Abstract
Background:
Microbiology is usually taught by conventional lectures, and its retention and application is observed to be poor among medical graduates/practitioners.
Aim and Objectives:
Introduction of case-based learning (CBL) in microbiology for second-year professional MBBS students.
Materials and Methods:
Students were divided into two groups of fifty each. Four clinical cases were used for CBL. One group had two CBL sessions whereas the other had didactic lectures (DLs) and then the groups were crossed over. Case scenario handouts were given to students a week before the session, and smaller groups were formed for discussions and presentations in CBL sessions. Posttest, in multiple choice questions format, was conducted in two phases: First, immediately after the completion of the four CBL and DL sessions, and second, 6 weeks after the first posttest. Student and faculty feedback was taken about CBL sessions.
Results:
Hundred MBBS students of the fourth semester voluntarily participated in the CBL study. The CBL scores were significantly higher than DL session scores (P = 0.015). This difference was more marked in scoring done after 6 weeks of session completion (P < 0.001). Student reported satisfaction in being taught by CBL method in 5-point Likert scale feedback form. Faculty feedback was positive for CBL.
Conclusions:
CBL helped in retention of knowledge and its application better than DL in our observation. More sessions on commonly encountered case scenarios will be useful for students in recalling basic science knowledge in their later years as practitioners.
Keywords: Active learning, case-based learning, didactic lectures, microbiology
Introduction
Medical educators are concerned about the conventional methods of teaching not providing a required impact on student learning.[1] The first 2½ years of medical study are devoted to basic sciences program where most educators place little or no emphasis on how the knowledge or skills will be applicable or useful in subjects taught at a later stage. Many students from the higher classes have stated that basic sciences curricula are theoretically overloaded, that they could recall less information, and that curricula were less applicable to clinical practice. In the absence of such teaching environment, students are more concentrated on gaining good marks, rather than focusing on how the basic science information could be applied in clinical scenarios. Similar to the above trend, the teaching of microbiology is mainly through conventional lectures and it has been observed that there is inadequate retention of microbiology and its unappropriate application to clinical science among medical graduates or practitioners. This is evident from the inappropriate sampling and irrational demands for rapid reporting by clinicians, as experienced by authors in their setup.
Active learning is required to facilitate student's learning. An environment requiring students to actively engage with the subject to generate knowledge rather than just receiving it passively through didactic lectures (DLs) needs to be created.[2,3,4,5] This form of learning creates stronger memory channels for the student to draw upon as they are actively engaged in applying their own knowledge and experiences.[1,2,6]
Thus, over the past two decades, there has been a paradigm shift in medical education with one method being inducing the students to process and apply the knowledge in clinical settings or scenarios. The medical educators seek to transform the traditional passive note-taking and rote study methods into a more active and interactive learning environment where students develop critical and analytical thinking skills and are more easily able to memorize information.[1,2,7,8]
Case-based learning (CBL) is one such method of active learning strategy involving an exploration of real-life case scenarios for an interactive student-centered pedagogy.[2,5] CBL is somewhat characteristically similar to the problem-based learning. Cases used in CBL are real-life situations that provide the student with the history and symptoms of a patient along with clinical signs and the laboratory investigation data. Students interact with each other and work together as a group to solve the case with the instructor acting as facilitator.[2,5,8] CBL approach to teaching requires faculty training and development for its effective implementation.[1]
The present study aimed to assess the effectiveness of CBL in retention of knowledge in medical microbiology and the perception of medical students and faculty for CBL.
Materials and Methods
The project was carried out with the MBBS second professional students (Paraclinical year; IV Semester; 2014 Batch) of a North West Indian Medical College after permission from the Institutional Ethics Committee. Hundred students voluntarily participated in the study. The participants were divided into two groups – Group 1 and 2, of 50 students each, using chit method. All the students were sensitized about group dynamics using an activity to explain and reinforce the points. Five faculty members from the Department of Microbiology were sensitized and trained for group dynamics and CBL.
Four clinical cases were prepared for the CBL sessions, two for each group. The topics covered in the clinical cases were Staphylococcus aureus, Group A Streptococci, Enterococcus, and hepatitis A virus. These cases were discussed with the faculty and questions for discussion during CBL session were finalized and validated. Group 1 had two CBL sessions whereas Group 2 had DLs on the same topics. After two sessions, the groups were crossed over. Group 1 had two CBL sessions followed by two DLs for the next two topics whereas Group 2 had two DLs on the first two topics followed by the CBL sessions for the next two topics. Figure 1 shows the flowchart of the methodology for conducting the CBL and didactic sessions for the two groups followed by feedback and posttest in two rounds. Each student of the group was given handout with the clinical case scenario a week before the session and asked to study about the case. CBL sessions were conducted in demonstration room and each lasted for 90 min. During the CBL session, the students were divided into five subgroups of ten students each. Each subgroup was seated around a table and provided with chart paper and color pens. Group dynamics were followed to discuss the case in the subgroups and present answers to questions on the clinical case in the main group. The faculty acted as facilitators and observers.
Figure 1.
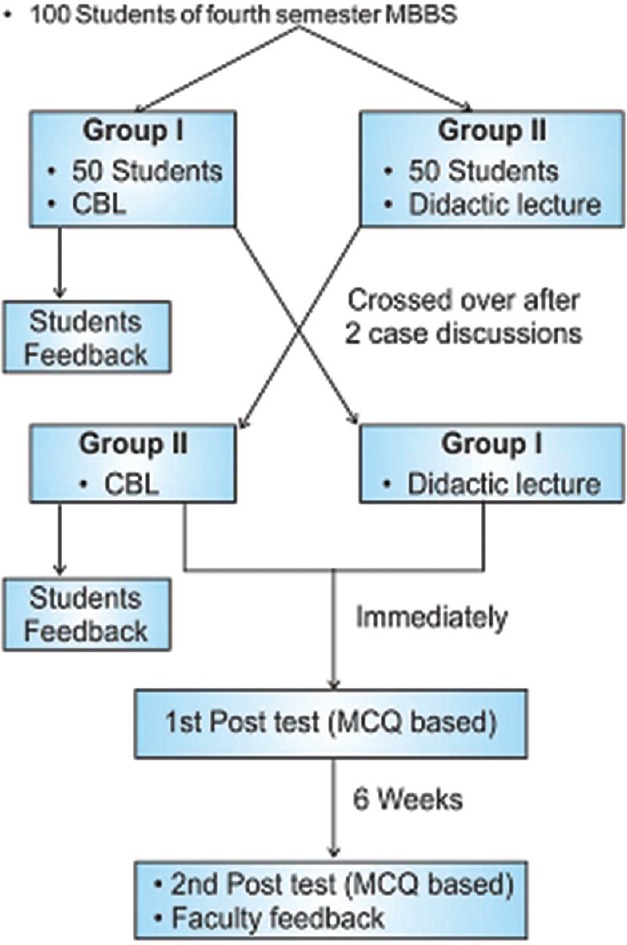
Flowchart of methodology
Feedback questionnaires for students and faculty were designed, validated, and pretested with colleagues and students from the previous batch. The students’ feedback form had two parts: (a) The first part was of twenty closed-ended questions with 5-point Likert scale to assess attitude towards CBL. (b) The second part had two open-ended questions regarding problems faced and suggestions on CBL sessions. Feedback was taken from students of each group after the completion of the two CBL sessions scheduled for their group.
The Faculty feedback was taken after 6 weeks of CBL sessions. The questionnaire had ten closed-ended questions with 5-point Likert scale response to assess the faculty perception of impact of CBL on student's knowledge retention, clinical reasoning, and peer interaction. One question was negative. There were two open-ended questions for suggestions on improvement and for getting an insight into implementation problems faced.
Posttest was conducted for the entire group of 100 students immediately after the four CBL and DL sessions were completed, and then a repeat test was taken after 6 weeks duration from the first posttest. The posttest was in multiple choice questions format with total twenty questions including randomly placed five questions on each of the four organisms included in the study. Based on the organism covered during CBL and DL for each individual, the posttest marks were divided into two categories (CBL and DL) of ten marks each for comparison between the two posttests.
Statistical analysis
Qualitative data were expressed in percentages, and quantitative data were expressed in the form of mean ± standard deviation and significance of difference assessed by t-test. Statistical significance was tested at 5% and expressed in terms of P value with P < 0.05 was considered statistically significant.
Observations and Results
A total of 100 students of the IV semester (Batch 2014) participated voluntarily in the study. The group included 63 girls and 37 boys.
On comparison, the class scores were highest for the CBL sessions than DLs sessions in both the tests: one taken immediately after the sessions and second taken at an interval of 6 weeks after the completion of sessions. The difference in the score of the two methods was found to be statistically significant. The difference in scores was greater in test taken after 6 weeks interval (P < 0.001) [Table 1].
Table 1.
Comparison between test marks of didactic lecture and case-based learning sessions
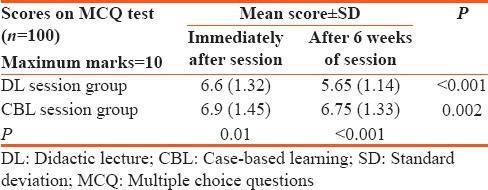
It was further observed that there was a decrease in the mean score of both the groups over time, but the decrease was significantly higher in the DL group than the CBL group [Table 1].
In evaluation immediately after the sessions, none of the students scored <3 marks, whereas, after a period of 6 weeks, one person in the DL group scored <3 marks out of 10 [Figure 2]. It is apparent from Figure 2 that, after an interval of 6 weeks, the scores in didactic session were much lower than the CBL sessions.
Figure 2.
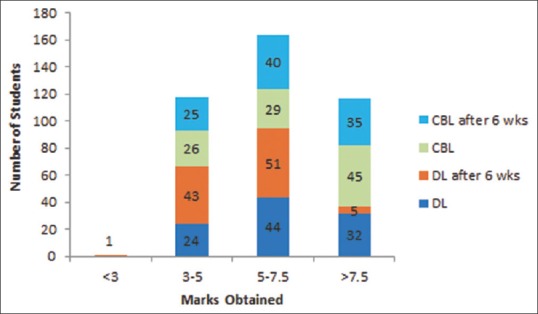
Comparison of marks obtained by number students in case-based learning versus didactic lecture
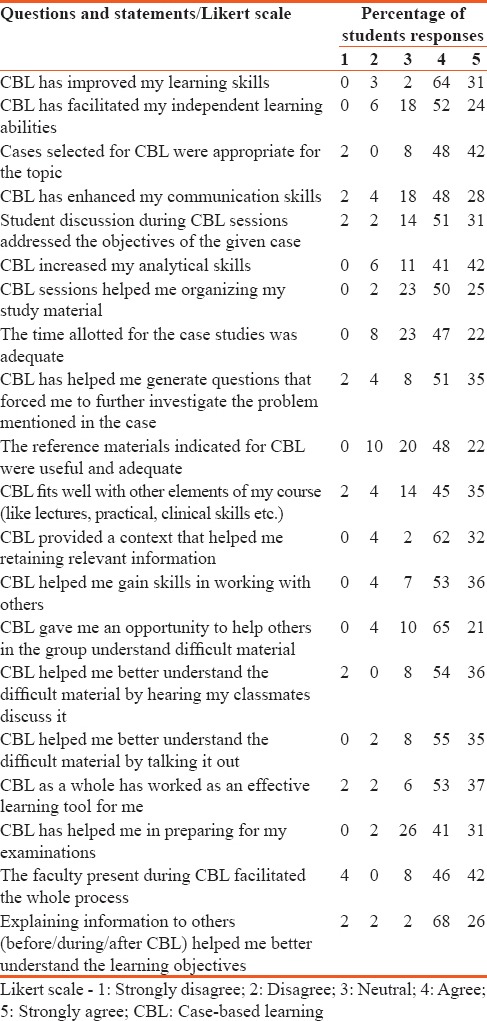
Most students reported satisfaction with the CBL sessions and liked this method of teaching microbiology. The median and mode score was 4 for all the twenty closed-ended 5-point Likert scale-based feedback questions. Students found an improvement in learning, analytical, interaction, and communication skills [Table 2]. Students also requested for more such sessions on a regular basis and to continue such method of teaching and interaction in the other semesters also. The students also commented that if more time was given for each session, they could have interacted more. They even suggested more resource material to be provided for the sessions.
Table 2.
Responses by the students on case-based learning on a 5 point Likert scale
Faculty feedback analysis showed that they observed an increase in interest (100%), retention of knowledge (100%), clinical reasoning abilities (80%), and interaction (40%) in students. The idea that CBL only imparts factual knowledge was refuted by four (80%) of the faculty, whereas one faculty was neutral about it. All stated that the cases were appropriate for the topic and well prepared but felt more time was required for sessions. Faculty found the method effective but more labor intensive.
Discussion
Medical science is a field where students are required to recall a lot of knowledge and skills learned during their medical school and also to keep updating that knowledge with the latest research and technology. Medical schools around the globe are adopting various interactive teaching methods to enhance learning and retention and to inculcate self-directed learning skills in medical students. However, the medical schools in this part of India are still following the conventional approach though some schools have started experimental implementation of interactive teaching methods for active learning to see the effect so that they can be adopted as a part of the curriculum.
On a similar theme, the present study was conducted in the Microbiology Department of a North West Indian Medical College for the fourth-semester students of MBBS to evaluate effectiveness of CBL as a tool for teaching microbiology and perception of student and faculty for CBL.
In the present study, it was observed that the learning by CBL method was significantly higher than the DL method (P = 0.01). Similar observations have been reported by Tathe and Singh, Chamberlain et al., and Blewett and Kisamor.[5,9,10]
The retention of knowledge as assessed by a posttest after 6 weeks was higher in CBL group than in DL group in the present study. This observation is similar to that reported by Ciraj et al., who observed better performance in CBL blocks and better scores overall, and Chamberlain et al.[2,9]
Student feedback was positive for CBL by most of the students. The median and mode on Likert scale feedback were 4 indicating most students “agreed” with the positive impact of CBL. In the present study, most students agreed that CBL was an effective learning tool, enhanced their learning skills and analytical skills, motivated for independent learning, and improved their communication skills. Similar findings have been reported by various studies from different parts of the country and from different specialties of medical schools’ teaching undergraduate students.[1,2,4,5,8,9,10,11,12,13,14] Students agreed that CBL was able to achieve the learning objectives of the topics covered in the present study. Similar observations have been reported by other authors too.[2,5]
Faculty, who were the facilitators for the CBL sessions, in their feedback said in unison that the cases were appropriate for the topic and well prepared. All faculties opined that the orientation for CBL conduction facilitated them for the sessions as observed by Gade and Charitoo.[14] Increased retention of knowledge and interest in microbiology by CBL sessions was observed by all the faculty similar to observations by other authors.[2,12] Faculty also observed enhanced clinical reasoning, better peer interactions, and communication skills in students in the present study and this has been reported by other authors too.[2,12,14]
CBL is a useful tool to bring about a change in the way a student approaches a clinical case scenario and uses the knowledge from basic sciences in clinical practice. It also develops the learning interest in students beyond the regular textbooks to tackle the cases. While a study by Ciraj et al. at Manipal reported a changed approach to the curriculum with division into blocks based on systems to effectively use CBL for teaching, such a complete change shall take many small gradual steps at most of the other institutes such as ours.[2] CBL will also lead to more interaction between students and faculty, thereby leading to more learning and more amicable atmosphere. Although CBL requires more efforts both from faculty and students, the end results are worth the extra effort put into it.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Hashim R, Azam N, Shafi M, Majeed S, Ali S. Perceptions of undergraduate medical students regarding case based learning and tutorial format. J Pak Med Assoc. 2015;65:1050–5. [PubMed] [Google Scholar]
- 2.Ciraj AM, Vinod P, Ramnarayan K. Enhancing active learning in microbiology through case based learning: Experiences from an Indian medical school. Indian J Pathol Microbiol. 2010;53:729–33. doi: 10.4103/0377-4929.72058. [DOI] [PubMed] [Google Scholar]
- 3.Armbruster P, Patel M, Johnson E, Weiss M. Active learning and student-centered pedagogy improve student attitudes and performance in introductory biology. CBE Life Sci Educ. 2009;8:203–13. doi: 10.1187/cbe.09-03-0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chan WP, Hsu CY, Hong CY. Innovative “Case-based integrated teaching” in an undergraduate medical curriculum: Development and teachers’ and students’ responses. Ann Acad Med Singapore. 2008;37:952–6. [PubMed] [Google Scholar]
- 5.Tathe SS, Singh AL. Case based lectures versus conventional lectures for teaching Medical Microbiology to undergraduate students. Int J Cur Res Rev. 2014;6:35–41. [Google Scholar]
- 6.Gülpinar MA, Yeǧen BC. Interactive lecturing for meaningful learning in large groups. Med Teach. 2005;27:590–4. doi: 10.1080/01421590500136139. [DOI] [PubMed] [Google Scholar]
- 7.Ghosh S. Combination of didactic lectures and case oriented problem solving tutorials towards better learning: Perceptions of students from a conventional medical curriculum. Adv Physiol Educ. 2007;31:193–7. doi: 10.1152/advan.00040.2006. [DOI] [PubMed] [Google Scholar]
- 8.Sharma N, Choudhary R. Evaluation of acceptance for case based learning in the undergraduate medical curriculum. Sch J Appl Med Sci. 2015;3:2365–8. [Google Scholar]
- 9.Chamberlain NR, Stuart MK, Singh VK, Sargentini NJ. Utilization of case presentations in medical microbiology to enhance relevance of basic science for medical students. Med Educ Online. 2012;17:15943. doi: 10.3402/meo.v17i0.15943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blewett EL, Kisamore JL. Evaluation of an interactive, case-based review session in teaching medical microbiology. BMC Med Educ. 2009;9:56. doi: 10.1186/1472-6920-9-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fatima N, Shameem M, Nabeela, Khan HM. Evaluation of case based lectures for teaching medical microbiology. Int Res J Eng Technol. 2015;2:272–5. [Google Scholar]
- 12.Singh PR, Bhatt R. Introduction of Case based learning for teaching anatomy in a conventional medical school. J Anat Soc India. 2011;60:232–5. [Google Scholar]
- 13.Nair SP, Shah T, Seth S, Pandit N, Shah GV. Case based learning: A method for better understanding of biochemistry in medical students. J Clin Diagn Res. 2013;7:1576–8. doi: 10.7860/JCDR/2013/5795.3212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gade S, Chari S. Case-based learning in endocrine physiology: An approach toward self-directed learning and the development of soft skills in medical students. Adv Physiol Educ. 2013;37:356–60. doi: 10.1152/advan.00076.2012. [DOI] [PubMed] [Google Scholar]


