Abstract
Purpose: The aim of this study was to identify sex venue-based networks among men who have sex with men (MSM) to inform HIV preexposure prophylaxis (PrEP) dissemination efforts.
Methods: Using a cross-sectional design, we interviewed MSM about the venues where their recent sexual partners were found. Venues were organized into network matrices grouped by condom use and race. We examined network structure, central venues, and network subgroups.
Results: Among 49 participants, the median age was 27 years, 49% were Black and 86% reported condomless anal sex (ncAS). Analysis revealed a map of 54 virtual and physical venues with an overlap in the ncAS and with condom anal sex (cAS) venues. In the ncAS network, virtual and physical locations were more interconnected. The ncAS venues reported by Blacks were more diffusely organized than those reported by Whites.
Conclusion: The network structures of sex venues for at-risk MSM differed by race. Network information can enhance HIV prevention dissemination efforts among subpopulations, including PrEP implementation.
Keywords: : dissemination, implementation, men who have sex with men, network analysis, preexposure prophylaxis for HIV, PrEP
Introduction
Over 40,000 new HIV infections occur each year in the United States (US).1 The majority of these new HIV infections occur among men who have sex with men (MSM) and the incidence has risen by 22% from 2005 to 2014 among Black MSM.2 The increased rates of HIV among Black MSM are due to: high proportions of those who are unaware of their status, infrequent HIV testing, lower rates of viral suppression among those who are HIV positive, structural barriers, same-race partners, high rates of condomless anal sex (ncAS) reported among both HIV-positive and HIV-negative MSM, low HIV serostatus disclosure rates among sexual partners, having known HIV-positive partners, and small and exclusive sexual networks.3–10 One in two Black MSM and one in 11 White MSM have a lifetime risk of HIV acquisition.11 To address these population-specific rates, HIV prevention programming will need to be culturally and contextually tailored.7,12,13
Preexposure prophylaxis (PrEP), the use of daily antiretrovirals to prevent HIV acquisition, provides the opportunity to lower HIV incidence significantly among populations most at risk. The iPrEX study, which evaluated the effectiveness of emtricitabine/tenofovir in HIV-negative MSM and transgender women, found that individuals who adhered to the drug had a 92% reduced risk of being infected with HIV.14 With proven safety and efficacy, PrEP is now recommended for at-risk populations, such as MSM.15,16
It is estimated that 1,232,000 adults in the United States are at risk for HIV and have indications for PrEP; 492,000 of whom are MSM.17 However, as of 2015, only 49,148 unique individuals had initiated PrEP, with 74% of those individuals being White (vs. 10% Black).18 To address the racial disparities in PrEP utilization, more effort is needed to improve knowledge dissemination, linkage to care, and delivery of services for racial and ethnic minorities.19,20
Regional implementation of an evidence-based innovation, such as PrEP, among consumers, providers, communities, and organizations can be considered a process that involves defined stages.21,22 Aarons et al. describe the four-stage model of implementation progress.21 The first or exploratory phase of implementation identifies the consumers' or communities' needs. One methodology suggested during this phase is network analysis.21 Network analysis can identify structural patterns to inform evidence-based implementation.12 One example of this is mapping out venues where MSM racial subgroups find condomless anal sexual partners, to identify dissemination targets for PrEP awareness programming.23,24
Approaching biomedical HIV prevention implementation from a network perspective is not a new concept. The network approach has proven advantageous since HIV transmission occurs in relation to sexual networks. Studies have shown that the characteristics of sexual networks play an important role in predicting HIV risk and can help guide prevention practices.10,23–28 Fundamentally, network analysis provides tools to map social structure, as well as analyze the relationships between objects in that social structure.29 Several measures provide a useful understanding of how to interpret these constructed networks: density measures the overall interconnectedness of the network; centrality indicates the relative prominence of individual members of the network; diameter provides a measure of how far apart on average members are in the network; and isolates identify those with no links within the identified network.12,29 Using these measures on high-risk sexual networks can inform PrEP service delivery planning.
For the purposes of guiding PrEP implementation efforts in St. Louis, Missouri, we employed network analysis as a strategy to identify the overall structure of sex venues as well as specific venues that occupy central positions in the network (i.e., “hot spots” for high-risk sexual activity among young adult MSM). Our goal with this network study was to identify network venue type (virtual vs. physical) relationships, structural characteristics of the networks, central locations, and racial differences. We explore the utility of these methods for guiding PrEP implementation strategies.
Methods
We conducted a cross-sectional observational network study among 49 MSM. Study eligibility was self-identified as MSM, age 18–35 years, self-reported race of African American/Black or Caucasian/White, self-reported anal sex within the past 6 months, and the ability to give informed consent. Recruitment occurred among African American/Black and Caucasian/White MSM so that we could report on networks among Black MSM in comparison to a group of White MSM as a control. The study was conducted from June 2014 to September 2015 in St. Louis. Participants were recruited using flyers placed at designated primary care and HIV specialty clinics, community-based organization facilities and events, clubs, bars, coffee shops, restaurants, bathhouses, websites, and smartphone applications. Both HIV-positive and HIV-negative individuals were included in this analysis to discern the meeting points where both positive and negative individuals were seeking sexual partners.
Participants were given a self-administered written survey. Participants were asked to provide the names of the clubs, bars, websites, smartphone applications, and other places that they used to find or meet with their anal sexual partners in the past 12 months for the following categories: all anal sex encounters, with condom anal sex (cAS), and ncAS. Participants were then asked to list the total number of times they visited these venues in the past 12 months. The names of the venues were then categorized into physical or virtual. Venues that were bars, clubs, coffeehouses, restaurants, or other physical locations were characterized as physical venues. It should be noted that virtual venues and local physical venue names were removed to maintain confidentiality and privacy. Virtual venues were smartphone applications (e.g., Grindr, SCRUFF, Jack'd, Tinder, Manhunt, Adam4Adam), other websites (e.g., Craigslist), and social networking websites (e.g., Facebook and Instagram). No information was gathered about the specific sexual partners of each study participant. The survey assessment included demographics (i.e., age, race, and gender), sexual risk behaviors, recreational drug use, and prior PrEP knowledge and use.
To capture sexual risk behavior, participants were asked to report a history of a diagnosed sexually transmitted infection (STI) (i.e., gonorrhea, chlamydia, or syphilis) in the past 12 months, as well as the number of total anal sex partners in the past 6 months, the number of HIV-positive anal sex partners in the past 6 months, and if they had a ncAS partner in the past 6 months. Participants were also asked if they had ever heard of PrEP before the day of the survey and if they were currently taking PrEP at the time of the survey. Participants were given a $25 grocery card as compensation for their time. All participants provided written informed consent. The Washington University in St. Louis Institutional Review Board approved the study.
Data analyses
Network analyses were performed using the identified list of physical and virtual venues gathered from the written survey and qualitative interview data, along with the sociodemographic data. Data were organized into two-mode affiliation networks.30 Two-mode affiliation networks here are networks in which participants are linked to the venues they visited. These data were then transposed into one-mode weighted networks of venues where venues are linked together if they shared any common participants (i.e., if one participant goes to venue A and then venue B, the two venues are linked with a tie with a weight of one). Venues were characterized as condomless or with condom based on survey responses. Characterization of venues as either “Black” or “White” was based on the reported race of the study participant who reported sexual encounters at that venue. Five venue networks were produced: All sex venues, cAS venues, ncAS venues, White ncAS venues, and Black ncAS venues.
Network descriptive statistics were calculated and compared across networks. Network size refers to the total number of venues in each network. Density is the proportion of observed ties to the maximum possible number of ties, and is a measure of interconnectedness.30 Betweenness centralization is a statistic summarizing the variability of node centrality in the network.30 Networks with high centralization exhibit hierarchical structure, in which some venues have high centrality, whereas most venues have low centrality. Transitivity is the extent to which two connected venues have a connection to a common third venue. Values are on a scale of 0 to 1 with higher numbers suggesting more of a tendency of triadic connections. Assortativity is a measure of the extent to which virtual venues connected with virtual venues and physical venues with physical venues.30 Values are positive when matching on this characteristic is high, and negative when matching is low. Finally, modularity is the chance-corrected statistic of the presence of cohesive subgroups, with higher scores indicating greater subgroup cohesion.31 Subgroup analysis was done of the venues related to this study participant's race and condom use. These subgroups in the networks were identified using the walktrap community detection algorithm.32 All network analyses were conducted using the igraph package version 1.0.1 in R version 3.3.0.33
Results
Participants had a median age of 27 years (interquartile range [IQR] 24–30), 51% were White, 49% were Black, 61% did not graduate college, and 88% were HIV negative. The median number of total anal sex partners in the past 6 months was four (IQR 2–7), and 86% reported having had ncAS in the past 6 months (Table 1). Thirty-three percent (16/49) reported having had an HIV-positive anal sex partner in the past 6 months. Fifty-two percent (25/48) of the study population reported recreational drug use within the past 6 months and 19% (9/48) reported having been diagnosed with a STI in the past 12 months. Marijuana was the most commonly reported recreational drug used (crack/cocaine, methamphetamines, and ecstasy were also reported) and there was no intravenous drug use reported among participants. Eighty-six percent of participants (42/49) had ever heard of PrEP and 13% (6/45) were taking PrEP at the time of the survey (Table 1).
Table 1.
Men Who Have Sex with Men Study Participant Demographics and Sexual Risk
| Characteristics | n (%) Total N = 49 |
|---|---|
| Median age (IQR) (years) | 27 (24–30) |
| Race | |
| White | 25 (51) |
| Black | 24 (49) |
| Education | |
| Less than college | 30 (61) |
| College graduate and postgraduate | 19 (39) |
| History of STI in the past 12 months | |
| No | 39 (81) |
| Yes | 9 (19) |
| Reported recreational drug use in the past 6 months | 25 (52) |
| HIV status | |
| Negative | 43 (88) |
| Positive | 4 (8) |
| Unknown | 2 (4) |
| Median number of anal sex partners in the past 6 months (IQR) | 4 (2–7) |
| Had a condomless anal sex partner in the past 6 months | 42 (86) |
| Had an HIV-positive anal sex partner in the past 6 months | 16 (33) |
| Had ever heard of PrEP | 42 (86) |
| Currently taking PrEP | 6 (13) |
IQR, interquartile range; PrEP, preexposure prophylaxis; STI, sexually transmitted infection.
MSM reported a total of 54 different physical or virtual venues where they met anal sex partners in the past 12 months (35% were physical and 65% were virtual). The most frequent venue reported was Digital Venue A (53%), a smartphone application. Study participants reported the following top three physical venues: (1) Club A (22%), (2) Club B (16%), and (3) Bar A (16%). Thirty-four (63%) venues were categorized as ncAS; the top three ncAS venues reported were: (1) Digital Venue A, (2) Digital Venue B, and (3) Club A. Figure 1 shows the overlap between venues reported by MSM study participants who used condoms, and venues where participants did not use condoms. Figure 1 also reveals the overlap between venues grouped by race. Eighteen venues overlapped between cAS and ncAS and 10 venues overlapped among Blacks and Whites. The top three ncAS venues reported by Blacks were: (1) Digital Venue B, (2) Digital Venue A, and (3) Club B, whereas the top three ncAS venues reported by Whites were: (1) Digital Venue A, (2) Club A, and (3) Digital Venue C.
FIG. 1.
Venn diagrams demonstrating an overlap of anal sex venues frequented by 49 men who have sex with men study participants, grouped by condom use and race.
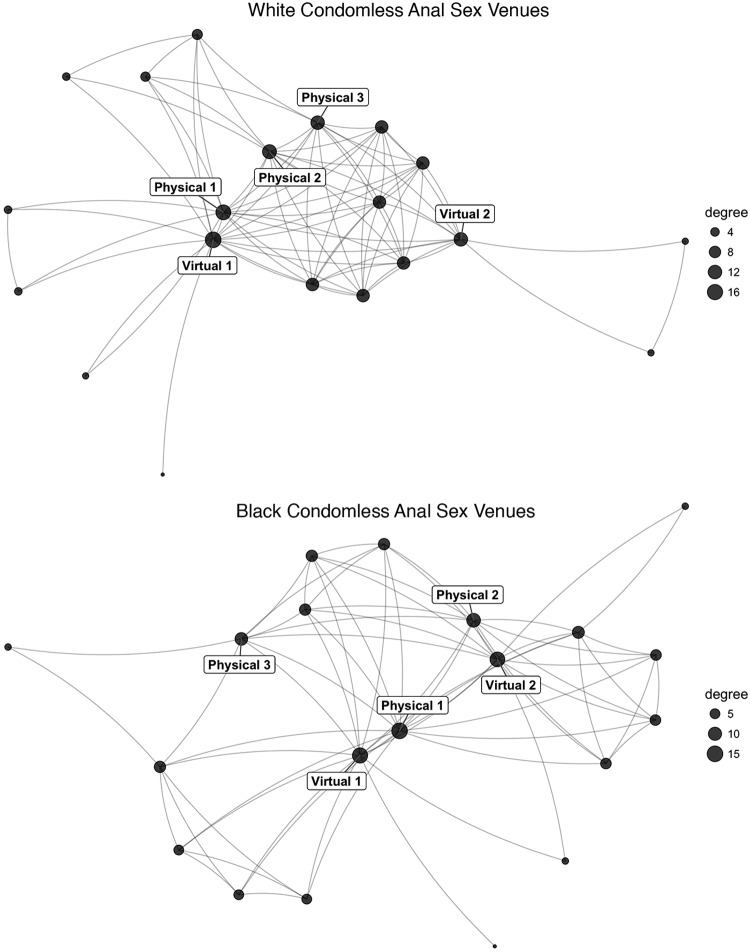
The structure of venue networks showed a diversity of interconnected physical and virtual locations. Within these graphs, central locations and subgroups can be visually identified as centrally positioned nodes and densely clustered groups, respectively (Fig. 2). These visual patterns are corroborated by the quantitative characteristics of the venue networks displayed in Table 2. The cAS and ncAS venue networks had similar global structural statistics in terms of centralization (0.16, 0.18) and density (0.20, 0.24). However, the cAS venue network had higher assortativity (0.15) and modularity (0.28), suggesting that virtual venues were more likely to be linked to other virtual venues and physical venues with physical venues. The result is a network with more internally homogenous communities. Finally, the White ncAS venue network was more dense (0.41) and centralized (0.28) compared with the Black ncAS venue network (density = 0.25, centralization = 0.15), which can be seen in the visualization as well (Fig. 3). In the diagram, the nodes are sized according to the number of ties received, known as degree. It is apparent that the Black ncAS was more diffusely organized with less central targets than the White ncAS network.
FIG. 2.
Virtual and physical anal sex venue network composition among men who have sex with men, grouped by condom use and race.
Table 2.
Sex Venue Network Characteristics Among Men Who Have Sex with Men (N = 49)
| Network | Size | Density | Centralization | Transitivity | Assortativity | Modularity |
|---|---|---|---|---|---|---|
| All anal sex | 54 | 0.19 | 0.17 | 0.54 | 0.12 | 0.21 |
| Condom anal sex | 39 | 0.20 | 0.16 | 0.60 | 0.15 | 0.28 |
| Condomless anal sex | 34 | 0.24 | 0.18 | 0.61 | −0.01 | 0.23 |
| White condomless anal sex | 20 | 0.41 | 0.28 | 0.75 | −0.02 | 0.17 |
| Black condomless anal sex | 24 | 0.25 | 0.15 | 0.64 | −0.04 | 0.20 |
The Black condomless anal sex venue network is less dense and less centralized than the White condomless anal sex venue.
FIG. 3.
Comparisons between White and Black Condomless Anal Sex Venue Networks. The Black network is more diffusely organized than the White network. Degree refers to the number of ties received by a node.
Central venues for seeking anal sex differed across the networks. For the ncAS and cAS networks, four out of the top five more central venues were virtual, with two in common (Digital Venues A and B). The ncAS had three virtual venues in the top five venues with less difference in the centrality across the five. The White ncAS had two virtual venues (Digital Venues A and D, a smartphone application and a social networking website, respectively) in the top five as highlighted in Figure 3. The Black ncAS had two virtual venues (Digital Venues A and B, two smartphone applications) in the top five (Fig. 3). One virtual venue (Digital Venue A) was in the top five of all networks. The central venues in the network represent important targets for implementation and dissemination efforts. Because of the less centralized structure of the Black condomless network, an approach targeting the subgroup communities may be needed in addition to the focus on central locations.
Discussion
This study was among the first to use network analysis to evaluate at-risk populations to inform PrEP implementation efforts. We identified virtual and physical venues where local young adult MSM, the majority of whom was HIV negative and not taking oral PrEP, met. Most MSM were meeting anal sex partners online and there were distinct venues where MSM met ncAS partners. Regardless of condom use, there was overlap between venue networks where MSM met partners. The ncAS and cAS venue networks had similar global network structures, but within the ncAS network, venues reported by Blacks tended to be more dispersed and locally clustered than those reported by Whites. Overall, Blacks reported meeting sex partners at different venues than Whites (i.e., Digital Venue B vs. A). Virtual venues emerged as effective locations to reach those within the sex venue networks, including one virtual venue that was present in the top five of all the networks analyzed.
These network structures suggest differing strategies for optimal PrEP implementation among MSM in St. Louis. First, central venues were identified that were key components of the network. Outreach using these venues to perform HIV testing, PrEP and other HIV prevention education, and linkage to care can strengthen steps along the PrEP care continuum for the local area.34,35 Second, reaching Black MSM may require engaging different venues than White MSM. We found that Digital Venue B was a central component of the ncAS network among Black MSM that may represent an ideal venue for PrEP implementation efforts. Third, there may be separate networks and venues where MSM meet partners with whom they engage in ncAS or cAS. Priority for PrEP awareness and linkage-to-care initiatives should be given to venues associated with ncAS.
We—authors affiliated with an academic PrEP clinical program—aim to collaborate with local community-based organizations and health department officials, through PrEP-specific forums that exist at the state and local levels, to disseminate study findings and to intensify HIV testing efforts at the specific locations identified in this analysis. Some of the physical venues identified in the study are known (i.e., bars and clubs), but some may be newly discovered “hotspots,” such as a skate rink and a few park locations. Disseminating a list of identified locations to community HIV prevention partners can hopefully lead to efforts to include these venues within current prevention programs. However, it is much clearer that more resources should focus on incorporating smartphone application companies into PrEP programming. HIV testing at the locations mentioned will also be coordinated with PrEP care referrals through the provider networks established in St. Louis, with the addition of insurance navigation as needed.36,37 We have demonstrated linkage to PrEP care, in St. Louis, through the use of smartphone applications for HIV testing and PrEP education by local organizations.38 We aim to intensify PrEP awareness campaigning efforts on the central virtual venues (i.e., smartphone applications) identified. New and dedicated HIV testing and PrEP awareness outreach efforts will need to be established for the venues identified that do not have communication with any “hotspots” (isolates within the venue network), such as the skate rink.
St. Louis's HIV incidence is highest among Black MSM and mirrors the national epidemic.1,2 Effective culturally tailored interventions will need to be developed and implemented to curb the epidemic in this population. The HIV Prevention Trials Network 073 demonstrated high oral PrEP uptake and adherence, as well as lower HIV incidence among at-risk Black MSM who were offered and accepted PrEP, which was in combination with theory-based counseling that promoted and supported PrEP use.19 Studies that define and identify racial and at-risk networks in local areas can complement such research trials to provide insight on how to reach these populations to offer evidence-based interventions.
Moreover, previous work has demonstrated that there may be significant differences in PrEP use among Black MSM compared with White MSM.18,39 In our study, the Black ncAS MSM venue network was more diffuse compared with the White ncAS MSM venue network. This translates into more locations that need to be targeted to reach Black MSM for PrEP implementation efforts. These results support the findings by Tieu et al. who reported small elusive sexual networks among Black HIV-negative MSM.10 The authors studied 1349 community-recruited MSM as part of the HIV Prevention Trials Network 061. The study demonstrated that sexual risk was associated with a larger network size. In another study, among HIV-positive Black MSM in Jackson, Mississippi, Oster et al. also reported a high degree of connectedness through a small number of venues for meeting partners.24
Network analysis proved beneficial in identifying PrEP awareness dissemination targets among MSM in this study. In St. Louis, the use of online-based HIV prevention messaging is likely the best approach to engage MSM and has been found to be acceptable.40 Reaching out to these platforms and creating regional PrEP messaging campaigns would likely be time efficient for public health officials.41 In addition, such campaigns can potentially bolster ongoing local prevention efforts, such as HIV testing, risk reduction counseling, and condom promotion and distribution. We found that physical venues hypothesized to play a central role in where sexual encounters occur in St. Louis, such as the bathhouse, were not present in the analysis, whereas new locations emerged (i.e., skating rink).
We promote the use of network analysis early in public health planning to optimize PrEP implementation. With many applications for HIV prevention, network analysis was used mainly as a tool to study HIV, STI, and other communicable disease transmission and has since evolved into an approach for developing and implementing health interventions for incidence reduction.10,23–28,42,43 Network methodologies have the potential to improve the efficiency of PrEP programmatic interventions to have the most impact on the HIV epidemic. The Centers for Disease Control and Prevention has made it a top priority to increase PrEP awareness and access for Black and Latino MSM with over $216 million allocated to 90 community-based organizations in 50 geographic areas, with high HIV prevalence and incidence, within 26 states in 2015 (PS15-1502: Comprehensive High-Impact HIV Prevention Projects for Community-Based Organizations).44 Network analysis does not require time-intensive data collection and this would be an opportune time to incorporate this underutilized methodology to map out potential information transmission networks early in the programmatic process.12 Network analysis can identify community opinion leaders and/or venues to maximize efforts, whether it be identifying a central node for at-risk behavior venues or where the most people could be reached with minimal effort or both.
This study has the limitations of a small sample size, social desirability and recall biases with self-reported sexual risk behaviors and serostatus, and selection bias from the areas recruited. However, recruitment was from a wide array of physical and virtual locations known to be used by the local MSM population. Given that the majority of recruited participants were at risk for HIV, based on their reported sexual risk behavior and HIV-negative serostatus, our findings have implications for PrEP programming geared toward the population sampled.
Future local studies can expand on this venue-based network analysis and see how individuals are linked to each other in terms of sexual transmission of HIV/STIs using phylogenetic studies, social network formation, and brokers in communication networks for information diffusion.45 A larger study would reveal a more extensive list of venues and could potentially identify hidden networks among each racial group.
Conclusion
This study demonstrates the use of network analysis in the armamentarium of methodologies to guide public health biomedical HIV prevention implementation. The technique may aid efficient PrEP outreach to facilitate the application of evidence-based interventions that promote and maintain PrEP use with the hopes of halting HIV transmission among at-risk sexual networks.
Acknowledgments
R.R.P. is supported by the Washington University Institute of Clinical and Translational Sciences grant UL1TR000448, subaward KL2TR000450, from the National Center for Advancing Translational Sciences of the National Institutes of Health, the National Institutes of Health grant R25MH83620, and the Washington University in St. Louis Institute for Public Health. P.A.C. is supported by the National Institute of Allergy and Infectious Diseases (1K23AI096923).
Disclaimer
Previous presentations of parts of these data were made at the 8th Annual Conference on the Science of Dissemination and Implementation, Washington, DC, December 14, 2015.45
Author Disclosure Statement
R.R.P. has received compensation from Gilead Sciences for consulting. K.H.M. has received unrestricted research grants from Gilead Sciences and ViiV Healthcare. No competing financial interests exist for any of the other authors.
References
- 1.Centers for Disease Control and Prevention: HIV Surveillance Report: Diagnoses of HIV infection in the United States and dependent areas, 2014. 2015. Available at www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-us.pdf Accessed September1, 2016
- 2.Centers for Disease Control and Prevention: Trends in U.S. HIV diagnoses, 2005–2014. 2016. Available at www.cdc.gov/nchhstp/newsroom/docs/factsheets/hiv-data-trends-fact-sheet-508.pdf Accessed September1, 2016
- 3.Centers for Disease Control and Prevention: HIV infection risk, prevention, and testing behaviors among men who have sex with men—National HIV behavioral surveillance, 20 U.S. cities, 2014. HIV Surveillance Special Report. 2016. Available at www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-hssr-nhbs-msm-2014.pdf Accessed September1, 2016
- 4.Mannheimer SB, Wang L, Wilton L, et al. : Infrequent HIV testing and late HIV diagnosis are common among a cohort of black men who have sex with men in 6 US cities. J Acquir Immune Defic Syndr 2014;67:438–445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention: Monitoring selected national HIV prevention and care objectives by using HIV surveillance data: United States and 6 dependent areas—2013. HIV Surveillance Supplemental Report. 2015. Available at www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-SurveillanceReport_vol20_no2.pdf Accessed September1, 2016
- 6.Millett GA, Flores SA, Peterson JL, Bakeman R: Explaining disparities in HIV infection among black and white men who have sex with men: A meta-analysis of HIV risk behaviors. AIDS 2007;21:2083–2091 [DOI] [PubMed] [Google Scholar]
- 7.Millett GA, Peterson JL, Flores SA, et al. : Comparisons of disparities and risks of HIV infection in Black and other men who have sex with men in Canada, UK, and USA: A meta-analysis. Lancet 2012;380:341–348 [DOI] [PubMed] [Google Scholar]
- 8.Clerkin EM, Newcomb ME, Mustanski B: Unpacking the racial disparity in HIV rates: The effect of race on risky sexual behavior among Black young men who have sex with men (YMSM). J Behav Med 2011;34:237–243 [DOI] [PubMed] [Google Scholar]
- 9.Newcomb ME, Mustanski B: Racial differences in same-race partnering and the effects of sexual partnership characteristics on HIV Risk in MSM: A prospective sexual diary study. J Acquir Immune Defic Syndr 2013;62:329–333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tieu HV, Liu TY, Hussen S, et al. : Sexual networks and HIV risk among black men who have sex with men in 6 U.S. cities. PLoS One 2015;10:e0134085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention: Lifetime Risk of HIV Diagnosis: Half of black gay men and a quarter of Latino gay men projected to be diagnosed within their lifetime. 2016. Available at www.cdc.gov/nchhstp/newsroom/2016/croi-press-release-risk.html Accessed October1, 2016
- 12.Valente TW, Palinkas LA, Czaja S, et al. : Social network analysis for program implementation. PLoS One 2015;10:e0131712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maulsby C, Millett G, Lindsey K, et al. : A systematic review of HIV interventions for black men who have sex with men (MSM). BMC Public Health 2013;13:625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grant RM, Lama JR, Anderson PL, et al. : Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med 2010;363:2587–2599 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention: Preexposure prophylaxis for the prevention of HIV infection in the United States-2014. A clinical practice guideline. 2014. Available at www.cdc.gov/hiv/pdf/prepguidelines2014.pdf Accessed September8, 2016
- 16.Marrazzo JM, del Rio C, Holtgrave DR, et al. : HIV prevention in clinical care settings: 2014 recommendations of the International Antiviral Society-USA Panel. JAMA 2014;312:390–409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith DK, Van H.andel M, Wolitski RJ, et al. : Vital signs: Estimated percentages and numbers of adults with indications for preexposure prophylaxis to prevent HIV acquisition—United States, 2015. MMWR Morb Mortal Wkly Rep 2015;64:1291–1295 [DOI] [PubMed] [Google Scholar]
- 18.Bush S, Magnuson D, Rawlings KM, et al. : Racial characteristics of FTC/TDF for pre-exposure prophylaxis (PrEP) users in the US. Abstract number 2651. Oral presentation at: ASM Microbe, Boston, Massachusetts, June16–20, 2016 [Google Scholar]
- 19.Wheeler DP, Fields S, Nelson LE, et al. : HPTN 073: PrEP uptake and use by Black men who have sex with men in 3 US cities. Abstract number 883LB. Poster presentation at: Conference on Retroviruses and Opportunistic Infections, Boston, Massachusetts, February22–25, 2016 [Google Scholar]
- 20.Doblecki-Lewis S, Liu A, Feaster D, et al. : Healthcare access and PrEP continuation in San Francisco and Miami after the US PrEP Demo Project. J Acquir Immune Defic Syndr 2017;74:531–538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aarons GA, Hurlburt M, Horwitz SM: Advancing a conceptual model of evidence-based practice implementation in public service sectors. Adm Policy Ment Health 2011;38:4–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Saldana L, Chamberlain P, Wang W, Hendricks Brown C: Predicting program start-up using the stages of implementation measure. Adm Policy Ment Health 2012;39:419–425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hurt CB, Beagle S, Leone PA, et al. : Investigating a sexual network of black men who have sex with men: Implications for transmission and prevention of HIV infection in the United States. J Acquir Immune Defic Syndr 2012;61:515–521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oster AM, Wejnert C, Mena LA, et al. : Network analysis among HIV-infected young black men who have sex with men demonstrates high connectedness around few venues. Sex Transm Dis 2013;40:206–212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Holloway IW, Rice E, Kipke MD: Venue-based network analysis to inform HIV prevention efforts among young gay, bisexual, and other men who have sex with men. Prev Sci 2014;15:419–427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Smith AM, Grierson J, Wain D, et al. : Associations between the sexual behaviour of men who have sex with men and the structure and composition of their social networks. Sex Transm Infect 2004;80:455–458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shah NS, Iveniuk J, Muth SQ, et al. : Structural bridging network position is associated with HIV status in a younger Black men who have sex with men epidemic. AIDS Behav 2014;18:335–345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Amirkhanian YA: Social networks, sexual networks and HIV risk in men who have sex with men. Curr HIV/AIDS Rep 2014;11:81–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Luke DA: Viewing dissemination and implementation research through a network lens. In: Dissemination and Implementation Research in Health: Translating Science to Practice. Edited by Brownson RC, Colditz GA, Proctor EK. New York: Oxford University Press, 2012, pp 154–191 [Google Scholar]
- 30.Wasserman S, Faust K: Social Network Analysis: Methods and Applications. New York: Cambridge University Press, 1994 [Google Scholar]
- 31.Newman ME, Girvan M: Finding and evaluating community structure in networks. Phys Rev E Stat Nonlin Soft Matter Phys 2004;69(2 Pt 2):026113. [DOI] [PubMed] [Google Scholar]
- 32.Pons P, Latapy M: Computing communities in large networks using random walks. J Graph Algorithm App 2006;10:191–218 [Google Scholar]
- 33.R Core Team: R: A language and environment for statistical computing. R Foundation for Statistical Computing. Vienna, Austria: Available at www.R-project.org Accessed September16, 2017 [Google Scholar]
- 34.Nunn AS, Brinkley-Rubinstein L, Oldenburg CE, et al. : Defining the HIV pre-exposure prophylaxis care continuum. AIDS 2017;31:731–734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kelley CF, Kahle E, Siegler A, et al. : Applying a PrEP continuum of care for men who have sex with men in Atlanta, Georgia. Clin Infect Dis 2015;61:1590–1597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Patel R, Wrigley D, Mayer K, Powderly W: High linkage to PrEP care in St. Louis using a pilot linkage to PrEP care community partnership program. Abstract number 5113. Poster presentation at: The 2015 National HIV Prevention Conference, Atlanta, Georgia, December6–9, 2015 [Google Scholar]
- 37.Missouri Department of Health and Senior Services: HIV preexposure prophylaxis (PrEP). Available at http://health.mo.gov/living/healthcondiseases/communicable/hivaids/prep.php Accessed July3, 2017
- 38.Patel RR, Harrison LC, Patel VV, et al. : HIV pre-exposure prophylaxis programs incorporating social applications can reach at-risk men who have sex with men for successful linkage to care in Missouri, USA. J Assoc Nurses AIDS Care 2017;28:428–430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chan PA, Mena L, Patel R, et al. : Retention in care outcomes for HIV pre-exposure prophylaxis implementation programmes among men who have sex with men in three US cities. J Int AIDS Soc 2016;19:20903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Holloway IW, Rice E, Gibbs J, et al. : Acceptability of smartphone application-based HIV prevention among young men who have sex with men. AIDS Behav 2014;18:285–296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chan PA, Towey C, Poceta J, et al. : Online hookup sites for meeting sexual partners among men who have sex with men in Rhode Island, 2013: A call for public health action. Public Health Rep 2016;131:264–271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.De P, Singh AE, Wong T, et al. : Sexual network analysis of a gonorrhoea outbreak. Sex Transm Infect 2004;80:280–285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bradshaw D, Raghwani J, Jacka B, et al. : Venue-based networks may underpin HCV transmissions amongst HIV-infected gay and bisexual men. PLoS One 2016;11:e0162002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Centers for Disease Control and Prevention: Organizations funded under PS15-1502: Comprehensive High-Impact HIV Prevention Projects for Community-Based Organizations. 2015. Available at /www.cdc.gov/hiv/pdf/funding/announcements/ps15-1502/cdc-hiv-ps15-1502-funding—by-state-and-grantee.pdf Accessed August20, 2016
- 45.Patel R, Goodenberger K, Tooba R, et al. : The promise of network science for clinical D&I—The use of social network analysis to identify dissemination targets and enhance D&I research study recruitment for pre-exposure prophylaxis for HIV (PrEP) among men who have sex with men. Abstract number 556. Poster presentation at: The 8th Annual Conference on the Science of Dissemination and Implementation, Washington, DC, December14–15, 2016 [Google Scholar]