Abstract
Rehabilitation of the burn patient aims to restore strength, coordination and mobility as closely to normal as possible and should begin immediately after initial admission. In the acute phase, baseline assessments are made against which all subsequent rehabilitation success is held. Splinting of joints at risk of developing scar contracture into favorable position is done aggressively and persistently as correction of contractures is more difficult than prevention. Exercise to preserve range of motion consists of passive but complete motion. In the intermediate phase, active full ROM movement and ambulation of steadily increasing distances, as well as resistive exercise and stretching aid in the prevention of muscle and bone atrophy and preserve muscle memory and coordination. In the long-term outpatient rehabilitation phase, individualized patient-centered exercise programs can be advantageous in achieving measurable and lasting positive rehabilitation outcomes. A defined combination of aerobic and resistive exercise is helpful to enable a physical transition towards independent living and performance of activities of daily life, as well as return to work as soon as possible. Rehabilitation is a continuum of equally essential steps, which extends over the whole course of inpatient and outpatient treatment of the burn patient.
Keywords: Rehabilitation, range of motion, splinting, aerobic and resistive exercise
Introduction
Medical and technical advancements over the last decades have greatly improved survival of acute thermal injury (1,2). With an increasing percentage of patients surviving severe and even massive burns, a paradigm shift is underway to accommodate for the specific acute, mid- and long-term medical needs of an increasing number patients who simply did not exist in the past.
Rehabilitation of the thermally injured patient is defined as the part of specialized healthcare that focuses primarily on regaining and improving strength, cognition and mobility following the injury. The overarching goal in doing so is to approach the degree of pre-injury abilities as closely as possible.
The challenges in the rehabilitation of burn patients are on one hand similar to those in other critically ill patients and on the other hand unique in regard to burn injury and its sequelae. Generally, prolonged immobility during intensive care, resulting in muscle and bone wasting (3,4), loss of strength and coordination (4), as well as complications arising from secondary infection are common problems in all critically ill patients (5–7). Specifically in patients with severe burn injury, factors such as periodically recurring operations (8,9), delayed closure and secondary infection of dermal wounds (10,11), pulmonary dysfunction resulting from inhalation injury (12), and the need for specific positioning of the patient in order to protect skin-grafted areas or donor sites represent serious challenges to early rehabilitation(13). Later in the course of hospitalization and outpatient treatment, challenges arise mostly from the formation of scar contractures over joints (14), cardiopulmonary dysfunction (15), the long term consequences of major amputations (16) and psychosocial successions of a burn (17).
In any case, the rehabilitation efforts necessary to reach the full potential of recovery correlate with the extent of burn injury, the age of the patient, the presence of concomitant injury or comorbidities and the individual capacity of the patient to perform the necessary tasks.
The main goals of burn related rehabilitation are to maximize functional and cosmetic outcomes. Important short term objectives focus on the preservation and improvement of range of motion (ROM) and functional ability. The most important long term target is to facilitate return to independent living and working and to compensate functional losses. An accepted approach towards the conceptualization of burn rehabilitation is the subdivision into its phases and their specific priorities.
Acute Rehabilitation Phase
Despite the vast challenges associated with it, there exists a broad consensus among experts that burn rehabilitation must start as early as possible (16,18–20). The acute phase of rehabilitation ranges from the patient’s admittance to the burn unit, over the days of early excision and skin grafting to the beginning of wound healing.
Baseline assessment
The first step in rehabilitation should be an initial assessment of the patient’s status that includes general information regarding the mechanism and extent of the sustained injury, as well as details that directly impact rehabilitation such as exposed tendons, the presence of concomitant fractures and inhalation injury. Next, baseline measurements of range of motion (ROM), muscle strength, sensation and a history and assessment of the ability to perform activities of daily life before and immediately after the injury are recorded and serve as reference for future rehabilitation improvement and success. Next, patient-centered short and long term rehabilitation goals are defined during the onset of early acute care.
Positioning and Splinting
The objectives of effective patient positioning and splinting are to minimize contractures and joint deformities, optimize joint alignment, maintain ROM and tissue elongation, facilitate remodeling of adhesions, prevent pressure points and sores, protect operated sites (skin grafts and flaps), assist weakened muscles, and reduce edema through elevation (13).
The therapeutic armamentarium ranges from splints, special mattresses and cut-out-foam, serial casting and strapping (21–23) to the surgical placement of pins (24) to maintain certain joint positions.
Special splints can be used to optimally position and prevent early contracture of the mouth (25–28), ear (29,30), nostrils, neck (31), shoulder and axilla (31,32)(Figure 1), elbow (33)(Figure 2), hip (31,32,34), knee, ankle and foot. The ankle equinus deformity is developing earliest, is most resilient to treatment and should be avoided whenever possible through proactive fixation of the joint as shown in Figure 3 (Multi Podus Splint TBC 47.7).
Figure 1.

Bilateral axillary splints to prevent formation of acute contracture.
Figure 2.
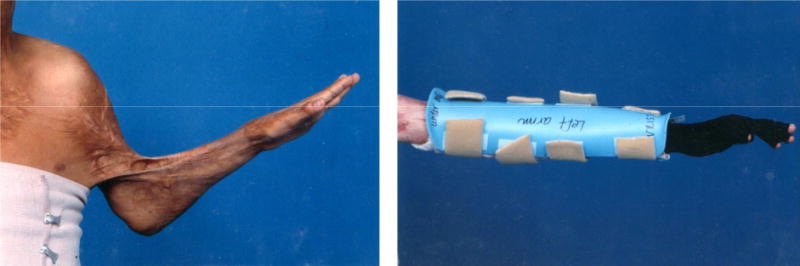
Severe elbow contracture and correct splinting of the elbow.
Figure 3.

Multipodus foot and ankle splint to prevent contracture. From Serghiou, MA, Ott S, Whitehead C, Cowan A, McEntire S, and Suman, OE (2012) Comprehensive rehabilitation of the burn patient, In Total Burn Care (Herndon, D. N., Ed.) 4th ed., pp 517–549, Elsevier, Philadelphia, PA, with permission.
The wrist and hand are especially prone to early contracture and should be splinted into 0–30° extension within the first 24–72 hours to prevent claw hand. The authors recommend MCP joints be splinted in 70–80° flexion and IP joints to full extension (13). The thumb is splinted in a combination of palmar and radial abduction and the MCP IP joints slightly flexed (13)(Figure 4).
Figure 4.

Severe wrist and hand contracture and correct splint placement for prevention
Patient positioning protocols that regulate frequent and defined position changes during extended periods of immobilization should be installed in every burn unit to prevent pressure points and ulcers. The supine patient position is preferred unless otherwise necessary.
Therapeutic exercise
Early physical therpay preserves joint mobility, promotes edema resolution, and prevents muscle atrophy, disuse osteoporosis, as well as respiratory and cardiac complications (13), while reducing functionally impairing scar contractures (19,35).
Exercise must be started immediately in any conservative and most operative patient management regimens (18). Procedures such as debridement and fasciotomy, or the placement of heterografts or synthetic dressing materials are not contraindications for exercise (32). The placement of skin grafts over joints may warrant a discontinuation of physical therpay in the particular area for 4–5 days but may otherwise not halt exercise efforts.
During the early phase of exercise, short duration and high frequency are favorable and complete active ROM exercise– preferably performed independently by the patient – is best (13). The patient moves major joints according to their full ROM to maintain mobility. If the patient is critically ill, intubated, medicated or otherwise unable to move fully and actively, assisted active ROM exercises are the treatment of choice followed by passive complete ROM if no active movement is possible (36).
Resistive exercise prevents muscle and bone atrophy, increases strength and proprioception and coordination (37). During the early phase, isometric exercise with or without gentle manual resistance during bed rest has been shown to conserve muscle memory(38).
Ambulation should be initiated as soon as the burn patient is medically stable to do so (37,39). Walking provides mild cardiovascular conditioning, prevents pressure sores, preserves muscle strength and function and increases appetite (13,40). A systematic analysis by Smith et al. demonstrated lower incidence of pulmonary embolism and deep vein thrombosis, as well as shorter duration of hospitalization when patients with lower extremity skin grafts ambulated immediately after surgery (39). The Unna Boot, an impregnated semi-rigid bandage, can be used in combination with lower extremity skin grafting and facilitate earlier ambulation and can be left in place for up to 7 days after grafting (41).
Intermediate Phase of Rehabilitation
The second phase of rehabilitation is entered when the patient ceases to be in critical condition and extends from the initial healing of debrided and grafted skin wounds to complete wound closure.
Objectives of this phase are to stretch the healing skin to maintain major joint ROM, preserve motor skill coordination, promote functional independence, maintain strength and endurance and further minimize muscle and bone atrophy.
Therapeutic exercise
In the intermediate phase and in favor of exercise, the patient is more alert, physically and medically improving, undergoes surgery with diminishing frequency, and is subject to fewer critical problems which could interfere with active rehabilitation.
In this phase, passive complete ROM should be used mainly to compare to active complete ROM which is the main driver of rehabilitative success. Strengthening utilizes manual resistance or light weights and particular efforts should be undertaken to target muscle groups which oppose common patterns of contracture (13,20).
Sustained stretching with low force and long duration can aid in prevention or reversal of contractures (37). The effect is based on the principles of physical conditioning and results in plastic elongation of connective tissue.
Encouragement to ambulate continues to be crucial and aims for daily increases in distance and the continuous reduction of assistance. While the patient is walking independently repeated gait assessment is performed to detect contractures of the hip and lower extremities early (13).
Long Term Rehabilitation
Therapeutic exercise and occupational therapy
After completion of wound healing or discharge from acute hospitalization into the outpatient setting, the burn patient is subject to long-term rehabilitation.
The main goals of this phase are to combine personal trainer based outpatient exercise with a high compliance to continuous, therapist-independent, exercising. If persistent in this phase, therapy should prioritize ameliorating ROM limitations, as even strengthened and conditioned muscle has not been found capable of generating sufficient force to elongate scar tissue and contractures on its own (36).
Ambulation is further encouraged to occur independently at community distances. Gait deformities can be refined to increase efficiency and decrease pain and long term sequelae of scar contractures.
A recent systematic review demonstrated that over 70 percent of burn survivors return to work within 3.3 years after their injury, but at the same time nearly 28% of all patients never find their way back into employment of any form(42). In order to better this discrepancy, which can be life altering for burn survivors, return to work and specialized occupational therapy should be a cornerstone of long-term rehabilitation. However recent literature indicates that there is little consensus and great need for standardization of these efforts(42,43).
Principles of developing outpatient exercise programs
In accordance with the continuum of care from inpatient to outpatient care, some basic concepts specific to exercise training and rehabilitation exist. These concepts pertain to whole body exercise and apply to progressive resistance exercise or aerobic exercise. Exercise programs should consider the frequency of exercise; the intensity of the exercise; the mode or equipment used and the duration of such exercises. We and others have published on the benefits of various exercise programs evaluated, but any program should accommodate individual patient characteristics and needs (44–46).
To develop realistic and achievable goals of outpatient exercise programs pre-burn activity and habits, medical problems and limitations, such as pain or weakness during ambulation or exercise, itching, ROM limitations, chronic medications and their potential side effects need to be reassessed after hospital discharge. Objective assessments to quantify baseline status and hold all future improvements due to exercise against include ECG with resting and peak heart rate and blood pressure, cardiopulmonary function tests such as resting and peak oxygen consumption, Borg’s rated perceived exertion, lean body mass assessed by dual-energy x-ray absorptiometry and isokinetic dynamometry (47–51). Contraindications to certain types of exercise are regularly updated by the American College of Sport Medicine (ACSM,(52)) and should be considered when designing individualized exercise programs. The main components of an exercise program consist of the specific prescription of aerobic and strength activities, as well as recreational activities. Optimal effects are achieved with aerobic exercised performed 3–5 days per week, and resistive strength activities on 2–3 days per week(53). Strengthening exercise continues the use of free weights while aerobic exercise relies on treadmill, elliptical, rower or cycle ergometers according to the patient’s individual needs. Table 1 illustrates an exemplary exercise program design as used at our institution. It is encouraged to base all progression of patient exercise on continuously collected data that is compared to baseline to achieve quantifiable and objective results. Patient and caregiver education about the program and its aims is mandatory for sustainable success regarding adherence and compliance (13). New, unpublished data of our group suggest that these exercise programs can be carried out in hospital based locations or in community based gyms. However, home exercise can also be successfully carried out.
Table 1.
Example of long term rehabilitative exercise program at Shriners Hospital for Children, Galveston.
| Aerobic workout | |
|---|---|
| • Intensity • Duration • Frequency • Mode |
70–85% of each individual’s previously determined individual peak aerobic capacity. Heart rate and rated perceived exertion is obtained at regular intervals during aerobic exercise 20–40 min 3–5 days per week Aerobic exercise on treadmills, cycle ergometers, arm ergometers, rowing machines, and outdoor activities such as soccer or kickball |
|
| |
| Resistance workout | |
| • Exercise type • Amount of load lifted and number of repetitions • Frequency • Exercise order • Type of exercises • Rest period |
Upper and lower body of core and assistance exercises The weight or load-lifted is set at approximately 50–60% of each individual’s 3 repetition maximum (RM) and lifted for 4–10 repetitions for three sets. During the 2nd week, the lifting load increases to 70–75% (3 sets, 4–10 repetitions) of individual 3RM and continues for weeks 2–6. Thereafter, training intensity is increased to 80–85% (3 sets, 8–12 repetitions) of the 3RM and implemented from weeks 7–12 2–3 days per week; alternating days of work with days of recovery Bench press, leg press or squats, shoulder press, biceps curl, leg curl, triceps curl, toe raises, and abdominals Eight basic resistance exercises done using variable-resistance machines or free weights: 4 for upper body, 3 for lower body, and abdominals 1 minute between sets |
Conclusion
Rehabilitation activities in the in- and outpatient setting differ based on the patient’s ability to complete certain tasks at varying stages of their reconvalescence. No phase of burn rehabilitation is more important than the other. Only if rehabilitation efforts go hand in hand along a continuum from admission to the burn unit to successful completion of long term rehabilitation goals can maximum outcomes be achieved.
Key points.
Rehabilitation of the burn patient aims to restore strength, coordination and mobility.
Occupational and physical therapy should begin immediately after admission.
A defined combination of aerobic and resistive exercise is helpful to enable a physical transition towards independent living and performance of activities of daily life, as well as return to work.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Gabriel Hundeshagen, Research Fellow, Department of Surgery, University of Texas Medical Branch and Shriners Hospital for Children, Galveston, 815 Market St 77550 Galveston, TX, gahundes@utmb.edu.
Oscar E Suman, Leon Hess Professor for Burn Injuries Research Professor; Director of Children’s Wellness Center, Associate Director of Research; Co-director of the Burn Center Research Management Office, Shriners Hospitals for Children, 815 Market St 77550 Galveston, TX, oesuman@utmb.edu.
Ludwik K Branski, Assistant Professor, Department of Surgery, University of Texas Medical Branch and Shriners Hospital for Children, Galveston, 815 Market St 77550 Galveston, TX.
References
- 1.Pereira CT, Barrow RE, Sterns AM, Hawkins HK, Kimbrough CW, Jeschke MG, et al. Age-dependent differences in survival after severe burns: a unicentric review of 1,674 patients and 179 autopsies over 15 years. J Am Coll Surg. 2006;202(3):536–548. doi: 10.1016/j.jamcollsurg.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 2.Jeschke MG, Chinkes DL, Finnerty CC, Kulp G, Suman OE, Norbury WB, et al. Pathophysiologic response to severe burn injury. Ann Surg. 2008 Sep;248(3):387–401. doi: 10.1097/SLA.0b013e3181856241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jeschke MG, Barrow RE, Mlcak RP, Herndon DN. Endogenous anabolic hormones and hypermetabolism: effect of trauma and gender differences. Ann Surg. 2005;241(5):759–768. doi: 10.1097/01.sla.0000161028.43338.cd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Mousawi AM, Williams FN, Mlcak RP, Jeschke MG, Herndon DN, Suman OE. Effects of exercise training on resting energy expenditure and lean mass during pediatric burn rehabilitation. J Burn Care Res Off Publ Am Burn Assoc. 2010 doi: 10.1097/BCR.0b013e3181db5317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Girou E, Schortgen F, Delclaux C, Brun-Buisson C, Blot F, Lefort Y, et al. Association of noninvasive ventilation with nosocomial infections and survival in critically ill patients. Jama. 2000;284(18):2361–2367. doi: 10.1001/jama.284.18.2361. [DOI] [PubMed] [Google Scholar]
- 6.Valles J, Rello J, Ochagavia A, Garnacho J, Alcalá MA. Community-acquired bloodstream infection in critically ill adult patients: impact of shock and inappropriate antibiotic therapy on survival. CHEST J. 2003;123(5):1615–1624. doi: 10.1378/chest.123.5.1615. [DOI] [PubMed] [Google Scholar]
- 7.Weber JM, Sheridan RL, Pasternack MS, Tompkins RG. Nosocomial infections in pediatric patients with burns. Am J Infect Control. 1997;25(3):195–201. doi: 10.1016/s0196-6553(97)90004-3. [DOI] [PubMed] [Google Scholar]
- 8.Herndon DN, Gore D, Cole M, Desai MH, Linares H, Abston S, et al. Determinants of mortality in pediatric patients with greater than 70% full-thickness total body surface area thermal injury treated by early total excision and grafting. J Trauma Acute Care Surg. 1987;27(2):208–212. doi: 10.1097/00005373-198702000-00020. [DOI] [PubMed] [Google Scholar]
- 9.Herndon DN, Barrow RE, Rutan RL, Rutan TC, Desai MH, Abston S. A comparison of conservative versus early excision. Therapies in severely burned patients. Ann Surg. 1989;209(5):547. doi: 10.1097/00000658-198905000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Church D, Elsayed S, Reid O, Winston B, Lindsay R. Burn Wound Infections. Clin Microbiol Rev. 2006 Apr;19(2):403–34. doi: 10.1128/CMR.19.2.403-434.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Singer AJ, Clark RAF. Cutaneous Wound Healing. N Engl J Med. 1999 Sep;341(10):2. 738–46. doi: 10.1056/NEJM199909023411006. [DOI] [PubMed] [Google Scholar]
- 12.Mlcak RP, Suman OE, Herndon DN. Respiratory management of inhalation injury. burns. 2007;33(1):2–13. doi: 10.1016/j.burns.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 13.Serghiou MA, Ott S, Whitehead C, Cowan A, McEntire S, Suman OE. Comprehensive rehabilitation of the burn patient. In: Herndon DN, editor. Total Burn Care. 4th. Elsevier; Philadelphia, PA: 2012. pp. 517–549. [Google Scholar]
- 14.Finnerty CC, Jeschke MG, Branski LK, Barret JP, Dziewulski P, Herndon DN. Hypertrophic scarring: the greatest unmet challenge after burn injury. The Lancet. 2016;388(10052):1427–1436. doi: 10.1016/S0140-6736(16)31406-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Duke JM, Randall SM, Fear MW, Boyd JH, Rea S, Wood FM. Long-term Effects of Pediatric Burns on the Circulatory System. Pediatrics. 2015;136(5):e1323–e1330. doi: 10.1542/peds.2015-1945. [DOI] [PubMed] [Google Scholar]
- 16.Ward RS, Hayes-Lundy C, Schnebly WA, Reddy R, Saffle JR. Rehabilitation of burn patients with concomitant limb amputation: case reports. Burns. 1990;16(5):390–392. doi: 10.1016/0305-4179(90)90015-o. [DOI] [PubMed] [Google Scholar]
- 17.Blakeney P, Herndon DN, Desai MH, Beard S, Wales-Scale P. Long-term psychosocial adjustment following burn injury. J Burn Care Res. 1988;9(6):661–665. doi: 10.1097/00004630-198811000-00022. [DOI] [PubMed] [Google Scholar]
- 18.Edgar D, Brereton M. Rehabilitation after burn injury. BMJ. 2004 Aug 7;329(7461):343–5. doi: 10.1136/bmj.329.7461.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Richard RL, Hedman TL, Quick CD, Barillo DJ, Cancio LC, Renz EM, et al. A clarion to recommit and reaffirm burn rehabilitation. J Burn Care Res. 2008;29(3):425–432. doi: 10.1097/BCR.0b013e318171081d. [DOI] [PubMed] [Google Scholar]
- 20.Serghiou M, Cowan A, Whitehead C. Rehabilitation after a burn injury. Clin Plast Surg. 2009;36(4):675–686. doi: 10.1016/j.cps.2009.05.008. [DOI] [PubMed] [Google Scholar]
- 21.Bennett GB, Helm P, Purdue GF, Hunt JL. Serial casting: a method for treating burn contractures. J Burn Care Res. 1989;10(6):543–545. [PubMed] [Google Scholar]
- 22.Ricks NR, Meagher DP., Jr The benefits of plaster casting for lower-extremity burns after grafting in children. J Burn Care Res. 1992;13(4):465–468. doi: 10.1097/00004630-199207000-00015. [DOI] [PubMed] [Google Scholar]
- 23.Johnson J, Silverberg R. Serial casting of the lower extremity to correct contractures during the acute phase of burn care. Phys Ther. 1995;75(4):262–266. doi: 10.1093/ptj/75.4.262. [DOI] [PubMed] [Google Scholar]
- 24.Fess EE, Philips CA. Hand splinting: principles and methods. Mosby Incorporated. 1987 [Google Scholar]
- 25.Ridgway CL, Warden GD. Evaluation of a vertical mouth stretching orthosis: two case reports. J Burn Care Res. 1995;16(1):74–78. doi: 10.1097/00004630-199501000-00014. [DOI] [PubMed] [Google Scholar]
- 26.Taylor LB, Walker J. A review of selected microstomia prevention appliances. Pediatr Dent. 1997;19:413–418. [PubMed] [Google Scholar]
- 27.Heinle JA, Kealey GP, Cram AE, Hartford CE. The microstomia prevention appliance: 14 years of clinical experience. J Burn Care Rehabil. 1987;9(1):90–91. doi: 10.1097/00004630-198801000-00023. [DOI] [PubMed] [Google Scholar]
- 28.Sykes L. Scar traction appliance for a patient with microstomia: A clinical report. J Prosthet Dent. 1996;76(5):464–465. doi: 10.1016/s0022-3913(96)90001-3. [DOI] [PubMed] [Google Scholar]
- 29.Harries CA, Pegg SP. Foam ear protectors for burnt ears. J Burn Care Rehabil. 1988;10(2):183–184. doi: 10.1097/00004630-198903000-00018. [DOI] [PubMed] [Google Scholar]
- 30.Manigandan C, Dhanaraj P. An innovative, cost-effective, pressure-relieving device for burned ears. Burns. 2004;30(3):269–271. doi: 10.1016/j.burns.2003.10.019. [DOI] [PubMed] [Google Scholar]
- 31.Leman CJ. Splints and accessories following burn reconstruction. Clin Plast Surg. 1992;19(3):721–731. [PubMed] [Google Scholar]
- 32.Malick MH, Carr JA. Manual on Management of the Burn Patient: Including Splinting, Mold and Pressure Techniques for Physicians, Occupational Therapists, Physical Therapists, Orthotists. Harmarville Rehabilitation Center, Educational Resource Division; 1982. [Google Scholar]
- 33.Richard RL. Use of the Dynasplint to correct elbow flexion burn contracture: a case report. J Burn Care Rehabil. 1985;7(2):151–152. [PubMed] [Google Scholar]
- 34.Walters BB. Splinting the burn patient. RAMSCO Publishing Company; 1987. [Google Scholar]
- 35.Okhovatian F, Zoubine N. A comparison between two burn rehabilitation protocols. Burns. 2007;33(4):429–434. doi: 10.1016/j.burns.2006.08.009. [DOI] [PubMed] [Google Scholar]
- 36.Richard R, Staley M. Burn care and rehabilitation: principles and practice. Vol. 12. FA Davis Company; 1994. [Google Scholar]
- 37.Wright PC. Fundamentals of acute burn care and physical therapy management. Phys Ther. 1984;64(8):1217–1231. doi: 10.1093/ptj/64.8.1217. [DOI] [PubMed] [Google Scholar]
- 38.Cronan T, Hammond J, Ward CG. The value of isokinetic exercise and testing in burn rehabilitation and determination of back-to-work status. J Burn Care Res. 1990;11(3):224–227. doi: 10.1097/00004630-199005000-00008. [DOI] [PubMed] [Google Scholar]
- 39.Smith TO. When should patients begin ambulating following lower limb split skin graft surgery? A systematic review. Physiotherapy. 2006;92(3):135–145. [Google Scholar]
- 40.Robson MC, Smith DJ, Jr, VanderZee AJ, Roberts L. Making the burned hand functional. Clin Plast Surg. 1992;19(3):663–671. [PubMed] [Google Scholar]
- 41.Harnar T, Engrav LH, Marvin J, Heimbach D, Cain V, Johnson C. Dr. Paul Unna’s boot and early ambulation after skin grafting the leg: a survey of burn centers and a report of 20 cases. Plast Reconstr Surg. 1982;69(2):359–360. doi: 10.1097/00006534-198202000-00034. [DOI] [PubMed] [Google Scholar]
- 42.Mason ST, Esselman P, Fraser R, Schomer K, Truitt A, Johnson K. Return to work after burn injury: a systematic review. J Burn Care Res Off Publ Am Burn Assoc. 2012 Feb;33(1):101–9. doi: 10.1097/BCR.0b013e3182374439. [DOI] [PubMed] [Google Scholar]
- 43.Simons M, King S, Edgar D. Occupational therapy and physiotherapy for the patient with burns: principles and management guidelines. J Burn Care Res. 2003;24(5):323–335. doi: 10.1097/01.BCR.0000086068.14402.C6. [DOI] [PubMed] [Google Scholar]
- 44.Suman OE, Herndon DN. Effects of cessation of a structured and supervised exercise conditioning program on lean mass and muscle strength in severely burned children. Arch Phys Med Rehabil. 2007;88(12):S24–S29. doi: 10.1016/j.apmr.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 45.Baldwin J, Li F. Exercise behaviors after burn injury. J Burn Care Res. 2013;34(5):529–536. doi: 10.1097/BCR.0b013e31827a2bcd. [DOI] [PubMed] [Google Scholar]
- 46.Suman OE, Spies RJ, Celis MM, Mlcak RP, Herndon DN. Effects of a 12-wk resistance exercise program on skeletal muscle strength in children with burn injuries. J Appl Physiol. 2001;91(3):1168–1175. doi: 10.1152/jappl.2001.91.3.1168. [DOI] [PubMed] [Google Scholar]
- 47.Myers J, Buchanan N, Walsh D, Kraemer M, McAuley P, Hamilton-Wessler M, et al. Comparison of the ramp versus standard exercise protocols. J Am Coll Cardiol. 1991;17(6):1334–1342. doi: 10.1016/s0735-1097(10)80144-5. [DOI] [PubMed] [Google Scholar]
- 48.Myers J, Bellin D. Ramp exercise protocols for clinical and cardiopulmonary exercise testing. Sports Med. 2000;30(1):23–29. doi: 10.2165/00007256-200030010-00003. [DOI] [PubMed] [Google Scholar]
- 49.Borg G, Hassmén P, Lagerström M. Perceived exertion related to heart rate and blood lactate during arm and leg exercise. Eur J Appl Physiol. 1987;56(6):679–685. doi: 10.1007/BF00424810. [DOI] [PubMed] [Google Scholar]
- 50.Noble BJ, Borg GA, Jacobs IRA, Ceci R, Kaiser P. A category-ratio perceived exertion scale: relationship to blood and muscle lactates and heart rate. Med Sci Sports Exerc. 1982;15(6):523–528. [PubMed] [Google Scholar]
- 51.Cucuzzo NA, Ferrando A, Herndon DN. The effects of exercise programming vs traditional outpatient therapy in the rehabilitation of severely burned children. J Burn Care Res. 2001;22(3):214–220. doi: 10.1097/00004630-200105000-00006. [DOI] [PubMed] [Google Scholar]
- 52.ACSM. Guidelines [Internet] [cited 2016 Dec 14]. Available from: http://www.acsm.org/public-information/acsm-journals/guidelines.
- 53.Pollock ML, Gaesser GA, Butcher JD, Després J-P, Dishman RK, Franklin BA, et al. ACSM position stand: the recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc. 1998;30(6):975–991. doi: 10.1097/00005768-199806000-00032. [DOI] [PubMed] [Google Scholar]


