Abstract
The aim of this study was to examine associations between selected physical functional limitations related to performing daily activities and psychological distress. We also aimed to investigate if these associations vary across age (moderation), and to explore pain, sense of mastery and social support as potential moderators and mediators. The study was based on pooled data from two rounds (2008 and 2012) of a Norwegian nationally representative cross-sectional health survey (N = 8520) including individuals aged ≥ 16 years (Age groups = 16–44 and ≥ 45 years). Physical functional limitations comprised decreased ability to: i) climb stairs, ii) carry objects, or iii) both. Psychological distress was measured as anxiety and depressive symptoms occurring separately or in combination (CAD). Of respondents reporting physical functional limitations, 8–14% reported depressive symptoms, 5–7% anxiety symptoms, and 13–28% reported CAD. Physical functional limitations were significantly associated with all three forms of psychological distress, particularly among individuals 16–44 years, and were more strongly related to CAD than to anxiety or depression occurring separately. The association with CAD was twice as strong when both types of physical functional limitations were present. Pain, sense of mastery and social support were significant modifiers of depression, whereas all three were significant mediators of the relationship between physical functional limitations and anxiety, depression and CAD. Sense of mastery mediated the relationship between physical functional limitations and CAD, but most strongly among those 16–44 years. Social support was only a significant mediator among those 45 years. Close associations between physical functional limitations and psychological distress highlight special needs among individuals experiencing daily functional limitations. The results also suggest that pain, low social support, and low sense of mastery may contribute to aggravate psychological distress.
Keywords: Anxiety, Depression, Moderation analysis, Mediation analysis
Highlights
-
•
Physical functional limitations were associated with psychological distress.
-
•
Younger individuals were more psychologically distressed by functional limitations.
-
•
Sense of mastery was both a moderator and mediator.
-
•
Pain was an important mediator.
Introduction
The World Health Organization (WHO) (2013) has estimated that 2.2–3.8% of people worldwide, aged 15 years and older, have significant difficulties in performing daily activities due to loss of physical function. Prevalence estimates indicate that as many as 16% of the US population between the ages of 18 and 44 have at least one functional disability (Courtney-Long et al., 2015). The prevalence estimates increase with age, and are reported to be 26% among individuals aged 45–64 and 36% among those 65 years and older in the same US sample (Courtney-Long et al., 2015).
Functional limitations are commonly defined as restricted ability to perform necessary daily tasks like carrying and walking, which require functional mobility and strength. There is an important distinction between basic functional limitations and reduced discretionary leisure activities (Parmelee, Harralson, Smith & Schumacher, 2007). Ability to function physically on a daily basis – and in a satisfactory way, is important to mental health (Christensen et al., 2009, Schnittker, 2005, Verbrugge and Jette, 1994). Functional limitations might lead to mental health problems (Chen et al., 2012), and mental health problems may increase the complexity, challenges, and difficulties for individuals with functional limitations (Kojima, 2012, Raphael et al., 2005). Despite the large scientific literature on the interrelationship between somatic and mental health (Lenze, 2001, Nosek et al., 2008, Scott et al., 2007), and the importance of physical daily functioning to mental health, relatively few studies have investigated the relationship between physical functional limitations and mental health. The few studies that are published to date have focused on the elderly (Lee et al., 2012, Lenze, 2001, Muramatsu et al., 2010, Stegenga et al., 2012, Suttajit et al., 2010) and shown that the relationship between physical functional limitations related to carrying and squatting and depressive symptoms, are stronger than those resulting from difficulties related to standing, running, and climbing stairs, although all limitations are significantly associated (Lee et al., 2012). Among younger individuals, functional limitations associated with arthritis and lower limb injury (such as problems walking, carrying, etc.) have also been shown to be related to psychological distress (McCarthy et al., 2003, Shih et al., 2006). Although the relationship between functional limitations and mental health problems is complex and is most likely bidirectional, longitudinal evidence suggests that disability often precedes depression (Chen et al., 2012).
Several factors, and perhaps most notably pain, sense of mastery and social support, might moderate or mediate the association between physical functional limitations and mental health, but such moderation and mediation mechanisms are scarcely investigated. Pain is well known to be associated with psychological distress (Bair et al., 2003, Campbell et al., 2003, Currie and Wang, 2004, McWilliams et al., 2003, Parmelee et al., 2007). To examine the impact of functional limitations on psychological distress, it is important to separate the impact of functional limitations from that of pain. Functional limitations are not always associated with pain, either because pain is under control (e.g., through medication), or due to lack of pain (Ramage-Morin and Gilmour, 2010). In this paper, we thus discuss a possible moderator and mediator role of pain.
Some studies have reported associations between physical functional limitations and pain on the one hand and between pain and psychological distress on the other (Alschuler et al., 2008, Ramage-Morin and Gilmour, 2010). However, to date, few have studied the relationship between pain, daily functioning and mental health thoroughly (Jensen, Moore, Bockow, Ehde & Engel, 2011). The only study known to us, by Parmelee et al. (2007), reported pain to mediate the relationship between basic functional limitations associated with osteoarthritis and depression. This mediator role was complete, eliminating any significant direct relationship between functional limitations and depression (Parmelee et al., 2007). More studies have examined functional limitations as mediators between pain and depression, but with mixed results. Some studies have shown the relationship to be not significant (Geerlings et al., 2002, Parmelee et al., 2007, Wang et al., 2012), whereas others have indicated significant associations (albeit with cancer patients, and not those with functional limitations), with the association shown to be strongest among the youngest patients (Dickens et al., 2000, Williamson, 2000).
Sense of mastery is also likely to moderate or mediate the association between functional limitations and psychological distress. Sense of mastery refers to whether individuals feel they are able to influence important outcomes in their lives. A moderator role can be envisioned in which sense of mastery buffers the direct association between functional limitations and mental health. However, a mediator role can also be envisioned where the indirect pathway via sense of mastery explain much of the relationship between functional limitations and psychological distress. In the latter case, functional limitations must have a significant impact on sense of mastery, which in turn must be directly associated with psychological distress. The direct pathway must be significantly changed upon addition of the mediator (e.g., sense of mastery). Functional limitations have previously been shown to be independently associated with sense of mastery (Yang, 2006). As described for pain, sense of mastery is also known to be independently associated with mental health (Ross and Mirowsky, 2013). High sense of mastery is commonly associated with both better mental and physical health, as well as improved overall functioning in life (Lavikainen et al., 2006, Taylor and Stanton, 2007), and a significant negative association has been reported for sense of mastery and episodes of major depression (Ross and Mirowsky, 2013). Jang, Haley, Small, and Mortimer (2002) have previously reported sense of mastery to moderate the relationship between functional disability and depression. However, in another study (Yang, 2006), a mediator, but not moderator role of mastery was reported for the same association (i.e., functional limitations and depression). Functional limitations and depression were more highly correlated among individuals reporting low, rather than high, sense of mastery (p < 0.001). It is possible that high levels of mastery lead to better management of health-related problems and more effective mobilization of personal resources and coping strategies, as has been observed in the elderly (Jang et al., 2002).
Another important factor in the relationship between functional limitations and psychological distress may be social support. Physical functional limitations may, for example, lead to isolation and loneliness. Low social support may thus mediate the relationship between functional limitations and psychological distress. Social support is commonly referred to as a person’s perception of being loved, cared for, and valued by others (Lavikainen et al., 2006, Taylor and Stanton, 2007, Thoits, 2011). Social support tends to make people less vulnerable to negative emotional conditions, more likely to participate in health-promoting activities and social events, as well as to provide a network for help and practical assistance when needed (Myers, 2000, Thoits, 2011, Umberson and Montez, 2010). Perceived social support may also increase feelings of self-esteem and self-worth, which in turn may lead to emotional well-being (Jang et al., 2002, Thoits, 2011). Lack of social support was found to act as a mediator in the relationship between diagnosed physical impairments (i.e., sensory and amnestic impairments) or functional limitations and psychological distress among the elderly in a previous Norwegian study (Bøen et al., 2012, Yang, 2006). Social support has also been identified as an important buffer (moderator) against psychological distress (Ehsan and De Silva, 2015, Kawachi and Berkman, 2001). Social support, through its ability to increase proactive coping, has been shown to significantly moderate psychological distress through a weakening of the association between physical impairment and depression in the elderly (Greenglass, Fiksenbaum & Eaton, 2006). Additionally, high levels of social support are associated with less pain and better physical functioning (Jensen et al., 2011). Thus, whereas high social support can be beneficial for health-related outcomes, low social support is associated with increased risk for compromised health and physical functioning (Gazmararian, Baker, Parker & Blazer, 2000).
The primary aim of this study was to explore the association between physical functional limitations and psychological distress. Additionally, we examined the potential moderator and mediator role of pain, sense of mastery, and social support. Previous research in this area has primarily focused on the elderly. In this study, we therefore explore these associations in different adult age groups. Analyses are based on a large regularly repeated Norwegian health survey including individuals aged 16 years or older (N = 8520). The sample is nationally representative and covers pooled data from two survey rounds (2008 and 2012). Functional limitations include difficulties with carrying objects and/or climbing stairs. Our main hypotheses were that difficulties in performing everyday tasks are related to greater psychological distress. We further postulated that this relationship is at least partly associated through an alternate pathway (mediator) of pain. Further, the psychosocial parameters sense of mastery and social support were postulated to act as either mediators or moderators. Finally, it was hypothesized that these relationships would be equally relevant for both the younger and the older populations.
Methods
Design and study population
We used pooled data from two rounds (2008 and 2012) of the regularly repeated Survey of Living Conditions conducted in Norway by Statistics Norway (SN). Both surveys consisted of a personal interview by either telephone or visitation, followed up by a postal questionnaire. In total 10,000 individuals aged 16 and older were randomly selected each survey year. Additional demographic information was obtained from national population registers and the sample was found to be representative for the age, gender, and regional distribution of the Norwegian population. The response rate for the gross sample (interview and the postal questionnaire) was 46.5% in 2008 and 41.1% in 2012. Data from 2008 and 2012 were merged into a single dataset to increase the sample size and statistical power (N = 8520).
Ethics
The Survey of Living Conditions for 2008 and 2012 was approved by the Regional Ethics Committee (REK) prior to the data collection. Participation was voluntary and the data were treated anonymously. The Norwegian Social Science Data Service (NSD) granted the present study access to the data.1
Measures
The dependent variable psychological distress was measured by the Hopkins Symptom Checklist (HSCL-25) (Derogatis, Lipman, Rickels, Uhlenhuth & Covi, 1974) which was included in the postal questionnaires. The HSCL-25 is commonly used as a self-report tool for identifying common mental health problems. HSCL-25 contains 25 items, including 10 items related to anxiety (HSCL-a) and 15 items related to depression (HSCL-d) which may be used as separate subscales. Responses are given on a scale from 1 = “not troubled” to 4 = “extremely troubled”. According to convention, a mean score equal to or greater than 1.75 indicates elevated risk for clinical anxiety or depression (Sandanger et al., 1998). For both subscales (i.e., HSCL-a and HSCL-d), we used this standard cut-off value to indicate high symptom levels (Winokur, Winokur, Rickels & Cox, 1984). As anxiety and depression tend to co-occur (Pollack, 2000), we combined the scores into four categories, reflecting 0 = no symptoms of anxiety or depression, 1 = only anxiety symptoms ( 1.75), 2 = only depressive symptoms ( 1.75), and finally 3 = comorbid anxiety and depressive symptoms (CAD; both subscales 1.75). Cronbach’s alpha for the full scale was 0.92, and for the HSCL-a and HSCL-d subscales, alphas were estimated to 0.82 and 0.89, respectively.
The exposure variable was physical functional limitations, restricted due to data availability, to the difficulties in functioning approach. In accordance with recommendations from the WHO (2011), the “difficulties in functioning approach” (“A restriction or inability to perform an activity in the manner or within the range considered normal”) is favored over an “impairment approach” (“Any temporary or permanent loss or abnormality of a body structure or function”) to measure the extent of functional limitations (Barbotte et al., 2001, WHO, 2011). Data on functional limitations were retrieved from the interview section of the surveys and assessed by two separate items. The first item dealt with whether or not the respondent had difficulties climbing up and down one floor of stairs without any rest. The second item asked whether the respondent had difficulties carrying a 5 kg object for more than 10 m. The difficulties should have lasted six months or more, and be present even with the use of assistive devices. The response alternatives were “yes” and “no” for both items. We combined responses to the two items into one variable with the categories 0 = “no difficulties”, 1 = “difficulties walking stairs”, 2 = “difficulties carrying”, and 3 = “difficulties with both walking stairs and carrying”. For the mediation analysis, this variable was recoded to include three groups: 0 = “no difficulties”, 1 = “one difficulty”, and 2 = “both difficulties present simultaneously”.
Pain was indicated by two questions: i) “Do you have bodily pain” (yes/no) and ii) “During the past four weeks, how often have you used the following drugs?” In the latter, the use of pain medication either with or without prescription were among the choice of drugs (response alternatives: 0 = “not used over the last four weeks”; 1 = “weekly, but not daily”; 2 = “at least every week”; and 3 = “daily”. The two alternatives of using pain medication with, or without prescription were combined. We constructed a new variable based on these two sources of information (0 = neither pain nor use of pain medication, 1 = either pain, but no medication use; or no pain, but pain medication use, and 2 = pain and use of medication).
Information on sense of mastery was obtained from the postal questionnaire. Sense of mastery was measured with a five item version of Pearlin and Schooler’s (1978) Mastery Scale (i.e., the perceived constraint facet of the scale). The five statements were: “I have little control over the things that happen to me”, “There is really no way I can solve some of the problems I have”, “There is little I can do to change important things in my life”, “I often feel helpless in dealing the with problems of my life” and “I sometimes feel like a piece in the game of life” (five response alternatives: 1 = “strongly agree” to 5 = “strongly disagree”). The sum scores were used in the analyses (range 5–25). Cronbach’s alpha was estimated to 0.84 in the current sample.
Information concerning social support was a part of the interview section of the survey. Social support was measured with the Oslo Social Support Scale (OSS-3) (Meltzer, 2003). This measure contains three items reflecting different dimensions of perceived social support; “How many people are so close to you that you can count on them if you have serious personal problems?” (1 = “none”, 2 = “1 or 2”; 3 = “3–5”; 4 = “5+”), “How much concern do people show in what you are doing?” (1 = “much interest”, 2 = “some interest”, 3 = “neither much or little interest”, 4 = “little interest”, and 5 = “no interest”) and “How easy is it to get practical help from neighbors if you should need it?” (1 = “quite easy”, 2 = “easy”, 3 = “neither easy or difficult”, 4 = “difficult”, and 5 = “very difficult”). The items were summed, giving a total score ranging between 3 and 14 (Dalgard et al., 2006; Lavikainen et al., 2006).
Information on age and gender was retrieved from national registers. Age was treated as a continuous variable when included as a confounder. To explore differences over periods in the life span, the age variable was grouped into three time periods, young adult (16–44 years), middle age adult (45–66 years), and elderly (≥ 67 years). When dichotomized for the mediation analyses, to have a relatively balanced sample size in each group, the groups were defined as 16–44 and ≥ 45 years. Information on level of education was obtained from the Norwegian population register and categorized into three educational levels; low (i.e., elementary and middle school/up to 9 years of education), medium (i.e., completed secondary high school or one year of university studies) and high (i.e., holding a bachelor or higher university degree). Family size was also obtained from the Norwegian population register and had two classifications. The classifications were, either having only 2 family members or having a family size that differed from 2 members. Self-rated health was selected as a proxy measure to adjust for chronic disease. It was used as a confounder and measured by a single question: “How do you evaluate your health in general?” with five response alternatives from very good to very bad. The variable was simplified to 3 categories: 1 = “very good/good”, 2 = “neither good nor bad”, and 3 = “bad or very bad”.
Data analysis
All analyses were conducted using SPSS version 23. Preliminary exploratory analyses, revealed Tolerance and VIF values that did not violate the multicollinearity assumption (Tolerance values were above 0.889 and VIF values beneath 1.124) (Pallant, 2013). In all analyses, data were weighted separately for each of the two survey years to account for dropout using information on gender, age, level of education, and family size from national registers. Individuals with underrepresented characteristics (i.e., gender (male)), age (age groups 16–24, 25–44 and ≥ 80 years), level of education (lowest levels through high school), and family size (having only 2 family members as opposed to different from 2) were weighted heavier than those with overrepresented characteristics (Lillegård, 2009).
Differences in prevalence were tested for significance using the z-test, and differences in the means using t-tests. Column means (t-tests) were compared for equality, pairwise between the three different age group categories. Column proportions (z-tests) were similarly tested using pairwise comparisons of the equality of the column proportions (%) for the three different age group categories. The p values of the tests were adjusted using the Bonferroni method. An alpha level of 0.05 was used for all tests.
Moderation and mediation analyses were prominent analyses in this study. Moderation measures if the significant relationship between the independent variable (in this case functional disability) and the dependent variable (mental health problems) is modified by a third parameter, the moderator. This is studied by first examining if the interaction term between the moderator and the independent variable is significant, and then examining the subsequent differences in the association of the independent and dependent variable at different levels of the moderator. Moderation in this study was assessed using model 1 of the PROCESS module (Hayes, 2013).
Mediation, on the other hand, attempts to determine if the relationship between the independent and dependent variable is better explained by their relationship to a third variable, the mediator. In these analyses, there is a direct and an indirect effect. Baron and Kenny (1986) were the first to propose actual conditions that need to be met for a variable to be considered as a mediator. These include for the case of consistent mediation models, four steps: 1) a significant association between independent and dependent variable, 2) a significant association between the independent variable and the mediator, 3) a significant association between mediator and dependent variable, and 4) a significant decrease in the association between independent and dependent variable when the mediator is added to the analyses. These methods have been refined and developed by Hayes, and implemented in the module PROCESS (Hayes, 2013). In addition, there exists a further model of mediation, the inconsistent mediation model, where the direct effect of the independent variable is strengthened instead of reduced, with the addition of the mediator. This model is called suppression, and indicates that much of the variation in the independent variable is associated with the mediator (MacKinnon, Krull & Lockwood, 2000).
The preliminary analysis of mediation was a hierarchal logistic regression analysis. Since the data were weighted to account for dropout, analyses were performed with the complex sample module in SPSS that adjusts the standard errors for the modified sample size (Osborne, 2011). The results were reported as odds ratios (OR) with 95% confidence intervals (CI). The three subscales of the HSCL-25 (anxiety, depression, and CAD) were entered as dependent variables in separate analyses. The analyses were adjusted for self-rated health as well as age, gender, survey year, and level of education. In step one, functional limitations were added as a categorical variable with “no functional difficulties” as reference group. Each of the mediating variables was entered separately in step two. In order to give a first impression of the existence of mediation, the OR and CI for functional limitations were compared between step one and step two to indicate if addition of the given mediator decreased the OR, or the association between the independent variable (i.e., functional limitations) and the dependent variables.
Three variables were used as mediators: 1) pain; 2) sense of mastery and 3) social support. The mediation analyses were performed by entering all three mediators simultaneously using the PROCESS module in SPSS (model 4) (Hayes, 2013). The logistic regression option in the PROCESS module was chosen since the outcome variable CAD was dichotomous. The PROCESS module provides 76 models to choose from, whereas model 1 is pure moderation of 1 moderator, and model 4 is pure mediation of 1–6 mediators. Mediation was tested for significance for the total pathway, and for the indirect pathway using the bootstrap method and finally the Sobel test – all provided in the PROCESS module. As the PROCESS module cannot handle weighted data, unweighted data were used in these analyses. Since mediation analyses (here a form of logistic regression) of weighted and unweighted data may differ, robustness was tested using logistic regression with and without weights. Weighted data were analyzed using logistic regression analyses in complex samples, whereas non-weighted data were analyzed using regular logistic regression analyses. Each of the independent variables and each of the mediators were tested, and the results indicated no major differences in either betas or the resulting significance tests.
A moderating role of age for the analysis of the mediating model was also tested using PROCESS. If age was found to be a significant moderator of the relationship between functional limitations and comorbid anxiety and depression, the mediation analyses would be repeated for the two age groups (i.e., 16–44 and ≥ 45 years).
Results
General characteristics
Table 1 shows the weighted prevalence of psychological distress and physical functional limitations, along with descriptive statistics for the moderator/mediator variables and socio-demographic information for the three age groups. The overall prevalence of anxiety symptoms, depressive symptoms, and CAD were 3.2%, 6.1% and 6.8%, respectively. There were significant differences in prevalence estimates in the three age groups, with generally lower prevalence in older age groups. A relatively low percentage (7.4%) reported functional difficulties, and of those, 2.9% reported having difficulties with carrying, 2.1% with climbing stairs, and 2.4% with both carrying and climbing stairs. A higher proportion of those over 66 years reported both forms of functional difficulties. Among the youngest individuals, a higher proportion reported no bodily pain or use of pain medication. However, there was no significant differences in pain levels in those between 45 and 66 years or those 67 or older. As many as 10–11% in these age groups both experienced pain and took pain medication. Levels of sense of mastery and social support were lower in those over 66 years. Overall, about 80% reported their health to be good or very good, but the proportion was higher in the youngest age group.
Table 1.
Prevalence (%) or mean of sample characteristics as a function of age groups (Weighted N = 17,686–18,720).
|
Age (years) |
|||||
|---|---|---|---|---|---|
| 16–44 | 45-66 | ≥ 67 | Total | ||
| Psychological distress | None | 81.4a | 85.8b | 87.7c | 84.0 |
| Anxiety alone | 3.6a | 2.6b | 3.0a.b | 3.2 | |
| Depression alone | 6.9a | 5.4b | 5.1b | 6.1 | |
| Comorbid Anxiety and Depression | 8.0a | 6.2b | 4.1c | 6.8 | |
| Physical functional limitations | None | 97.1a | 92.9b | 77.1c | 92.6 |
| Climbing stairs | 0.6a | 1.7b | 7.8c | 2.1 | |
| Carrying | 1.4a | 3.2b | 7.5c | 2.9 | |
| Climbing stairs and carrying | 1.0a | 2.2b | 7.6c | 2.4 | |
| Self-rated health | Good/Very good | 85.7a | 75.3b | 68.6c | 79.3 |
| Neither good or bad | 10.3a | 15.5b | 19.5c | 13.6 | |
| Bad/Very bad | 4.0a | 9.2b | 11.9c | 7.1 | |
| Gender | Male | 52.2a | 51.0a | 44.6b | 50.6 |
| Female | 47.8a | 49.0a | 55.4b | 49.4 | |
| Education | Low | 30.9a | 23.6b | 38.6c | 29.5 |
| Medium | 38.6a | 46.6b | 44.7b | 42.5 | |
| High | 30.6a | 29.8a | 16.7b | 28.0 | |
| Survey year | 2008 | 49.3a | 47.8a.b | 45.2b | 48.1 |
| 2012 | 50.7a | 52.2a.b | 54.8b | 51.9 | |
| Pain | No pain or pain medication | 75.5a | 64.5b | 65.2b | 70.1 |
| Pain but no medication, or no pain but medication | 18.5a | 25.1b | 24.3b | 21.7 | |
| Both pain and pain medication | 6.0a | 10.4b | 10.5b | 8.2 | |
| Sense of mastery | Mean(SE) | 14.7a(0.04) | 14.9b(0.05) | 13.5c(0.09) | 14.6(0.03) |
| Social support | Mean(SE) | 12.1a(0.02) | 11.8b(0.03) | 11.1c(0.04) | 11.8(0.02) |
Note: Values in the same row not sharing the same subscript are significantly different at p < 0,05 in the two-sided test of equality for column proportions. Cells with no subscript are not included in the test. Tests assume equal variances.
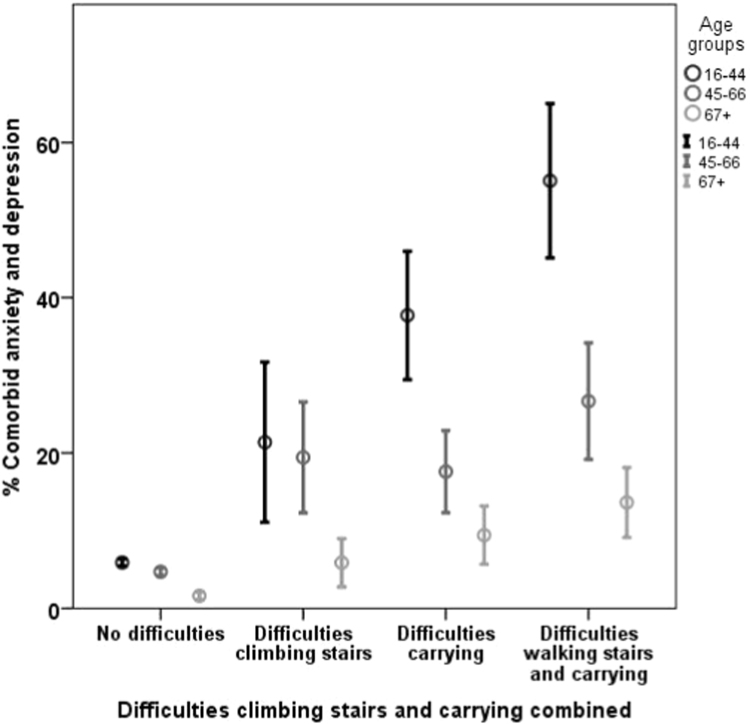
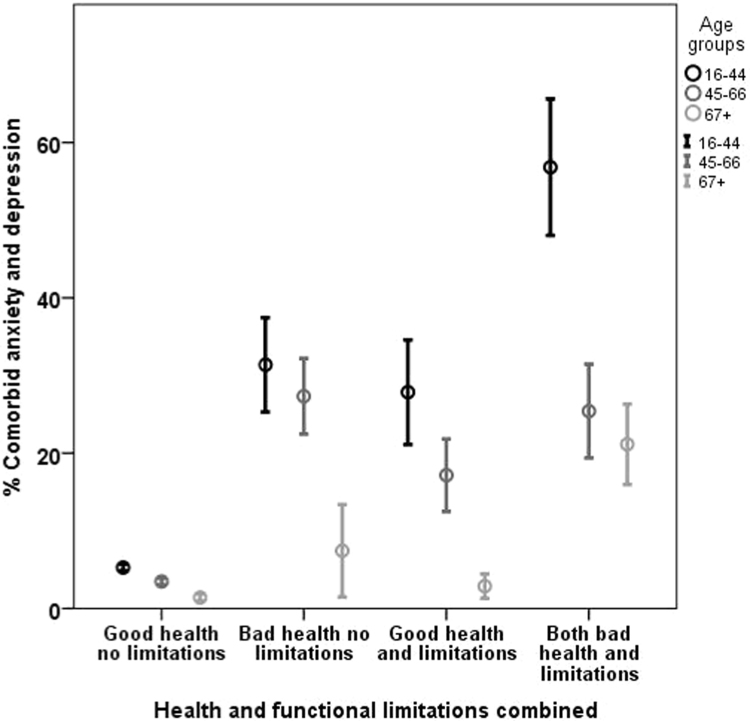
As shown in Table A.1 and Fig. A.1 in the Appendix A, the percentage reporting psychological distress (particularly depressive problems and CAD) was higher in those reporting physical functional limitations, with the prevalence of CAD being particularly high (28%) among those reporting both functional limitations. This was especially true for the youngest population. The proportion reporting pain or use of pain medication were significantly greater among individuals reporting both forms of functional limitations. However, there were significantly more with pain/use of pain medication among those with problems carrying (31%) than with problems climbing stairs (18%). Individuals reporting functional limitations also reported lower mastery and social support. Additionally, one observes a similar degree of CAD with poor health as seen with functional limitations. This difference is most evident among those 44 years or less (Table A.2 and Fig. A.2 in the Appendix A).
Fig. A.1.
Percent of the population (with CI as error bars) with physical functional limitations exhibiting comorbid anxiety and depression by age group (weighted data).
Fig. A.2.
Percent of the population (with CI as error bars) with good or poor self-rated health and/or physical functional limitations exhibiting comorbid anxiety and depression by age group (Weighted data). A dichotomous version of both physical functional limitations and self-rated health were combined to create the new variable used here.
Logistic regression analyses
Table 2 shows the association between functional limitations and psychological distress when controlling for self-rated health, gender, educational level, survey year and age. All three groups of functional limitations were significantly associated with psychological distress in terms of CAD. The association was especially strong for those reporting difficulties with both carrying and climbing stairs. Difficulties climbing stairs, and the two limitations combined, were also significantly associated with depressive problems occurring independently, whereas anxiety was only significantly related to combined functional limitations. This suggests increased severity of psychological distress with increased severity of physical functional limitations. Entering sense of mastery in Step 2 reduced the OR for depression and CAD – for all three forms of functional limitations. These declines in ORs indicate that sense of mastery may mediate the association between functional limitations and CAD. Adding pain led to increased ORs for difficulties climbing stairs for both depressive symptoms and CAD, and for combined functional limitations for depressive symptoms. This indicates that much of the variation associated with functional limitations was associated with pain, hence a suppression mediation effect. There was a standard mediation effect of pain, as indicated by reduced association between combined functional limitations and CAD. The introduction of social support to the model resulted in reduced ORs for depressive symptoms and CAD.
Table 2.
The association (odds ratio) between physical functional limitations and anxiety, depression or both (CAD) before or after inclusion of pain, sense of mastery (SM) and social support (SS) as analyzed by hierarchal regression (OR with 95% confidence interval). (Weighted-N = 17,278).
| Weighted sample size W-N |
Physical functional limitations |
||
|---|---|---|---|
| Difficulties climbing stairs | Difficulties carrying | Difficulties climbing stairs and carrying | |
| 339 | 507 | 428 | |
| Anxiety symptoms | |||
| Step 1 | 1.67[0.77–3.61]NS | 1.56[0.72–3.40]NS | 2.49[1.23–5.04]* |
| Step 2 Pain | 1.91[0.82–4.49]NS | 1.34[0.75–2.43]NS | 1.98[0.85–4.58]NS |
| Step 2 SM | 1.75[0.77–3.96]NS | 1.63[0.72–3.69]NS | 1.86[0.86–4.01]NS |
| Step 2 SS | 1.72[0.79–3.40]NS | 1.63[0.75–3.54]NS | 2.51[1.19–5.29]* |
| Depressive symptoms | |||
| Step 1 | 1.92[1.13–3.27]* | 1.40[0.82–2.39]NS | 3.07[1.95–4.83]*** |
| Step 2 Pain | 2.26[1.28–3.99]** | 1.35[0.75–2.43]NS | 3.59[2.07–4.64]*** |
| Step 2 SM | 1.72[0.95–3.12]NS | 1.17[0.60–2.30]NS | 1.76[0.98–3.16]NS |
| Step 2 SS | 1.86[1.07–3.24]* | 1.22[0.69–2.14]NS | 2.70[1.67–4.34]*** |
| Comorbid Anxiety and Depressive symptoms | |||
| Step 1 | 2.63[1.44–4.79]** | 3.24[2.10–5.02]*** | 6.43[3.90–10.59]*** |
| Step 2 Pain | 3.30[1.69–6.45]*** | 2.13[1.30–3.50]** | 4.64[2.68–8.04]*** |
| Step 2 SM | 2.20[1.10–4.39]* | 2.38[1.30–4.37]** | 3.00[1.61–5.64]** |
| Step 2 SS | 2.32[1.22–4.40]* | 2.53[1.58–4.05]*** | 5.20[3.14–8.61]*** |
Gender, age, education level, self-rated health and year, were controlled for in all blocks.
Pain or pain medication, sense of mastery (SM) and social support (SS) were added in separate analyses in block 2.
All data were weighted and the analyses were performed using the module complex samples.
Note: S = significant; NS = non-significant. Significance: p < 0.05 = *; p < 0.01 = **; p < 0.001 = ***.
Moderation analyses
The moderator analyses (model 1 in PROCESS) showed mixed results as seen in Table 3. Pain was only a significant modifier for depression. By contrast, sense of mastery moderated the relationship between functional limitations and both depression and CAD. Finally, social support was only a significant modifier for depression.
Table 3.
Results of moderator and mediator analyses (models 1 and 4, PROCESS) for the three parameters pain, sense of mastery and social support, in the association between increasing functional limitations and the three measures of psychological distress, anxiety, depression and comorbid anxiety and depression (CAD). For moderator analyses significance level of interaction term is provided, and for mediator analyses indirect and direct effect estimates.
|
Psychological distress |
|||
|---|---|---|---|
| Effect | AnxietyN = 6818 | DepressionN = 7032 | CADN = 7024 |
| Moderator Analyses (Significance level) | |||
| Pain | 0.060 | 0.016 | 0.194 |
| Sense of mastery | 0.269 | 0.004 | 0.000 |
| Social support | 0.836 | 0.015 | 0.816 |
| Mediation analyses (Effect estimator(SE)) | |||
| Direct | 0.08(.12)NS | 0.07(.09)NS | -0.00(.10)NS |
| Indirect | |||
| Pain | 0.08(.02)*** | 0.04(.01)*** | 0.11(.02)*** |
| Sense of mastery | 0.07(.02)*** | 0.14(.04)*** | 0.23(.04)*** |
| Social support | -0.02(.01)NS | 0.02(.01)* | 0.03(.01)** |
Analyses controlled for gender, age, self-rated health and year. p < 0.05 = *; p < 0.01=**; p < 0.001 = ***.
Mediation analyses
The mediator analysis (Table 3) (model 4 in PROCESS), showed that pain (pain and/or use of medication) and sense of mastery significantly mediated the relationship between functional limitations and all three mental health outcomes. The indirect effect of social support was only significant for depression and CAD. For CAD, the indirect pathway showed a significant positive relationship between physical functional limitations and pain, and a negative relationship with sense of mastery and social support. The reverse was seen in the relationship between each of the mediators and CAD. All relationships were highly significant (p < 0.001) (data not shown). The indirect pathways, when testing for mediation of all three parameters simultaneously, accounted for all the variation, as the direct pathway was reduced to non-significance for anxiety, depression and CAD. These results confirm the results from the logistic regression analyses for pain and sense of mastery, and indicate complete mediation. Thus, the association between psychological distress observed in those with functional limitations is mostly explained through pain as well as reduced sense of mastery and low social support. The reverse scenario, in which pain is the independent variable and functional limitations the mediator, was tested and found to be non-significant (data not shown).
Moderation of mediated association
Moderator analysis (model 1 in PROCESS), on the other hand showed a significant moderator role for age in the relationship between functional limitations and CAD (data not shown).
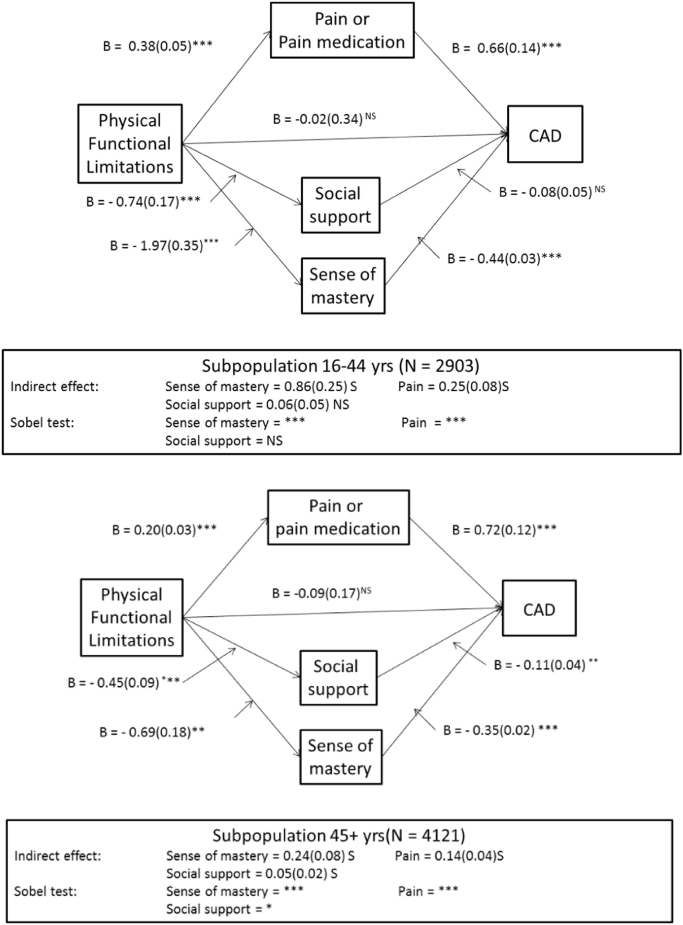
Since age was a significant modifier, the mediator roles of pain, sense of mastery and social support were also tested separately in the two age groups. To test if these indirect and direct pathways differed across age, the analyses were repeated for the age group 16–44 years and ≥ 45 years. The results (Fig. 1) indicated that the relationship between physical functional limitations and pain was twice as strong in the younger age group, and the associations between functional limitations and sense of mastery and social support were three times as great. The relationship between pain and CAD, although significant in both age groups, was only slightly higher in the younger. Similarly, the negative association between sense of mastery and CAD was 25% higher in the younger group. The relationship between social support and CAD was not significant in the younger group. There was no direct relationship between physical functional limitations and CAD in either age group.
Fig. 1.
Indirect (mediation) or direct association between the physical functional limitations and comorbid anxiety and depression (CAD) by pain, sense of mastery and social support in two age groups (age is moderator); those 44 and younger (16–44 years, upper panel) and those 45 years and older (lower panel). Gender, age, survey year and self-rated health were controlled for. Pain, sense of mastery (SM) and social support (SS) were added simultaneously. All data analyzed using model 4 of the PROCESS module. Significance for the 3 indirect effects were examined using bootstrapping/Sobel test. Note. S = significant; NS = non-significant. Significance: p < 0.05 = *; p < 0.01 = **; p < 0.001 = ***.
Discussion
This cross-sectional study examined the association between physical functional limitations and psychological distress using a large and representative sample of the Norwegian population. Additionally, the moderating and mediating roles of pain, sense of mastery and social support, were investigated.
A total of 7.4% of the respondents reported physical functional limitations in terms of having answered “yes” to having trouble climbing stairs, carrying 5 kg weight, or both. These estimates are higher than the prevalence estimates for physical functional limitations reported globally (WHO, 2013), but may reflect differences in either the type of difficulties or the severity of difficulties examined. The overall prevalence for Norway in the WHO study was 4.3% (WHO, 2011). In the current study, three percent of respondents between 16 and 44 years reported at least one physical functional limitation as compared to 13% of those 67 years and older.
The present study indicates that having difficulties with everyday activities, such as carrying and climbing stairs, is related to more anxiety and depressive problems (controlling for self-rated health). The associations between comorbid anxiety and depressive problems and functional limitations were not only consistently significant, but also greater than those with anxiety or depression separately (Scott et al., 2007).
Our study also indicates that the association between having both functional limitations (i.e.carrying and climbing stairs) and psychological distress is not only significant but twice as high (β = 6.4; p < 0.001) as the association for either form of functional limitation alone (β = 2.6; p < 0.01 for difficulties climbing stairs, and β = 3.2; p < 0.001 for difficulties carrying). This suggests that the risk of developing psychological distress increases when individuals have more than one form of functional limitation. The prevalence of CAD was estimated to 27% among those reporting combined functional limitations in the age group 45–66 years as compared to 19% among those reporting one functional limitation. The respective prevalence estimates in the younger age group (16–44 years) were 55% and 21%. Additionally, in the younger age group, higher prevalence of CAD was observed for those reporting difficulties with carrying (38%), than those reporting difficulties climbing stairs (21%). This difference is supported by findings from a previous study by Lee et al. (2012) who found difficulties carrying to be more closely related to depression than having difficulties climbing stairs. The current study, however, indicates that the probability of experiencing either depression or anxiety (not comorbid) is not significantly different with either form of functional limitation.
Moderation or mediation of primary association
This study explored three parameters as either moderator or mediators, namely pain, sense of mastery, and social support. None of these parameters were modifiers of anxiety, all three were modifiers of depression and only sense of mastery was a modifier of CAD. Pain and sense of mastery showed a partial mediating effect for the association between functional limitations and all three forms of psychological distress. Social support did not mediate the relationship between functional limitations and anxiety, but did with depression and CAD – while controlling for gender, age, year of study and self-rated health. The three mediators (pain, sense of mastery and social support) may represent alternative pathways that may in part explain the association with psychological distress. As described in the literature, all three mediators are significantly associated with psychological distress (Bair et al., 2003, Lavikainen et al., 2006, Ross and Mirowsky, 2013, Taylor and Stanton, 2007, Thoits, 2011). However, all three are also significantly associated with increased physical functional limitations.
Pain is a very important element, that often, although not always, is present with physical functional limitations. Pain is associated with psychological distress, especially depression, but also anxiety (Bair et al., 2003, Campbell et al., 2003, Currie and Wang, 2004, McWilliams et al., 2003, Parmelee et al., 2007). There have been three scenarios proposed in the literature concerning the relationship between functional limitations, pain and psychological distress: 1) functional limitations are the independent variable, psychological distress the dependent variable and pain the mediator, 2) pain is the independent variable, psychological distress the dependent variable and functional limitations the mediator, and finally 3) both pain and functional limitations have independent association with psychological distress. The current study confirmed a significant mediator role for pain in the association between functional limitations and three forms of psychological distress, and moderator role with depression. As such, our findings corroborate findings of a mediator role for pain as reported by Parmelee and colleagues on osteoarthritis (Parmelee et al., 2007). The reverse scenario, where functional limitations are the mediator in an association between pain and psychological distress, was not observed in this study. Along with earlier research findings (Alschuler et al., 2008, Banks and Kerns, 1996, Lakke et al., 2012, Ramage-Morin and Gilmour, 2010), our study is thus in line with the first scenario presented above and indicates that pain is likely to be a major contributing factor to excess psychological distress among individuals with functional limitations. The combined moderator and mediator role of pain with depression, may partially explain the disparate results reported in the literature. The association between pain and depression, partially described through biopsychosocial models, may result in increased disability as well as increased use of health care systems (Bair et al., 2003, Campbell et al., 2003).
Sense of mastery is also an important factor, that relates both to functional limitations and to psychological distress. High levels of mastery could potentially play a preventive role in the development of symptoms of psychological distress when faced with functional limitations indicative of a moderator role. When individuals are faced with limitations, it is conceivable that their feelings of mastery will be diminished suggestive of a mediator role.
This study confirmed a moderator role for sense of mastery on depression and CAD, indicative of a buffering role. However, a significant mediator role was likewise observed. A similar finding was described earlier, also using Pearlin’s measure of sense of mastery (Yang, 2006). We also found the expected negative association between sense of mastery and psychological distress, as has been seen earlier (Ross & Mirowsky, 2013). Sense of mastery partially mediated the association between increased physical functional limitations and psychological distress. Earlier reports describe a moderating influence (Jang et al., 2002), although this is contested (Yang, 2006). Others report a clear mediator relationship (Yang, 2006). Our data suggest that the relationship between functional limitations and psychological distress is both partly regulated through an independent pathway through sense of mastery and through a moderation of the association. Reduced sense of mastery resulting from functional limitations may in turn, lead to increased psychological distress. This relationship was strongest in the younger age group, emphasizing the need for health-related systems to employ measures to promote mastery among individuals with functional limitations, especially in those between 16 and 44 years.
Finally, physical functional limitations may result in individuals isolating themselves more, and having more trouble in socializing, thus reducing social support. Social support may promote coping behavior in individuals with functional limitations. Although this study found only a slight moderator role of social support with depression, it found a significant mediator role, including both a decrease in social support with more limitations, and a negative association between social support and psychological distress. However, the mediator role of social support was weaker than for sense of mastery and pain. The current study thus is supported by the previous studies indicating social support as an important buffer (moderator) against psychological distress (Ehsan and De Silva, 2015, Greenglass et al., 2006, Kawachi and Berkman, 2001).
Moderation of mediated association
A moderator role for age was indicated in this study. This finding corroborates previously reported findings of higher levels of psychological distress in younger individuals with combined physical functional limitations (McCarthy et al., 2003, Schnittker, 2005, Shih et al., 2006). Hence, mediation was examined separately across age groups (16–44 or ≥ 45 years).
Pain was a significant mediator in the relationship between functional limitations and CAD in both age groups. The relationship between increased physical functional limitations and pain is substantially stronger in the population 16–44 years than among those 45 or older, indicating a moderator role of age on the mediator pain. Pain was particularly strongly and significantly related to CAD. This association was substantially greater among the younger (16–44 years). A stronger association between activity restriction and depression has also previously been observed in younger as opposed to older cancer patients (Williamson, 2000).
Overall, our study also suggests that the association between functional limitations and psychological distress is stronger, and the mediating role of sense of mastery is particularly important in the younger age groups. These findings are in line with the theories proposed by Verbrugge and Jette (1994), indicating greater emotional intensity among young people, but perhaps more likely greater expectations related to health, activity, and ability to manage daily activities in the young, thus leading to greater psychological distress. Additionally, these results may also reflect that functional limitations in younger individuals are associated with more severe, and perhaps unexpected disease scenarios, than in the elderly, whose problems gradually increase with age and are expected. The results may also reflect that with increasing age, psychological distress may be less dependent on perceived mastery and control (Verbrugge & Jette, 1994).
The findings pertaining to social support were mixed. Social support was found to be a significant mediator in the older age group ( 45 years). However, social support was not a significant mediator in the younger age group (< 45 years). Our results are thus in agreement with previous studies among the elderly, indicating that social support significantly mediates the relationship between functional limitations and psychological distress (Bøen et al., 2012, Yang, 2006).
Strengths and limitations
This study has several notable strengths including a large sample that is nationally representative for the Norwegian population and a specific weighting system that accounted for identified non-responders. However, the response rate in both survey years was relatively modest and the dropout followed a social gradient (i.e., lower response rate among those with low socioeconomic background). Although this may lead to underestimation of the relationship between functional limitations and psychological distress, the use of weights based on national register information on dropout characteristics for each survey year, should partially remediate this.
Furthermore, our study was based on self-report with no clinical validation. Our measures of psychological distress, sense of mastery, and social support are well established and show excellent psychometric properties (Clench-Aas et al., 2017, Lavikainen et al., 2006). Both HSCL-25, and anxiety and depression separately, have been shown to be reliable and valid measures of emotional symptoms and psychological distress (Derogatis et al., 1974, Sandanger et al., 1998, Winokur et al., 1984). HSCL-25 predicts depression better than other diagnoses, and anxiety as second best (Strand, Dalgard, Tambs & Rognerud, 2003). However, it is a disadvantage that some of the items in HSCL-25, particularly anxiety items, queries about physical symptoms (headache, dizziness, fatigue or trembling). These items are important in identifying anxiety, but through their association with either functional limitations or somatic disease, could potentially lead to somewhat inflated associations.
Functional limitations were only measured with two specific questions, which makes the definition of functional limitations quite narrow, possibly decreasing the generalizability of the findings. Lack of information on specific diagnoses were not available to this study and constitutes another important limitation. However, self-rated health, as used in the study, has been shown to predict mortality and to reflect somatic health conditions fairly well (Quesnel–Vallée, 2007). Of note, self-rated health may also reflect an element of mood, or mental health, that may have weakened the relationships observed between functional limitations and CAD in this study.
Although the study used data collected in two survey rounds, the design was cross-sectional and causal conclusions are therefore not possible. Cross-sectional designs also preclude conclusions on the directionality of the association. Earlier studies have found that psychological distress has a disabling effect, which means that the possibility exists that psychological distress in itself may increase the feeling of loss of functionality under certain conditions (Purdie, Kellett & Bickerstaffe, 2012). The associations are therefore potentially bidirectional. However, Ormel, Rijsdijk, Sullivan, van Sonderen and Kempen, (2002) reported that disabilities/daily functioning had a faster and stronger effect on depression than depression had on disabilities/daily functioning.
Conclusion
This study shows that 28% of those with combined physical functional limitations related to walking or carrying show signs of clinical-level anxiety and depression. Therefore, common health problems associated with having functional limitations should be extended to include psychological distress. Sense of mastery is an important moderator, and pain, (low) sense of mastery and (low) social support appear to constitute important mediating factors. Psychological distress seems to be more prevalent in the younger age groups with functional limitations. Individuals having functional limitations thus constitute a particularly vulnerable group. The strong association between functional limitations and psychological distress observed in this study highlights the need for increased awareness among health professionals of the risk of mental health problems in individuals with physical functional limitations. The important mediating influences related to pain, low sense of mastery and low social support are special areas that need to be addressed especially among the younger population.
Conflicts of interest
There are not conflicts of interest for any of the authors.
Footnotes
Data is organized and made available anonymously by Norwegian Social Science Data Services (NSD). Neither SN nor NSD are responsible for data analysis or interpretations presented here.
Appendix A
Table A1.
Prevalence of psychological distress, pain and self-rated health, and mean (SE-standard error) of sense of mastery and social support, according to level of physical functional limitations (Weighted N = 18297).
| Physical functional limitations |
|||||
|---|---|---|---|---|---|
| No difficulties | Difficulties climbing stairs | Difficulties carrying | Difficulties climbing stairs and carrying | ||
| Psychological distress | None | 86.0a | 69.5b | 67.6b | 51.4c |
| Anxiety alone | 2.9a | 6.5b | 4.7a.b | 6.3b | |
| Depression alone | 5.7a | 10.7b.c | 7.6a.b | 14.3c | |
| Comorbid Anxiety and Depression | 5.5a | 13.3b | 20.1c | 27.9d | |
| Pain | No pain or pain medication | 73.2a | 53.9b | 27.9c | 20.9c |
| Pain but no medication, or no pain but medication | 20.5a | 27.7b | 41.2c | 33.9c | |
| Both pain and pain medication | 6.2a | 18.4b | 30.9c | 45.2d | |
| Self-rated health | Good/Very good | 83.9a | 39.6b | 38.9b | 19.5c |
| Neither good or bad | 12.2a | 25.6b.c | 29.5b | 21.5c | |
| Bad/Very bad | 3.9a | 34.8b | 31.5b | 59.0c | |
| Sense of mastery | Mean(SE) | 14.9a(0.03) | 12.1b(0.25) | 12.6b(0.23) | 9.7c(0.27) |
| Social support | Mean(SE) | 11.9a(0.02) | 11.2b(0.13) | 10.8b(0.11) | 10.1c(0.13) |
Note: Values in the same row not sharing the same subscript are significantly different at p <,05 in the two-sided test of equality for column proportions. Tests assume equal variances.
Table A2.
Prevalence (%) of psychological distress, physical functional limitations and pain, and mean (SE-standard error) of sense of mastery and social support, according to level of subjective general health (Weighted N = 18,297).
|
Self-rated health |
|||
|---|---|---|---|
| Good/Neutral | Poor | ||
| Psychological distress | None | 88.7a | 59.4b |
| Anxiety alone | 2.5a | 5.0b | |
| Depression alone | 4.5a | 13.2b | |
| Comorbid Anxiety and Depression | 4.4a | 22.3b | |
| Physical functional limitations | No difficulties | 95.3a | 52.7b |
| Physical functional difficulties | 4.7a | 47.3b | |
| Pain | No pain or pain medication | 73.3a | 24.9b |
| Pain but no medication. or no pain but medication | 20.7a | 35.6b | |
| Both pain and use of pain medication | 6.0a | 39.5b | |
| Sense of mastery | Mean(SE) | 14.9a (0.03) | 10.7b (0.14) |
| Social support | Mean(SE) | 11.8a (0.01) | 10.9b (0.07) |
Good subjective health = Good/very good and neither good or bad. Poor = Bad/Very bad
Note: Values in the same row not sharing the same subscript are significantly different at p < .05 in the two-sided test of equality for column proportions. Tests assume equal variances.1.3
Data is weighted.
References
- Alschuler K.N., Theisen‐Goodvich M.E., Haig A.J., Geisser M.E. A comparison of the relationship between depression, perceived disability, and physical performance in persons with chronic pain. European Journal of Pain. 2008;12:757–764. doi: 10.1016/j.ejpain.2007.11.003. [DOI] [PubMed] [Google Scholar]
- Bair M.J., Robinson R.L., Katon W., Kroenke K. Depression and pain comorbidity: A literature review. Archives of Internal Medicine. 2003;163:2433–2445. doi: 10.1001/archinte.163.20.2433. [DOI] [PubMed] [Google Scholar]
- Banks S.M., Kerns R.D. Explaining high rates of depression in chronic pain: A diathesis-stress framework. Psychological Bulletin. 1996;119:95. [Google Scholar]
- Barbotte E., Guillemin F., Chau N. Prevalence of impairments, disabilities, handicaps and quality of life in the general population: A review of recent literature. Bulletin of the World Health Organization. 2001;79:1047–1055. [PMC free article] [PubMed] [Google Scholar]
- Baron R.M., Kenny D.A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bøen H., Dalgard O.S., Bjertness E. The importance of social support in the associations between psychological distress and somatic health problems and socio-economic factors among older adults living at home: A cross sectional study. BMC Geriatrics. 2012;12:27. doi: 10.1186/1471-2318-12-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell L.C., Clauw D.J., Keefe F.J. Persistent pain and depression: A biopsychosocial perspective. Biological Psychiatry. 2003;54:399–409. doi: 10.1016/s0006-3223(03)00545-6. [DOI] [PubMed] [Google Scholar]
- Chen C.-M., Mullan J., Su Y.-Y., Griffiths D., Kreis I.A., Chiu H.-C. The longitudinal relationship between depressive symptoms and disability for older adults: A population-based study. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2012;67:1059–1067. doi: 10.1093/gerona/gls074. [DOI] [PubMed] [Google Scholar]
- Christensen K., Doblhammer G., Rau R., Vaupel J.W. Ageing populations: The challenges ahead. The Lancet. 2009;374:1196–1208. doi: 10.1016/S0140-6736(09)61460-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clench-Aas J., Nes R.B., Aarø L.E. The perceived constraints subscale of the Sense of Mastery Scale: Dimensionality and measurement invariance. Quality of Life Research. 2017;26:127–138. doi: 10.1007/s11136-016-1359-6. [DOI] [PubMed] [Google Scholar]
- Courtney-Long E.A., Carroll D.D., Zhang Q.C., Stevens A.C., Griffin-Blake S., Armour B.S. Prevalence of disability and disability type among adults—United States, 2013. Morbidity and Mortality Weekly Report. 2015;64:777–783. doi: 10.15585/mmwr.mm6429a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie S.R., Wang J. Chronic back pain and major depression in the general Canadian population. Pain. 2004;107:54–60. doi: 10.1016/j.pain.2003.09.015. [DOI] [PubMed] [Google Scholar]
- Dalgard O.S., Dowrick C., Lehtinen V., Vazquez-Barquero J.L., Casey P., Wilkinson G., Dunn G. Negative life events, social support and gender difference in depression. Social psychiatry and psychiatric epidemiology. 2006;41(6):444–451. doi: 10.1007/s00127-006-0051-5. [DOI] [PubMed] [Google Scholar]
- Derogatis L.R., Lipman R.S., Rickels K., Uhlenhuth E.H., Covi L. The Hopkins Symptom Checklist (HSCL): A self‐report symptom inventory. Behavioral Science. 1974;19:1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- Dickens C., Jayson M., Sutton C., Creed F. The relationship between pain and depression in a trial using paroxetine in sufferers of chronic low back pain. Psychosomatics. 2000;41:490–499. doi: 10.1176/appi.psy.41.6.490. [DOI] [PubMed] [Google Scholar]
- Ehsan A.M., De Silva M.J. Social capital and common mental disorder: A systematic review. Journal of Epidemiology and Community Health. 2015 doi: 10.1136/jech-2015-205868. [DOI] [PubMed] [Google Scholar]
- Gazmararian J., Baker D., Parker R., Blazer D.G. A multivariate analysis of factors associated with depression: Evaluating the role of health literacy as a potential contributor. Archives of Internal Medicine. 2000;160:3307–3314. doi: 10.1001/archinte.160.21.3307. [DOI] [PubMed] [Google Scholar]
- Geerlings S.W., Twisk J.W.R., Beekman A.T.F., Deeg D.J.H., van Tilburg W. Longitudinal relationship between pain and depression in older adults: Sex, age and physical disability. Social Psychiatry and Psychiatric Epidemiology. 2002;37:23–30. doi: 10.1007/s127-002-8210-2. [DOI] [PubMed] [Google Scholar]
- Greenglass E., Fiksenbaum L., Eaton J. The relationship between coping, social support, functional disability and depression in the elderly. Anxiety, Stress, and Coping. 2006;19:15–31. [Google Scholar]
- Hayes A.F. Guilford Press; New York, NY: 2013. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. [Google Scholar]
- Jang Y., Haley W.E., Small B.J., Mortimer J.A. The role of mastery and social resources in the associations between disability and depression in later life. Gerontologist. 2002;42:807–813. doi: 10.1093/geront/42.6.807. [DOI] [PubMed] [Google Scholar]
- Jensen M.P., Moore M.R., Bockow T.B., Ehde D.M., Engel J.M. Psychosocial factors and adjustment to chronic pain in persons with physical disabilities: A systematic review. Archives of Physical Medicine Rehabilitation. 2011;92:146–160. doi: 10.1016/j.apmr.2010.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I., Berkman L.F. Social ties and mental health. Journal of Urban Health. 2001;78:458–467. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kojima M. Epidemiologic studies of psychosocial factors associated with quality of life among patients with chronic diseases in Japan. The Journal of Epidemiology. 2012;22:7–11. doi: 10.2188/jea.JE20110114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakke S.E., Wittink H., Geertzen J.H., van der Schans C.P., Reneman M.F. Factors that affect functional capacity in patients with musculoskeletal pain: A Delphi Study among scientists, clinicians, and patients. Archives of Physical Medicine Rehabilitation. 2012;93:446–457. doi: 10.1016/j.apmr.2011.10.016. [DOI] [PubMed] [Google Scholar]
- Lavikainen J., Fryers T., Lehtinen V. Stakes & EU; Helsinki: 2006. Improving mental health information in Europe: Proposal of the MINDFUL project; p. 167. [Google Scholar]
- Lee C.T., Yeh C.J., Lee M.C., Lin H.S., Chen V.C., Hsieh M.H. Social support and mobility limitation as modifiable predictors of improvement in depressive symptoms in the elderly: Results of a national longitudinal study. Archives of Gerontology Geriatrics. 2012;55:530–538. doi: 10.1016/j.archger.2012.03.002. [DOI] [PubMed] [Google Scholar]
- Lenze E.J. The association of late-life depression and anxiety with physical disability: A review of the literature and prospectus for future research. The American Journal of Geriatric Psychiatry. 2001;9:113–135. [PubMed] [Google Scholar]
- Lillegård, M. (2009). Frafallsanalyse av Levekårsundersøkelsen 2008 (Notater 2009/62) (p. 15). Statistisk Sentralbyrå.
- MacKinnon D.P., Krull J.L., Lockwood C.M. Equivalence of the mediation, confounding and suppression effect. Prevention Science: The Official Journal of the Society for Prevention Research. 2000;1:173. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy M.L., MacKenzie E.J., Edwin D., Bosse M.J., Castillo R.C., Starr A. Psychological distress associated with severe lower-limb injury. The Journal of Bone Joint Surgery. 2003;85:1689–1697. doi: 10.2106/00004623-200309000-00006. [DOI] [PubMed] [Google Scholar]
- McWilliams L.A., Cox B.J., Enns M.W. Mood and anxiety disorders associated with chronic pain: An examination in a nationally representative sample. Pain. 2003;106:127–133. doi: 10.1016/s0304-3959(03)00301-4. [DOI] [PubMed] [Google Scholar]
- Meltzer H. Developement of a common instrument for mental health. In: Nosikov A., Gudex C., editors. EUROHIS: Developing Common Instruments for Health Surveys. IOS Press; Amsterdam: 2003. pp. 35–60. [Google Scholar]
- Muramatsu N., Yin H., Hedeker D. Functional declines, social support, and mental health in the elderly: Does living in a state supportive of home and community-based services make a difference? Social Science Medicine. 2010;70:1050–1058. doi: 10.1016/j.socscimed.2009.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers D.G. The funds, friends, and faith of happy people. American Psychologist. 2000;55:56. doi: 10.1037//0003-066x.55.1.56. [DOI] [PubMed] [Google Scholar]
- Nosek M.A., Hughes R.B., Robinson-Whelen S. The complex array of antecedents of depression in women with physical disabilities: Implications for clinicians. Disability and Rehabilitation. 2008;30:174–183. doi: 10.1080/09638280701532219. [DOI] [PubMed] [Google Scholar]
- Ormel J., Rijsdijk F.V., Sullivan M., van Sonderen E., Kempen G.I. Temporal and reciprocal relationship between IADL/ADL disability and depressive symptoms in late life. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2002;57:338–347. doi: 10.1093/geronb/57.4.p338. [DOI] [PubMed] [Google Scholar]
- Osborne J.W. Best practices in using large, complex samples: The importance of using appropriate weights and design effect compensation. Practical Assessment, Research Evaluation. 2011;16:2. [Google Scholar]
- Pallant J. Open University Press; McGraw-Hill Education (UK): 2013. SPSS survival manual: A step by step guide to data analysis using SPSS. [Google Scholar]
- Parmelee P.A., Harralson T.L., Smith L.A., Schumacher H.R. Necessary and discretionary activities in knee osteoarthritis: Do they mediate the pain–depression relationship? Pain Medicine. 2007;8:449–461. doi: 10.1111/j.1526-4637.2007.00310.x. [DOI] [PubMed] [Google Scholar]
- Pearlin L.I., Schooler C. The structure of coping. Journal of Health and Social Behavior. 1978;19:2–21. [PubMed] [Google Scholar]
- Pollack M.H., Marzol P.C. Pharmacotherapeutic options in the treatment of comorbid depression and anxiety. CNS spectrums. 2000;5:23–30. doi: 10.1017/s1092852900007781. [DOI] [PubMed] [Google Scholar]
- Purdie F., Kellett S., Bickerstaffe D. Predictors of functional disability in disability welfare claimants. Journal of Occupational Rehabilitation. 2012;22:447–455. doi: 10.1007/s10926-012-9368-y. [DOI] [PubMed] [Google Scholar]
- Quesnel–Vallée A. Self-rated health: Caught in the crossfire of the quest for ‘true’ health? International Journal of Epidemiology. 2007;36(6):1161–1164. doi: 10.1093/ije/dym236. [DOI] [PubMed] [Google Scholar]
- Ramage-Morin P.L., Gilmour H. Chronic pain at ages 12–44. Health Reports. 2010;21:53–61. [PubMed] [Google Scholar]
- Raphael B., Schmolke M., Wooding S. Links between mental and physical health and illness. In: Herrman H., Saxena S., Moodie R., editors. Promoting mental health. World Health Organization; Geneva: 2005. pp. 132–147. [Google Scholar]
- Ross C.E., Mirowsky J. Handbook of the sociology of mental health. Springer; 2013. The sense of personal control: Social structural causes and emotional consequences; pp. 379–402. [Google Scholar]
- Sandanger I., Moum T., Ingebrigtsen G., Dalgard O.S., Sørensen T., Bruusgaard D. Concordance between symptom screening and diagnostic procedure: The Hopkins Symptom Checklist-25 and the Composite International Diagnostic Interview I. Social Psychiatry and Psychiatric Epidemiology. 1998;33:345–354. doi: 10.1007/s001270050064. [DOI] [PubMed] [Google Scholar]
- Schnittker J. Chronic illness and depressive symptoms in late life. Social Science Medicine. 2005;60:13–23. doi: 10.1016/j.socscimed.2004.04.020. [DOI] [PubMed] [Google Scholar]
- Scott K.M., Bruffaerts R., Tsang A., Ormel J., Alonso J., Angermeyer M.C. Depression–anxiety relationships with chronic physical conditions: Results from the World Mental Health Surveys. Journal of Affective Disorders. 2007;103:113–120. doi: 10.1016/j.jad.2007.01.015. [DOI] [PubMed] [Google Scholar]
- Shih M., Hootman J.M., Strine T.W., Chapman D.P., Brady T.J. Serious psychological distress in US adults with arthritis. Journal of General Internal Medicine. 2006;21:1160–1166. doi: 10.1111/j.1525-1497.2006.00573.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stegenga B.T., Nazareth I., Torres-Gonzales F., Xavier M., Svab I., Geerlings M.I. Depression, anxiety and physical function: Exploring the strength of causality. Journal of Epidemiology and Community Health. 2012;66:e25. doi: 10.1136/jech.2010.128371. [DOI] [PubMed] [Google Scholar]
- Strand B.H., Dalgard O.S., Tambs K., Rognerud M. Measuring the mental health status of the Norwegian population: A comparison of the instruments SCL-25, SCL-10, SCL-5 and MHI-5 (SF-36) Nordic Journal of Psychiatry. 2003;57:113–118. doi: 10.1080/08039480310000932. [DOI] [PubMed] [Google Scholar]
- Suttajit S., Punpuing S., Jirapramukpitak T., Tangchonlatip K., Darawuttimaprakorn N., Stewart R. Impairment, disability, social support and depression among older parents in rural Thailand. Psychological Medicine. 2010;40:1711–1721. doi: 10.1017/S003329170999208X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S.E., Stanton A.L. Coping resources, coping processes, and mental health. Annual Review of Clinical Psychology. 2007;3:377–401. doi: 10.1146/annurev.clinpsy.3.022806.091520. [DOI] [PubMed] [Google Scholar]
- Thoits P.A. Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior. 2011;52:145–161. doi: 10.1177/0022146510395592. [DOI] [PubMed] [Google Scholar]
- Umberson D., Montez J.K. Social relationships and health a flashpoint for health policy. Journal of Health and Social Behavior. 2010;51:S54–S66. doi: 10.1177/0022146510383501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbrugge L.M., Jette A.M. The disablement process. Social Science Medicine. 1994;38:1–14. doi: 10.1016/0277-9536(94)90294-1. [DOI] [PubMed] [Google Scholar]
- Wang Q., Jayasuriya R., Man W.Y.N., Fu H. Does functional disability mediate the pain–depression relationship in older adults with osteoarthritis? A longitudinal study in China. Asia Pacific Journal of Public Health. 2012;27:NP382–NP391. doi: 10.1177/1010539512443974. [DOI] [PubMed] [Google Scholar]
- WHO . World Health Organization; Geneva: 2011. World report on disability; p. 325. [PubMed] [Google Scholar]
- WHO . World Health Organization; 2013. Disability and health. Fact sheet no. 352. [Google Scholar]
- Williamson G.M. Extending the activity restriction model of depressed affect: Evidence from a sample of breast cancer patients. Health Psychology. 2000;19:339–347. [PubMed] [Google Scholar]
- Winokur A., Winokur D.F., Rickels K., Cox D.S. Symptoms of emotional distress in a family planning service: Stability over a four-week period. The British Journal of Psychiatry. 1984;144:395–399. doi: 10.1192/bjp.144.4.395. [DOI] [PubMed] [Google Scholar]
- Yang Y. How does functional disability affect depressive symptoms in late life? The role of perceived social support and psychological resources. Journal of Health and Social Behavior. 2006;47:355–372. doi: 10.1177/002214650604700404. [DOI] [PubMed] [Google Scholar]