Abstract
Background
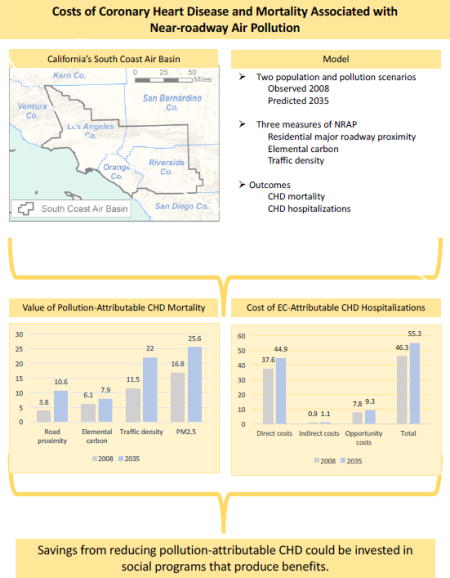
Emerging evidence indicates that the near-roadway air pollution (NRAP) mixture contributes to CHD, yet few studies have evaluated the associated costs.
Objective
We integrated an assessment of NRAP-attributable CHD in Southern California with new methods to value the associated mortality and hospitalizations.
Methods
Based on population-weighted residential exposure to NRAP (traffic density, proximity to a major roadway and elemental carbon), we estimated the inflation-adjusted value of NRAP-attributable mortality and costs of hospitalizations that occurred in 2008. We also estimated anticipated costs in 2035 based on projected changes in population and in NRAP exposure associated with California’s plans to reduce greenhouse gas emissions. For comparison, we estimated the value of CHD mortality attributable to PM less than 2.5 µm in diameter (PM2.5) in both 2008 and 2035.
Results
The value of CHD mortality attributable to NRAP in 2008 was between $3.8 and $11.5 billion, 23% (major roadway proximity) to 68% (traffic density) of the $16.8 billion attributable to regulated regional PM2.5. NRAP-attributable costs were projected to increase to $10.6 to $22 billion in 2035, depending on the NRAP metric. Cost of NRAP-attributable hospitalizations for CHD in 2008 was $48.6 million and was projected to increase to $51.4 million in 2035.
Conclusions
We developed an economic framework that can be used to estimate the benefits of regulations to improve air quality. CHD attributable to NRAP has a large economic impact that is expected to increase by 2035, largely due to an aging population. PM2.5 -attributable costs may underestimate total value of air pollution-attributable CHD.
Keywords: Vehicle emissions, cardiovascular disease, burden of disease, micro-costing analysis, and cost of illness
Graphical abstract
Introduction
Coronary heart disease (CHD) caused around one in six deaths in the United States in 2010.1 In the same year direct medical costs of CHD were $35.7 billion and are projected to almost triple, to $106.4 billion by 2030.2 Thus, policies that reduce the burden of CHD have potentially large economic benefits.
Globally, ambient particulate matter less than 2.5 µm in aerodynamic diameter (PM2.5) is the second leading environmental contribution to the global burden of disease, accounting for 3.1 million deaths in 2010.3 In 2012 there were an estimated 1.2 million deaths from coronary heart disease attributable to PM2.5.4 Emerging evidence indicates that the mixture of near roadway air pollution (NRAP) also causes CHD.5,6,7,8 However, there have been few studies examining the population burden and cost of NRAP.
We recently estimated the number of cases of NRAP- and PM2.5 -attributable CHD mortality and NRAP-attributable hospitalizations in California’s South Coast Air Basin for 2008 and the burden of CHD expected in 2035 in an aging population.9 The year 2035 was used to demonstrate the potential effects of the Southern California Regional Transportation Plan which is likely to increase the number of people living near busy roads. The transportation plan is in response to landmark Californian legislation (Senate Bill 375) to reduce greenhouse gas emissions in the state. Because a third of greenhouse gases are from cars and trucks, the plan aims to reduce vehicle miles traveled through compact urban development and high density housing along public transportation corridors.10 These corridors often have heavy vehicular traffic.10 We showed that the usual approach to estimating air pollution-attributable CHD burden of disease based on population exposure to PM2.5, which ignores the contribution of NRAP, may substantially underestimate the total burden of pollution-attributable CHD. Knowing the total costs of pollution-attributable CHD is essential to evaluating alternative strategies to reduce greenhouse gases.
The U.S. Environmental Protection Agency (EPA) developed an approach to valuing cardiovascular costs of PM2.5 in the U.S.11 Value of mortality was based on the value of a statistical life (VSL). The EPA used the cost-of-illness (COI) associated with a myocardial infarction to calculate costs from a CHD hospitalization. The EPA’s COI includes direct costs, primarily the cost of hospitalization, plus indirect costs, measured as lost earnings over a five-year period subsequent to the acute illness.
We expanded on the EPA’s approach by assigning costs to a more complete estimate of the CHD burden attributable to air pollution, one that includes the effects of both PM2.5 and NRAP. We estimated this burden for California’s South Coast Air Basin (SoCAB) in 2008 and 2035. We applied an improved framework for estimating the costs of hospitalization, which reflects recent advances in medical technology for non-fatal myocardial infarction that have increased the role of medical management and decreased use of expensive coronary artery bypass grafts. We defined the indirect cost to the individual as lost income above what is covered by short-term disability insurance. We accounted for recent reductions in the median duration of lost work after CHD hospitalization. Finally, we estimated opportunity costs associated with the value of time that could have been spent on activities if not for the CHD.
Methods
We used previous estimates of the number of CHD deaths and hospitalizations attributable to NRAP in the SoCAB,9 as described below and in the Online Supplement. SoCAB includes the densely populated southern part of Los Angeles County, western urbanized portions of Riverside and San Bernardino counties and all of Orange County. This region has heavy vehicular traffic corridors and has among the highest concentrations of PM2.5 in the U.S. We adjusted all cost estimates from primary and secondary sources to 2014 U.S. dollars using the consumer price index.12
Air pollution-attributable CHD burden
Detailed methods used to estimate the population-weighted exposure, the pollution-attributable fraction and number of CHD hospitalizations and deaths in 2008 have been described previously.9 Those estimates were projected for 2035 under a compact development scenario from the Southern California Regional Transportation Plan.9 In summary, mortality and hospitalizations attributable to NRAP in SoCAB were estimated for an at-risk population of 3.32 million individuals aged 45 years and older in 2008 (35% of the total population of 15.5 million in SoCAB in 2008), and for the projected 8.0 million individuals aged 45 and older (43% of the total population of 18.5 million) in 2035. In order to distinguish the effect of the aging population on the 2035 attributable estimate from the effect of air pollution, we also estimated the hypothetical attributable burden of CHD in a 2035 population with the same age structure as in 2008.
We chose concentration-response functions appropriate for the study population.9 (See Table S1 in Online Supplement). We estimated mortality attributable to NRAP and PM2.5 in each county in SoCAB and SoCAB overall in 2008 and 2035. We used three measures of NRAP: parcel proximity to a major roadway (a dichotomous indicator of whether the center of each residential plot is within 150 m of a freeway or expressway or within 50 m of a major arterial), elemental carbon (a continuous measure which is a marker in southern California for diesel exhaust particulate exposure),13 and traffic density within 300 m of each SoCAB parcel (a continuous measure defined as the distance-decayed annual average daily volume of traffic surrounding each plot). NRAP-attributable hospitalization concentration-response functions for CHD were available for elemental carbon (EC) only.
We used the population-weighted prevalence of near-roadway proximity and mean traffic density, and the mean EC and PM2.5 concentration exceeding background levels of 0.12 and 5.6 µg/m3, respectively. We estimated NRAP-related elemental carbon (EC) using a line source dispersion model and assigned a regional component of EC in a 4×4 km grid. Traffic density was adjusted downward in 2035 for anticipated reductions in fleet-average PM2.5 emissions. Annual average PM2.5 mass concentrations in each 4×4 km grid were assigned to all parcels in the grid in 2008 and in projected plots in 2035, accounting for anticipated changes in fleet emissions and vehicular mix.
CHD-mortality was based on ICD-10 codes I20-I25 and CHD-related hospitalizations were based on ICD-9 codes 410–414 and 429.2. These codes correspond to the concentration-response functions used to estimate the burden of disease (Table S1 in Online Supplement). The baseline hospital discharge rates were limited to non-fatal events. The CHD-specific mortality data included those hospitalizations that ended in death and CHD-specific mortality outside a hospitalization. We assumed that the known age-specific mortality and hospitalization rates in 2008 would be the same in 2035 (see Online Supplement).
Value of CHD mortality
We estimated the total value of mortality by multiplying the number of deaths by the value of a statistical life (VSL), $8.8 million in 2014 dollars.11,14 The largest source of uncertainty in the valuation of mortality is the VSL. Thus we calculated confidence intervals treating VSL as a random variable and the number of deaths as a constant (Table 1).
Table 1.
Value and Costs of CHD Outcomes Per Pollution-attributable Case
| Outcome | Value in Thousands of 2014 USD (95% CI) |
|
|---|---|---|
|
| ||
| Age 45–64 | Age 65+ | |
| Fatal case of CHD | ||
| Value of a statistical lifea | 8,800,000 (900,000, 23,200,000) | 8,800,000 (900,000, 23,200,000) |
| Hospitalization for nonfatal case of CHD | ||
| Direct costs | ||
| Inpatient hospitalizationb,* | 23,881 | 25,348 |
| Medical care in year following dischargec,* | 16,084 | 16,084 |
| Indirect costs | ||
| Lost income, age 45–64d | 2,392 (2,391, 2,393) | NA |
| Opportunity costse,* | ||
| Complete activity restricted | 3971 | 7687 |
| Minor restricted activity | 2287 | 2287 |
| Total cost of hospitalizationf,* | 48,615 | 51,406 |
Value of a statistical life is from the US EPA.11
Age-specific estimates are from the Healthcare Cost and Utilization Project database.15
These are the weighted average of one-year cost estimates.16
Lost income is the difference between what would have been earned in the absence of hospitalization and the total payments received from short term disability insurance.17
For cases 65+, there are 16.55 hours/day of leisure time lost during complete activity restriction. For cases 45–64, there are 8.55 hours/day of leisure time lost because 8 hours/day are accounted for in lost wages.
Sum of the direct, indirect and opportunity costs.
Standard errors not available.
Direct cost of CHD hospitalizations
We defined the direct medical costs of hospitalization for CHD as the cost of the hospitalization and the cost of CHD-related medical care during the year following discharge for CHD. We estimated the mean cost of a hospitalization for CHD to be $23,881 for those aged 45–64 and $25,348 for those aged 65 and over using the Healthcare Cost and Utilization Project California database15 and the ICD codes used in Ghosh, et al..9 We estimated the average direct medical costs incurred during the year following discharge to be $16,084 using a study of selected CHD diagnoses.16 Follow-up costs included outpatient treatment, medical office visits and pharmaceutical treatment.
Direct cost of hospitalization and subsequent care summed to $39,965/attributable case aged 45–64 and $41,432/attributable case aged 65 and over (Table 1).
Indirect cost of CHD hospitalizations
A common measure of indirect cost of morbidity is the associated lost income.11,14 For the population aged 45–64, we estimated lost income over the 6 months following hospitalization as the difference between what would have been earned in the absence of hospitalization and the total payments received from short term disability insurance, which was $2,392/case.17 (See Table 1).
Opportunity cost of CHD hospitalizations
We assumed that individuals experience 19 days (5 days in hospital and 2 weeks after discharge) with complete activity restriction (Online Supplement). We estimated this opportunity cost for the working aged population as 19 days × 8.55 hours/day (mean number of hours spent in leisure and household activities)18 × $24.45/hour (the median wage rate in the population under 65 years). In the working age population, lost wages were included as part of the indirect cost of hospitalization described above. For the population age 65+ the opportunity cost was calculated based on 16.55 hours18 that otherwise would be spent on leisure and household activities (8.55 hours plus 8 hours that the younger population lost in wages).
Following complete activity restriction individuals have 28 days of minor restricted activity,11,19 which costs $81.65/day.11,20
The total opportunity cost was $6,258 per case age 45–64 and $9,974 per case age 65+ (Table 1).
Total costs of hospitalization
The direct costs, indirect costs and opportunity costs of nonfatal CHD hospitalization summed to $48,615 for each case aged 45–64 and $51,406 for each case 65+ (Table 1). To get the total costs of hospitalization we multiplied the count of hospitalizations in each age group (ages 45–64 and 65+) by the sum of the direct costs, indirect costs and opportunity costs of those hospitalizations. We included the standard errors for each estimated cost when it was available from the source data (Table 1). Because the standard errors were not available for most cost components, the joint distribution of the total cost per hospitalization was analytically intractable. We therefore calculated confidence intervals treating the count of hospitalizations as a random variable and the estimated total cost per hospitalization as a constant.
The value of CHD mortality uses a societal approach.11,14 The value of a statistical life is based on very small risks of death and represents what society would be willing to pay to avoid one expected death on average.11 The cost of hospitalization uses an individual approach which is based on costs incurred by each person. The societal approach and individual approach are conceptually very different; therefore, we did not aggregate the value of mortality and costs of hospitalization.
Results
Estimates of the value to society of NRAP-attributable CHD deaths in 2008 varied from $3.8 billion for the 430 deaths attributable to major roadway proximity to $11.5 billion for the 1,300 deaths attributable to traffic density (Table 2). The estimated value of mortality using elemental carbon was $6.1 billion. The value of mortality attributable to PM2.5 was $16.8 billion (1,900 deaths). The NRAP-related value of mortality was 23%, 36% and 68% the value of mortality attributable to regulated regional PM2.5, depending on whether NRAP was measured as roadway proximity, elemental carbon or traffic density, respectively. For 2035 the value of CHD mortality attributable to NRAP ranged from $7.9 billion for the 900 deaths attributable to major roadway proximity to $22.0 billion for the 2,500 deaths attributable to traffic density, only modestly less than the $25.6 billion value of 2,900 deaths attributable to PM2.5. The value of mortality relative to PM2.5 increased in 2035 for roadway proximity and traffic density. However, much of the increased attributable mortality resulted from the change in population age. Were the age distribution to remain the same as in 2008, the value of mortality in 2035 would range from $5.6 billion for the 630 deaths attributable to elemental carbon to $15 billion for the 1,700 deaths attributable to traffic density (Table S2 in Online Supplement). These values are almost as large as the $17.6 billion value of the 2,000 deaths attributable to PM2.5 if the 2008 age distribution were applied to the 2035 population.
Table 2.
Current and Projected Value of Mortality from CHD by Near-roadway Air Pollution Metric and PM2.5
| 2008 | 2035 | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Number of Deaths (95% CI)a |
Cost in Millions of 2014 USD (95% CI)b |
Proportion of cost of burden relative to PM2.5 c |
Number of Deaths (95% CI)a |
Cost in Millions of 2014 USD (95% CI) |
Proportion of cost of burden relative to PM2.5 c |
|
| NRAP Measures | ||||||
| Road Proximity | 430 (270, 600) | 3,791 (368, 9,973) | 23% | 1,200 (820, 1,600) | 10,579 (1,028, 27,833) | 41% |
| Elemental Carbon | 690 (360, 1,000) | 6,083 (591, 16,004) | 36% | 900 (470, 1,300) | 7,935 (771, 20,875) | 31% |
| Traffic Density | 1,300 (440, 2,000) | 11,461 (1,113, 30,152) | 68% | 2,500 (860, 4,000) | 22,040 (2,141, 57,985) | 86% |
|
| ||||||
| PM2.5 | 1,900 (1,400, 2,400) | 16,751 (1,627, 44,069) | - | 2,900 (2,200, 3,600) | 25,567 (2,483, 67,263) | - |
In 2008 there were approximately 920 CHD hospitalizations attributable to elemental carbon. The aggregate cost of these hospitalizations was $22.8 million, and the aggregate cost of care in the year following the hospitalization was $14.8 million (Table 3), totaling $37 million in direct costs. The indirect cost of lost earnings due to CHD was $0.9 million. The opportunity cost --- the value of lost time for non-wage earning activities --- was $2.3 million for those aged 45–64 and $5.5 million for those 65 years of age and older. By 2035, CHD hospitalizations attributable to elemental carbon were projected to increase to 1,100/year, generating $27.2 million in costs of initial hospitalization and an additional $17.7 million in one-year follow-up costs. Lost income following a CHD-hospitalization was projected to increase to $1.1 million. The opportunity cost following a hospitalization was estimated to be $2.8 million for those aged 45–65 years and $6.5 million for those 65 years and older. In total, we estimated the cost of CHD hospitalizations attributable to the elemental carbon measure of NRAP to be $46.3 million in 2008. This cost was projected to increase to $55.3 million per year by 2035. That value would be $42.2 million in 2035 if the age distribution were to remain the same as in 2008 (Table S2 in Online Supplement).
Table 3.
Current and Projected Costs of Hospitalization for CHD Attributable to Elemental Carbon
| 2008 | 2035 | |||
|---|---|---|---|---|
|
|
|
|||
| Number of Cases (95% CI)1 |
Aggregate Cost2 in Millions of 2014 Dollars (95% CI)3 |
Number of Cases (95% CI)a |
Aggregate Cost2 in Millions of 2014 Dollars (95% CI)3 |
|
|
| ||||
| Direct Costs | ||||
| Inpatient | ||||
| Hospitalizationa | ||||
| 45–64 | 372 (129, 606) | 8.9 (3.1, 14.5) | 444 (154, 687) | 10.6 (3.7, 16.4) |
| 65+ | 548 (191, 894) | 13.9 (4.8, 22.7) | 656 (226, 1,013) | 16.6 (5.7, 25.7) |
| All ages | 920 (320, 1,500) | 22.8 (7.9, 37.1) | 1,100 (380, 1,700) | 27.2 (9.4, 42.0) |
| Medical care in year following dischargeb | 920 (320, 1,500) | 14.8 (5.1, 24.1) | 1,100 (380, 1,700) | 17.7 (6.1, 27.3) |
|
| ||||
| Indirect Costs | ||||
| Lost income, age 45–64c | 372 (129, 606) | 0.9 (0.3, 1.4) | 444 (154, 687) | 1.1 (0.4, 1.6) |
|
| ||||
| Opportunity Costs | ||||
| Age 45–64 | 372 (129, 606) | 2.3 (0.8, 3.8) | 444 (154, 687) | 2.8 (1., 4.3) |
| Age 65+ | 548 (191, 894) | 5.5 (1.9, 8.9) | 656 (226, 1,013) | 6.5 (2.3, 10.1) |
|
| ||||
| Total Cost | 46.3 (16.1, 75.4) | 55.3 (19.1, 85.5) | ||
Number of cases and 95% confidence interval (CI) are from Ghosh, et al.9
These estimates are the number of cases multiplied by cost (from Table 1) of each outcome (95% confidence intervals [CI]).
The uncertainty interval for the aggregate cost treats cost as a constant and the count estimate as a random variable
Discussion
This is one of the first studies to estimate the cost of NRAP-associated CHD and the first, to our knowledge, to project future costs in an aging population. We estimated the costs of PM2.5 and of NRAP separately, because regional PM2.5 is unlikely to characterize the sharp gradient in effects of the near-roadway pollutant mixture. Limited research suggests that the effects are independent,25 and the possibility of synergistic effects of PM2.5 and NRAP has not been evaluated. Of the three NRAP proxy exposures, elemental carbon is likely to have the greatest overlap with the effects of PM2.5.9 However, to the extent that the effects are independent, CHD risk assessment and economic studies, which typically have estimated only PM2.5 population-attributable effects,11 have substantially underestimated the economic impact. The NRAP-related value of mortality in 2008 ranged from approximately $3.8 billion to $11.5 billion, 23% (roadway proximity) to 68% (traffic density) of the $16.8 billion attributable to regulated regional PM2.5. Under a future scenario mandated by California’s landmark legislation to reduce greenhouse gas emissions, the anticipated value of mortality due to air pollution in 2035 was estimated to increase, largely due to the increase in a susceptible, aging population. The projected underestimate in attributable value of mortality due to NRAP relative to PM2.5 increased in 2035 for both major road residential proximity and traffic density, because the compact urban development strategy to reduce greenhouse gas emissions is expected to increase the proportion of people in SoCAB living in close proximity to roadways with heavy vehicular traffic.9
The value to society of NRAP-attributable CHD mortality was much larger than the costs of non-fatal hospitalizations. In 2008, for example, elemental carbon accounted for $6.1 billion in preventable mortality, more than 100 times the $46 million cost attributable to non-fatal hospitalizations. When comparing these numbers, it is important to note that they measure different concepts. The value assigned to preventable death reflects societal willingness to pay to reduce the risk of one death on average. It is relevant for development of policy, but it is not an economic cost paid by an individual. In contrast, many of the air pollution-attributable non-fatal costs are borne directly by the individual and their insurers. These costs are approximately $50,000 in the year following hospitalization (Table 1) and the proportion of these costs paid directly by the individual are likely to cause hardship -- the median household income in Los Angeles County during 2009–2013 was slightly over $56,000.21 These costs are also currently likely to be borne disproportionately by racial and ethnic communities that are more likely than other populations to live within 150 m of a major highway.22,23
There has been only limited previous study of the economic burden of CHD attributable to NRAP. A study of the population aged 65 years and older in 10 European cities found that not including the long-term effects of NRAP on the development of CHD led to an underestimate in the subsequent acute effects (hospitalizations) due to NO2 by 97% and of corresponding costs by 95%.24 These results cannot be compared to ours as we did not account for the long-term effect of NRAP on the development of CHD in the estimated attributable number of cases of hospitalization or mortality. We may have underestimated the NRAP-attributable burden and cost of disease by not doing so.
Uncertainty in estimates of effects of NRAP-attributable mortality are reflected in the almost three-fold differences between the three markers of exposure (Table 2). The confidence intervals derived from our previous estimates of the air pollution-attributable CHD characterize a set of uncertainties. The valuation of mortality also has substantial uncertainty. We used the VSL which was derived by the US EPA as the mean of a distribution fitted to 26 published VSL estimates with confidence intervals ranging from slightly less than $1 million to over $23 million.11 We used the EPA’s VSL in order for our results to be comparable to other studies of the cost of mortality in the US.
We made conservative assumptions in estimating the cost of hospitalization. We used the minimum expected time of complete and minor activity restriction. We did not include costs associated with effects after one year:26 persistent fatigue,27 depression,28 not returning to work,29 or complications from inpatient care. The estimate of lost wages per person is likely to be low, because the data used for this estimate include individuals who were not hospitalized for CHD.17 California has mandated short-term disability coverage, but some portion of independent contractors and self-employed likely do not have such coverage.
Uncertainty is associated with projecting the disease burden to 2035, including predicting population growth and changes in the age distribution.9,10,30,31 Treatment for CHD has evolved rapidly even over the last decade,16 but the effects of new treatments and of changing risk factors such as obesity are difficult to predict. By assuming that direct cost of a hospitalization will not change, our estimates reflect the change in total costs attributable to changes in the burden of air pollution.
The methods for estimating cost of non-fatal CHD refined and expanded on the existing approach used by EPA.11 We included the effects of NRAP, incorporated direct costs of hospitalizations that reflect current medical technologies, utilized more accurate estimates of lost income, and added the opportunity cost of time lost to illness. Accounting for the opportunity cost increased the per-illness cost by up to 15% for those aged 45–64 years and 24% for those 65 years and older in 2008 (Table 1). The increase in the aggregate cost across SoCAB was $7.8 million, or 16.8% of total costs of hospitalizations (Table 3).
Healthcare related to NRAP-attributable CHD lead to large public expenditures with substantial opportunity costs to the public. In 2008, 61% of all hospitalizations for heart attacks were covered by Medicare and 9% were covered by Medi-Cal.32 Therefore, based on costs in Table 3, we estimate that $25 million in Medicare and Medi-Cal expenditures could have been avoided if NRAP exposure were reduced to background levels in SoCAB. If that $25 million had instead been invested in evidence-based smoking cessation programs, it would have yielded a benefit of $24.7 to $36.9 billion based on the expected return on investments for these programs.33
Levels of PM2.5 have declined markedly over the last several decades, and vehicle emissions control programs have reduced many components of the NRAP mixture. National standards such as Tier-2 and Tier-3 vehicle standards34 are expected to further reduce EC exposure. However, our analysis suggests that policies to reduce greenhouse gas emissions from vehicles that relied more heavily on zero- or close-to-zero emission vehicles and protective urban designs would maximize the health co-benefits of these policies. Examples of protective design include distance buffers and physical barriers between traffic corridors and residences. Buffers of even 150m and barriers can substantially reduce peak exposures to NRAP and should be designed to encourage walking and use of public transportation.35,36
Our approach could be used to refine estimates of the health co-benefits of strategies for reducing greenhouse gas emissions and benefits of air pollution regulations more generally.37 For example, in cost-benefit analyses of proposed regulation, the EPA includes the lost wages of those in the working-aged population, but does not include the value of time for those over 65 years who have a nonfatal heart attack.11 We estimated this to be $9,900 for each person aged 65 years or older who experienced a hospitalization for CHD. The value of time for those aged 45–64 years that is not included in current current EPA estimates is $6,200 per person.
We conclude that the value of mortality from CHD attributable to NRAP in Southern California in 2008 was a substantial proportion of the estimated $16.8 billion value of PM2.5 - attributable CHD mortality. Thus, the typically estimated PM2.5 -attributable costs may underestimate the true cost of air pollution. Although the value of mortality was substantially larger than of hospitalization, individuals hospitalized for CHD due to NRAP incurred costs of about $46 million in 2008. The opportunity costs of lost time due to illness contributed substantially to the large impact borne by victims of non-fatal CHD and their families. These costs are projected to rise substantially in spite of reductions in greenhouse gas emissions projected by the year 2035, due largely to population growth and aging. However, there remain unexploited opportunities to optimize health co-benefits of greenhouse gas reduction by reducing population exposure to NRAP.
Supplementary Material
HIGHLIGHTS.
In Southern California, mortality from coronary heart disease attributable to near-roadway air pollution exposure accounts for yearly economic costs of $3.8 – $11.5 billion.
Near-roadway-attributable hospitalization for heart disease accounts for costs estimated to be $48.6 million.
The burden and cost of near-roadway air pollution-attributable heart disease are projected by 2035 to increase markedly under current transportation plans, due largely to an aging population.
Acknowledgments
Meredith Millet, California Department of Public Health, provided data that we used to estimate the rates of mortality and hospitalization for the SoCAB. Support was provided by funds from an air quality violations settlement agreement between the South Coast AQMD, a California state regulatory agency, and BP. Other funding support included NIH grants P01ES022845, P01ES009581, R01ES016535, R01ES014447, R01ES014708, and P30ES007048; U.S. EPA grants RD83544101, RD831861 and R826708-01; and the Hastings Foundation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ, et al. Heart disease and stroke statistics-2014 update: a report from the American Heart Association. Circulation. 2014;129:e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heidenreich PA, Trogdon JG, Khavjou OA, Butler J, Dracup K, Ezekowitz MD, et al. Forecasting the future of cardiovascular disease in the United States. Circulation. 2011;123:933–44. doi: 10.1161/CIR.0b013e31820a55f5. [DOI] [PubMed] [Google Scholar]
- 3.Lim S. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–2260. doi: 10.1016/S0140-6736(12)61766-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Global Health Observatory Data. [Retreived April 15, 2016]; from http://www.who.int/gho/phe/outdoor_air_pollution/burden/en/
- 5.Brook RD, Rajagopalan S, Pope CA, Brook JR, Bhatnagar A, Diez-Roux AV. Particulate matter air pollution and cardiovascular disease: An update to the scientific statement from the American Heart Association. Circulation. 2010;121:2331–2378. doi: 10.1161/CIR.0b013e3181dbece1. [DOI] [PubMed] [Google Scholar]
- 6.Gan WQ, Koehoornd M, Davies HW, Demers PA, Tamburic L, Brauer M. Long-term exposure to traffic-related air pollution and the risk of coronary heart disease hospitalization and mortality. Environmental Health Perspectives. 2011;119:501–7. doi: 10.1289/ehp.1002511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gan WQ, Tamburic L, Davies HW, Demers PA, Koehoorn M, Brauer M. Changes in residential proximity to road traffic and the risk of death from coronary heart disease. Epidemiology. 2010;21:642–9. doi: 10.1097/EDE.0b013e3181e89f19. [DOI] [PubMed] [Google Scholar]
- 8.Kan H, Heiss G, Rose KM, Whitsel EA, Lurmann F, London SJ. Prospective analysis of traffic exposure as a risk factor for incident coronary heart disease: the atherosclerosis risk in communities (aric) study. Environmental Health Perspectives. 2008;116:1463-. doi: 10.1289/ehp.11290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ghosh R, Lurmann F, Perez L, Penfold B, Brandt S, Wilson J, et al. Near-roadway air pollution and coronary heart disease: burden of disease and potential impact of a greenhouse gas reduction strategy in southern California. Environmental Health Perspectives. 2015:1–31. doi: 10.1289/ehp.1408865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.SCAG. Regional transportation plan 2012 – 2035. Sustainable communities strategy. Towards a sustainable future. Los Angeles, CA: Southern California Association of Governments; 2012. [Retrieved February 5, 2013]. from http://rtpscs.scag.ca.gov/documents/2012/final/f2012RTPSCS. [Google Scholar]
- 11.US EPA. Health and welfare benefits analyses to support the second section 812 benefit-cost analysis of the clean air act: final report. Washington, D.C.: U.S. Environmental Protection Agency; 2011. [Google Scholar]
- 12.Bureau of Labor Statistics, U. D. CPI Databases. [Retrieved March 18, 2016];2015 from http://www.bls.gov/cpi/data.htm.
- 13.Geller MD, Sardar SB, Phuleria H, Fine PM, Sioutas C. Measurements of particle number and mass concentrations and size distributions in a tunnel environment. Environmental Science and Technology. 2005;39:8653–8663. doi: 10.1021/es050360s. [DOI] [PubMed] [Google Scholar]
- 14.US EPA. Guidelines for preparing economic analyses. Washington, D.C.: U.S. Environmental Agency; 2010. [Google Scholar]
- 15.HCUP State Inpatient Databases (SID) Healthcare Cost and Utilization Project (HCUP) Rockville, MD: Agency for Healthcare Research and Quality; 2011. [PubMed] [Google Scholar]
- 16.Zhao Z, Winget M. Economic burden of illness of acute coronary syndromes: medical and productivity costs. BMC Health Services Research. 2011;11(35) doi: 10.1186/1472-6963-11-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Page RL, Ghushchyan V, Gifford B, Read RA, Raut M, Crivera C, et al. The economic burden of acute coronary syndromes for employees and their dependents. Journal of Occupational and Environmental Medicine. 2013;55:761–7. doi: 10.1097/JOM.0b013e318297323a. [DOI] [PubMed] [Google Scholar]
- 18.Bureau of Labor Statistics, U. D. American Time Use Survey. [Retrieved March 18, 2016];2015 from http://www.bls.gov/tus/
- 19.Ho PM, Eng MH, Rumsfeld JS, Spertus JA, Peterson PN, Jones PG, et al. The influence of age on health status outcomes after acute myocardial infarction. American Heart Journal. 2008;155:855–61. doi: 10.1016/j.ahj.2007.11.032. [DOI] [PubMed] [Google Scholar]
- 20.Ostro BD, Tran H, Levy JI. The health benefits of reduced tropospheric ozone in California. Journal of Air & Waste Management Association. 2006;56:1007–1021. doi: 10.1080/10473289.2006.10464511. [DOI] [PubMed] [Google Scholar]
- 21.U.S. Census Bureau. State & County QuickFacts: Los Angeles County, California. [Retrieved March 18, 2016];2015 from http://quickfacts.census.gov/qfd/states/06/06037.html.
- 22.Boehmer TK, Foster SL, Henry JR, Woghiren-Akinnifesi EL, Yip FY. Residential proximity to major highways — United States, 2010. Centers for Disease Control and Prevention, Morbidity and Mortality Weekly Report. 2013;62(03):46–50. [PubMed] [Google Scholar]
- 23.Chart-asa C, Gibson JM. Health impact assessment of traffic-related air pollution at the urban project scale: influence of variability and uncertainty. Science of the Total Environment. 2015;506–507:409–421. doi: 10.1016/j.scitotenv.2014.11.020. [DOI] [PubMed] [Google Scholar]
- 24.Chanel O, Perez L, Künzli N, Medina S, Aphekom group The hidden economic burden of air pollution-related morbidity: evidence from the Aphekom project. European Journal of Health Economics. 2015 doi: 10.1007/s10198-015-0748-z. [DOI] [PubMed] [Google Scholar]
- 25.Hoffman B, Moebus S, Stang A, Beck EM, Dragano N, Mohlenkamp S. Residence close to high traffic and prevalence of coronary heart disease. European Heart Journal. 2006;27:2696–2702. doi: 10.1093/eurheartj/ehl278. [DOI] [PubMed] [Google Scholar]
- 26.Dodson JA, Arnold SV, Reid KJ, Gill TM. Physical function and independence one year following myocardial infarction: observations from the TRIUMPH registry. American Heart Journal. 2012;163(5):790–79. doi: 10.1016/j.ahj.2012.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fedriksson-Larsson U, Alsen P, Brink E. I've lost the person I used to be - Experiences of the consequences of fatigue following myocardial infarction. International Journal of Qualitative Studies on Health Well-being. 2013;8:20836–20845. doi: 10.3402/qhw.v8i0.20836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shapiro P. Management of depression after myocardial infarction. Current Cardiology Reports. 2015;17:634–642. doi: 10.1007/s11886-015-0634-4. [DOI] [PubMed] [Google Scholar]
- 29.Worcester MU, Elliott PC, Turner A, Pereira JJ, Murphy BM, Le Grande MR, et al. Resumption of work after acute coronary syndrome or coronary artery bypass graft surgery. Heart, Lung and Circulation. 2014;23:444–453. doi: 10.1016/j.hlc.2013.10.093. [DOI] [PubMed] [Google Scholar]
- 30.California Department of Finance. Report P-2: State and County Population Projections – Race/Ethnicity and 5-Year Age Groups, 2010–2060 (by Year) [accessed 10 September 2013];2013 Available: http://www.dof.ca.gov/research/demographic/reports/projections/P-2/
- 31.SCAQMD. Final 2012 air quality management plan. Diamond Bar, CA: South Coast Air Quality Management District; 2013. [Retrieved February 5, 2013]. from http://www.aqmd.gov/docs/default-source/clean-air-plans/air-quality-management-plans/2012-air-quality-management-plan/final-2012-aqmp-(february-2013)/main-document-final-2012.pdf. [Google Scholar]
- 32.OSHPD. OSHPD health facts: Trends in cardiac care in California, 1988 to 2008. Part II. trends in heart attack hospitalizations. Sacramento, CA: Office of Statewide Health Planning and Development; 2011. [Google Scholar]
- 33.Fellows J, Rehm R, Hornbrook M, Hollis J, Haswell TC, Dickerson J, et al. Making the business case for smoking cessation and ROI calculator. Center for Health Research; 2004. [Google Scholar]
- 34.US EPA. EPA sets tier 3 motor vehicle emission and fuel standards. Washington, D.C.: U.S. Environmental Agency; 2014. [Google Scholar]
- 35.Zhu Y, Hinds WC, Kim S, Shen S, Sioutas C. Study of ultrafine particles near a major highway with heavy-duty diesel traffic. Atmospheric Environment. 2002;36:4323–4335. [Google Scholar]
- 36.Hagler GS, Lin MY, Khlystov A, Baldauf RW, Isakov Z, Faircloth J, Jackson LE. Field investigations of roadside vegetative and structural barrier impact on near-road ultrafine particle concentrations under a variety of wind conditions. Science of the Total Environment. 2012;419:7–15. doi: 10.1016/j.scitotenv.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 37.Revesz R, Livermore M. Retaking Rationality. How Cost-Benefit Analysis Can Better Protect the Environment and Our Health. New York, NY: Oxford University Press; 2008. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


