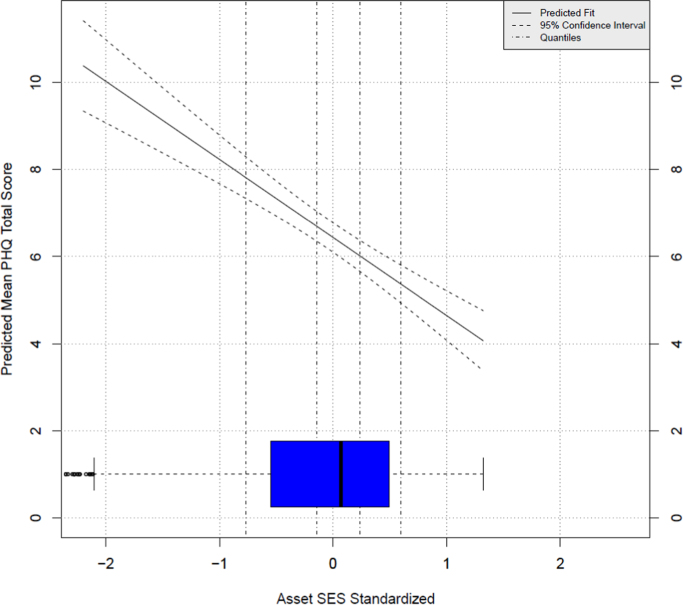
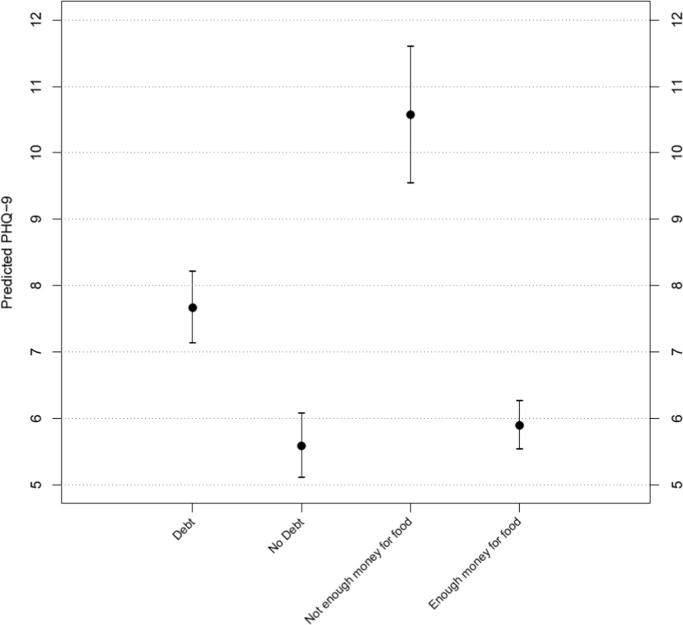
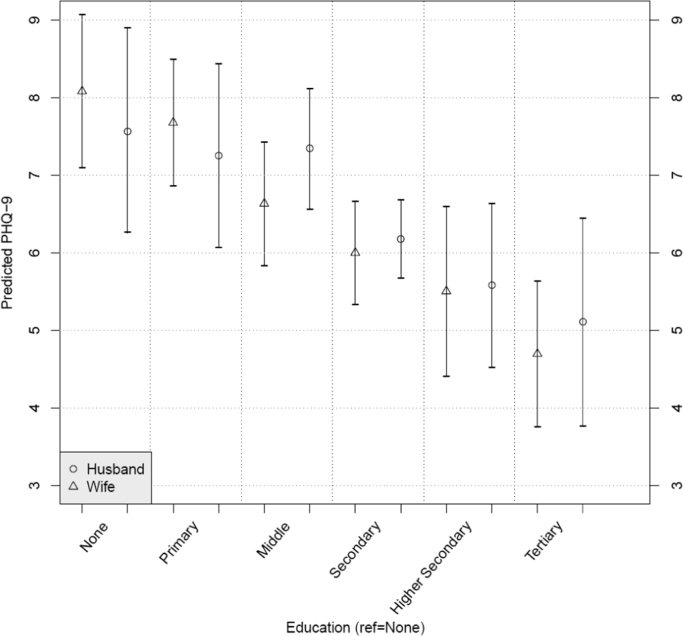
The association between the gradient SES indicators as well as the binary poverty measures with PHQ-9 scores are shown in Table 2. Regression coefficients for each predictor are modeled separately, with corresponding predicted PHQ-9 values shown for the asset index score (Fig. 1), for debt and food insecurity (Fig. 2) and for husband’s and woman’s education (Fig. 3).
Table 2.
SES variables and depression symptoms (PHQ-9 score), each predictor modeled separately.
| Variable of interest | Level | Coeff. | (95% CI) | P-value | Adjusted R-squared |
|---|---|---|---|---|---|
| Asset Index score | -1.79 | (-2.24, -1.34) | <0.001 | 0.093 | |
| Woman’s education | None (0) | reference | <0.001 | 0.071 | |
| Primary (1–5) | -0.41 | (-1.68, 0.86) | |||
| Middle (6–8) | -1.45 | (-2.72, -0.18) | |||
| Secondary (9–10) | -2.08 | (-3.28, -0.88) | |||
| Higher secondary (11–12) | -2.58 | (-4.07, -1.09) | |||
| Tertiary (>12) | -3.39 | (-4.78, -2.00) | |||
| Husband’s education | None (0) | reference | <0.001 | 0.056 | |
| Primary (1–5) | -0.31 | (-2.07, 1.45) | |||
| Middle (6–8) | -0.22 | (-1.75, 1.31) | |||
| Secondary (9–10) | -1.39 | (-2.80, 0.02) | |||
| Higher secondary (11–12) | -1.99 | (-3.68, -0.30) | |||
| Tertiary (>12) | -2.45 | (-4.33, -0.57) | |||
| Food security | Family does not have enough money for food | reference | <0.001 | 0.102 | |
| Family does have enough money for food | -4.68 | (-5.78, -3.58) | |||
| Family Debt | Family has debt | reference | <0.001 | 0.074 | |
| Family has no debt | -2.08 | (-2.81, -1.35) |
All models adjusted for mother’s age and number of living children
Fig. 1.
Predicted PHQ-9 Total Score by standardized level of the Asset SES Index, adjusted for mother’s age and number of living children. Score is predicted at the mean of mother’s age and number of living children.
Fig. 2.
Predicted PHQ-9 Total Score for debt and food security binary variables, each separately adjusted for mother’s age and number of living children. Score is predicted at the mean of mother’s age and number of living children.
Fig. 3.
Predicted PHQ-9 Total Score for husband and wife education, each separately adjusted for mother’s age and number of living children. Score is predicted at the mean of mother’s age and number of living children.
In the single predictor model, each standard deviation increase in asset score was associated with a 1.79 point lower PHQ-9 score (95% CI: -2.24, -1.34). Multiple options for the shape of the associations were tested using spline regressions, but the linear model had the best fit as indicated by the AIC (Akaike information criterion). There was no evidence of a threshold effect that would suggest dichotomization of a poverty level based on assets. Instead a negative gradient was observed (Fig. 1), as for education (Fig. 3). The association between education and depression symptoms was also along an inverse gradient, with a more pronounced association between the woman’s (vs. the husband’s) education and depression symptoms (Fig. 3).
Focusing on the binary poverty measures, women whose families were food insecure reported PHQ-9 scores 4.68 points higher (95% CI: 3.58, 5.78) than those whose families were not, placing the mean PHQ-9 score for women reporting food insecurity at 10.6 (95% CI: 9.6, 11.6). This level of depression symptoms is within what is considered the depressed range. Being in a family in debt was associated with a 2.08 point higher PHQ-9 score (95% CI: 1.35, 2.81) (Fig. 2).
In multivariable models, we evaluated the simultaneous association between multiple SES variables and depression symptoms. Table 3 presents findings from a series of regressions that sequentially add each SES variable into the regression model containing assets. Food insecurity (model 1) and debt (model 2) continued to independently predict depression symptoms together with the asset index. After the inclusion of these variables in the model, both the woman’s education (model 3) and the husband’s (model 4) were no longer statistically significantly correlated with depression symptoms. The findings were unchanged when we altered the order in which the SES variables are added to the model. The model consisting of assets, food insecurity, and debt (model 2) accounted for 13.8% of the variance in depression scores, while the addition of the education variables did not confer any additional explanatory power.
Table 3.
PHQ-9 regression on SES variables.
| Adjusted Model 1 |
Adjusted Model 2 |
Adjusted Model 3 |
Adjusted Model 4 |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Covariate | Level | Coeff. | (95% CI) | P-value | Adjusted R-squared | Coeff. | (95% CI) | P-value | Adjusted R-squared | Coeff. | (95% CI) | P-value | Adjusted R-squared | Coeff. | (95% CI) | P-value | Adjusted R-squared |
| Asset index score | -1.44 | (-1.91, -0.97) | <0.001 | 0.129 | -1.50 | (-2.05, -0.95) | <0.001 | 0.138 | -1.21 | (-1.76, -0.66) | <0.001 | 0.138 | -1.01 | (-1.60, -0.42) | <0.001 | 0.134 | |
| Food security | Family does not have enough money for food | reference | <0.001 | reference | <0.001 | reference | <0.001 | reference | <0.001 | ||||||||
| Family does have enough money for food | -3.59 | (-4.73, -2.45) | -3.4 | (-4.58, -2.22) | -3.33 | (-4.51, -2.15) | -3.32 | (-4.52, -2.12) | |||||||||
| Family Debt | Family has debt | reference | 0.010 | reference | 0.010 | reference | 0.010 | ||||||||||
| Family has no debt | -1.07 | (-1.81, -0.33) | -1.04 | (-1.78, -0.30) | -1.03 | (-1.79, -0.27) | |||||||||||
| Woman’s education | None (0) | reference | 0.430 | reference | 0.510 | ||||||||||||
| Primary (1–5) | 0.05 | (-1.26, 1.36) | 0.02 | (-1.29, 1.33) | |||||||||||||
| Middle (6–8) | -0.48 | (-1.81, 0.85) | -0.50 | (-1.85, 0.85) | |||||||||||||
| Secondary (9–10) | -0.72 | (-2.05, 0.61) | -0.74 | (-2.09, 0.61) | |||||||||||||
| Higher secondary (11–12) | -1.01 | (-2.62, 0.60) | -1.03 | (-2.68, 0.62) | |||||||||||||
| Tertiary (>12) | -1.34 | (-2.93, 0.25) | -1.35 | (-3.02, 0.32) | |||||||||||||
| Husband’s education | None (0) | reference | 0.996 | ||||||||||||||
| Primary (1–5) | 0.49 | (-1.31, 2.29) | |||||||||||||||
| Middle (6–8) | 0.39 | (-1.16, 1.94) | |||||||||||||||
| Secondary (9–10) | 0.33 | (-1.16, 1.82) | |||||||||||||||
| Higher secondary (11–12) | 0.24 | (-1.62, 2.10) | |||||||||||||||
| Tertiary (>12) | 0.33 | (-1.77, 2.43) | |||||||||||||||
All models adjusted for mother’s age and number of living children
Discussion
Summary
The goal of the study was to examine the association between multiple socioeconomic indicators, designed to test both a gradient and threshold association with depression symptoms, among a sample of pregnant women living in rural Pakistan. We found that lower assets, food insecurity, and debt were independently associated with higher depression symptoms. An initial statistically significant association with educational attainment (both the woman’s and the husband’s) was attenuated once the other SES variables were included in the model. Furthermore, the association of the asset index score with depression symptoms was linear, with no evidence of a threshold effect. In other words, these data support the existence of an SES-mental health gradient, suggesting that binary indicators capturing poverty, while also associated with depression, do not tell the entire story. The incremental association between SES and mental health persists above a level of absolute material deprivation.
Assets
We used the polychoric principal components analysis method to create an asset index score. This method of scoring is especially useful across cultural contexts where different assets may be more important than others. For example, in the Kang et al. (2016) study in Delhi, India, ownership of a washing or a sewing machine was weighed more strongly than in this sample, indicating that these two items were stronger indicators of higher SES in the India sample (Kang et al., 2016). This asset index can also be used to identify non-linear associations or inflection points that might be a valid guide for the determination of a locally valid threshold for poverty.
In previous work in Pakistan, socioeconomic factors including assets such as electrical appliances and motor vehicles, among others, were found to be correlated with lower psychological distress symptoms (Mumford, Minhas, Akhtar, Akhter & Mubbashar, 2000). However, these associations were relatively weak, a finding that was potentially attributed to the relative socioeconomic homogeneity of the sample (Mumford, Saeed, Ahmad, Latif & Mubbashar, 1997). The relative homogeneity of a population can lead to small cell sizes (in a ‘rich’ tertile, for example, when the majority of the population is poor), resulting in wide confidence intervals and a seemingly weak correlation between higher SES and mental health (Shidhaye & Patel 2010).
The population sample presented in the current analysis has a range of assets; for example, only 4.9% of people in the bottom quintile owned a car while, at the top, 38.7% did.
The regression coefficient for the asset score remained stable and statistically significant even after adjusting for all other SES variables. Since household assets usually change slowly over time, the asset score itself likely captures the longer term, cumulative effects of economic stress. However, relying on only an asset score would miss the mental health consequences of recent negative shocks, such as loss of work/income or newly acquired debt. Some researchers have argued that these changes in socioeconomic indicators are more important for current mental health symptoms (Araya et al., 2003, Das et al., 2007).
It is noteworthy that the continuous asset index variable revealed a gradient in the association with depression symptoms with no evidence of a threshold effect below a certain level of assets. This finding is consistent with research from HIC revealing that individuals in the top socioeconomic position have fewer health problems than those just below, even when both are well above a poverty line (Marmot et al., 1991). Our finding suggests that the mental health gradient in LMIC may extend above a poverty line as well. Fewer LMIC studies explicitly compare whether gradient vs. threshold characterizations of SES measures are a better fit. Furthermore, although often gradient associations are reported, the common use of the term ‘poverty’ implies an association driven by individuals at the very bottom of the SES scale (Cooper et al., 2012, Kang et al., 2016). In this study, 239 cases of a positive screen for depression (39.1% of total depression cases) came from women living in households above the median asset score. This population distribution reinforces the idea that interventions focused exclusively on improving the SES solely of those at the very bottom might have only a limited impact on the population prevalence of depression (Rose 1985).
Education
Education is a commonly used marker of SES in LMIC (Cooper et al., 2012): it is easily measured and fairly stable in adulthood; yet its relationship with an individual’s current level of socioeconomic standing is potentially complex. It is also possible that education may affect the reporting of depression symptoms. In the analyses presented here, the woman’s own educational attainment was more strongly correlated with her depression symptoms than her husband’s education. There is also a gradient among women with a lowering of depression symptoms with each educational milestone. Both woman’s and husband’s education levels were correlated with assets, as well as with each other; and this may partially explain why education did not remain a significant contributor in the final model. Importantly, we do not interpret this finding to mean that education is not relevant for mental health; but rather that the mechanisms involved in its link to depression are potentially similar to those of assets or flow through assets. Education captures SES earlier in the life-course, and it has been interpreted as a more upstream determinant of health (Cutler & Lleras-Muney, 2006). If the role of education is mediated through the other domains such as current assets, then its main association is likely to be ameliorated. Additionally, educational attainment may also uniquely reflect the ‘social’ component of socioeconomic status that is not well captured in the other SES measures.
Food insecurity
The presence of food insecurity was meant to capture the experience of poverty itself (vs. an SES gradient) and so it is not surprising that its presence was correlated with the highest depression symptoms. It reflects both the low level of a basic necessity available to the family, as well as the psychological stress that this may cause, and so likely influences mental health through multiple pathways. For example, recent experimental research suggests that uncertainty about basic needs can create cognitive load, leading to suboptimal decision making in other domains of life which, in turn, can worsen poverty (Lichand & Mani 2016). Furthermore, evidence that the link between food insecurity and mental health varies by season, with stronger associations during times when most people in the community are food secure and weaker associations when food insecurity is more prevalent, points to the importance of one’s social environment in either buffering or exacerbating this link with mental health (Cole & Tembo, 2011). Similarly, food insecurity may be especially stigmatizing to women, who may then be less likely to activate their social networks for support, leading to more distress (Piperata, Schmeer, Rodrigues & Salazar Torres, 2016).
Debt
Although the presence of debt on its own is not indicative of poverty, in areas with poorly functioning credit markets and high interest rates, people may be more likely to borrow only under duress. Difficulties in paying back a loan can lead a family to deplete assets and fall deeper into a poverty trap (Krishna, 2010). The inclusion of debt may therefore help us understand the local context better, although any findings may not be widely generalizable. Our findings of worse depression symptoms in the presence of debt are also consistent with those from a prior study in Pakistan in which women whose families were in debt and who were categorized as lower SES by the local community health worker (the study’s definition of ‘poor’) had 3 times higher odds of having persistent depression relative to women were not considered poor (Rahman & Creed, 2007). Indeed, in the current study there was weak evidence that the association between debt and depression symptoms was stronger among those towards the bottom of the asset score distribution, although this difference did not reach statistical significance (results not shown). Even in contexts outside of poor functioning credit markets, having debt can cause psychological distress. For example, in one poverty alleviation intervention that provided even low-interest loans in South Africa, the authors found that stress levels increased among those receiving the new loans (Fernald, Hamad, Karlan, Ozer & Zinman, 2008).
Limitations
The current study has several limitations. We were not able to examine the contribution of other SES indicators such as income, expenditure, employment, or occupation. The majority of women in this sample were not able to estimate either the household income (62% were not able to provide this information) or expenditure (53% were not able to). Concerns about the accuracy of expenditure data have been raised before (Xu, Ravndal, Evans & Carrin, 2009); and in this study area, financial matters, including food shopping, are more commonly handled by men. Although this is not unique to a rural Pakistan setting, it does present a challenge in research specific to income/expenditure and women’s mental health in such settings. Additionally, in this sample there was little variation in employment or occupation indicators: 91% of husbands were employed; all of them were manual laborers. Only 6% of the women were employed outside the household. Our analyses also only focused on a narrow set of social disadvantage factors related to socioeconomic status. Other social vulnerability factors such as exposure to intimate partner violence, lack of empowerment, or pressure to have male children are also strongly associated with women’s mental health and may be potential sources of omitted variable bias/confounding in our results. Our team’s ongoing research is examining the contribution of these factors to maternal mental health. Our study population comprises entirely of pregnant women so the findings should not be generalized beyond this population. Given the cross-sectional, observational nature of these data, we make no claims about the causal relationship, or its direction, between the SES variables and depression symptoms. There is growing evidence illustrating how both the social selection (mental health problems leading to lower SES) and social causation (lower SES causing mental health problems) pathways can simultaneously create the observed association between SES and mental health, both in high and low income countries (Lund et al., 2011, Quidt and Haushofer, 2016).
Conclusions
Together, the asset, debt, and food insecurity indicators in this study explained about 13% of the variance in the depression symptoms, which is more than what has been reported in high income countries or for non-mental health outcomes (Glymour & Rudolph, 2016). This is consistent with the idea that mental health may be more sensitive to the social context and might even be on the pathway between low socioeconomic status and physical health problems such as cardiovascular disease. For example, the stress and worry associated with lower socioeconomic status may in itself be an important independent mechanism leading to worse mental and physical health (Reading & Reynolds, 2001).
Recent evidence from experimental interventions may be able to contribute key data towards estimating the relative contribution of each link in the SES-mental health cycle: There are a growing number of (a) poverty reduction programs that assess mental health outcomes and (b) mental health interventions that assess economic outcomes (Lund et al., 2011). For example, Mexico’s Opportunidades conditional cash transfer program has shown improved mental health outcomes, although not all programs have been successful (Ozer et al., 2011, Madhani et al., 2015, Green et al., 2016, Kilburn et al., 2016). Evaluations of the economic impact of mental health interventions (addressing the social drift hypothesis) are still relatively rare. A few studies have reported improvements in patient employment levels post intervention (Hu, Wang & Fu, 2007), ability to participate in economic activities (Bolton et al., 2003), or increased financial empowerment (Baranov, Bhalotra, Biroli & Maselko, 2017), but others have not found an association (Lund et al., 2011). In the current sample, formal labor participation by all women is very low, and one might argue that the household indicators of SES are largely outside of her control. This would make the social drift mechanism a somewhat less likely explanation for our findings. Looking forward, analyses based on experimental studies have significant potential to elucidate both the social causation and social drift pathways (De Silva, 2015, Lund, 2015).
Independent of the contribution of each causal pathway, the data presented here strongly support the idea of a gradient between different socioeconomic indicators and depression symptoms. While a dichotomous poverty measure may be easier to measure and perhaps more likely to yield a larger and statistically significant correlation with mental health, it is not ideal for gaining a better understanding of the nature of the association between lower socioeconomic status and mental health. We hence strongly recommend that, whenever possible, indicators of socioeconomic status be presented in a gradient, and not dichotomous, fashion in order to gain the most from the available data.
Our findings are also consistent with the idea that various domains of SES, such as assets and food insecurity, potentially have independent pathways leading to mental health. A better understanding of any underlying relationship will also result from a deeper understanding of the theoretical basis, and lived experience, of a given socioeconomic indicator (e.g. (Mill, 1865, Sen, 1999, Banerjee & Duflo, 2011)). Health researchers are generally not exposed to this wider literature (Araya et al., 2003), leading to a critique that convenience of measurement has guided choice of SES measures and not their theorized associations with other variables of interest (Cooper et al., 2012). Future research that measures SES with multiple, theoretically anchored, domains holds the most promise in improving our understanding of the nature of the SES-mental health relationship.
Acknowledgments
This study was funded by a grant from the NIH R01HD075875 and NIMH grant #U19MH95687. We would like to thank the team at the Human Development Research Foundation (HDRF) including Rakshanda Liaqat, Tayyiba Abbasi, Maria Sharif, Samina Bilal, Qurat-ul-Ain, Anum Nisar, Amina Bibi, Shaffaq Zufiqar Sonia Khan, Ahmed Zaidi, Ikhlaq Ahmad, and Najia Atif. Finally, we are very grateful to the women who participated in the study.
Conflicts of interest
None.
This project has been supported by NICHD grant #R01HD075875 and NIMH grant #U19MH95687.
Ethics approval
This study was approved by Ethical Institutional Review Boards at the Human Development Research Foundation (HDRF), Duke University, and University of North Carolina.
Footnotes
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.ssmph.2017.10.004.
Contributor Information
Joanna Maselko, Email: jmaselko@unc.edu.
Sonia Bhalotra, Email: srbhal@essex.ac.uk.
Appendix A. Supplementary material
Supplementary material
.
References
- Araya R., Lewis G., Rojas G., Fritsch R. Education and income: Which is more important for mental health? Journal of Epidemiology and Community Health. 2003;57(7):501–505. doi: 10.1136/jech.57.7.501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banerjee, A. and Duflo E. (2011). Poor Economics: A Radical Rethinking of the Way to Fight Global Poverty, PublicAffairs.
- Baranov, V., Bhalotra S., Biroli P. and Maselko J. (2017). Maternal Depression, Women’s Empowerment, and Parental Investment: Evidence from a Large Randomized Control Trial Working Paper.
- Bolton P., Bass J., Neugebauer R., Verdeli H., Clougherty K.F., Wickramaratne P., Speelman L., Ndogoni L., Weissman M. Group interpersonal psychotherapy for depression in rural Uganda - A randomized controlled trial. JAMA—Journal of the American Medical Association. 2003;289(23):3117–3124. doi: 10.1001/jama.289.23.3117. [DOI] [PubMed] [Google Scholar]
- Brown S., Lumley J. Physical health problems after childbirth and maternal depression at six to seven months postpartum. British Journal of Obstetrics and Gynaecology. 2000;107(10):1194–1201. doi: 10.1111/j.1471-0528.2000.tb11607.x. [DOI] [PubMed] [Google Scholar]
- Burns J.K. Poverty, inequality and a political economy of mental health. Epidemiology and Psychiatric Sciences. 2015;24(2):107–113. doi: 10.1017/S2045796015000086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coast E., Leone T., Hirose A., Jones E. Poverty and postnatal depression: A systematic mapping of the evidence from low and lower middle income countries. Health place. 2012;18(5):1188–1197. doi: 10.1016/j.healthplace.2012.05.004. [DOI] [PubMed] [Google Scholar]
- Cole S.M., Tembo G. The effect of food insecurity on mental health: Panel evidence from rural Zambia. Social Science & Medicine. 2011;73(7):1071–1079. doi: 10.1016/j.socscimed.2011.07.012. [DOI] [PubMed] [Google Scholar]
- Cooper S., Lund C., Kakuma R. The measurement of poverty in psychiatric epidemiology in LMICs: Critical review and recommendations. Social Psychiatry and Psychiatric Epidemiology. 2012;47(9):1499–1516. doi: 10.1007/s00127-011-0457-6. [DOI] [PubMed] [Google Scholar]
- Cutler D.M., Lleras-Muney A. National Bureau of Economic Research; 2006. Education and health: Evaluating theories and evidence. [Google Scholar]
- Das J., Do Q.T., Friedman J., McKenzie D., Scott K. Mental health and poverty in developing countries: Revisiting the relationship. Social Science Medicine. 2007;65(3):467–480. doi: 10.1016/j.socscimed.2007.02.037. [DOI] [PubMed] [Google Scholar]
- De Silva M.J. Making mental health an integral part of sustainable development: The contribution of a social determinants framework. Epidemiology and Psychiatric Sciences. 2015;24(2):100–106. doi: 10.1017/S2045796015000049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernald L.C., Hamad R., Karlan D., Ozer E.J., Zinman J. Small individual loans and mental health: A randomized controlled trial among South African adults. BMC Public Health. 2008;8:409. doi: 10.1186/1471-2458-8-409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filmer D., Pritchett L.H. Estimating wealth effects without expenditure data—or tears: An application to educational enrollments in states of india*. Demography. 2001;38(1):115–132. doi: 10.1353/dem.2001.0003. [DOI] [PubMed] [Google Scholar]
- Fisher J., Mello M.C. d, Patel V., Rahman A., Tran T., Holton S., Holmes W. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: A systematic review. Bulletin of the World Health Organization. 2012;90:139–149. doi: 10.2471/BLT.11.091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fraz K., Khan S., Sikander S. Screening for depression in coronary artery disease patients using PHQ-9. The Health. 2013;4(1):3–6. [Google Scholar]
- Galler J.R., Ramsey F.C., Harrison R.H., Taylor J., Cumberbatch G., Forde V. Postpartum maternal moods and infant size predict performance on a national high school entrance examination. Journal of Child Psychology and Psychiatry. 2004;45(6):1064–1075. doi: 10.1111/j.1469-7610.2004.t01-1-00299.x. [DOI] [PubMed] [Google Scholar]
- Galobardes B., Shaw M., Lawlor D.A., Davey Smith George, Lynch J. Indicators of soceioeconomic position methods in social epidemiology. In: Oakes J.M., Kaufman J.S., editors. Methods in social epidemiology. Jossey-Bass; San Francisco, CA: 2006. pp. 47–85. [Google Scholar]
- Gelaye B., Rondon M.B., Araya R., Williams M.A. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. The Lancet Psychiatry. 2016;3(10):973–982. doi: 10.1016/S2215-0366(16)30284-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gholizadeh L., Ali khan S., Vahedi F., Davidson P.M. Sensitivity and specificity of Urdu version of the PHQ-9 to screen depression in patients with coronary artery disease. Contemporary Nurse. 2017;53(1):75–81. doi: 10.1080/10376178.2017.1283245. [DOI] [PubMed] [Google Scholar]
- Glymour M.M., Avendano M., Kawachi I. Socioeconomic status and health. In: Berkman L.F., Kawachi I., Glymour M.M., editors. Social epidemiology. Oxford University Press; 2014. [Google Scholar]
- Glymour M.M., Rudolph K.E. Causal inference challenges in social epidemiology: Bias, specificity, and imagination. Social Science Medicine. 2016;166:258–265. doi: 10.1016/j.socscimed.2016.07.045. [DOI] [PubMed] [Google Scholar]
- Green E.P., Blattman C., Jamison J., Annan J. Does poverty alleviation decrease depression symptoms in post-conflict settings? A cluster-randomized trial of microenterprise assistance in Northern Uganda. Global Mental Health. 2016;3:9. doi: 10.1017/gmh.2015.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hemingway H., Nicholson A., Stafford M., Roberts R., Marmot M. The impact of socioeconomic status on health functioning as assessed by the SF-36 questionnaire: The Whitehall II Study. American Journal of Public Health. 1997;87(9):1484–1490. doi: 10.2105/ajph.87.9.1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howe L.D., Galobardes B., Matijasevich A., Gordon D., Johnston D., Onwujekwe O., Patel R., Webb E.A., Lawlor D.A., Hargreaves J.R. Measuring socio-economic position for epidemiological studies in low-and middle-income countries: A methods of measurement in epidemiology paper. International journal of Epidemiology. 2012:dys037. doi: 10.1093/ije/dys037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu X., Wang Y., Fu H. Synthetical family treatment for depression: A randomized-controlled single-blind study among 76 cases (in Chinese) Journal of Clinical Rehabilitative Tissue Engineering Research. 2007;11:7787–7790. [Google Scholar]
- Kang E., Delzell D.A.P., McNamara P.E., Cuffey J., Cherian A., Matthew S. Poverty indicators and mental health functioning among adults living with HIV in Delhi, India. Aids Care-Psychological and Socio-Medical Aspects of Aids/HIV. 2016;28(4):416–422. doi: 10.1080/09540121.2015.1099604. [DOI] [PubMed] [Google Scholar]
- Kilburn K., Thirumurthy H., Halpern C.T., Pettifor A., Handa S. Effects of a large-scale unconditional cash transfer program on mental health outcomes of young people in Kenya. Journal of Adolescent Health. 2016;58(2):223–229. doi: 10.1016/j.jadohealth.2015.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolenikov S., Angeles G. Carolina Population Center, University of North Carolina; Chapel Hill: 2004. The use of discrete data in PCA: Theory, simulations, and applications to socioeconomic indices. [Google Scholar]
- Kolenikov S., Angeles G. Socioeconomic status measurement with discrete proxy variables: is principal component analysis a reliable answer? Review of Income and Wealth. 2009;55(1):128–165. [Google Scholar]
- Krishna A. Oxford University Press; New York: 2010. One illness away: Why people become poor and how they escape poverty. [Google Scholar]
- Kroenke K., Spitzer R.L., Williams J.B.W. The PHQ-9 – Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichand G., Mani A. Harvard University; 2016. Cognitive droughts. (Working Paper) [Google Scholar]
- Lorant V., Deliege D., W E., Robert A., Philippot P., Ansseau M. Socioeconomic inequalities in depression: A meta-analysis. American Journal of Epidemiology. 2003;157:98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Lund C. Poverty, inequality and mental health in low- and middle-income countries: Time to expand the research and policy agendas. Epidemiology and Psychiatric Sciences. 2015;24(2):97–99. doi: 10.1017/S2045796015000050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund C., Breen A., Flisher A.J., Kakuma R., Corrigall J., Joska J.A., Swartz L., Patel V. Poverty and common mental disorders in low and middle income countries: A systematic review. Social Science Medicine. 2010;71(3):517–528. doi: 10.1016/j.socscimed.2010.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lund C., De Silva M., Plagerson S., Cooper S., Chisholm D., Das J., Knapp M., Patel V. Poverty and mental disorders: Breaking the cycle in low-income and middle-income countries. The Lancet. 2011;378(9801):1502–1514. doi: 10.1016/S0140-6736(11)60754-X. [DOI] [PubMed] [Google Scholar]
- Madhani F.I., Tompkins C., Jack S.M., Fisher A. Participation in micro-finance programmes and women’s mental health in South Asia: A modified systematic review. Journal of Development Studies. 2015;51(9):1255–1270. [Google Scholar]
- Marmot M.G., Smith G.D., Stansfeld S., Patel C., North F., Head J., White I., Brunner E., Feeney A. Health inequalities among British civil-servants – The Whitehall-II study. Lancet. 1991;337(8754):1387–1393. doi: 10.1016/0140-6736(91)93068-k. [DOI] [PubMed] [Google Scholar]
- Maselko J., Sikander S., Bangash O., Bhalotra S., Franz L., Ganga N., Rajan D.G., O’Donnell K., Rahman A. Child mental health and maternal depression history in Pakistan. Social Psychiatry and Psychiatric Epidemiology. 2016;51(1):49–62. doi: 10.1007/s00127-015-1143-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mill J.S. Longman, Green, Longman, Roberts & Green; London: 1865. Principles of political economy, with some of their applications to social philosophy. [Google Scholar]
- Mumford D.B., Minhas F.A., Akhtar I., Akhter S., Mubbashar M.H. Stress and psychiatric disorder in urban Rawalpindi - Community survey. British Journal of Psychiatry. 2000;177:557–562. doi: 10.1192/bjp.177.6.557. [DOI] [PubMed] [Google Scholar]
- Mumford D.B., Saeed K., Ahmad I., Latif S., Mubbashar M.H. Stress and psychiatric disorder in rural Punjab - A community survey. British Journal of Psychiatry. 1997;170:473–478. doi: 10.1192/bjp.170.5.473. [DOI] [PubMed] [Google Scholar]
- Ozer E.J., Fernald L.C.H., Weber A., Flynn E.P., VanderWeele T.J. Does alleviating poverty affect mothers' depressive symptoms? A quasi-experimental investigation of Mexico’s Oportunidades programme. International Journal of Epidemiology. 2011;40(6):1565–1576. doi: 10.1093/ije/dyr103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel V., Araya R., Chowdhary N., King M., Kirkwood B., Nayak S., Simon G., Weiss H. Detecting common mental disorders in primary care in India: A comparison of five screening questionnaires. Psychological Medicine. 2008;38(02):221–228. doi: 10.1017/S0033291707002334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piperata B.A., Schmeer K.K., Rodrigues A.H., Salazar Torres V.M. Food insecurity and maternal mental health in Leon, Nicaragua: Potential limitations on the moderating role of social support. Social Science & Medicine. 2016;171:9–17. doi: 10.1016/j.socscimed.2016.10.029. [DOI] [PubMed] [Google Scholar]
- Quidt, J.D. and Haushofer J. (2016). Depression for Economists. NBER Working Paper. N. B. o. E. Research. Cambridge, MA.
- Rahman A., Creed F. Outcome of prenatal depression and risk factors associated with persistence in the first postnatal year: Prospective study from Rawalpindi, Pakistan. Journal of Affective Disorders. 2007;100(1-3):115–121. doi: 10.1016/j.jad.2006.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman A., Iqbal Z., Bunn J., Lovel H., Harrington R. Impact of maternal depression on infant nutritional status and illness - A cohort study. Archives of General Psychiatry. 2004;61(9):946–952. doi: 10.1001/archpsyc.61.9.946. [DOI] [PubMed] [Google Scholar]
- Reading R., Reynolds S. Debt, social disadvantage and maternal depression. Social Science Medicine. 2001;53(4):441–453. doi: 10.1016/s0277-9536(00)00347-6. [DOI] [PubMed] [Google Scholar]
- Rose G. Sick Individuals and Sick Populations. International Journal of Epidemiology. 1985;14(1):32–38. doi: 10.1093/ije/14.1.32. [DOI] [PubMed] [Google Scholar]
- Rutstein, S.O. and Johnson K. (2004). The DHS Wealth INdex. DHS Comparative REports. Claverton, Maryland, USA, MEASURE DHS+. 6.
- Sen A. Random House; New York: 1999. Development as freedom. [Google Scholar]
- Shidhaye R., Patel V. Association of socio-economic, gender and health factors with common mental disorders in women: A population-based study of 5703 married rural women in India. International Journal of Epidemiology. 2010;39(6):1510–1521. doi: 10.1093/ije/dyq179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sikander S., Lazarus A., Bangash O., Fuhr D.C., Weobong B., Krishna R.N., Ahmad I., Weiss H.A., Price L., Rahman A., Patel V. The effectiveness and cost-effectiveness of the peer-delivered Thinking Healthy Programme for perinatal depression in Pakistan and India: The SHARE study protocol for randomised controlled trials. Trials. 2015;16:14. doi: 10.1186/s13063-015-1063-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith, A. (1776). An Inquiry into the Nature and Causes of the Wealth of Nations. London.
- Turner E.L., Sikander S., Bangash O., Zaidi A., Bates L., Gallis J., Ganga N., O’Donnell K., Rahman A., Maselko J. The effectiveness of the peer-delivered Thinking Healthy PLUS (THPP+) Program for maternal depression and child socioemotional development in Pakistan: Study protocol for a randomized controlled trial. Trials. 2016;17(1):442. doi: 10.1186/s13063-016-1530-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vyas S., Kumaranayake L. Constructing socio-economic status indices: How to use principal components analysis. Health Policy and Planning. 2006;21(6):459–468. doi: 10.1093/heapol/czl029. [DOI] [PubMed] [Google Scholar]
- Xu K., Ravndal F., Evans D.B., Carrin G. Assessing the reliability of household expenditure data: Results of the World Health Survey. Health Policy. 2009;91(3):297–305. doi: 10.1016/j.healthpol.2009.01.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material