Abstract
Background
Anemia is common among people living with HIV infection and is frequently associated with poor quality of life and poor prognosis. It has been well described in antiretroviral naïve individuals and those on non-nucleoside reverse transcriptase inhibitor-based first line antiretroviral therapy (ART) regimens. However there is limited information on anemia for ART experienced individuals on protease inhibitor-based second line ART regimens in resource limited settings. Our objective was to describe the prevalence and risk factors of anemia in this ART experienced population in Malawi.
Methods
We conducted a cross-sectional study using routine facility data at two HIV clinics in Lilongwe, Malawi. The analysis included individuals receiving protease inhibitor-based second line ART. Clinical and laboratory data were collected at routine clinic visits. We used descriptive statistics, two-sample t-tests and multivariate logistic regression for data analysis.
Results
Three hundred seventy-seven records were included in this analysis (37% male, median age 41 years, median CD4 count 415 cells/μL). The prevalence of anemia was 125/377 (33.2%) − mild, moderate and severe anemia was 17.5%, 13.8%, and 1.9% respectively. Female participants had a higher prevalence than male participants (43.6% vs. 15.7%, p < 0.001). In multivariate logistic regression, female sex (adjusted odds ratio (aOR) 5.3; 95% CI 2.9–9.5) and a CD4 count <200 cell/ul (aOR 3.1; 95%CI 1.6–6.0) were associated with increased risk of having anemia while a BMI ≥30 kg/m2 (aOR 0.8; 95% CI 0.6–1.0) and being on ART for more than 10 years (aOR 0.4; 95% CI 0.2–0.9) were associated with reduced risk of anemia. Being on a zidovudine- containing ART regimen was not associated with anemia.
Conclusion
Anemia is common in people on second line ART in Lilongwe, Malawi. Screening for anemia in this population would be a useful strategy; especially for female patients, those who are underweight and have a low CD4 cell counts.
Keywords: Anemia, Second line, Art, HIV, Cross-sectional
Background
Anemia is common among individuals with Human Immunodeficiency Virus (HIV) infection [1]. Sub-Saharan Africa has a high prevalence of people living with HIV (PLHIV) with anemia. In these individuals anemia is associated with malnutrition, low CD cell counts and comorbidities such as tuberculosis [2, 3]. Whether the person is on ART or not, the presence of anemia predicts poor clinical outcomes such as death, clinical progression to AIDS, morbidity and a poor quality of life [4–6]. However, individuals who recover from anemia have better clinical outcomes [7].Therefore reducing anemia is a key component of care in people living with HIV.
Starting antiretroviral therapy (ART) improves hemoglobin levels and provides a protective effect against development of new anemia [8, 9]. As a result, people on ART have lower prevalence of anemia than those who are ART-naïve; underlining the value of ART in treating anemia [1, 5]. However in resource-limited settings data on the occurrence of anemia in PLHIV who have been on ART for several years. For PLHIV on second line ART regimens, the prevalence and risk factors of anemia are not well known even though persistent anemia continues to be clinically relevant while taking ART [10, 11].
As PLHIV are now living longer and HIV/AIDS programs across sub-Saharan Africa are maturing, more people are failing their first line ART regimens and are requiring second line ART regimens [11]. By 2016, approximately 1% of PLHIV (8811 PLHIV) in Malawi’s national ART program were on second line ART regimens and this number has been increasing every following year [12]. Therefore, studies need to address the gap in knowledge on anemia during long term ART treatment. HIV/AIDS programs should have strategies in place to improve survival and to reduce morbidity while people are on ART including strategies to identify those people at a greater risk of anemia during ART treatment.
We studied a cohort of ART-experienced Malawians on second line ART to describe the prevalence of and risk factors for anemia.
Methods
Study setting
We conducted a cross-sectional study using routine facility data from the Lighthouse (LH) and Martin Preuss Centre (MPC) HIV clinics in Lilongwe, Malawi, two tertiary referral ART clinics. The Lighthouse Trust, operating both LH clinic and MPC, is the largest provider of adult HIV care for PLHIV in Malawi. The integrated TB/HIV care program and Option B+ program for HIV positive pregnant and breastfeeding women and their families is based at MPC, while all other services are provided at both sites. ART regimens are standardized in the Malawi HIV/AIDS treatment guidelines [13]. Following first line ART regimen failure, patients start a second line ART regimen consisting of 2 NRTIs and a PI. The PIs used are atazanavir/ritonavir (ATV/r) and lopinavir/ritonavir (LPV/r). The NRTIs are tenofovir/lamivudine (TDF/3TC), zidovudine/lamivudine (AZT/3TC) and abacavir/lamivudine (ABC/3TC).
Stable individuals are seen at 3 month intervals for routine clinic visits. At these visits, a clinical assessment is done, tuberculosis is excluded by a 4 question symptom screen and cotrimoxazole prophylaxis and antiretroviral treatment are supplied. Viral load monitoring is done at 6 months following initiation of a new antiretroviral treatment regimen and then every 2 years thereafter per Malawi HIV/AIDS treatment guidelines [13]. There is no routine laboratory monitoring during ART.
Study population
Study participants were identified from the clinics’ Electronic Medical Records (EMR) system. As part of implementation of the viral load monitoring policy at Lighthouse and Martin Preuss clinics, patients on second line ART for at least 6 months had viral load and safety laboratory tests. Adults (age ≥ 18 years) receiving PI-based second line antiretroviral regimens were included in this analysis.
Study procedures
The data covers the period between October 2013 and April 2014. At their first routine clinic visits during this period, the study participants had clinical evaluations done and blood draws for full blood count (FBC), CD4 count, liver function tests, renal function tests, and viral load. Blood samples were processed at the UN-Project Laboratory in Lilongwe. VL was measured using the Abbott Real Time HIV-1 assay system. CD4 cell counts were measured by flow cytometry using the Becton Dickinson FACSCount system (Becton Dickinson, Mountain View, California, USA). FBC was analyzed in the Beckman Coulter AcT 5diff Cap Pierce hematology analyzer (Beckman Coulter, Miami, FL), while liver and renal function tests were analyzed in the Roche Cobas C 311 chemistry analyzer.
The clinical evaluation and results of the laboratory tests were recorded into the EMR that is used at clinic visits. The EMR is used for recording clinical evaluations and for prescribing and dispensing drugs. Laboratory results, demographic information, antiretroviral treatment history, weight and height were extracted from the EMR into a database.
Variables
The WHO hemoglobin concentrations for the diagnosis of anemia and assessment of severity were used to define anemia as hemoglobin (Hb) <12.0 g/dl for non-pregnant women and Hb <13.0 g/dl for men [14]. Anemia was further classified as mild (11–11.9 g/dl in non-pregnant women, 11–12.9 in men), moderate (8–10.9 g/dl for both sexes) and severe (<8 g/dl for both sexes) [14]. We used the WHO immunological classification for established HIV infection to classify HIV-associated immunodeficiency by CD4 counts: none or not significant (≥500 cells/μl), mild (350–499 cells/μl), advanced (200–349 cells/μl) and severe (<200 cells/μl) [15]. We used the WHO definition of virologic failure to define viral suppression as a viral load ≤1000 copies/ml [16]. Weight and height measurements were used to calculate the body mass index (BMI) which was classified as underweight (<18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25–29.9 kg/m2) and obese (≥30 kg/m2). Serum creatinine, age, and sex were used to calculate the estimated glomerular filtration rate (GFR) using the 4-V MDRD eq. [17]. The mean corpuscular volumes (MCV) and mean corpuscular hemoglobin (MCH) were classified using the local UNC Project Laboratory reference values. The MCV and MCH were used to classify anemia.
Statistical analysis
We used descriptive statistics to describe the population and to obtain the prevalence of anemia. We compared the means of the hemoglobin, age, total time on ART, time on second line ART, BMI and GFR between those with anemia and without anemia using two-sample t-tests. The categorical variables sex, second line regimen, viral load, CD4 count, MCV and RDW were analyzed using Chi-square and Fishers exact tests. Bivariable and multivariable logistic regression was used to estimate odds ratios (OR) for factors associated with anemia. All predictor variables were entered into a bidirectional stepwise variable selection multivariate model to identify the best set of risk factors for anemia. P-values for inclusion and removal of a variable were set at 0.05 and 0.1 respectively. We used a p-value of <0.05 to test significance and 95% confidence intervals (CI) to estimate precision. All statistical analyses were done using STATA SE version 12.1 (College Station, Texas).
Results
Three hundred ninety-two individuals on second line ART were enrolled in the study. 5 records were excluded from the analysis because the individuals were not on second line ART; they had been erroneously included and their records showed they were not on second line ART during data analysis. An additional 10 records were excluded because the age was less than 18 as per inclusion criteria for this analysis. Therefore 377 records were included in the analyses.
Approximately two-thirds (237/377) of the study participants were female (Table 1). This is consistent with the ratio of men/women in the study clinic so women are not overrepresented. The average age of the participants was 41.9 years (SD = 9.6). More than three quarters of the participants (289/377) had been receiving ART for more than 5 years; the mean duration of ART use was 7.4 years (SD = 2.8). Anemic participants were significantly younger (40.5 years vs. 42.6 years, p-value = 0.01) and had been on second line ART for a shorter duration (2.9 years vs. 3.7 years, p-value = 0.004) than the non-anemic participants. There were no pregnant women.
Table 1.
Characteristics of HIV-infected patients on second line ART in two urban HIV clinics in Lilongwe, Malawi, means ±SD or n (%)
| Characteristic | Anemic | Not anemic | P-value† |
|---|---|---|---|
| n = 125a | n = 252a | ||
| Sex (%) | |||
| Male | 22 (17.6) | 118 (46.8) | <0.001 |
| Female | 103 (82.4) | 134 (53.2) | |
| Age, mean (SD) years | 40.5 (9.4) | 42.6 (9.6) | 0.01 |
| Total time on ART, mean (SD) years | 7.1 (2.5) | 7.5 (3.0) | 0.17 |
| Time on second line ART, mean (SD) years | 2.9 (2.0) | 3.7 (2.4) | 0.004 |
| Second line regimen (%) | |||
| Contains AZTb | 19 (15.2) | 48 (19.1) | 0.37 |
| Does not contain AZT | 106 (84.8) | 204 (81.0) | |
| CD4 count (×103cells/ul) | |||
| > 500 | 42 (35.0) | 89 (35.7) | 0.003 |
| 350–499 | 30 (24.0) | 72 (28.9) | |
| 200–349 | 23 (18.4) | 61 (24.5) | |
| < 200 | 30 (24.0) | 27 (10.8) | |
| Viral suppression (copies/ml) | |||
| < =1000 | 110 (89.4) | 230 (91.6) | 0.365 |
| > 1000 | 13 (10.6) | 21 (8.4) | |
| Body mass index, mean (SD) kg/m2 | 24.2 (5.1) | 25.1 (5.2) | 0.17 |
| Estimated glomerular filtration rate | 91.5 (31.0) | 91.8 (29.9) | 0.17 |
Anemia defined as Hb <12.0 g/dl for non-pregnant women and Hb <13.0 g/dl for men
aMissing values not included in the totals
bAZT- zidovudine
†p-value for t-test or chi-squared test as appropriate
The distribution of hemoglobin values between male and female participants is shown in Fig. 1. Men had higher hemoglobin values (median of 14.5 mg/dl; interquartile range (IQR) 13.6–15.5 mg/dl) than women (median of 12.3 mg/dl; IQR 11.1–13.1 mg/dl).
Fig. 1.
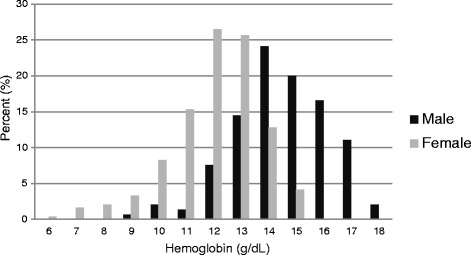
Distribution of hemoglobin among HIV infected patients on second line ART in male and female participants at 2 urban HIV clinics in Lilongwe, Malawi
The prevalence of anemia was 125/377 (33.2%). Female participants had a higher prevalence than male participants (43.6% vs. 15.7%, p < 0.001). There were no differences in the total time on ART, time on second line ART and participants with suspected virologic failure on second line ART between male and female participants (data not shown).
The prevalence of mild, moderate and severe anemia was 66/377 (17.5%), 55/377 (13.8%) and 7/377 (1.9%) respectively. Among people who had anemia, most of the cases had normocytic (87/125) and normochromic (98/125) anemia (Table 2). A few cases had microcytosis (13/125) and macrocytosis (25/125). All 7 cases with severe anemia were female; 6 of these cases had microcytic, hypochromic anemia while 1 case had normocytic, normochromic anemia. 48/52 cases with moderate anemia were female participants while only 4 cases with moderate anemia were male participants. Most men with anemia (18/22 of men with anemia) had mild anemia.
Table 2.
Description of the type and severity of anemia, n = 125
| Mild | Moderate | Severe | P-value† | ||
|---|---|---|---|---|---|
| (N = 66) | (N = 52) | (N = 7) | |||
| sex | 0.002 | ||||
| Male | 18 (27.3) | 4 (7.7) | 0 (0.0) | ||
| Female | 48 (72.7) | 48 (92.3) | 7 (100) | ||
| MCV | <0.001 | ||||
| <71 | 1 (1.5) | 6 (11.5) | 6 (85.7) | ||
| 71–95 | 51 (77.3) | 35 (67.3) | 1 (14.3) | ||
| >95 | 14 (21.2) | 11 (21.2) | 0 (0.0) | ||
| MCH | <0.001 | ||||
| <23 | 0 (0.0) | 9 (17.3) | 6 (85.7) | ||
| 23–34 | 62 (93.9) | 35 (75.0) | 1 (14.3) | ||
| >34 | 4 (6.1) | 4 (7.7) | 0 (0.0) | ||
MCV− mean corpuscular volume
MCH− mean corpuscular hemoglobin
†p-value for chi-squared test
During multivariate logistic regression female sex (adjusted odds ratio (aOR) = 4.1; 95% CI 2.5–7.0) and a CD4 count <200 cell/ul (aOR = 2.4; 95% CI 1.3–4.4) were associated with increased risk of having anemia while being on ART for more than 10 years (aOR = 0.4; 95% CI 0.2–0.8) and having a BMI ≥ 30 kg/m2 were associated with a reduced risk of anemia (Table 3). Age, viral suppression, glomerular filtration rate and the presence of AZT in the current regimen were not associated with anemia.
Table 3.
Factors associated with anemia in HIV-infected patients on second line ART at two urban HIV clinics in Lilongwe, Malawi
| Unadjusted Odds Ratios | Adjusted Odds Ratios | |||
|---|---|---|---|---|
| Characteristic | (95% CI) | p-value | (95% CI) | p-value |
| Sex | ||||
| Male | 1 | 1 | 1 | |
| Female | 4.1 (2.5–7.0) | <0.001 | 5.3 (2.9–9.5) | <0.001 |
| Age | ||||
| ≤29 | 1 | |||
| 30–39 | 1.4 (0.6–3.2) | 0.39 | ||
| 40–49 | 0.9 (0.4–1.9) | 0.69 | ||
| ≥50 | 0.6 (0.3–1.5) | 0.30 | ||
| Total time on ART (years) | ||||
| 0–5 | 1 | 1 | 1 | |
| 6–10 | 1.2 (0.7–2.0) | 0.60 | ||
| 11–15 | 0.4 (0.2–0.8) | 0.02 | 0.4 (0.2–0.9) | 0.02 |
| Second line ART regimen | ||||
| contains AZT | 1 | |||
| does not contain AZT | 1.3 (0.7–2.4) | 0.36 | ||
| CD4 cell count | ||||
| ≥500 | 1 | 1 | 1 | |
| 350–499 | 0.8 (0.5–1.6) | 0.67 | ||
| 200–349 | 0.8 (0.4–1.5) | 0.47 | ||
| <200 | 2.4 (1.3–4.4) | 0.01 | 3.1(1.6–6.0) | 0.001 |
| Viral load | ||||
| <=1000 | 1 | |||
| >1000 | 1.3 (0.6–2.7) | 0.49 | ||
| Body mass index | ||||
| <18.5 | 1.5 (0.7–3.5) | 0.33 | ||
| 18.5–24.9 | 1 | 1 | 1 | |
| 25–29.9 | 1.0 (0.6–1.8) | 0.86 | ||
| ≥30 | 0.6 (0.3–1.1) | 0.08 | 0.8 (0.6–1.0) | 0.02 |
| Glomerular filtration rate | ||||
| >90 | 1 | |||
| 30–89 | 0.7 (0.5–1.1) | 0.15 | ||
| <30 | 9.0 (1–78.4) | 0.047 | ||
CI-confidence intervals
AZT- zidovudine
Discussion
We found that anemia was common in this cohort on second line ART. The prevalence was highest in women who also had lower hemoglobin values and more severe degrees of anemia. Being female and a CD4 count <200 cell/ul were risk factors for anemia while BMI ≥30 kg/m2 and being on ART for more than 10 years were associated with reduced risk of anemia.
Although ART use is associated with a decrease in the prevalence of anemia, the prevalence in our study population was high [1, 8, 18]. Among the general adult population in Malawi, the prevalence of anemia ranges from 17% in men to 28% in non-pregnant women [19, 20]. Compared to this, we report a higher prevalence of 33.2% in people on second line ART− 15.7% in men and 43.6% in women. The prevalence of anemia in this study is similar to the prevalence observed in people on first line ART regimens where it was reported at 38.2% in a study of people on first line ART regimens [21]. However this prevalence is lower than the prevalence in ART naïve individuals which was reported at 77.4% in one study [22]. This is consistent with studies that show that ART reduces the prevalence of anemia in people living with HIV [21, 22].
The high prevalence of anemia in our study population is still worrying and points to a larger problem— that anemia remains untreated in large numbers of people on ART. This is a concern because anemia lowers the quality of life, an important treatment goal while on ART, and increases the risk of progression to AIDS and death [4–6]. The high prevalence of anemia highlights the need to address causes of anemia in people on ART.
The mechanism of anemia in this study population as in other populations living with HIV is multifactorial and includes both HIV-related and non-HIV related causes. The HIV-related causes are HIV itself which causes anemia of chronic disease due to chronic inflammation; opportunistic infections such as mycobacteria and fungi and neoplasms such as lymphoma which infiltrate bone marrow and inhibit maturation of progenitor cells as well as medications used during treatment of HIV and associated conditions such as zidovudine and cotrimoxazole [3, 7]. Treating HIV-related anemia should be with effective ART; appropriate treatment for the opportunistic conditions and removal of any suspected medications [1, 7, 23]. In our study, a few anemic participants (13/377) had VL >1000 cps/ml and were suspected to have treatment failure while the rest of the participants had viral suppression. We did not have data on current and past medical history and drug history (other than the ART history). However since this was a very ART experienced cohort, it is possible that participants had a significant history of opportunistic conditions and drugs that can cause anemia.
Endemic causes of anemia play a role in both the general population and in people living with HIV. In sub-Saharan Africa, these are chronic malnutrition; nutritional deficiencies such as iron deficiency, vitamin B12 deficiency and folate deficiency; infections and parasite infestations such as malaria, schistosomiasis and hookworms; pregnancy and hemoglobin disorders such as thalassemia, other hemoglobinopathies and other rare congenital hematologic disorders [24–26]. In settings such as ours where the anemia prevalence is already high from endemic causes, HIV infection worsens pre-existing anemia through its effects of chronic inflammation and immunosuppression [27].
Despite iron deficiency being a common cause of anemia within African populations, there was no preponderance of microcytosis nor hypochromia in our study population to suggest that iron deficiency is an important cause of anemia in the study participants []. Other studies have reported high rates of iron deficiency in people living with HIV and in those on ART [26]. A possible reason for the low prevalence of iron deficiency anemia in our study population is that this was an urban population which is associatied with lower prevalence of iron deficiency that rural populations [25]. In addition, the study participants were continuously in care at the HIV clinics with access to clinical assessments and hemoglobin level checks. The participants had many opportunities to be diagnosed with anemia and to have iron supplementation. The WHO recommends presumptive iron supplementation, anti-helminthic and anti-malarial therapy to treat anemia in resource limited settings where large workloads for health workers and inadequate laboratory capabilities make diagnosing specific causes of anemia difficult [28]. This approach is recommended in the Malawi Standard Treatment Guidelines and in other African countries [29]. However, a study in Mozambique showed that there is need for additional efforts to find and treat specific causes of anemia in PLHIV including in those on ART [30].
Nearly half of the female participants in this study had anemia, consistent with studies that show high prevalence of anemia in women living with HIV. Women living HIV are at a higher risk of severe anemia than men [4, 30]. The high prevalence in the women also reflects an overall higher prevalence of anemia in women in the general population [2]. In addition, six out of the seven women that had severe anemia in this study had microcytosis that indicates iron deficiency anemia − all were given iron supplementation. In contrast, almost all men had mild anemia except for 4 cases with moderate anemia. Whether additional factors such as differential ART failure in women, contribution of anemia in failure of first line ART regimen or use of NNRTI for prevention of mother to child transmission (PMTCT) may have contributed to the high prevalence of anemia in women this study is not known. Women could benefit from routine screening for anemia before starting ART and routine hemoglobin monitoring while they are on ART.
There are several reasons for the high proportion of women in our study population. In Malawi, more women are infected with HIV than men; women tend to present for health services more frequently than men [20] and with the Option B+ program that has been implemented since 2011, pregnant women are systematically targeted for HIV testing and those who have HIV start life-long ART regardless of the CD4 cell count [13]. As a result, more women are on ART than men. Our study population has similar gender demographics with the overall clinic population so that women are not overrepresented in the study population. From our findings, there was no difference in time spent on first line ART, time on second line ART and in virologic suppression between men and women.
We did not see an association between AZT in the current second line ART regimen and anemia in our analysis. This is in contrast with the widely recognized risk of anemia reported in association with AZT use [4, 31, 32]. We suspect that the lack of an association was because participants who would have been anemic at initiation of ART were not started on an AZT-based ART regimen and those that were suspected of having AZT associated anemia would have already been switched from AZT before these data were collected. Huffam et al. also reported that prior ART experience could be protective against subsequent development of AZT associated anemia in later regimens [33]. This is relevant to this study population that had significant prior ART experience. Participants in this study spent an average of 7.4 years on ART. In addition, some studies have reported that AZT is not a significant risk factor for anemia when it is used as part of a combinational ART regimen as is the case in our study population [21, 29].
In this study, we described anemia in among an ART-experienced cohort on PI-based second line ART. A strength of this analysis is that it was conducted on a well-characterized cohort that is generalizable because it used data collected during routine clinic visits.
An important limitation of the study is the lack of data on other known risk factors for anemia such as the presence of fever, opportunistic infections (e.g. TB, oral candidiasis) and concurrent use of other medication which were not measured and were not included in the analysis [27]. When analyzing the data on AZT, we were not able to look at substitutions that were made prior to the date of sample collection. This could have the effect of confounding by indication the significance of AZT in the ART regimens. Because Hb monitoring is not routinely done for patients on ART outside of the two facilities included in this study, the prevalence reported may be different than that in the wider HIV-infected population on second line ART.
Conclusion
The study shows that anemia is present at a high prevalence in ART experienced people on second line ART regimens. The study further shows the need to identify and treat the causes of anemia in addition to giving them ART. As would be expected, female patients, those with CD4 cell count less than 200cells/ul were at higher risk of anemia while those who were overweight had lower risk of anemia. Further longitudinal follow-up studies are needed to explore long term hemoglobin changes after antiretroviral treatment is initiated and to find the specific causes of anemia in people on ART.
Acknowledgements
We would like to thank patients who were on second line ART at LH and MPC HIV clinics during the study period. We would like to thank Hannock Tweya and the Lighthouse Trust Monitoring and Evaluation department for data extraction from the EMR system.
Funding
We acknowledge the D43 (TW010060–01) grant through MH for supporting the study. RF and DO were supported by the Fogarty Global Health Fellows Program Consortium (1R25TW009340–01). RF and RL were supported by the Doris Duke Charitable Foundation International Scholars Program. The funders had no role in study design, data collection and analysis nor preparation of the manuscript.
Availability of data and materials
Data extracted from the EMR at the LH and MPC HIV clinics are proprietary of the Malawi Ministry of Health as part of the Malawi National HIV/AIDS program thus we cannot make it available in a public repository. A de-identified dataset can be made on request by contacting the corresponding author who will contact the Ministry of Health and collaborators to get permission for use.
Abbreviations
- 4-V MDRD
4-Variable Modification of Diet in Renal Disease equation
- ABC/3TC
Abacavir/lamivudine
- AIDS
Acquired Immunodeficiency Syndrome
- aOR
Adjusted Odds Ratio
- ART
Antiretroviral Therapy
- ATV/r
Atazanavir/ritonavir
- AZT
Zidovudine
- BMI
Body Mass Index
- CI
Confidence Interval
- EFV
Efavirenz
- EMR
Electronic Medical Record
- FBC
Full Blood Count
- GRF
Glomerular filtration rate
- Hb
Hemoglobin
- HIV
Human Immunodeficiency Virus
- HIV-RNA
Human Immunodeficiency Virus Ribonucleic Acid
- IRB
Institutional Review Board
- LH
Lighthouse HIV Clinic
- LPV/r
Lopinavir/ritonavir
- MCH
Mean corpuscular hemoglobin
- MCV
Mean corpuscular volume
- NHSRC
National Health Sciences Research Committee
- NNRTI
Non-Nucleoside Reverse Transcriptase Inhibitor
- NRTI
Nucleoside Reverse Transcriptase Inhibitor
- NVP
Niverapine
- OR
Odds Ratio
- PI
Protease Inhibitor
- PLHIV
People living with HIV
- PMTCT
Prevention of Mother to Child Transmission
- RDW
Red cell Distribution Width
- SD
Standard Deviation
- SSA
Sub-Saharan Africa
- TB
Tuberculosis
- TDF/3TC
Tenofovir/lamivudine
- TDF/3TC/EFV
Tenofovir/lamivudine/efavirenz
- WHO
World Health Organization
- ZDV/3TC
Zidovudine/Lamivudine
Authors’ contributions
MN, RL, CS and MH conceptualized and designed the study. MN did the literature search. MN, NER, CCS, DO, RF and MH analyzed the data and generated the figs. MN, RL, CS, NER, CCS, DO, RF and MH interpreted the data. MN, RL, CS, NER, CCS, RB, PT, DO, RF and MH revised the manuscript and contributed intellectually. All authors have read and approved the final manuscript.
Ethics approval and consent to participate
This analysis used routine data collected during implementation of the viral load monitoring policy at Lighthouse Trust and Martin Preuss HIV clinic. The data was retrospectively extracted from the facilities EMR system. The study was approved by the Malawi National Health Sciences Research Committee (NHSRC) and the Biomedical Institutional Review Board of the University of North Carolina at Chapel Hill, United States. From these two review boards, retrospective reviews of existing programmatic data are exempt from formal consenting procedures. All data collected were de-identified prior to analysis.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
McNeil Ngongondo, Phone: +265 999 782 183, Email: mngongondo@unclilongwe.org.
Nora E. Rosenberg, nrosenbe@email.unc.edu
Christopher C. Stanley, Email: cstanley@unclilongwe.org
Robertino Lim, Email: robertinolim@gmail.com.
Dennis Ongubo, Email: dongubo@gmail.com.
Richard Broadhurst, Email: richard_broadhurst@med.unc.edu.
Colin Speight, Email: colinspeight88@yahoo.co.uk.
Robert Flick, Email: robbie.flick@gmail.com.
Petros Tembo, Email: p_tembo@lighthouse.org.mw.
Mina C. Hosseinpour, Email: mina_hosseinipour@med.unc.edu
References
- 1.Kyeyune R, Saathoff E, Ezeamama AE, Loscher T, Fawzi W, Guwatudde D. Prevalence and correlates of cytopenias in HIV-infected adults initiating highly active antiretroviral therapy in Uganda. BMC Infect Dis. 2014;14:496. doi: 10.1186/1471-2334-14-496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization . Worldwide prevalence of anemia 1993–2005: WHO global database on anemia. Geneva, Switzerland: WHO; 2008. [Google Scholar]
- 3.Semba RD, Gray GE. Pathogenesis of anemia during human immunodeficiency virus infection. J Investig Med. 2001;49(3):225–239. doi: 10.2310/6650.2001.33967. [DOI] [PubMed] [Google Scholar]
- 4.Owiredu W, Quaye L, Amidu N, Addai-Mensah O. Prevalence of anaemia and immunological markers among Ghanaian HAART-naive HIVpatients and those on HAART. Afr Health Sci. 2011;11(1):2–15. [PMC free article] [PubMed] [Google Scholar]
- 5.Sullivan PS, Hanson DL, Chu SY, Jones JL, Ward JW. Epidemiology of anemia in human immunodeficiency virus (HIV)-infected persons: results from the multistate adult and adolescent spectrum of HIV disease surveillance project. Blood. 1998;91:301–308. [PubMed] [Google Scholar]
- 6.Mocroft A, Kirk O, Barton SE, Dietrich M, Proenca R, Colebunders R, Pradier C, dArminio MA, Ledergerber B, Lundgren JD. Anaemia is an independent predictive marker for clinical prognosis in HIV-infected patients from across Europe. EuroSIDA study group. AIDS. 1999;13:943–950. doi: 10.1097/00002030-199905280-00010. [DOI] [PubMed] [Google Scholar]
- 7.Redig AJ, Berliner N. Pathogenesis and clinical implications of HIV-related anemia in 2013. Hematol Am Soc Hematol Educ Program. 2013;2013:377–381. doi: 10.1182/asheducation-2013.1.377. [DOI] [PubMed] [Google Scholar]
- 8.Moore RD, Forney D. Anemia in HIV-infected patients receiving highly active antiretroviral therapy. J Acquir Immune Defic Syndr. 2002;29:54–57. doi: 10.1097/00042560-200201010-00007. [DOI] [PubMed] [Google Scholar]
- 9.Berhane K, Karim R, Cohen MH, Masri-Lavine L, Young M, Anastos K, Augenbraun M, Watts DH, Levine AM. Impact of highly active antiretroviral therapy on anemia and relationship between anemia and survival in a large cohort of HIV-infected women: Women's interagency HIV study. J Acquir Immune Defic Syndr. 2004;37:1245–1252. doi: 10.1097/01.qai.0000134759.01684.27. [DOI] [PubMed] [Google Scholar]
- 10.Denue BA, Kida IM, Hammagabdo A, Dayar A, Sahabi MA. Prevalence of anemia and immunological markers in HIV-infected patients on highly active antiretroviral therapy in northeastern Nigeria. Infect Dis. 2013;6:25–33. doi: 10.4137/IDRT.S10477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hosseinipour MC, van Oosterhout JJ, Weigel R, Phiri S, Kamwendo D, Parkin N, et al. The public health approach to identify antiretroviral therapy failure: high-level nucleoside reverse transcriptase inhibitor resistance among Malawians failing first-line antiretroviral therapy. AIDS (London, England) 2009;23(9):1127–1134. doi: 10.1097/QAD.0b013e32832ac34e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ministry of Health. Malawi Ministry of Health Integrated HIV Program Report April–June 2016. 2016. 1–37 p.
- 13.Ministry of Health and Population and National AIDS Commission. Clinical management of HIV/AIDS in children and adults. Third ed. Lilongwe, Malawi: MOH; 2014.
- 14.World Health Organization. Hemoglobin concentrations for the diagnosis of anemia and assessment of severity. 2011. http://www.who.int/vmnis/indicators/haemoglobin/en/. Accessed on 5 June 2016.
- 15.World Health Organization. WHO case definitions of HIV for surveillance and revised clinical staging and immunological classification of HIV-related disease in adults and children. 2006. http://www.who.int/hiv/pub/vct/hivstaging/en/. Accessed on 5 June 2016.
- 16.World Health Organization. Consolidated guidelines on the use of antiretroviral drugs for treating and preventing HIV infection. 2016. http://www.who.int/hiv/pub/arv/arv-2016/en/. 15 December 2016. [PubMed]
- 17.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Annals of Internal Medicine. 130(6):461–70. [DOI] [PubMed]
- 18.Moore RD, Keruly JC, Chaisson RE. Anemia and survival in HIV infection. JAcquir immune Defic Syndr hum. Retrovirology. 1998;19:29–33. doi: 10.1097/00042560-199809010-00004. [DOI] [PubMed] [Google Scholar]
- 19.Ministry of Health, Malawi, UNICEF/CDC Report of the National Micronutrient Survey. 2001.
- 20.National Statistical Office (NSO) and ICF Macro. 2016. Malawi Demographic and Health Survey 2015. Zomba, Malawi, and Calverton, Maryland, USA: NSO and ICF Macro.
- 21.Johannessen A, Naman E, Gundersen S, Bruun J. Antiretroviral treatment reverses HIV-associated anemia in rural Tanzania. BMC Infect Dis. (2011;11(190) [DOI] [PMC free article] [PubMed]
- 22.Gedefaw L, Yemane T, Sahlemariam Z, Yilma D. Anemia and risk factors in HAART Naïve and HAART experienced HIV positive persons in south West Ethiopia: a comparative study. PLoS One. 2013;8 [DOI] [PMC free article] [PubMed]
- 23.Bain BJ. Pathogenesis and pathophysiology of anemia in HIV infection. Curr Opin Hematol. 1999;6(2):89–93. doi: 10.1097/00062752-199903000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Ivan E, Crowther NJ, Mutimura E, et al. Helminthic infections rates and malaria in HIV-infected pregnant women on anti-retroviral therapy in Rwanda. PLoS Negl Trop Dis. 2013;7(8):e2380. doi: 10.1371/journal.pntd.0002380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Balarajan Y, Ramakrishnan U, Özaltin E, Shankar AH, Subramanian SV. Anaemia in low-income and middle-income countries. Lancet. 2011;378:2123–2135. doi: 10.1016/S0140-6736(10)62304-5. [DOI] [PubMed] [Google Scholar]
- 26.Kupka R, Msamanga GI, Mugusi F, et al. Iron status is an important cause of anemia in HIV-infected Tanzanian women but is not related to accelerated HIV disease progression. J Nutr. 2007;137(10):2317–2323. doi: 10.1093/jn/137.10.2317. [DOI] [PubMed] [Google Scholar]
- 27.Van den Broek NR, White SA, Neilson JP. The relationship between asymptomatic human immunodeficiency virus infection and the prevalence and severity of anemia in pregnant Malawian women. Am J Trop Med Hyg. 1998;59(6):1004–1007. doi: 10.4269/ajtmh.1998.59.1004. [DOI] [PubMed] [Google Scholar]
- 28.Stoltzfus R., Dreyfus M.L. Guidelines for the use of iron supplements to prevent and treat iron deficiency anemia. Edited by INACG, WHO and UNICEF. IUNACG. Washington.1998.
- 29.Volberding PA, Levine AM, Dieterich D, et al. Anemia in HIV infection: clinical impact and evidence-based management strategies. Clin Infect Dis. 2004;38:1454–1463. doi: 10.1086/383031. [DOI] [PubMed] [Google Scholar]
- 30.E, Brentlinger Paula, Silva Wilson P, Vermund Sten, Valverde Emilio, Buene Manuel, Moon Troy D. 2015. "Practical Management of HIV-Associated Anemia in Resource-Limited Settings: Prospective Observational Evaluation of a New Mozambican Guideline." AIDS research and human retroviruses. [DOI] [PMC free article] [PubMed]
- 31.Volberding P. Consensus statement: anemia in HIV infection—current trends, treatment options, and practice strategies. The anemia in HIV working group. Clin Ther. 2000;22:1004–1020. doi: 10.1016/S0149-2918(00)80081-8. [DOI] [PubMed] [Google Scholar]
- 32.Curkendall SM, Richardson JT, Emons MF, Fisher AE. 12. Everhard F. Incidence of anaemia among HIV-infected patients treated with highly active antiretroviral therapy. HIV Med. 2007;8:483–490. doi: 10.1111/j.1468-1293.2007.00500.x. [DOI] [PubMed] [Google Scholar]
- 33.Huffam SE, Srasuebkul P, Zhou J. Prior antiretroviral therapy experience protects against zidovudine-related anemia. HIV Med. 2007;8:465–471. doi: 10.1111/j.1468-1293.2007.00498.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data extracted from the EMR at the LH and MPC HIV clinics are proprietary of the Malawi Ministry of Health as part of the Malawi National HIV/AIDS program thus we cannot make it available in a public repository. A de-identified dataset can be made on request by contacting the corresponding author who will contact the Ministry of Health and collaborators to get permission for use.


