Abstract
Context:
Early clinical exposure (ECE) is one of the important tools to teach basic science to the MBBS students. It is one form of vertical integration between basic science and clinical subjects. This study is an effort at exploring the use of ECE as a motivational tool toward better learning in neuroanatomy for first year MBBS students.
Aim:
This study aims to make the students interested and motivated to study neuroanatomy by using ECE as learning tool in neuroanatomy and to make the students enable to retain the knowledge of neuroanatomy more efficiently and correlate the knowledge of neuroanatomy with neuromedicine.
Settings and Design:
This study was conducted in collaboration with the Departments of Anatomy, General Medicine and Medical Education Unit in the year 2016. This was cross-sectional study.
Subjects and Methods:
One hundred and fifty students of 1st Professional MBBS were subdivided into two groups. After preliminary classes on brain, brainstem, and spinal cord for both groups, conventional lecture classes were taken for Group A only on upper motor neuron (UMN) and lower motor neuron (LMN) paralysis, and only Group B visited General Medicine ward where HOD, General Medicine showed and examined patients of UMN paralysis and LMN paralysis, elicited different symptoms, and discussed different investigation. It was followed by assessment of all by problem-based multiple choice questions (MCQ) and short answer questions. Then, Group B attended lecture class on different cranial nerve palsy whereas Group A visited medicine ward. It was followed by assessment of both groups by problem-based MCQ and short answer questions. The performance was compared. Then, the feedback of the students on ECE was collected by means of reflection writing followed by administration of questionnaire. Then, the perception of teachers regarding ECE was recorded by focused group discussion.
Statistical Analysis Used:
Student's t-test was used to compare the performance of both batches. Reflection writing and focus group discussion were analyzed qualitatively.
Results:
There was a significant difference in Group A (P = 0.019) but no significant difference in Group B (P = 0.679). All the teachers opined that ECE was an efficient method but more time and interdepartmental collaboration were necessary.
Conclusions:
Group A improved performance due to ECE but Group B maintained the motivational effect of it. Therefore, ECE can be used as an effective learning tool.
Keywords: Correlate, early clinical exposure, learning tool, neuroanatomy
Introduction
In the present setup of undergraduate medical curriculum, the MBBS students are exposed to the clinical setup beginning from the second year onward. Therefore, in the first year immediately after the admission to the MBBS course, the students are exposed to the theory as well as practical classes of basic sciences involving discipline based didactic lectures. It is teacher centered and examination oriented with emphasis on memorization of facts and figures. Hence, there is neither the scope for correlating the knowledge of basic sciences with clinical experience nor they become familiar with the hospital environment during the first year of MBBS. Anatomy is one of the basic sciences taught in the first year. It is very dry and monotonous subject to many freshmen due to its vast and complex syllabus covered in the limited time span of 8–9 months.[1] Again the assessment what is usually practiced, based on the knowledge-domain of Miller's pyramid. As a consequence, students are not able to recollect the basic relevant knowledge of anatomy which should be effectively applied to the clinical situations during their clinical posting in wards specifically during 3rd Prof Part–I and 3rd Prof Part-II MBBS courses.[2,3,4] Hence, in the 1st year of MBBS, the teaching sometimes becomes spoon-fed instead of the self-directed approach.
To improve this scenario, it has become necessary to introduce the students to clinical problems in the first undergraduate year itself. Early clinical exposure (ECE) was one of the important elements as recommended by “Revised Regulations for Graduate Medical Education 2012” with the objectives to enable the students to “recognize the relevance of basic sciences in patient care and relate to experience of patients as a motivation to learn.”[5] ECE can be helpful not only for better retention of knowledge due to integrated knowledge of basic sciences but also make the learners motivated and more interested in the basic sciences and may elevate the level of self-confidence. ECE also promotes self-directed learning and analytical skills in students and ensures professional identity.[1] Hence, anatomy will be better understood, retained, and later practically applied if learnt in a clinically significant setup.
This study was done with several objectives; the most important among them was to make the students interested in neuroanatomy learning. Other significant objectives were to compare the performance of the students in neuroanatomy with and without clinical exposure and to assess the feedback of the students regarding ECE. To analyze the perception of teachers of anatomy and general medicine regarding ECE was another vital objective of the study.
Subjects and Methods
This study was conducted in collaboration with the Departments of Anatomy, General Medicine, and Medical Education Unit in the year 2016. This was cross-sectional study. After getting approval from the Institutional Ethics Committee, core group member was trained and sensitized regarding the ECE and a module was prepared. The 150 students of 1st Prof. MBBS of the session 2015–2016 were subdivided into two Groups A and B of 75 each according to Roll number. Each of the group was subdivided into 3 batches (A1, A2, A3 and B1, B2, B3 – each composed of 25 students). After preliminary classes on brain, brainstem, and spinal cord, conventional lecture classes were taken for Group A on upper motor neuron (UMN) paralysis and lower motor neuron (LMN) paralysis in the Department of Anatomy by the teachers of anatomy, and Group B visited General Medicine ward where HOD, General Medicine showed and examined patients of UMN paralysis and LMN paralysis, elicited different symptoms, and discussed different investigation findings such as CT scan. Three classes were arranged for each batch spread over three weeks. Hence, each of the six batches had one class in one week for consecutive 3 weeks. Each class was for 1 h. It was followed by assessment of all the students by problem-based multiple choice questions (MCQ) and short answer question. Then, the groups were reversed, i.e., Group A attended the clinical classes in general medicine ward and Group B attended the conventional classes in anatomy department. The time distribution was the same. The topics were different cranial nerve palsy like 3rd, 4th, 6th, 5th, 7th, and 10th cranial nerve palsy. It was followed by assessment of both the groups with the help of problem-based MCQ and short answer questions. The performance of the same student with ECE was compared to that without ECE by paired t-test. Then, the feedback of the students on ECE was collected by means of reflection writing followed by administration of pretested, prevail dated questionnaire. The feedback was analyzed qualitatively. Then, the perception of the seven teachers (4 anatomy teachers and 3 general medicine teachers) regarding ECE was recorded by focus group discussion (FGD) and analyzed qualitatively.
Results
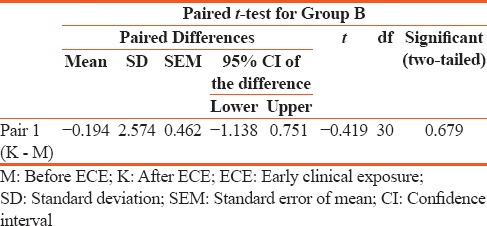
There was an interesting finding while comparing the performance of the same student of the same group with or without clinical exposure using paired t-test using SPSS version 20. There was a significant difference of performance of students of Group A (P = 0.019), but no significant difference was there among students of Group B (P = 0.679) [Tables 1 and 2].
Table 1.
Comparison of performance of students of Group A before and after early clinical exposure
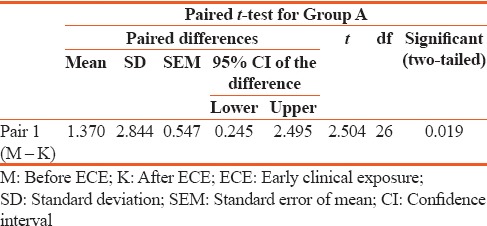
Table 2.
Comparison of performance of students of Group B before and after early clinical exposure
There was an initial sensitization program on reflection writing for students. Out of 150 students, 95 submitted reflection writing. About 63.33% was the response rate. About 48.64% commented that elicitation of characteristic symptom was the “Aha moment.” Nearly, 32.43% informed that their first experience for clinical exposure as medical student was the “Aha moment” for them [Figure 1].
Figure 1.
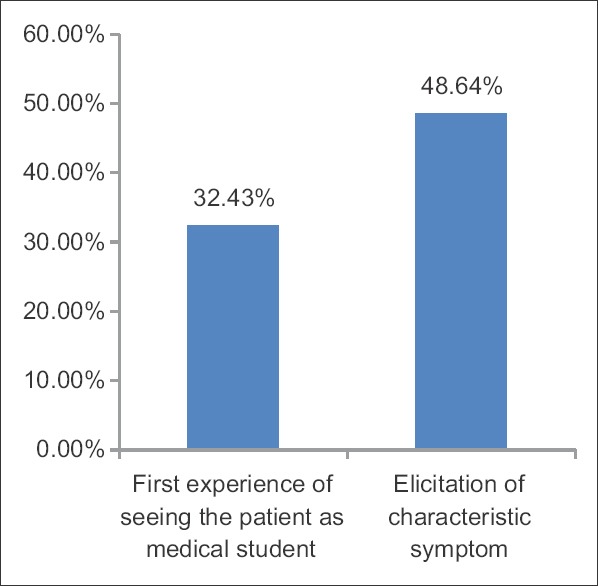
Reflection writing “Aha moment”
Nearly, 51.35% students expressed their opinion that ECE helped in correlation of their theory knowledge with practical experience. About 54.05% students told that ECE would result in easier and longer retention of book knowledge. About 37.83% students informed that ECE is helpful for better understanding of the concept in depth [Figure 2].
Figure 2.
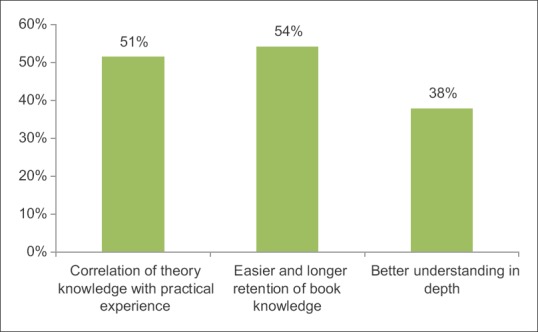
Reflection writing “so what?”
As a result of ECE, 27.02% students felt motivated as they told that they needed to study hard to be a good doctor in future. About 16.21% wanted more such clinical experience. Nearly, 24.32% reflected that they became interested in neuroanatomy. About 2.07% opined that integrated teaching is not necessary and 54.05% students realized the importance of neuroanatomy [Figure 3].
Figure 3.
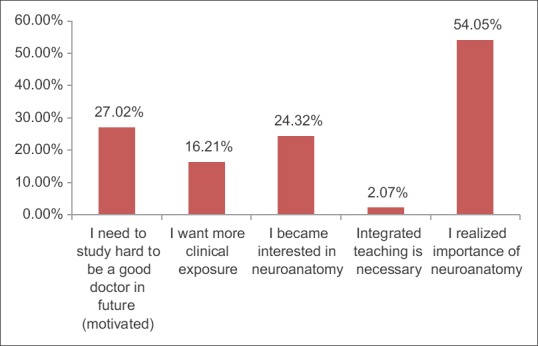
Reflection writing “What next?”
In the questionnaire, there were 8 close-ended questions on 5-point Likert scale (1 = strongly disagree, 5 = strongly agree) and one close-ended question on overall rating of ECE (1 = poor, 5 = excellent). Hundred and thirty-seven students submitted anonymous questionnaire. Response rate was 91.33%. However, 87.6% rated ECE in neuroanatomy as excellent, 9.3% rated it as good, and 3.1% rated it as satisfactory. The questionnaire is given in Table 3.
Table 3.
Students’ Questionnaire
In FGD, all the teachers agreed that ECE increases the motivation, improves retention of knowledge, and helped in correlation of theory knowledge with practical experience. However, the teachers especially those of anatomy expressed that it is difficult to arrange ECE for each and every topic due to huge syllabus and time constraint. The teachers of general medicine informed that it is difficult to get the sensitized teachers to take ECE classes after disbursing so many responsibilities. It was also evident from FGD that it required good collaboration between the departments and training of the faculty members to some extent.
Discussion
In the present study, paired t-test showed that the performance of the students has been significantly improved after ECE among the students in the Group A reflecting that ECE is important to increase their interest in neuroanatomy. However, in Group B students of which were exposed to ECE initially followed by traditional class were also successful to maintain their performance even after traditional class due to the sustained inspiring effect of ECE. ECE was helpful to motivate them to read neuroanatomy resulting into no significant difference of performance in the latter group even after traditional class (Group B). A study done by Tayade et al. in 2014 showed significant difference between ECE and non-ECE groups.[6]
In different studies, ECE has been suggested to motivate the medical freshmen to develop a better insight.[3,7,8,9,10,11,12,13,14] ECE enables medical students to obtain a better and deeper understanding of medicinal theory and practice through the application of their knowledge in real hospital situations.[9]
One previous study showed that early clinical experience called for more attention to the importance of basic sciences and increased the students’ interest in studying basic sciences.[3]
Similar to the present study, other studies also concluded that ECE is a time-consuming method and cannot be applied to each topic of gross anatomy as tenure of first MBBS is only one year and three basic subjects have to be covered. Hence, although it is a very effective teaching–learning method, it cannot replace the lectures. To increase its efficacy, there should be a hybrid method, whereby the entire syllabus is not covered, but ECE is used only for a few important and common conditions.[1,15]
Another challenge that can be encountered during ECE implementation is identifying and coordinating with supportive clinical departments and cooperative patients.[16] ECE consumes more workforce, infrastructure, and extra efforts on the part of the faculty which is another drawback.
Conclusion
To conclude, ECE though challenging, is a way to motivate the students and help in better retention of the knowledge.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
I want to acknowledge Dr. TejinderSingh, Dr. Dinesh Badyal, Dr. Sarabmeet Singh Lehl, and Dr. Sukhinder Baidwan for their inspiration and Dr. Dipanjan Bandyopadhyay and Dr. Samir Chandra Ghosh Roy for their constant support without which it was not possible to accomplish this.
References
- 1.Chari S, Gupta M, Gade S. The early clinical exposure experience motivates first year MBBS students: A study. Int J Educ Sci. 2015;8:403–5. [Google Scholar]
- 2.Patel V, Patel PR. MCI regulations on graduate medical education 2012 – Are we ready for paradigm shift? NHL J Med Sci. 2012;1:5–6. [Google Scholar]
- 3.Prithishkumar IJ, Holla SJ. Early clinical exposure as a teaching learning tool to teach neuroanatomy for first year occupational and physical therapy students – Our preliminary experience. Indian J Physiother Occup Ther Int J. 2012;6:59–62. [Google Scholar]
- 4.Sathishkumar S, Thomas N, Tharion E, Neelakantan N, Vyas R. Attitude of medical students towards Early Clinical Exposure in learning endocrine physiology. BMC Med Educ. 2007;7:30. doi: 10.1186/1472-6920-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sawant SP, Rizvi S. Importance of early clinical exposure in learning anatomy. Scholars J Appl Med Sci. 2015;3:1035–8. [Google Scholar]
- 6.Tayade MC, Bhimani N, Kulkarni NB, Dandekar KN. The impact of early clinical exposure on first M.B.B.S. students. Int J Healthc Biomed Res. 2014;2:176–81. [Google Scholar]
- 7.Dornan T, Bundy C. What can experience add to early medical education? Consensus survey. BMJ. 2004;329:834. doi: 10.1136/bmj.329.7470.834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Littlewood S, Ypinazar V, Margolis SA, Scherpbier A, Spencer J, Dornan T, et al. Early practical experience and the social responsiveness of clinical education: Systematic review. BMJ. 2005;331:387–91. doi: 10.1136/bmj.331.7513.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chisholm MA, William E. Using actual patients in the classroom to develop positive student attitudes toward pharmaceutical care. Am J Pharm Educ. 1999;63:296–9. [Google Scholar]
- 10.Abramovitch H, Shenkman L, Schlank E, Shoham S, Borkan J. A tale of two exposures: A comparison of two approaches to early clinical exposure. Educ Health (Abingdon) 2002;15:386–90. doi: 10.1080/1357628021000012732. [DOI] [PubMed] [Google Scholar]
- 11.Wartman S, Davis A, Wilson M, Kahn N, Sherwood R, Nowalk A, et al. Curricular change: Recommendations from a national perspective. Acad Med. 2001;76:S140–5. doi: 10.1097/00001888-200104001-00028. [DOI] [PubMed] [Google Scholar]
- 12.Verma M. Early clinical exposure: New paradigm in medical and dental education. Contemp Clin Dent. 2016;7:287–8. doi: 10.4103/0976-237X.188536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Das P, Biswas S, Singh R, Mukherjee S, Ghoshal S, Pramanik D, et al. Effectiveness of early clinical exposure in learning respiratory physiology among the newly entrant MBBS students. J Adv Med Educ Prof. 2017;5:6–10. [PMC free article] [PubMed] [Google Scholar]
- 14.Johnson AK, Scott CS. Relationship between early clinical exposure and first-year students’ attitudes toward medical education. Acad Med. 1998;73:430–2. doi: 10.1097/00001888-199804000-00018. [DOI] [PubMed] [Google Scholar]
- 15.Satheesha N, Komattil R, Nagabhooshana S, Kuvady LB. Teaching anatomy in a problem-based learning (PBL) curriculum. Neuroanatomy. 2006;5:2–3. [Google Scholar]
- 16.Vernon DT. Attitudes and opinions of faculty tutors about problem-based learning. Acad Med. 1995;70:216–23. doi: 10.1097/00001888-199503000-00013. [DOI] [PubMed] [Google Scholar]


