Abstract
Objective
To evaluate the feasibility and acceptability of a Facebook-delivered post-partum weight loss intervention.
Methods
Overweight/obese post-partum women received a 12-week weight loss intervention via Facebook. Feasibility outcomes were recruitment, retention, engagement, and acceptability. Weight loss was an exploratory outcome.
Results
Participants (n=19) were 3.5 (SD: 2.2) months post-partum with baseline BMI 30.1 (SD: 4.2) kg/m2. Retention was 95%. Forty-two percent of participants visibly engaged on the last day of the intervention, and 100% in the last 4 weeks. Eighty-eight percent were likely/very likely to participate again and 82% likely/very likely to recommend the program to a post-partum friend. Average 12-week weight loss was 4.8% (SD: 4.2%); 58% lost ≥5%.
Conclusions and Implications
Findings suggest that this Facebook-delivered intervention is feasible and acceptable and supports research to test efficacy for weight loss. Research is needed on how best to engage participants in social network-delivered weight loss interventions.
Keywords: postpartum, weight loss, social media, pilot study
Introduction
While post-partum weight retention averages 0.5–3 kg, as many as half of women retain ≥5 kg at 1 year, and post-partum weight retention contributes to obesity for many women.1–3 In a recent study, 30% of women who were normal weight pre-pregnancy were overweight at 1 year post-partum, 44% of overweight women had transitioned to obesity, and 97% of obese women remained obese.2 A recent meta-analysis found lifestyle interventions (diet or exercise or both) to be modestly efficacious for post-partum weight loss in randomized controlled trials, yet almost all required in-person participation,4 which is logistically challenging for many women.5–7
Facebook may be an efficient platform for delivering weight loss programming to post-partum women. Facebook is currently the most popular online social network,8 and is used by 81% of online moms.9 Three-quarters percent of Facebook users engage on the platform daily, including 55% who engage multiple times per day,8 for upwards of 50 minutes a day.10 Many women already seek support about health and parenting from their Facebook network. A recent Pew Internet Research survey found that 66% of mothers obtained helpful parenting information from their Facebook network in the past 30 days, and 50% received social/emotional support about a parenting issue.9 Delivering a post-partum weight loss intervention via Facebook allows us to connect with post-partum women where they are, more fully integrating into their lives and daily routines.11 The aim of this study was to assess the feasibility and acceptability of a post-partum weight loss intervention delivered via a private Facebook group.
Methods
Post-partum women were recruited from the inpatient maternity units at UMass Memorial Health Care (UMMHC) in Worcester, MA and the surrounding community in summer 2014. Research staff approached women on the maternity unit between 24–48 hours post-partum, briefly described the study, and obtained permission to contact them in 6–8 weeks. Research staff also posted flyers in the UMMHC outpatient obstetric clinics, on the University of Massachusetts Medical School intranet, and on the Worcester-area Craigslist. Additionally, staff contacted participants from a previous research study of pregnant women who had consented to contact for future research. Research staff screened interested women for eligibility over the phone. Eligible women were ≥18 years old, between 6 weeks and 12 months post-partum, overweight or obese (25 kg/m2 ≤ body mass index (BMI) < 45 kg/m2) based on height and weight self-reported at screening, comfortable participating in English, owned a scale, owned a smartphone, had a Facebook account to which they logged in at least weekly, and had permission to participate from their primary care provider or obstetrician/gynecologist. Exclusion criteria were pregnancy or plans to conceive during the study period, previous or planned bariatric surgery, medical conditions that prevented increasing physical activity or making dietary changes, medications affecting weight, inability to walk ¼ mile without stopping, Type 1 or 2 diabetes, or plans to move during the study period. The University of Massachusetts Medical School Institutional Review Board approved this study.
At a 60-minute baseline visit, participants provided informed consent, staff measured participants’ height and weight, and participants reported their demographics and reproductive and weight history via a secure web form.12 Following the intervention, participants completed an in-person visit, at which staff measured participants’ weight and participants provided feedback on the intervention. Participants received a $50 gift card after completing follow-up.
Participants received a 12-week lifestyle intervention via a secret Facebook group (i.e., a private group in which membership is by invitation only, posts are only viewable by group members, and the group does not appear in searches). The intervention was based on the Diabetes Prevention Program (DPP),13 adapted for the post-partum period and delivery via Facebook. The DPP has established efficacy for weight loss,14 and has been translated to multiple settings and populations15 including primary care via the Internet16 and the post-partum period.17,18 DPP curriculum includes behavioral strategies such as self-monitoring, stimulus control, problem solving, social support, environmental restructuring, stress management, and relapse prevention.13 Investigators converted the didactic content of the DPP into Facebook posts or links to online articles which were included in intervention posts.19 Adaptations for the post-partum period17,18 included specific nutritional needs for breastfeeding women, kid-friendly recipes, links to exercise videos to do with children and/or at home, negotiating responsibilities to care for self, and challenges to lifestyle change common among post-partum women.5,7,20,21 Two coaches (a licensed clinical psychologist and a health promotion researcher) posted a topic of the day, provided support, and encouraged participants to engage in discussion. An obstetrician and a physical therapist with experience with perinatal women were also available to answer questions, particularly those related to their clinical expertise. Participants were provided individualized calorie goals to facilitate a weekly weight loss of 1–2 lbs. For breastfeeding participants, calorie goals accounted for lactation.22 Participants were encouraged to increase physical activity gradually up to a goal of 150 minutes of moderate-intensity physical activity per week. Participants were encouraged to track diet and physical activity using MyFitnessPal®, a free mobile app available for iPhone and Android phones.
Feasibility outcomes were recruitment, retention, engagement, and intervention acceptability. Research staff tracked recruitment efforts and documented reasons for ineligibility. The retention rate was calculated as the rate of completion of the follow-up assessment. Objective engagement data were downloaded from Facebook using NCapture add-on to NVivo 10 software, and the number of posts and replies written by each participant, and the number of posts or replies liked by each participant were summed. Some participant posts were in response to an intervention post (e.g., a post asking participants to post a photo); these posts were considered replies, similar to previous research.23 Engagement variables were not normally distributed, and thus were described by median, inter-quartile range (IQR), and range. Sustained engagement was calculated as the date of the latest post or reply, or date of post or comment liked.24 At follow-up, participants rated on 5-point Likert scales how likely they would be to recommend the program to a post-partum friend and whether they would participate again following a subsequent pregnancy.18
Participants self-reported pre-pregnancy weight and gestational weight gain from the pregnancy they most recently delivered. Post-partum weight retention (lbs) was calculated by subtracting self-reported pre-pregnancy weight from measured baseline weight, and significant post-partum weight retention was defined to be ≥5kg.25 Absolute (lbs) and percent weight loss was calculated from weight measured at baseline and follow-up. Weight loss was calculated using weight measured during week 10 for 1 woman who moved out of state, and using weight self-reported at the end of week 12 for the 1 woman who did not complete her follow-up assessment. Clinically significant weight loss was defined as ≥5%.26 Analyses were conducted in SAS 9.4 (SAS Institute, Inc., Cary, NC).
Results
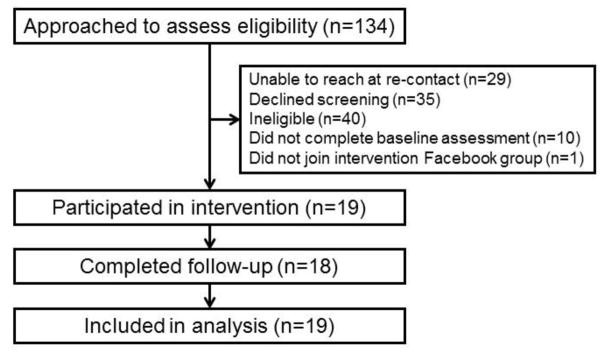
Recruitment and retention are shown in Figure. Forty-three percent (n=30/70) of women screened were eligible. The most common reason for ineligibility was normal weight (n=14; 35% of ineligible individuals). One woman did not complete follow-up; the retention rate was 95%.
Figure.
Participant Flow Diagram
Participants (n=19) were 31.5 (SD: 3.2) years old and 3.5 (SD: 2.2) months post-partum (Table). Average BMI was 30.1 (SD: 4.2) kg/m2 at baseline; 42% were obese, and 63% had retained ≥5kg from pre-pregnancy. Seventy-four percent were breastfeeding, and 63% had 2 or more children. Eighty-four percent were married, and 16% were living with a partner.
Table.
Characteristics of the Sample of Post-Partum Women (n=19), n (%) or M ± SD
| Age (years) | 31.5 ± 3.2 |
|
| |
| Months post-partum | 3.4 ± 2.1 |
|
| |
| Currently breastfeeding | 14 (74) |
|
| |
| Body mass index (BMI; kg/m2) at baseline | 30.1 ± 4.2 |
|
| |
| Gestational weight gain in index pregnancy (lbs) | 35.7 ± 14.1 |
|
| |
| Post-partum weight retention (lbs) at baseline | 14.2 ± 18.0 |
|
| |
| Race/ethnicity | |
| Non-Hispanic white | 14 (74) |
| Non-Hispanic black | 1 (5) |
| Hispanic/Latina | 2 (11) |
| Asian | 2 (11) |
|
| |
| Education | |
| Less than Bachelor’s | 2 (11) |
| Bachelor’s degree/some graduate school | 6 (32) |
| Graduate degree | 11 (58) |
|
| |
| Married | 16 (84) |
|
| |
| Work status | |
| Employed full-time | 10 (53) |
| Employed part-time | 2 (11) |
| Homemaker | 6 (32) |
| Student | 1 (5) |
Over 12 weeks, participants posted a median of 2 original posts (IQR: 1–3, range: 0–5) and 24 replies (IQR: 15–31, range: 6–76), and liked a median of 32 posts or comments (IQR: 16–51, range: 10–172). Engagement was sustained through the end of the intervention – 42% of participants posted, commented, or “liked” a post or comment on the last day of the intervention, 63% during the last week, and 100% in the last 4 weeks.
Participants found the intervention to be acceptable. The majority (88%) of women said they would be likely/very likely to participate again if they had another baby (41% very likely, 47% likely, 6% neutral, 6% unlikely, and none very unlikely), and 82% would be likely/very likely to recommend the program to a post-partum friend (29% very likely, 53% likely, 12% neutral, 6% unlikely, and none very unlikely).
Eighteen women lost weight; 1 woman gained weight. On average, women lost 7.7 lbs (SD: 8.1 lbs, range: 16.9 lbs gained to 20.8 lbs lost), representing 4.8% of their baseline weight (SD: 4.2%, range: 6.7% gained to 11.8% lost). Fifty-eight percent of participants lost ≥5%.
Discussion
The current study extends research on the use of Facebook to deliver behavioral interventions. Weight loss interventions that deliver at least 1 intervention component via Facebook appear promising.11,27–31 In the only study to date that focused on post-partum women, a Facebook group provided a forum for support and links to additional resources as part of a multicomponent post-partum weight loss intervention that also included daily text messages and counseling calls with an interventionist.11 In this study, women in the intervention condition lost 2.8% of their baseline weight, and a third (n=3/9) achieved 5% or greater weight loss.11 In the current study, women lost an average of 4.8%, with 58% losing 5% or greater of their baseline weight. Findings from the current study suggest that delivering weight loss programming to post-partum women entirely via a private Facebook group is feasible and acceptable, and that intervention visits may not be necessary to help post-partum women achieve clinically meaningful weight loss. A recent trial found that low-income post-partum women receiving assistance through the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) who participated in a weight loss intervention delivered via an interactive website, text messages, and monthly in-person meetings achieved greater weight loss at 12 months than women receiving WIC assistance alone.32 In that study, women saw significantly greater weight loss than the comparison condition yet attended on average only 4.4 out of 12 monthly in-person sessions,32 further supporting the feasibility of post-partum weight loss programming delivered remotely. Given implications for cost-effectiveness, this question should be explored in future research.
Delivering lifestyle interventions entirely online can overcome barriers many post-partum women face to participating in in-person programs (e.g., childcare, busy schedules).5–7 Facebook provides opportunity to embed the intervention into women’s daily lives,33 a strength of this delivery mode as behavior analytic theory has long shown that delayed consequences and feedback have diminished impact on behavior.34 The average of 50 minutes per day users spend on Facebook10 provides ample opportunity to cue women to engage in healthy behaviors offline. Facebook can connect post-partum women with other post-partum women seeking to lose weight, even across wide geography, important because moms, especially first-time moms, often seek out other moms for advice and support,9,35 and these social connections can provide support and modeling for healthy behaviors related to weight loss.36
Remote delivery via online social networks such as Facebook may also facilitate sustained engagement and retention in weight loss programs. Indeed, 1 participant moved out of state yet was able to continue participating in the intervention. The ability to deliver a lifestyle intervention and conduct assessments remotely allows interventions to reach far more post-partum women. While traditional recruitment methods were used for this pilot study, recruitment of post-partum women directly from Facebook into a Facebook-delivered lifestyle intervention could ensure participants are regular users.37 If further testing demonstrates efficacy for weight loss, this Facebook-delivered post-partum weight loss intervention could be provided remotely to women across a wide geographic area and thus this treatment model has high potential reach and impact.
In this study, women remained engaged throughout the 12 weeks of the intervention, with almost half of the sample visibly engaging on the last day of the intervention and 100% during the last 4 weeks. However, the extent of visible engagement (i.e., posts, replies, likes) was quite variable, with some women engaging minimally. How to optimally engage participants in behavioral interventions delivered via online social networks is an active area of research.23,27 Future research examining which topics or intervention posts received high or low engagement may inform the development of social media delivered behavioral interventions.
This study has limitations. The results from this single-arm pilot study do not provide insight into how much weight women would have lost in absence of intervention. However, in the current study women lost −3.5 kg on average, similar to recent trials of web-based post-partum weight loss interventions (e.g., average losses of −3.3 kg at 14 weeks,11 −3.1 kg at 6 months32), and women in the comparison conditions in these trials did not achieve meaningful weight loss (i.e., +0.5 kg,11 −1.0 kg32), supporting research to test the efficacy of this intervention. As the majority of the sample was highly educated, partnered, and non-Hispanic white, our findings may not be generalizable to less educated women, single mothers, or women of racial/ethnic minorities, and future research should include more diverse samples.
Implications for Research and Practice
Delivering evidence-based weight loss strategies via a private Facebook group has the potential for public health impact. This pilot study suggests that this approach is feasible and acceptable to post-partum women, and supports further research to assess intervention efficacy.
Acknowledgments
This study was supported by a grant from the Joseph P. Healey Endowment Fund. Additional support provided by NIH grants KL2TR000160 (MEW), U01HL105268 (MEW), R34HL136979 (MEW), UL1TR000161 (RSX), R25CA172009 (CNM), and K24HL124366 (SLP).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Gore SA, Brown DM, West DS. The role of postpartum weight retention in obesity among women: a review of the evidence. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine. 2003;26(2):149–159. doi: 10.1207/S15324796ABM2602_07. [DOI] [PubMed] [Google Scholar]
- 2.Endres LK, Straub H, McKinney C, et al. Postpartum weight retention risk factors and relationship to obesity at 1 year. Obstetrics and gynecology. 2015;125(1):144–152. doi: 10.1097/AOG.0000000000000565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gould Rothberg BE, Magriples U, Kershaw TS, Rising SS, Ickovics JR. Gestational weight gain and subsequent postpartum weight loss among young, low-income, ethnic minority women. Am J Obstet Gynecol. 2011;204(1):52.e51–11. doi: 10.1016/j.ajog.2010.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lim S, O’Reilly S, Behrens H, Skinner T, Ellis I, Dunbar JA. Effective strategies for weight loss in post-partum women: a systematic review and meta-analysis. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2015 doi: 10.1111/obr.12312. [DOI] [PubMed] [Google Scholar]
- 5.Montgomery KS, Bushee TD, Phillips JD, et al. Women’s challenges with postpartum weight loss. Maternal and child health journal. 2011;15(8):1176–1184. doi: 10.1007/s10995-010-0681-9. [DOI] [PubMed] [Google Scholar]
- 6.Carter-Edwards L, Ostbye T, Bastian LA, Yarnall KS, Krause KM, Simmons TJ. Barriers to adopting a healthy lifestyle: insight from postpartum women. BMC research notes. 2009;2:161. doi: 10.1186/1756-0500-2-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Groth SW, David T. New mothers’ views of weight and exercise. MCN The American journal of maternal child nursing. 2008;33(6):364–370. doi: 10.1097/01.NMC.0000341257.26169.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Greenwood S, Perrin A, Duggan M. Social Media Update 2016. 2016 http://www.pewinternet.org/2016/11/11/social-media-update-2016/
- 9.Duggan M, Lenhart A, Lampe C, Ellison NB. Parents and Social Media. 2015 http://www.pewinternet.org/2015/07/16/parents-and-social-media/
- 10.Owens JC. [Accessed 14 June 2016];People spend more time with Facebook than actual friends. 2016 http://www.marketwatch.com/story/people-spend-more-time-with-facebook-friends-than-with-actual-friends-2016-04-27.
- 11.Herring SJ, Cruice JF, Bennett GG, Davey A, Foster GD. Using Technology to Promote Postpartum Weight Loss in Urban, Low-Income Mothers: A Pilot Randomized Controlled Trial. Journal of nutrition education and behavior. 2014 doi: 10.1016/j.jneb.2014.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. Journal of biomedical informatics. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes care. 2002;25(12):2165–2171. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. The New England journal of medicine. 2002;346(6):393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Whittemore R. A systematic review of the translational research on the Diabetes Prevention Program. Translational behavioral medicine. 2011;1(3):480–491. doi: 10.1007/s13142-011-0062-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McTigue KM, Conroy MB, Hess R, et al. Using the internet to translate an evidence-based lifestyle intervention into practice. Telemedicine journal and e-health : the official journal of the American Telemedicine Association. 2009;15(9):851–858. doi: 10.1089/tmj.2009.0036. [DOI] [PubMed] [Google Scholar]
- 17.Rosal MC, Lemon SC, Nguyen OH, Driscoll NE, Ditaranto L. Translation of the diabetes prevention program lifestyle intervention for promoting postpartum weight loss among low-income women. Translational behavioral medicine. 2011;1(4):530–538. doi: 10.1007/s13142-011-0069-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ferrara A, Hedderson MM, Albright CL, et al. A pregnancy and postpartum lifestyle intervention in women with gestational diabetes mellitus reduces diabetes risk factors: a feasibility randomized control trial. Diabetes care. 2011;34(7):1519–1525. doi: 10.2337/dc10-2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pagoto S, Waring ME, May CN, et al. Adapting Behavioral Interventions for Social Media Delivery. Journal of medical Internet research. 2016;18(1):e24. doi: 10.2196/jmir.5086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chang M-W, Nitzke S, Guilford E, Adair CH, Hazard DL. Motivators and Barriers to Healthful Eating and Physical Activity among Low-Income Overweight and Obese Mothers. Journal of the American Dietetic Association. 2008;108(6):1023–1028. doi: 10.1016/j.jada.2008.03.004. [DOI] [PubMed] [Google Scholar]
- 21.Mailey E, Huberty J, Dinkel D, McAuley E. Physical activity barriers and facilitators among working mothers and fathers. BMC Public Health. 2014;14(1):657. doi: 10.1186/1471-2458-14-657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.United States Department of Agriculture National Agricultural L. Interactive DRI [Dietary Reference Intake] for Healthcare Professionals. 2012 [Google Scholar]
- 23.Hales S, Davidson C, Turner-McGrievy G. Varying social media post types differentially impacts engagement in a behavioral weight loss intervention. Translational behavioral medicine. 2014;4(4):355–362. doi: 10.1007/s13142-014-0274-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eysenbach G. The law of attrition. Journal of medical Internet research. 2005;7(1):e11. doi: 10.2196/jmir.7.1.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Herring SJ, Rich-Edwards JW, Oken E, Rifas-Shiman SL, Kleinman KP, Gillman MW. Association of postpartum depression with weight retention 1 year after childbirth. Obesity. 2008;16(6):1296–1301. doi: 10.1038/oby.2008.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wing RR, Lang W, Wadden TA, et al. Benefits of modest weight loss in improving cardiovascular risk factors in overweight and obese individuals with type 2 diabetes. Diabetes care. 2011;34(7):1481–1486. doi: 10.2337/dc10-2415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Merchant G, Weibel N, Patrick K, et al. Click “like” to change your behavior: a mixed methods study of college students’ exposure to and engagement with facebook content designed for weight loss. Journal of medical Internet research. 2014;16(6):e158. doi: 10.2196/jmir.3267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Napolitano MA, Hayes S, Bennett GG, Ives AK, Foster GD. Using Facebook and text messaging to deliver a weight loss program to college students. Obesity. 2013;21(1):25–31. doi: 10.1002/oby.20232. [DOI] [PubMed] [Google Scholar]
- 29.Willis EA, Szabo-Reed AN, Ptomey LT, et al. Distance learning strategies for weight management utilizing social media: A comparison of phone conference call versus social media platform. Rationale and design for a randomized study. Contemporary clinical trials. 2016;47:282–288. doi: 10.1016/j.cct.2016.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Godino JG, Merchant G, Norman GJ, et al. Using social and mobile tools for weight loss in overweight and obese young adults (Project SMART): a 2 year, parallel-group, randomised, controlled trial. Lancet Diabetes Endocrinol. 2016;4(9):747–755. doi: 10.1016/S2213-8587(16)30105-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pagoto S, Waring M, Olendzki E, Oleski J, May C, Evans M. The feasibility of incentivizing participation in an online social network weight loss program. Proceedings of the 50th Hawaii International Conference on System Sciences [peer-reviewed manuscript]; 2017. [Google Scholar]
- 32.Phelan S, Hagobian T, Brannen A, et al. Effect of an Internet-Based Program on Weight Loss for Low-Income Postpartum Women: A Randomized Clinical Trial. Jama. 2017;317(23):2381–2391. doi: 10.1001/jama.2017.7119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hartman MA, Hosper K, Stronks K. Targeting physical activity and nutrition interventions towards mothers with young children: a review on components that contribute to attendance and effectiveness. Public health nutrition. 2011;14(8):1364–1381. doi: 10.1017/S1368980010001941. [DOI] [PubMed] [Google Scholar]
- 34.Fisher W, Piazza C, Roane H. Handbook of Applied Behavior Analysis. New York, NY: Guildford Press; 2011. [Google Scholar]
- 35.Holtz B, Smock A, Reyes-Gastelum D. Connected Motherhood: Social Support for Moms and Moms-to-Be on Facebook. Telemedicine journal and e-health : the official journal of the American Telemedicine Association. 2015;21(5):415–421. doi: 10.1089/tmj.2014.0118. [DOI] [PubMed] [Google Scholar]
- 36.Motteli S, Siegrist M, Keller C. Women’s social eating environment and its associations with dietary behavior and weight management. Appetite. 2017;110:86–93. doi: 10.1016/j.appet.2016.12.014. [DOI] [PubMed] [Google Scholar]
- 37.Lohse B. Facebook is an effective strategy to recruit low-income women to online nutrition education. Journal of nutrition education and behavior. 2013;45(1):69–76. doi: 10.1016/j.jneb.2012.06.006. [DOI] [PubMed] [Google Scholar]