Abstract
Many large provider networks are investing heavily in preventing disease within the communities that they serve. We explore the potential benefits and challenges associated with tackling depression at the community level using a unique dataset designed for one such provider network. The economic costs of having depression (increased medical care use, lower quality of life, and decreased workplace productivity) are among the highest of any disease. Depression often goes undiagnosed, yet many believe that depression can be treated or prevented altogether. We explore the prevalence, distribution, economic burden, and the psychosocial and economic factors associated with undiagnosed depression in a lower-income neighborhood in northern Manhattan. Even using state-of-the art data to “diagnose” the risk factors within a community, it can be challenging for provider networks to act against such risk factors.
Highlights
-
•
Risk factors for undiagnosed depression include psychological stress, drug use, and co-morbid medical conditions.
-
•
Based on QALYs lost, the per-resident burden of having undiagnosed depression is $9950 of lost QALYs per resident.
-
•
Less advantaged residents bear an even greater economic burden of having undiagnosed depression.
-
•
There are both benefits and challenges associated with tackling depression at the community level.
Introduction
Depression is a leading cause of disability globally, costing $233 billion in the U.S. alone (in 2016 dollars) (Bremner et al., 2003). Moreover, it is estimated that in the U.S., around two-thirds of all cases of depression are undiagnosed (Wamala et al., 1999). Left undiagnosed and thus untreated, depression can worsen and significantly diminish quality of life and workplace productivity.
As such, there is a large push in the U.S. both nationally and locally, to identify and treat depression and other mental illnesses. For example, federal and state governments have provided billions of dollars in support of programs aimed at effective treatment of illness, including mental illness (Sparer, Muennig, & Brown, 2016). At the federal level, the Centers for Medicare and Medicaid Services have put in place penalties a for providers whose patients are readmitted to the hospital within 30 days of discharge (Sparer et al., 2016). Higher rates of 30-day all-cause readmission occur among individuals with a mental health condition when compared to individuals without a mental health condition (Sparer et al., 2016, Freedland et al., 2016, Ahmedani et al., 2015, Lyons et al., 1997). At the state level, programs such as the Delivery System Reform Incentive Payment (DSRIP) Program, provide funds to providers who propose innovative ways to identify and treat illnesses before they become more serious. Finally, some provider networks, hospitals, and the City of New York are launching initiatives that aim to reduce the prevalence of undiagnosed depression in the communities that they serve via depression screening and treatment in the medical setting (New York City).
Another mechanism through which health professionals work to reduce societal costs associated with depression and mental illness is via social interventions that might serve as primary prevention modalities to reduce the onset of depression (Sparer et al., 2016). Psychosocial stressors such as emotional abuse, physical abuse, exposure to crime, poor housing conditions, lacking health insurance, and financial stress have been identified as important risk factors for depression (Beattie, 2005, Harris and Brown, 1996). Interventions that effectively address the underlying psychosocial risk factors of depression can therefore also work to improve quality of life and workplace productivity, reducing the overall costs of depression to society (Sparer et al., 2016).
In the current study, we examine the prevalence, distribution, psychosocial risk factors, and costs of undiagnosed depression in a low-income neighborhood in northern Manhattan with the aim of identifying potential points of intervention. Having information on what specific risk factors exist in the social environment and how they impact health is instrumental to effectively planning and implementing public health interventions. Further, we are able to put a value on the societal costs of undiagnosed depression using the EQ-5D, a comprehensive measure of morbidity (Rabin and de Charro, 2001).
Methods
The 2015 Washington Heights Community Survey is a telephone survey administered in both English and Spanish to 2489 sample households in Washington Heights from March to September 2015. Eligible participants had to be 18 years or older and a resident of zip codes 10032 and 10033. The questionnaire included questions on neighborhood social and economic conditions, health care access, general health and health conditions. The survey had an American Association for Public Opinion Research (AAPOR) Response Rate of 16.8%. Prior to analyses using publicly available de-identified data from the survey, sample weights were developed to account for differential probabilities of selection among households. The weights were further calibrated using the distribution of adult demographic characteristics for Washington Heights found in the American Community Survey (ACS) in 2009–2013.
Measures of interest
To measure our outcome of interest, undiagnosed depression, we utilized respondent report of ever diagnosed with depression by a health provider (diagnosed depression) and PHQ-9 depression as determined by the Patient Health Questionnaire-9 (PHQ-9). The survey item determining diagnosed depression asked “Have you ever been told by a health professional that you have a depressive disorder, including depression, major depression, dysthymia, or minor depression?” The PHQ-9 is a population-level screening instrument for depression with a sensitivity of 88% and specificity of 88% (Kroenke and Spitzer, 2002). A PHQ-9 score ≥10, (Kroenke and Spitzer, 2002) one cut-off for clinical depression, was utilized in this study. Respondents with PHQ-9 assessed depression who reported never been diagnosed with depression by a health provider, were considered to have undiagnosed depression.
The correlates of primary interest measured respondent psychosocial and general health status. These included psychological stress, quality of care (receipt of flu vaccination in past year), presence of diagnosed health conditions (asthma, heart condition, hypocholesteremia, hypertension, and diabetes), whether respondent is obese, and exposure to health risks including smoking status, current alcohol use, and drug use (any lifetime use of heroin, crack, cocaine, and methamphetamines). Psychological stress was measured as the count of stressful life events in the past year including serious illness, being a victim of a crime, unemployment, serious financial problems, death of close friends or family, and relationship problems.
Other correlates of interest included socioeconomic factors such as employment status (not employed, employed, or not in labor force), receipt of food assistance, and health care access measured as health insurance coverage type (none, public coverage from Medicare or Medicaid, or private coverage via employer, school, family member or self-pay). Additional individual and community social measures included self-rated health status (indicator for fair or poor versus good to excellent health), having high acculturation (measured as acculturation score above three), number of years lived in Washington Heights, nativity, and neighborhood collective efficacy. Acculturation scores represent the average of responses to a battery of four survey items on language preference for reading, thinking, and speaking with friends and household members with values ranging from one to five. Collective efficacy refers to the notion that community members believe in ability of their community to allocate, coordinate, and integrate resources (Zaccaro et al., 1995, Bandura, 1996). Health utilization measures such as having a usual source of medical care, emergency department (ED) utilization (no, one, or more than one ED visit in past year), and whether respondent had delayed medical care due to cost concerns were also considered in these analyses.
Finally, to assess the disease burden the community bears due to undiagnosed depression, we quantified the health related quality of life (HRQoL) attributable to undiagnosed depression in Washington Heights using the EQ-5D index score. The EQ-5D is a measure based on societal preferences for health states, such as mental and physical well-being (Rabin and de Charro, 2001). The EQ-5D uses exercises grounded in economic theory to link questions about mobility, anxiety and depression, self-care, pain and discomfort, and usual activities to a nationally-weighted representative sample to generate a score with values from 0 to 1 with higher values indicating better quality of life (Muennig and Bounthavong, 2016). For instance, a score of 0.85 on the anxiety and depression scale means that people would be willing to live a life that is 15% shorter (85% of their expected survival) in exchange for not feeling anxious or depressed. Because one represents perfect health and zero represents death, an HRQoL score of 0.85 over one year represents 0.85 years of “perfect” health. The power of this instrument is that it provides a grounded way of putting a dollar value on changes in health. The Environmental Protection Agency, for example, values a quality-adjusted life year (QALY) at $100,000 (a QALY is a year of perfect health) (Muennig and Bounthavong, 2016). In the example given above, if health providers or interventions could rid that person of their anxiety and depression, we would gain 0.15•$100,000 or $15,000.
Statistical analysis
First, we present a descriptive summary of depression and undiagnosed depression in Washington Heights. This is presented in graphic form and contextualized, where relevant, to provide a sense of the geographic distribution of depression and undiagnosed depression as well as associated socioeconomic characteristics in the community.
Multiple regression models were used to identify statistically significant correlates of undiagnosed depression. Of particular interest was how psychosocial and general health measures along with socioeconomic factors, acculturation and nativity, neighborhood collective efficacy, health care access and utilization, quality of care, and health risks were associated with depression after controlling for demographic characteristics (gender, race/ethnicity, and age). Further, to elucidate the societal costs of undiagnosed depression, we specified via regression modelling, the quality-adjusted life years (QALYs) lost to undiagnosed depression and important correlates identified from multiple regression analysis.
Survey weights were utilized in all statistical analyses to account for unequal probability of selection and possible non-response bias in the data and to ensure that the sample was representative of the population; a p-value < 0.05 was considered statistically significant. All analyses were conducted using SAS 9.4 and ArcMap 10.3.1.
Results
Table 1 provides the unweighted frequencies alongside weighted relative frequency distribution for all measures of interest. Estimates show that the sample was equally male and female with 66% Hispanic, 17% non-Hispanic white, and 11% non-Hispanic Black or African-American. The proportion of Hispanics in this neighborhood is higher than that of Manhattan (25.7%) and New York City (28.2%) (American Community Survey 5-Year Estimates, 2010-2014) in 2015. Most respondents had health insurance coverage (91.3%) and a usual source of medical care (86.7%) but nearly a quarter (21.6%) reported delaying medical care due to cost and over 30% report being in fair or poor health.
Table 1.
Distribution of socioeconomic factors, other demographic characteristics, health utilization measures, general health measures, and exposure to health risks overall and stratified by presence of undiagnosed depression status, Washington Heights Community Survey, New York, 2015.
| Measure | Total | Has undiagnosed depression |
|---|---|---|
| n (weighted %) | n (weighted %) | |
| Undiagnosed depression | 180 (7.6) | -- |
| Diagnosed depression | 273 (8.0) | -- |
| PHQ-9 depression | 313 (11.6) | -- |
| Socioeconomic factors | ||
| Employment status | ||
| Employed at work | 1001 (45.6) | 54 (6.2) |
| Employed, not at work | 26 (1.0) | 3 (10.8) |
| Not in labor force | 1128 (36.0) | 84 (7.1) |
| Unemployed | 298 (17.4) | 36 (11.3) |
| Receipt of food assistance | ||
| No | 1568 (65.3) | 96 (7.4) |
| Yes | 918 (34.7) | 83 (7.7) |
| Other demographic factors | ||
| Age (mean +/- SE) | 43.26 +/- 0.53 | 43.22 +/- 0.55 |
| Gender | ||
| Male | 742 (49.9) | 57 (7.9) |
| Female | 1704 (50.1) | 122 (7.4) |
| Race/ethnicity | ||
| Hispanic | 1476 (66.1) | 116 (7.5) |
| White or other non-Hispanic | 691 (22.7) | 45 (8.8) |
| Black non-Hispanic | 293 (11.2) | 17 (5.5) |
| Health insurance coverage | ||
| None | 129 (8.7) | 12 (5.0) |
| Private | 935 (37.1) | 58 (7.7) |
| Public | 1357 (51.4) | 105 (7.6) |
| Other | 53 (2.9) | 5 (14.8) |
| Acculturation score | ||
| ≤3 | 1203 (56.1) | 99 (7.2) |
| >3 | 1263 (43.9) | 81 (8.0) |
| Nativity | ||
| Native-born | 1158 (45.5) | 73 (6.5) |
| Foreign-born | 1330 (54.5) | 107 (8.4) |
| Neighborhood collective efficacy(mean +/- SE) | 3.50 +/- 0.02 | 3.51 +/- 0.02 |
| Health utilization measures | ||
| Whether respondent had a usual source of medical care | ||
| No | 265 (13.3) | 23 (8.3) |
| Yes | 2213 (86.7) | 155 (7.4) |
| Number of times respondent went to ER in past 12 months | ||
| None | 1865 (75.4) | 103 (6.5) |
| Once | 335 (14.3) | 34 (8.6) |
| More than once | 278 (10.4) | 42 (13.7) |
| Whether respondent had delayed medical care due to cost concerns | ||
| No | 1979 (78.4) | 115 (6.5) |
| Yes | 510 (21.6) | 65 (11.3) |
| General health measures | ||
| Global self-rated health | ||
| At least good health | 1584 (68.0) | 77 (6.2) |
| Fair/poor health | 904 (31.9) | 103 (10.3) |
| Has diagnosed asthma | ||
| No | 2034 (83.4) | 133 (6.5) |
| Yes | 454 (16.6) | 47 (12.7) |
| Has a diagnosed heart condition | ||
| No | 2323 (96.2) | 161 (7.4) |
| Yes | 166 (3.8) | 19 (11.1) |
| Has diagnosed high cholesterol | ||
| No | 1565 (69.5) | 102 (6.4) |
| Yes | 912 (30.5) | 77 (10.0) |
| Has diagnosed diabetes | ||
| No | 2048 (87.0) | 139 (7.4) |
| Yes | 441 (13.0) | 41 (8.7) |
| Has diagnosed hypertension | ||
| No | 1449 (68.1) | 97 (7.3) |
| Yes | 1035 (31.9) | 83 (8.1) |
| Received flu vaccine in past year | ||
| No | 1075 (47.6) | 72 (7.1) |
| Yes | 1407 (52.4) | 108 (8.0) |
| Whether respondent is obese | ||
| No | 1745 (74.2) | 115 (7.6) |
| Yes | 682 (25.8) | 59 (7.2) |
| Exposure to health risks | ||
| Smoking status | ||
| Non-smoker | 2229 (89.8) | 151 (7.1) |
| Smoker | 252 (10.2) | 28 (11.2) |
| Current alcohol use | ||
| No | 1160 (41.3) | 92 (8.7) |
| Yes | 1317 (58.7) | 73 (5.1) |
| Drug use (any lifetime use of heroin, crack, cocaine, and methamphetamines) | ||
| No | 1980 (84.3) | 128 (6.6) |
| Yes | 427 (15.7) | 42 (12.2) |
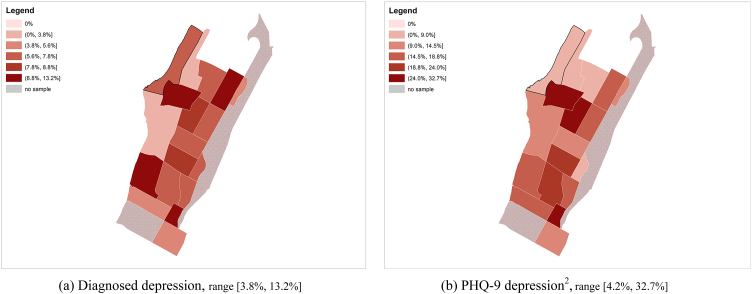
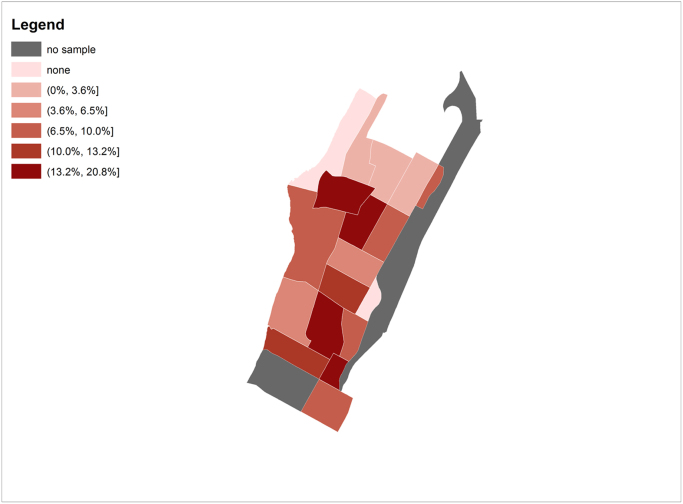
Estimated prevalence of undiagnosed depression in Washington Heights is 7.6% with 11.6% of residents having PHQ-9 depression and 8.0% with diagnosed depression. Table 1 further provides the distribution of undiagnosed depression in socio-demographic sub-groups we see, for example, among residents who are employed and at work, about 6% have undiagnosed depression while among those who are unemployed, the prevalence of undiagnosed depression is 11.3%. Fig. 1 maps the geographic distribution of depression at the census tract level in Washington Heights, New York. Panel (a) shows the prevalence of diagnosed depression, and panel (b) maps the prevalence of those with PHQ-9 depression. We see that many communities with a high prevalence of diagnosed depression actually have a low prevalence of depression detected by the PHQ-9. For one, the upper left-hand census tract (in the extreme northwest of neighborhood) is among a subset of communities with higher rates of diagnosed depression and relatively low rates of depression as identified by the PHQ-9. Fig. 2 maps the census tract-level prevalence of undiagnosed depression in Washington Heights, New York.
Fig. 1.
Two views of depression at the census tract level in Washington Heights, New York (Bremner et al., 2003). Panel (a) shows levels of clinically diagnosed depression. Panel (b) shows the prevalence of depression diagnosed as having a score ≥ 10 on the nine-item Patient Health Questionnaire (PHQ-9). In many census tracts with high levels of clinically diagnosed depression, the actual prevalence of depression, as measured by PHQ-9, is low. Tracts with greater prevalence of clinically diagnosed depression also have highest mean levels of educational attainment, income, and access to health care in this neighborhood. 1. Color intensity in map increases with prevalence; greyed out tracts indicate tracts with no data. 2. PHQ-9 depression prevalence has been adjusted to account for the instrument sensitivity.
Fig. 2.
Distribution of undiagnosed depression at the census tract level in Washington Heights, New York. 1. Color intensity in map increases with prevalence; greyed out tracts indicate tracts with no data. 2. PHQ-9 depression prevalence has been adjusted to account for the instrument sensitivity.
Results from multiple logistic regression model for having diagnosed depression showed that after controlling for demographic characteristics, factors associated significantly with type of health care access such as having private health insurance versus none, OR = 2.12, 95% CI [1.13, 3.95], and having a medical home, OR = 2.35, 95% CI [1.15, 4.78], were associated with increased odds of having diagnosed depression. The odds of having diagnosed depression did not differ significantly between residents with public insurance and those with no insurance, suggesting that, in this neighborhood, the type of health insurance one possesses might be as important as the presence of health insurance as a driver of depression diagnosis. Other factors associated with having diagnosed depression included being on a food assistance program, OR = 2.81, 95% CI [1.55, 5.08], and psychological stress, OR = 1.39, 95% CI [1.22, 1.59].
Factors such as being unemployed, OR = 2.27, 95% CI [1.33, 4.69], and delaying medical care, OR = 2.25, 95% CI [1.45, 3.47], were found to be associated with increased odds of having PHQ-9-diagnosed depression from adjusted logistic regression analysis. Other factors associated with PHQ-9 depression include having high cholesterol, OR = 1.78, 95% CI [1.18, 2.69], drug use, OR = 3.05, 95% CI [1.73, 5.37], and psychological stress, OR = 1.40, 95% CI [1.22, 1.60]. Health insurance access and having a usual source of medical care were not significantly associated with having PHQ-9 depression.
Correlates found to be associated with undiagnosed depression in adjusted analysis are shown in Table 2. Increased psychological stress, measured as the count of past year stressful life events, was associated with a 30% increased odds of having undiagnosed depression, OR = 1.29, 95% CI [1.10, 1.51]. Further, any lifetime drug use doubled the odds of having undiagnosed depression, OR = 2.17, 95% CI [1.13, 4.18], and having asthma was associated with a 75% increased odds of having undiagnosed depression OR = 1.75, 95% CI [1.01, 3.04]. Every unit increase in neighborhood collective efficacy was associated with 40%-decreased odds of having undiagnosed depression.
Table 2.
Independent correlates of undiagnosed depressiona, n = 2229, Washington Heights, New York, 2015.
| Covariates | Adjusted OR | 95% CI | df | p-value |
|---|---|---|---|---|
| Psychological stress count | 1.29 | (1.10, 1.51) | 1 | 0.002 |
| Collective efficacy score | 0.63 | (0.43, 0.94) | 1 | 0.022 |
| Any lifetime drug use | 2.17 | (1.13, 4.18) | 1 | 0.020 |
| Has diagnosed asthma | 1.75 | (1.01, 3.04) | 1 | 0.046 |
| Likelihood Ratio Test for Global Null Hypothesis | 8 | < 0.0001 | ||
Model adjusts for gender, age, and race/ethnicity.
Economic burden of undiagnosed depression
Based on QALYs lost, the per-resident burden of disease attributable to undiagnosed depression in Washington Heights was estimated to be $9950 of lost QALYs per resident when compared to residents without undiagnosed depression (see Table 3). Moreover, we can see that even greater economic burden of having undiagnosed depression is borne by less advantaged residents. Each unit increase in the count of psychological stress is associated with an increased burden of disease of $2750 per resident on average. A resident with no lifetime drug use, experiences increased QALY compared to a resident with any lifetime drug use worth an average of $2,550. Having asthma was associated with increased burden of disease valued at $3500, on average. Furthermore, each unit decrease in collective efficacy score is associated with an increased burden of disease, worth an average of $1470 per resident.
Table 3.
The health-related costs of undiagnosed depression, Washington Heights, New York, 2015.
| Factors | Estimated change in HRQoL Index | Per resident monetary cost/burdena |
|---|---|---|
| Having no undiagnosed depression associated with estimated baseline HRQoL of 0.9542 | ||
| Undiagnosed depression | -0.0995 | $9950 |
| Psychological stress count | -0.0275 | $2750 |
| Collective efficacy score | +0.0147 | ($1470) |
| Any lifetime drug use | -0.0255 | $2550 |
| Has diagnosed asthma | -0.0350 | $3500 |
The value of an HRQoL score of 1.0 is $100,000.
Discussion
We found that having diagnosed depression is related to health access and utilization, whereas PHQ-9-diagnosed depression or undiagnosed depression is related to psychosocial factors. A likely explanation for the strong association between having health insurance and diagnosed depression is that those who have access to medical care are more likely to be diagnosed with depression. Likewise, having a medical home is associated with a diagnosis of depression, likely because care is coordinated and providers are more likely to screen and treat depression. Disconcertingly, those who were insured with Medicaid had similar odds of diagnosed depression as uninsured residents. This is possibly a reflection of Medicaid quality in this particular geographic area, as the Oregon Health Insurance Experiment did show increased diagnosis and treatment of clinical depression (Baicker et al., 2013).
There is evidence that depression is more likely to be overlooked, and thus undiagnosed, when clinicians are preoccupied with treating a comorbid somatic disorder rather than focusing on the patient as a whole (Smith et al., 1990). Universal screening with the PHQ-2 is one intervention that medical provider networks could implement to lower undiagnosed depression and lessen the related personal and societal costs. Targeted screening and treatment for those with Medicaid and those without health insurance in this neighborhood is needed. However, it is likely not the only geographic region in need of attention. For instance, this area is served by a large academic medical center that has invested heavily in collaborative care. Collaborative care models that integrate primary and specialty mental health care have been shown to both facilitate the detection of depressive symptoms and the proper treatment and management of the disease (Sorlie and Rogot, 1990; Muennig, Quan, Chiuzan, & Glied, 2015) However, there is little evidence that this has worked among Medicaid patients in this community.
Collaborative care, though, is unlikely to be the only answer to this problem. To effectively combat health threats that arise from conditions within a community, many researchers feel that it is necessary to target the underlying social risk factors before they have a chance to manifest as a disease, such as depression. In Washington Heights, significant correlates for undiagnosed depression include psychological stress, low collective efficacy, drug use, and co-morbid medical conditions. These potential risk factors also come at a very high social cost (even using the conservative $100,000/QALY threshold and excluding costs associated with premature mortality) (Muennig and Bounthavong, 2016). Were society to spend $1500 per resident on improving collective efficacy, the intervention would break even after one year were it able to improve our collective efficacy measure by one point. It is important to realize that this figure represents “societal costs” only—pain, suffering, and lost productivity; it does not include medical billing costs. We were unable to include medical billing cost data because the appropriate data could not be linked to the community survey at the time that it was designed.
Nevertheless, some of these psychosocial measures highlight the difficulties that provider networks face as they attempt to improve the health of their patient population. How, exactly, does a medical provider improve collective efficacy? How does a medical provider reduce stressful life events within a community? For social policymakers, these questions are thorny, but more represent more familiar terrain. Many psychosocial characteristics are related to poor socioeconomic status, so it could be that more traditional anti-poverty programs could help mitigate the social costs of undiagnosed depression. For example, the Earned Income Tax Credit has been shown to show positive effects on mental health (Rehkopf et al., 2014). The Oregon Health Insurance Experiment showed that Medicaid reduced the incidence of depression, possibly partially through reducing financial stressors (Baicker et al., 2013).
Even when moving up the policy chain, problems such as collective efficacy are difficult to tackle. Collective efficacy refers to the notion that community members believe in the ability of the collective to competently allocate, coordinate, and integrate resources – this serves to empower a community and can reflect the social status of a community (Markowe et al., 1985). The means for improving collective efficacy within a community are not clear, but might include interventions outside of the reach of most large medical providers. For instance, improved policing can reduce crime and community disorder in some contexts, (Bremner et al., 1999) and could itself be a stressor by inflaming situations that might otherwise end peacefully in one locality versus another (Bremner, 2001). Even if they were to meddle in higher-level social policies, is unlikely that most providers would wish to wade into such contentious interventions. Other potential interventions, such as working with the built environment, also seem out of scope for providers.
This does not mean that there is no way forward. It may be that psychological stressors and collective efficacy are intertwined, since stress might damage interpersonal relationships and community bonding (Bremner et al., 1997). As such, it could be important to refer patients to community resources such as vocational assistance and housing subsidies as part of targeted case management for depressed patients (Sparer et al., 2016). With respect to psychological stress, more targeted wellness program (e.g., meditation) might be effective at addressing undiagnosed depression, both directly, (Sephton et al., 2007) and through reduction of psychological stress (Speca, Carlson, Goodey, & Angen, 2000).
Interestingly, diagnosed asthma is associated with undiagnosed depression, suggesting that steroid use or the stress induced by having this chronic disease could be risk factors for depression. If it is the former, then community-based asthma prevention programs could be effective at reducing undiagnosed depression. However, we found no association between the presence of mice or cockroaches in the home and depression in this cross-sectional study.
It is also plausible that psychological stressors and the prevalence of co-morbid illnesses such as asthma are also intertwined. For example, childhood exposure to abuse has been shown to promote biological susceptibility to traffic-related air pollution and thus onset of asthma at an early age (Bremner et al., 1995). As chronic medical illnesses are a risk factor for depression, programs that target patients with chronic disorders could help impede the onset of depression itself. However, if this is the case, then it may be that simply providing quality care is the best intervention possible.
Limitations
When interpreting the results of this research, it is important to note that the study response rate is only 16.8%. To address bias concerns due to non-response, weighting adjustments for non-response using raking method were implemented in these analyses. Further, the target population for this study is unique in that Washington Heights is a low-income neighborhood with higher than proportions of racial-ethnic minorities and foreign-born residents than Manhattan and New York City. While this is an important population to assess, the study results may not be fully generalizable to the patient population of other provider networks. Also note that as with all self-reported data, responses to the survey are subject to response bias; this may be particularly true for questions regarding mental health. However, some effort was made to avoid this during data collection, as respondents were able to respond to mental health questions via an interactive voice response mechanism versus directly through the interviewer. Finally, while innovative with respect to content, the survey was cross-sectional in design. Our return-on-investment estimates are based on simple correlations and should be considered exploratory.
Conclusion
Even using state-of-the art data to “diagnose” the risk factors within a community, it can be challenging for provider networks to act against such risk factors.
Ethical Statement
Funding for Sharifa Z. Williams, Grace S. Chung, and Peter M. Muennig was provided by the Dean’s Office, Columbia University Mailman School of Public Health. The study sponsor had no role in study design; collection, analysis, and interpretation of data; writing the report; and the decision to submit the report for publication.
Sharifa Z. Williams, Grace S. Chung, and Peter M. Muennig have no financial disclosures.
This manuscript has been submitted solely to Social Science and Medicine – Population Health. It has not been previously published, either in whole or in part, nor have the findings been posted online. We confirm full access to all aspects of the research and writing process and take final responsibility for the paper.
Contributor Information
Sharifa Z. Williams, Email: szw2101@cumc.columbia.edu.
Grace S. Chung, Email: sc4125@cumc.columbia.edu.
Peter A. Muennig, Email: pm124@columbia.edu.
References
- Ahmedani B.K., Solberg L.I., Copeland L.A. Psychiatric comorbidity and 30-day readmissions after hospitalization for heart failure, AMI, and pneumonia. Psychiatric Services. 2015;66(2):134–140. doi: 10.1176/appi.ps.201300518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American community survey 5-year estimates. 2010-2014.
- Baicker K., Taubman S.L., Allen H.L. The oregon experiment — Effects of medicaid on clinical outcomes. New England Journal of Medicine. 2013;368(18):1713–1722. doi: 10.1056/NEJMsa1212321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Prentice-Hall; Englewood Cliffs, NJ: 1996. Social foundations of thought and action: A social cognitive theory. [Google Scholar]
- Beattie G. (2005). Social causes of depression. Retrieved April;6:2006.
- Bremner J.D. Hypotheses and controversies related to effects of stress on the hippocampus: An argument for stress-induced damage to the hippocampus in patients with posttraumatic stress disorder. Hippocampus. 2001;11(2):75–81. doi: 10.1002/hipo.1023. (discussion 82-74) [DOI] [PubMed] [Google Scholar]
- Bremner J.D., Licinio J., Darnell A. Elevated CSF corticotropin-releasing factor concentrations in posttraumatic stress disorder. The American Journal of Psychiatry. 1997;154(5):624–629. doi: 10.1176/ajp.154.5.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bremner J.D., Narayan M., Staib L.H., Southwick S.M., McGlashan T., Charney D.S. Neural correlates of memories of childhood sexual abuse in women with and without posttraumatic stress disorder. The American journal of psychiatry. 1999;156(11):1787–1795. doi: 10.1176/ajp.156.11.1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bremner J.D., Randall P., Scott T.M. MRI-based measurement of hippocampal volume in patients with combat-related posttraumatic stress disorder. The American journal of psychiatry. 1995;152(7):973–981. doi: 10.1176/ajp.152.7.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bremner J.D., Vythilingam M., Vermetten E. MRI and PET study of deficits in hippocampal structure and function in women with childhood sexual abuse and posttraumatic stress disorder. American Journal of Psychiatry. 2003;160(5):924–932. doi: 10.1176/appi.ajp.160.5.924. [DOI] [PubMed] [Google Scholar]
- Freedland K.E., Carney R.M., Rich M.W., Steinmeyer B.C., Skala J.A., Davila-Roman V.G. Depression and Multiple Rehospitalizations in Patients With Heart Failure. Clinical cardiology. 2016;39(5):257–262. doi: 10.1002/clc.22520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris T.O., Brown G.W. Social causes of depression. Current Opinion in Psychiatry. 1996;9(1):3–10. [Google Scholar]
- Kroenke K., Spitzer R. The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals. 2002;32:509–515. [Google Scholar]
- Lyons J.S., O’Mahoney M.T., Miller S.I., Neme J., Kabat J., Miller F. Predicting readmission to the psychiatric hospital in a managed care environment: Implications for quality indicators. The American Journal of Psychiatry. 1997;154(3):337–340. doi: 10.1176/ajp.154.3.337. [DOI] [PubMed] [Google Scholar]
- Markowe H.L., Marmot M.G., Shipley M.J. Vol. 291. 1985. Fibrinogen: A possible link between social class and coronary heart disease; pp. 1312–1314. (British Medical Journal (Clinical research ed)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muennig P., Bounthavong M. John Wiley & Sons; San Francisco: 2016. Cost-effectiveness analysis in health: A practical approach. [Google Scholar]
- Muennig P.A., Quan R., Chiuzan C., Glied S. Considering whether medicaid is worth the cost: Revisiting the oregon health study. American Journal of Public Health. 2015;105(5):866–871. doi: 10.2105/AJPH.2014.302485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- New York City. A roadmap for mental health for all. Available online at: 〈https://thrivenyc.cityofnewyork.us/wp-content/uploads/2016/03/ThriveNYC.pdf〉. (Accessed 30 March 2017).
- Rabin R., de Charro F. EQ-5D: A measure of health status from the EuroQol Group. Annals of Medicine. 2001;33:337–343. doi: 10.3109/07853890109002087. [DOI] [PubMed] [Google Scholar]
- Rehkopf D.H., Strully K.W., Dow W.H. The short-term impacts of Earned Income Tax Credit disbursement on health. International Journal of Epidemiology. 2014;43(6):1884–1894. doi: 10.1093/ije/dyu172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sephton S.E., Salmon P., Weissbecker I. Mindfulness meditation alleviates depressive symptoms in women with fibromyalgia: Results of a randomized clinical trial. Arthritis Care Research. 2007;57(1):77–85. doi: 10.1002/art.22478. [DOI] [PubMed] [Google Scholar]
- Smith G.D., Shipley M.J., Rose G. Magnitude and causes of socioeconomic differentials in mortality: Further evidence from the Whitehall Study. Journal of Epidemiology and Community Health. 1990;44(4):265–270. doi: 10.1136/jech.44.4.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorlie P.D., Rogot E. Mortality by employment status in the National Longitudinal Mortality Study. American Journal of Epidemiology. 1990;132(5):983–992. doi: 10.1093/oxfordjournals.aje.a115741. [DOI] [PubMed] [Google Scholar]
- Sparer M., Brown L., Muennig P. (2016). (Re) Defining the health care delivery system: The role of social services. (KPMG White Paper, Draft Copy. For resease June, 2016.).
- Sparer M., Muennig P., Brown L. (2016). (Re)defining the health care delivery system: the role of social services. Available online at: 〈https://assets.kpmg.com/content/dam/kpmg/pdf/2016/07/9-salud-re-defining-the-healthcare-delivery-system-the-role-of-social-services.pdf〉. (Accessed 15 August 2016).
- Speca M., Carlson L.E., Goodey E., Angen M. A randomized, wait-list controlled clinical trial: The effect of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients. Psychosomatic Medicine. 2000;62(5):613–622. doi: 10.1097/00006842-200009000-00004. [DOI] [PubMed] [Google Scholar]
- Wamala S.P., Lynch J., Horsten M., Mittleman M.A., Schenck-Gustafsson K., Orth-Gomer K. Education and the metabolic syndrome in women. Diabetes care. 1999;22(12):1999–2003. doi: 10.2337/diacare.22.12.1999. [DOI] [PubMed] [Google Scholar]
- Zaccaro S.J., Blair V., Peterson C., Zazanis M. Self-efficacy, adaptation, and adjustment. Springer; New York: 1995. Collective efficacy; pp. 305–328. [Google Scholar]