Abstract
Background
Dexmedetomidine has been shown to confer direct renoprotection by stabilizing the sympathetic system, exerting anti-inflammatory effects and attenuating ischemia/reperfusion (I/R) injury in preclinical studies. Results from clinical trials of dexmedetomidine on acute kidney injury (AKI) following adult cardiac surgery are controversial.
Methods
We searched EMBASE, PubMed, and Cochrane CENTRAL databases for randomized controlled trials (RCTs) comparing the renal effect of dexmedetomidine versus placebo or other anesthetic drugs in adult patients undergoing cardiac surgery. The primary outcome was the incidence of AKI. The secondary outcomes were mechanical ventilation (MV) duration, intensive care unit (ICU) stay and hospital length of stay(LOS), and postoperative mortality (in-hospital or within 30 days).
Results
Ten trials with a total of 1575 study patients were selected. Compared with controls, dexmedetomidine significantly reduced the incidence of postoperative AKI [68/788 vs 97/787; odds ratio(OR), 0.65; 95% confidence interval (CI), 0.45–0.92; P = 0.02; I2 = 0.0%], and there was no difference between groups in postoperative mortality (4/487 vs 11/483; OR, 0.43; 95% CI, 0.14–1.28; P = 0.13; I2 = 0.0%), MV duration [in days; n = 1229; weighted mean difference(WMD), −0.22; 95% CI, −2.04 to 1.70; P = 0.81], ICU stay (in days; n = 1363; WMD, −0.85; 95% CI, −2.14 to 0.45; P = 0.20), and hospital LOS (in days; n = 878; WMD, −0.24; 95% CI, −0.71 to 0.23; P = 0.32).
Conclusions
Perioperative administration of dexmedetomidine in adult patients undergoing cardiac surgery may reduce the incidence of postoperative AKI. Future trials are needed to determine the dose and timing of dexmedetomidine in improving outcomes, especially in patients with decreased baseline kidney function.
Keywords: Dexmedetomidine, Acute kidney injury, Cardiac surgery, Meta-analysis
Background
Acute kidney injury (AKI) following cardiac surgery is a widely recognized complication in association with high mortality risk [1, 2]. AKI is tightly interrelated with hemodynamic status, inflammatory and nephrotoxic components [3]. Both hemodynamic instability and sympathetic activity during surgery are harmful for renal function [4].Almost half of these patients need mechanical ventilation(MV) support and are related with prolonged intensive care unit (ICU) stay [5, 6].Moreover, along with the increasing high-risk population including advanced age, diabetes mellitus, severe cardiac failure, especially in association with cardiopulmonary bypass, AKI after cardiac surgery has become an interesting and challenge issue in clinical practice [7]. As yet, there is no definite strategy for preventing AKI after cardiac surgery [8].
Dexmedetomidine, a highly selective α2 adrenoreceptor agonist, induces sedation, analgesia, hemodynamic stabilization, anti-inflammation, as well as diuresis [9], and has theoretical advantage for reducing renal injury in animal studies [10, 11]. Several single-center randomized controlled trials (RCTs) with relatively small sample size have addressed this question and the results are controversial [12–14]. Whether perioperative dexmedetomidine could reduce the risk for AKI in adult patients undergoing cardiac surgery remains unclear. In addition, there has been no systematic review that comprehensively focuses on the potential renal effect of dexmedetomidine in adult cardiac surgery. Therefore, we conducted a meta-analysis to evaluate the effect of perioperative dexmedetomidine (compared to placebo or other drugs) on the risk for AKI and mortality.
Methods
Search strategy and study criteria
This meta-analysis was performed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta- analyses) guidelines [15] and approved by the Institutional Review Board in Beijing Shijitan Hospital, Capital Medical University. We did a systematic search in PubMed (1999 to March 2017), EMBASE (1999 to March 2017), and Cochrane Library (1999 to March 2017) using the keywords “dexmedetomidine,” “cardiac surgery,” “heart surgery,” “kidney,” and “renal.” English-published RCTs concerning adult patients were included. Exclusion criteria were as follows: emergency surgery, or studies without reporting AKI incidence.
Literature review and data extraction
The literature review and data extraction were independently completed by 2 investigators (BS and SZW). In case of duplicate records pertaining to a single study, we considered the PubMed database to take precedence. Disagreements were handled by discussion for consensus. Quality assessment was completed using the Cochrane risk of bias tool and Jadad scale. Data extraction included patient characteristics (age, proportion of males, proportion with diabetes, proportion with history of myocardial infarction, proportion with hypertension, baseline left ventricular ejection fraction, baseline creatinine levels, β-blocker use, and statin use), as well as dexmedetomidine dosage.
Postoperative outcomes
The primary end point was incidence of AKI (defined as RIFLE, AKIN, KDIGO within 7 days after cardiac surgery). Secondary outcomes included all-cause mortality (in-hospital or within 30 days), mechanical ventilation(MV) duration, ICU length of stay, and hospital length of stay(LOS).
Statistical analysis
For dichotomous outcomes (reported with incidence), we calculated the odds ratio (OR) with 95% confidence interval (CI). For continuous outcomes (reported as mean ± standard deviation, median and interquartile range, or median and range), we calculated mean differences for each study according to the statistical method of Hozo et al. [16] and used weight (the inverse variance of the estimate) to pool the estimate (weighted mean difference, WMD) with 95% CI. We used the random-effect model to pool all the data for the potential clinical inconsistency. Heterogeneity was assessed with the inconsistency statistic (I2). Publication bias was assessed by Begg’s test and Egger’s test. P < 0.05 (2 sided) was considered to be statistically significant for hypothesis testing. All statistical analyses were performed in REVMAN (version 5.0; Cochrane Collaboration, Oxford, UK) and Stata (version 9.0; StataCorp LP).
Results
Study characteristics
Figure 1 shows the PRISMA flow chart for the RCTs screening and selection process for inclusion in this study. Ten trials enrolling 1575 study subjects ultimately met our criteria (Fig. 1). Two studies were for coronary artery bypass grafting(CABG) [17, 19], seven were for combined cardiac surgery [12–14, 18, 20–22] and 1 was for aortic vascular surgery [23]. Six trials used placebo as control [12, 14, 17, 19, 22, 23], whereas two used propofol [18, 20], one used morphine [21] or remifentanil [13]. Dexmedetomidine was continuously infused at a rate of 0.2 to 0.8μg/kg/h for 24 h after a loading dose (0.4-1μg/kg) in 4 studies [13, 18, 22, 23] or infused at a rate of 0.04 to 1.5μg/kg/h without a loading dose in 6 [12, 14, 17, 19–21].
Fig. 1.

Flow diagram of studies included into meta-analysis
For postoperative outcomes, AKI incidence was reported in 9 trials [12–14, 17, 19–23], need for dialysis in 1 [18], mortality in 6 [12, 18, 20–23], mechanical ventilation duration in 8 [13, 14, 17–22], ICU stay in 8 [12–14, 17, 18, 20–22], and hospital stay in 6 [13, 17, 18, 20–22].
Study design and patient characteristics were summarized in Tables 1 and 2. The quality assessment was listed in Table 3.
Table 1.
Summarized Study Design of Included Randomized Trials
| Study | Country | Surgery | Dexmedetomidine Dose | Control | Time and Duration of intervention or Control | No. of Patients | Clinical End Point | AKI Definition | Follow-Up |
|---|---|---|---|---|---|---|---|---|---|
| Balkanay2015 I [17] | Turkey | On-PUMP CABG | 0.04μg/kg/h-0.05μg/kg/h | placebo | Start preCPB and last for 24 h | 31 vs 28 | AKI;MV duration; ICU stay; Hospital stay | RIFLE | In hospital |
| Balkanay2015II [17] | Turkey | On-PUMP CABG | 0.04μg/kg/h-0.05μg/kg/h | placebo | Start preCPB and last for 24 h | 29 vs 28 | AKI;MV duration; ICU stay; Hospital stay | RIFLE | In hospital |
| Cho 2015 [12] | Korea | Combined | 0.04μg/kg/h | placebo | Start immediately after anesthetic induction and last for 24 h | 100 vs100 | AKI; Mortality; ICU stay; | AKIN | In hospital |
| DjaianiG 2016 [18] | Canada | Combined | 0.4μg/kg 0.2–0.7μg/kg/h | propofol | Start postsurgery and last for 24 h | 91 vs 92 | AKI; Mortality; MV duration; ICU stay; Hospital stay | NA | In hospital |
| Leino 2011 [19] | Finland | On-PUMP CABG | 0.6 ng/ml | placebo | Start immediately after anesthetic induction and last for 4 h arrive ICU | 35 VS 31 | AKI; MV duration; | RIFLE | In hospital |
| Li 2017 [14] | China | Combined | 0.1μg/kg/h-0.6μg/kg/h | placebo | Start preCPB and last until the end of MV | 142 vs143 | AKI;MV duration; ICU stay | KDIGO | 30 days after surgery |
| Liu 2016 [20] | China | Combined | <1.5μg/kg/h | propofol | Start after surgery and last until the end of MV | 44 vs 44 | AKI; Mortality; MV duration; ICU stay; Hospital stay | AKIN | In hospital |
| Park 2014 [13] | Korea | Combined | 0.5μg/kg 0.2–0.8μg/kg/h | remifentanil | Start after surgery and last until extubation | 67 vs 75 | AKI; MV duration; ICU stay; Hospital stay | Cr > 100%abovebaseline or new dialysis need | In hospital |
| Shehabi2009 [21] | Australia | Combined | 0.1–0.7μg/kg/ml | morphine | Start within 1 h of adminssin to CICU until the removal of chest drains | 152 vs147 | AKI; Mortality; MV duration; ICU stay; Hospital stay | NA | 12 days after surgery |
| Ammar 2016 [22] | Egypt | Combined | 1 μg/kg over 15 min, followed by 0.5 μg/kg/h | placebo | Start preCPB and last until 6 h after surgery | 25 vs 25 | AKI; Mortality; MV duration; ICU stay; Hospital stay | NA | 30 days after surgery |
| Soliman 2016 [23] | Egypt | Aortic vascular surgery | 1 μg/kg 0.3 μg/kg/h | placebo | Start 15 min before induction maintained to the end of surgery | 75 vs 75 | AKI; Mortality; | Cr > 115 μmol/L | In hospital |
Abbreviations: AKI Acute kidney injury, CABG Coronary artery bypass graft, CPB Cardiopulmonary bypass, ICU Intensive care unit, CICU Cardiac intensive care unit, MV Mechanical ventilation, NA Not available, Cr Creatinine, RIFLE Risk–Injury–Failure–Loss–End-stage renal disease, AKIN Acute Kidney Injury Network, KDIGO Kidney Disease Improving Global Outcomes
Table 2.
Summarized patient characteristic of the included randomized trials
| Study | Age | Male (%) | DM (%) | HP (%) | PreMI (%) | LVEF (%) | CPB duration (min) | Anesthetics | Baseline Serum Creatinine | β-blocker (%) | Statins (%) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Balkanay 2015 I [17] | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Balkanay 2015II [17] | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Cho 2015 [12] | 63 | 48 | 19.5 | 45.5 | NA | 61.5 | 131 | Sevoflurane | 33 | NA | 63 |
| DjaianiG 2016 [18] | 72.55 | 75.4 | 21.9 | 75.4 | 16.4 | NA | 98.99 | Isoflurane | 53 | 68.85 | 72.55 |
| Leino 2011 [19] | 60.86 | 89.4 | NA | NA | NA | NA | NA | Isoflurane | NA | NA | 60.86 |
| Li 2017 [14] | 67.18 | 69.1 | 32.3 | 63.2 | 9.8 | NA | 102.99 | Sevoflurane | 69.73 | 48.42 | 67.18 |
| Liu 2016 [20] | 54.75 | 39.8 | 12.5 | 29.5 | NA | 65 | 71.15 | Sevoflurane | NA | NA | 54.75 |
| Park 2014 [13] | 53.81 | 55.6 | 9.15 | 27.5 | NA | 61.87 | 166.75 | Sevoflurane | NA | NA | 53.81 |
| Shehabi2009 [21] | 71.25 | 75.3 | 29.5 | 80.1 | 36.6 | NA | 98.98 | Sevoflurane | NA | NA | 71.25 |
| Ammar 2016 [22] | 57.25 | 76 | 68 | 82 | NA | NA | 66.2 | Isoflurane | 94 | 56 | 57.25 |
| Soliman 2016 [23] | 58.1 | 50 | 30.7 | 48.7 | 8.6 | 52.9 | NA | NA | 36.67 | NA | 58.1 |
Abbreviations: DM Diabetes mellitus, HP Hypertension, PreMI Previous myocardial infarction, LVEF Left ventricular ejection fraction, CPB Cardiopulmonary bypass, NA Not available
Values are given as means unless otherwise specified
Table 3.
Summarized Quality Assessment of Included Randomized Trials
| Study | Random sequence generation | Allocation Concealment | Blinding of participants and personnel | Blinding of outcome assessment | Attrition bias | Selective reporting | Jadad scale |
|---|---|---|---|---|---|---|---|
| Balkanay 2015 I [17] | Yes | Unclear | Yes | Yes | Unclear | Unclear | 4 |
| Balkanay 2015 II [17] | Yes | Unclear | Yes | Yes | Unclear | Unclear | 4 |
| Cho 2015 [12] | Yes | Sealed envelopes | Blinding of personnel | Yes | Unclear | Unclear | 4 |
| Djaiani G 2016 [18] | Yes | Sealed envelopes | Blinding of personnel | No | Yes | Unclear | 3 |
| Leino 2011 [19] | Yes | Sealed envelopes | No | Yes | Yes | Unclear | 5 |
| Li 2017 [14] | Yes | Sealed envelopes | Yes | No | Yes | Unclear | 5 |
| Liu 2016 [20] | Yes | Unclear | Unclear | Unclear | Unclear | Unclear personnel | 1 |
| Park 2014 [13] | Yes | Unclear | Unclear | Unclear | Unclear | Unclear | 1 |
| Shehabi 2009 [21] 2009 |
Yes | Unclear | Yes | No | Yes | Unclear | 5 |
| Ammar 2016 [22] | Yes | Unclear | Yes | Yes | Unclear | Unclear | 4 |
| Soliman 2016 [23] | Yes | Unclear | Yes | No | Unclear | Unclear | 4 |
Effect of Dexmedetomidine on incidence of AKI, and mortality
The outcome of AKI was reported in 1575 study participants, and the overall incidence was 10.48% (dexmedetomidine group, 68/788; control group, 97/787). The postoperative incidence of AKI was significantly reduced by dexmedetomidine (10 studies with 11 comparision; OR, 0.65; 95% CI, 0.45–0.92; P = 0.02; I2 = 0.0%; Fig. 2). Different analysis method (Mantel-Haenszel or Inverse Variance) or different summary statistics (RR vs OR vs RD) was listed in Table 4.There was no evidence of significant publication bias (Begg’s test, P = 0.22; Egger’s test, P = 0.32; Fig. 3).
Fig. 2.

Dexmedetomidine (Dex) reduced the incidence of acute kidney injury
Table 4.
Different analysis method and summary statistics for the incidence of acute kidney injury
| Analysis method | OR | 95%CI | I2 | P | RD | 95%CI | I2 | P | RR | 95%CI | I2 | P |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mantel-Haenszel | 0.65 | 0.45,0.92 | 0% | 0.02 | −0.02 | −0.04,0.01 | 46% | 0.28 | 0.72 | 0.54,0.95 | 0% | 0.02 |
| Inverse Variance | 0.65 | 0.45,0.92 | 0% | 0.02 | −0.01 | −0.04,0.01 | 21% | 0.22 | 0.72 | 0.54,0.95 | 0% | 0.02 |
Abbreviations: OR Odds ratio, RR Risk ratio, RD Risk difference, CI Confidence interval
Fig. 3.
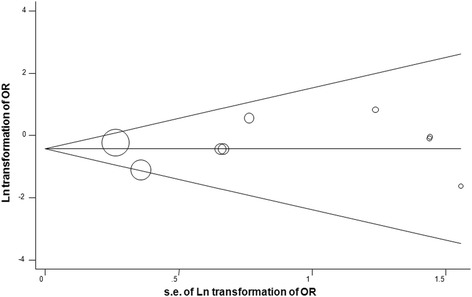
Funnel plot assessment of potential publication bias
Subgroup analyses for the potential sources of heterogeneity were listed in Table 5. We divided study participants into 11 groups according to different characteristics such as age(year, ≥60 versus <60), proportion of male (≥60% versus <60%), proportion with diabetes (≥25% versus <25%), CPB duration(min, ≥100 versus <100), statin use(≥60% versus <60%), loading dose (use or not), continuous infusion dosing (low versus high), controlled type (placebo versus nonplacebo), administration timing (pre/intraoperative versus postoperative), surgical type (CABG only versus combined) surgery, JADAD score (≥3 versus <3). Overall, no significant differences existed in the incidence of AKI (Table 5).
Table 5.
Subgroup analyses for the potential sources of heterogeneity
| Subgroup | Endpoint | No. of Comparisons | OR WMD | 95% CI | P Value | I2 | PDifference Value |
|---|---|---|---|---|---|---|---|
| 1. Age(years) | AKI | 9 | 0.64 | 0.41~ 1.01 | 0.06 | 43.8% | 0.18 |
| ≥ 60 | 5 | 0.54 | 0.31~ 0.94 | 0.03 | 32% | ||
| < 60 | 4 | 1.12 | 0.45~ 2.79 | 0.81 | 0% | ||
| 2. Gender(Male%) | AKI | 9 | 0.64 | 0.41~ 1.01 | 0.06 | 0% | 0.91 |
| ≥ 60 | 4 | 0.70 | 0.28~ 1.74 | 0.45 | 47% | ||
| < 60 | 5 | 0.75 | 0.46~ 1.20 | 0.22 | 0.0% | ||
| 3. Previous DM (%) | AKI | 8 | 0.64 | 0.41 ~ 1.01 | 0.22 | 0% | 0.86 |
| ≥ 25 | 4 | 0.75 | 0.48 ~ 1.18 | 0.22 | 0% | ||
| < 25 | 4 | 0.68 | 0.21 ~ 2.14 | 0.51 | 49% | ||
| 4.CPB duration(minutes) | AKI | 7 | 0.65 | 0.38 ~ 1.14 | 0.13 | 0% | 0.59 |
| ≥ 100 | 3 | 0.61 | 0.27 ~ 1.36 | 0.22 | 60% | ||
| < 100 | 4 | 0.85 | 0.34 ~ 2.15 | 0.73 | 0% | ||
| 5.Statin (%) | AKI | 9 | 0.64 | 0.41 ~ 1.01 | 0.06 | 43.8% | 0.18 |
| ≥ 60 | 5 | 0.54 | 0.31~ 0.94 | 0.03 | 32% | ||
| < 60 | 4 | 1.12 | 0.45 ~ 2.79 | 0.81 | 0% | ||
| 6.Loading dose use | AKI | 10 | 0.65 | 0.45 ~ 0.92 | 0.02 | 0% | 0.86 |
| Yes | 4 | 0.72 | 0.24 ~ 2.10 | 0.54 | 0% | ||
| No | 6 | 0.64 | 0.40 ~ 1.02 | 0.06 | 16% | ||
| 7. Continuous infusion | AKI | 9 | 0.61 | 0.42 ~ 0.88 | 0.008 | 68.3% | 0.08 |
| ≥ 0.1 μg/kg/h | 6 | 0.76 | 0.49~ 1.18 | 0.22 | 0% | ||
| < 0.1 μg/kg/h | 3 | 0.37 | 0.19 ~ 0.72 | 0.003 | 0% | ||
| 8. Control drugs | AKI | 11 | 0.65 | 0.45 ~ 0.92 | 0.02 | 0% | 0.33 |
| Placebo | 7 | 0.60 | 0.40 ~ 0.89 | 0.01 | 2% | ||
| Others | 4 | 0.96 | 0.40 ~ 2.29 | 0.93 | 0% | ||
| 9. Dex administration | AKI | 11 | 0.65 | 0.45 ~ 0.92 | 0.02 | 0% | 0.21 |
| Pre/Intraoperation | 8 | 0.59 | 0.40 ~ 0.87 | 0.007 | 0% | ||
| Postoperation | 3 | 1.11 | 0.45 ~ 2.74 | 0.83 | 0% | ||
| 10. Surgical procedures | AKI | 11 | 0.65 | 0.45 ~ 0.92 | 0.02 | 0% | 0.87 |
| CABG or Aortic surgery | 4 | 0.72 | 0.24 ~ 2.16 | 0.56 | 0% | ||
| Combined | 7 | 0.65 | 0.38 ~ 1.14 | 0.13 | 33% | ||
| 11. JADAD score | AKI | 11 | 0.65 | 0.45 ~ 0.92 | 0.02 | 65.7% | 0.09 |
| ≥ 3 | 9 | 0.59 | 0.41 ~ 0.86 | 0.006 | 0% | ||
| < 3 | 2 | 1.88 | 0.53 ~ 6.73 | 0.33 | 0% |
Abbreviations: AKI Acute kidney injury, OR Odds ratio, CI Confidence interval, DM Diabetes mellitus, CPB Cardiopulmonary bypass, Dex Dexmedetomidine, CABG Coronary artery bypass graft
Sensitivity analysis excluding each included study at a time revealed that the Cho 2015 study was inconsistent with the direction and size of the overall AKI- reducing effect of dexmedetomidine (P = 0.34),and the other studies were consistent with the direction and size of the overall AKI- reducing effect of dexmedetomidine (P for all <0.04).
The outcome of mortality was reported in 970 study participants, and the overall incidence was 1.5% (dexmedetomidine group, 4/487; control group, 11/483). There were no statistically significant reduction for mortality owing to perioperative dexmedetomidine (6 studies; OR, 0.43; 95% CI, 0.14–1.28; P = 0.13; I2 = 0.0%; Fig. 4).
Fig. 4.

Forest plot for mortality
Effect of Dexmedetomidine on MV duration, ICU stay and hospital stay
A trend toward reduction of postoperative MV duration(8 studies WMD, −0.22; 95%CI, −2.04 to 1.70; P = 0.81; I2 = 68%; Fig. 5), ICU stay(8 studies; WMD, −0.85; 95%CI, −2.14 to 0.45; P = 0.20; I2 = 0%; Fig. 6) and hospital stay (6 studies; WMD, −0.24; 95%CI, −0.71 to 0.23; P = 0.32; I2 = 55%; Fig. 7) by dexmedetomidine was observed, although there were not statistically significant.
Fig. 5.

Forest plot for mechanical ventilation duration
Fig. 6.
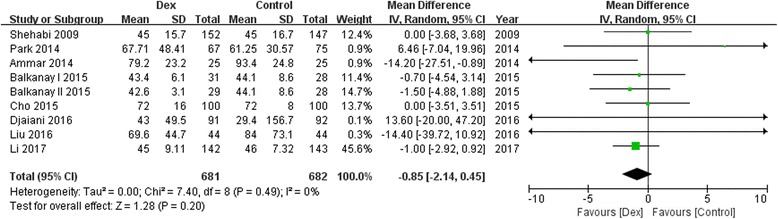
Forest plot for intensive care unit stay
Fig. 7.

Forest plot for hospital length of stay
Discussion
In this meta-analysis of 10 RCTs involving 1575 adult patients undergoing cardiac surgery, we found that perioperative dexmedetomidine use was associated with a decrease in postoperative AKI risk. However, postoperative parameters including MV duration, ICU stay and hospital LOS appeared to be no significant decrease as a result of the dexmedetomidine use. To the best of our knowledge, this is the first meta-analysis evaluating the safety and efficacy of dexmedetomidine for the prevention of cardiac surgery associated AKI.
AKI is a common complication with an estimated incidence about 7% to 45% in adult cardiac surgery [24]. Small increases in postoperative serum creatinine levels after cardiac surgery have been reported to be associated with increased morbidity and mortality even if the renal function has returned to normal at discharge [25]. For this reason, strategies to lower the incidence of postoperative AKI are of high interest to clinicians.
Dexmedetomidine is widely used for perioperative anesthesia/analgesia, and may have a more profound renal protection by stabilizing the sympathetic system, exerting anti-inflammatory effects and attenuating ischemia/reperfusion (I/R) injury [10, 26]. In this meta-analysis, positive renoprotective effects were shown in 3 studies [12, 17, 22] and only 1 [12] study showed the prevention for the AKI. However, there were also controversial or negative studies pertaining to the effect of dexmedetomidine. Our analysis combining all these positive and negative studies showed a reduced incidence of AKI in association with the dexmedetomidine use. In view of the definition for AKI using conventional tests such as the blood urea nitrogen, serum creatinine levels, urine output quantity and creatinine clearance rate, it may result in delay in the timely detection of kidney injury and can lead to false-negative results, and dexmedetomidine for the prevention of AKI may be more effective than the current results.
In the included trials, dexmedetomidine was used with a loading dose (0.4μg/kg-1μg/kg) and continuous infusion (0.04–0.6μg/kg/h). Balkanay enrolled adult patients undergoing CABG found a significant difference between high dose group (8 μg/kg) and low dose group (4 μg/kg) for the 24th postoperative hour in the mean values of neutrophil gelatinase-associated lipocalin (NGAL) [17], indicating that dexmedetomidine had marked effects on renoprotection in a dose-dependent fashion. Our subgroup analyses showed that dexmedetomidine infusion without loading dose or at low continuous dose appeared to be safe and potentially efficacious by avoiding undesirable haemodynamic effects and was possibly more effective for renal-protection, although there was no significant difference (P = 0.86 and P = 0.08).To date, the optimal dose of dexmedetomidine to improve kidney function after cardiac surgery is unclear. The optimal dose of dexmedetomidine on postoperative renal events can’t be drew because of the lack of detailed patient data. Future large and well-designed randomized trails should explore the more appropriate dose of dexmedetomidine to maximize its renal protective effect with less side effects affecting prognosis.
The timing of dexmedetomidine administration in relation to cardiac surgery is emerging as an important consideration. In 6 of 10 included trials [12, 14, 17, 19, 22, 23], dexmedetomidine was used in a preemptive strategy, and early intervention of dexmedetomidine before the cardiopulmonary bypass seems to be critical for its organ-protective effect against I/R injury [27]. Dexmedetomidine pretreatment attenuated the I/R injury by reducing inflammatory response mediated by toll-like receptor4 expression [28, 29]. Our subgroup analyses indicated that dexmedetomidine was possibly more effective for renal-protection with pre/intraoperative administration compared with postoperative administration, but there was no significant difference (P = 0.21).Our findings do not provide a strong guidance on this question, and it merits further investigation. Future trials in this area would most likely be of greatest benefit.
Two recent expert consensus articles on postoperative AKI have been recently published, which discussed also new possible therapies/preventive measures [30, 31]. Our results was in keeping with one of the article conducted by M. Joannidis and colleagues, which showed dexmedetomidine was promising to reduce the rate of AKI, although no recommendation can be given on the basis of current data. Our subgroup analyses showed that dexmedetomidine was possibly effective for renal-protection compared with placebo but not against other treatments(P = 0.33). The advantages of dexmedetomidine compared with other anesthetics still call for further research.
Our analysis has several disadvantages. First, AKI in cardiac surgery is common and may have several different causes. It is difficult to establish a protective role for dexmedetomidine. We were unable to access individual patient data, so the influences of age, sex, and other confounding factors may be underestimated. Second, the definition of AKI was not uniform in the included trials. Third, sample size in each study is relatively low, so future large clinical studies were needed. Fourth, the exclusion of non-English studies may be inappropriate, however, the assessment of publication bias did not show statistical significance. Fifth, Bland [32] and Kwon & Reis [33] have argued that the statistical method of Hozo et al. may have limited their statistical ability to detect differences. When samples are not normally distributed. So the effect of dexmedetomidine may be overestimation, especially for negative findings. Last, perioperative dexmedetomidine might be of most benefit for certain patients who are at different stage of AKI, but most of the included study did not report the existed renal impairment before surgery.
Conclusion
In summary, available evidence from the present meta-analysis suggests that perioperative administration of dexmedetomidine in adult cardiac surgery might reduce the incidence of AKI. Future trials are needed to be much larger and ascertain the optimal dose and, more importantly, the time of the dose, especially in patients with decreased kidney function at baseline.
Acknowledgements
Not applicable.
Funding
This work was supported by Beijing Shijitan Hospital Youth Funds (grant no. 2016-q08).
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AKI
Acute kidney injury
- AKIN
Acute Kidney Injury Network
- CI
Confidence interval
- I/R
Ischemia/reperfusion
- ICU
Intensive care unit
- KDIGO
Kidney Disease Improving Global Outcomes
- OR
Odds ratio
- PRISMA
Preferred Reporting Items for Systematic Review and Meta-Analysis
- RCTs
Randomized controlled trials
- RIFLE
Risk–Injury–Failure–Loss–End-stage renal disease
- WMD
Weighted mean difference
Authors’ contributions
Study design: YL; data acquisition: BS and SZW; data analysis/interpretation: YL, FPL and JZ; supervision or mentorship: WC. Each author contributed important intellectual content during manuscript drafting or revision and accepts accountability for the overall work by ensuring that questions pertaining to the accuracy or integrity of any portion of the work are appropriately investigated and resolved. YL and WC take responsibility that this study has been reported honestly, accurately, and transparently. All authors approved the final manuscript.
Ethics approval and consent to participate
This meta-analysis was approved by the Institutional Review Board in Shijitan Hospital, Capital Medical University, Beijing.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Yang Liu, Email: liuyang2002whu@whu.edu.cn.
Bo Sheng, Email: 13718303769@163.com.
Suozhu Wang, Email: 153226464@qq.com.
Feiping Lu, Email: leafreding@126.com.
Jie Zhen, Email: 13811799239@139.com.
Wei Chen, Phone: +86-10-63926256, Email: heart2008whu@163.com.
References
- 1.Rosner MH, Okusa MD. Acute kidney injury associated with cardiac surgery. Clin J Am Soc Nephrol. 2006;1:19–32. doi: 10.2215/CJN.00240605. [DOI] [PubMed] [Google Scholar]
- 2.Ortega-Loubon C, Fernández-Molina M, Carrascal-Hinojal Y, Fulquet-Carreras E. Cardiac surgery-associated acute kidney injury. Ann Card Anaesth. 2016;19:687–698. doi: 10.4103/0971-9784.191578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Makris K, Spanou L. Acute kidney injury: definition, pathophysiology and clinical phenotypes. Clin Biochem Rev. 2016;37:85–98. [PMC free article] [PubMed] [Google Scholar]
- 4.O'Neal JB, Shaw AD, Billings FT., 4th Acute kidney injury following cardiac surgery: current understanding and future directions. Crit Care. 2016;20:187. doi: 10.1186/s13054-016-1352-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stafford-Smith M, Podgoreanu M, Swaminathan M, et al. Association of genetic polymorphisms with risk of renal injury after coronary bypass graft surgery. Am J Kidney Dis. 2005;45:519–530. doi: 10.1053/j.ajkd.2004.11.021. [DOI] [PubMed] [Google Scholar]
- 6.Elmistekawy E, McDonald B, Hudson C, et al. Clinical impact of mild acute kidney injury after cardiac surgery. Ann Thorac Surg. 2014;98:815–822. doi: 10.1016/j.athoracsur.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 7.Xu J, Jiang W, Fang Y, Teng J, Ding X. Management of Cardiac Surgery-Associated Acute Kidney Injury. Contrib Nephrol. 2016;187:131–142. doi: 10.1159/000443011. [DOI] [PubMed] [Google Scholar]
- 8.Shin SR, Kim WH, Kim DJ, Shin IW, Sohn JT. Prediction and prevention of acute kidney injury after cardiac surgery. Biomed Res Int. 2016;2016:2985148. doi: 10.1155/2016/2985148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Giovannitti JA, Jr, Thoms SM, Crawford JJ. Alpha-2 adrenergic receptor agonists: a review of current clinical applications. Anesth Prog. 2015;62:31–39. doi: 10.2344/0003-3006-62.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gu J, Sun P, Zhao H, et al. Dexmedetomidine provides renoprotection against ischemia-reperfusion injury in mice. Crit Care. 2011;15:R153. doi: 10.1186/cc10283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tan F, Chen Y, Yuan D, Gong C, Li X, Zhou S. Dexmedetomidine protects against acute kidney injury through downregulating inflammatory reactions in endotoxemia rats. Biomed Rep. 2015;3:365–370. doi: 10.3892/br.2015.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cho JS, Shim JK, Soh S, Kim MK, Kwak YL. Perioperative dexmedetomidine reduces the incidence and severity of acute kidney injury following valvular heart surgery. Kidney Int. 2016;89:693–700. doi: 10.1038/ki.2015.306. [DOI] [PubMed] [Google Scholar]
- 13.Park JB, Bang SH, Chee HK, Kim JS, Lee SA, Shin JK. Efficacy and safety of dexmedetomidine for postoperative delirium in adult cardiac surgery on cardiopulmonary bypass. Korean J Thorac Cardiovasc Surg. 2014;47:249–254. doi: 10.5090/kjtcs.2014.47.3.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li X, Yang J, Nie XL, et al. Impact of dexmedetomidine on the incidence of delirium in elderly patients after cardiac surgery: a randomized controlled trial. PLoS One. 2017;12:e0170757. doi: 10.1371/journal.pone.0170757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, The ADG, PRISMA group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(1):13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Balkanay OO, Goksedef D, Omeroglu SN, Ipek G. The dose-related effects of dexmedetomidine on renal functions and serum neutrophil gelatinase-associated lipocalin values after coronary artery bypass grafting: a randomized, triple-blind, placebo-controlled study. Interact Cardiovasc Thorac Surg. 2015;20:209–214. doi: 10.1093/icvts/ivu367. [DOI] [PubMed] [Google Scholar]
- 18.Djaiani G, Silverton N, Fedorko L, et al. Dexmedetomidine versus Propofol sedation reduces delirium after cardiac surgery: a randomized controlled trial. Anesthesiology. 2016;124:362–368. doi: 10.1097/ALN.0000000000000951. [DOI] [PubMed] [Google Scholar]
- 19.Leino K, Hynynen M, Jalonen J, Salmenperä M, Scheinin H, Aantaa R. Renal effects of dexmedetomidine during coronary artery bypass surgery: a randomized placebo-controlled study. BMC Anesthesiol. 2011;11:9. doi: 10.1186/1471-2253-11-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Liu X, Zhang K, Wang W, Xie G, Fang X. Dexmedetomidine sedation reduces atrial fibrillation after cardiac surgery compared to propofol: a randomized controlled trial. Crit Care. 2016;20:298. doi: 10.1186/s13054-016-1480-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shehabi Y, Grant P, Wolfenden H, et al. Prevalence of delirium with dexmedetomidine compared with morphine based therapy after cardiac surgery: a randomized controlled trial (DEXmedetomidine COmpared to morphine-DEXCOM study) Anesthesiology. 2009;111:1075–1084. doi: 10.1097/ALN.0b013e3181b6a783. [DOI] [PubMed] [Google Scholar]
- 22.Ammar AS, Mahmoud KM, Kasemy ZA, Helwa MA. Cardiac and renal protective effects of dexmedetomidine in cardiac surgeries: a randomized controlled trial. Saudi J Anaesth. 2016;10:395–401. doi: 10.4103/1658-354X.177340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Soliman R, Zohry G. The myocardial protective effect of dexmedetomidine in high-risk patients undergoing aortic vascular surgery. Ann Card Anaesth. 2016;19:606–613. doi: 10.4103/0971-9784.191570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lau G, Wald R, Sladen R, Mazer CD. Acute kidney injury in cardiac surgery and cardiac intensive care. Semin Cardiothorac Vasc Anesth. 2015;19:270–287. doi: 10.1177/1089253215593177. [DOI] [PubMed] [Google Scholar]
- 25.Lassnigg A, Schmid ER, Hiesmayr M, et al. Impact of minimal increases in serum creatinine on outcome in patients after cardiothoracic surgery: do we have to revise current definitions of acute renal failure? Crit Care Med. 2008;36:1129–1137. doi: 10.1097/CCM.0b013e318169181a. [DOI] [PubMed] [Google Scholar]
- 26.Ueki M, Kawasaki T, Habe K, Hamada K, Kawasaki C, Sata T. The effects of dexmedetomidine on inflammatory mediators after cardiopulmonary bypass. Anaesthesia. 2014;69:693–700. doi: 10.1111/anae.12636. [DOI] [PubMed] [Google Scholar]
- 27.Zhang XY, Liu ZM, Wen SH, et al. Dexmedetomidine administration before, but not after, ischemia attenuates intestinal injury induced by intestinal ischemia-reperfusion in rats. Anesthesiology. 2012;116:1035–1046. doi: 10.1097/ALN.0b013e3182503964. [DOI] [PubMed] [Google Scholar]
- 28.Liu G, Song H, Qiu L, et al. Dexmedetomidine preconditioning inhibits the long term inflammation induced by renal ischemia/reperfusion injury in rats. Acta Cir Bras. 2016;31:8–14. doi: 10.1590/S0102-865020160010000002. [DOI] [PubMed] [Google Scholar]
- 29.Lempiäinen J, Finckenberg P, Mervaala EE, et al. Dexmedetomidine preconditioning ameliorates kidney ischemia-reperfusion injury. Pharmacol Res Perspect. 2014;2:e0004. doi: 10.1002/prp2.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Joannidis M, Druml W, Forni LG, et al. Prevention of acute kidney injury and protection of renal function in the intensive care unit: update 2017: Expert opinion of the Working Group on Prevention, AKI section, European Society of Intensive Care Medicine. Intensive Care Med. 2017;43(6):730-49. 10.1007/s00134-017-4832-y. [DOI] [PMC free article] [PubMed]
- 31.Bellomo R, Ronco C, Mehta RL, et al. Acute kidney injury in the ICU: from injury to recovery: reports from the 5th Paris International Conference. Ann Intensive Care. 2017;7(1):49. 10.1186/s13613-017-0260-y. [DOI] [PMC free article] [PubMed]
- 32.Bland M. Estimating mean and standard deviation from the sample size, three quartiles, minimum, and maximum. Int J Stat Med Res. 2015;4:57–64. doi: 10.6000/1929-6029.2015.04.01.6. [DOI] [Google Scholar]
- 33.Kwon D, Reis IM. Simulation-based estimation of mean and standard deviation for meta-analysis via approximate Bayesian computation (ABC) BMC Med Res Methodol. 2015;15:61. doi: 10.1186/s12874-015-0055-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.


