Abstract
This Viewpoint is based on a recent panel featured at the 2017 Winter Conference on Brain Research in which the psychiatric comorbidities of HIV infection were discussed. Psychiatric comorbid conditions occur at high rates in HIV infected patients, complicating treatment and contributing to poor outcomes. A complex relationship between HIV infection and psychiatric comorbidity is an active area of investigation, but increased awareness of the impact of psychiatric complications of NeuroAIDS is needed in both the laboratory and the clinic to better understand and treat these interrelated conditions.
Keywords: Psychiatric comorbidity, HIV, NeuroAIDS
Over 30 years ago, soon after discovering that HIV was the likely cause of AIDS, reports emerged that the virus was present in the brains of AIDS patients. The link between HIV/AIDS and associated neurological complications was thus established, and the term NeuroAIDS ultimately came to be adopted. A spectrum of cognitive impairments, collectively referred to as HIV-associated neurocognitive disorders (HAND), is the defining feature of NeuroAIDS, but the field has to a certain extent failed to incorporate psychiatric comorbidities of HIV infection into its nosology.1 This has become increasingly important as a higher prevalence of substance abuse, depression, post-traumatic stress disorder (PTSD), sleep disturbance, and psychosis has been observed in this population (https://www.psychiatry.org/psychiatrists/practice/professional-interests/hiv-psychiatry/resources; Table 1).1,2 Despite elevated risk, clinicians often fail to adequately diagnose and treat comorbid psychiatric conditions in HIV-infected patients, creating an impediment to effective care.1–3 Not only do these conditions potentially contribute to cognitive impairments, but mounting evidence suggests that they constitute an independent and substantial health burden.
Table 1.
| psychiatric comorbidity | prevalence |
|---|---|
| substance use | 40–74% |
| depression | 22–50% |
| anxiety disorders | 2–40% |
| PTSD | ∼30% |
| sleep disturbance | 10–50% |
| severe mental illness/psychosis | 0.2–15% |
Mechanistic studies are unraveling a complex relationship between HIV infection, neuroinflammation, and psychiatric and neurological comorbidities that warrants greater scrutiny. For example, in some cases, mental illness may be the direct consequence of neuropathology associated with HIV infection, but in other cases mental illness is a risk factor for HIV exposure that goes on to complicate disease course and treatment after seroconversion. We recently held a panel at the 2017 Winter Conference on Brain Research (WCBR) entitled The Neuropsychiatric Impact of HIV in which some of the latest research into the link between HIV and psychiatric comorbidities was presented. Here we highlight some of the findings discussed by the panel with an eye toward emphasizing the role of the more common psychiatric and neurological conditions in NeuroAIDS.
The World Health Organization (WHO) estimates that 36.7 million people were infected with HIV worldwide in 2015, 2.1 million of which were newly infected that year (http://www.who.int/hiv/data/en). Epidemiologic studies examining subsets of HIV/AIDS patients indicate that the rates of psychiatric symptoms including substance abuse, depression, PTSD, sleep disturbance, and psychosis are between 1.5 and 8 times higher in the HIV-infected population compared with the general population or noninfected, demographically similar comparator groups.1–3 While a general consensus has been reached that psychiatric comorbidities are enriched in HIV-infected patients, prevalence estimates vary depending on subject/comparator demographics, screening criteria for comorbidities, sample size, geographic region, and the year in which the study was performed. Access to combined antiretroviral therapy (cART) is also a key variable. In 2015, about 46% of HIV-infected patients worldwide had access to cART, with global cART coverage increasing at a rate of 4–5% per year. Although cART suppresses viral replication and extends life, it has not been able to completely eliminate the symptoms of NeuroAIDS. By increasing life expectancy, widespread access to cART may actually elevate the lifetime prevalence of chronic mental illness, as has been the case with HAND. Despite diminished occurrence of severe HIV-dementia after the advent of cART, a concomitant increase in mild and moderate forms of HAND has translated to largely unchanged prevalence estimates.1 If risk for HIV-associated psychiatric symptoms follows a similar course, then any shift in diagnosis caused by the changing treatment landscape may be one of degree rather than number. In this shifting landscape, there is a significant need for cohort studies that will clearly identify the prevalence and severity of comorbid psychiatric disease in HIV-infected patients.
In addition to imposing an independent mental health burden, psychiatric conditions that are comorbid with HIV infection can worsen clinical outcomes for patients. A recent investigation into the causes of hospital admissions for adult patients4 showed that 9% of hospitalizations across five continents were attributable to psychiatric disorders. In Europe, the number was as high as 13%, with the only more frequent cause of hospitalization being AIDS-related infection. Even in HIV-infected patients that do not require hospitalization, psychiatric comorbid conditions can contribute to poor clinical outcomes and higher mortality rates that are due in part to reduced medication adherence.1 Indeed, several studies have found that treatment of mental health symptoms can improve cART adherence, highlighting the importance of considering psychiatric comorbidities within the diagnosis and treatment framework of NeuroAIDS.
A considerable amount of evidence has implicated a bidirectional relationship between HIV infection and certain mental illness in which neuroinflammatory and stress-related factors play a contributing role (Figure 1).1–3 Comorbid substance abuse exemplifies this relationship. It is well documented that substance abuse can increase the probability of HIV exposure and infection (i.e., via injection drug use or risky sexual behavior). Perhaps less obvious are recent findings that suggest HIV infection may itself promote drug-seeking behavior and increase the likelihood of relapse in patients undergoing treatment for substance abuse.5 These behavioral modifications in HIV-infected patients have been linked to increases in proinflammatory cytokines and alterations in neural reward circuitry that may be due to residual production of nonstructural viral proteins. For example, transgenic mice expressing Tat under a glial-acidic fibrillary acidic promoter exhibit greater sensitivity to methamphetamine reward and increased mesolimbic levels of serotonin and dopamine.5
Figure 1.
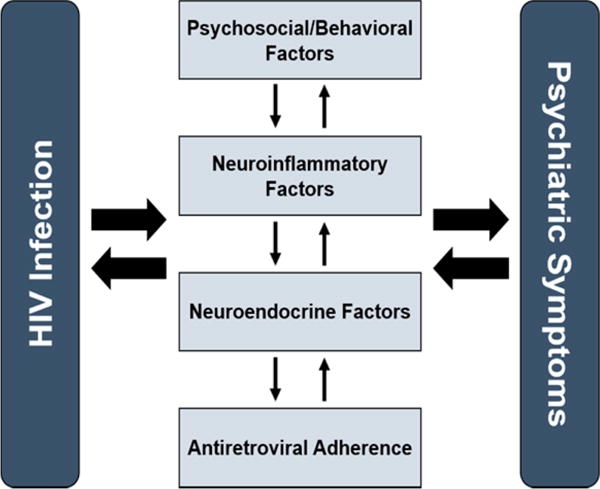
Complex causal relationship between HIV infection and psychiatric comorbidities with interdependent intermediary factors.
A similarly complex story emerges when considering the relationship between HIV and depression. Depression is one of the most common psychiatric comorbidities in HIV-infected patients.1,2 Numerous links have been identified between chronic neuroinflammation, stress-induced neuroendocrine changes, aberrant neurotransmitter signaling and depressed mood.2 In HIV-infected patients, clinical findings have shown a positive correlation between depression and systemic or cerebrospinal fluid (CSF) levels of inflammatory cytokines such as tumor necrosis factor alpha (TNFα), interleukin 1β (IL-1β), and IL-6.2 Preclinical models generally corroborate these findings, and have connected elevated levels of these cytokines to disturbances in glutamatergic and monoaminergic pathways in cortical and subcortical regions of the brain.2
Impairments in mood regulation associated with HIV extend to anxiety symptoms as evidenced by increased prevalence of anxious disorders including generalized anxiety disorder and PTSD.1,3 The neurobiology of PTSD includes alterations in the hypothalamic pituitary adrenal (HPA) axis and impaired cortical gating of amygdala reactivity. These alterations in neural circuitry are thought to underlie the persistence of intrusive fearful memories, hyperarousal, and nightmares. Although an abundance of data from preclinical model systems have shown prolonged increases of inflammatory cytokines and stress hormones induced by HIV infection, it has yet to be empirically determined whether these persistent physiologic changes modify PTSD progression or warrant a distinct treatment approach (i.e., balancing pharmacologic and psychotherapeutic approaches). For example, selective serotonin reuptake inhibitors (SSRIs), which are otherwise only partially effective in PTSD patients, also exhibit anti-inflammatory properties that may make these drugs particularly beneficial in an HIV-infected subgroup with comorbid PTSD.3
The above highlights some of the more common psychiatric conditions associated with HIV infection, and some discussed by the WCBR panel, but they are by no means an exhaustive list. Taken together, these psychiatric comorbidities represent a considerable health burden that merits heightened attention from both researchers and clinicians. Although it is clear that mental illness is both a risk factor and manifestation of HIV infection, many unanswered questions remain about the mechanistic connection between the two. Recognizing the importance of this relationship and addressing these questions through empirical study will be critical for improving the long-term managed care of HIV-infected patients, and to understand the interconnected pathobiology of HIV-infection and psychiatric disease.
Footnotes
ORCID
Barbara S. Slusher: 0000-0001-9814-4157
Notes
The authors declare no competing financial interest.
References
- 1.Owe-Larsson B, Sall L, Salamon E, Allgulander C. HIV infection and psychiatric illness. Afr J Psych. 2009;12:115–28. doi: 10.4314/ajpsy.v12i2.43729. [DOI] [PubMed] [Google Scholar]
- 2.Del Guerra FB, Fonseca JLI, Figueiredo VM, Ziff EB, Konkiewitz EC. Human immunodeficiency virus-associated depression: contributions of immuno-inflammatory, monoaminergic, neurodegenerative, and neurotrophic pathways. J Neuro-Virol. 2013;19:314–327. doi: 10.1007/s13365-013-0177-7. [DOI] [PubMed] [Google Scholar]
- 3.Neigh GN, Rhodes ST, Valdez A, Jovanovic T. PTSD co-morbid with HIV: Separate but equal, or two parts of a whole? Neurobiol Dis. 2016;92:116–23. doi: 10.1016/j.nbd.2015.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ford N, Shubber Z, Meintjes G, Grinsztejn B, Eholie S, Mills EJ, Davies MA, Vitoria M, Penazzato M, Nsanzimana S, Frigati L, O’Brien D, Ellman T, Ajose O, Calmy A, Doherty M. Causes of hospital admission among people living with HIV worldwide: a systematic review and meta-analysis. lancet HIV. 2015;2:e438–44. doi: 10.1016/S2352-3018(15)00137-X. [DOI] [PubMed] [Google Scholar]
- 5.Kesby JP, Markou A, Semenova S. The effects of HIV-1 regulatory TAT protein expression on brain reward function, response to psychostimulants and delay-dependent memory in mice. Neuropharmacology. 2016;109:205–15. doi: 10.1016/j.neuropharm.2016.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]


