Highlights
-
•
Neighborhood affluence protects against the risk of poor birth outcome.
-
•
The protective effect of affluence holds for Whites, Blacks, Hispanics and Asians.
-
•
Mediation of these pathways by prenatal smoking varies by racial group.
-
•
The discourse on neighborhoods and birth outcomes should include affluence.
Introduction
Poor birth outcomes, such as preterm birth (PTB; < 37 weeks) or low birth weight (LBW; < 2500 g), are important markers of future life chances. PTB is the leading risk factor for infant mortality in the United States (Goldenberg, Culhane, Iams, & Romero, 2008); both PTB and LBW are associated with neurodevelopmental problems, language disorders, learning disabilities, and poor adult health (Behrman and Butler, 2007, Goldenberg and Culhane, 2007). Poor birth outcomes are highly stratified by race-ethnicity and socioeconomic status. Black women consistently exhibit a twofold risk of PTB and LBW relative to White women; some Hispanic and Asian subgroups, such as Puerto Ricans and Cambodians, also exhibit excess risk relative to Whites (Blumenshine et al., 2010, Martin et al., 2008). That poor and some minority populations bear a disproportionate burden of poor health at birth is a key public health challenge facing the United States (Healthy People, 2020).
The etiology of poor birth outcomes is multifactorial, yet we have only a preliminary understanding of the full set of risk factors and causal pathways contributing to LBW and PTB. Known risk factors have been identified at the individual- and neighborhood-level. Neighborhood deprivation (Buka et al., 2003, Messer et al., 2006b, Pickett et al., 2002), residential segregation (Mendez, Hogan, & Culhane, 2014), local crime rates (Messer et al., 2006a, Morenoff, 2003, Schempf et al., 2009), and low neighborhood-level education (Messer et al., 2008, Nkansah-Amankra et al., 2010, Pearl et al., 2001, Subramanian et al., 2006) are well-documented risk factors of LBW and PTB. Yet only one study has examined the effect of neighborhood affluence on birth outcomes (Roberts, 1997).
Neighborhood affluence is distinct in both its definition — it signals the presence of highly educated, wealthy residents employed in prestigious occupations who can effectively draw local institutions to their community that can stabilize the neighborhood and meet the basic needs of residents — and its implications for health — health-promoting institutions benefit all residents, regardless of individual-level socioeconomic status. A strong body of evidence indicates neighborhood affluence is a key predictor of self-reported health and objectively-measured health status that persists in its effect when other key covariates are included, such as neighborhood disadvantage, individual-level socioeconomic status and insurance coverage (Browning and Cagney, 2003, Browning et al., 2003, Cagney et al., 2005, King et al., 2011, Matthews and Yang, 2010, Wen et al., 2003). Several of these studies even show that neighborhood disadvantage is no longer a statistically significant predictor of health status once neighborhood affluence is considered.
The one study that has examined affluence in relation to birth outcomes examined a single outcome (LBW) in one location (Chicago) and did not run race-specific models (Roberts, 1997) — an important feature of any neighborhood analysis on the basis that long-standing patterns of residential segregation in the U.S. imply women of various racial or ethnic groups occupy different spaces. Moreover, most studies examining neighborhood disadvantage and birth outcomes have not explored racial or ethnic differences beyond Black-White disparities; such an examination is essential given that Hispanics and Asians comprise rapidly growing segments of the U.S. population (Ennis et al., 2011, Pew Research Center, 2013). In addition, a pressing question in the neighborhood effects literature is, through what mechanism does neighborhood context affect health (Matthews & Yang, 2010; Wen et al., 2003)? This question has received inadequate attention in birth outcomes studies. Overall, a more comprehensive assessment of the role of neighborhood affluence is likely to reveal promising new insights into the social determinants of poor infant health.
This study contributes to this discourse by developing new hypotheses of how the sociological construct of neighborhood affluence may affect birth outcomes, and how this association may be mediated by prenatal health behaviors. We also discuss how neighborhood affluence may differentially affect the birth outcomes of Black, White, Hispanic, and Asian women. We then test the association between neighborhood affluence and two birth outcomes (LBW, PTB) and assess the extent to which these associations are mediated by a key prenatal health behavior (prenatal smoking). We do so using race/ethnic-stratified multilevel models and population-based birth record data from The State of New Jersey over a ten-year period (1996–2006). We conclude by discussing the key implication of our study as it relates to including neighborhood affluence in future studies assessing the etiology of poor birth outcomes.
Background
Social environments are central to individual-level health. Social environments shape social norms that govern behaviors, attitudes, and practices; constrain opportunities for individuals to engage in health-promoting behaviors; regulate access to resources that people can use to procure health; facilitate a high degree of social control that can limit the opportunity for individuals to engage in illegal or harmful behavior; and mediate stressors that, in turn, may lead to the adoption of unhealthy coping mechanisms (Kawachi and Berkman, 2003, Link and Phelan, 1995, Sampson, 2003, Sampson et al., 2002).
Neighborhood context and birth outcomes
Culhane and Elo (2005) developed a conceptual framework linking neighborhood context (indicated by the social environment, service environment, and physical characteristics) to birth outcomes via a pathway mediated by individual-level health behaviors, psychosocial factors, and social support, as well as maternal stress physiology. We use this framework to guide our study.
In accordance with their framework, emerging evidence suggests living in an impoverished, resource-poor neighborhood; exposure to dilapidated housing; residential instability; institutional practices (e.g., redlining); residential segregation; and exposure to environmental toxicants increase the risk of PTB and LBW (Behrman and Butler, 2007, Bell et al., 2006, Buka et al., 2003, Culhane and Elo, 2005, Debbink and Bader, 2011, Grady, 2006, Halfon and Hochstein, 2002, Hogan et al., 2012, Hogue et al., 2001, Lu et al., 2010, Misra et al., 2003, Morenoff, 2003, Walton, 2009).
Neighborhood disadvantage, in particular, has received a great deal of attention in this literature. Several studies using the Neighborhood Deprivation Index (NDI), a measure created by public health scholars specifically with birth outcomes in mind (Messer et al., 2006b), have produced convincing evidence linking neighborhood deprivation with PTB risk [see for example, Messer et al., 2006a, O’Campo et al., 2008]. The NDI includes an indicator of education (proportion of individuals with less than a high school degree) and an indicator of occupational prestige (proportion of males in management and professional occupations), along with several other indicators related to poverty and income. Similarly, other deprivation indices used in perinatal epidemiology combine indicators of education, occupational prestige, or housing values, along with indictors of poverty, unemployment, crowded housing, and/or family composition in the same index [see (Messer et al., 2006b) for a review]. Our goal is to draw on sociological theory and research to disentangle indicators reflecting the sociological construct of neighborhood affluence (education, occupational prestige, housing values) from those of neighborhood disadvantage (e.g., poverty, unemployment).
With respect to evidence of pathways linking neighborhood context to birth outcomes, maternal stress is a key mediator of the effect of neighborhood poverty on LBW (Nkansah-Amankra, 2010) and birth weight, along with perceived locus of control and social support (Schempf et al., 2009). Violent crime mediates at least part of the effect of neighborhood disadvantage on birth weight (Masi, Hawkley, Piotrowski, & Pickett, 2007) and of residential isolation segregation on preterm birth among Black women (Kramer, Cooper, Drews-Botsch, Waller, & Hogue, 2010). The most convincing evidence of mediation demonstrates maternal behavioral risk factors—such as prenatal smoking, drug use, and delayed prenatal care—explained a substantial proportion (30%) of the association between neighborhood disadvantage and lower birth weight (Schempf et al., 2009).
Neighborhood affluence and birth outcomes
Neighborhood affluence is not simply the absence of disadvantage, but rather a unique and independent attribute of neighborhoods that plays a key role in contributing to an individual’s wellbeing. The conceptual distinctions between neighborhood affluence and disadvantage are well-described in sociological theory; we discuss this in more detail below. An empirical distinction has also been demonstrated with factor analyses producing two orthogonal factors reflecting neighborhood disadvantage and affluence (Morenoff et al. 2007).
Urban sociologists have long-since theorized about how neighborhoods impact individuals. Social disorganization theory argues that neighborhoods characterized by high concentrations of poverty are also resource-poor; meaning, they do not effectively draw or maintain local institutions that provide key social, economic, and health-related resources to its residents (Kornhauser, 1978, Shaw and McKay, 1942). Yet local institutions thrive in neighborhoods comprised of high concentrations of middle- and upper-class residents who can reliably provide resources to ensure their survival; this is the key concept reflected by neighborhood affluence. All residents, in turn, benefit from the local institution’s resources and services (Browning and Cagney, 2003, Robert, 1998), regardless of their individual-level socioeconomic status or resources.
Neighborhood affluence is commonly operationalized by educational attainment (the proportion of individuals ages 25+ with a college degree or higher), occupational prestige (the proportion of individuals ages 16+ employed in professional or managerial positions), and wealth (median housing values) (King et al., 2011, Morenoff et al., 2007). Central to this literature is that affluence is not equivalent to aggregate levels of high school completion or college education; instead, additional indicators of occupational prestige and wealth (not income), play a key role.
Multiple studies have shown that, when neighborhood poverty and neighborhood affluence are considered jointly, poverty has inconsistent effects on poor health while affluence consistently protects against poor health (Browning and Cagney, 2003, Browning et al., 2003, Wen et al., 2003). If similar evidences emerges in the case of birth outcomes, this would support the necessity of shifting our conceptual understanding of how neighborhood context impacts birth outcomes by including both neighborhood affluence and disadvantage.
We propose high levels of neighborhood affluence can enhance a mother’s ability to secure access to high-quality prenatal healthcare services and other local institutional resources that may reduce her level of stress or elicit healthy coping mechanisms that translate into the adoption of healthy prenatal behaviors. Such neighborhoods may also foster opportunities for pregnant women to engage in physical activity and secure access to healthy foods, and are more likely to contain local organizations that help women realize their reproductive intentions (e.g., family planning, breastfeeding). In turn, access to quality care, healthy diets, healthy prenatal behaviors, and routine engagement in moderate physical activity can protect against the risk of poor birth outcomes. Therefore, we hypothesize that:
H1:
Neighborhood affluence is inversely associated with the risk of poor birth outcomes, net of neighborhood disadvantage.
This hypothesis is buttressed by studies that have assessed poor birth outcomes using constructs similar to that which is discussed here. Roberts (1997) used a measure of neighborhood socioeconomic status (the proportion of white-collar workers, median family income, and median adult education level) to indicate “neighborhood quality”, and showed low levels of neighborhood quality were associated with an increased risk of LBW in Chicago in 1990. (Recall that race-stratified models were not included in this study—a point to which we return in the next section.) Higher levels of neighborhood education are associated with lower risk of LBW and PTB, and with higher birth weight (Nkansah-Amankra, 2010, Pearl et al., 2001, Subramanian et al., 2006). As we previously argued however, aggregated education is not a sufficient indicator of neighborhood affluence; aggregated occupational prestige and wealth are also integral to the construct of neighborhood affluence. Messer et al. (2008) showed that, when measured as separate variables, low neighborhood-level education and low proportion of residents employed in managerial/professional occupations predicted increased PTB risk among non-Hispanic White and Black women across eight study sites.
Race-ethnic differentials in the association between neighborhood affluence and birth outcomes
Discriminatory institutional and social processes, such as racialized redlining practices for mortgages, are key factors in determining where people live (Ncube, Enquobahrie, Albert, Herrick, & Burke, 2016) and have a demonstrable impact on birth outcomes (Mendez et al., 2014). Prior work in the perinatal health literature argues that, due to historical patterns of racial residential segregation, Black and White women occupy different spaces with varying levels (and ranges) of disadvantage; therefore, it is critical to stratify such models by race-ethnicity (Messer et al., 2006b, O’Campo et al., 2008). Studies emerging from sociology reveal that neighborhood affluence is also stratified by race-ethnicity (Solari, 2012), implying that historically disadvantaged minority populations (such as Blacks, and some Hispanics and Asians) likely have access to fewer local institutions providing health-promoting resources than more-advantaged populations.
The empirical literature is inconsistent with respect to which racial group is most negatively affected by neighborhood disadvantage. A recent meta-analysis showed neighborhood disadvantage was significantly associated with PTB and LBW risk among both White and Black mothers, but the effects were generally weaker among Black mothers (Ncube et al., 2016). Similarly, a separate study showed the association between the NDI and PTB risk was weaker among Blacks (in the most versus least deprived neighborhoods) than among Whites (O’Campo et al., 2008). O’Campo and colleagues speculate this finding may reflect a narrower range of NDI in the neighborhoods in which black (versus White) women reside.
Evidence of the opposite pattern has also emerged however. A meta-analysis showed that five out of six studies examining race/ethnic-stratified models of area-based socioeconomic indicators and PTB showed neighborhood disadvantage predicted increased PTB risk among Blacks and Hispanics but not Whites (Blumenshine et al., 2010). Other studies showed neighborhood disadvantage to be associated with lower birthweight (Buka et al., 2003), as well as increased risk of PTB (Messer et al., 2006a) among Black, but not White, women. Janevic et al. (2010) showed negative effects on term LBW among African, Mexican, African American, and Hispanic Caribbean (but not Asian) women living in the most deprived (versus least deprived) neighborhoods; only White women living in the 2nd and 3rd (versus 1st) quartiles of deprivation were at increased risk.
Evidence emerging from studies assessing the effects of constructs similar to neighborhood affluence are also mixed. In a national study, median household income was negatively associated with LBW for Mexicans and Whites, but not for Puerto Ricans, Cubans, and Blacks (Gorman, 1999). Messer et al. (2008) showed that the increased risk of PTB associated with low neighborhood-level education and a low proportion of residents employed in managerial/professional occupations was weaker among Black women than among White women. Yet another study found that higher aggregated education is associated with reduced birth weight for Black and Asian mothers, but not White, U.S.-born Latina or foreign-born Latina mothers (Pearl et al., 2001). Due to the mixed state of the literature, we hypothesize:
H2:
The association of neighborhood affluence, net of disadvantage, with birth outcomes varies by maternal race-ethnicity.
The role of prenatal smoking in mediating the neighborhood affluence—birth outcome association
Returning to Culhane and Elo’s (2005) framework, we propose that neighborhood affluence, at least in part, protects against the risk of poor birth outcomes by shaping prenatal health behaviors, stress responses, and access to services. This assertion remains untested.
For a variable M to mediate an association between X and Y, several conditions must be met: an association must be documented between X and Y, X and M, and M and Y; also, the X-Y association is reduced in magnitude (and, oftentimes, in the level of statistical significance) when M is introduced (Baron & Kenny, 1986). We assess the final condition using Sobel Goodman mediation tests (discussed in the Statistical Analysis section below). We explore the association between X and Y by testing H1.
We select prenatal smoking as the mediator variable (M) on the basis that it has been identified as the leading preventable risk factor for infant morbidity and mortality (Cnattingius, 2004) and is generally considered by economists to have a causal effect on birth weight (Reichman et al., 2006, Wehby et al., 2011); clear physiological pathways have also been documented (Rogers, 2009). This prior evidence firmly establishes the association between M and Y.
Although rates of prenatal smoking vary by race-ethnicity, prenatal smoking increases PTB risk for both White and Black women (Ahern, Pickett, Selvin, & Abrams, 2003). Moreover, heavy active smoking is a stronger risk factor for LBW among Black and Hispanic (versus White) women (Windham, Hopkins, Fenster, & Swan, 2000). Therefore, we expect to find a significant association between M and Y for White, Black, and Hispanic women. Rates of prenatal smoking among Asians are typically very low (Curtin & Mathews, 2016); therefore, we do not anticipate prenatal smoking will be an integral factor explaining neighborhood effects on LBW or PTB among this subgroup.
In terms of the association between X and M, we argue that because neighborhood affluence signals the ability of residents to draw local institutions to their community that can serve all residents, women living in areas of high affluence may have better access to organizational and institutional resources that can be drawn upon to quit smoking. Therefore, we assert higher levels of neighborhood affluence are likely to be associated with a lower risk of prenatal smoking. Thus, we hypothesize that:
H3:
Prenatal smoking significantly mediates the association between neighborhood affluence and poor birth outcomes among white, black, and hispanic women.
Methods
Data and sample
This study analyzes the Electronic Birth Certificate (EBC) records of 1,215,806 births in New Jersey from 1996 to 2006. We successfully geocoded 95.7% of all EBC records, then used the FIPS code to append neighborhood-level data to the individual (birth record)-level data.
The analytic sample includes all live (n = 1,213,278), singleton (n = 1,163,697) infants with no known birth defects (n = 1,139,217) and plausible [according to (Oken, Kleinman, Rich-Edwards, & Gillman, 2003)] gestational ages (n = 1,136,055) born to non-Hispanic Black, non-Hispanic White, Hispanic, and Asian women (n = 1,133,897) residing in an urban census tract (meaning, a census tract in which 100% of the total population was inside an urbanized area), for whom a plausible geocode could be assigned (n = 846,478). Multiple births were excluded on the basis of distinct distributions of birthweight and gestational age, relative to singleton births (Alexander, Kogan, Martin, & Papiernik, 1998); infants with significant birth defects were excluded given substantial dissimilarities between these and otherwise healthy infants (Mathews, MacDorman, & Thoma, 2015). We selected tracts to maximize opportunities for comparison with the existing literature on the topic. Similarly, we included only urban areas on the basis that past indices of neighborhood disadvantage and affluence were developed for, and tested within, urban areas.
Measures
Birth outcomes and maternal health behaviors
We examined two birth outcomes: LBW (<2500 g) and PTB (delivery at <37 weeks). Maternal health behaviors included any prenatal smoking during the last trimester of pregnancy (yes/no).
Neighborhood affluence and neighborhood disadvantage
We replicated indices for neighborhood affluence and neighborhood disadvantage from past research (King et al., 2011). The affluence index consists of the proportion of 16+ year old civilian workers in professional/managerial occupations, proportion of 25+ year olds with a college degree or higher, and median home values. [These variables were internally consistent (Cronbach’s alpha = .93) indicating scale reliability. An exploratory factor analysis (EFA) demonstrated a single factor solution explaining 78% of the variance. The disadvantage index consists of the proportion of households with income <$15,000, proportion of households with income >=$50,000 (reverse coded), proportion of families in poverty, proportion of households receiving public assistance, total unemployment rate, and proportion of vacant housing units (Cronbach’s alpha = .92). An EFA revealed a single factor solution explaining 74% of the variance. We standardized all variables and constructed each index by taking the average value of the standardized variables. Thus, values of each index can be interpreted as the number of standard deviations away from the New Jersey state urban mean levels. To avoid imposing an assumption of linearity on the association between the neighborhood indices and birth outcomes, we calculated quartiles of each index. Hereafter we refer to quartile 1 as “very low”, quartile 2 as “moderately low”, quartile 3 as “moderately high,” and quartile 4 as “very high.” A Pearson’s correlation matrix of the quartiles of affluence and disadvantage is presented in Appendix A.
We obtained data on these measures for all urban census tracts in New Jersey from the three decennial censuses spanning our data: 1990, 2000, and 2010. Linear interpolation was used to calculate estimates of each indicator for intercensal years. This step produced index scores that approximate the maternal neighborhood environment during the infant’s actual year of birth. Index scores were merged with data from the birth certificate based on infant’s birth year and mother’s census tract at the time of delivery.1
In supplementary analyses, we replicated all models replacing neighborhood disadvantage quartiles with quartiles of the Neighborhood Deprivation Index (NDI), which is calculated based on the tract-level proportion of: households with public assistance income, unemployed adults over age 16 years old, households with income below the federal poverty level, female-headed households with children, adults with no high school diploma, households with an annual income <$30,000, adult males in managerial occupations, and crowded households (i.e. >1 person per room). The Pearson correlation between the neighborhood disadvantage index and the NDI in our data was .95. All multivariable analyses using the NDI in place of neighborhood disadvantage were extremely similar in both magnitude and pattern of significance. (Results available upon request.).
Maternal and infant covariates
Some scholars argue that any observed effect of neighborhoods on health may not reflect an independent (causal) effect, but instead may signal residual confounding—whereby an unmeasured individual-level factor—such as SES that is integral in an individual’s decision of where to live and can also affect reproductive health outcomes—confounds the neighborhood-health association. Studies attempt to safeguard against residual confounding by including measures of individual-level SES, such as maternal education, paternal education, and family income (Cubbin et al., 2008); we adopt this approach in our study. Thus, we include the following maternal covariates: level of education [did not complete high school, high school diploma (reference), some college, Bachelor’s degree or higher]; employment in the year preceding the birth (yes/no); participation in Medicaid/Healthy Start during pregnancy (yes/no) as a proxy of woman’s income and financial resources at that time; marital status (married/unmarried); father named on the birth certificate (yes/no); foreign (versus native) born status; and age [10–14, 15–19, 20–24, 25–29 (reference), 30–34, 35–39, and 40+]. Infant covariates included male sex (yes/no) and parity (1, 2, 3+). Birth year fixed effects were included to account for temporal changes in birth outcomes over the study period.
Statistical analyses
We first plot neighborhood affluence against neighborhood disadvantage to assess the extent to which the two indices are distinct. Next, we describe our sample with summary statistics for all analytic variables stratified by race-ethnicity. We then construct race/ethnic-specific multilevel generalized linear regression models in Stata 13.0 where infant i is nested within neighborhood j (Raudenbush & Bryk, 2001). We present estimates from two-level random-intercept models with robust standard errors using all eligible births.
We evaluated the proportion of neighborhood-level (level 2) variance explained in each model using modified R2 statistics, based on a strategy outlined in Raudenbush and Bryk (2001). To do so, we define the baseline residual variance () for each outcome by estimating a null model that includes all level-1, but no level-2, covariates. Then we include the neighborhood indices (either one at a time, or together) in the model to define the tau value for the adjusted model (). We estimate of the proportion of level-2 variance explained according to the following formula:
Thus, the R2level-2 is interpreted as the proportion of true between-tract variance that is explained by each neighborhood index (or, set of neighborhood indices when both are included).
We assess mediation using Sobel-Goodman mediation tests (Baron & Kenny, 1986). Here, we rely on the neighborhood affluence and neighborhood disadvantage indices to simplify the calculation and interpretation of mediation. As a result, we describe results relating to mediation as providing preliminary, not conclusive, evidence of mediation.
Missing data in the EBC records is minimal (0–2%). We employ complete case analysis on the basis that this method produces unbiased estimates when missingness depends only on the independent variables modeled, and not on the response variable (Allison, 2000).
Results
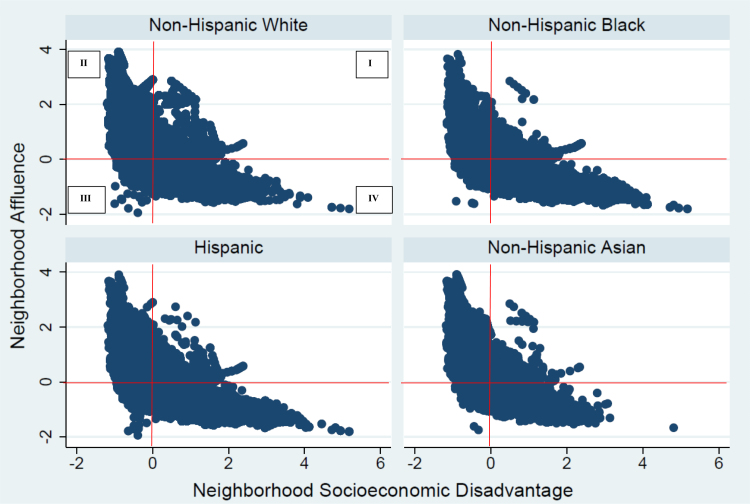
Fig. 1 plots neighborhood affluence against neighborhood disadvantage. Results suggest the two indices capture empirically distinct dimensions of neighborhood context; this holds for all four race-ethnic groups observed. Nearly one quarter of infants in our sample were born to mothers living in neighborhoods characterized by low affluence and low disadvantage (Quadrant III, N = 174,241, 20.6%), or high affluence and high disadvantage (Quadrant I, N = 27,164, 3.2%). These proportions are remarkably similar by race-ethnicity.
Fig. 1.
Plot of neighborhood affluence versus neighborhood socioeconomic disadvantage in New Jersey, 1996–2006, by maternal race-ethnicity.
Appendix B further portrays this distinction. Neighborhoods within QIII are characterized as working-class: both disadvantage (mean = -.33) and affluence are relatively low (mean = -.35). Compared to neighborhoods in the two high-disadvantage quadrants, neighborhoods falling into QIII contained a lower proportion of families living in poverty [5%; versus 11% (QI) and 20% (QIV)] and a lower total unemployment rate [.06; versus .10 (QI) and .14 (QIV)]. However, comparing working-class neighborhoods in QIII to those falling into the two high-affluence quadrants shows lower proportions of civilians ages 16+ in professional/managerial occupations [23%; versus 35% (QI) and 40% (QII)] and lower proportions of individuals aged 25+ who have a college degree [28%; versus 45% (QI) and 53% (QII)].
We also explored the extent to which practice follows theory, whereby neighborhoods defined as affluent in our analysis contained local institutions that could benefit the health and wellbeing of all community members and/or stabilize the neighborhood. Indeed, supplementary analyses (not shown) demonstrated that the percent of private (K-12) school enrollment increased as the level of neighborhood affluence increased; the reverse held for public (K-12) school enrollment. Supplementary analyses further suggested communities in which local clusters of high-high affluence were observed (based on a LISA map generated in R), also boasted high rankings in a summary measure of Health Factors (defined by health behaviors, access to and quality of clinical care, social and economic factors, community safety, environmental quality, and built environment) generated by the RWJF County Health Rankings (University of Wisconsin Population Health Institute, 2010).
Table 1 shows that non-Hispanic White (hereafter, “White”) and Asian mothers are, on average, exposed to neighborhoods characterized by below-average levels of disadvantage (-.41 and -.40, respectively) and above-average levels of affluence (.39 and .46, respectively). The opposite holds for Hispanic mothers (disadvantage = .39; affluence = -.48). On average, non-Hispanic Black (hereafter, “Black”) women are exposed to the most disadvantaged (.69) and least affluent (-.53) neighborhoods. These patterns are further described in Appendix C, which presents box plots showing values of the median and interquartile range of each neighborhood index.
Table 1.
Characteristics of the study sample.
| Variable | Percent or Mean (Standard Deviation) |
||||
|---|---|---|---|---|---|
| Non-Hispanic White | Non-Hispanic Black | Hispanic | Asian | ||
| Neighborhood-level Characteristics (level-2; n = 4,183) | |||||
| Neighborhood Affluence index (range: -1.9 - 3.9) | .39 (.86) | -.53 (.60) | -.48 (.64) | .46 (.77) | |
| Neighborhood Disadvantage index (range: -1.2 - 5.2) | -.41 (.56) | .69 (.97) | .39 (.78) | -.40 (.52) | |
| Individual-level Characteristics (level-1; n = 846,478) | |||||
| Low birth weight (%) | 3.95 | 11.20 | 5.64 | 6.13 | |
| Preterm birth (%) | 6.25 | 13.19 | 7.93 | 6.74 | |
| Prenatal smoking (%) | 11.28 | 13.44 | 5.29 | 1.13 | |
| Mother was foreign-born (%) | 12.12 | 20.46 | 72.37 | 94.41 | |
| Maternal education | |||||
| Less than high school (%) | 5.33 | 21.07 | 37.42 | 4.77 | |
| High school completion (%) | 26.80 | 40.05 | 34.79 | 12.90 | |
| Some college (%) | 22.92 | 23.82 | 16.43 | 21.10 | |
| Bachelor’s degree or higher (%) | 44.95 | 15.07 | 11.37 | 61.23 | |
| Mother employed in the past year (%) | 69.41 | 60.81 | 47.85 | 55.47 | |
| Medicaid/Healthy Start during pregnancy (%) | 10.74 | 44.50 | 46.52 | 9.74 | |
| Married at birth (%) | 85.54 | 30.88 | 44.75 | 94.24 | |
| Did not name father on birth certificate (%) | 2.83 | 24.89 | 9.47 | 1.55 | |
| Maternal age at birth (range = 13–63) | 30.62 (5.43) | 26.45 (6.52) | 26.51 (6.16) | 30.30 (4.78) | |
| Male infant (%) | 51.22 | 50.88 | 51.14 | 51.30 | |
| Parity | |||||
| One (%) | 41.74 | 38.32 | 40.30 | 49.42 | |
| Two (%) | 35.44 | 30.22 | 33.59 | 37.75 | |
| Three or higher (%) | 22.81 | 31.46 | 26.11 | 12.83 | |
| Sample Size | 390,936 | 153,864 | 218,949 | 69,760 | |
Source: Electronic Birth Certificate Records from the State of New Jersey (1996 – 2006).
Table 2 presents the results of a series of race-stratified models predicting the risk of LBW. Results for PTB were extremely similar to those for LBW and are available from the authors upon request. The first series of models presents results for non-Hispanic Whites. Model 1 includes only level-1 covariates; all coefficients are in the expected direction based on past research. Birth year fixed-effects are included in this, and all other models, but are not shown. The value of tau here (.017) is taken as the null, indicating the total amount of between-neighborhood variance in LBW. Model 2 adds quartiles of neighborhood disadvantage. Relative to residing in a neighborhood with a very low level of disadvantage, residing in a neighborhood with a moderately low (adjusted odds ratio (AOR): 1.09, 95% confidence interval (CI): 1.04–1.14), moderately high (AOR: 1.13, 95% CI: 1.07–1.19), or very high (AOR: 1.22, 95% CI: 1.13–1.32) level of disadvantage is associated with increased odds of LBW. Model 3 is nested within Model 1 and adds neighborhood affluence. Living in a neighborhood with a moderately low (AOR: .89, 95% CI: .84–.95), moderately high (AOR: .84, 95% CI: .79–.90), or very high (AOR: .77, 95% CI: .72–.82) level of affluence is associated with lower odds of LBW. Model 4 includes both neighborhood disadvantage and affluence; disadvantage is no longer significantly associated with LBW, whereas the point estimates for affluence are only slightly attenuated.
Table 2.
Odds ratios from the multilevel logistic regression model predicting low birth weight status, by maternal race-ethnicity.
| Non-Hispanic White |
Non-Hispanic Black |
|||||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | Model 8 | |
| Neighborhood Characteristics | ||||||||
| Neighborhood Disadvantage (ref = Quartile 1) | ||||||||
| Quartile 2 | 1.09*** | 1.04 | 1.08 | 1.00 | ||||
| [1.04, 1.14] | [.99, 1.09] | [.98, 1.18] | [.90, 1.11] | |||||
| Quartile 3 | 1.13*** | 1.03 | 1.16*** | 1.03 | ||||
| [1.07, 1.19] | [.97, 1.10] | [1.06, 1.26] | [.92, 1.15] | |||||
| Quartile 4 | 1.22*** | 1.08 | 1.30*** | 1.13* | ||||
| [1.13, 1.32] | [.99, 1.18] | [1.20, 1.41] | [1.01,1.26] | |||||
| Neighborhood Affluence (ref = Quartile 1) | ||||||||
| Quartile 2 | 0.89*** | 0.90** | 0.91*** | 0.95* | ||||
| [.84, .95] | [.84, .97] | [.88, .95] | [.91, .99] | |||||
| Quartile 3 | 0.84*** | 0.86*** | 0.86*** | 0.93 | ||||
| [.79, .90] | [.80, .92] | [.81, .91] | [.86, 1.00] | |||||
| Quartile 4 | 0.77*** | 0.80*** | 0.74*** | 0.81*** | ||||
| [.72, .82] | [.73, .87] | [.69, .80] | [.73, .90] | |||||
| Maternal and Infant Characteristics | ||||||||
| Mother was foreign-born | 0.84*** | 0.83*** | 0.83*** | 0.82*** | 0.66*** | 0.66*** | 0.67*** | 0.67*** |
| Maternal Education (ref = high school completion) | ||||||||
| Less than high school | 1.38*** | 1.36*** | 1.35*** | 1.35*** | 1.19*** | 1.18*** | 1.18*** | 1.17*** |
| Some college | 0.83*** | 0.83*** | 0.84*** | 0.84*** | 0.85*** | 0.86*** | 0.86*** | 0.86*** |
| Bachelor’s degree or higher | 0.66*** | 0.68*** | 0.69*** | 0.69*** | 0.72*** | 0.74*** | 0.75*** | 0.75*** |
| Mother employed in the past year | 1.01 | 1.00 | 1.00 | 1.00 | 0.80*** | 0.81*** | 0.80*** | 0.81*** |
| Participated in Medicaid/Healthy Start | 1.10*** | 1.07* | 1.07* | 1.07* | 0.82*** | 0.81*** | 0.81*** | 0.81*** |
| Mother married at birth | 0.65*** | 0.65*** | 0.66*** | 0.66*** | 0.71*** | 0.72*** | 0.72*** | 0.72*** |
| Mother named father on birth certificate | 1.22*** | 1.22*** | 1.22*** | 1.22*** | 1.15*** | 1.15*** | 1.15*** | 1.14*** |
| Maternal age at birth (ref = age 25–29) | ||||||||
| Less than 19 | 0.69*** | 0.69*** | 0.69*** | 0.69*** | 0.65*** | 0.65*** | 0.64*** | 0.64*** |
| 20–24 | 0.84*** | 0.83*** | 0.83*** | 0.83*** | 0.79*** | 0.79*** | 0.79*** | 0.79*** |
| 30–34 | 1.12*** | 1.13*** | 1.14*** | 1.14*** | 1.27*** | 1.28*** | 1.28*** | 1.28*** |
| 35–39 | 1.40*** | 1.42*** | 1.43*** | 1.43*** | 1.56*** | 1.58*** | 1.58*** | 1.58*** |
| 40+ | 1.96*** | 1.99*** | 2.01*** | 2.01*** | 1.81*** | 1.84*** | 1.84*** | 1.84*** |
| Male infant | 0.84*** | 0.84*** | 0.84*** | 0.84*** | 0.82*** | 0.82*** | 0.82*** | 0.82*** |
| Parity (ref = first birth) | ||||||||
| Second birth | 0.55*** | 0.55*** | 0.55*** | 0.55*** | 0.75*** | 0.75*** | 0.75*** | 0.75*** |
| Third or higher order birth | 0.54*** | 0.53*** | 0.53*** | 0.53*** | 0.80*** | 0.79*** | 0.79*** | 0.79*** |
| Log likelihood | -61,672 | -61,654 | -61,641 | -61,639 | -49,084 | -49,050 | -49,051 | -49,042 |
| Nested model comparison | M2 vs. M1 | M3 vs. M1 | M4 vs. M3 | M6 vs. M5 | M7 vs. M5 | M8 vs. M7 | ||
| Level of significance from likelihood ratio test | 0.000 | 0.000 | 0.176 | 0.000 | 0.000 | 0.003 | ||
| Preferred model (based on LR test) | M2 | M3 | M3 | M6 | M7 | M8 | ||
| Tau | 0.017 | 0.017 | 0.014 | 0.015 | 0.013 | 0.008 | 0.009 | 0.007 |
| R2level2 | 0 | 0.176 | 0.118 | 0.385 | 0.308 | 0.462 | ||
| Hispanic |
Asian |
|||||||
|---|---|---|---|---|---|---|---|---|
| Model 9 | Model 10 | Model 11 | Model 12 | Model 13 | Model 14 | Model 15 | Model 16 | |
| Neighborhood Characteristics | ||||||||
| Neighborhood Disadvantage (ref = Quartile 1) | ||||||||
| Quartile 2 | 1.11* | 1.10 | 1.14** | 1.04 | ||||
| [1.01, 1.23] | [.99, 1.22] | [1.05,1.24] | [.95, 1.14] | |||||
| Quartile 3 | 1.25*** | 1.21*** | 1.24*** | 1.05 | ||||
| [1.14, 1.37] | [1.09, 1.36] | [1.13,1.37] | [.92, 1.19] | |||||
| Quartile 4 | 1.39*** | 1.31*** | 1.40*** | 1.17 | ||||
| [1.26, 1.52] | [1.16, 1.47] | [1.22,1.60] | [.99, 1.39] | |||||
| Neighborhood Affluence (ref = Quartile 1) | ||||||||
| Quartile 2 | 0.88*** | 0.93** | 1.04 | 1.09 | ||||
| [.84, .93] | [.88, .98] | [.90,1.21] | [.93, 1.27] | |||||
| Quartile 3 | 0.86*** | 0.96 | 0.91 | 0.98 | ||||
| [.80, .91] | [.89, 1.04] | [.79,1.05] | [.83, 1.16] | |||||
| Quartile 4 | 0.76*** | 0.91 | 0.75*** | 0.83* | ||||
| [.70, .83] | [.81, 1.01] | [.65, .87] | [.69, .99] | |||||
| Maternal and Infant Characteristics | ||||||||
| Mother was foreign-born | 0.72*** | 0.71*** | 0.71*** | 0.71*** | 1.00 | 0.98 | 0.98 | 0.97 |
| Maternal Education (ref = high school completion) | ||||||||
| Less than high school | 1.08** | 1.07** | 1.07** | 1.06** | 1.08 | 1.06 | 1.06 | 1.06 |
| Some college | 0.95 | 0.96 | 0.96 | 0.96 | 0.92 | 0.94 | 0.95 | 0.95 |
| Bachelor’s degree or higher | 0.86*** | 0.89** | 0.89** | 0.90** | 0.77*** | 0.81*** | 0.82*** | 0.83*** |
| Mother employed in the past year | 0.96* | 0.96 | 0.96* | 0.96 | 1.05 | 1.06 | 1.05 | 1.05 |
| Participated in Medicaid/Healthy Start | 0.89*** | 0.87*** | 0.87*** | 0.87*** | 0.93 | 0.90 | 0.89 | 0.89* |
| Mother married at birth | 0.82*** | 0.84*** | 0.83*** | 0.84*** | 0.86* | 0.89 | 0.89 | 0.90 |
| Mother named father on birth certificate | 1.25*** | 1.24*** | 1.24*** | 1.24*** | 1.21 | 1.21 | 1.22 | 1.22 |
| Maternal age at birth (ref = age 25–29) | ||||||||
| Less than 19 | 1.02 | 1.01 | 1.01 | 1.01 | 0.91 | 0.92 | 0.92 | 0.92 |
| 20–24 | 0.98 | 0.98 | 0.98 | 0.98 | 1.11 | 1.10 | 1.10 | 1.10 |
| 30–34 | 1.14*** | 1.15*** | 1.15*** | 1.15*** | 0.99 | 1.00 | 1.01 | 1.01 |
| 35–39 | 1.45*** | 1.48*** | 1.47*** | 1.48*** | 1.22*** | 1.25*** | 1.26*** | 1.26*** |
| 40+ | 1.81*** | 1.85*** | 1.84*** | 1.85*** | 1.85*** | 1.89*** | 1.89*** | 1.90*** |
| Male infant | 0.86*** | 0.86*** | 0.86*** | 0.86*** | 0.91** | 0.91** | 0.91** | 0.91** |
| Parity (ref = first birth) | ||||||||
| Second birth | 0.70*** | 0.70*** | 0.70*** | 0.70*** | 0.67*** | 0.68*** | 0.67*** | 0.67*** |
| Third or higher order birth | 0.74*** | 0.73*** | 0.73*** | 0.73*** | 0.64*** | 0.64*** | 0.63*** | 0.63*** |
| Log likelihood | -44,438 | -44,401 | -44,409 | -44,396 | -15,379 | -15,363 | -15,355 | -15,353 |
| Nested model comparison | M10 vs. M9 | M11 vs. M9 | M12 vs. M11 | M14 vs. M13 | M15 vs. M13 | M16 vs. M15 | ||
| Level of significance from likelihood ratio test | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.184 | ||
| Preferred model (based on LR test) | M10 | M11 | M12 | M14 | M15 | M15 | ||
| Tau | 0.021 | 0.018 | 0.018 | 0.017 | 0.034 | 0.028 | 0.029 | 0.028 |
| R2level2 | 0.143 | 0.143 | 0.190 | 0.176 | 0.147 | 0.176 | ||
Note: ***p < .001, **p < .01, *p < .05 (two-tailed). Birth year fixed effects included in all models but not shown. 95% confidence intervals shown only for neighborhood variables.
Likelihood ratio tests (also presented in Table 2) are used to compare nested models, and show Model 3 is the preferred model for non-Hispanic Whites. Importantly, this suggests the addition of neighborhood disadvantage, above and beyond mother-level factors and neighborhood-level affluence, does not significantly improve model fit. This key finding is buttressed by two additional factors — that the tau value, indicating the amount of unexplained between-neighborhood variance in LBW, is lowest in Model 3, and that the R2level 2 is highest in Model 3, indicating that the inclusion of neighborhood affluence in Model 3 explains the greatest amount [(.017 - .014)/.017 = .176, or 17.6%] of between-neighborhood variance in LBW.
Among non-Hispanic Black women, the total between-neighborhood variance in LBW is .013 (Model 5). Residing in a neighborhood with a moderately high (AOR: 1.16, 95% CI: 1.06–1.26) or very high (AOR: 1.30, 95% CI, 1.20–1.41) level of disadvantage, relative to a very low level of disadvantage, is associated with increased odds of LBW (see Model 6). Conversely, living in a neighborhood with a moderately low (AOR: .91, 95% CI: .88–.95), moderately high (AOR: .86, 95% CI: .81–.91), or very high (AOR: .74, 95% CI: .69–.80) level of affluence is associated with lower odds of LBW (see Model 7). When both neighborhood disadvantage and affluence are included (in Model 8), only very high (versus very low) neighborhood disadvantage is statistically significant; this point estimate is reduced in both size (by more than half) and significance relative to model 6. For affluence, moderately low and very high affluence remain significantly different from very low levels; some attenuation in the magnitude of effect is also observed. Likelihood ratio tests show Model 8 is the best fit of the data for this subgroup; together, neighborhood affluence and disadvantage explain nearly half (46.2%) of the between-neighborhood variance in LBW.
Among Hispanic mothers, neighborhood disadvantage (Model 10) and neighborhood affluence (Model 11) are associated with the odds of LBW in the expected directions, but when both are included (in Model 12), two contrasts of neighborhood disadvantage [moderately high (AOR: 1.21, 95% CI: 1.09–1.36) and very high (AOR: 1.31, 95% CI: 1.16–1.47), relative to very low] remain statistically significant; the point estimates are only slightly attenuated relative to Model 10. On the other hand, only moderately low (versus very low) affluence remains statistically significant (AOR, .93, 95% CI: .88–.98). Still, the model including both neighborhood disadvantage and neighborhood affluence (Model 12) is preferred according to the likelihood ratio test; together these neighborhood-level factors explain 19% of the between-neighborhood variance in LBW.
Results for Asian mothers show higher quartiles of neighborhood disadvantage are associated with increased odds of LBW (Model 14), but, importantly, these associations did not remain significant in the full model (16) when neighborhood affluence was included. Very high (versus very low) neighborhood affluence is associated with decreased odds of LBW (AOR: .75, 95% CI: .65–.87; Model 15); this contrast was reduced in both size and statistical significance in the full model but remained statistically significant (AOR: .83, 95% CI: .69–.99). The model including only neighborhood affluence but not disadvantage (Model 15) was preferred according to the likelihood ratio test; in this model, neighborhood affluence explains 14.7% of the between-neighborhood variance in LBW.
These results demonstrate broad support for Hypothesis 1—that neighborhood affluence is protective against the risk of poor birth outcomes, above and beyond the effects of neighborhood disadvantage. This finding is buttressed by a set of supplementary analyses we performed, in which we replicated these analyses for several other birth outcomes (very LBW, small for gestational age, PTB, early PTB, and late PTB; findings for LBW also shown for comparison). Here we employed index values instead of quartile groupings for ease of presentation, although results for quartile groups were extremely similar. Results are presented in Appendix D. Neighborhood affluence was protective against the risk of poor birth outcome in nearly all (19 out of 24) cases. Furthermore, in 12 instances, we would have incorrectly concluded that neighborhood context was not significantly related to a key birth outcome had we explored only neighborhood disadvantage, and not affluence. These were all cases in which disadvantage was not a significant predictor of poor birth outcome, but neighborhood affluence was.
With respect to Hypothesis 2, Table 2 results suggest the effects of affluence are the most consistent and, in most cases, the strongest among White mothers, but are nontrivial among Black and Asian mothers as well. (Here we interpret findings from the preferred model for each race-ethnic group.) All else equal, a White woman residing in a neighborhood with a moderately low (versus very low) level of affluence, has an 11% reduced odds of LBW; for Black women, this contrast is associated with a 5% reduction, and for Hispanic women, a 7% reduction (the OR for Asian women here is not significant). Similarly, residing in a moderately high (versus very low) level of neighborhood affluence is associated with a 16% decreased odds of LBW for White women (the OR for all other race-ethnic groups is not significant). Residing in a neighborhood characterized by very high (versus very low) affluence is associated with a 23% reduction in the odds of LBW for White women; the corollary is 19% for Black women, and 25% for Asian women (the contrast is not statistically significant for Hispanic women). Here we see that the OR for Asian women (.75) exceeds that of White women (.77), suggesting affluence plays an important role in LBW risk for Asian women as well. Affluence appears to play less of a role in contributing to LBW risk among Hispanic women in our data.
Table 3 presents a summary of results from multilevel logistic regression models examining prenatal smoking as a mediator of neighborhood effects on LBW. Again, the results for PTB were extremely similar to those for LBW and are not presented (results available upon request). The first model shown for each race-ethnic group in Table 3 is comparable to the group-specific full model presented in Table 2, except that here, the index values of neighborhood affluence and disadvantage are included. Logit coefficients and standard errors are presented. The second model for each group adds prenatal smoking. Statistics presented at the bottom of Table 3 can be used to assess the extent to which prenatal smoking mediates the observed neighborhood effects on LBW.
Table 3.
Results from logistic regression models examining prenatal smoking as a mediator of neighborhood effects on low birth weight.
| Non-Hispanic White |
Non-Hispanic Black |
Hispanic |
Asian |
|||||
|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | Model 8 | |
| Neighborhood Disadvantage | 0.035 | 0.041 | 0.048*** | 0.041** | 0.126*** | 0.119*** | 0.033 | 0.027 |
| (0.021) | (0.021) | (0.014) | (0.014) | (0.018) | (0.018) | (0.045) | (0.045) | |
| Neighborhood Affluence | -0.095*** | -0.078*** | -0.089*** | -0.085*** | -0.038 | -0.041 | -0.163*** | -0.165*** |
| (0.015) | (0.015) | (0.023) | (0.023) | (0.023) | (0.023) | (0.032) | (0.032) | |
| Prenatal Smoking | 0.548*** | 0.556*** | 0.478*** | -0.073 | ||||
| (0.023) | (0.023) | (0.036) | (0.150) | |||||
| Maternal and Infant Covariates | Included | Included | Included | Included | Included | Included | Included | Included |
| Log likelihood | -61,586 | -60,994 | -48,721 | -48,132 | -44,280 | -44,055 | -15,317 | -15,299 |
| LR test: improved model fit? | Yes | Yes | Yes | Yes | ||||
| Neighborhood Disadvantage | ||||||||
| Sobel-Goodman Mediation Test Statistic | – | 10.41*** | 10.89*** | – | ||||
| Proportion explained by prenatal smoking | none | 14.6% | 5.5% | none | ||||
| Neighborhood Affluence | ||||||||
| Sobel-Goodman Mediation Test Statistic | -21.16*** | – | – | – | ||||
| Proportion explained by prenatal smoking | 17.9% | none | none | none | ||||
Note: ***p < .001, **p < .01, *p < .05 (two-tailed). Logit coefficients and standard errors presented. Maternal and infant covariates include: maternal education at birth, employment in year prior to birth, Medicaid status, foreign-born status, marital status, age, if she named the father on the birth certificate, infant sex, parity, and birth year fixed effects.
Among non-Hispanic Whites, higher levels of neighborhood affluence are protective against the risk of LBW; neighborhood disadvantage is not significant (see Model 1). Prenatal smoking is associated with increased odds of LBW (AOR = e.548 = 1.73, 95% CI: 1.66–1.82; see Model 2). A likelihood ratio test indicates the addition of prenatal smoking is an improvement to the model. In terms of mediation, because neighborhood disadvantage is not a significant predictor of LBW (either here, or in Table 2 Model 4), condition 1 is not met and mediation of the neighborhood disadvantage—LBW association by prenatal smoking is not assessed. Results from Sobel-Goodman mediation tests demonstrate prenatal smoking was a significant mediator (z = -21.16, p < .001) of the neighborhood affluence—LBW association, and explains 17.9% of this association [(-.095 - -.078)/-.095 = .179].
Results for non-Hispanic Black and Hispanic women are similar: prenatal smoking is associated with increased odds of LBW (non-Hispanic Black: AOR = 1.74; Hispanic: AOR = 1.61), and its addition to the full model confers a significant improvement in model fit for both race-ethnic groups. Sobel-Goodman mediation tests demonstrate prenatal smoking is a statistically significant mediator of the neighborhood disadvantage—LBW association (non-Hispanic Black: z = 10.41, p < .001; Hispanic: z = 10.89, p < .001), explaining 14.6% of this association for Black women and 5.5% of this association for Hispanic women. In both groups, prenatal smoking is not a significant mediator linking the neighborhood affluence index to LBW. For Asian women, prenatal smoking is not a significant predictor of LBW and therefore no potential mediation is assessed.
We explored the extent to which these mediation results were robust to assumptions made about confounding in the modeling process (T. VanderWeele, 2016a) by estimating the total effect and controlled direct effect of neighborhood affluence (or disadvantage) on LBW, separately by race-ethnicity, using inverse probability weighted marginal structural modeling. This approach uses weighting to account for confounding of the exposure-outcome and, in the case of the controlled direct effect, the mediator-outcome relation. Results (available upon request) suggest these findings are robust. Among non-Hispanic White women, the controlled direct effect of neighborhood affluence on LBW was weaker in magnitude than the total effect of neighborhood affluence on LBW, but remained statistically significant and substantively meaningful. Similarly, the controlled direct effect of neighborhood disadvantage on LBW tended to be weaker than the total effect for non-Hispanic Black and Hispanic women but remained statistically significant. For all women, prenatal smoking was a significant predictor of LBW status. This lends further evidence that neighborhood affluence operates on LBW both through pathways mediated by prenatal smoking and pathways not mediated by prenatal smoking.
Discussion
This study examined whether neighborhood affluence — a sociological construct signaling the presence of highly educated, wealthy residents employed in prestigious occupations who can effectively draw local institutions to their community that can stabilize the neighborhood and meet the basic needs of residents — was protective against the risk of LBW and PTB using race/ethnic-stratified multilevel models and population-based data from New Jersey. Potential mediation by a key maternal prenatal health behavior, prenatal smoking, was also assessed. This study was informed by a broader literature on adult health showing neighborhood affluence to be an important, and at times, superior construct (relative to neighborhood disadvantage) in explaining how an individual’s health is affected by their social environment.
Our study contributes three new findings to the literature. Grounded in social disorganization theory (Kornhauser, 1978, Shaw and McKay, 1942), we hypothesized that neighborhood affluence would be inversely associated with the risk of poor birth outcomes (H1), and that this association would vary by maternal race-ethnicity (H2). Study findings demonstrated broad support for both hypotheses. Even in the very different spaces occupied by the four race-ethnic groups examined here (White, Black, Hispanic, Asian), affluence persisted in its effect as a protective factor against the risk of LBW (and PTB; results not shown); importantly, affluence also persisted in its effect after neighborhood disadvantage was included in the model. In addition, the association between neighborhood affluence and poor birth outcome was the most consistent, and appeared to be the strongest among White mothers, but played a nontrivial role in contributing to LBW (and PTB) risk among Asian and Black mothers as well. The birth outcomes of Hispanic mothers appeared to be the least influenced by neighborhood affluence.
Both study findings are new contributions to the literature, but the protective effect of affluence observed for all race-ethnic groups is consistent with studies examining the role of neighborhood-level education in protecting against the risk of poor birth outcome (Messer et al., 2008, Nkansah-Amankra et al., 2010, Pearl et al., 2001, Subramanian et al., 2006) and with Roberts (1997) study showing the protective effect of neighborhood quality on LBW risk in Chicago in 1990. Roberts’ study was the only past study to use a construct similar to what we assess here; however, Roberts did not employ race-stratified models. Our study expands knowledge in this area by showing that the protective effect of affluence on birth outcomes is observed among White, Black, Hispanic, and Asian women in New Jersey. Compared with past research, our study also more fully describes the theoretical processes undergirding these associations.
Supplementary analyses also showed that higher levels of the neighborhood affluence index were associated with decreased risk of poor birth outcome in 19 out of 24 race-stratified models (predicting LBW, very LBW, small for gestational age, PTB, early PTB, and late PTB). Furthermore, in 12 instances, we would have incorrectly concluded that neighborhood context was not significantly related to a key birth outcome had we explored only neighborhood disadvantage and not affluence. Such evidence may help reconcile mixed findings from past studies showing inconsistent effects of neighborhoods on birth outcomes risk [e.g., Cubbin et al., 2008].
This finding challenges the extant research in this field that has, until now, focused largely on disadvantage. Instead, this study finding suggests both neighborhood affluence and disadvantage are key constructs in terms of understanding how neighborhood context can affect birth outcomes. We also provided evidence demonstrating that affluence is not simply the converse of disadvantage; more than a quarter of mothers in our sample lived in neighborhoods characterized by low-disadvantage/low-affluence or high-disadvantage/high-affluence. Consistent with past research (King et al., 2011, Morenoff et al., 2007), this suggests disadvantage and affluence describe unique aspects of women’s social environment.
More consistent effects of affluence on the risk of poor birth outcome among White (versus Black, Hispanic, and Asian) mothers adds to the mixed state of the literature examining race-specific effects of constructs similar to neighborhood affluence. This finding is somewhat consistent with the findings of Gorman (1999) and Messer et al. (2008), but different from Pearl et al. (2001) study showing a significant association between low neighborhood education and decreased birthweight only for Black and Asian, but not White or Latina mothers. Future research should continue to explore the race-specific effects of neighborhood affluence on perinatal health to further inform this literature.
While not a main focus of our study, results also documented that neighborhood disadvantage, net of neighborhood affluence, was not significantly associated with the risk of poor birth outcome among White and Asian mothers, but remained statistically significant for Black and Hispanic mothers. These findings are new contributions to the literature, given that no prior research has tested the role of disadvantage net of affluence within a race-specific model. This finding is generally consistent however with past work showing neighborhood disadvantage is particularly important for the birth outcomes of Black women (Blumenshine et al., 2010, Buka et al., 2003, Janevic et al., 2010, Messer et al., 2006a).
Our study’s third contribution is that we revealed a plausible individual-level mechanism, prenatal smoking, underlying the association between neighborhood context and birth outcomes. Prenatal smoking explained approximately 18% of the association between the neighborhood affluence index and LBW among White mothers, and approximately 14% and 5% the association between the neighborhood disadvantage index and LBW among Black and Hispanic mothers, respectively. Our study results are consistent with past research showing the effect of neighborhood disadvantage on birth outcomes is mediated by prenatal smoking (Schempf et al., 2009), but goes beyond past research by showing this mediation is observed for Black and Hispanic mothers only. Our work also adds to the literature by showing prenatal smoking mediates the effect of neighborhood affluence for White mothers. Future studies should examine other potential mediators of neighborhood affluence on birth outcomes. As has been shown in relation to neighborhood disadvantage (Masi et al., 2007, Nkansah-Amankra, 2010, Schempf et al., 2009), violent crime, maternal stress, and lack of social support may be particularly insightful.
Because the analyses presented in Table 3 relied on neighborhood affluence (and disadvantage) index values instead of quartile groupings, we couch our results as preliminary evidence of statistical mediation of prenatal smoking. However, these results were buttressed by a supplementary analysis estimating the controlled direct effect of neighborhood affluence (and disadvantage), by quartiles, on LBW using inverse probability weighted structural marginal models, and showing partial mediation of these associations by prenatal smoking. These results are also consistent with a fairly wide literature supporting a descriptive association between neighborhood deprivation and prenatal smoking (Finch et al., 2001, Nkansah-Amankra, 2010, Räisänen et al., 2014) and a causal association between prenatal smoking and birth weight (Reichman et al., 2006, Wehby et al., 2011). Overall, the evidence supports the plausibility of prenatal smoking as a mediator. Future work however should continue to capitalize on the burgeoning interest in mediation analysis in public health [see for example VanderWeele, 2016a, VanderWeele, 2016b] to expand this line of inquiry.
Study limitations should be noted. If a mother moved during pregnancy, our indicator of maternal neighborhood environment represents her neighborhood at birth, but not her prenatal neighborhood. Future studies with data on maternal residence at the time of conception and at birth could explore these differences. Additionally, administratively-defined neighborhood boundaries, such as tracts, only approximate the social spaces individuals encounter (Galster, 2001), but are a reasonable approximation for neighborhoods (O’Campo, O’Brien Caughy, Oakes, & Kaufman, 2006). Furthermore, neighborhood effects may be misestimated (Oakes, 2004, Roux, 2004). Due to the nature of vital records data, we include several, but not all, preconception factors that may select women into the neighborhoods they lived in at the time of birth. Thus, the estimated effects of neighborhood disadvantage and affluence on adverse birth outcomes may be confounded by omitted variables determining both (a) the type of neighborhood in which women live at the time of birth, and (b) offspring’s health at birth. Future efforts should seek to replicate these findings using quasi-experimental methods that estimate mothers’ selection into a residential neighborhood. These efforts may be particularly useful in the case of affluence, whereby, a woman’s early life experiences (e.g., in the family-of-origin, through interacting with schools and other local institutions) likely condition her ability to reside in a high or low affluent area as well as key factors linking the neighborhood environment to birth outcomes; according to Culhane and Elo (2005) these include key health behaviors, psychosocial factors, social support, and maternal stress physiology.
In conclusion, this study documents the critical role of neighborhood affluence, above and beyond that of disadvantage, for several birth outcomes. This study adds new knowledge of two distal factors, neighborhood affluence and disadvantage, in the social environment that may, in the future, be confirmed as underlying causes (Link & Phelan, 1995) of poor birth outcomes and risky maternal prenatal health behaviors. In doing so, this study moves us closer to identifying the root causes of poor birth outcomes. Future research should seek to replicate this study’s findings in other populations. If replicated, this could lay the foundation upon which to develop innovative policy initiatives and prevention/intervention programs designed to improve birth outcomes in the United States and reduce stark racial disparities in birth outcomes.
Conflict of interest statement
The authors declare no conflict of interest, real or otherwise.
Ethics approval
This research was approved by the Institutional Review Boards at University of California, Irvine (9300) and University of North Carolina at Chapel Hill (12-296).
Acknowledgements
This research received support from the Eunice Kennedy Shriver National Institute of Child Health and Human Development: K99/R00 HD075860 (PI: Kane); Training Program in Reproductive, Perinatal and Pediatric Epidemiology, T32-HD52468 (PI: Siega-Riz); and P2C HD050924 (PI: Morgan) via computing and geospatial analysis support. Opinions reflect those of the authors and not necessarily those of the granting agency. The authors wish to thank Julien Teitler and Nancy Reichman for obtaining the data, and Brian Frizzelle for programming support.
Footnotes
Because census tract boundaries change over time, we identified 4183 urban tract-based neighborhoods that were temporally unique over the 10-year study period. We investigated alternatives methods to account for over-time boundary changes, including using normalized tract data, and determined that those methods do not necessarily provide more confident results than our approach.
Contributor Information
Jennifer B. Kane, Email: jbkane@uci.edu.
Gandarvaka Miles, Email: glgray@live.unc.edu.
Jennifer Yourkavitch, Email: yourkavi@live.unc.edu.
Katherine King, Email: katherine.king@duke.edu.
Appendix A
See Appendix Table A1.
Table A1.
Pearson correlations between quartiles of the Neighborhood Disadvantage (ND) Index and the Neighborhood Affluence (NA) Index.
| ND, Q1 | ND, Q2 | ND, Q3 | ND, Q4 | NA, Q1 | NA, Q2 | NA, Q3 | NA, Q4 | |
|---|---|---|---|---|---|---|---|---|
| ND, Q1 | 1 | |||||||
| ND, Q2 | -0.333* | 1 | ||||||
| ND, Q3 | -0.333* | -0.333* | 1 | |||||
| ND, Q4 | -0.333* | -0.333* | -0.333* | 1 | ||||
| NA, Q1 | -0.333* | -0.300* | 0.040* | 0.593* | 1 | |||
| NA, Q2 | -0.296* | 0.014* | 0.322* | -0.039* | -0.332* | 1 | ||
| NA, Q3 | -0.011* | 0.339* | -0.085* | -0.243* | -0.332* | -0.332* | 1 | |
| NA, Q4 | 0.643* | -0.053* | -0.276* | -0.3150 | -0.332* | -0.332* | -0.332* | 1 |
Appendix B
See Appendix Table B1.
Table B1.
Mean of neighborhood affluence and neighborhood disadvantage indices, and proportions of indicator variables for each index, by quadrant of affluence versus disadvantage plot.
| Variable | Quadrant I | Quadrant II | Quadrant III | Quadrant IV |
|---|---|---|---|---|
| (High disadvantage, High affluence) | (Low disadvantage, High affluence) | (Low disadvantage, Low affluence) | (High disadvantage, Low affluence) | |
| Neighborhood Affluence | .53 | .89 | -.35 | -.75 |
| Indicators: | ||||
| Percent of Civilians Aged 16+ in Professional/Managerial Occupations | 34.77% | 40.41% | 23.27% | 16.50% |
| Percent of Individuals Aged 25+ with College Degree or Higher | 45.35% | 52.95% | 28.20% | 19.41% |
| Median Home Value | $237,399 | $271,694 | $156,634 | $132,712 |
| Neighborhood Disadvantage | .56 | -.67 | -.33 | .93 |
| Indicators: | ||||
| Percent of Households with Incomes < $15,000 | 17.94% | 6.83% | 10.33% | 25.57% |
| Percent of Households with Incomes >= $50,000 | 43.69% | 67.58% | 51.65% | 30.39% |
| Percent of Families in Poverty | 10.92% | 2.87% | 5.06% | 20.35% |
| Percent of Households receiving Public Assistance Income | 3.48% | 1.34% | 2.44% | 9.17% |
| Total Unemployment Rate | .10 | .04 | .06 | .14 |
| Percent of Housing Units that are Vacant | 20.96% | 3.43% | 4.43% | 9.67% |
| Number of Level-2 Units | 145 | 1,730 | 919 | 1,389 |
Source: Electronic Birth Certificate Records from the State of New Jersey (1996 – 2006)
Appendix C
See Appendix Fig. 2.
Fig. 2.
Box Plot of the neighborhood affluence index (Panel A) and the neighborhood disadvantage index (Panel B), by maternal race-ethnicity.
Appendix D
See Appendix Table D1.
Table D1.
Summary of results from multilevel models regressing perinatal health outcomes on affluence and disadvantage.
|
Non-Hispanic White |
non-Hispanic Black |
Hispanic |
non-Hispanic Asian |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| AOR [95% CI] | R2level2 | AOR [95% CI] | R2level2 | AOR [95% CI] | R2level2 | AOR [95% CI] | R2level2 | |||
| Low Birth Weight | ||||||||||
| Neighborhood Affluence index | .909*** | .176 | .914*** | .231 | .963 | 0.19 | .849*** | .353 | ||
| [.883, .936] | [.873, .957] | [.920, 1.007] | [.797, .905] | |||||||
| Neighborhood Disadvantage index | 1.036 | .000 | 1.049** | .385 | 1.134*** | .381 | 1.034 | .118 | ||
| [.994, 1.080] | [1.021, 1.079] | [1.094, 1.176] | [.947, 1.129] | |||||||
| Very Low Birth Weight | ||||||||||
| Neighborhood Affluence index | .856*** | .462 | .884** | .235 | .856** | .381 | .808* | .022 | ||
| [.798, .917] | [.809, .966] | [.770, .952] | [.670, .974] | |||||||
| Neighborhood Disadvantage index | .973 | .000 | 1.078** | .324 | 1.159*** | .429 | .971 | .000 | ||
| [.880, 1.074] | [1.022, 1.137] | [1.071, 1.254] | [.751, 1.255] | |||||||
| Small for Gestational Age | ||||||||||
| Neighborhood Affluence index | .958** | .107 | .878*** | .300 | .953* | .188 | .914*** | .186 | ||
| [.934, .982] | [.841, .916] | [.918, .990] | [.871, .960] | |||||||
| Neighborhood Disadvantage index | 1.103*** | .179 | .976 [.951, 1.002] |
.100 | 1.069*** [1.037, 1.102] |
.250 | 1.066 [.996, 1.142] |
.163 | ||
| [1.065, 1.143] | ||||||||||
| Preterm Birth | ||||||||||
| Neighborhood Affluence index | .923*** | .065 | .980 | .100 | 1.011 | .043 | .885*** | .161 | ||
| [.899, .947] | [.938, 1.023] | [.973, 1.052] | [.833, .940] | |||||||
| Neighborhood Disadvantage index | .981 | .000 | 1.087*** | .300 | 1.120*** | .174 | 1.014 | .065 | ||
| [.943, 1.019] | [1.058, 1.117] | [1.084, 1.157] | [.930, 1.104] | |||||||
| Early Preterm Birth | ||||||||||
| Neighborhood Affluence index | .886*** | .074 | .934* | .130 | .919* | .250 | .863* | .047 | ||
| [.843, .932] | [.873, .999] | [.853, .990] | [.760, .980] | |||||||
| Neighborhood Disadvantage index | .987 | .000 | 1.092*** | .304 | 1.162*** | .375 | 1.015 | .000 | ||
| [.917, 1.062] | [1.049, 1.137] | [1.098, 1.231] | [.851, 1.210] | |||||||
| Late Preterm Birth | ||||||||||
| Neighborhood Affluence index | .931*** | .033 | 1.014 | .000 | 1.043 | .000 | .895*** [.837, .957] |
.139 | ||
| [.906, .957] | [.964, 1.067] | [.998, 1.089] | ||||||||
| Neighborhood Disadvantage index | .966 [.926, 1.008] |
.000 | 1.076*** [1.043, 1.110] |
.200 | 1.096*** [1.057, 1.137] |
.045 | 1.011 [.918, 1.112] |
.083 | ||
Note: ***p < .001, **p < .01, *p < .05 (two-tailed). All models include: maternal education at birth, employment in year prior to birth, insurance status, foreign-born status, marital status, age, if she named the father on the birth certificate, infant sex, parity, place of delivery, and birth year fixed effects.
Appendix E
See Appendix Table E1.
Table E1.
Percent (or mean) of each indicator comprising the neighborhood affluence and neighborhood disadvantage indices, by quartile.
| 1st Quartile | 2nd Quartile | 3rd Quartile | 4th Quartile | |
|---|---|---|---|---|
| Indicators of Neighborhood Disadvantage | ||||
| % of HHs with Incomes < $15 K | 4.57% | 9.07% | 14.45% | 28.76% |
| % of HHs with Incomes >= $50 K | 74.24% | 57.61% | 44.25% | 27.44% |
| % of Families in Poverty | 1.79% | 3.71% | 8.93% | 23.31% |
| % of HHs receiving Public Assistance | 0.99% | 1.78% | 3.62% | 10.67% |
| Total Unemployment Rate | 3.81% | 5.30% | 7.85% | 15.33% |
| % of Housing Units that are Vacant | 2.41% | 3.97% | 6.44% | 12.45% |
| Number of Level-2 Units | 1,044 | 1,044 | 1,044 | 1,043 |
| Indicators of Neighborhood Affluence | ||||
| % in Professional/Managerial Occupations (16+) | 14.26% | 22.26% | 31.70% | 45.82% |
| % with College Degree (25+) | 15.94% | 27.46% | 40.02% | 61.01% |
| Median Home Value | $117,954 | $159,394 | $195,380 | $324,103 |
| Number of Level-2 Units | 1,044 | 1,044 | 1,044 | 1,043 |
References
- Ahern J., Pickett K.E., Selvin S., Abrams B. Preterm birth among African American and white women: A multilevel analysis of socioeconomic characteristics and cigarette smoking. Journal of Epidemiology and Community Health. 2003;57(8):606–611. doi: 10.1136/jech.57.8.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexander G.R., Kogan M., Martin J., Papiernik E. What are the fetal growth patterns of singletons, twins, and triplets in the United States? Clinical Obstetrics and Gynecology. 1998;41(1):115–125. doi: 10.1097/00003081-199803000-00017. [DOI] [PubMed] [Google Scholar]
- Allison P.D. Multiple imputation for missing data: A cautionary tale. Sociological Methods Research. 2000;28(3):301–309. [Google Scholar]
- Baron R.M., Kenny D.A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Behrman R.E., Butler A.S. National Academy Press; 2007. Preterm Birth: Causes, Consequences, and Prevention. [PubMed] [Google Scholar]
- Bell J.F., Zimmerman F.J., Almgren G.R., Mayer J.D., Huebner C.E. Birth outcomes among urban African-American women: A multilevel analysis of the role of racial residential segregation. Social Science & Medicine. 2006 doi: 10.1016/j.socscimed.2006.08.011. [DOI] [PubMed] [Google Scholar]
- Blumenshine P., Egerter S., Barclay C.J., Cubbin C., Braveman P.A. Socioeconomic disparities in adverse birth outcomes: A systematic review. American Journal of Preventive Medicine. 2010;39(3):263–272. doi: 10.1016/j.amepre.2010.05.012. [DOI] [PubMed] [Google Scholar]
- Browning C.R., Cagney K.A. Moving beyond poverty: Neighborhood structure, social processes, and health. Journal of Health and Social Behavior. 2003:552–571. [PubMed] [Google Scholar]
- Browning C.R., Cagney K.A., Wen M. Explaining variation in health status across space and time: Implications for racial and ethnic disparities in self-rated health. Social Science & Medicine. 2003;57(7):1221–1235. doi: 10.1016/s0277-9536(02)00502-6. [DOI] [PubMed] [Google Scholar]
- Buka S.L., Brennan R.T., Rich-Edwards J.W., Raudenbush S.W., Earls F. Neighborhood support and the birth weight of urban infants. American Journal of Epidemiology. 2003;157(1):1. doi: 10.1093/aje/kwf170. [DOI] [PubMed] [Google Scholar]
- Cagney K.A., Browning C.R., Wen M. Racial disparities in self-rated health at older ages: What difference does the neighborhood make? The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2005;60(4):S181–S190. doi: 10.1093/geronb/60.4.s181. [DOI] [PubMed] [Google Scholar]
- Cnattingius S. The epidemiology of smoking during pregnancy: Smoking prevalence, maternal characteristics, and pregnancy outcomes. Nicotine Tobacco Research. 2004;6(Suppl. 2):S125–S140. doi: 10.1080/14622200410001669187. [DOI] [PubMed] [Google Scholar]
- Cubbin C., Marchi K., Lin M., Bell T., Marshall H., Miller C., Braveman P. Is neighborhood deprivation independently associated with maternal and infant health? Evidence from Florida and Washington. Maternal and Child Health Journal. 2008;12(1):61–74. doi: 10.1007/s10995-007-0225-0. [DOI] [PubMed] [Google Scholar]
- Culhane J.F., Elo I.T. Neighborhood context and reproductive health. American Journal of Obstetrics and Gynecology. 2005;192(5):S22–S29. doi: 10.1016/j.ajog.2005.01.071. [DOI] [PubMed] [Google Scholar]
- Curtin S.C., Mathews T.J. Smoking prevalence and cessation before and during pregnancy: data from the birth certificate, 2014. National Vital Statistics Reports. 2016;65(1):1–14. [PubMed] [Google Scholar]
- Debbink M.P., Bader M.D. Racial residential segregation and low birth weight in Michigan’s metropolitan areas. American Journal of Public Health. 2011;101(9):1714–1720. doi: 10.2105/AJPH.2011.300152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ennis, S.R., Ríos-Vargas, M., & Albert, N.G. (2011). The Hispanic Population: 2010. Washington, D.C.
- Finch B.K., Vega W.A., Kolody B. Substance use during pregnancy in the state of California, USA. Social Science & Medicine. 2001;52(4):571–583. doi: 10.1016/s0277-9536(00)00161-1. [DOI] [PubMed] [Google Scholar]
- Galster G. On the nature of neighbourhood. Urban studies. 2001;38(12):2111. [Google Scholar]
- Goldenberg R.L., Culhane J., Iams J.D., Romero R. Epidemiology and causes of preterm birth. The Lancet. 2008;371(9606):75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldenberg R.L., Culhane J.F. Low birth weight in the United States. The American Journal of Clinical Nutrition. 2007;85(2):584S–590S. doi: 10.1093/ajcn/85.2.584S. [DOI] [PubMed] [Google Scholar]
- Gorman B.K. Racial and ethnic variation in low birthweight in the United States: Individual and contextual determinants. Health Place. 1999;5(3):195–207. doi: 10.1016/s1353-8292(99)00009-x. [DOI] [PubMed] [Google Scholar]
- Grady S.C. Racial disparities in low birthweight and the contribution of residential segregation: A multilevel analysis. Social Science & Medicine. 2006;63(12):3013–3029. doi: 10.1016/j.socscimed.2006.08.017. [DOI] [PubMed] [Google Scholar]
- Halfon N., Hochstein M. Life course health development: An integrated framework for developing health, policy, and research. Milbank Quarterly. 2002;80(3):433–479. doi: 10.1111/1468-0009.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healthy People (2020). Foundational Health Measures: General Health Status. Retrieved from 〈http://www.healthypeople.gov/2020/about/GenHealthAbout.aspx〉.
- Hogan V.K., Rowley D., Bennett T., Taylor K.D. Life course, social determinants, and health inequities: Toward a national plan for achieving health equity for African American infants—a concept paper. Maternal and Child Health Journal. 2012;16(6):1143. doi: 10.1007/s10995-011-0847-0. [DOI] [PubMed] [Google Scholar]
- Hogue C.J., Hoffman S., Hatch M.C. Stress and preterm delivery: A conceptual framework. Paediatric and Perinatal Epidemiology. 2001;15(s2):30–40. doi: 10.1046/j.1365-3016.2001.00006.x. [DOI] [PubMed] [Google Scholar]
- Janevic T., Stein C.R., Savitz D.A., Kaufman J.S., Mason S.M., Herring A.H. Neighborhood deprivation and adverse birth outcomes among diverse ethnic groups. Annals of Epidemiology. 2010;20(6):445–451. doi: 10.1016/j.annepidem.2010.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I., Berkman L.F. Oxford University Press; New York: 2003. Neighborhoods and Health. [Google Scholar]
- King K.E., Morenoff J.D., House J.S. Neighborhood context and social disparities in cumulative biological risk factors. Psychosomatic Medicine. 2011;73(7):572. doi: 10.1097/PSY.0b013e318227b062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kornhauser R.R. University of Chicago Press; Chicago, IL: 1978. Social sources of delinquency: An appraisal of analytic models. [Google Scholar]
- Kramer M.R., Cooper H.L., Drews-Botsch C.D., Waller L.A., Hogue C.R. Metropolitan isolation segregation and Black–White disparities in very preterm birth: A test of mediating pathways and variance explained. Social Science & Medicine. 2010;71(12):2108–2116. doi: 10.1016/j.socscimed.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link B.G., Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995:80–94. [PubMed] [Google Scholar]
- Lu M.C., Kotelchuck M., Hogan V., Jones L., Wright K., Halfon N. Closing the black-white gap in birth outcomes: A life-course approach. Ethnicity Disease. 2010;20(1 0 2):S2. [PMC free article] [PubMed] [Google Scholar]
- Martin J.A., Kung H.C., Mathews T.J., Hoyert D.L., Strobino D.M., Guyer B., Sutton S.R. Annual summary of vital statistics: 2006. Pediatrics. 2008;121(4):788. doi: 10.1542/peds.2007-3753. [DOI] [PubMed] [Google Scholar]
- Masi C.M., Hawkley L.C., Piotrowski Z.H., Pickett K.E. Neighborhood economic disadvantage, violent crime, group density, and pregnancy outcomes in a diverse, urban population. Social Science & Medicine. 2007;65(12):2440–2457. doi: 10.1016/j.socscimed.2007.07.014. [DOI] [PubMed] [Google Scholar]
- Mathews T.J., MacDorman M.F., Thoma M.E. Infant mortality statistics from the 2013 period linked birth/infant death data set. National Vital Statistics Reports. 2015;64(9):1–30. [PubMed] [Google Scholar]
- Matthews S.A., Yang T.C. Exploring the role of the built and social neighborhood environment in moderating stress and health. Annals of Behavioral Medicine. 2010;39(2):170–183. doi: 10.1007/s12160-010-9175-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendez D.D., Hogan V.K., Culhane J.F. Institutional racism, neighborhood factors, stress, and preterm birth. Ethnicity health. 2014;19(5):479–499. doi: 10.1080/13557858.2013.846300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messer L.C., Kaufman J.S., Dole N., Savitz D.A., Laraia B.A. Neighborhood crime, deprivation, and preterm birth. Annals of Epidemiology. 2006;16(6):455–462. doi: 10.1016/j.annepidem.2005.08.006. [DOI] [PubMed] [Google Scholar]
- Messer L.C., Laraia B.A., Kaufman J.S., Eyster J., Holzman C., Culhane J.…O’campo P. The development of a standardized neighborhood deprivation index. Journal of Urban Health. 2006;83(6):1041–1062. doi: 10.1007/s11524-006-9094-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messer L.C., Vinikoor L.C., Laraia B.A., Kaufman J.S., Eyster J., Holzman C.…O’Campo P. Socioeconomic domains and associations with preterm birth. Social Science & Medicine. 2008;67(8):1247–1257. doi: 10.1016/j.socscimed.2008.06.009. [DOI] [PubMed] [Google Scholar]
- Misra D.P., Guyer B., Allston A. Integrated perinatal health framework: A multiple determinants model with a life span approach. American Journal of Preventive Medicine. 2003;25(1):65–75. doi: 10.1016/s0749-3797(03)00090-4. [DOI] [PubMed] [Google Scholar]
- Morenoff J.D. Neighborhood mechanisms and the spatial dynamics of birth weight. American Journal of Sociology. 2003;108(5):976–1017. doi: 10.1086/374405. [DOI] [PubMed] [Google Scholar]
- Morenoff, J.D., Hansen, B.B., House, J.S., Williams, D.R., Kaplan, G.A., & Hunte, H.E. (2007). Understanding Social Disparities in Hypertension Prevalence, Awareness, Treatment, and Control: The Role of Neighborhood Context. Retrieved from Ann Arbor, MI. [DOI] [PMC free article] [PubMed]
- Ncube C.N., Enquobahrie D.A., Albert S.M., Herrick A.L., Burke J.G. Association of neighborhood context with offspring risk of preterm birth and low birthweight: A systematic review and meta-analysis of population-based studies. Social Science & Medicine. 2016;153:156–164. doi: 10.1016/j.socscimed.2016.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nkansah-Amankra S. Neighborhood contextual factors, maternal smoking, and birth outcomes: Multilevel analysis of the South Carolina PRAMS survey, 2000–2003. Journal of Women’ States Health. 2010;19(8):1543–1552. doi: 10.1089/jwh.2009.1888. [DOI] [PubMed] [Google Scholar]
- Nkansah-Amankra S., Luchok K.J., Hussey J.R., Watkins K., Liu X. Effects of maternal stress on low birth weight and preterm birth outcomes across neighborhoods of South Carolina, 2000–2003. Maternal and Child Health Journal. 2010;14(2):215–226. doi: 10.1007/s10995-009-0447-4. [DOI] [PubMed] [Google Scholar]
- O’Campo P., Burke J.G., Culhane J., Elo I.T., Eyster J., Holzman C.…Laraia B.A. Neighborhood deprivation and preterm birth among non-Hispanic Black and White women in eight geographic areas in the United States. American Journal of Epidemiology. 2008;167(2):155–163. doi: 10.1093/aje/kwm277. [DOI] [PubMed] [Google Scholar]
- O’Campo P., O’Brien Caughy M., Oakes J., Kaufman J. Jossey Bass; San Francisco (CA): 2006. Measures of Residential Community Contexts Methods in Social Epidemiology; pp. 193–208. [Google Scholar]
- Oakes J.M. The (mis) estimation of neighborhood effects: Causal inference for a practicable social epidemiology. Social Science & Medicine. 2004;58(10):1929–1952. doi: 10.1016/j.socscimed.2003.08.004. [DOI] [PubMed] [Google Scholar]
- Oken E., Kleinman K.P., Rich-Edwards J., Gillman M.W. A nearly continuous measure of birth weight for gestational age using a United States national reference. BMC Pediatrics. 2003;3(1):6. doi: 10.1186/1471-2431-3-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearl M., Braveman P., Abrams B. The relationship of neighborhood socioeconomic characteristics to birthweight among 5 ethnic groups in California. American Journal of Public Health. 2001;91(11):1808–1814. doi: 10.2105/ajph.91.11.1808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center (2013). The Rise of Asian Americans. Retrieved from Washington, D.C.
- Pickett K.E., Ahern J.E., Selvin S., Abrams B. Neighborhood socioeconomic status, maternal race and preterm delivery: A case-control study. Annals of Epidemiology. 2002;12(6):410–418. doi: 10.1016/s1047-2797(01)00249-6. [DOI] [PubMed] [Google Scholar]
- Räisänen S., Kramer M.R., Gissler M., Saari J., Hakulinen-Viitanen T., Heinonen S. Smoking during pregnancy was up to 70% more common in the most deprived municipalities—A multilevel analysis of all singleton births during 2005–2010 in Finland. Preventive Medicine. 2014;67:6–11. doi: 10.1016/j.ypmed.2014.06.026. [DOI] [PubMed] [Google Scholar]
- Raudenbush S.W., Bryk A.S. 2nd ed. Vol. 1. Sage Publications; Thousand Oaks, CA: 2001. Hierarchical Linear Models: Applications and Data Analysis Methods. [Google Scholar]
- Reichman, N.E., Corman, H., Noonan, K., & Dave, D. (2006). Typically Unobserved Variables (TUVs) and Selection into Prenatal Inputs: Implications for Estimating Infant Health Production Functions. Retrieved from.
- Robert S.A. Community-level socioeconomic status effects on adult health. Journal of Health and Social Behavior. 1998:18–37. [PubMed] [Google Scholar]
- Roberts E.M. Neighborhood social environments and the distribution of low birthweight in Chicago. American Journal of Public Health. 1997;87(4):597. doi: 10.2105/ajph.87.4.597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers J.M. Tobacco and pregnancy. Reproductive Toxicology. 2009;28(2):152–160. doi: 10.1016/j.reprotox.2009.03.012. [DOI] [PubMed] [Google Scholar]
- Roux A.V.D. Estimating neighborhood health effects: The challenges of causal inference in a complex world. Social Science & Medicine. 2004;58(10):1953–1960. doi: 10.1016/S0277-9536(03)00414-3. [DOI] [PubMed] [Google Scholar]
- Sampson R.J. Oxford University Press; Nueva York: 2003. Neighborhood-Level Context and Health: Lessons from Sociology. [Google Scholar]
- Sampson R.J., Morenoff J.D., Gannon-Rowley T. Assessing” neighborhood effects”: Social processes and new directions in research. Annual Review of Sociology. 2002:443–478. [Google Scholar]
- Schempf A., Strobino D., O’Campo P. Neighborhood effects on birthweight: An exploration of psychosocial and behavioral pathways in Baltimore, 1995–1996. Social Science & Medicine. 2009;68(1):100–110. doi: 10.1016/j.socscimed.2008.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw, C.R., & McKay, H.D. (1942). Juvenile Delinquency and Urban Areas. Chicago, Ill.
- Solari C.D. Affluent neighborhood persistence and change in US cities. City Community. 2012;11(4):370–388. doi: 10.1111/j.1540-6040.2012.01422.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subramanian S.V., Chen J.T., Rehkopf D.H., Waterman P.D., Krieger N. Comparing individual-and area-based socioeconomic measures for the surveillance of health disparities: A multilevel analysis of Massachusetts births, 1989–1991. American Journal of Epidemiology. 2006;164(9):823. doi: 10.1093/aje/kwj313. [DOI] [PubMed] [Google Scholar]
- University of Wisconsin Population Health Institute (2010). County Health Rankings: 2010. Retrieved from 〈http://www.countyhealthrankings.org/sites/default/files/states/CHR2010_NJ_0.pdf〉.
- VanderWeele T. Mediation analysis: A practitioner’s guide. Annual Review of Public Health. 2016;37:17–32. doi: 10.1146/annurev-publhealth-032315-021402. [DOI] [PubMed] [Google Scholar]
- VanderWeele T.J. Mediation analysis: A practitioner’s guide. Annual Review of Public Health. 2016;37:17–32. doi: 10.1146/annurev-publhealth-032315-021402. [DOI] [PubMed] [Google Scholar]
- Walton E. Residential segregation and birth weight among racial and ethnic minorities in the United States. Journal of Health and Social Behavior. 2009;50(4):427–442. doi: 10.1177/002214650905000404. [DOI] [PubMed] [Google Scholar]
- Wehby G.L., Fletcher J.M., Lehrer S.F., Moreno L.M., Murray J.C., Wilcox A., Lie R.T. A Genetic Instrumental Variables Analysis of the Effects of Prenatal Smoking on Birth Weight: Evidence from Two Samples. Biodemography and Social Biology. 2011;57(1):3–32. doi: 10.1080/19485565.2011.564468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen M., Browning C.R., Cagney K.A. Poverty, affluence, and income inequality: Neighborhood economic structure and its implications for health. Social Science & Medicine. 2003;57(5):843–860. doi: 10.1016/s0277-9536(02)00457-4. [DOI] [PubMed] [Google Scholar]
- Windham G.C., Hopkins B., Fenster L., Swan S.H. Prenatal active or passive tobacco smoke exposure and the risk of preterm delivery or low birth weight. Epidemiology. 2000;11(4):427–433. doi: 10.1097/00001648-200007000-00011. [DOI] [PubMed] [Google Scholar]