Abstract
Background:
Embryo donation, as one of the novel assisted reproductive technologies (ART), has remained a controversial issue. This is due to this methods' need for individuals from outside the family circle. Their presence can cause many ethical issues and complicate the designing and planning of the embryo donation process. The present study was conducted with the aim to assess the ethical challenges of embryo donation from the view point of embryo donors and recipients.
Material and Methods:
This descriptive, cross-sectional study was conducted on 192 couples (96 embryo donators and 96 embryo recipients) referring to Isfahan Fertility and Infertility Center and Royan Institute, Iran. The subjects were selected through convenience sampling. The data collection tool was the researcher-made Ethical Challenges Questionnaire. Data were analyzed in SPSS software.
Results:
Embryo donors and recipients expresses the most important ethical challenges of embryo donation in the principle of justice (70.20%) and respect for autonomy (42.57%), respectively.
Conclusions:
The four ethical principles are important in the view of embryo donors and recipients; however, they highlighted the importance of the principle of respect for autonomy considering the existing barriers in the services of infertility centers. Legislators and relevant authorities must take measures toward the development of guidelines for this treatment method in the framework of ethics principles and incorporate all four principles independently.
Keywords: Assisted reproductive technology, embryo donation, embryo donor, embryo recipient, ethics
Introduction
In the current decade, there has been widespread utilization of assisted reproductive technology (ART), such as embryo donation, which is used in the absence of sperm or healthy eggs, the possibility of transmission of a genetic disease to the next generation,[1,2,3] and a history of failed in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI).[4] With the birth of the first IVF infant in 1978, many ethical issues regarding its consequences for individuals, society, and nature[5] were put forward. Due to the rapid growth of ART and the necessity for frequent evaluation of professional and social organizations, some ethical and legal questions have remained unresolved.[1] Countries such as Sweden, Russia, and Holland have attempted to reduce the proposed ethical issues;[6] however, embryo donation has remained a controversial topic.[1] The views of embryo donors and recipients can complicate the designing and planning of the embryo donation process[7,8] and social and ethical complications regarding embryo donation require the determination of its complete meaning from the view of donors and recipients.[9] The results of previous studies on the attitudes of donor and recipient couples during the embryo donation process have shown that anonymity of the donor and confidence in sharing genetic's history and couples' personality characteristics are more important than physical characteristics, screening tests,[10] the possibility of future contact with the child, and received fee.[11] The attitude of embryo donors and recipients can be a foundation for the development of policy-making and decision-making regarding this program.[7]
Despite the passage of two decades since the first embryo donation in Iran and the referral of infertile couples from other countries to Iran,[3] new population policies and greater attention to this topic and individuals' attitudes toward the ethical issues of embryo donation are of grave importance. Thus, the present study was conducted with the aim to evaluate the ethical challenges of embryo donation from the view point of embryo donors and recipients.
Material and Methods
This descriptive, cross-sectional study was conducted on 192 couples (96 embryo donators and 96 embryo recipients) referring to Isfahan Fertility and Infertility Center and Royan Institute, Iran in 2015. The subjects were selected through convenience sampling from among individuals who had the study inclusion criteria. The inclusion criteria consisted of having a medical record at one of the centers as an embryo donor or recipient and willing to participate in the study. The data collection tool was a researcher-made questionnaire derived from the four medical ethics principles (principles of respect for autonomy, nonmaleficence, beneficence, and justice). It contained 33 questions for embryo donors and 39 questions for embryo recipients. The validity and reliability of the questionnaire were, respectively, approved by 15 professors and faculty members of the School of Nursing and Midwifery and Cronbach's alpha (the donor scale: 0.91; the recipient scale: 0.81). The questionnaire was completed by the subjects at the time of referral to Isfahan Fertility and Infertility Center and Royan Institute, and after the researcher obtained informed consent from the subjects and insured them of the confidentiality of data. The sample volume was calculated with using equation Z2S2/d2 and the consideration of 95% CI (Z = 1.96).
The questionnaire was scored based on the importance of each item in the viewpoint of donors and recipients based on a 5-point Likert scale (very little: 1 point; very much: 5 points). Results are presented as mean and percentage in each medical ethics principle in the two groups of donors and recipients. Data were analyzed using mean and standard deviation, and Pearson correlation tests in SPSS (The Statistical Package for the Social Sciences)software (version 16, SPSS Inc., Chicago, IL, USA).
Ethical considerations
This study was approved by the Ethics Committee of Isfahan University of Medical Sciences, Iran, and was derived from research project number 394459. Moreover, written informed consent forms were obtained from all participants in this study.
Results
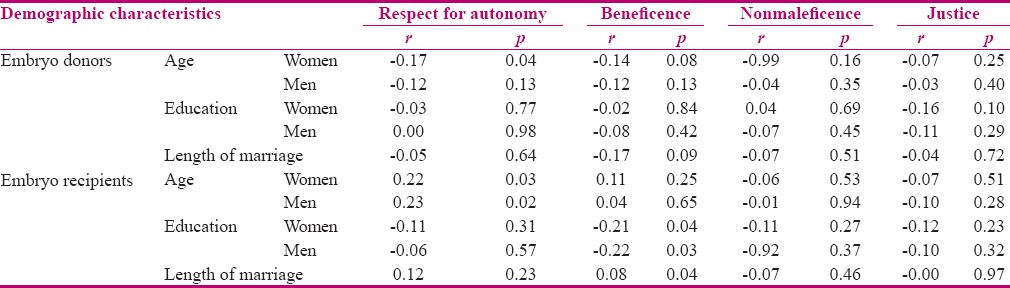
The mean (SD) age of the female and male embryo donors was 28 (4.35) and 32 (4.57) years, respectively. The majority of women (57.30%) had secondary education. In addition, 87.50% of women were homemakers. Most men had elementary education and were self-employed (50% and 54.2%, respectively). The mean age of female and male embryo recipients was 36 (5.4) and 40 (6.64) years, respectively. Most female embryo recipients had secondary education and were homemakers (39.60% and 78.11%, respectively). The majority of male embryo recipients (32.33%) had secondary education. Moreover, 54.20% of male embryo recipients were self-employed. Mean number of embryo transfers in embryo recipients was two times and the most common cause of infertility was the male factor (86.6%). The different aspects of ethical challenges of embryo donation from the point of view of donors and recipients are presented in Table 1 and the relationship of some related factors with these challenges in the couples are presented in Table 2.
Table 1.
Mean ethical challenges scores of embryo donation in embryo donors and recipients
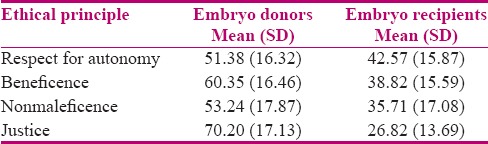
Table 2.
The relationship of the demographic characteristics of embryo donors and recipients with mean score of ethical challenges
Discussion
In the present study, couples referring to Isfahan Fertility and Infertility Center and Royan Institute for embryo transfer were evaluated. The evaluation of embryo recipients showed that most women were homemakers and most men were self-employed and had secondary education. The most common cause of their referral was male factor infertility (86.6%). In the study by Isaksson et al., most egg and sperm recipients were employed and had university education.[12] Donated eggs had been used in cases with female factor infertility and donated sperm in cases with male factor infertility.[12] This was not in agreement with the present study. Today, sperm donation is the only treatment approach for male factor infertility.[13] However, in Iran, due to religious barriers, different views of Islamic jurists regarding the incompatibility of sperm donation with the Sharia law,[14] and lack of a comprehensive law in this regard, embryo donation is the only acceptable solution to male factor infertility in Iran and has religious credibility.
Regarding the ethical challenges of embryo donation from the views of donors, the results showed that there were more ethical challenges in the field of justice compared to other ethical fields. Svanberg et al.[15] Bay et al.[16] and Gurtin et al.[17] reported that the majority of donors desired to be informed of the results of the embryo transfer and the number of offspring. Access to genetic origins and the possibility of future communication with the offspring are essential to them. Furthermore, most donors preferred that the recipient was an acquaintance[15,17] and to disclose the donation process to relatives and disclosure and openness of the embryo donation to the offspring and family's.[16,17] Knowledge of the health, social, and economic status of the donor was also of great importance to them.[15,17] Based on the questions addressed in this study, in terms of the principle of justice, the disclosure of the donation to the offspring, future communication of the donor and recipient families, and having the same nationality were the most important challenges noted by the donors. Therefore, the results of the present study are in accordance with that of previous studies. The issue of confidentiality and secrecy during the donation process is an issue which has attracted the attention of many countries providing this treatment method. This is due to the concern that the donor being an acquaintance and the possibility of future communication with the offspring may be a threat to the family structure of the recipients. In addition, lack of disclosure of the donation to relatives and the offspring may result in future consanguineous marriages and the mixing of generations, and therefore, high prevalence of genetic diseases and congenital anomalies. Therefore, the confidentiality of embryo donation is the most controversial ethical issue among the issues related to embryo donation. As a result, the issue of confidentiality has been considered in the official embryo donation guidelines.[2] This illustrates the significance of the ethical principle of justice in countries which provide this treatment method.
From the point of view of embryo recipients, the most ethical challenges of embryo donation were present in the principle of respect for autonomy. Laruelle et al.[18] Blyth et al.,[19] and Isaksson et al.[12] emphasized recipients' desire to receive a summary of the donors' characteristics (such as age, number of children, and medical history), for an anonymous donation, and lack of communication of the genetic parents with the offspring.[18,19] In the present study, the principle of respect for autonomy based on comprehensive counseling, conscious selection, and consent procurement has been noted by the recipients as the most important challenge. This was not in agreement with the results of the abovementioned studies.
The most important responsibility of the treatment team regarding infertility treatment is the consideration of the ethical principle of nonmaleficence. Based on this ethical principle, they can clarify the ethical realities of third-party reproduction based on the most important ethical principles related to these methods from the point of view of couples seeking these methods. As a result, this principle places a heavier responsibility on assisted reproductive service providers, including donor-assisted reproduction, compared to other ethical responsibilities.[14] Nevertheless, the results of this study and the principle of respect for autonomy, as the foundation of the medical ethics approach, illustrate the necessity of the implementation of integrated programs according to a suitable care standard which contains the ethical principle of respect for autonomy.
A limitation of this study was the lack of accuracy of information due to both embryo donors' and recipients' lack of desire to reveal the embryo donation. To increase the accuracy of the obtained information, the researcher tried to create favorable circumstances during the interviews and obtain the participants' confidence.
Conclusion
The four ethical principles were important in the view of embryo donors and recipients; however, the importance of the principle of respect for autonomy, considering the existing barriers in the services of infertility centers, was highlighted. It seems that the law of embryo donation to infertile couples in Iran, in comparison to the laws of other countries, has deficiencies. Thus, legislators and relevant authorities must take measures toward the development of guidelines for this treatment method in the framework of ethics principles and incorporate all four principles independently through the consideration of the experiences and laws of other countries and the cultural dimensions of the society.
Financial support and sponsorship
Isfahan University of Medical Sciences, Isfahan, Iran (Grant No.394459).
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The researchers express their gratitude to all the participants who made this study possible for their cooperation.
References
- 1.Berezina PR, Zhao Y. The ethical legal and social issues impacted by modern assisted reproductive technologies. Obstet Gynaecol Int. 2012;2012:686253. doi: 10.1155/2012/686253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wennerholm WB. Cryopreservation of embryo and oocytes: Obstetric outcome and health in children. Hum Reprod. 2000;15:18–25. doi: 10.1093/humrep/15.suppl_5.18. [DOI] [PubMed] [Google Scholar]
- 3.Tatary F, Mohammadpour Y, Shamsi E, Abbasi M. Ethical aspects of embryo and gametes donation from the perspective of the four principles medical. J Med Ethic. 2013;27:156. [In persian] [Google Scholar]
- 4.MacCallum F, Golombok S. Embryo donation families: Mothers' decisions regarding disclosure of donor conception. Hum Reprod. 2007;22:2888–95. doi: 10.1093/humrep/dem272. [DOI] [PubMed] [Google Scholar]
- 5.Pence GE. Classic cases in medical ethics: Accounts of cases that have shaped medical ethics, with philosophical, legal, and historical backgrounds. 4th ed. McGraw Hill: 2004. [Google Scholar]
- 6.Abbasi M, Rezaii R. Comparative study of embryo donation and medical and jurisprudence. Med Law J. 2011;24:12. [Google Scholar]
- 7.Flynn J. Embryo Donation for Pregnancy: Psychology, Philosophy and Policy. Res Bio Ethic. 2013;7:2–7. [Google Scholar]
- 8.Practice Committee of American Society for Reproductive Medicine, Practice Committee of Society for Assisted Reproductive Technology. 2008 Guidelines for gamete and embryo donation: A Practice committee Report. Fertil Steril. 2008;90:30–44. doi: 10.1016/j.fertnstert.2008.08.090. [DOI] [PubMed] [Google Scholar]
- 9.Hammarberg K, Johnson L, Petrillo T. Gamete and embryo donation and surrogacy in Australia: The social context and regulatory framework. Int Fertil Steril. 2011;4:176–83. [In persian] [PMC free article] [PubMed] [Google Scholar]
- 10.Hart V, Plath D. Egg donor wanted: Social work with women looking for an egg donor. Austr Soc Work. 2011;64:515–25. [Google Scholar]
- 11.Newton RC, McDermid A, Tekpetey F, Tummon IS. Embryo donation: Attitudes toward donation procedures and factors predicting willingness to donate. Hum Reprod. 2003;18:878–84. doi: 10.1093/humrep/deg169. [DOI] [PubMed] [Google Scholar]
- 12.Isaksson S, Svanberg AS, Sydsjo G, Thurin-Kjellberg A, Karlstrom N, Solensten G, et al. Two decades after legislation on identifiable donors in Sweden: Are recipient couples ready to be open about using gamete donation. Hum Reprod. 2011;26:853–60. doi: 10.1093/humrep/deq365. [DOI] [PubMed] [Google Scholar]
- 13.Goedeke S, Payne D. Embryo donation in New Zealand: A pilot study. Hum Reprod. 2009;24:1939–45. doi: 10.1093/humrep/dep116. [DOI] [PubMed] [Google Scholar]
- 14.Roshan M. Legal review gamete and embryo donation. Payesh J. 2006;6:407–14. [In persian] [Google Scholar]
- 15.Svanberg AS, Sydsjö G, Bladh M, Lampic C. Attitudes about donor information differ greatly between IVF couples using their own gametes and those receiving or donating oocytes or sperm. J Assist Reprod Genet. 2016;33:703–10. doi: 10.1007/s10815-016-0694-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bay B, Larsen PB, Kesmodel US, Ingerslev HJ. Danish sperm donors across three decades: Motivations and attitudes. Int J Fertile Steril 101. :252–7. doi: 10.1016/j.fertnstert.2013.09.013. [DOI] [PubMed] [Google Scholar]
- 17.Gurtin ZB, Ahuja KK, Golombok S. Emotional and relational aspects of egg-sharing: Egg-share donors' and recipients' feelings about each other each other's treatment outcome and any resulting children. Hum Reprod. 2012;27:1690–701. doi: 10.1093/humrep/des085. [DOI] [PubMed] [Google Scholar]
- 18.Laruelle C, Place I, Demeestere I, Englert Y, Delbaere A. Anonymity and secrecy options of recipient couples and donors, and ethnic origin influence in three types of oocyte donation. Hum Reprod. 201;;6:382–90. doi: 10.1093/humrep/deq346. [DOI] [PubMed] [Google Scholar]
- 19.Blyth E, Kramer W, Schneider J. Perspectives, experiences, and choices of parents of children conceived following oocyte donation. Reprod Med J. 2013;26:179–88. doi: 10.1016/j.rbmo.2012.10.013. [DOI] [PubMed] [Google Scholar]


