Abstract
Background
There is scant research that simultaneously analyzes the joint effects of long-term unemployment, poverty and public expenditure policies on poorer self-perceived health during the financial crisis. The aim of the study is to analyze the joint relationship between long-term unemployment, social deprivation, and regional social public expenditure on one side, and self-perceived health in Spain (2007–2011) on the other.
Methods
Longitudinal data were extracted from the Survey on Living Conditions, 2007–2010 and 2008–2011 (9105 individuals and 36,420 observations), which were then used to estimate several random group effects in the constant multilevel logistic longitudinal models (level 1: year; level 2: individual; level 3: region). The dependent variable was self-perceived health. Individual independent interest variables were long and very long term unemployment, available income, severe material deprivation and regional variables were per capita expenditure on essential public services and per capita health care expenditure.
Results
All of the estimated models show a robust association between bad perceived health and the variables of interest. When compared to employed individuals, long term unemployment increases the odds of reporting bad health by 22% to 67%; very long-term unemployment (24 to 48 months) increases the odds by 54% to 132%. Family income reduces the odds of reporting bad health by 16% to 28% for each additional percentage point in income. Being a member of a household with severe material deprivation increases the odds of perceiving one’s health as bad by between 70% and 140%. Regionally, per capita expenditure on essential public services increases the odds of reporting good health, although the effect of this association was limited.
Conclusions
Long and very long term unemployment, available income and poverty were associated to self-perceived bad health in Spain during the financial crisis. Regional expenditure on fundamental public services is also associated to poor self-perceived health, although in a more limited fashion. Results suggest the positive role in health of active employment and redistributing income policies.
Keywords: Long term unemployment, Self-reported health, Spain, Multilevel logistic longitudinal regression, Great recession, Income, Poverty, Social public expenditure, Social health determinants
Background
The financial crisis, which started in 2008, has brought about a social crisis, which has worsened the health conditions of individuals throughout Europe [1, 2], with particularly severe effects in Southern countries [3, 4], due to the conjunction of recession and stark austerity policies [5, 6].
In Spain the crisis has caused a dramatic increase in unemployment and poverty, while social protection policies have weakened [7, 8]. Unemployment skyrocketed from 8.3% in 2007 to 28.1% in 2013, the last year of the crisis, whereas these deleterious effects were much more moderate in other European countries [9]. One of the main reasons for this sudden increase is the historical dualization of the Spanish labor market since the year 1984, when a binary divide was established between indefinite contracts, with high severance pay for laidoff workers, and temporary contracts with low severance compensation. Before the financial crisis, 88% of the 18.5 million yearly contracts were temporary. For the first few years of the crisis, the increase in unemployment affected mainly workers with the latter modality of contract, which went from 31.6% in 2007 to 21.9% in early 2013 [10]. In other words, the strong increase in unemployment was caused by the harsh dualization of the labor market and the asymmetrical impact of the financial crisis, and is probably not closely related to the health of workers. This labor dynamic is in agreement with current models used in institutions and in the theory of labor segmentation [11].
Between 2007 and 2011 long-term unemployment increased in Spain from 22% to 43% [12]. This increase, along with wage deflation, has caused an escalation of poverty and a drop in available income [13]. In the period 2007–2011, available income of Spanish households in constant 2011 Euros dropped from 26,773 to 22,146 [14] and severe material deprivation rose by 53% between 2009 and 2014, leaving 7% of the Spanish population in such a dire situation [15].
The existing literature does not agree on the definition of long-term unemployment. Brenner et al. (2016) or Romeu (2006) classified unemployment as long term when it lasts between one and two years, and as very long term when it lasts over two years [16, 17]. In other works, long term designates unemployment over one year in length [18, 19], over two years [20, 21], between one and three years [22] or over five years [23]. For the purposes of our study we will follow the definition of Brenner et al. (2016) [16].
This evidence at the international level regarding the effect of long-term unemployment on health shows contradictory conclusions. Some studies found a negative impact of long-term unemployment on health [16–18, 22, 23] whereas others found no such link [20, 24].
For instance, in 2013 Herbig et al. reviewed the existing literature to conclude that long-term unemployment increases mortality and the incidence of the most prevalent mental conditions [18]. Along the same lines, a recent study by Brenner et al. (2016) for all member states of the EU found that long-term unemployment is linked to bad self-perceived health, and that the longer the unemployment the higher the incidence of the perception of bad health [16].
Nevertheless, for example, Tøge et al. (2015), using the Survey on Living Conditions (SLC) from 28 European countries (2008–2011), applied fixed-effects regression models but failed to find an association between both variables [24].
In Spain, the only study linking unemployment length with perceived health after the 2008 crisis is the work carried out by Urbanos and González (2015) with data from the National Spanish Health Survey 2011–2012 [19]. Their results indicate that being unemployed has a detrimental effect on mental and self-perceived health, and that this effect increases the longer the unemployment spell lasts.
Socioeconomic conditions and the decrease in family income are linked to poor health indicators [25, 26]. Aittomäki et al. (2012, 2014) used longitudinal data to analyze how health inequalities are associated with the specifics of the labor market and family income [27, 28]. Poverty and material deprivation are risk factors [29, 30] associated with poor perceived health [31] mental illness [32] both for the general population and for specific groups such as children or the elderly [33–35]. In Spain, the available evidence points at material deprivation as a risk factor for health [36, 37].
The international literature has looked into the matter of social public expenditure and health-care expenditure and their impact on the health of individuals, and has found that they have a positive effect across countries both at the global [38, 39], OECD [40, 41], and European levels [1, 42–47]. Conversely, Huijts et al. (2014) found that expenditure on active employment policies, unemployment benefits, and even total social expenditure had a very limited effect (even negative for women) in moderating the detrimental effects of unemployment on self-perceived health [48].
The main goal of the present study is to analyze the relationship between self-perceived health and two dimensions which are intimately linked with changes happened in the Spanish labor market after the financial crisis: long-term unemployment and social deprivation. In addition, a second goal at the regional level is to look into the relationship between regional social public expenditure and self-perceived health. The first goal requires considering four variables of interest: long- and very-long-term unemployment, income, and severe material deprivation. For the second goal two variables will be considered: per capita expenditure on fundamental public services and public per capita health-care expenditure. To this end, a longitudinal database was built using the Spanish SLC 2007–2011. Multilevel methods have been employed to integrate regional variables in order to produce a coherent hierarchy of data.
To the extent of our knowledge, no previous studies have dealt with the relationship between the financial crisis and the perceived health of the population using a set of variables that allows for the simultaneous consideration of long- and very-long-term unemployment, poverty and public social expenditure.
Methods
With the goal of observing the employment history of given individuals, a database was built from the longitudinal data files of the SLC between 2007 and 2010 and 2008–2011 [49]. Only individuals with continuous presence in the data during the four years were included. Individuals under 16 and over 65 were excluded. The longitudinal database includes 36,420 observations from 9105 individuals in 17 regions during the financial crisis of 2007–2011 in Spain. In the Spanish SLC, perceived health is a categorical variable with five possible answers (very good, good, fair, bad, and very bad), which in most models described in this study are collapsed into two (very good, good: good; fair, bad or very bad: bad).
Table 1 displays the individual and regional variables selected for each level.
Table 1.
Individual and regional variables used to analyze the relationship between long-term unemployment and health
| LEVEL 1 (year): 36,420 observations | ||
| Years | 2007–2011 | |
| LEVEL 2 (individual) 9105 individuals | ||
| Dependent variable | Self-perceived health (collapsed): Good (Very good/Good) - Bad (Fair/Bad/Very bad) Self-perceived health: Very good/Good/Fair/Bad/Very bad |
|
| Independent variables | ||
| Individual | Sociodemographic | Age (range: 16–65)a Gender (male/female) Chronic illness or chronic disability (Yes/No) |
| Socioeconomic | Education level (Primary/Secondary/Higher) Activity status (Employed/Student/Homemaker/Other inactivity/Unemployed <12 months/ Long-term Unemployed, 12–23 months/Very-long-term unemployed (24–48 months) Equivalent household incomeb (Neperian logarithm) Severe material deprivation (Yes/No) |
|
| LEVEL 3 (regional) 17 regions. | ||
| Regional | Public expenditure policies | Essential public services per capitab,c Health-care public expenditure per capitab |
aCentered continuous variable
bNominal values were converted to real values using 2007 as the base year and Consumer Price Index (National Statistics Institute) as a deflator
cEssential public services include: health care (primary, specialized, and hospital assistance, public health, clinical research); education (kindergarten, primary, secondary, post-secondary, and higher, grants, support services to education); and social protection (retirement, illness, disability, advanced age, protection of families, unemployment, housing, attention to social exclusion)
Source: the authors
The dependent variable was self-perceived health, as recorded in the SLC under “General health status”. Self-perceived health provides a multidimensional approach to health [50–52]; and is a good predictor of mortality [53, 54], morbidity [55], disability, and use of health services [56–58]. For the purposes of our research, self-perceived health was collapsed as a dichotomous variable: good self-perceived health (very good or good) and bad self-perceived health (fair, bad, or very bad). This dichotomization follows the trend of most of the related literature [59–61], which allowed us to compare results against those of previous research.
Independent variables at the individual level include gender, activity status and education level, in accordance with previous studies on self-perceived health [18, 60–63]. The variable “activity status” combines the answer categories as defined by the subject and the information provided by the question regarding monthly activity (employed, student, homemaker and/or caretaker, inactive (retired, disabled, and other forms of economic inactivity).
Unemployment variable has been categorized in being unemployed less than 12 months, being unemployed between 12 and 23 months, and being unemployed between 24 and 48 months. These categories correspond to what the literature refers to as long-term unemployment (between 12 and 23 months) and very-long-term unemployment (more than 24 months, −between 24 and 48 months-) [16].
Chronic disease may affect the odds of being unemployed and, in turn, a given individual may see their chronic condition worsen due to their losing their job or spending a long time unemployed. In order to check for robustness, our models have been tested with and without this variable [19].
Income level is one of the main components of the social gradient of health [64, 65]. Given the evidence about the moderating role of family income on the link between employment status and individual health, we have introduced the independent variable “equivalent household income” [66]. This variable has been calculated by applying the OECD modified equivalence scale to available household income [67]. The variable “severe material deprivation” was introduced in the model because it is one of the components of the AROPE index (At Risk Of Poverty or social Exclusion). This indicator is obtained from the SLC and is harmonized at the European level: it includes people who declare being unable to afford at least four of a list of nine concepts listed in the Europe 2020 strategy, and who are therefore considered to be at risk of poverty [68].
Regionally, certain ecological variables have been introduced to account for public expenditure policies: expenditure on essential public services (education, health-care, and social protection [69], and public health-care expenditure [70].
Given that our study looks into the relationship between individual and regional variables and perceived health in a simultaneous way, we have employed a random group effects in the constant longitudinal multilevel logistic model. This approach is well suited for hyerarchical structures incorporating different levels of information, in which individuals share certain characteristics due to their belonging to the same higher level (the region), and repeated measurements are available over a certain time span, as it allows for the estimation of variance for each level.
In order to be able to contrast how health is related to long and very long unemployment, income and individual social deprivation, as well as its association with the regional social and economic context, in the present work we have estimated a series of longitudinal multilevel logistic models (level 1: year; level 2: individual; and level 3: region), with random intercept. These multilevel models address the lack of independence of ordinary least squares models through the inclusion of hyerarchical data, and avoid the ecological fallacy (in which aggregated data are interpreted at the individual level) and the atomistic fallacy (in which individual data are interpreted at the aggregated level) [71].
The multilevel logistic regression model points at the dependent variable Yijk (perceived health; collapsed into good or bad health for year i) following a binomial distribution Yijk ~ Binomial(1,πijk) with variance Y, conditioned on π, Var(Yijk|πijk) = (1-πijk), where πijk is the likelihood of presenting the feature of interest for year i, being i = 2007, …, 2011, j the subject, j = 1, ..., 9105, and being k the region, with k = 1, …, 17.
Analytically:
where β0 is the independent term, Xijk the explanatory variables at individual level j, and βhits associated coefficients; Zjk are the explanatory variables at the regional level k, and αm its associated coefficients. The error term divides the dependent variable into three parts, once for each hierarchical level.
In addition, and in order to confirm that the loss of information resulting from collapsing perceived health into fewer categories does not skew the results of the estimated odds ratios of the variables of interest, an ordered logit model was estimated with the self-perceived health in its original five categories. This longitudinal multilevel ordered logit model can be written in terms of a latent response y*ijk:
The ordinal of self-assessed health variable yijk is related to the latent response via the threshold model: yijk = 1 if y*ijk ≤ k1, yijk = 2 if k1 < y*ijk ≤ k2, yijk = 3 if k2 < y*ijk ≤ k3, yijk = 4 if k3 < y*ijk ≤ k4 and yijk = 5 if k4 < y*ijk where k parameters are the cutpoints, which will be estimated together with parameters β and α in the model.
In order to be able to estimate the extent to which the areas under analysis (regions) determine individual differences in health status, we calculate the variance partition coefficient (VPC) [72], and the median odds ratio (MOR) of the region as per the latent-variable method [73].
In total, 9 models were developed to estimate the relationship between the variables of interest and self-perceived health in Spain (2007–2011). Starting from the base model, the first three models treat chronic illness differently and use different subsamples (Table 3). Being Model 1 the base model, Model 2 controls for chronic illness, Model 3 excludes from the sample those individuals whose chronic illness appeared during the four follow-up years. Model 4 excludes those individuals who were unemployed at the beginning of the panel (in January 2007 for panel 2007–2010 and in January 2008 for panel 2008–2011), in order to avoid merging recently unemployed with long term unemployed people. By estimating this model we may check our results for robustness regarding the presence of individuals who were already unemployed at the beginning of the panel.
Table 3.
Multilevel model of the association of individual and regional variables with self-perceived health, Spain 2007–2011
| SEQUENTIAL ESTIMATION OF MODELS 2007–2011 PANEL | Model 1 PURE PANEL ORIGINAL DATABASE Without controlling for chronically ill |
Model 2 PURE PANEL ORIGINAL DATABASE |
Model 3 NO CHRONICALLY ILL INDIVIDUALS ALTOGETHER |
Model 4 EXCLUDING UNEMPLOYED AT THE BEGINNING OF THE PANEL |
|---|---|---|---|---|
| SAMPLE | 34,692 OBSERVATIONS 9003 INDIVIDUALS |
34,692 OBSERVATIONS 9003 INDIVIDUALS |
27,008 OBSERVATIONS 8306 INDIVIDUALS |
32,324 OBSERVATIONS 8385 INDIVIDUALS |
| INDIVIDUAL LEVEL: YEARS 2007–2011 | ||||
| Chronic illness | – | 23.54 (21.07–26.3) *** | – | 23.24 (20.69–26.12) *** |
| Centered age | 1.09 (1.09–1.1)*** | 1.06 (1.06–1.07) *** | 1.07 (1.06–1.08) *** | 1.06 (1.06–1.07) *** |
| Female | 1.37 (1.18–1.59) *** | 1.42 (1.25–1.62) *** | 1.53 (1.3–1.8) *** | 1.41 (1.23–1.62) *** |
| Education level (primary as reference) | ||||
| Secondary education | 0.62 (0.53–0.73) *** | 0.63 (0.54–0.73) *** | 0.70 (0.58–0.84) *** | 0.62 (0.53–0.72) *** |
| Higher education | 0.28 (0.23–0.34) *** | 0.31 (0.26–0.37) *** | 0.32 (0.26–0.41) *** | 0.31 (0.26–0.38) *** |
| Activity (employed as reference) | ||||
| Student | 0.62 (0.44–0.88) *** | 0.49 (0.36–0.67) *** | 0.34 (0.21–0.54) *** | 0.51 (0.37–0.71) *** |
| Homemaking | 1.46 (1.21–1.76) *** | 1.23 (1.03–1.46) *** | 0.99 (0.79–1.23) *** | 1.28 (1.07–1.54) *** |
| Other inactive | 4.84 (4.-5.85)*** | 3.07 (2.57–3.67) *** | 1.96 (1.51–2.53) *** | 3.13 (2.6–3.78) *** |
| Long and Very long Unemployment | ||||
| Unemployed between 1 and 11 months | 1.08 (0.85–1.38) | 0.96 (0.78–1.18) | 0.99 (0.76–1.28) | 0.99 (0.8–1.24) *** |
| Unemployed between 12 and 23 months | 1.61 (1.29–2.01) *** | 1.41 (1.17–1.7) *** | 1.37 (1.08–1.73) *** | 1.43 (1.16–1.76) *** |
| Unemployed between 24 and 48 months | 2.32 (1.79–3.02) *** | 1.81 (1.46–2.26) *** | 1.72 (1.31–2.26) *** | 1.60 (1.19–2.13) *** |
| Socioeconomic variables | ||||
| Equivalent household income | 0.80 (0.74–0.86) *** | 0.75 (0.69–0.8) *** | 0.76 (0.7–0.83) *** | 0.72 (0.67–0.78) *** |
| Severe material deprivation | 2.10 (1.57–2.8) *** | 1.95 (1.46–2.6) *** | 1.74 (1.19–2.55) *** | 1.97 (1.43–2.72) *** |
| REGIONAL LEVEL: 17 REGIONS | ||||
| Health-care expenditure | 1.00 (1.00–1.001)*** | 0.99 (0.99–1.001) | 1.00 (0.99–1.001) | 1.00 (0.99–1.001) |
| Fundamental public services | 0.99 (0.99–0.99)*** | 0.99 (0.99–0.99)*** | 0.99 (0.99–0.99)*** | 0.99 (0.99–0.99)*** |
p-value < 0.01 = ***; p-value< 0.05 = **; p-value < 0.10 = *. Source: Prepared by the authors based on data from the Survey on Living Conditions. Instituto Nacional de Estadística (2014). http://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176807&menu=ultiDatos&idp=1254735976608. Accessed 27 Dec 2016
The following four models reproduce the previous sequence, but with a subsample including only those individuals who reported having good or very good health at the begining of the panel (Table 4). In other words, in these models none of the individuals who later found themselves unemployed, particularly for the long or very long term, reported to perceive their health as poor.
Table 4.
Multilevel model of the association of individual and regional variables with self-perceived health for people in good health at the beginning of the panel, Spain 2007–2011
| SEQUENTIAL ESTIMATION OF MODELS 2007–2011 PANEL Excluding bad health at the beginning of the panel |
Modelo 5 PURE PANEL Not controlling for chronically ill individuals |
Model 6 PURE PANEL ORIGINAL DATABASE |
Model 7 NO CHRONICALLY ILL INDIVIDUALS ALTOGETHER |
Model 8 WITHOUT UNEMPLOYED AT THE BEGINNING OF THE PANEL |
Model 9 PURE PANEL ORIGINAL DATABASE SELF-PERCEIVED HEALTH IN 5 CATEGORIES ORDERED MEOLOGIT |
|---|---|---|---|---|---|
| SAMPLE | 28,142 OBSERVATIONS 7313 INDIVIDUALS |
28,142 OBSERVATIONS 7313 INDIVIDUALS |
24,321 OBSERVATIONS 7140 INDIVIDUALS |
26,372 OBSERVATIONS 8218 INDIVIDUALS |
34,692 OBSERVATIONS 9003 INDIVIDUALS |
| Chronic illness | – | 19.86 (17.-23.19) *** | 40.21 (34.89–46.34) *** | – | 19.76 (16.8–23.24) *** |
| Centered age | 1.06 (1.05–1.07) *** | 1.04 (1.03–1.05) *** | 1.06 (1.05–1.07) *** | 1.05 (1.04–1.06) *** | 1.04 (1.04–1.05) *** |
| Female | 1.29 (1.08–1.54) *** | 1.32 (1.12–1.55) *** | 1.50 (1.3–1.74) *** | 1.34 (1.08–1.66) *** | 1.32 (1.12–1.57) *** |
| Secondary education | 0.69 (0.56–0.86) *** | 0.65 (0.53–0.79) *** | 0.60 (0.51–0.71) *** | 0.69 (0.54–0.89) *** | 0.65 (0.53–0.8) *** |
| Higher education | 0.38 (0.3–0.5) *** | 0.37 (0.29–0.47) *** | 0.27 (0.22–0.33) *** | 0.35 (0.25–0.48) *** | 0.37 (0.29–0.48) *** |
| Student | 0.57 (0.38–0.86) *** | 0.49 (0.33–0.73) *** | 0.48 (0.33–0.7) *** | 0.37 (0.21–0.66) *** | 0.51 (0.34–0.77) *** |
| Homemaking | 1.08 (0.84–1.38) | 1.02 (0.8–1.3) | 1.23 (1.01–1.5) ** | 0.90 (0.65–1.24) | 1.01 (0.78–1.3) |
| Other inactive | 2.26 (1.71–3.00) *** | 1.67 (1.26–2.2) *** | 3.31 (2.69–4.08) *** | 1.49 (1.-2.22) *** | 1.65 (1.24–2.21) *** |
| Unemployed between 1 and 11 months | 1.10 (0.83–1.46) | 0.97 (0.75–1.25) | 0.90 (0.71–1.15) | 0.99 (0.71–1.4) | 1.02 (0.77–1.33) *** |
| Unemployed between 12 and 23 months | 1.67 (1.29–2.17) *** | 1.52 (1.2–1.93) *** | 1.45 (1.18–1.8) *** | 1.38 (1.02–1.88) *** | 1.56 (1.2–2.03) *** |
| Unemployed between 24 and 48 months | 1.93 (1.42–2.63) *** | 1.64 (1.23–2.17) *** | 1.84 (1.37–2.46) *** | 1.54 (1.07–2.21) *** | 1.71 (1.2–2.43) *** |
| Equivalent household income | 0.81 (0.74–0.89) *** | 0.77 (0.7–0.84) *** | 0.74 (0.68–0.8) *** | 0.76 (0.67–0.85) *** | 0.76 (0.69–0.84) *** |
| Severe material deprivation | 2.40 (1.62–3.54) *** | 2.13 (1.44–3.17) *** | 2.29 (1.65–3.18) *** | 2.01 (1.2–3.37) *** | 2.11 (1.36–3.29) *** |
| Health-care expenditure | 1.00 (0.99–1.00) | 1.00 (0.99–1.00) | 1.00 (1.00–1.00)* | 1.00 (1.00–1.00)* | 1.00 (1.00–1.00) |
| Fundamental public services | 1.00 (1.00–1.00)*** | 1.00 (1.00–1.00) *** | 1.00 (1.00–1.00) *** | 1.00 (1.00–1.00) *** | 1.00 (1.00–1.00) *** |
p-value < 0.01 = ***; p-value < 0.05 = **; p-value < 0.10 = *. Ref. Reference cathegory. Source: Prepared by the authors based on data from the Survey on Living Conditions. Instituto Nacional de Estadística (2014). http://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176807&menu=ultiDatos&idp=1254735976608. Accesed 27 Dec 2016
The goal of these models is testing our coefficients for sensitivity when good-health individuals are selected at the beginning of their panel. Some of them may fall ill and become unemployed for this reason, but among the unemployed the percentage of individuals reporting good health has increased (from 78.56% in 2007 to 82.44% in 2011; see Table 2). The last model, number 9, estimates an longitudinal, multilevel, ordered logit model in order to assess the extent to which the results found for the variables of interest are affected by the loss of information caused by collapsing self-perceived health from its five original categories into just two.
Table 2.
Self-perceived health for population subsets, Spain 2007–2011
| Collapsed Health | Bad Health % | Good Health % | Total |
|---|---|---|---|
| LEVEL 1: YEARS | |||
| 2007 | 78.56% (N = 3521) | 21.44% (N = 961) | 100% (N = 4482) |
| 2008 | 81.51% (N = 7311) | 18.49% (N = 1658) | 100% (N = 8969) |
| 2009 | 78.93% (N = 7102) | 21.07% (N = 1896) | 100% (N = 8998) |
| 2010 | 79.39% (N = 7131) | 20.61% (N = 1851) | 100% (N = 8982) |
| 2011 | 82.44% (N = 3705) | 17.56% (N = 789) | 100% (N = 4494) |
| Unemployed 2007 | 71.47% (N = 228) | 28.53% (N = 91) | 100% (N = 319) |
| Unemployed 2008 | 73.96% (N = 531) | 26.04% (N = 187) | 100% (N = 718) |
| Unemployed 2009 | 75.49% (N = 878) | 24.51% (N = 285) | 100% (N = 1163) |
| Unemployed 2010 | 77% (N = 974) | 23% (N = 291) | 100% (N = 1265) |
| Unemployed 2011 | 82.22% (N = 555) | 17.78% (N = 120) | 100% (N = 675) |
| LEVEL 2: INDIVIDUAL | |||
| Sex | |||
| Male | 81.84% (N = 14,147) | 18.16% (N = 3139) | 100% (N = 17,286) |
| Female | 78.45% (N =14,623) | 21.55% (N = 4016) | 100% (N = 18,639) |
| Age | |||
| > 25 years | 94.84% (N = 5108) | 5.16% (N = 278) | 100% (N = 5386) |
| 25–34 | 91.65% (N = 5938) | 8.35% (N = 541) | 100% (N = 6479) |
| 35–44 | 82.78% (N = 7131) | 17.22% (N = 1483) | 100% (N = 8614) |
| 45–54 | 73.51% (N = 6714) | 26.49% (N = 242) | 100% (N = 9134) |
| 55–65 | 61.45% (N = 3879) | 38.55% (N = 2433) | 100% (N = 6312) |
| Education level | |||
| Primary | 63.81% (N = 4207) | 36.19% (N = 2386) | 100% (N = 6593) |
| Secondary | 82.43% (N = 15,329) | 17.57% (N = 3267) | 100% (N = 18,596) |
| Higher | 89.26% (N = 8905) | 10.74% (N = 1071) | 100% (N = 9976) |
| Employment Status | |||
| Employed | 85.39% (N = 18,571) | 14.61% (N = 3177) | 100% (N = 21,748) |
| Unemployed | 76.47% (N = 3166) | 23.53% (N = 974) | 100% (N = 4140) |
| Student | 96.44% (N = 3111) | 3.56% (N = 115) | 100% (N = 3226) |
| Homemaking | 66.38% (N = 2654) | 33.62% (N = 1344) | 100% (N = 3998) |
| Other inactive | 45.03% (N = 1265) | 54.97% (N = 1544) | 100% (N = 2809) |
| Unemployed <12 months | 85.73% (N = 3455) | 14.27% (N = 575) | 100% (N = 4030) |
| Unemployed 13–23 months | 76.91% (N = 3300) | 23.09% (N = 991) | 100% (N = 4291) |
| Unemployed 24–48 months | 72.21% (N = 2009) | 27.84% (N = 775) | 100% (N = 2784) |
| Equivalent household income | |||
| (−49,189.42, -29,331.98€) | 33.33% (N = 2) | 66.67% (N = 4) | 100% (N = 6) |
| -9474.53€ | 69.23% (N =36) | 30.77% (N = 16) | 100% (N = 52) |
| 10,382.91€ | 74.21% (N = 8697) | 25.79% (N = 3023) | 100% (N = 1172) |
| 30,240.35€ | 82.39% (N =18,036) | 17.61% (N = 3855) | 100% (N = 21,891) |
| 50,097.79€ | 88.34% (N =1781) | 11.66% (N = 235) | 100% (N = 2016) |
| 69,955.23€ | 90.34% (N = 187) | 9.66% (N = 20) | 100% (N = 207) |
| 89,812.67€ | 92.31% (N =24) | 7.69% (N = 2) | 100% (N = 26) |
| 129,527.60€ | 100% (N = 4) | 0% (N = 0) | 100% (N = 4) |
| 149,385.00€ | 100% (N =3) | 0% (N = 0) | 100% (N = 3) |
| Severe material deprivation | 58.95% (N = 484) | 41.05% (N = 337) | 100% (N = 821) |
| LEVEL 3:REGIONS | |||
| Galicia | 71.08% (N = 1870) | 28.92% (N = 761) | 100% (N = 2631) |
| Asturias | 82.8% (N = 1386) | 17.2% (N = 288) | 100% (N = 1674) |
| Cantabria | 81% (N = 942) | 19% (N = 221) | 100% (N = 1163) |
| Pais vasco | 85.5% (N = 1533) | 14.5% (N = 260) | 100% (N = 1793) |
| Navarra | 87.14% (N = 1226) | 12.86% (N = 181) | 100% (N = 1407) |
| Rioja | 82.4% (N = 1072) | 17.6% (N = 229) | 100% (N = 1301) |
| Aragón | 80.58% (N = 1324) | 19.42% (N = 319) | 100% (N = 1643) |
| Madrid | 82.27% (N = 2515) | 17.73% (N = 542) | 100% (N = 3057) |
| Castilla y León | 77.78% (N = 1869) | 22.22% (N = 534) | 100% (N = 2403) |
| Castilla la Mancha | 81.47% (N = 1609) | 18.53% (N = 366) | 100% (N = 1975) |
| Extremadura | 82.2% (N = 1288) | 17.8% (N = 279) | 100% (N = 1567) |
| Cataluña | 81.24% (N = 2846) | 18.76% (N = 657) | 100% (N = 3503) |
| Comunidad Valenciana | 80.9% (N = 2393) | 19.1% (N = 565) | 100% (N = 2958) |
| Baleares | 83.86% (N = 904) | 16.14% (N = 174) | 100% (N = 1078) |
| Andalucía | 78.01% (N = 3359) | 21.99% (N = 947) | 100% (N = 4306) |
| Murcia | 79.31% (N = 1296) | 20.69% (N = 338) | 100% (N = 1634) |
| Canarias | 73.03% (N = 1338) | 26.97% (N = 494) | 100% (N = 1832) |
Source: Prepared by the authors based on data from the Survey on Living Conditions. Instituto Nacional de Estadística (2014) http://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176807&menu=ultiDatos&idp=1254735976608. Accessed 5 Jan 5 2017
All models of multilevel regression were planned and executed using the STATA 14.0 statistical software package [74].
Results
Table 2 shows the data regarding self-perceived health according to individual, family, and regional variables. The variable of interest at the individual level (activity status) shows that inactive (42.4%), homemaking (33.6%), or unemployed individuals (23.5%) report having worse health than those who are employed (14.6%) or studying (3.6%). Among the unemployed, the time spent with no employment affects how one’s health is perceived: the proportion of the unemployed who report good health when being unemployed for less than 12 months is higher (85.7%) than for those who have been unemployed for between one and two years (76.9%). This percentage is lowest among those who have been unemployed for between two and four years (72.16%).
As for the rest of individual variables, the analysis points at males having better self-perception of health (81.8%) than females (78.4%). Education level is associated with improved perception of one’s health, and age is linked with worsened perception of one’s health. As family income level increases, so does reported health, and being a member of a severely materially deprived household has a strong negative relationship with subjective health.
Table 3 shows the results of the first four multilevel models, which calculates the modulating effect of individual and regional variables on the association between unemployment and self-perceived health, depending on whether chronic illness is being controlled for or not (Models 1 and 2) or by dropping all the chronically ill people from the sample as in Model 3. As it has been described in the methodology section, in model 4 unemployed individuals at the beginning of panel are dropped.
Table 4 shows the results of the same sequence of models when the subsample contains those individuals who reported having good or very good health at the beginning of the panel. It also shows the results of the longitudinal, multilevel, ordered logit model.
The multilevel models used to estimate the association of long- and very-long-duration unemployment with the self-perceived health of individuals between 2007 and 2011 shows that long- and very–long-duration unemployment are associated with how health is subjectively perceived. Figure 1 shows the odds ratios for long- and very-long duration unemployment and other variables of interest in the main models.
Fig. 1.
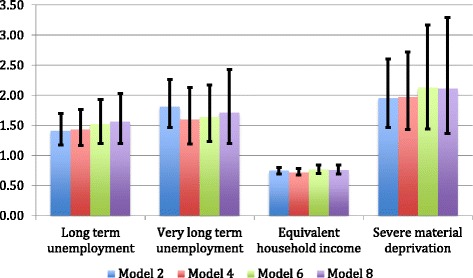
Odds ratios for the association between long and very-long term unemployment, income, job insecurity, poverty, and self-perceived health in Spain (2007–2011). Source: Prepared by the authors based on data from the Survey on Living Conditions. Instituto Nacional de Estadística (2014). http://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176807&menu=ultiDatos&idp=1254735976608. Accessed 27 Dec 2016
By comparing the results of the first three estimations, it is apparent that there are no significant changes between the odds ratios of the variables of interest (Table 3). For instance, and regarding the long-term unemploment (between 12 and 23 months) and very-long-term unemployment (between 24 and 48 months) variables, odds ratios for models 1, 2, and 3 are 1.61, 1.41, and 1.37 for long-term unemployment, and 2.32, 1.81 and 1.72 for very-long-term unemployment. To sum up, after excluding chronically ill subjects from the sample the model remains stable regarding the relationship between long-term and very-long-term unemployment, income, poverty, and poor perceived health.
In addition, model 4 exclude subjects who were unemployed at the beginning of the panel. The odds ratios for these models are also similar to those of the full sample concerning the three individual variables of interest and the two regional variables (Table 3). For instance, for the variables concerning long-term and very-long-term unemployment odds ratios are 1.43 and 1.60. The analysis of the subsample that included only those individuals reporting good or very good at the beginning of the panel shows that results remain stable (Table 4, Fig. 1). In Model 8, in which subjects reported good health, and were not unemployed at the beginning of the panel, the odds ratio for the long-term unemployed (between 12 and 23 months) is 1.56, which increases for the very-long-term unemployed (between 24 and 48 months), 1.71.
The estimation performed with the longitudinal ordered logit model (Model 9) yields similar odds ratios in the variables of interest to those of the base model. For instance, concerning long-term and very-long-term unemployment, coefficients are 1.41 and 1.81 in Model 2, and 1.22 and 1.60 in the longitudinal ordered model. These results hold for all other variables of interest across all estimations.
In basic models, and controlling for chronic illness (numbers 2 and 6), the household income variable was associated with a reduction of the odds of declaring bad health of 25% and 23% respectively for each additional percentage point in income. Being a member of a household with severe material deprivation increased by 95% and 113% respectively the odds of perceiving one’s health as bad compared with households not presenting severe material deprivation. In Tables 3 and 4 and the Fig. 1, these data are consistent across the models. This is the case of Model 4, which excluded the unemployed at the beginning of the panel (28% increase for income and 97% decrease for severe material deprivation) and of the model dealing only with individuals in good or very good health, excluding the unemployed at the beginning of the panel (24% increase for income and 111% decrease for severe material deprivation, Model 8). The rest of individual variables behaved according to what has been described in the previous literature.
The analysis of VPC in the basic model number 2 showed that 1.4% of variance in the odds of reporting bad health can be attributed to the modulating effect that regional variables exert on the association between unemployment and self-perceived health. The calculation of the MOR shows that, when comparing two randomly selected regions, the likelihood of declaring bad health was 34% higher in one than in the other (in the median case).
Results regarding the influence of regional public expenditure on the association between long- and very-long-term unemployment and self-perception of health show that expenditure on essential public services is associated with better self perceived health: for each additional percentage point of increase in health-care, education, and social protection the odds of declaring bad health decreases by 0.01% (in every model, 1–9). Public health-care expenditure per capita did not yield statistically significant results.
Discussion
Before discussing our results, some limitations must be acknowledged. Firstly, and given the bidirectional nature of the relationship between the variables of interest and perceived health, this study is not able to establish a causal relationship between the associations we have identified [75]. This becomes particularly relevant regarding the link between bad perceived health and long-term unemployment.
The literature has identified two processes linking bad perceived health and unemployment. On the one hand, the causal hypothesis suggests that unemployment is a risk factor for health. On the other, the selection hypothesis states that it is poor health which excludes workers from the labor market [76–78]. Three metaanalyses concluded that longitudinal studies provide enough evidence for both the causal and the selection hypotheses [79–81]. More recently, some studies have yielded certain evidence supporting the latter [82, 83]. The work of Reeves et al. (2014) suggests that the financial crisis in Europe has had particularly severe effects on people with bad health, who are more prone to losing their jobs when market conditions worsen [84]. Heggebø and Dahl (2015), however, pointed out that while the selection effect has remained constant throughout time in the EU, in countries like Spain, where the financial crisis has brought about a swift increase in unemployment and high rates of unemployment population, a change has taken place in the breakdown of the unemployed population, which now includes a higher percentage of individuals who report to have good health [85]. This overrepresentation of the healthy among the unemployed can be interpreted as a consequence of a massive, sudden loss of employment, and supports the causal hypothesis. During the first years after the onset of the crisis (which is the period covered in our analysis), the destruction of employment affected temporary workers on a greater measure, since their lay-off costs are smaller than those of permanent workers [10].
Our results are consistent with this hypothesis. The percentage of unemployed individuals reporting good health has increased from 78.56% in 2007 to 82.44% in 2011. In addition, when only considering the subsample reporting good health at the beginning of the study, results show a robust association between long-term unemployment and bad perceived health, which increases with the time spent unemployed.
However, the selection effect may well play an important role in long-term unemployment, particularly when employers use poor health as an indicator for low productivity in their recruitment processes, in a context of low labor demand brought about by the financial crisis [84]. Subsequent studies should explore the evolution of unemployment since the end of the financial crisis (2014), in a context of sustained creation of jobs, and contemplate in their methodological approaches the need to analyze the endogenic nature of the association between unemployment and health, for example by using structural equation modeling [27].
Secondly, although self-perceived health is one of the best global health indicators, several significant dissonances have been described with objective indicators of morbimortality when populations have been compared [86, 87]. Amartya Sen (2009) suggested employing a social context to examine the statistics on the perception of bad health, with a critical analysis of positional perspectives [88]. Contemplating some features of the labor market which may amount to risk factors for health, like job insecurity or involuntary part-time work, might provide a more thorough and detailed analysis of labor markets and their influence on health.
Yet another limitation originates from the SLC not including individual lifestyle information. In this regard it only records data concerning self-perceived health, chronic illness, and limitations for activity in daily life. This is however the only survey conducted in Spain to offer longitudinal information about the activity and employment status of individuals.
The present study offers evidence of the association between long- and very-long-term unemployment, loss of family income, and living in a household that is severely materially deprived with bad self-perception of health. All estimated models show similar and consistent results for all variables of interest.
According to our results, bad perceived health is associated with long- and very-long-term unemployment, and worsens as the time spent unemployed increases. This is in agreement with part of the literature published in this regard before the onset of the financial crisis [16–18, 22, 23] and with the work of Urbanos and González (2015), regarding the Spanish situation after the crisis [19].
Some evidence exists that certain health conditions and causes of mortality (such as suicide) increase due to the deleterious effect of recessions on mental health [2, 5]. Ähs and Westerling (2005) compared self-perceived bad health during times of low (1983–1989) and high (1992–1997) rates of unemployment in Sweden and, after controlling for sociodemographic factors and long-term health conditions, differences in self-perceived health between the employed and the unemployed were higher at times of high unemployment [89]. Drydakis (2015) recently published his results regarding the negative impact of unemployment on the mental health and self-perceived health of Greek individuals in the period 2008–2013 [90].
However, our study revealed that, by following the professional history of individuals along four years since the onset of the crisis, a robust association appears between long- and very-long-term unemployment and the deterioration of the perception of their own health, after controlling for other individual and regional variables.
Our results also show that, after only one year of unemployment, perceived health worsens. One tentative explanation for this phenomenon is that a change in expectations takes place when the reality of being unemployed and losing income settles in and reveal itself as a permanent situation, thus increasing uncertainty about the future and causing stress and anxiety [91].
Labor policies aimed at reducing the long-term unemployment rate as a strategy to improve the health of the population are particularly attractive, since they are synergistic with macroeconomic policies of fiscal consolidation and sustained economic growth [92]. In a recent research, Doménech and González Páramo (2017) have shown how a reduction of 8% in structural unemployment would in the long term mean an increase in GDP and public expenditure per working-age population of more than 20% [93]. Additionally, according to the results of this study, health would likely be improved by the reduction of long-term unemployment and the reduction of social deprivation.
In the present study household income decreased the odds of reporting bad health by 16% to 28% (depending on the model) for each percentage point of income increase. Conversely, being member of a household with severe material deprivation affected the perception of health and increased the odds of perceiving one’s health as bad by 70% to 140% (depending on the model). These results are in agreement with several others that found a positive correlation between unemployment, low social and economic level, and bad health [25, 28, 78, 94–97]. In Spain, the link between material deprivation and bad health was already proved in studies performed both prior to the onset of the financial crisis [36] and after [37].
The fact that severe material deprivation is associated with bad health is probably due to two mechanisms: an increase in the general susceptibility to illness and a set of specific factors, which increase the risk of death (healthy lifestyle, overweight, obesity, alcohol consumption, smoking, etc. [98]. The work of Ayllón and Gábos (2016) suggests that a vicious circle is established in which living in conditions of material deprivation for a long time erodes the human and social capital of individuals and worsens their health [99]. Long-term unemployment thus breeds poverty and material deprivation, which in turn decrease the chances of entering the labor market.
Regional per capita expenditure on essential public services is associated with better perceived health, although its influence is limited, whereas per capita expenditure on health-care did not show to have any significant relationship with self-perceived health. These results do not agree with those of other authors [40, 41, 100]. For instance, Ng and Muntaner (2015) found that expenditure on health-care, social services, and education reduced mortality rates in the provinces of Canada [101]. Huijts et al. (2014), on the other hand, did not find a link between social protection policies, health-care expenditure, and perceived health [48].
Conclusions
To conclude, this is the first longitudinal study carried out in Spain after the financial crisis to analyze the joint association of long-term unemployment, income, poverty, and severe material deprivation (closely derived from long-term unemployment) with bad perceived health. Our results provide robust evidence that long-term unemployment is related to bad health.
Finally, by using multilevel models we were able to find robust estimators regarding the relationship between social and health-care public expenditure policies in the Spanish regions and perceived health, which turned out to be limited in the case of the former and non significant for the latter.
Our results are particularly relevant for the design of public policies aimed at reducing the weight of social determinants in health. Specifically, these results should be considered when formulating active employment policies, safety nets for the long-term unemployed, and policies of redistribution focused on families with low-income levels and material deprivation.
Acknowledgements
The authors are grateful to the Health Department of the Andalusian Board for the funding.
Funding
This work was supported by the Health Department of the Andalusian Board (2013–2015) under Grant PI-0682-2012.
The Health Department did not participate in the design of the study, collection, analysis, and interpretation of data nor in writing the manuscript.
The cost of translation of the work was supported by “Research Aid Program of the Faculty of Economics and Business Sciences of the University of Granada for the revision of scientific texts”.
Availability of data and materials
The dataset generated and analysed during the current study is available in the “Repositorio Institucional de la Universidad de Granada” repository, http://hdl.handle.net/10481/45608
Martín, J., Benítez, V. and López del Amo, M.P. 2017. “Longitudinal Life Conditions Survey Database 2007-2011. Influence of unemployment length, poverty and social public expenditure on self perceived health in Spain”. From the publicly accessible microdata of the Survey on Living Conditions. Spanish National Statistics Institute. Applied Economics Department, University of Granada: Granada. Available at: http://hdl.handle.net/10481/45608. Accessed 30 march 2017.
The datasets analysed during the current study are available at:
Instituto Nacional de Estadística (2014). Encuesta de Condiciones de Vida. http://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176807&menu=ultiDatos&idp=1254735976608. Accessed 23 Dec 2016.
Fundación BBVA e Ivie (Instituto Valenciano de Investigaciones Económicas). Gasto en los servicios públicos fundamentales en España y sus comunidades autónomas (2002–2013). Mayo de 2015. http://www.fbbva.es/TLFU/tlfu/esp/areas/econosoc/bbdd/gastos_servicios_publicos_comunidades.jsp Accessed 23 Dec 2016.
Fundación BBVA e Ivie (Instituto Valenciano de Investigaciones Económicas). Gasto sanitario público en España. Agosto de 2013. http://www.ivie.es/es/banco/gasto-sanitario-publico.php. Accessed 23 Dec 2016.
The stata commands run to estimate the models in Stata 14 are:
xtset panelvar timevar [, tsoptions] (to declare longitudinal nature of data).
melogit depvar fe_equation [|| re_equation] [|| re_equation ...] [, options] (to estimate logit model).
meologit depvar fe_equation [|| re_equation] [|| re_equation ...] [, options] (to estimate logit ordered model).
Abbreviations
- AROPE
At Risk Of Poverty or social Exclusion
- MOR
Median Odds Ratio
- SLC
Survey on Living Conditions
- VPC
Variance Partition Coefficient
Authors’ contributions
M. Puerto López del Amo González MPLAG, Vivian Benítez VB, José J. Martín JJM. All the authors above have taken part in the conception, design and writing of this article. More specifically, JJM coordinated the development of the research, the writing of the paper and its critical review; VB collected the data, estimated the multilevel models, reviewed the literature, and drafted the text; and MPLAG designed the project, reviewed the literature and drafted the text. All authors have contributed to the interpretation of results, have reviewed all aspects of the research, and have approved the final version.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
M. Puerto López del Amo González, Phone: +34616285074, Email: puerto.lopezdelamo@hotmail.es.
Vivian Benítez, Phone: +34687504866, Email: vivben75@gmail.com.
José J. Martín-Martín, Phone: +34677842143, Email: jmartin@ugr.es, Email: josejesus.martin@gmail.com
References
- 1.Stuckler D, Basu S, Suhrcke M, Coutts A, McKee M. The public health effect of economic crises and alternative policy responses in Europe: an empirical analysis. Lancet. 2009;374(9686):315–323. doi: 10.1016/S0140-6736(09)61124-7. [DOI] [PubMed] [Google Scholar]
- 2.Suhrcke M, Stuckler D. Will the recession be bad for our health? It depends. Soc Sci Med. 2012;74(5):647–653. doi: 10.1016/j.socscimed.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 3.De Vogli R. The financial crisis, health and health inequities in Europe: the need for regulations, redistribution and social protection. Int J Equity Health. 2014;13:58. doi: 10.1186/s12939-014-0058-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jackson T. Health and the economic crisis. BMJ. 2013;346:f4140. doi: 10.1136/bmj.f4140. [DOI] [Google Scholar]
- 5.Karanikolos M, Mladovsky P, Cylus J, Thomson S, Basu S, Stuckler D, et al. Financial crisis, austerity, and health in Europe. Lancet. 2013;381(9874):1323–1331. doi: 10.1016/S0140-6736(13)60102-6. [DOI] [PubMed] [Google Scholar]
- 6.McKee M, Karanikolos M, Belcher P, Stuckler D. Austerity: a failed experiment on the people of Europe. Clin Med (Lond) 2012;12(4):346–350. doi: 10.7861/clinmedicine.12-4-346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Instituto Nacional de Estadística. Encuesta de Población Activa. 2016. http://www.ine.es/jaxiT3/Tabla.htm?t=4887&L=0. Accessed 3 Dec 2016.
- 8.Pérez García F, Cucarella Tormo V, Hernández Lahiguera L. Servicios públicos, diferencias territoriales e igualdad de oportunidades. Valencia: Fundación BBVA-Ivie; 2015.
- 9.Eurostat. Labour Force Survey. http://ec.europa.eu/eurostat/web/lfs/data/main-tables# Accessed 23 Dec 2016.
- 10.Muñoz de Bustillo R. Paisajes después de la batalla. El mercado de trabajo en España tras la Gran Recesión. Rev. Esp. Terc. Sect. 2016;32(Cuatrimestre I):17–45.
- 11.Layard R, Nickell S, Jackman R. Unemployment: macroeconomic performance and the labour market. Oxford: Oxford University Press; 1991. [Google Scholar]
- 12.Gradín C, Cantó O, del Río C. Unemployment and spell duration during the great recession in the EU. Int J Manpow. 2015;36(2):216–235. doi: 10.1108/IJM-10-2012-0152. [DOI] [Google Scholar]
- 13.Organization for the Economic Cooperation and Development . In it together: why less inequality benefits all. France: OECD Publishing; 2015. [Google Scholar]
- 14.Goerlich Gisbert FJ. Distribución de la renta, crisis económica y políticas redistributivas. Bilbao: Fundación BBVA; 2016. [Google Scholar]
- 15.Llano Ortiz JC. El estado de la pobreza. 5° informe. Seguimiento del indicador de riesgo de pobreza y exclusión social en España (2009–2014) Madrid: EAPN-España; 2015. [Google Scholar]
- 16.Brenner MH. Duration of unemployment and self-perceived health in Europe. Directorate-General for Employment, Social Affairs and Inclusion. Luxembourg: European Union; 2016. [Google Scholar]
- 17.Romeu LR. Effects of short- and long-term unemployment on health satisfaction: evidence from German data. Appl Econ. 2006;38(20):2335–2350. doi: 10.1080/00036840500427692. [DOI] [Google Scholar]
- 18.Herbig B, Dragano N, Angerer P. Health in the long-term unemployed. Dtsch Arztebl Int. 2013;110(23–24):413–419. doi: 10.3238/arztebl.2013.0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Urbanos RM, González B. The influence of the economic crisis on the association between unemployment and health: an empirical analysis for Spain. Eur J Health Econ. 2015;16(2):175–184. doi: 10.1007/s10198-014-0563-y. [DOI] [PubMed] [Google Scholar]
- 20.Galić Z, ŠVerko Z. Unemployment, (re)employment, and health. Rev Psychol. 2008;15(1–2):3–10. [Google Scholar]
- 21.Clark AE. A Note on Unhappiness and Unemployment Duration. IZA Discussion Paper. 2006; 2046. https://pdfs.semanticscholar.org/e91a/ce7c2b39f1f89cc323bd94cd288c49235cb6.pdf. Accessed 6 Jan 2017.
- 22.Couch KA, Reznik GL, Tamborini CR, Iams HM. Economic and health implications of long-term unemployment: earnings, disability benefits, and mortality. Res Labor Econ. 2013;38:259–305. doi: 10.1108/S0147-9121(2013)0000038008. [DOI] [Google Scholar]
- 23.Gaspar K. The relationship between unemployment and health. Central European University. Department of Economics. In partial fulfillment of the requirements for the degree of Masters of Arts. Budapest, Hungary. 2009. http://econ.core.hu/file/download/szirak11/gaspar.pdf. Accessed 5 Jan 2017.
- 24.Tøge AG, Blekesaune M. Unemployment transitions and self-rated health in Europe: a longitudinal analysis of EU-SILC from 2008 to 2011. Soc Sci Med. 2015;143:171–178. doi: 10.1016/j.socscimed.2015.08.040. [DOI] [PubMed] [Google Scholar]
- 25.Arber S, Fenn K, Meadows R. Subjective financial well-being, income and health inequalities in mid and later life in Britain. Soc Sci Med. 2014;100:12–20. doi: 10.1016/j.socscimed.2013.10.016. [DOI] [PubMed] [Google Scholar]
- 26.Abikulova AK, Tulebaev KA, Akanov AA, Turdalieva BS, Kalmahanov SB, Kumar AB, et al. Inequalities in self-rated health among 45+ year-olds in Almaty, Kazakhstan: a cross-sectional study. BMC Public Health. 2013;13:654. doi: 10.1186/1471-2458-13-654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Aittomäki A, Martikainen P, Laaksonen M, Lahelma E, Rahkonen O. Household economic resources, labour-market advantage and health problems - a study on causal relationships using prospective register data. Soc Sci Med. 2012;75(7):1303–1310. doi: 10.1016/j.socscimed.2012.05.015. [DOI] [PubMed] [Google Scholar]
- 28.Aittomäki A, Martikainen P, Rahkonen O, Lahelma E. Household income and health problems during a period of labour-market change and widening income inequalities - a study among the Finnish population between 1987 and 2007. Soc Sci Med. 2014;100:84–92. doi: 10.1016/j.socscimed.2013.10.023. [DOI] [PubMed] [Google Scholar]
- 29.Leskošek V. Social determinants of health: the indicators for measuring the impact of poverty on health. Slov J Public Health. 2011;51:21–32. [Google Scholar]
- 30.Schütte S, Chastang J-F, Parent-Thirion A, Vermeylen G, Niedhammer I. Association between socio-demographic, psychosocial, material and occupational factors and self-reported health among workers in Europe. J Public Health (Oxf) 2014;36(2):194–204. doi: 10.1093/pubmed/fdt050. [DOI] [PubMed] [Google Scholar]
- 31.Saito M, Kondo K, Kondo N, Abe A, Ojima T, Suzuki K, et al. Relative deprivation, poverty, and subjective health: JAGES cross-sectional study. PLoS One. 2014;9(10):e111169. doi: 10.1371/journal.pone.0111169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kiely KM, Leach LS, Olesen SC, Butterworth P. How financial hardship is associated with the onset of mental health problems over time. Soc Psychiatry Psychiatr Epidemiol. 2015;50(6):909–918. doi: 10.1007/s00127-015-1027-0. [DOI] [PubMed] [Google Scholar]
- 33.Pillas D, Marmot M, Naicker K, Goldblatt P, Morrison J, Pikhart H. Social inequalities in early childhood health and development: a European-wide systematic review. Pediatr Res. 2014;76(5):418–424. doi: 10.1038/pr.2014.122. [DOI] [PubMed] [Google Scholar]
- 34.Rajmil L, Fernandez de Sanmamed M-J, Choonara I, Faresjö T, Hjern A, Kozyrskyj AL, et al. Impact of the 2008 economic and financial crisis on child health: a systematic review. Int J Environ Res Public Health. 2014;11(6):6528–6546. doi: 10.3390/ijerph110606528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Groffen DAI, Bosma H, van den Akker M, Kempen GIJM, van Eijk JTM. Material deprivation and health-related dysfunction in older Dutch people: findings from the SMILE study. Eur J Pub Health. 2008;18(3):258–263. doi: 10.1093/eurpub/ckm119. [DOI] [PubMed] [Google Scholar]
- 36.Borrell C, Muntaner C, Benach J, Artazcoz L. Social class and self-reported health status among men and women: what is the role of work organisation, household material standards and household labour? Soc Sci Med. 2004;58(10):1869–1887. doi: 10.1016/S0277-9536(03)00408-8. [DOI] [PubMed] [Google Scholar]
- 37.Blázquez M, Cottini E, Herrarte A. The socioeconomic gradient in health: how important is material deprivation? J Econ Inequal. 2013;12:239–264. doi: 10.1007/s10888-013-9248-5. [DOI] [Google Scholar]
- 38.Maruthappu M, Ng KY, Williams C, Atun R, Zeltner T. Government health care spending and child mortality. Pediatrics. 2015;135(4):e887–e894. doi: 10.1542/peds.2014-1600. [DOI] [PubMed] [Google Scholar]
- 39.Maruthappu M, Shalhoub J, Tariq Z, Williams C, Atun R, Davies AH, et al. Unemployment, government healthcare spending, and cerebrovascular mortality, worldwide 1981-2009: an ecological study. Int J Stroke. 2015;10(3):364–371. doi: 10.1111/ijs.12408. [DOI] [PubMed] [Google Scholar]
- 40.Bradley EH, Elkins BR, Herrin J, Elbel B. Health and social services expenditures: associations with health outcomes. BMJ Qual Saf. 2011;20(10):826–831. doi: 10.1136/bmjqs.2010.048363. [DOI] [PubMed] [Google Scholar]
- 41.Navarro V, Muntaner C, Borrell C, Benach J, Quiroga A, Rodríguez-Sanz M, et al. Politics and health outcomes. Lancet. 2006;368(9540):1033–1037. doi: 10.1016/S0140-6736(06)69341-0. [DOI] [PubMed] [Google Scholar]
- 42.Bambra C, Eikemo TA. Welfare state regimes, unemployment and health: a comparative study of the relationship between unemployment and self-reported health in 23 European countries. J Epidemiol Community Health. 2009;63(2):92–98. doi: 10.1136/jech.2008.077354. [DOI] [PubMed] [Google Scholar]
- 43.Ferrarini T, Nelson K, Sjöberg O. Unemployment insurance and deteriorating self-rated health in 23 European countries. J Epidemiol Community Health. 2014; 10.1136/jech-2013-203721. [DOI] [PMC free article] [PubMed]
- 44.Maruthappu M, Ng K, Williams C, Atun R, Agrawal P, Zeltner T. The association between government healthcare spending and maternal mortality in the European Union, 1981–2010: a retrospective study. BJOG: Int J Obstet Gy. 2015;122(9):1216–1224. doi: 10.1111/1471-0528.13205. [DOI] [PubMed] [Google Scholar]
- 45.Maruthappu M, Da Zhou C, Williams C, Zeltner T, Atun R. Unemployment, public-sector health care expenditure and HIV mortality: an analysis of 74 countries, 1981-2009. J Glob Health. 2015;5(1):010403. doi: 10.7189/jogh.05.010403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Maruthappu M, Watkins JA, Waqar M, Williams C, Ali R, Atun R, et al. Unemployment, public-sector health-care spending and breast cancer mortality in the European Union: 1990–2009. Eur J Pub Health. 2015;25(2):330–335. doi: 10.1093/eurpub/cku167. [DOI] [PubMed] [Google Scholar]
- 47.Shahidi FV, Siddiqi A, Muntaner C. Does social policy moderate the impact of unemployment on health? A multilevel analysis of 23 welfare states. Eur J Pub Health. 2016;26(6):1017–1022. doi: 10.1093/eurpub/ckw050. [DOI] [PubMed] [Google Scholar]
- 48.Huijts T, McKee M, Reeves A, Stuckler D. PP45 job loss and self-rated health during the crisis: the mitigating effect of social protection expenditure in 23 European countries. J Epidemiol Community Health. 2014;68(Suppl 1):A65. doi: 10.1136/jech-2014-204726.140. [DOI] [Google Scholar]
- 49.Instituto Nacional de Estadística. Encuesta de Condiciones de Vida. 2014. http://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176807&menu=ultiDatos&idp=1254735976608. Accessed 23 Dec 2016.
- 50.Singh-Manoux A, Martikainen P, Ferrie J, Zins M, Marmot M, Goldberg M. What does self rated health measure? Results from the British Whitehall II and French Gazel cohort studies. J Epidemiol Commun H. 2006;60(4):364–372. doi: 10.1136/jech.2005.039883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Robine JM, Jagger C, Egidi V. Selection of a coherent set of health indicators for the European Union. Phase II: final report. Montpellier (Francia): Euro-REVES; 2002. [Google Scholar]
- 52.Morcillo V, de Lorenzo-Cáceres A, Domínguez P, Rodríguez R, Torijano MJ. Desigualdades en la salud autopercibida de la población española mayor de 65 años. Gac Sanit. 2014;28(6):511–521. doi: 10.1016/j.gaceta.2014.05.008. [DOI] [PubMed] [Google Scholar]
- 53.Jylhä M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Social Sci Med. 2009;69:307–316. doi: 10.1016/j.socscimed.2009.05.013. [DOI] [PubMed] [Google Scholar]
- 54.Sargent-Cox KA, Anstey KJ, Luszcz MA. The choice of self-rated health measures matter when predicting mortality: evidence from 10 years follow-up of the Australian longitudinal study of ageing. BMC Geriatr. 2010;10:18–30. doi: 10.1186/1471-2318-10-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kaplan GA, Goldberg DE, Everson SA, Cohen RD, Salonen R, Tuomilehto J, et al. Perceived health status and morbidity and mortality: evidence from the Kuopio ischaemic heart disease risk factor study. Int J Epidemiol. 1996;25:259–265. doi: 10.1093/ije/25.2.259. [DOI] [PubMed] [Google Scholar]
- 56.van Doorslaer E, Wagstaff A, van der Burg H, Christiansen T, De Graeve D, Duchesne I, et al. Equity in the delivery of health care in Europe and the US. J Health Econ. 2000;19:553–583. doi: 10.1016/S0167-6296(00)00050-3. [DOI] [PubMed] [Google Scholar]
- 57.van Doorslaer E, Koolman X, Jones AM. Explaining income-related inequalities in doctor utilisation in Europe: a decomposition approach. J Health Econ. 2004;13:629–647. doi: 10.1002/hec.919. [DOI] [PubMed] [Google Scholar]
- 58.Sáez M. Condicionantes en la utilización de los servicios de atención primaria. Evidencias empíricas e inconsistencias metodológicas. Gac Sanit. 2003;17:412–419. doi: 10.1016/S0213-9111(03)71778-6. [DOI] [PubMed] [Google Scholar]
- 59.Manor O, Matthews S, Power C. Dichotomous or categorical response? Analysing self-rated health and lifetime social class. Int J Epidemiol. 2000;29:149–157. doi: 10.1093/ije/29.1.149. [DOI] [PubMed] [Google Scholar]
- 60.Aguilar-Palacio I, Carrera-Lasfuentes P, Rabanaque MJ. Salud percibida y nivel educativo en España: tendencias por comunidades autónomas y sexo (2001-2012). Gac Sanit. 2015;29(1):37–43. [DOI] [PubMed]
- 61.Haseli-Mashhadi N, Pan A, Ye X, Wang J, Qi Q, Liu Y, et al. Self-rated health in middle aged and elderly Chinese: distribution, determinants and associations with cardio-metabolic risk factors. BMC Public Health. 2009;9:368. doi: 10.1186/1471-2458-9-368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Mcfadden E, Luben R, Bingham S, Wareham N, Kinmonth AL, Khaw KT. Social inequalities in self-rated health by age: cross-sectional study of 22457 middle-aged men and women. BMC Public Health. 2008;8:230. doi: 10.1186/1471-2458-8-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Norström F, Virtanen P, Hammarström A, Gustafsson PE, Janlert U. How does unemployment affect self-assessed health? A systematic review focusing on subgroup effects. BMC Public Health. 2014;14:1310. doi: 10.1186/1471-2458-14-1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Marmot M, Theorell T. Social class and cardiovascular disease: the contribution of work. Int J Health Serv. 1988;18(4):659–674. doi: 10.2190/KTC1-N5LK-J1PM-9GRQ. [DOI] [PubMed] [Google Scholar]
- 65.Subramanian SV, Kawachi I. Income inequality and health: what have we learned so far? Epidemiol Rev. 2004;26(1):78–91. doi: 10.1093/epirev/mxh003. [DOI] [PubMed] [Google Scholar]
- 66.Lim H, Kimm H, Song IH. The relationship between employment status and self-rated health among wage workers in South Korea: the moderating role of household income. Health Soc Work. 2015;40(1):26–33. doi: 10.1093/hsw/hlu042. [DOI] [PubMed] [Google Scholar]
- 67.OECD. What are equivalence scales. In: OECD Project on Income Distribution and Poverty. 2014. http://www.oecd.org/eco/growth/OECD-Note-EquivalenceScales.pdf. Accessed 6 Jan 2017.
- 68.Guio AC, Gordon D, Marlier E. Measuring material deprivation in the EU: indicators for the whole population and child-specific indicators. Eurostat methodologies and working papers. 2012 edition. Luxembourg: Publications office of the European Union; 2012. http://ec.europa.eu/eurostat/documents/3888793/5853037/KS-RA-12-018-EN.PDF. Accessed 6 Jan 2017.
- 69.Fundación BBVA e Ivie (Instituto Valenciano de Investigaciones Económicas). Gasto en los servicios públicos fundamentales en España y sus comunidades autónomas (2002–2013). 2015. http://www.fbbva.es/TLFU/tlfu/esp/areas/econosoc/bbdd/gastos_servicios_publicos_comunidades.jsp. Accessed 23 Dec 2016.
- 70.Fundación BBVA e Ivie (Instituto Valenciano de Investigaciones Económicas). Gasto sanitario público en España. 2013. http://www.ivie.es/es/banco/gasto-sanitario-publico.php. Accessed 23 Dec 2016.
- 71.Goldstein H. Multilevel Statistical Models. 4. West Sussex: Wiley; 2011. [Google Scholar]
- 72.Goldstein H, Browne W, Rasbash J. Partitioning variation in multilevel models. Underst Stat. 2002;1(4):223–231. doi: 10.1207/S15328031US0104_02. [DOI] [Google Scholar]
- 73.Merlo J, Chaix B, Ohlsson H, Beckman A, Johnell K, Hjerpe P, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health. 2006;60(4):290–297. doi: 10.1136/jech.2004.029454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.STATA. Data analysis and statistical software. 2016. http://www.stata.com/. Accessed 6 Jan 2017.
- 75.Robins JM, Hernán MA. Estimation of the causal effects of time-varying exposures. In: Verbeke G, Davidian M, Fitzmaurice G, Molenberghs G, editors. Longitudinal data analysis. Chapter 23. London: Chapman and Hall; 2008. pp. 553–599. [Google Scholar]
- 76.Heponiemi T, Elovainio M, Manderbacka K, Aalto A-M, Kivimäki M, Keskimäki I. Relationship between unemployment and health among health care professionals: health selection or health effect? J Psychosom Res. 2007;63(4):425–431. doi: 10.1016/j.jpsychores.2007.04.005. [DOI] [PubMed] [Google Scholar]
- 77.Economou A, Nikolaou A, Theodossiou I. Are recessions harmful to health after all?: evidence from the European Union. J Econ Stud. 2008;35(5):368–384. doi: 10.1108/01443580810903536. [DOI] [Google Scholar]
- 78.Lundin A, Lundberg I, Hallsten L, Ottosson J, Hemmingsson T. Unemployment and mortality—a longitudinal prospective study on selection and causation in 49321 Swedish middle-aged men. J Epidemiol Community Health. 2010;64(01):22–28. doi: 10.1136/jech.2008.079269. [DOI] [PubMed] [Google Scholar]
- 79.McKee-Ryan F, Song Z, Wanberg CR, Kinicki AJ. Psychological and physical well-being during unemployment: a meta-analytic study. J Appl Psychol. 2005;90(1):53–76. doi: 10.1037/0021-9010.90.1.53. [DOI] [PubMed] [Google Scholar]
- 80.Paul KI, Moser K. Unemployment impairs mental health: meta-analyses. J Vocat Behav. 2009;74(3):264–282. doi: 10.1016/j.jvb.2009.01.001. [DOI] [Google Scholar]
- 81.Roelfs DJ, Shor E, Davidson KW, Schwartz JE. Losing life and livelihood: a systematic review and meta-analysis of unemployment and all-cause mortality. Soc Sci Med. 2011;72(6):840–854. doi: 10.1016/j.socscimed.2011.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.van Rijn RM, Robroek SJW, Brouwer S, Burdorf A. Influence of poor health on exit from paid employment: a systematic review. Occup Environ Med. 2014;71(4):295–301. doi: 10.1136/oemed-2013-101591. [DOI] [PubMed] [Google Scholar]
- 83.Minton JW, Pickett KE, Dorling D. Health, employment, and economic change, 1973-2009: repeated cross sectional study. BMJ. 2012;344:e2316. doi: 10.1136/bmj.e2316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Reeves A, Karanikolos M, Mackenbach J, McKee M, Stuckler D. Do employment protection policies reduce the relative disadvantage in the labour market experienced by unhealthy people? A natural experiment created by the great recession in Europe. Soc Sci Med. 2014;121:98–108. doi: 10.1016/j.socscimed.2014.09.034. [DOI] [PubMed] [Google Scholar]
- 85.Heggebø K, Dahl E. Unemployment and health selection in diverging economic conditions: compositional changes? Evidence from 28 European countries. Int J Equity Health. 2015;14:121. doi: 10.1186/s12939-015-0258-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Sen A. Health: perception versus observation. BMJ. 2002;324(7342):860–861. doi: 10.1136/bmj.324.7342.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Castro A, Espinosa I, Rodríguez P, Santos P. Relación entre el estado de salud percibido e indicadores de salud en la población española. Int J Clin Health Psychol. 2007;7:883–898. [Google Scholar]
- 88.Sen A. The idea of justice. New York: Penguin Press; 2009. [Google Scholar]
- 89.Åhs A, Westerling R. Self-rated health in relation to employment status during periods of high and of low levels of unemployment. Eur J Pub Health. 2006;16(3):294–304. doi: 10.1093/eurpub/cki165. [DOI] [PubMed] [Google Scholar]
- 90.Drydakis N. The effect of unemployment on self-reported health and mental health in Greece from 2008 to 2013: a longitudinal study before and during the financial crisis. Soc Sci Med. 2015;128:43–51. doi: 10.1016/j.socscimed.2014.12.025. [DOI] [PubMed] [Google Scholar]
- 91.Marmot M, Friel S, Bell R, Houweling TA, Taylor S. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet. 2008;372(9650):1661–1669. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- 92.BBBVA Research. “Hacia un mercado de trabajo más eficiente y equitativo.” Observatorio Económico de España. 2016. Accessed 23 July. http://goo.gl/xbYmdQ.
- 93.Doménech R, González-Páramo JM. Estabilidad presupuestaria y reformas estructurales en España: lecciones de la crisis y opciones de futuro. BBVA Research. https://www.bbvaresearch.com/wp-content/uploads/2017/06/EWatch_maq_esp.pdf. Accessed 23 July 2017.
- 94.Catalano R, Bellows B. Commentary: if economic expansion threatens public health, should epidemiologists recommend recession? Int J Epidemiol. 2005;34(6):1212–1213. doi: 10.1093/ije/dyi145. [DOI] [PubMed] [Google Scholar]
- 95.Gallo WT, Bradley EH, Falba TA, Dubin JA, Cramer LD, Bogardus ST, et al. Involuntary job loss as a risk factor for subsequent myocardial infarction and stroke: findings from the health and retirement survey. Am J Ind Med. 2004;45(5):408–416. doi: 10.1002/ajim.20004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lawlor DA, Mishra GD. Family matters: designing, analysing and understanding family based studies in life course epidemiology. 1. Oxford; New York: Oxford University Press; 2009. [Google Scholar]
- 97.Larson K, Halfon N. Family income gradients in the health and health care access of US children. Matern Child Health J. 2010;14(3):332–342. doi: 10.1007/s10995-009-0477-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Benach J, Yasui Y, Borrell C, Sáez M, Pasarin MI. Material deprivation and leading causes of death by gender: evidence from a nationwide small area study. J Epidemiol Community Health. 2001;55(4):239–245. doi: 10.1136/jech.55.4.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Ayllón S, Gábos A. The Interrelationships between the Europe 2020 Poverty and Social Exclusion Indicators. Soc Indic Res 2016;1–25.
- 100.De Vogli R. Unemployment and suicides during the recession in Italy. BMJ. 2013;347:f4908. doi: 10.1136/bmj.f4908. [DOI] [PubMed] [Google Scholar]
- 101.Ayllón S, Gábos A. The Interrelationships between the Europe 2020 Poverty and Social Exclusion Indicators. Soc Indic Res. 2016;130:1025. https://doi.org/10.1007/s11205-015-1212-2.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The dataset generated and analysed during the current study is available in the “Repositorio Institucional de la Universidad de Granada” repository, http://hdl.handle.net/10481/45608
Martín, J., Benítez, V. and López del Amo, M.P. 2017. “Longitudinal Life Conditions Survey Database 2007-2011. Influence of unemployment length, poverty and social public expenditure on self perceived health in Spain”. From the publicly accessible microdata of the Survey on Living Conditions. Spanish National Statistics Institute. Applied Economics Department, University of Granada: Granada. Available at: http://hdl.handle.net/10481/45608. Accessed 30 march 2017.
The datasets analysed during the current study are available at:
Instituto Nacional de Estadística (2014). Encuesta de Condiciones de Vida. http://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176807&menu=ultiDatos&idp=1254735976608. Accessed 23 Dec 2016.
Fundación BBVA e Ivie (Instituto Valenciano de Investigaciones Económicas). Gasto en los servicios públicos fundamentales en España y sus comunidades autónomas (2002–2013). Mayo de 2015. http://www.fbbva.es/TLFU/tlfu/esp/areas/econosoc/bbdd/gastos_servicios_publicos_comunidades.jsp Accessed 23 Dec 2016.
Fundación BBVA e Ivie (Instituto Valenciano de Investigaciones Económicas). Gasto sanitario público en España. Agosto de 2013. http://www.ivie.es/es/banco/gasto-sanitario-publico.php. Accessed 23 Dec 2016.
The stata commands run to estimate the models in Stata 14 are:
xtset panelvar timevar [, tsoptions] (to declare longitudinal nature of data).
melogit depvar fe_equation [|| re_equation] [|| re_equation ...] [, options] (to estimate logit model).
meologit depvar fe_equation [|| re_equation] [|| re_equation ...] [, options] (to estimate logit ordered model).


