Abstract
Background
Neurocritical care provides multidisciplinary, specialized care to critically ill neurological patients, yet an understanding of the proportion of the population able to rapidly access specialized Neurocritical Care Units (NCUs) in the United States is currently unknown. We sought to quantify geographic access to NCUs by state, division, region, and for the US as a whole. In addition, we examined how mode of transportation (ground or air ambulance), and prehospital transport times affected population access to NCUs.
Methods
Data were obtained from the Neurocritical Care Society (NCS), US Census Bureau and the Atlas and Database of Air Medical Services. Empirically derived prehospital time intervals and validated models estimating prehospital ground and air travel times were used to calculate total prehospital times. A discrete total prehospital time interval was calculated for each small unit of geographic analysis (block group) and block group populations were summed to determine the proportion of Americans able to reach a NCU within discrete time intervals (45, 60, 75, and 90 min). Results are presented for different geographies and for different modes of prehospital transport (ground or air ambulance).
Results
There are 73 NCUs in the US using ground transportation alone, 12.8, 20.5, 27.4, and 32.6% of the US population are within 45, 60, 75, and 90 min of an NCU, respectively. Use of air ambulances increases access to 36.8, 50.4, 60, and 67.3 within 45, 60, 75, and 90 min, respectively. The Northeast has the highest access rates in the US using ground ambulances and for 45, 60, and 75 min transport times with the addition of air ambulances. At 90 min, the West has the highest access rate. The Southern region has the lowest ground and air access to NCUs access rates for all transport times.
Conclusions
Using NCUs registered with the NCS, current geographic access to NCUs is limited in the US, and geographic disparities in access to care exist. While additional NCUs may exist beyond those identified by the NCS database, we identify geographies with limited access to NCUs and offer a population-based planning perspective on the further development of the US neurocritical care system.
Keywords: Access to health care, Air ambulances, Delivery of health care, Emergency medical services, Intensive care units, Nervous system diseases
Introduction
Traumatic brain injury, stroke, and subarachnoid hemorrhage comprise just a few of the diseases treated in Neurocritical Care Units (NCUs) that care for critically ill neurological patients. Although, national data does not exist on the use of NCUs by patients with each of these conditions, these diseases account for more than 180,000 deaths annually in the US [1, 2]. While neurocritical care is a young specialty, formally recognized as a medical specialty in 2005 [3], treatment in multidisciplinary NCUs has been shown to reduce length of stay and resource utilization, decrease costs, and improve outcomes for patients with intracerebral hemorrhage, acute ischemic stroke (AIS), subarachnoid hemorrhage, and trauma [4–8].
In addition to improved outcomes for critically ill neurological patients, recent data also suggest that delayed access to NCUs may harm patient outcomes [9, 10]. Given the benefits of NCU care, and the need for timely access to care, adequate access of the US population to NCUs is warranted. The current distribution of NCUs throughout the United States is unknown and units have emerged without a developed plan or strategic framework. A population-based planning approach has been used in healthcare to identify accessibility of resources and to create strategic plans to deliver care more efficiently [11]. This approach has been used to more efficiently develop systems of care for other unplanned critical illnesses requiring rapid access to facilities with specialized resources including trauma care, stroke care, burn care, and critical care services [12–17].
As a nascent specialty with a tremendous growth opportunity and with an important tie to many other conditions utilizing population-based planning, this approach can help neurocritical care develop in a manner that maximizes timely access to care and synergy with other developing integrated networks of care for time sensitive conditions. As an initial step toward this goal, we sought to analyze access to NCUs throughout the United States on state, regional, divisional, and national levels to quantify where access to NCUs in the US currently exists.
Materials and Methods
Data Sources
Population Data
Data from the US Census Bureau and US Postal Service (Claritas Incorp., Ithaca, NY) were used to assemble population data [18, 19]. We utilized the smallest unit of analysis that provides demographic characteristics (block groups) as our primary geographic unit of analysis. For 2009, 208,667 US block groups were identified with population estimates and population-weighted centroids. Each block group contains between 600 and 3,000 people and does not cross state or county borders. Population-weighted centroids were assigned to each block group based upon the geographic distribution of residents so that a single point in space could be used to generate access calculations.
Neurocritical Care Units
NCUs were identified from publicly released data from the Neurocritical Care Society (NCS) [20]. Sites independently reported their designation as a NCU but no formal verification or accrediting agency was involved in their listing. To be included in this study, every site registered with the NCS was independently reviewed to determine whether the site was a NCU. We defined a NCU as a location that cared for both medical and surgical patients who were critically ill with neurological illness in a dedicated intensive care unit. Publicly available information through the internet was reviewed and if a designation was ambiguous, center directors were contacted either by phone or through email. Units that did not provide both medical and surgical care were excluded.
Air Ambulances
Data for air ambulance base station locations and capabilities were obtained from the 2009 Atlas and Database of Air Medical Services [21]. These data include location, type, and air speed of rotary aircraft housed at the base station that respond to emergency calls in the US. Fixedwing aircraft were excluded from calculations.
Access Calculations
Access to NCUs was determined by summing the population that could reach a NCU within four fixed prehospital care times (45, 60, 75, and 90 min) selected a priori because they had been used in previous medical facility access calculations and because they were clinically meaningful [12, 13, 15, 17]. To do this, we calculated the straight line distance from each block group centroid to the closest NCU, converted this distance to drivable distance, and applied empirically derived prehospital time intervals and drive speeds. All drive times assume that prehospital providers may not cross state lines to arrive the closest NCU. Exploratory analyses were done to examine how permitting the crossing of state lines would impact access to care.
In the first step of this process, block groups were uniquely linked to the nearest NCU and not counted twice. Straight line distances were calculated using the longitude and latitude for block group centroids and NCUs. These straight line distances were then converted into drivable distances using established mathematical conversions specific to the average population density of the originating and the destination block group [22, 23]. Next, population density specific and empirically derived prehospital drive speeds of 20.1, 47.5, and 56.4 mph for urban, suburban, and rural populations, respectively, were used to calculated ambulance transport intervals (Fig. 1) [16]. As this calculated time only represented the driving time from patient to hospital, we multiplied by an empirically derived coefficient describing the relation between the response interval (from dispatch to scene arrival) and the transport interval (1.6, 1.5, and 1.4 min for urban, suburban, and rural areas, respectively). All programing code was written in Visual C++ (Microsoft Corporation, Redmond, WA).
Fig. 1.
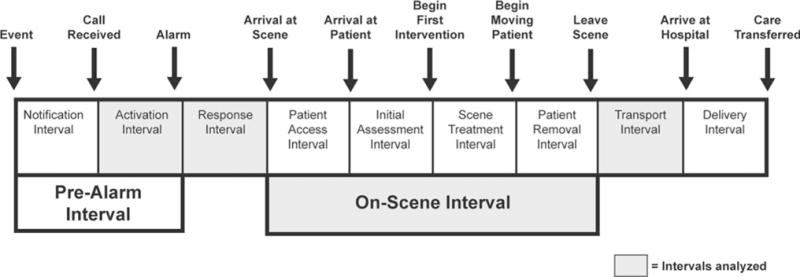
Specific time intervals and time stamps for prehospital transportation of a patient. Adapted with permission from prehospital emergency care by National Association of EMS Physicians (US) reproduced with permission of Hanley & Belfus, Inc. in the format Journal via Copyright Clearance Center
While response and transport intervals (driving time) account for the majority of the total prehospital time, complete measure of the prehospital time interval requires the inclusion of additional times to account for other essential prehospital activities [16]. The time from the 911 telephone call until ambulance dispatch was 1.4, 1.4, and 2.9 min for urban, suburban, and rural areas, respectively [16]. An additional 13.5, 13.5, and 15.1 min based on urban, suburban, and rural areas were also added to the model to account for the time spent on scene preparing the patient for transport as has been done previously [13, 15].
In the end, drive time estimates (response and transport intervals) as well as fixed prehospital intervals (dispatch and on-scene intervals) were summed for each block group to determine the total number of minutes it would take for the population of that block group to arrive at the closest NCU. The populations of block groups meeting different time cut-offs (45, 60, 75, and 90 min) were then summed to determine the populations able to arrive at a NCU. Results are presented at the level of the state, the division, the region, and for the US as a whole across the four time intervals [22, 23].
In addition to the estimates above, we also calculated estimates to care for alternative prehospital policies. In our time assessments including prehospital helicopter transport, we assumed that helicopters travel in straight lines for the purpose of calculating distances. To calculate flying times, we used helicopter depot-specific cruise speed by distance from helicopter base to block group centroid and then the straight-line distance to the nearest NCU. As in ground ambulance transport, additional time intervals that constitute important components of the total prehospital interval were added into our model including an activation time constant of 3.5 min and an on-scene time of 21.6 min [16]. Considering various state regulations on interstate travel of ambulances which affect trauma, prehospital, care and stroke care, we also evaluated the restriction or ability to cross state boundaries on access rates. This analysis was exempt from full review by the Institutional Review Board at the University of Pennsylvania.
Results
National Access
Seventy-three NCUs were identified in the US (Fig. 2). Nearly, 1 in 8 Americans (12.8%) have access to a NCU within 45 min by ground transportation. Roughly, 1 in 5 Americans (20.5%) have access to a NCU within 60 min, approximately 1 in 4 Americans (27.4%) within 75 min and almost 1 in 3 Americans within 90 min (32.6%). Use of air ambulances improves access to NCUs with 36.8, 50.4, 60.0, and 67.3% of the US population have access to a NCU within 45, 60, 75, and 90 min, respectively (Table 1; Fig. 2).
Fig. 2.
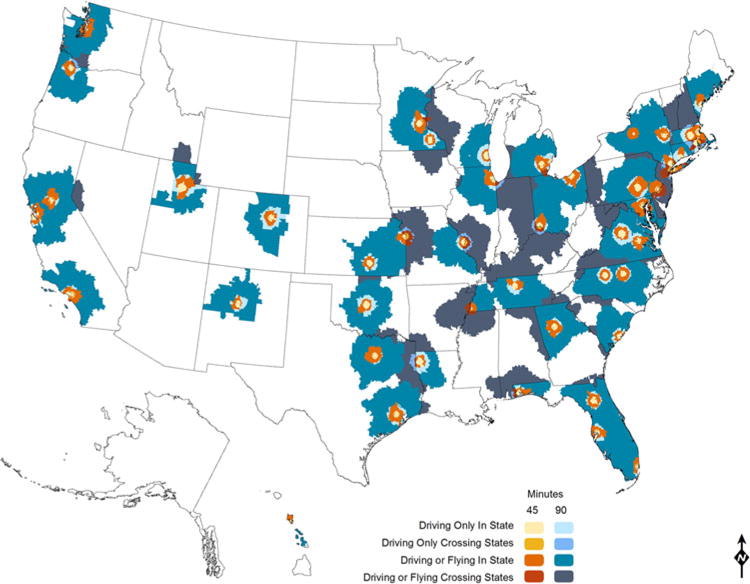
National access to Neurocritical Care Units within 45 and 90 min of travel time for in-state and cross-state restrictions by either ground or with the addition of air ambulance
Table 1.
Population access to NICUs by total US, census region, division, and state levels for 45, 60, 75, and 90 min for either ground or optional air ambulance transport
| Census region, division, state (number of NICUs) | % of population
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Ground ambulance
|
Ground or air ambulance
|
|||||||
| 45 | 60 | 75 | 90 | 45 | 60 | 75 | 90 | |
| US (73) | 12.8 | 20.5 | 27.4 | 32.6 | 36.8 | 50.4 | 60.0 | 67.3 |
| Northeast (18) | 18.5 | 29.0 | 37.7 | 43.8 | 45.5 | 59.8 | 67.2 | 70.6 |
| New England (7) | 23.8 | 36.2 | 45.4 | 53.4 | 49.0 | 70.6 | 82.5 | 84.2 |
| CT (1) | 14.8 | 24.6 | 35.1 | 48.7 | 42.1 | 85.1 | 99.0 | 100.0 |
| ME (1) | 14.1 | 19.7 | 25.6 | 33.4 | 30.1 | 52.1 | 80.3 | 89.5 |
| MA (4) | 30.8 | 49.1 | 61.1 | 69.2 | 68.4 | 85.7 | 97.2 | 98.0 |
| NH (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| RI (1) | 66.9 | 83.5 | 92.8 | 96.2 | 66.9 | 83.5 | 92.8 | 96.2 |
| VT (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Middle Atlantic (11) | 16.6 | 26.4 | 35.0 | 40.4 | 44.3 | 56.0 | 61.9 | 65.7 |
| NJ (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| NY (7) | 27.8 | 42.9 | 55.0 | 61.7 | 64.9 | 79.3 | 85.8 | 90.7 |
| PA (4) | 11.0 | 19.3 | 28.4 | 35.7 | 43.2 | 59.1 | 68.0 | 73.0 |
| Midwest (18) | 14.2 | 22.5 | 28.8 | 33.7 | 33.3 | 46.4 | 56.0 | 64.9 |
| East North Central (11) | 13.5 | 22.0 | 29.2 | 35.1 | 35.1 | 50.3 | 61.9 | 72.2 |
| IL (4) | 19.7 | 31.5 | 41.8 | 49.7 | 57.8 | 69.9 | 72.3 | 80.8 |
| IN (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| MI (3) | 9.9 | 21.8 | 32.9 | 40.3 | 29.0 | 52.0 | 72.8 | 83.0 |
| OH (3) | 14.6 | 22.5 | 28.3 | 34.6 | 39.4 | 57.8 | 73.4 | 93.7 |
| WI (1) | 18.3 | 24.9 | 28.6 | 32.9 | 25.3 | 44.0 | 65.6 | 71.6 |
| West North Central (7) | 15.8 | 23.4 | 27.9 | 30.7 | 29.2 | 37.5 | 42.5 | 48.1 |
| IA (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| KS (2) | 28.7 | 36.1 | 40.5 | 46.3 | 48.5 | 59.4 | 72.4 | 85.4 |
| MN (3) | 27.3 | 44.4 | 54.7 | 58.9 | 57.0 | 72.7 | 79.9 | 85.0 |
| MO (2) | 16.3 | 23.4 | 27.5 | 30.6 | 26.1 | 35.5 | 39.9 | 48.4 |
| NE (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| ND (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| SD (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| South (20) | 8.9 | 15.3 | 21.9 | 26.9 | 30.0 | 43.0 | 55.9 | 64.0 |
| South Atlantic (13) | 9.5 | 16.3 | 23.5 | 29.2 | 33.3 | 53.5 | 73.5 | 83.0 |
| DE (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| DC (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| FL | 10.5 | 18.1 | 25.7 | 31.8 | 39.0 | 64.1 | 89.1 | 98.6 |
| GA | 12.6 | 24.4 | 35.8 | 44.5 | 42.6 | 60.1 | 67.1 | 77.6 |
| MD | 15.1 | 24.9 | 33.5 | 41.8 | 76.0 | 94.4 | 97.8 | 98.2 |
| NC | 8.0 | 12.6 | 20.7 | 27.4 | 21.0 | 55.0 | 74.4 | 88.0 |
| SC | 6.7 | 9.5 | 12.5 | 13.3 | 12.2 | 17.7 | 26.0 | 49.2 |
| VA | 6.8 | 10.6 | 14.9 | 18.4 | 17.8 | 30.9 | 83.4 | 89.5 |
| WV (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| East South Central (2) | 4.3 | 6.9 | 8.8 | 10.6 | 10.9 | 16.7 | 19.5 | 24.2 |
| AL (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| KY (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| MS (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| TN (2) | 12.6 | 19.9 | 25.4 | 30.8 | 31.5 | 48.3 | 56.6 | 70.3 |
| West South Central (5) | 10.2 | 18.1 | 26.0 | 31.2 | 34.1 | 39.2 | 45.1 | 52.7 |
| AR (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| LA (1) | 7.3 | 8.2 | 8.7 | 9.5 | 8.2 | 9.8 | 10.9 | 17.1 |
| OK (1) | 20.8 | 27.4 | 30.7 | 32.8 | 29.4 | 37.3 | 53.2 | 76.0 |
| TX (3) | 10.3 | 20.7 | 31.5 | 38.5 | 43.4 | 49.4 | 55.4 | 61.8 |
| West (17) | 13.2 | 20.4 | 26.9 | 32.2 | 44.1 | 58.6 | 64.8 | 72.0 |
| Mountain (4) | 12.1 | 18.5 | 21.8 | 24.3 | 24.3 | 31.9 | 34.7 | 35.6 |
| AZ (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| CO (1) | 20.0 | 41.1 | 48.9 | 52.9 | 52.0 | 76.0 | 84.3 | 86.6 |
| ID (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| MT (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| NM (1) | 30.0 | 36.6 | 39.7 | 41.1 | 37.2 | 50.5 | 53.9 | 56.6 |
| UT (2) | 39.2 | 47.5 | 57.2 | 69.4 | 73.5 | 81.1 | 85.9 | 87.4 |
| NV (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| WY (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| Pacific (13) | 13.6 | 21.2 | 29.1 | 35.6 | 52.9 | 70.3 | 78.1 | 88.1 |
| AK (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| CA (10) | 13.6 | 21.7 | 30.4 | 37.7 | 55.4 | 73.6 | 82.6 | 93.9 |
| HI (1) | 23.5 | 31.0 | 41.1 | 53.1 | 70.2 | 70.2 | 77.5 | 81.2 |
| OR (1) | 27.4 | 35.7 | 41.8 | 44.4 | 44.4 | 60.4 | 64.0 | 78.7 |
| WA (1) | 5.6 | 10.1 | 14.8 | 19.3 | 45.9 | 65.0 | 68.7 | 71.1 |
Transportation is restricted to within state travel
Of the four US Census regions, the West, Northeast, Midwest, and South have 17, 18, 18, and 20 NCUs, respectively. Among divisions, the East South Central has the fewest with 2 NCUs and the Pacific and South Atlantic divisions each have the most with 13 NCUs.
By ground transportation, the Northeast region has the highest access to NCUs. Rates increase from 18.5, 29.0, 37.7 to 43.8% for 45, 60, 75, and 90 min, respectively. The South has the lowest access to NCUs. Population access is 8.9, 15.3, 21.9, and 26.9% for 45, 60, 75, and 90 min, respectively (Table 1).
With the addition of helicopters as an option for transport, the Northeast continues to have the highest access for 45, 60, and 75 min at 45.5, 59.8, and 67.2%. However, the West has 72.0% of the population within 90 min of NCU when flying or driving. The South still has the lowest access despite the addition of helicopters at 30.0, 43.0, 55.9, and 64.0% within 45, 60, 75, and 90 min, respectively (Table 1).
At the state level, 30 states have at least one NCU and two have more than five NCUs (California-10 and New York-7). No states have 100% access when using ground transportation for any timeframe. When helicopters are an option, only one state (Connecticut) has 100% access. Twenty-one states have no access regardless of timeframe or mode of transportation (Table 1).
Interstate Border Policy
When ground ambulances are allowed to cross state borders, national access minimally improves by 0.6, 1.4, 2.1, and 2.8% (with access rates of 13.4, 21.9, 29.5, and 35.4%) for 45, 60, 75, and 90 min, respectively. When helicopters are allowed to cross state borders, a larger increase in access is noticed with intervals of 4.1, 6.7, 9.3, and 12.9% (with access rates of 40.9, 57.1, 69.4, and 80.2%) within 45, 60, 75, and 90 min, respectively (Table 2).
Table 2.
Population access to NICUs by total US, census region, division, and state levels for 45, 60, 75, and 90 min for either ground or optional air ambulance transport
| Census region, division, state (number of NICUs) | % of population
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Ground ambulance
|
Ground or air ambulance
|
|||||||
| 45 | 60 | 75 | 90 | 45 | 60 | 75 | 90 | |
| US (73) | 13.4 | 21.9 | 29.5 | 35.4 | 40.9 | 57.1 | 69.4 | 80.2 |
| Northeast (18) | 20.3 | 33.2 | 44.4 | 53.4 | 59.9 | 78.9 | 88.7 | 95.4 |
| New England (7) | 25.0 | 39.8 | 50.5 | 59.4 | 55.7 | 82.3 | 94.7 | 96.6 |
| CT (1) | 16.4 | 29.5 | 45.0 | 58.7 | 54.0 | 99.6 | 100.0 | 100.0 |
| ME (1) | 14.1 | 19.7 | 25.6 | 33.4 | 30.1 | 52.1 | 80.3 | 89.5 |
| MA (4) | 32.7 | 54.4 | 67.0 | 75.6 | 74.8 | 93.9 | 99.7 | 100.0 |
| NH (0) | 0.0 | 0.0 | 0.2 | 6.6 | 0.5 | 33.6 | 96.4 | 99.4 |
| RI (1) | 66.9 | 83.5 | 93.0 | 96.4 | 79.4 | 99.9 | 100.0 | 100.0 |
| VT (0) | 0.0 | 0.0 | 0.0 | 0.3 | 0.0 | 3.8 | 31.0 | 46.2 |
| Middle Atlantic (11) | 18.6 | 30.8 | 42.3 | 51.3 | 61.4 | 77.6 | 86.5 | 95.0 |
| NJ (0) | 9.0 | 20.5 | 33.6 | 47.6 | 65.1 | 97.4 | 100.0 | 100.0 |
| NY (7) | 27.8 | 42.9 | 55.1 | 63.0 | 71.1 | 79.5 | 85.9 | 91.2 |
| PA (4) | 11.0 | 19.3 | 28.4 | 35.7 | 43.6 | 60.8 | 78.1 | 97.4 |
| Midwest (18) | 15.1 | 24.3 | 31.6 | 37.2 | 37.0 | 52.7 | 67.9 | 81.4 |
| East North Central (11) | 13.8 | 23.0 | 31.2 | 37.7 | 38.1 | 56.4 | 75.3 | 90.6 |
| IL (4) | 20.8 | 34.0 | 45.7 | 54.0 | 61.5 | 75.9 | 79.7 | 92.8 |
| IN (0) | 0.2 | 2.1 | 6.5 | 10.0 | 6.5 | 16.3 | 64.1 | 86.7 |
| MI (3) | 9.9 | 21.8 | 32.9 | 40.3 | 30.2 | 52.7 | 75.7 | 88.4 |
| OH (3) | 14.6 | 22.5 | 28.3 | 34.6 | 42.0 | 63.6 | 76.2 | 94.9 |
| WI (1) | 18.3 | 24.9 | 28.9 | 33.7 | 26.4 | 49.0 | 75.1 | 85.2 |
| West North Central (7) | 18.1 | 27.3 | 32.5 | 35.8 | 34.5 | 44.4 | 50.8 | 60.3 |
| IA (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 5.6 | 17.9 |
| KS (2) | 28.7 | 36.1 | 40.5 | 46.3 | 48.6 | 60.0 | 72.7 | 86.6 |
| MN (3) | 27.3 | 44.4 | 54.7 | 58.9 | 58.2 | 73.6 | 80.2 | 85.2 |
| MO (2) | 24.1 | 36.7 | 43.3 | 48.0 | 43.2 | 57.7 | 65.0 | 80.2 |
| NE (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.3 |
| ND (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| SD (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| South (20) | 9.1 | 15.7 | 22.3 | 27.4 | 31.6 | 47.9 | 63.0 | 76.2 |
| South Atlantic (13) | 9.5 | 16.3 | 23.5 | 29.3 | 35.4 | 59.4 | 78.3 | 91.2 |
| DE (0) | 0.0 | 0.0 | 2.7 | 8.1 | 54.2 | 84.9 | 100.0 | 100.0 |
| DC (0) | 0.0 | 0.0 | 0.0 | 0.0 | 100.0 | 100.0 | 100.0 | 100.0 |
| FL | 10.5 | 18.1 | 25.7 | 31.8 | 39.0 | 64.1 | 89.1 | 98.6 |
| GA | 12.6 | 24.4 | 35.8 | 44.5 | 42.6 | 60.1 | 69.1 | 82.6 |
| MD | 15.1 | 24.9 | 33.5 | 41.9 | 76.1 | 94.9 | 99.1 | 100.0 |
| NC | 8.0 | 12.6 | 20.7 | 27.4 | 21.0 | 55.0 | 74.9 | 89.7 |
| SC | 6.7 | 9.5 | 12.5 | 13.3 | 12.2 | 17.7 | 30.2 | 76.1 |
| VA | 6.8 | 10.6 | 14.9 | 18.4 | 19.8 | 58.3 | 91.2 | 98.2 |
| WV (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.8 | 15.4 | 42.1 |
| East South Central (2) | 5.5 | 8.8 | 10.9 | 13.3 | 13.7 | 25.9 | 41.7 | 62.1 |
| AL (0) | 0.0 | 0.2 | 0.4 | 1.2 | 0.4 | 12.3 | 22.7 | 40.6 |
| KY (0) | 4.9 | 7.8 | 8.5 | 9.0 | 8.3 | 19.7 | 54.6 | 83.9 |
| MS (0) | 0.0 | 0.0 | 0.1 | 1.4 | 4.9 | 8.6 | 15.0 | 32.6 |
| TN (2) | 12.6 | 19.9 | 25.4 | 30.8 | 31.5 | 48.3 | 59.5 | 77.0 |
| West South Central (5) | 10.2 | 18.2 | 26.1 | 31.4 | 34.2 | 39.9 | 48.3 | 58.4 |
| AR (0) | 0.0 | 0.4 | 1.2 | 1.4 | 1.7 | 5.5 | 13.4 | 43.4 |
| LA (1) | 7.3 | 8.2 | 8.7 | 9.5 | 8.2 | 9.8 | 10.9 | 19.8 |
| OK (1) | 20.8 | 27.4 | 30.7 | 32.8 | 29.4 | 37.3 | 54.7 | 78.4 |
| TX (3) | 10.3 | 20.7 | 31.5 | 38.6 | 43.5 | 49.7 | 58.1 | 64.2 |
| West (17) | 13.3 | 20.8 | 27.4 | 32.8 | 44.6 | 59.2 | 66.1 | 73.6 |
| Mountain (4) | 12.1 | 18.5 | 21.8 | 24.3 | 24.3 | 31.9 | 36.4 | 38.6 |
| AZ (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| CO (1) | 20.0 | 41.1 | 48.9 | 52.9 | 52.0 | 76.0 | 84.3 | 86.6 |
| ID (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 6.5 |
| MT (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| NM (1) | 30.0 | 36.6 | 39.7 | 41.1 | 37.2 | 50.5 | 53.9 | 56.6 |
| UT (2) | 39.2 | 47.5 | 57.2 | 69.4 | 73.5 | 81.1 | 85.9 | 87.4 |
| NV (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 13.9 | 20.8 |
| WY (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 2.7 | 3.3 |
| Pacific (13) | 13.8 | 21.8 | 29.8 | 36.5 | 53.6 | 71.2 | 79.2 | 89.0 |
| AK (0) | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| CA (10) | 13.6 | 21.7 | 30.4 | 37.7 | 55.4 | 73.6 | 82.6 | 93.9 |
| HI (1) | 23.5 | 31.0 | 41.1 | 53.1 | 70.2 | 70.2 | 77.5 | 81.2 |
| OR (1) | 27.4 | 35.7 | 41.8 | 44.4 | 44.4 | 60.4 | 64.0 | 78.8 |
| WA (1) | 7.1 | 14.7 | 20.4 | 25.7 | 51.0 | 71.8 | 76.9 | 78.3 |
Transportation can cross state borders
Among regions, the Northeast had the highest incremental increase in access rates regardless of mode of transportation. Using ground transportation, access rates increased by 1.7, 4.2, 6.7, and 9.6% (with access rates of 20.3, 33.2, 44.4, and 53.4%) and air ambulance transport increased access rates by 14.4, 19.1, 21.4, and 24.9% (with access rates of 59.9, 78.9, 88.7, and 95.4%) within 45, 60, 75, and 90 min, respectively. The South and West had minimal improvement with the relaxation of the interstate restriction with increases of 0.2, 0.3, 0.4, and 0.6% in the South (with access rates of 9.1, 15.7, 22.3, and 27.4%) and in the West, 0.1, 0.4, 0.5, and 0.6% with the West (with access rates of 13.3, 20.8, 27.4, and 32.8%) within 45, 60, 75, and 90 min, respectively. With the option of air transport, the West had the lowest incremental increase in access with interval increases of 0.5, 0.6, 1.3, and 1.6% (with access rates of 44.6, 59.2, 66.1, and 73.6%) within 45, 60, 75, and 90 min, respectively (Table 2).
Discussion
We present the first data on population access to neurocritical care in the US. Only one-third of the US has access to neurocritical care by ground within 90 min and there are significant regional variations with the Northeast and the South having the highest and lowest respective access, regardless of mode of transportation. While the West has the highest access for intrastate transport, it requires the use of air ambulances and only minimally improves over the Northeast. In addition, examination of state border policies shows that there is a minimal improvement in access rates and the West drops to last when state borders restrictions are relaxed. Even when air ambulances are utilized under the most relaxed conditions, one-third of the country still does not have timely neurocritical care access. Allowing transportation across state borders had a minimal effect for ground transportation but dramatically increased access with the option of air ambulances.
Evaluating access to NCUs provides insight into state, regional, and national variability in neurocritical care access. For a young specialty such as neurocritical care, this is essential to move forward and identify which information is necessary to strategically plan where and how to grow. Yet, this study also raises numerous questions and highlights the need for additional data to further enhance population-based planning. For example, which patients need immediate prehospital transportation to facilities with NCUs? What is the appropriate number of neurocritical care beds for a population? Are there regional differences in need for neurocritical care beds? What is the ideal timeframe to get a patient to a NCU to optimize outcomes and does this vary by condition?
This study is the first step in beginning to systematically coordinate the planning of neurocritical care in the US. These results provide clinicians, hospital administrators, and public policy makers with information to identify public access to NCUs. By focusing on the areas that have the lowest access, efforts can be targeted to maximize population access in an efficient manner. Important next steps will need to consider the important overlap between other related resources such as prehospital care, EDs, stroke centers, trauma centers, and other critical care beds. The population-based approach to emergency care planning provides the opportunity to develop an integrated, coordinated, and comprehensive system of emergency care. Neurocritical care plays a growing and vital role in the emergency care system. Given its multidisciplinary overlap in care of acutely ill and injured patients, potential for growth, regional variation and identified disparities, neurocritical care and critically ill neurological patients stand to benefit from such an approach.
Limitations
Our results should be considered in light of several limitations. There is no standardized timeframe for access to care in a NCU. The time limits of 45, 60, 75, and 90 min were chosen based on earlier study combined with our judgment as to what response times could have been clinically meaningful [12, 13, 15–17]. In addition, this analysis was conducted using publicly available information from the NCS and could result in a selection bias. The purpose of this study was to identify access to NCUs given existing information and the NCS is the only repository of such information. As the NCS list is a self-reported document compiled from members of that organization, there are two limitations to use this data source. First, there is no standardized definition regarding characteristics of a NCU and thus this list may include primary stroke centers (PSC) as designated by the Joint Commission, which do not provide broader critical care coverage in addition to neurosurgical care. While efforts were made to specifically differentiate PSCs from NCUs, misclassification could potentially result. Without a standardized definition or accrediting body for NCUs, some sites could have been inappropriately misclassified. Second, there may be NCUs that meet the criteria for inclusion not in the NCS database that were not included in this study. However, while standardizing the definition of NCUs and identifying all possible NCUs is an important area of future research, is beyond the scope of available data and this study. Such biases could result in either falsely increased or decreased access for particular regions of the country. Another limitation is that our assumptions were based upon prehospital transport of patients to facilities with NCUs rather than interfacility transportation. Interfacility transfer would require prehospital diagnostics and destination protocols and a realistic system would instead require comprehensive understanding of transfer patterns between hospitals. Emergency Department boarding is another important consideration not factored into this model because it could affect a patient’s ability to be cared for within a NCU. But, models such as the one presented in this article provide insight and inform planning. As understanding of system dynamics improves, more complex models can be developed to capture additional facets of the care system. Further limitations include the use of prehospital time intervals which were developed for trauma, not neurocritical care emergencies. However, these are the best estimates of prehospital times that are available. This model also fails to address neurocritical care emergencies that happen to inpatients in facilities without NCUs. Finally, this analysis only takes into account the presence of a NCU, not the specific number of resources available to a NCU (such as beds). Future use of greater detail per hospital unit (i.e., bed size) could be used to refine future calculations of geographic access to neurocritical care resources for large populations.
Conclusions
Current geographic access to NCUs is low throughout the US, particularly the Southern region. A reliance on air ambulances is necessary until additional better geographic distribution of NCUs can occur.
Acknowledgments
Tara D. Jackson, PhD, Vicky Tam, MS, and Karl A. Dailey, BS provided programing and mapping support. Dr. Ward is supported by a fellowship grant from the Emergency Medicine Foundation. Dr. Carr is supported by a career development award from the Agency for Healthcare Research and Quality (K08HS017960). Dr. Branas is partially funded by a research grant also from the Agency for Healthcare Research and Quality (R01HS018362). Air medical data were obtained from the Atlas and Database of Air Medical Services (ADAMS), compiled by and under license from CUBRC’s Center for Transportation Injury Research (CenTIR) in alliance with the Association of Air Medical Services (AAMS) and the air medical industry, with support from the Federal Highway Administration. This manuscript is solely the responsibility of the authors and does not necessarily represent the official views of either CUBRC, AAMS or the US DOT.
Contributor Information
Michael J. Ward, Department of Emergency Medicine, University of Cincinnati, 231 Albert Sabin Way, Room 1654H ML 0769, Cincinnati, OH 45267-0769, USA
Lori A. Shutter, Departments of Neurosurgery & Neurology, UC Neuroscience Institute, University of Cincinnati, Cincinnati, OH, USA
Charles C. Branas, Department of Biostatistics and Epidemiology, University of Pennsylvania School of Medicine, Philadelphia, PA, USA
Opeolu Adeoye, Departments of Emergency Medicine and Neurosurgery, Division of Neurocritical Care, University of Cincinnati, Cincinnati, OH, USA.
Karen C. Albright, Comprehensive Stroke Center, University of Alabama at Birmingham, Birmingham, AL, USA
Brendan G. Carr, Departments of Emergency Medicine & Epidemiology, Perelman School of Medicine, University of Pennsylvania, Philadelphia, PA, USA
References
- 1.Xu JQ, Kochanek KD, Murphy SL, Tejada-Vera B. Deaths: final data for 2007. National Center for Health Statistics; 2010. http://www.cdc.gov/NCHS/data/nvsr/nvsr58/nvsr58_19.pdf. Accessed 10 Sep 2010. [PubMed] [Google Scholar]
- 2.Coronado VG, Xu L, Basavaraju SV, et al. Surveillance for traumatic brain injury-related deaths—United States, 1997–2007. MMWR Surveill Summ. 2011;60:1–32. [PubMed] [Google Scholar]
- 3.Mayer SA. Neurological intensive care: emergence of a new specialty. Neurocrit Care. 2006;5:82–4. doi: 10.1385/NCC:5:2:82. [DOI] [PubMed] [Google Scholar]
- 4.Bershad EM, Feen ES, Hernandez OH, Suri MF, Suarez JI. Impact of a specialized neurointensive care team on outcomes of critically ill acute ischemic stroke patients. Neurocrit Care. 2008;9:287–92. doi: 10.1007/s12028-008-9051-5. [DOI] [PubMed] [Google Scholar]
- 5.Diringer MN, Edwards DF. Admission to a neurologic/neurosurgical intensive care unit is associated with reduced mortality rate after intracerebral hemorrhage. Crit Care Med. 2001;29:635–40. doi: 10.1097/00003246-200103000-00031. [DOI] [PubMed] [Google Scholar]
- 6.Mirski MA, Chang CW, Cowan R. Impact of a neuroscience intensive care unit on neurosurgical patient outcomes and cost of care: evidence-based support for an intensivist-directed specialty ICU model of care. J Neurosurg Anesthesiol. 2001;13:83–92. doi: 10.1097/00008506-200104000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Suarez JI, Zaidat OO, Suri MF, et al. Length of stay and mortality in neurocritically ill patients: impact of a specialized neurocritical care team. Crit Care Med. 2004;32:2311–7. doi: 10.1097/01.ccm.0000146132.29042.4c. [DOI] [PubMed] [Google Scholar]
- 8.Varelas PN, Schultz L, Conti M, Spanaki M, Genarrelli T, Hacein-Bey L. The impact of a neuro-intensivist on patients with stroke admitted to a neurosciences intensive care unit. Neurocrit Care. 2008;9:293–9. doi: 10.1007/s12028-008-9050-6. [DOI] [PubMed] [Google Scholar]
- 9.Naval NS, Carhuapoma JR. Impact of pattern of admission on ICH outcomes. Neurocrit Care. 2010;12:149–54. doi: 10.1007/s12028-009-9302-0. [DOI] [PubMed] [Google Scholar]
- 10.Rincon F, Mayer SA, Rivolta J, et al. Impact of delayed transfer of critically ill stroke patients from the Emergency Department to the Neuro-ICU. Neurocrit Care. 2010;13:75–81. doi: 10.1007/s12028-010-9347-0. [DOI] [PubMed] [Google Scholar]
- 11.Carr BG, Addyson DK. Geographic information systems and emergency care planning. Acad Emerg Med. 2010;17:1274–8. doi: 10.1111/j.1553-2712.2010.00947.x. [DOI] [PubMed] [Google Scholar]
- 12.Albright KC, Branas CC, Meyer BC, et al. ACCESS: acute cerebrovascular care in emergency stroke systems. Arch Neurol. 2010;67:1210–8. doi: 10.1001/archneurol.2010.250. [DOI] [PubMed] [Google Scholar]
- 13.Branas CC, MacKenzie EJ, Williams JC, et al. Access to trauma centers in the United States. JAMA. 2005;293:2626–33. doi: 10.1001/jama.293.21.2626. [DOI] [PubMed] [Google Scholar]
- 14.Carr BG, Addyson DK, Kahn JM. Variation in critical care beds per capita in the United States: implications for pandemic and disaster planning. JAMA. 2010;303:1371–2. doi: 10.1001/jama.2010.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carr BG, Branas CC, Metlay JP, Sullivan AF, Camargo CA., Jr Access to emergency care in the United States. Ann Emerg Med. 2009;54:261–9. doi: 10.1016/j.annemergmed.2008.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carr BG, Caplan JM, Pryor JP, Branas CC. A meta-analysis of prehospital care times for trauma. Prehosp Emerg Care. 2006;10:198–206. doi: 10.1080/10903120500541324. [DOI] [PubMed] [Google Scholar]
- 17.Klein MB, Kramer CB, Nelson J, Rivara FP, Gibran NS, Concannon T. Geographic access to burn center hospitals. JAMA. 2009;302:1774–81. doi: 10.1001/jama.2009.1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Census 2000 datasets. 2000 http://www2.census.gov/census_2000/datasets/ Accessed 28 March 2011.
- 19.Geography Division UCB. Centers of population computation for 1950, 1960, 1970, 1980, 1990 and 2000.
- 20.Neurocritical Care Society. http://maps.google.com/maps/ms?ie=UTF8&hl=en&msa=0&msid=108542175118493601623.00047fcc91780cd976daf&ll=33.000884,-111.965918&spn=29.210936,91.784334&source=embed. Accessed 2 Feb 2011.
- 21.Atlas & Database of Air Medical Services. 2009 http://www.adamsairmed.org/ Accessed 28 March 2011.
- 22.Love RF, Morris JG. Mathematical-models of road travel distances. Manag Sci. 1979;25:130–9. [Google Scholar]
- 23.Love RF, Morris JG, Wesolowsky GO. Facilities location: models & methods. New York: North-Holland Publishers; 1988. [Google Scholar]


