ABSTRACT
Studies of innate glial cell responses for progressive human immunodeficiency virus type one (HIV-1) infection are limited by a dearth of human disease-relevant small-animal models. To overcome this obstacle, newborn NOD/SCID/IL2Rγc−/− (NSG) mice were reconstituted with a humanized brain and immune system. NSG animals of both sexes were transplanted with human neuroglial progenitor cells (NPCs) and hematopoietic stem cells. Intraventricular injection of NPCs symmetrically repopulated the mouse brain parenchyma with human astrocytes and oligodendrocytes. Human glia were in periventricular areas, white matter tracts, the olfactory bulb and the brain stem. HIV-1 infection led to meningeal and perivascular human leukocyte infiltration into the brain. Species-specific viral-neuroimmune interactions were identified by deep RNA sequencing. In the corpus callosum and hippocampus of infected animals, overlapping human-specific transcriptional alterations for interferon type 1 and 2 signaling pathways (STAT1, STAT2, IRF9, ISG15, IFI6) and a range of host antiviral responses (MX1, OAS1, RSAD2, BST2, SAMHD1) were observed. Glial cytoskeleton reorganization, oligodendrocyte differentiation and myelin ensheathment (MBP, MOBP, PLP1, MAG, ZNF488) were downregulated. The data sets were confirmed by real-time PCR. These viral defense-signaling patterns paralleled neuroimmune communication networks seen in HIV-1-infected human brains. In this manner, this new mouse model of neuroAIDS can facilitate diagnostic, therapeutic and viral eradication strategies for an infected nervous system.
KEY WORDS: Humanized mice, Hematopoietic stem progenitor cells, Neuronal progenitors, Astrocytes, HIV-1
Summary: In mice with a humanized brain and immune system, systemic infection led to human-specific transcriptional induction of glial interferon antiviral innate immune pathways and alteration of neuronal progenitor differentiation and myelination.
INTRODUCTION
Despite uncovering many pathophysiological mechanisms that underlie human immunodeficiency virus (HIV)-associated neurocognitive disorders, deficits in neuroimmune communications remain incompletely understood (Gelman et al., 2012; Saylor et al., 2016). As the virus is species specific, co-morbid disease conditions that lead to impaired immune, glial and neural cell function cannot be studied in a small animal. Transgenic mice containing the whole viral genome or individually expressed proteins, and animals injected with viral proteins or human infected cells in brain tissue mirror only specific disease components (Gorantla et al., 2012). Lentiviral infections of nonhuman primates, cats and ungulates can mirror select aspects of HIV nervous system disease (Narayan and Clements, 1989), but not all neurovirologic processes (Jaeger and Nath, 2012). Such limitations are also seen in mice possessing a sustainable human immune system. Although humanized animals are susceptible to HIV infection and support persistent viral replication, the resultant structural and functional changes that occur in the brain are limited (Boska et al., 2014; Dash et al., 2011; Gorantla et al., 2010). The absence of human glial cells and differences in viral responses in the setting of divergent patterns of murine and human brains limit mechanistic studies (Oberheim et al., 2009).
The missing link in realizing a rodent model of HIV-1 human brain disease rests in the availability of human glia (astrocytes and oligodendrocytes). Glia are the most abundant cell type in the human central nervous system, and play pivotal roles in brain homeostasis and metabolism. While astrocytes, not oligodendrocytes, show limited susceptibility to HIV infection (Chauhan, 2015; Farina et al., 2007; Pfefferkorn et al., 2016; Russell et al., 2017), in disease, communication between both cell types and infected mononuclear phagocytes (monocyte macrophages and microglia) herald changes in the evolution of the brain's pro-inflammatory microenvironment (Bednar et al., 2015). The restriction to viral infection reflects absent receptors for viral entry (Schweighardt and Atwood, 2001) and coordination with less studied intracellular innate immunity protective pathways.
Further complicating glial responses during progressive viral infection are the interactions between lymphocytes and monocytes that traffic into the nervous system during viral infection (Dou et al., 2006; Epstein and Gendelman, 1993; González-Scarano and Martín-García, 2005; Gorantla et al., 2010). Thus, a disease model that accurately replicates nervous system viral infection must contain both human immune and glial cell elements (Gorantla et al., 2012). This can be achieved by reconstitution of the mouse brain with human neural progenitor cells (NPCs). Transplantable NPCs readily produce neuronal and glial lineage cells in the rodent brain (Nunes et al., 2003; Uchida et al., 2000). The mice contain human hematopoietic stem progenitor cells (HSPCs) readily generating lymphocyte and monocyte macrophages susceptible to HIV-1 infection. Human glial cells evolve from intraventricular NPC transplantation at birth (Han et al., 2013; Windrem et al., 2014).
In the current study, dual blood and brain humanized mice, when infected with a macrophage-tropic C-C motif chemokine receptor 5 HIV-1ADA, were examined for resultant effects on glial homeostasis. Transcriptional evaluations of two brain regions, the hippocampus (Hip) and corpus callosum (CC), demonstrated glial disease footprints for affecting antiviral human-specific immune responses. The importance of this model is underscored by specific glial transcriptional signatures that closely mirror human disease (Gelman et al., 2012; Sanfilippo et al., 2017; Sanna et al., 2017).
RESULTS
Human NPC engraftment
Mice were reconstituted with human immunocytes and glial cells. Newborn irradiated NSG mice were transplanted intraventricularly with human NPCs and intrahepatically with cluster of differentiation 34 (CD34)+ HSPCs from the same donor. NPCs were isolated from fetal human brains to generate neurospheres, from which a single cell suspension was prepared and transplanted at 105 cells/mouse (experiments 1 and 2, n=19) or 0.5×105 (experiments 3 and 4, n=26). The fate and distribution of human NPCs in mouse brain were then evaluated at 6 months of age. To analyze human glial cell distribution, paraffin-embedded and formalin-fixed tissue was sectioned along the sagittal plane from midline to the anatomical end of the CC [∼2.5 mm, according to the adult mouse brain atlas (Paxinos and Franklin, 2001) from left and right hemispheres. In two experiments (n=19), these glial cells were found in equal measure across both hemispheres on sagittal sections with distributions in the periventricular area (PV), CC, ventral striatum (STRv), cerebral cortex, midbrain (MB), cerebellum (CB) and Hip areas. Human cells were present in the olfactory bulb, lateral olphactory tract, anterior commissure, caudoputamen, MB, pons and medulla (Fig. 1B,C,D, Table 1; Fig. S1). A large proportion of the human cells in mouse brains were glial fibrillary acidic protein (GFAP)+, with typical astrocyte morphology based on size and process. To distinguish these human and mouse astrocytes, staining with nonspecies-specific (rb Dako/Z0034) and human-specific (ms STEM123) GFAP antibodies was performed. Human astrocytes commonly replaced their murine counterparts with nearly 70-80% occupancy in the PV and CC (Fig. 1B, indicated by asterisks). There was limited occupancy of human astrocytes in the frontal cortex (FC) and CB in 1/3 of the analyzed mice (Fig. 1E). Surprisingly, nearly 40% of human nuclei protein (hN, MAB4383)-positive cells in the CC and 20-30% of hN-positive cells in the Hip and STR were positive for OLIG2 (rb 1538-Olig2), an oligodendrocyte/progenitor transcriptional factor (Fig. 1D,F). A similar pattern (for the PV, CC, Hip, SRTv, MB) with less density of distribution of human cells was observed in two subsequent experiments. To confirm the glial lineage of the NPCs, we investigated their fate in short-term cultures. Mixtures of neural lineage cells arising from parental progenitors included GFAP/microtubule-associated protein (MAP) glial progenitors, nestin/GFAP neural progenitors (with radial glia characteristics), glutamic acid decarboxylase 67 (GAD67)-negative and class III β-tubulin (Tuj-1)+ neuronal lineage cells (Fig. S2). These data indicated that cells derived from neurospheres retained multi-lineage competence. Expanded human glial cells were integrated in mouse brain tissue without activation of human microglial cells (Fig. 2). We concluded that, generated by neurospheres, NPCs when transplanted at birth in brain lateral ventricle were able to efficiently repopulate NSG mouse brain with some variability, differentiate into astrocytes and retain oligodendrocyte development potential.
Fig. 1.
Glial humanization of the mouse brain. (A) Human lymphoid and brain progenitor cells were transplanted to mice at birth. Blue arrow indicates injection of neural progenitor cells (NPC) into the lateral ventricle (LV). Red arrow indicates intrahepatic (ih) injection of hematopoietic stem/progenitor cells (HSPC). (B) Representative view under a 1× objective lens from a 5-μm paraffin-embedded sagittal section stained for human-specific GFAP (brown). Asterisks indicate fields where cell images were captured for display (C) and quantified (E). (C) Staining with human astrocyte-specific antibodies (hu-GFAP, red) and total glial fibrillary acidic protein (GFAP; green) was performed. Representative images from different brain regions are shown. Original images were collected by a Leica DM6 system at 1000× magnification. Nuclei were stained with 4′,6-diamidino-2-phenylindole (DAPI; blue). Scale bar: 20 μm. (D) Oligodendrocyte-specific nuclear staining (OLIG2; green) and total human-specific nuclear (hN, red) staining was performed, and representative images are shown. The original magnification was 400×. Scale bar: 50 μm. The dashed line in D demarcates the CC from the FC. (E,F) Quantitative data showing the number of human glial cells from one of four experiments with 10 animals. The average percentage of human cells was assessed on two to four representative sagittal sections from each mouse for a selected field of view of the same brain region under 400× magnification. Distribution and proportion of hu-GFAP+ astrocytes among the total number of GFAP+ cells (E); distribution and proportion of hN+ cells positive for OLIG2 (F). Each symbol represents an individual mouse. Data are mean± s.e.m. *P<0.05, **P<0.01, ***P<0.001 by Kruskal–Wallis test. Animals were analyzed at 6 months of age and reconstitution characteristics are shown in Table 1.
Table 1.
Human glial cell distribution pattern on sagittal plane
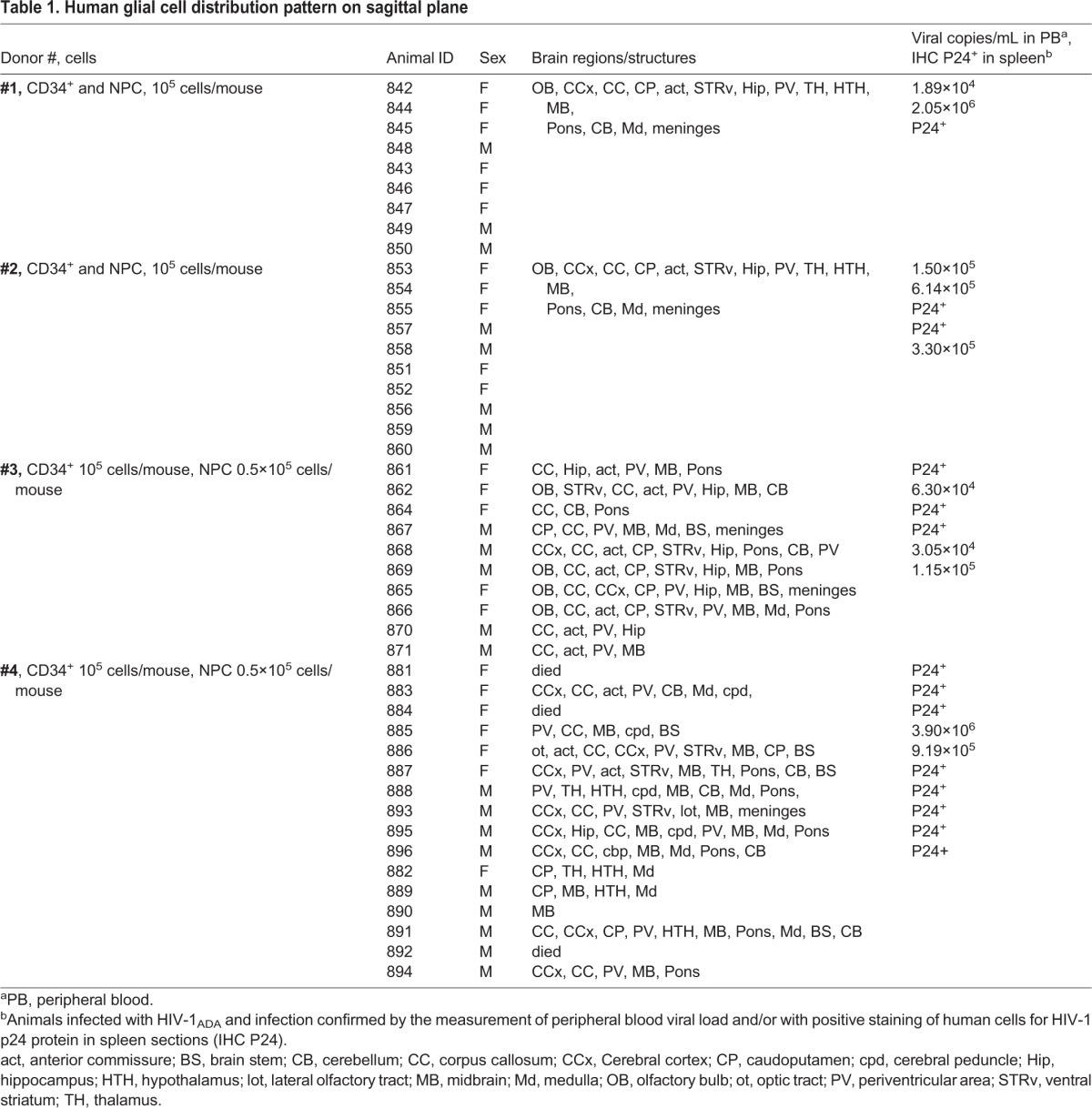
Fig. 2.
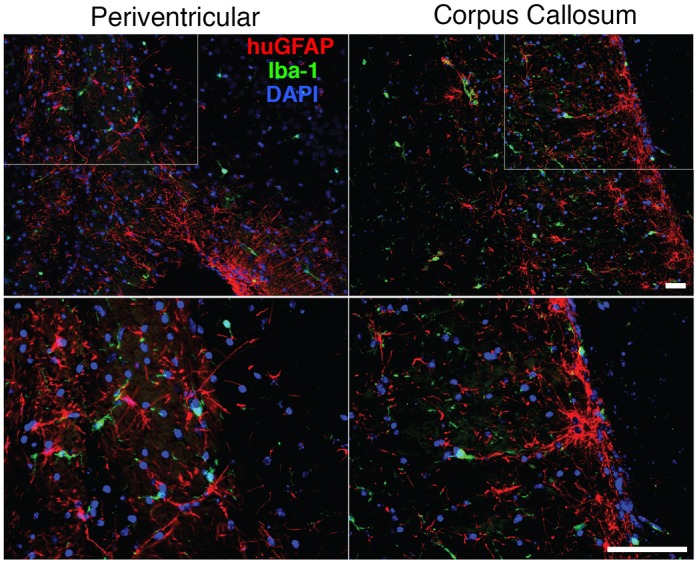
Interaction of human and mouse glial cells. Sagittal section of paraffin-embedded brain tissue stained for human astrocytes (hu-GFAP, red) and mouse microglial cells (Iba-1, green). Original images in the PV and CC were collected by a Leica DM6 system at 100× magnification. The boxed areas are shown at 400× magnification in the bottom panels. Scale bars: 100 μm. Mouse microglial cells are in contact with human astrocytes. There were no morphological signs of activation, formation of microglial nodules or active phagocytosis of human cells.
Assessment of peripheral humanization efficiency
A human peripheral hemato-lymphoid system was established in the NSG mice (Fig. 3). Flow cytometric analyses of peripheral blood of humanized mice at 24 weeks of age showed that among human CD45+ cells, B (CD19+) and T lymphocytes (CD3+) were present (Fig. 3A). The CD14+ monocyte population in peripheral blood was present (Fig. 3B), reflecting previously published observations from our laboratories (Araínga et al., 2016; Dash et al., 2011; Gorantla et al., 2010). In the brain, human peripheral blood leukocytes infiltrated the meningeal and perivascular spaces, and parenchyma. The majority of HLA-DR cells were located in the meningeal space, with fewer numbers in the perivascular space and brain parenchyma (Fig. 3C,D). As we published previously (Gorantla et al., 2010), among these, the greater part were CD163+ macrophages, and some showed branching appearances. Less than 20% of HLA-DR cells were CD4+, and 9% were CD8+ T lymphocytes (Fig. 3C,E). The data were collected in animals with similar levels of human cells in peripheral blood (n=7).
Fig. 3.
Human immune cell repopulation of mouse blood and brain. (A) Fluorescence-activated cell sorting (FACS) analysis of peripheral blood. Representative plots of human cluster of differentiation 45 (CD45)+ cells and human CD3, CD19 and CD14 cells gated from the CD45 lymphocyte population. (B) Percentage of human cells in the peripheral blood of all dual reconstituted mice used in the studies. Each symbol represents an individual mouse. (C) Representative images of the distribution of human immune cells in brain. Paraffin-embedded 5-μm sections were stained for human-specific markers: human leukocyte antigen-antigen D related (HLA-DR), CD163 CD4 and CD8. Representative images from different brain regions are shown. Images were captured by a Nuance multiplex system at an original magnification of 200×. Insets show cells at a magnification of 1000×. Scale bars: 100 μm (20 μm in insets). (D,E) Quantification of human cells positive for HLA-DR, CD163, CD8 and CD4 in selected regions. Numbers represent frequencies of positive cells per section; seven mice with similar levels of lymphoid reconstitution were analyzed. Sagittal sections 10 apart from the midline to the anatomical end of CC [∼2.5 mm according to the adult mouse brain atlas (Paxinos and Franklin, 2001)] from left and right hemispheres were used. Data are mean±s.e.m. Of the regions analyzed, the meninges was the compartment most occupied by HLA-DR+ cells (****P<0.0001) (D) and human cells (*P<0.05, ** P<0.01, ***P<0.001 by Kruskal–Wallis test and Dunn's multiple comparison test) (E).
HIV-1 infection of the dual lymphoid and brain humanized mice
At 24 weeks of age, the mice were divided into two groups. One group was infected intraperitoneally with HIV-1ADA at 104 infectious particles in a volume of 100 μl. We did not observe a significant decline in human CD4+ cells at the time of infection. At ∼5 weeks, flow cytometric analyses showed a ∼20% drop in circulating CD4+ T cell numbers among the CD3+ cell population (P=0.023) in selected animals with similar levels of human cells in peripheral blood (n=6/group). An increase in the CD8+ T lymphocytes in proportion to CD4+ T cells was observed (Fig. 4A,B). After infection, HIV-1 p24+ cells were present in the spleen (Fig. 4C), and mice showed a median of 1.6×105 viral RNA copies/ml blood (Fig. 4D). The brain tissue of infected animals [FC and striatum (STR)] was analyzed for the presence of viral RNA (Fig. 4E). Levels of viral RNA expression in the brain tissue remained low (<50 copies/µg of RNA) compared to the levels observed by systemic infection. HIV-1-infected human cells were observed in the meninges (Fig. 4F). HIV-1 infection influenced immunocyte infiltration in the brain and glial reconstitution. Numbers of human immunocytes were analyzed in animals with comparable levels of peripheral blood leukocyte repopulation by counting HLA-DR+ and CD163+ cells/sagittal section in HIV-1-infected (n=5) and uninfected (n=6) dual transplanted mice. A statistically significant twofold increase in the number of brain-infiltrating immunocytes following HIV-1 infection was observed in the meninges in HIV-1-infected mice compared with uninfected dual reconstituted mice (218.2±8.6 versus 112.0±13.3 cells/section; P=0.0002). In the brain parenchyma, activated human HLA-DR+ cells were 29.8±2.8 and 17.0±3.2 cells/section in infected and uninfected mice, respectively (P=0.017). The majority of human immunocytes were CD163+ macrophages (Fig. 4G). In the spleen, HIV-1 p24 cells were present (Fig. 4C), and the proportion of stained cells for the HIV-1 Nef and p24 proteins in spleen were similar (not shown). To analyze changes in glial cells, animals from two experiments with similar and broad distribution of human glial cells were selected. Sections from these animals were stained for human-specific GFAP, counterstained with Hematoxylin, and then subjected to unbiased digital image analysis (DEFINIENS Tissue Studio®) to assess human glial cell repopulation in 5-µm sections. The total number of nucleated cells/sagittal section remained consistent across the animal groups (107,061±5147 and 110,908±6483 cells/section) (Fig. 4H). In comparison to uninfected controls (n=18), HIV-1-infected mice (n=19) had a lower proportion of human astrocytes/sagittal section (20.7±1.5% versus 15.9±1.4% of human-specific GFAP+ cells, respectively; P=0.022). Serial sections also were stained for human (hu)-GFAP, HIV-1 p24 and Nef. No astrocytes were identified stained with p24 and Nef viral proteins (data not shown). Systemic HIV-1 infection of dual humanized animals increased the influx of human macrophages and affected the number of hu-GFAP-expressing cells.
Fig. 4.
HIV-1 infection affects human cell distributions in dual blood and brain humanized mice. (A) Examples showing CD4+ cell decline in the peripheral blood of HIV-1-infected mice, with a relative increase in the CD8+ cell compartment. (B) Quantification of human CD4 and CD8T cells in the peripheral blood of infected (n=6) and control (n=6) mice. Multiple t-tests using the Holm–Sidak method for multiple comparisons correction were applied to examine significant differences between groups. Data are mean±s.e.m. *Adjusted P=0.045. (C) Immunohistology of spleen sections shows HLA-DR+ cells and the presence of HIV-1-infected cells stained for HIV-1 p24. Images were captured by a Nuance multiplex system at an original magnification of 200×. Scale bar: 100 μm. (D) Peripheral viral load was determined by a COBAS Amplicor System. Each symbol represents an individual infected mouse from all experiments. (E) Viral RNA levels were determined by semi-nested RT-PCR in the HIV+ group (n=3, red) and the control group (n=3, blue) in two brain regions, FC and STR. (F) Immunohistology of brain sections showing the presence of activated HLA-DR+ cells and HIV-1 p24+-infected cells on adjacent serial section. Representative images from the meningeal space containing vascular vessels are shown. Images were captured by a Nuance multiplex system at an original magnification of 200×. Insets show cells at a magnification of 1000×. Scale bars: 100 μm (20 μm in inset). (G) Quantification of infiltrating HLA-DR+ and CD163+ cells in the brain regions of HIV-1-infected (n=5) and uninfected dual reconstituted mice (n=6). Two-way ANOVA using Sidak's multiple comparisons correction was used to examine significant differences between groups. Data are mean±s.e.m. *P=0.017, ****P<0.0001. (H) Quantification of human GFAP+ (left) and all nucleated cells (right) on representative sagittal brain sections of HIV-1-infected (n=18) and control (n=19) mice. Unpaired t-tests were used to examine significant differences between groups. Each point is an individual animal’s averaged counts from two sections presented as mean±s.e.m. *P=0.022; ns, not significant.
Human cell-based transcriptional changes in the HIV-1-infected humanized mouse brain
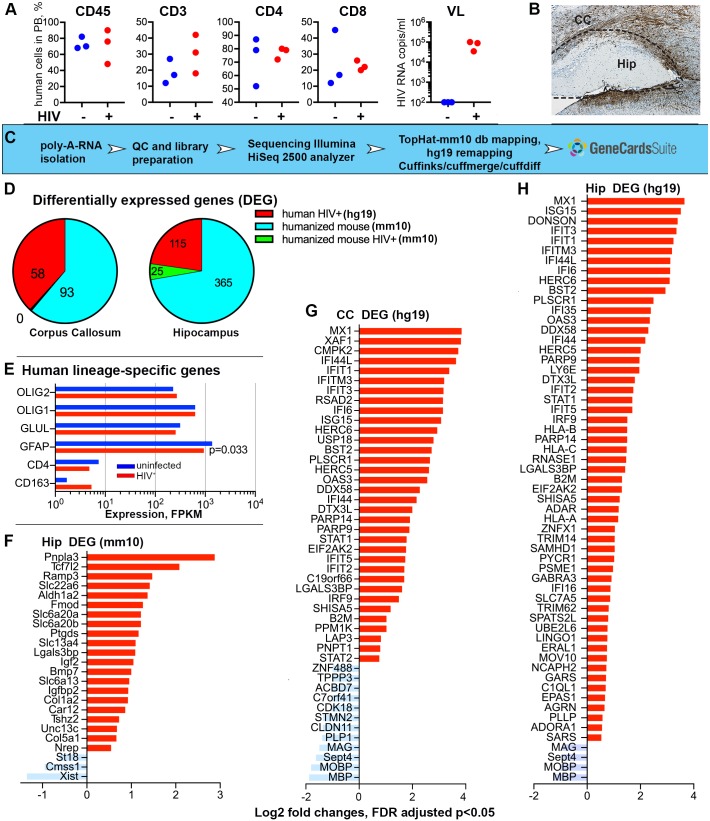
To assess the pathobiological outcomes of viral infection following peripheral immune and brain humanization, we applied deep sequencing to evaluate the transcriptional profiles seen as a consequence of virus-immune cells-glia crosstalk. We selected three uninfected and three infected animals with similar patterns of human immune cell repopulation, similar patterns of astrocyte distribution and density, and similar peripheral viral loads (for infected mice) for study (Fig. 5A). Three equivalent-aged unmanipulated NSG mice served as controls. Hip and CC repopulated by human glial cells were dissected for sequencing (Fig. 5B). All sequenced reads (∼100 bp length) were aligned to the mouse database of the University of California Santa Cruz Genome Browser (GRCm38/mm10; genome.ucsc.edu/). The experiment was designed to search for differentially expressed mouse genes as a result of human cell engraftment and HIV-1-infection (Breschi et al., 2017). Subsequently, the reads unmapped to the mouse genome were realigned to the human genome (GRCh38/hg19) to find human-specific transcriptional changes. The overall mapped mm10 reads average ratio was 92% for all nine Hip samples and 94% for all nine CC samples. For the HIV-1-infected and uninfected humanized mice, the unmapped to mouse database reads were run against the human genome. The average ratio for mapped reads was 32% and 26% for the Hip and CC, respectively. Analyses using the mouse database identified 365 differentially expressed transcripts in the Hip, and 93 in the CC, as a result of the engraftment of human glial cells. When compared to humanized mouse transcripts, few mouse transcripts were differentially expressed as a result of HIV-1 infection in Hip only (Fig. 5E). When the reads unmapped to the mouse genome were realigned to the human reference genome, 115 and 58 human transcripts were found differentially expressed in the Hip and CC, respectively, following infection (Fig. 5F,G). The expression [in fragments per kilobase of transcript per million mapped reads (FPKM)] of the human lineage-specific genes CD163 and CD4 (macrophages and lymphocytes) was significantly lower than that of the genes for human glial transcription factors OLIG1 and OLIG2 (progenitors and oligodendrocyte commitment), GFAP and glutamate-ammonia ligase (glutamine synthase family) genes expressed by astrocytes. HIV-1 infection reduced the expression of human GFAP (FPKM log2 changes -0.55, P=0.033). Expression of mouse cell lineage-specific markers was not statistically significantly affected (data not shown). Region-specific alterations of mouse transcriptome by engrafted human glial cells are summarized in Table S1, Figs S3 and S4. Glial humanization of mouse brain induced region-specific transcriptional changes associated with multiple biological processes and is of interest beyond this report (Goldman et al., 2015).
Fig. 5.
HIV-1 infection induces transcriptional alterations in the brains of dual humanized mice. (A) Characteristics of peripheral reconstitution and the levels of HIV-1 infection in mice examined by RNA sequence analysis (n=3 per group). Percentage of human CD45, CD3, CD4 and CD8 cells, as well as HIV-1 viral load in the peripheral blood of HIV-1-infected dual reconstituted mice (HIV+, red) and control dual reconstituted mice (control, blue) are shown. Three unmanipulated NSG mice of the same age were used as a control and were negative for all these parameters. (B) Representative image of human glial cell reconstitution and scheme of CC and Hip microdissection. (C) A flow chart of transcriptomic and DEG analysis. (D) Identification of differentially expressed genes. Sequenced reads were mapped to the mouse database (mm10) and comparisons were conducted: (1) between non-manipulated NSG mice and dual reconstituted NSG mice to find differences induced by humanization (humanized mouse mm10, blue color); (2) between uninfected and HIV-1-infected dual reconstituted mice to observe differences of mouse transcriptome induced by infection (humanized mouse mm10, green). In the CC, such differences were not identified. Reads unmapped to the mm10 database was realigned to the human database (hg19) and comparisons were conducted between uninfected and HIV-1-infected dual reconstituted mice (human HIV+ hg19, red). (E) Confirmation of the expression of human cell lineage-specific genes for the Hip (hg19) and effects of infection on human GFAP downregulation were statistically significant in t-test comparison, P=0.033, but did not reach significance with FDR adjustment. Expression of mouse cell lineage-specific genes was unaffected by HIV-1 infection. (F-H) Up- and downregulated mouse genes in the Hip of HIV-1-infected dual reconstituted mice compared to uninfected mice (mm10). Up- and downregulated human genes in the CC and Hip of HIV-1-infected dual reconstituted mice compared to uninfected mice (hg19). Genes with 1.5-fold changes with FDR-adjusted P<0.05 were graphed.
Changes in the mouse brain transcriptome following HIV-1 infection
HIV-1-induced transcriptional changes analyzed with alignment to mouse genome identified 25 differentially expressed genes (DEGs) (Fig. 5E) and, according to the GeneCards® integrative database, identified Gene Ontology (GO) biologic processes gene sets that could be associated with metabolic processes, blood vessel development and extracellular matrix re-organization (ALDH1A2, TCF7L2, COL1A2, COL5A1, FMOD, BMP7) as well as neurotransmitters, sugars, organic acids, anion transmembrane transport (SLC6A13, SLC6A20, SLC22A6, SLC13A4) and cellular responses to hormone stimulus (IGFBP2, RAMP3). Few downregulated genes were observed (ST18, XIST) and expression levels of these genes are presented in Table S2. Changes in neurotransmitter expression in the Hip of infected humanized mouse brains could affect cognition (Zhou and Danbolt, 2013) and require further evaluation. For example, IGFBP2 expression was downregulated by humanization, upregulated by HIV-1 infection and is associated with inflammatory responses in HIV-1-infected patients (Helle et al., 2001; Suh et al., 2015). XIST expression was initially upregulated by glial humanization and downregulated by HIV-1 infection. These changes are related to the control of gene expression (Groen and Morris, 2013) but do not reflect ongoing viral infection.
Species-specific transcriptional alterations in humanized brain following HIV-1 infection
The major observation is species-specific transcriptional changes in dual humanized HIV-1-infected mice brains. In contrast to mouse transcriptome, alignment to the human genome reveals an overlapping pattern of upregulated and downregulated genes in the Hip and CC (Fig. 5F,G; Fig. S4, Table S2). The upregulated genes were strongly associated with type 1 and 2 interferon (IFN) responses and specific signaling pathways. These were linked to host viral defense responses (MX1, IFIT families, PLSCR1, EIF2AK2, IFI16, ADAR, OAS3, MX1, BST2, RSAD2), RNA catabolism (CMPK2, PNPT1), ISG15 protein conjugation, regulation of type 1 IFN production (HERC6, ISG15, DXT3L, DDX58, PPAR9, PPM1K) and cytokine-mediated signaling. The spectrum of upregulated genes in the Hip overlapped with that of the CC-upregulated genes. In addition, upregulated genes associated with norepinephrine metabolic processes (EPAS1, LY6E) and those related to neural and glial differentiation (PARP10, GARS, AGRN, SOX10, LINGO1) were found. In the CC and Hip, the identified downregulated genes were linked to myelination and axon ensheathment (MBP, MOBP, MAG, PLP1, CLDN11), neural progenitor differentiation (STMN2, ZNF488, IGFBP5, BIN1, APLP1), glial structural integrity, lipid metabolism, ion transportation and cell cycle regulation (Fig. S4, Table S2). Identified transcriptional changes show ongoing human glial antiviral response to HIV-1 infection.
Human astrocytes produce type 1 IFN during infected macrophage-astrocyte co-cultivation
The upregulated expression of genes related to type 1 IFN responses in the chimeric murine brains following HIV-1 infection prompts the need for investigation of the possible source of IFN. Although almost all nucleated cells can produce type 1 IFN, plasmacytoid dendritic cells are the most potent IFN producers (Steinman, 1991). However, prior studies have demonstrated that astrocytes abortively infected by neurotropic viruses are also a potent source of IFN beta (IFN-β) in mice (Pfefferkorn et al., 2016). To identify the source of type 1 IFN in response to HIV-1 infection in dual humanized mice, we used transwell systems to co-culture human fetal astrocytes and HIV-1-infected monocyte-derived macrophages (MDMs). After 3 days of co-culture with HIV-1-infected MDMs and astrocytes, astrocytes were found to produce IFN-β. The levels of IFN-β reached a peak at 5 days. Three independent donors were used; a representative experiment is shown in Fig. 6. The concentration of IFN-β produced by HIV-infected MDMs alone remained at relatively low levels (approximately 15 pg/ml, detection limit). The concentration of IFN-β in control astrocytes and MDMs was below detectable throughout the experimental observation period.
Fig. 6.

Astrocyte production of IFN-β. Levels of human IFN-β were measured by ELISA in the supernatants collected from astrocytes (Astr, green), a co-culture of astrocytes and control monocyte-derived macrophages (Astr+MDM, red), a co-culture of astrocytes and HIV-infected macrophages (Astr+HIV-MDM, blue), HIV-1-infected MDMs (HIV-MDM, purple) and controls (MDM, orange). The x-axis indicates the time points before and after co-culture (24 h, 3, 5 and 7 days). Data are expressed as the mean of triplicate technical replicates from one of three independent experiments (each performed with distinct donors). Student t-tests were performed to compare astrocytes with and without HIV-1-infected MDMs (red and blue) for each time point (2 and 4 days). Data are mean±s.e.m.; **P=0.0029, ***P=0.0004, ****P<0.0001.
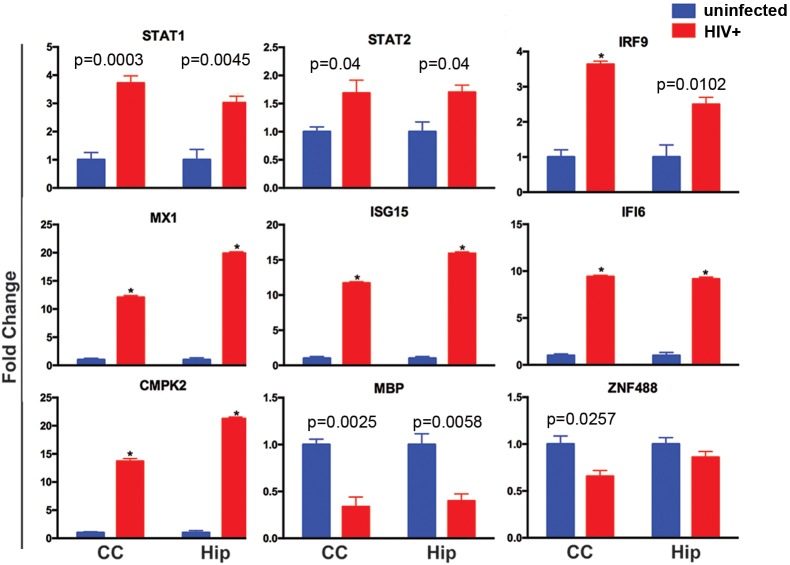
RT-PCR confirmation of IFN-stimulated human genes in the infected humanized brain
To confirm the altered expression and species specificity of the IFN signaling pathway-related transcripts, we applied real-time PCR assays to re-examine the selected genes found affected in RNA sequencing using human- and mouse-specific primers and probes. Crucial elements of the upstream of the type 1 IFN response pathway, STAT1, STAT2 and IRF9, were found to be 3.72, 1.69 and 3.64 times (P=0.0003, P=0.039, P=0.00002) upregulated, respectively, in the CC of HIV-1-infected dual reconstituted mice, compared with control dual reconstituted mice. Upregulation of these three genes was also found in the Hip of HIV-infected humanized mice (P=0.004, P=0.020, P=0.010, respectively) (Fig. 7). The downstream IFN-inducible genes, such as MX1, ISG15, IFI6 and CMPK2, were also found to be significantly upregulated in both the CC (12.09, 11.69, 9.41 and 13.69 times, respectively; P<0.000001) and Hip (19.90, 15.90, 9.17 and 21.25 times, respectively; P<0.000001) of HIV-1-infected humanized mice compared with control animals. We confirmed species-specific upregulation of IRF9/STAT1/STAT2 IFN-stimulated response elements that mediate resistance to viruses (Cheon et al., 2013). Among the myelination- and glial integrity-associated genes, the expression of MBP was reduced 2.94 and 2.5 times (P=0.0058, P=0.0013) in the Hip and CC of HIV-1 infected mice, respectively. The expression of ZNF488 was only found to be significantly downregulated in the CC (P=0.0129), but not in the Hip, of the HIV-1-infected group. Mouse MBP RT-PCR failed to demonstrate any gene expression difference between the HIV-1-infected and control animal groups (Fig. 7).
Fig. 7.
Real-time PCR confirmation of affected human genes in humanized mice brain tissues. Selected human gene expression profiles in the CC and Hip were confirmed by TaqMan® real-time PCR. The HIV-1-infected (n=6) and control (n=5) groups are illustrated. The fold change in gene expression of human STAT1, STAT2, IRF9, MX1, ISG15, IFI6, CMPK2, MBP and ZNF488 between the HIV-1 infected and control groups were determined by using the 2−ΔΔCT method, where ΔCt=Cttarget–CtGAPDH and Δ(ΔCt)=ΔCtHIV–ΔCtcontrol. Multiple t-tests using Holm–Sidak method for multiple comparisons correction were applied to examine significant group differences. Data are mean±s.e.m.; *FDR-adjusted P<0.00001.
DISCUSSION
A mouse model reflecting HIV-1 infection of the nervous system was created that contains both human immune and glial cells in lymphoid organs and brain, respectively. This model represents the combination of NPC transplantation to generate human glia (Nunes et al., 2003; Uchida et al., 2000) and CD34+ HSPC reconstitution to forge a human immune system (Ito et al., 2002). The model builds on previous work demonstrating that transplantation of human neurosphere-derived NPC can occur in a living mouse with functional human-derived neurons and glia (Tamaki et al., 2002; Uchida et al., 2000). Early transplantation proved to be essential to optimize migratory responses of human glia in the mouse brain to facilitate replacement of their murine counterparts through brain subregions (Han et al., 2013; Windrem et al., 2014). Glial-biased differentiation can be explained in two ways. The in situ fate of NPCs is influenced by the local postnatal development of white matter (Nunes et al., 2003). The molecular signals in the recipient white matter might provide the migration route for human cells and facilitate a glia-oriented fate. Second, the expansion of the neural progenitor cells in vitro in the presence of fibroblast growth factor (FGF) and leukemia inhibitory factor (LIF) might drive these cells toward a stage where glial bias is increased with concomitant loss of neurogenic potential (Elkabetz et al., 2008).
We successfully show that human NPCs when transplanted at an early postnatal age demonstrate broad glial distribution through the brain. By 6 months of age, considerable numbers of human astrocytes were seen to have repopulated multiple brain regions along white-matter tracts. Moreover, we found considerable numbers of human OLIG2-positive cells (Fig. 1), signaling the emergence of significant oligodendrocyte differentiation (OLIG1) (Fig. 3D). The broad variability in glial cell distribution and density was associated, in part, with the number of transplanted cells, NPC gestation and collection times, and the stem cell properties that are affected by the number of cell passages and the accuracy of intraventricular injections.
The distribution of human immunocytes in the brain varied, and was comparable to that previously observed in humanized mice created by CD34+ cell transplantation and subsequent HIV-1 infection (Gorantla et al., 2010; Honeycutt et al., 2016). Notably, the majority of human immunocytes present in the brain were observed in the meninges. These were predominantly CD163+ human macrophages. High levels of systemic HIV-1 infection with infected meningeal- and brain-infiltrating cells at lower numbers than those seen in peripheral tissues were detected. Thus, the model reflects three principal features of human brain disease that includes a functional immune system with mobile brain-penetrant monocyte macrophages, sustained high levels of systemic viral infection and the presence of glial target cells that determine alterations in the brain microenvironment. Most importantly, each of the cell types was able to interact with the other in a physiological manner. Unlike a number of operative disease models, our model enables the effects of HIV-1 infection on human brain cells and human-specific immune changes that result from persistent systemic infection to be fully evaluated.
We applied RNA sequencing for dissection of species-specific changes to assess the relevance of the model to human disease. To perform comparison analyses, we selected animals with similar levels of peripheral blood reconstitution and a similar pattern of glial cell distribution. Indeed, our findings in the transcriptome of HIV-1-infected dual reconstituted mice corroborated the relevance of the animal model system. As the most abundant cell type in the brain, astrocytes react to injury or viral infection through cellular activation (Sabri et al., 2003). While HIV-1 infection of CD4+ T lymphocytes, perivascular macrophages and microglia is well recognized (Yadav and Collman, 2009), infection of astrocytes remains unresolved. The question that has remained is whether low level infection of astrocytes or mere exposure of astrocytes to infected cells or HIV-1 itself could cause important physiological changes that alter the brain's functional capacities. Indeed, in contrast to high levels of systemic infections, low levels of HIV-1 RNA were seen in analyzed tissue samples. Although restriction of astrocyte infection can occur at the level of cell entry (Gorry et al., 2003), this in no way detracts from the notion that significant innate immune responses could still occur by the limited virus that is present and explain what was observed at transcriptional levels. Indeed, >30 human genes significantly upregulated in the CC and Hip were found to be closely related to innate and adaptive immunity, HIV host restriction factors and IFN-stimulated factors (Fig. 5; Fig. S4). These findings support the idea that low levels of virus can induce considerable effects in the brain's innate antiviral immune responses. Noticeably, STAT1/STAT2 and IRF9 form a transcriptional complex upon activation of type 1 IFN receptors; this complex can subsequently translocate to the nucleus and induce the expression of a broad spectrum of IFN-stimulated genes that serve to contain infection (Schreiber, 2017). Among such IFN-stimulated factors, MX1, OAS3, RSAD2 (viperin), and all the IFI and IFIT family, are involved in combating viruses at nearly every stage of the viral life cycle (Espert et al., 2005; Fricke et al., 2014; Laguette et al., 2011; Lu et al., 2011; Nasr et al., 2012; Neil et al., 2008; Okumura et al., 2006; Rivieccio et al., 2006; Spragg and Emerman, 2013). In the Hip, in addition to the upregulated genes introduced previously, class I HLA genes were found to be upregulated, which is yet another downstream effect of the type 1 IFN response.
The upregulation of the human-specific IFN signaling-related genes IRF9/STAT1/STAT2 was confirmed by real-time PCR assays using human-specific probes. We also confirmed, by RT-PCR, upregulation of a rare mRNA transcript identified by RNA sequencing for CMPK2, which could belong to infiltrating human macrophages as well as glial cells, and further affirm that the factors serve as a viral restriction factor (Lazear et al., 2013). However, no change in expression of the host restriction factors was reflected in the mouse transcriptional profile as a result of HIV-1 infection. This confirms that HIV-1 can neither efficiently enter mouse cells due to the absence of specific receptors, nor trigger a pattern recognition response by murine cellular defense machinery after viral infection. We cannot exclude the influence of time following HIV-1 infection. Longer times could induce murine innate immune responses that could secondarily alter human cell linked neural damage.
This vigorous type 1 IFN signaling response further leads to the question of what cell source produces type 1 IFN in these dual reconstituted mouse brains. Owing to the increased infiltration of macrophages into the brain during systemic HIV-1 infection in these mice, we tested the interaction between these two cell types for type 1 IFN production in response to HIV-1 infection. The astrocyte production of IFN-β in response to various neurotropic viruses was documented (Pfefferkorn et al., 2016). Neither macrophages nor astrocytes produce type 1 IFN in amounts comparable to those produced by plasmocytoid dendritic cells in response to HIV-1 (Fitzgerald-Bocarsly et al., 2008; Wijewardana et al., 2009). We were able to confirm that the possible source of IFN-β occurs through their interactions with infected macrophages. The transwell co-culture of HIV-1ADA-infected MDMs and astrocytes revealed the temporally dependent dynamics of IFN-β production.
The cellular machinery that glia use to protect themselves from infection could also secondarily create an inflammatory cascade. This could then lead to restricted astrocyte infection and programmed cell death (Thompson et al., 2001). Through the use of unbiased image analysis we found a limited, yet significant, decrease in the number of human GFAP+ astrocytes in the brains of chimeric mice infected with HIV-1 and reduced expression of GFAP (Figs 4 and 6). A similar scenario is known to occur in quiescent CD4T cells, which undergo an abortive infection with accumulation of incomplete reverse viral transcripts (Monroe et al., 2014). In support of this theory, our data showed significant upregulation of genes serving as cytoplasmic sensors for nucleic acids, such as DDX58, DDX60 and IFI6 (Li et al., 2016). Therefore, the downstream signaling and effects of these RNA sensors in glial cells are certainly worthy of further investigation. We also cannot exclude compromised neurogenesis by HIV-1-induced interferon-related pathways, which preclude astrocyte differentiation (Carryl et al., 2015; Geffin and McCarthy, 2013).
The identified downregulated genes are mostly crucial for oligodendrocyte differentiation and myelination. Among them, ZNF488 is a transcriptional factor that interacts and cooperates with Olig2 to promote oligodendrocyte differentiation (Wang et al., 2006). PLP1, MAG, MOBP and MBP are encoding structure proteins of the myelin sheath. CLDN11 encodes a crucial component of the tight junctions between the myelin sheath (Gow et al., 1999; Morita et al., 1999). Upregulation of LONGO1 expression also could inhibit myelination and oligodendrocyte differentiation (Jepson et al., 2012). Together, all of these transcriptional changes suggest early alterations in the structure and function of white matter during HIV infection. This might potentially lead to a compromise in the integrity of the glial system and consequent neural dysfunction.
In summary, we successfully established the dual reconstituted chimeric mouse model that contained both a human immune system and human glia. This model allowed us to access how glial-immunocyte crosstalk might be affected by HIV-1 infection. Using sequencing, we found that the transcriptional profiles from the chimeric brains overlap, in large measure, with the disease profile found in human HIV-1-infected patients with cognitive impairments, encephalitic brains and acute SIV infection (Borjabad et al., 2011; Cserhati et al., 2015; Gelman et al., 2012; Sanfilippo et al., 2017; Sanna et al., 2017; Siangphoe and Archer, 2015; Winkler et al., 2012). These findings underscore the protective role astrocytes have in defending the brain from HIV-1 infection and damage of myelination processes. This model also provides a platform to further investigate the pathobiology of HIV nervous system infection and viral cell reservoirs needed for novel disease-combating therapies and eradication measures.
MATERIALS AND METHODS
Animals, cell transplantation and HIV-1 infection
Newborn NOD/SCID/IL2Rγc−/− (NSG, www.jax.org/strain/005557) mice were bred at the University of Nebraska Medical Center (UNMC). Animal procedures strictly followed the Institutional Animal Care and Use Committee-approved protocols at UNMC and were in adherence with the Animal Welfare Act and the Public Health Service Policy on Humane Care and Use of Laboratory Animals. P0-1 litters were irradiated with 1 Gy (RS 2000 X-ray Irradiator, Rad Source Technologies, Inc., Suwanee, GA, USA). Pups were intrahepatically injected with 5×105 CD34+ HSPCs. These mice were simultaneously transplanted with 0.5-1×105 NPCs into the right lateral ventricle. Two samples of human liver and brain from gestation day 97 (experiments 1 and 2), and two samples from gestation day 117 (experiments 3 and 4), were used to create four cohorts of experimental animals. NPCs were generated by four to six passages. A total of 45 dual reconstituted animals were created: 23 females and 22 males. Blood samples collected from the facial vein were evaluated by flow cytometry starting 8 weeks post-engraftment to monitor expansion of human leukocytes. Mice with established human hemato-lymphoid reconstitution (∼5 months of age) were intraperitoneally infected (n=22) with the macrophage-tropic ADA HIV-1 strain and euthanized 5 weeks after the infection was established (Table 1).
NPC isolation and culture
Human NPCs were isolated from human fetal brains provided by the University of Washington Medical Center Laboratory of Developmental Biology (R24HD000836-51). Informed consent was obtained from all tissue donors and all clinical investigation was conducted according to the principles expressed in the Declaration of Helsinki. The UNMC Scientific Research Oversight Committee (SROC) and Institutional Review Boards at the University of Washington Medical Center and UNMC approved the protocol. Cells were isolated from human fetal brains as previously described (Nunes et al., 2003). Briefly, single cell suspensions were cultivated in NS-A medium (STEMCELL, Mountain View, Canada), containing N2 supplement (1:100; Fisher Scientific, Waltham, MA, USA), neural survival factor-1 (NSF1; 1:50; Lonza, Walkersville, MD, USA), LIF (10 ng/ml; Sigma-Aldrich, St. Louis, MO, USA), epidermal growth factor (EGF; 20 ng/ml; Fisher, MA, USA) and basic fibroblast growth factor (bFGF; 20 ng/ml; STEMCELL), for 14 days before passage. Four hours before injection, the neurospheres were dissociated into single cell suspension with 0.25% Trypsin (Gibco, Grand Island, NY, USA). The single cell suspensions were plated on polystyrene-coated coverslips and cultured for 48 h in vitro. Immunofluorescent cytology was applied to investigate the differential potential of the NPCs.
Human HSPC isolation
Matched to the brain sample, the fetal liver tissue was processed with 0.5 mg/ml DNase, collagenase and hyaluronidase (all from Sigma-Aldrich) using a gentleMACS™ Dissociator (Miltenyi Biotec, Auburn, CA, USA). Cell suspensions were passed through a 40-µm cell strainer and then centrifuged through leukocyte separation medium (MP Biomedicals, Santa Ana, CA, USA) at 100 g for 30 min, with acceleration set to 9, and deceleration set to 1. The intermediate layer of cells was collected for positive isolation of CD34+ cells using a magnetic isolation kit (Miltenyi Biotec, Auburn, CA, USA). CD34+ cells were stored in liquid nitrogen using a freezing medium with 50% fetal bovine serum (FBS), 40% Roswell Park Memorial Institute (RPMI)-1640 medium (Hyclone, Logan, UT, USA), and 10% dimethyl sulfoxide (DMSO; Sigma-Aldrich).
Flow cytometry
Blood samples were collected from a facial vein in ethylenediaminetetraacetic acid (EDTA)-containing tubes (BD Microtainer, Franklin Lakes, NJ, USA) and centrifuged at 300 g for 5 min. Plasma was stored for HIV viral load measurements. Blood cells were reconstituted in a buffer of 2% FBS in phosphate-buffered saline and incubated with antibodies against human cell markers, including CD45+ fluorescein isothiocyanate (FITC, BD/555482), CD3+ Alexa Fluor 700 (BD/561805), CD19+ R-phycoerythrin (PE) cyanine 7 (Cy7, BD/555414), CD4+ allophycocyanin (APC, BD/ 561841), CD8+ Brilliant Violet™ 450 (BV450, BD/562428) and CD14+ PE (BD/555398), for 30 min at 4°C. Samples were analyzed using a BD LSR2 flow cytometer using acquisition software FACS Diva v6 (BD Biosciences, USA), and data were analyzed using FLOWJO analysis software v10.2 (Tree Star, USA; www.flowjo.com). Gates were assigned according to the appropriate control population.
Measurements of viral load in plasma and brain tissues
Viral RNA copies in the murine plasma were determined by using a COBAS Amplicor System v1.5 kit (Roche Molecular Diagnostics, Pleasanton, CA, USA). Expression of HIV-1 group-specific antigen (gag) RNA in brain tissues were analyzed by reverse transcription (RT)-PCR with previously published primers and probes (Araínga et al., 2016). Briefly, cortex and striatum from three HIV-infected dual reconstituted mice and three control dual reconstituted mice were micro-dissected and transferred to 700 µl QIAzol solution (Qiagen, Valencia, CA, USA) for RNA isolation using an RNeasy Mini kit (Qiagen). A Verso cDNA synthesis kit (Thermo Fisher Scientific) prepared cDNA according to the manufacturer's instructions. For the first round of conventional PCR, we used the following primers: sense 5′-TCAGCCCAGAAGTAA-TACCCATGT-3′ and antisense 5′-TGCTATGTCAGTTCCCCTTGGTTCTCT-3′. The PCR settings were as follows: 94°C for 3 min, 15 cycles of 94°C for 30 s, 55°C for 30 s, and 72°C for 1 min. The product of the first PCR was subsequently used as a template in the second semi-nested real-time PCR amplification performed on the ABI StepOne Plus real-time PCR machine (Applied Biosystems, MA, USA) using TaqMan detection chemistry. The primers and probe used for the second PCR were: sense 5′-TCAGCCCAGAAGTAATACCCATGT-3′, antisense 5′-CACTGTGTTTAGCATGGTGTTT-3′, and TaqMan probe FAM-ATTATCAGAAGGAGCCACCCCACAAGA-TAMRA. The real-time PCR settings were as follows: 50°C for 2 min, 95°C for 10 min, 45 cycles of 95°C for 15 s, and 60°C for 1 min. ACH2 cells (8×105) containing one integrated copy of HIV-1 per cell were used in triplicate as standards, with cell and HIV copy numbers ranging in serial 10-fold dilutions from 105 to 102 deoxyribonucleic acid (DNA) copies/reaction.
Immunohistochemistry
Brain tissue was cut sagittally, and the left and right hemispheres from experiments 1 and 2, and right hemispheres from experiments 3 and 4, were fixed with 4% paraformaldehyde for 24 h at 4°C, and then embedded in paraffin. Paraffin-embedded 5-µm thick tissue sections were processed with Declere Solution (Sigma-Aldrich) according to the manufacturer's instructions. Tissue was blocked with 10% normal goat serum in Tris-buffered saline and 0.05% Tween 20 (TBST) for 45 min and then incubated with mouse (ms) anti-human GFAP (1:1000; Y40420/STEM123, TaKaRa Bio, USA), ms anti-human nuclear antigen (1:200; MAB4383, Millipore, Billerica, MA, USA), ms anti-human cytoplasmic marker (1:1000; Takara/STEM121, Mountain View, Canada), ms anti-Nef (1:200; sc-65904, Santa Cruz Biotechnology, Santa Cruz, CA, USA), ms anti-HLA-DR (1:500; M0746, Dako, Carpinteria, CA, USA), ms anti-CD163 (1:50; MA5-11458, Thermo, Denver, CO, USA), rabbit (rb) anti-GFAP (1:1000; Z0034, Dako), and rb anti-human CD4 and CD8 (1:500; ab133616 and ab101500, Abcam, Cambridge, MA, USA). Secondary antibodies were horseradish peroxidase (HRP)-conjugated goat anti-ms and goat anti-rb immunoglobulin G (IgG). Brightfield images were captured and photographed using 20× and 100× objectives on a Nuance Multispectral Tissue Imaging system (CRi, Wobum, MA). Immunostained sections were scanned using a high-resolution scanner (Ventana Medical Systems, Inc., Oro Valley, AZ, USA). DEFINIENS Tissue Studio® software (Definiens AG, Munich, Germany; www.definiens.com/) was used to analyze the brain sections stained for human glial and immune cells. Spleen and brain tissue sections were analyzed for HIV-1 p24 protein staining with anti-HIV-1 p24 (1:10; M0857, Dako). None of the human-specific antibodies had cross-reactivity and stained mouse brain sections were not reconstituted with human cells.
Immunofluorescence
For immunofluorescent staining of paraffin-embedded tissue, sections were processed and blocked as described above. Ms anti-human GFAP, ms anti-human nuclei, rb anti-GFAP, and rb anti-Olig2 (1:500; PhosphoSolution/1538, Aurora, CO, USA) were applied. A Leica DM6 system (Leica Microsystems, Wetzlar, Germany) was used for immunofluorescent imaging. The intensity of illumination and the position of the subregion on the microscope were consistent across all images. For immunofluorescent characterization of cultivated NPCs, ms anti-human GFAP (1:200; Abcam), ms anti-MAP2 (1:200; Santa Cruz Biotechnology), ms anti-glutamic acid decarboxylase 67 (GAD67; 1:500; Millipore), rb anti-nestin (1:200; Millipore), and rb anti-Tuj-1 (1:500; Biolegend, San Diego, CA, USA) were applied. Secondary antibodies were Alexa Fluor 488-conjugated goat anti-ms IgG (1:00; Invitrogen, Grand Island, NY, USA) and Alexa Fluor 594-conjugated goat anti-ms IgG (1:00; Invitrogen). A Leica DM6 system (Leica Microsystems) and a Zeiss LSM510 confocal system (Carl Zeiss Microscopy, Jena, Germany) were also used for immunofluorescent imaging.
Next generation sequencing
Left hemispheres from experiments 3 and 4 of the reconstituted mouse brains (0.5×105 cells/mouse) were dissected by region and flash-frozen for RNA extraction. The brain tissue of three age-matched NSG mice was also collected for nonreconstituted controls. For sequencing, Hip and CC RNA from brain tissue from three uninfected dual-reconstituted animals, three HIV-1-infected mice and three NSG nonreconstituted controls were preserved (RNAlater™, Invitrogen). Tissue was transferred to 700 µl of QIAzol solution (Qiagen) for RNA isolation using an RNeasy Mini kit (Qiagen). After nucleic acid integrity was analyzed, samples were deep sequenced using 100 bp/read, ≤40 million reads/sample using an Illumina HiSeq 2500 Sequence Analyzer (Illumina, Inc., San Diego, CA, USA). Reads were trimmed using the fqtrim (ccb.jhu.edu/software/fqtrim/) software to remove ambiguous bases from the reads. Read alignment and differential gene expression was performed using the programs from the Tuxedo RNA-seq tool pipeline. The trimmed reads were then aligned to the mouse genome (version mm10/GRCm38) and the hg19 human genome (when necessary) using the TopHat aligner (ccb.jhu.edu/software/tophat/index.shtml), version 2.1.1. The ratio of aligned reads per total reads was calculated to assure quality alignments. Unaligned reads coming from the humanized samples were remapped to the hg19 database. FPKM values were calculated for each gene in each sample using Cufflinks software, version 2.2.1 (cole-trapnell-lab.github.io/cufflinks/). This was performed to calculate each gene's expression level in each sample. An FDR-adjusted P value of 5% was used in all Cuffdiff sample comparisons. For both regions (Hip and CC), the control samples (NSG unmanipulated) to the humanized mouse samples (blood and brain reconstituted), and the humanized mouse samples to the humanized mouse samples with HIV, were compared. The reads were mapped to the mm10 mouse genome and the mouse transcriptome. For both tissues, the unmapped reads, which did not map to the mouse genome, were collected and remapped to the human genome. This was performed in order to see what human genes were expressed in these tissues. Cuffdiff was specifically used because it normalizes the expression values and protects against overdispersion so that the values fit into a normalized bell curve (Trapnell et al., 2012).
Macrophage and human fetal astrocyte isolation and cultivation
Human monocytes were isolated by leukapheresis from HIV-1/2 and hepatitis seronegative donors. Human monocytes (2×105) were seeded in the inserts of 24-well transwell plates with a pore size of 0.4 μm. (Corning Costar, Corning, NY, USA). Dulbecco's Modified Eagle's Medium (DMEM) with 10% heat-inactivated pooled human serum, 2 mM L-glutamine, 50 µg/ml gentamicin, 10 µg/ml ciprofloxacin and macrophage colony-stimulating factor (MCSF)-enriched conditioned medium maintained at 37°C in a 5% CO2 incubator was used (Gendelman et al., 1988). On day 7, differentiated MDMs were infected with HIV-1ADA [multiplicity of infection (MOI)=0.01] for 12 h. Infected macrophages were maintained in DMEM containing 10% heat-inactivated pooled human serum, 2 mM L-glutamine, 50 µg/ml gentamicin and 10 µg/ml ciprofloxacin for another 6 days before the inserts were transferred to wells with astrocytes at the bottom. Human fetal astrocytes (HFAs) were isolated and cultured from fetal donors (Nath et al., 1995). HFAs (5×105) were seeded at the bottom of 24-well transwell plates and maintained in DMEM/F12 (Invitrogen) containing 10% FBS and antibiotics. Supernatants from HIV-1-infected and control MDM cultures were collected from 2 to 6 days before MDM and astrocyte co-cultivation. Supernatants from the transwell system were collected at 24 h, 3, 5 and 7 days.
IFN-β enzyme-linked immunosorbent assay
IFN-β was measured in the supernatants of astrocytes, a co-culture of astrocytes and control macrophages, a co-culture of astrocytes and HIV-infected macrophages, HIV-infected macrophages and control macrophages using the Human IFN-β bioluminescent ELISA kit (www.invivogen.com/lumikine-hifnb), according to the manufacturer's instructions.
RT-PCR for human and mouse transcripts
First-strand cDNA was prepared from CC and Hip using the same method described above. For both brain regions, we compared the control humanized mouse samples to the humanized mouse samples with HIV. The catalog numbers of all TagMan® real-time PCR assays from Life Technologies are as follows: hu-STAT1 (Hs01013996_m1), hu-STAT2 (Hs01013123_m1), hu-IRF9 (Hs00196051_m1), hu-MX1 (Hs00895609_m1), hu-ISG15 (Hs01921425_s1), hu-CMPK2 (Hs01013364_m1), hu-IFI6 (Hs00242571_m1), hu-MBP (Hs00921945_m1), hu-ZNF488 (Hs00289045_s1), hu-GAPDH (Hs03929097_g1), ms-MX1 (Mm00487796_m1), ms-MBP (Mm01266402_m1), ms-GAPDH (Mm999999_g1). The real-time PCR settings were as follows: 50°C for 2 min, 95°C for 10 min, 40 cycles of 95°C for 15 s, and 60°C for 1 min. All real-time assays were carried out with an Applied Biosystems StepOnePlus Real-Time PCR System. The fold change of each target gene mRNA relative to GAPDH between the HIV+ group and the control group was determined. This was performed by using threshold cycle (Ct) and the 2−ΔΔCT method, where ΔCt=Cttarget–CtGAPDH and Δ(ΔCt)=ΔCtHIV–ΔCtcontrol.
Statistical analysis
Values from all quantified astrocytes, oligodendrocytes, macrophages and lymphocytes and cell groups were averaged and presented as mean±s.e.m.; multiple t-tests using the Holm–Sidak method for multiple comparisons correction was applied to examine significant differences between groups. Two-way analysis of variance (ANOVA) using Sidak's multiple comparisons correction was used to examine significant differences between groups. For RNA sequencing data, the TopHat/Cuffdiff pipeline was run on the reads for each sample in order to identify differentially expressed genes (Trapnell et al., 2012).
Supplementary Material
Acknowledgements
We thank Prasanta Dash, Raghubendra Sing Dagur and Mariluz Anamelva Arainga Ramirez for technical support; and Li Wu, Yan Cheng, and Amanda Branch-Woods for assistance with preparing cells and managing animals. Assistance from Cathy Gebhart, Technical Director of The Molecular Diagnostics Laboratory, for viral load analysis is noted and appreciated. We also acknowledge the UNMC Flow Cytometry Research Facility (Philip Hexley, Director) for technical support.
Footnotes
Competing interests
The authors declare no competing or financial interests.
Author contributions
Conceptualization: S.G., H.E.G., L.Y.P.; Methodology: W.L., S.G., H.E.G., L.Y.P.; Validation: W.L., S.G., L.Y.P.; Formal analysis: W.L., L.Y.P.; Investigation: W.L., S.G., L.Y.P.; Resources: L.Y.P.; Data curation: W.L., S.G., L.Y.P.; Writing - original draft: W.L., L.Y.P.; Writing - review & editing: S.G., H.E.G., L.Y.P.; Supervision: S.G., H.E.G., L.Y.P.; Project administration: H.E.G., L.Y.P.; Funding acquisition: S.G., H.E.G., L.Y.P.
Funding
This work was supported by the National Institutes of Health (028555), the National Institute of Neurological Disorders and Stroke (36126), the National Institute of Mental Health (64570), the National Institute on Aging (043540), the NIH Office of the Director (018546), the National Institute of General Medical Sciences (103427), and the National Cancer Institute (036727).
Supplementary information
Supplementary information available online at http://dmm.biologists.org/lookup/doi/10.1242/dmm.031773.supplemental
References
- Araínga M., Su H., Poluektova L. Y., Gorantla S. and Gendelman H. E. (2016). HIV-1 cellular and tissue replication patterns in infected humanized mice. Sci. Rep. 6, 23513 10.1038/srep23513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bednar M. M., Sturdevant C. B., Tompkins L. A., Arrildt K. T., Dukhovlinova E., Kincer L. P. and Swanstrom R. (2015). Compartmentalization, Viral Evolution, and Viral Latency of HIV in the CNS. Curr. HIV/AIDS Rep. 12, 262-271. 10.1007/s11904-015-0265-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borjabad A., Morgello S., Chao W., Kim S.-Y., Brooks A. I., Murray J., Potash M. J. and Volsky D. J. (2011). Significant effects of antiretroviral therapy on global gene expression in brain tissues of patients with HIV-1-associated neurocognitive disorders. PLoS Pathog. 7, e1002213 10.1371/journal.ppat.1002213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boska M. D., Dash P. K., Knibbe J., Epstein A. A., Akhter S. P., Fields N., High R., Makarov E., Bonasera S., Gelbard H. A. et al. (2014). Associations between brain microstructures, metabolites, and cognitive deficits during chronic HIV-1 infection of humanized mice. Mol. Neurodegener 9, 58 10.1186/1750-1326-9-58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breschi A., Gingeras T. R. and Guigó R. (2017). Comparative transcriptomics in human and mouse. Nat. Rev. Genet. 18, 425-440. 10.1038/nrg.2017.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carryl H., Swang M., Lawrence J., Curtis K., Kamboj H., Van Rompay K. K. A., De Paris K. and Burke M. W. (2015). Of mice and monkeys: can animal models be utilized to study neurological consequences of pediatric HIV-1 infection? ACS Chem. Neurosci. 6, 1276-1289. 10.1021/acschemneuro.5b00044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chauhan A. (2015). Enigma of HIV-1 latent infection in astrocytes: an in-vitro study using protein kinase C agonist as a latency reversing agent. Microbes Infect. 17, 651-659. 10.1016/j.micinf.2015.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheon H., Holvey-Bates E. G., Schoggins J. W., Forster S., Hertzog P., Imanaka N., Rice C. M., Jackson M. W., Junk D. J. and Stark G. R. (2013). IFNbeta-dependent increases in STAT1, STAT2, and IRF9 mediate resistance to viruses and DNA damage. EMBO J. 32, 2751-2763. 10.1038/emboj.2013.203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cserhati M. F., Pandey S., Beaudoin J. J., Baccaglini L., Guda C. and Fox H. S. (2015). The National NeuroAIDS Tissue Consortium (NNTC) Database: an integrated database for HIV-related studies. Database (Oxford) 2015, bav074 10.1093/database/bav074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dash P. K., Gorantla S., Gendelman H. E., Knibbe J., Casale G. P., Makarov E., Epstein A. A., Gelbard H. A., Boska M. D. and Poluektova L. Y. (2011). Loss of neuronal integrity during progressive HIV-1 infection of humanized mice. J. Neurosci. 31, 3148-3157. 10.1523/JNEUROSCI.5473-10.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dou H., Morehead J., Bradley J., Gorantla S., Ellison B., Kingsley J., Smith L. M., Chao W., Bentsman G., Volsky D. J. et al. (2006). Neuropathologic and neuroinflammatory activities of HIV-1-infected human astrocytes in murine brain. Glia 54, 81-93. 10.1002/glia.20358 [DOI] [PubMed] [Google Scholar]
- Elkabetz Y., Panagiotakos G., Al Shamy G., Socci N. D., Tabar V. and Studer L. (2008). Human ES cell-derived neural rosettes reveal a functionally distinct early neural stem cell stage. Genes Dev. 22, 152-165. 10.1101/gad.1616208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epstein L. G. and Gendelman H. E. (1993). Human immunodeficiency virus type 1 infection of the nervous system: pathogenetic mechanisms. Ann. Neurol. 33, 429-436. 10.1002/ana.410330502 [DOI] [PubMed] [Google Scholar]
- Espert L., Degols G., Lin Y.-L., Vincent T., Benkirane M. and Mechti N. (2005). Interferon-induced exonuclease ISG20 exhibits an antiviral activity against human immunodeficiency virus type 1. J. Gen. Virol. 86, 2221-2229. 10.1099/vir.0.81074-0 [DOI] [PubMed] [Google Scholar]
- Farina C., Aloisi F. and Meinl E. (2007). Astrocytes are active players in cerebral innate immunity. Trends Immunol. 28, 138-145. 10.1016/j.it.2007.01.005 [DOI] [PubMed] [Google Scholar]
- Fitzgerald-Bocarsly P., Dai J. and Singh S. (2008). Plasmacytoid dendritic cells and type I IFN: 50 years of convergent history. Cytokine Growth Factor. Rev. 19, 3-19. 10.1016/j.cytogfr.2007.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fricke T., White T. E., Schulte B., de Souza Aranha Vieira D. A., Dharan A., Campbell E. M., Brandariz-Nuñez A. and Diaz-Griffero F. (2014). MxB binds to the HIV-1 core and prevents the uncoating process of HIV-1. Retrovirology 11, 1 10.1186/s12977-014-0068-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geffin R. and McCarthy M. (2013). Innate immune responses to HIV infection in the central nervous system. Immunol. Res. 57, 292-302. 10.1007/s12026-013-8445-4 [DOI] [PubMed] [Google Scholar]
- Gelman B. B., Chen T., Lisinicchia J. G., Soukup V. M., Carmical J. R., Starkey J. M., Masliah E., Commins D. L., Brandt D. and Grant I. (2012). The National NeuroAIDS Tissue Consortium brain gene array: two types of HIV-associated neurocognitive impairment. PLoS ONE 7, e46178 10.1371/journal.pone.0046178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gendelman H. E., Orenstein J. M., Martin M. A., Ferrua C., Mitra R., Phipps T., Wahl L. A., Lane H. C., Fauci A. S., Burke D. S. et al. (1988). Efficient isolation and propagation of human immunodeficiency virus on recombinant colony-stimulating factor 1-treated monocytes. J. Exp. Med. 167, 1428-1441. 10.1084/jem.167.4.1428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman S. A., Nedergaard M. and Windrem M. S. (2015). Modeling cognition and disease using human glial chimeric mice. Glia 63, 1483-1493. 10.1002/glia.22862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Scarano F. and Martín-García J. (2005). The neuropathogenesis of AIDS. Nat. Rev. Immunol. 5, 69-81. 10.1038/nri1527 [DOI] [PubMed] [Google Scholar]
- Gorantla S., Makarov E., Finke-Dwyer J., Castanedo A., Holguin A., Gebhart C. L., Gendelman H. E. and Poluektova L. (2010). Links between progressive HIV-1 infection of humanized mice and viral neuropathogenesis. Am. J. Pathol. 177, 2938-2949. 10.2353/ajpath.2010.100536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorantla S., Poluektova L. and Gendelman H. E. (2012). Rodent models for HIV-associated neurocognitive disorders. Trends Neurosci. 35, 197-208. 10.1016/j.tins.2011.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorry P. R., Ong C., Thorpe J., Bannwarth S., Thompson K. A., Gatignol A., Vesselingh S. L. and Purcell D. F. (2003). Astrocyte infection by HIV-1: mechanisms of restricted virus replication, and role in the pathogenesis of HIV-1-associated dementia. Curr. HIV Res. 1, 463-473. 10.2174/1570162033485122 [DOI] [PubMed] [Google Scholar]
- Gow A., Southwood C. M., Li J. S., Pariali M., Riordan G. P., Brodie S. E., Danias J., Bronstein J. M., Kachar B. and Lazzarini R. A. (1999). CNS myelin and sertoli cell tight junction strands are absent in Osp/claudin-11 null mice. Cell 99, 649-659. 10.1016/S0092-8674(00)81553-6 [DOI] [PubMed] [Google Scholar]
- Groen J. N. and Morris K. V. (2013). Chromatin, non-coding RNAs, and the expression of HIV. Viruses 5, 1633-1645. 10.3390/v5071633 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han X., Chen M., Wang F., Windrem M., Wang S., Shanz S., Xu Q., Oberheim N. A., Bekar L., Betstadt S. et al. (2013). Forebrain engraftment by human glial progenitor cells enhances synaptic plasticity and learning in adult mice. Cell Stem Cell 12, 342-353. 10.1016/j.stem.2012.12.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helle S. I., Ueland T., Ekse D., Froland S. S., Holly J. M., Lonning P. E. and Aukrust P. (2001). The insulin-like growth factor system in human immunodeficiency virus infection: relations to immunological parameters, disease progression, and antiretroviral therapy. J. Clin. Endocrinol. Metab. 86, 227-233. 10.1210/jc.86.1.227 [DOI] [PubMed] [Google Scholar]
- Honeycutt J. B., Wahl A., Baker C., Spagnuolo R. A., Foster J., Zakharova O., Wietgrefe S., Caro-Vegas C., Madden V., Sharpe G. et al. (2016). Macrophages sustain HIV replication in vivo independently of T cells. J. Clin. Invest. 126, 1353-1366. 10.1172/JCI84456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito M., Hiramatsu H., Kobayashi K., Suzue K., Kawahata M., Hioki K., Ueyama Y., Koyanagi Y., Sugamura K., Tsuji K. et al. (2002). NOD/SCID/gamma(c)(null) mouse: an excellent recipient mouse model for engraftment of human cells. Blood 100, 3175-3182. 10.1182/blood-2001-12-0207 [DOI] [PubMed] [Google Scholar]
- Jaeger L. B. and Nath A. (2012). Modeling HIV-associated neurocognitive disorders in mice: new approaches in the changing face of HIV neuropathogenesis. Dis. Model Mech. 5, 313-322. 10.1242/dmm.008763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jepson S., Vought B., Gross C. H., Gan L., Austen D., Frantz J. D., Zwahlen J., Lowe D., Markland W. and Krauss R. (2012). LINGO-1, a transmembrane signaling protein, inhibits oligodendrocyte differentiation and myelination through intercellular self-interactions. J. Biol. Chem. 287, 22184-22195. 10.1074/jbc.M112.366179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laguette N., Sobhian B., Casartelli N., Ringeard M., Chable-Bessia C., Ségéral E., Yatim A., Emiliani S., Schwartz O. and Benkirane M. (2011). SAMHD1 is the dendritic-and myeloid-cell-specific HIV-1 restriction factor counteracted by Vpx. Nature 474, 654-657. 10.1038/nature10117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazear H. M., Lancaster A., Wilkins C., Suthar M. S., Huang A., Vick S. C., Clepper L., Thackray L., Brassil M. M., Virgin H. W. et al. (2013). IRF-3, IRF-5, and IRF-7 coordinately regulate the type I IFN response in myeloid dendritic cells downstream of MAVS signaling. PLoS Pathog. 9, e1003118 10.1371/journal.ppat.1003118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li P., Kaiser P., Lampiris H. W., Kim P., Yukl S. A., Havlir D. V., Greene W. C. and Wong J. K. (2016). Stimulating the RIG-I pathway to kill cells in the latent HIV reservoir following viral reactivation. Nat. Med. 22, 807-811. 10.1038/nm.4124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu J., Pan Q., Rong L., Liu S.-L. and Liang C. (2011). The IFITM proteins inhibit HIV-1 infection. J. Virol. 85, 2126-2137. 10.1128/JVI.01531-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe K. M., Yang Z., Johnson J. R., Geng X., Doitsh G., Krogan N. J. and Greene W. C. (2014). IFI16 DNA sensor is required for death of lymphoid CD4 T cells abortively infected with HIV. Science 343, 428-432. 10.1126/science.1243640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morita K., Sasaki H., Fujimoto K., Furuse M. and Tsukita S. (1999). Claudin-11/OSP-based tight junctions of myelin sheaths in brain and Sertoli cells in testis. J. Cell Biol. 145, 579-588. 10.1083/jcb.145.3.579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Narayan O. and Clements J. E. (1989). Biology and pathogenesis of lentiviruses. J. Gen. Virol. 70, 1617-1639. 10.1099/0022-1317-70-7-1617 [DOI] [PubMed] [Google Scholar]
- Nasr N., Maddocks S., Turville S. G., Harman A. N., Woolger N., Helbig K. J., Wilkinson J., Bye C. R., Wright T. K. and Rambukwelle D. (2012). HIV-1 infection of human macrophages directly induces viperin which inhibits viral production. Blood 120, 778-788. 10.1182/blood-2012-01-407395 [DOI] [PubMed] [Google Scholar]
- Nath A., Hartloper V., Furer M. and Fowke K. R. (1995). Infection of human fetal astrocytes with HIV-1: viral tropism and the role of cell to cell contact in viral transmission. J. Neuropathol. Exp. Neurol. 54, 320-330. 10.1097/00005072-199505000-00005 [DOI] [PubMed] [Google Scholar]
- Neil S. J. D., Zang T. and Bieniasz P. D. (2008). Tetherin inhibits retrovirus release and is antagonized by HIV-1 Vpu. Nature 451, 425-430. 10.1038/nature06553 [DOI] [PubMed] [Google Scholar]
- Nunes M. C., Roy N. S., Keyoung H. M., Goodman R. R., McKhann G., Jiang L., Kang J., Nedergaard M. and Goldman S. A. (2003). Identification and isolation of multipotential neural progenitor cells from the subcortical white matter of the adult human brain. Nat. Med. 9, 439-447. 10.1038/nm837 [DOI] [PubMed] [Google Scholar]
- Oberheim N. A., Takano T., Han X., He W., Lin J. H. C., Wang F., Xu Q., Wyatt J. D., Pilcher W., Ojemann J. G. et al. (2009). Uniquely hominid features of adult human astrocytes. J. Neurosci. 29, 3276-3287. 10.1523/JNEUROSCI.4707-08.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okumura A., Lu G., Pitha-Rowe I. and Pitha P. M. (2006). Innate antiviral response targets HIV-1 release by the induction of ubiquitin-like protein ISG15. Proc. Natl. Acad. Sci. USA 103, 1440-1445. 10.1073/pnas.0510518103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paxinos G. and Franklin K. B. J. (2001). The mouse brain in stereotaxic coordinates. San Diego: Academic Press. [Google Scholar]
- Pfefferkorn C., Kallfass C., Lienenklaus S., Spanier J., Kalinke U., Rieder M., Conzelmann K.-K., Michiels T. and Staeheli P. (2016). Abortively infected astrocytes appear to represent the main source of interferon beta in the virus-infected brain. J. Virol. 90, 2031-2038. 10.1128/JVI.02979-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rivieccio M. A., Suh H.-S., Zhao Y., Zhao M.-L., Chin K. C., Lee S. C. and Brosnan C. F. (2006). TLR3 ligation activates an antiviral response in human fetal astrocytes: a role for viperin/cig5. J. Immunol. 177, 4735-4741. 10.4049/jimmunol.177.7.4735 [DOI] [PubMed] [Google Scholar]
- Russell R. A., Chojnacki J., Jones D. M., Johnson E., Do T., Eggeling C., Padilla-Parra S. and Sattentau Q. J. (2017). Astrocytes resist HIV-1 fusion but engulf infected macrophage material. Cell Rep. 18, 1473-1483. 10.1016/j.celrep.2017.01.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabri F., Titanji K., Milito A. and Chiodi F. (2003). Astrocyte activation and apoptosis: their roles in the neuropathology of HIV infection. Brain Pathol. 13, 84-94. 10.1111/j.1750-3639.2003.tb00009.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanfilippo C., Pinzone M. R., Cambria D., Longo A., Palumbo M., Di Marco R., Condorelli F., Nunnari G., Malaguarnera L. and Di Rosa M. (2017). OAS gene family expression is associated with HIV-related neurocognitive disorders. Mol. Neurobiol. 54, 1-10 10.1007/s12035-017-0460-3 [DOI] [PubMed] [Google Scholar]
- Sanna P. P., Repunte-Canonigo V., Masliah E. and Lefebvre C. (2017). Gene expression patterns associated with neurological disease in human HIV infection. PLoS ONE 12, e0175316 10.1371/journal.pone.0175316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saylor D., Dickens A. M., Sacktor N., Haughey N., Slusher B., Pletnikov M., Mankowski J. L., Brown A., Volsky D. J. and McArthur J. C. (2016). HIV-associated neurocognitive disorder--pathogenesis and prospects for treatment. Nat. Rev. Neurol. 12, 234-248. 10.1038/nrneurol.2016.27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreiber G. (2017). The molecular basis for differential type I interferon signaling. J. Biol. Chem. 292, 7285-7294. 10.1074/jbc.R116.774562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schweighardt B. and Atwood W. J. (2001). HIV type 1 infection of human astrocytes is restricted by inefficient viral entry. AIDS Res. Hum. Retroviruses 17, 1133-1142. 10.1089/088922201316912745 [DOI] [PubMed] [Google Scholar]
- Siangphoe U. and Archer K. J. (2015). Gene expression in HIV-associated neurocognitive disorders: a meta-analysis. JAIDS J. Acquir. Immune Defic. Syndr. 70, 479-488. 10.1097/QAI.0000000000000800 [DOI] [PubMed] [Google Scholar]
- Spragg C. J. and Emerman M. (2013). Antagonism of SAMHD1 is actively maintained in natural infections of simian immunodeficiency virus. Proc. Natl Acad. Sci. USA 110, 21136-21141. 10.1073/pnas.1316839110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinman R. M. (1991). The dendritic cell system and its role in immunogenicity. Annu. Rev. Immunol. 9, 271-296. 10.1146/annurev.iy.09.040191.001415 [DOI] [PubMed] [Google Scholar]
- Suh H.-S., Lo Y., Choi N., Letendre S. and Lee S. C. (2015). Insulin-like growth factors and related proteins in plasma and cerebrospinal fluids of HIV-positive individuals. J. Neuroinflammation 12, 72 10.1186/s12974-015-0288-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tamaki S., Eckert K., He D., Sutton R., Doshe M., Jain G., Tushinski R., Reitsma M., Harris B., Tsukamoto A. et al. (2002). Engraftment of sorted/expanded human central nervous system stem cells from fetal brain. J. Neurosci. Res. 69, 976-986. 10.1002/jnr.10412 [DOI] [PubMed] [Google Scholar]
- Thompson K. A., McArthur J. C. and Wesselingh S. L. (2001). Correlation between neurological progression and astrocyte apoptosis in HIV-associated dementia. Ann. Neurol. 49, 745-752. 10.1002/ana.1011 [DOI] [PubMed] [Google Scholar]
- Trapnell C., Roberts A., Goff L., Pertea G., Kim D., Kelley D. R., Pimentel H., Salzberg S. L., Rinn J. L. and Pachter L. (2012). Differential gene and transcript expression analysis of RNA-seq experiments with TopHat and Cufflinks. Nat. Protoc. 7, 562-578. 10.1038/nprot.2012.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uchida N., Buck D. W., He D., Reitsma M. J., Masek M., Phan T. V., Tsukamoto A. S., Gage F. H. and Weissman I. L. (2000). Direct isolation of human central nervous system stem cells. Proc. Natl. Acad. Sci. USA 97, 14720-14725. 10.1073/pnas.97.26.14720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang S.-Z., Dulin J., Wu H., Hurlock E., Lee S.-E., Jansson K. and Lu Q. R. (2006). An oligodendrocyte-specific zinc-finger transcription regulator cooperates with Olig2 to promote oligodendrocyte differentiation. Development 133, 3389-3398. 10.1242/dev.02522 [DOI] [PubMed] [Google Scholar]
- Wijewardana V., Brown K. N. and Barratt-Boyes S. M. (2009). Studies of plasmacytoid dendritic cell dynamics in simian immunodeficiency virus infection of nonhuman primates provide insights into HIV pathogenesis. Curr. HIV Res. 7, 23-29. 10.2174/157016209787048483 [DOI] [PubMed] [Google Scholar]
- Windrem M. S., Schanz S. J., Morrow C., Munir J., Chandler-Militello D., Wang S. and Goldman S. A. (2014). A competitive advantage by neonatally engrafted human glial progenitors yields mice whose brains are chimeric for human glia. J. Neurosci. 34, 16153-16161. 10.1523/JNEUROSCI.1510-14.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winkler J. M., Chaudhuri A. D. and Fox H. S. (2012). Translating the brain transcriptome in neuroAIDS: from non-human primates to humans. J. Neuroimmune Pharmacol. 7, 372-379. 10.1007/s11481-012-9344-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yadav A. and Collman R. G. (2009). CNS inflammation and macrophage/microglial biology associated with HIV-1 infection. J. Neuroimmune Pharmacol. 4, 430-447. 10.1007/s11481-009-9174-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y. and Danbolt N. C. (2013). GABA and glutamate transporters in brain. Front. Endocrinol. (Lausanne) 4, 165 10.3389/fendo.2013.00165 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.