Supplemental Digital Content is available in the text.
Key Words: surgery, mortality, weekend care, weekend effect
Abstract
Background:
An association between weekend health care delivery and poor outcomes has become known as the “weekend effect.” Evidence for such an association among surgery patients has not previously been synthesized.
Objective:
To systematically review associations between weekend surgical care and postoperative mortality.
Methods:
We searched PubMed, EMBASE, and references of relevant articles for studies that compared postoperative mortality either; (1) according to the day of the week of surgery for elective operations, or (2) according to weekend versus weekday admission for urgent/emergent operations. Odds ratios (ORs) and corresponding 95% confidence intervals (CIs) for postoperative mortality (≤90 d or inpatient mortality) were pooled using random-effects models.
Results:
Among 4027 citations identified, 10 elective surgery studies and 19 urgent/emergent surgery studies with a total of >6,685,970 and >1,424,316 patients, respectively, met the inclusion criteria. Pooled odds of mortality following elective surgery rose in a graded manner as the day of the week of surgery approached the weekend [Monday OR=1 (reference); Tuesday OR=1.04 (95% CI=0.97–1.11); Wednesday OR=1.08 (95% CI=0.98–1.19); Thursday OR=1.12 (95% CI=1.03–1.22); Friday OR=1.24 (95% CI=1.10–1.38)]. Mortality was also higher among patients who underwent urgent/emergent surgery after admission on the weekend relative to admission on weekdays (OR=1.27; 95% CI=1.08–1.49).
Conclusions:
Postoperative mortality rises as the day of the week of elective surgery approaches the weekend, and is higher after admission for urgent/emergent surgery on the weekend compared with weekdays. Future research should focus on clarifying underlying causes of this association and potentially mitigating its impact.
Weekend health care within numerous medical disciplines has been associated with poorer outcomes relative to care provided during regular weekday hours.1–4 This phenomenon has become known as the “weekend effect” and has been speculated to result from decreased staffing and resource availability, leading to shortfalls in care, and poor outcomes.2–7 Several recent cohort studies have assessed for a weekend effect among surgery patients by examining associations between weekend care and postoperative mortality.3,6,8–12 However, variability in study design and findings has led to uncertainty about the consistency and generalizability of such associations.
An assessment of the weekend effect among surgery patients is complicated by differences in temporal risk profiles and institutional care patterns for patients undergoing elective versus urgent or emergent surgical procedures. Elective surgeries are uncommonly performed on the weekend at many hospitals,3,6,13 and risk profiles of elective cases that are selected for weekend operations may differ relative to weekday procedures.3,13 As a result, direct comparisons of outcomes for weekend versus weekday elective surgeries are highly vulnerable to selection bias. This selection bias can be mitigated by comparing outcomes for elective procedures performed early in the week (eg, Monday) to those performed late in the week (eg, Friday), where the early postoperative period (a known interval of vulnerability to complications14) falls on the weekend.
Patients undergoing urgent or emergent surgeries are also potentially affected by a weekend effect. However, an assessment for a weekend effect in this population must consider the potential impact of inpatient preoperative care quality and delays to urgent or emergent surgery on outcomes. Examining urgent or emergent surgery outcomes by day of admission (weekend vs. weekday), rather than day of surgery, accounts for such potential differences between weekend and weekday care.
Recognizing the important differences between elective versus urgent or emergent surgery pertaining to a potential weekend effect, we performed a systematic review and 2 separate meta-analyses to assess: (1) mortality among patients undergoing elective operations according to the day of the week of surgery from Monday to Friday; and (2) mortality among patients undergoing urgent or emergent operations according to admission on the weekend versus weekdays.
METHODS
We conducted a systematic review and meta-analysis following a preestablished protocol and reported our work in accordance with the meta-analysis of observational studies in epidemiology (MOOSE) guidelines.15
Search Strategy and Selection Criteria
We searched PubMed, Ovid EMBASE, and references of included articles without date or language restrictions. Conference abstracts and unpublished data were permitted for inclusion. The complete search strategy is shown in eTable 1 (Supplemental Digital Content 1, http://links.lww.com/MLR/B514). The search was last updated on December 3, 2016. Two reviewers (S.A.S. and J.M.Y.) selected articles independently and in duplicate. κ statistics with 95% confidence intervals (CIs) were calculated to quantify agreement between reviewers. Studies were included if the following criteria were met: (1) the study reported on patients who underwent surgery stratified by day of operation (from Monday to Friday) for elective cases or day of admission (weekend vs. weekday) for urgent or emergent cases; (2) the study reported an odds ratio (OR) for short-term mortality (with its associated 95% CI), or data that permitted calculation of these values. Studies that reported on nonoperative endoscopy and/or interventional radiologic procedures performed outside of the operating room were excluded. Studies that reported results for a subset of patients that met these inclusion/exclusion criteria, but did not report the number of patients in the relevant subset were included since the metaanalytic techniques utilized here assigned study weights based on the SE of the effect estimate (ie, from the 95% CI of an OR) rather than from the number of patients in individual studies.
Urgent/emergent surgery was defined as any surgery that due to its acuity, was performed during the same hospital visit that the decision to proceed with surgery was made, or after an outpatient waiting interval of <48 hours. Surgeries classified as urgent or emergent by study authors without specifying a definition or for which such categorization could easily be inferred (eg, appendectomies for appendicitis) were classified as urgent/emergent. Studies not meeting the definition for urgent/emergent were classified as elective. The weekend was defined as calendar days Saturday and Sunday. Studies with a weekend definition that differed by no more than 8 hours at the beginning and/or end of this interval or that contained holidays were included. Short-term mortality was defined as death before discharge from hospital following surgery or within a fixed time frame ≤90 days following surgery.
Data Extraction
Two reviewers (S.A.S. and J.M.Y.) extracted data independently and in duplicate using a prespecified data extraction form. Discrepancies between reviewers were resolved by consensus. Extracted data elements included: study design, source of cohort, total number of patients, patient characteristics, study characteristics, type of surgeries performed, crude mortality rate, and unadjusted or adjusted ORs with associated 95% CIs for mortality for weekends or individual weekdays as applicable.
Risk of Bias Assessment
The risk of bias of included studies was assessed using a component-based approach16 incorporating elements of the quality assessment tool developed by Hayden et al.17 Studies were scored as “high,” “low,” or “unclear” risk of bias for each of the following domains: participation, attrition, outcome measurement, statistical analysis, and confounding measure and account. The specific criteria applied to the assessment of risk of bias within each of the specified domains are shown in eTable 2 (Supplemental Digital Content 1, http://links.lww.com/MLR/B514). Bias in prognostic factor measurement (eg, day of surgery or weekend vs. weekday classification) was not included given the lack of plausible mechanisms for systematic misclassification of exposures.
Data Synthesis and Analysis
Meta-analyses were conducted separately for studies of elective surgery patients and studies of urgent/emergent surgery patients. ORs for mortality were pooled on the log scale for each individual day of surgery from Tuesday to Friday relative to Monday for elective surgery and for weekend admissions relative to weekday admissions for urgent/emergent surgery. All analyses were performed using the DerSimonian and Laird random-effects models.18 If multiple estimates were reported from a single study, the most adjusted estimate was used in meta-analyses. When not reported by study authors, ORs with 95% CIs for short-term mortality were calculated from crude study data. In circumstances where studies reported ORs (and 95% CIs) for mortality using a reference group different than that specified here (eg, Friday as a reference group in elective surgery instead of Monday), we derived measures according to the desired reference group mathematically.19
Statistical heterogeneity was quantified using I2 inconsistency statistics, which quantify the percentage of interstudy variability due to factors other than chance or sampling variation.20 Stratified and metaregression analyses were performed to explore whether several prespecified covariates explained interstudy variation. These covariates included hospital teaching status, surgical specialty, geographic area of the source population of the cohort (Europe vs. North America vs. other), crude mortality rate of the cohort (dichotomized as high or low based on the median-crude mortality of included studies), each of the risk of bias domains noted previously, and degree of covariate adjustment (dichotomized as high or low based on the median number of covariates for which adjustment was undertaken). For stratified and metaregression analyses by surgical specialty, in circumstances where individual studies reported multiple OR estimates deemed pertinent to a single surgical specialty (eg, ORs for hip replacements and knee replacements deemed pertinent to orthopedic surgery), the single study OR estimates were combined using fixed-effect models and then pooled with ORs from other studies in random-effects analyses.
In circumstances where >1 study reported data from the same cohort (introducing potential for duplicate inclusion of patients), only the largest cohort was included in the main analysis. Sensitivity analyses were performed by repeating analyses after substituting the smaller potentially overlapping cohorts for the larger cohort included in the main analysis.21 In a circumstance where results from the same cohort were published twice with differing levels of statistical adjustment,6,22 the most adjusted estimate was included in the meta-analysis. However, pertinent subgroup estimates from the less adjusted study7 were included in our stratified analysis and metaregression when not reported within the more adjusted study.22 We assessed for small study effects potentially indicative of publication bias using funnel plots and the Egger funnel plot asymmetry test.23 In the presence of funnel plot asymmetry, we conducted Duval and Tweedie24 trim and fill analyses, which adjust for small study effects potentially due to publication bias. Analyses were conducted using Stata version 14.1 (Stata Corp. LP, College Station, TX).
RESULTS
Study Identification
Among 4027 citations identified, 29 studies were included in the systematic review (see eFig. 1, Supplemental Digital Content 1, http://links.lww.com/MLR/B514, for details of the study selection process). These included 10 studies with a total of >6,685,970 elective surgery patients3,13,22,25–31 and 19 studies with a total of >1,424,316 urgent/emergent surgery patients8–12,32–45 (exact sample sizes not calculable as 2 studies did not specify the number of patients included in the pertinent analyses29,34). Data from 13 elective surgery cohorts and 24 urgent/emergent surgery cohorts were analyzed as 6 studies3,9,32,34,35,40 reported on >1 cohort meeting our inclusion criteria. The κ statistic for interrater agreement for inclusion during title and abstract screening was 0.66 (95% CI=0.60–0.72), and that during full-text review was 0.93 (95% CI=0.89–0.98).
Characteristics of Included Studies
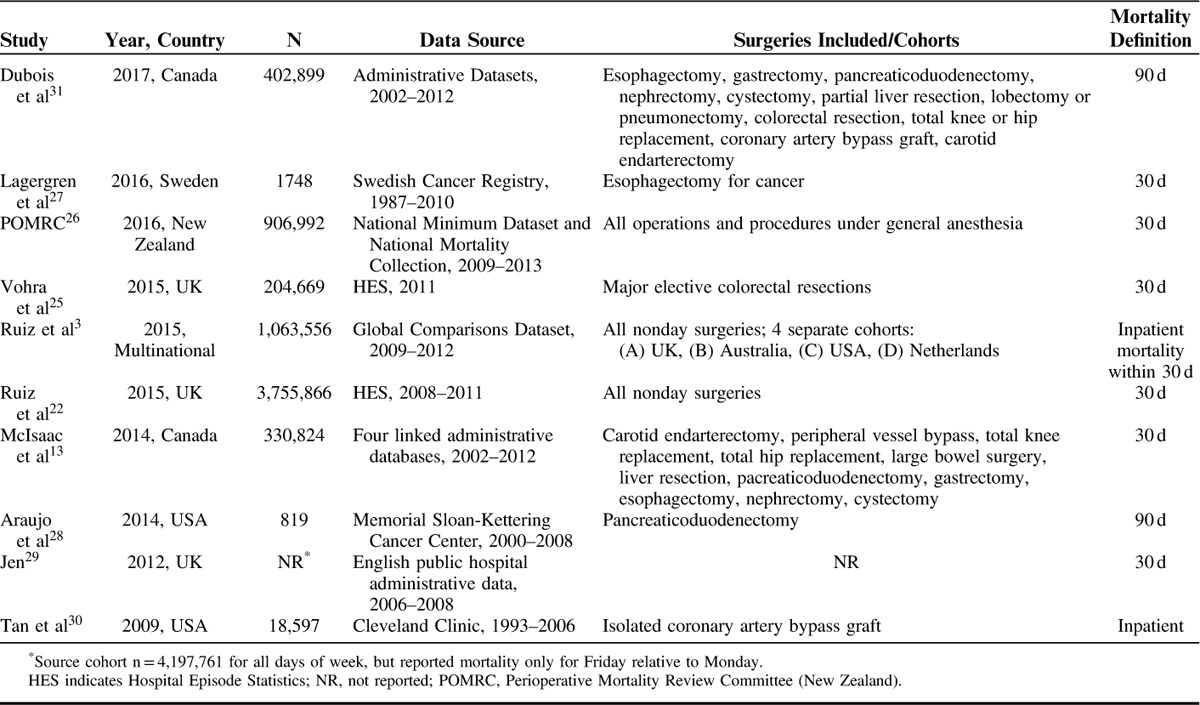
The 10 studies identified that reported on elective surgery patients had sample sizes ranging from 819 to 3,755,866 patients (Table 1). Eight of the studies were multicenter3,13,22,25–27,29,31 and 2 were single center.28,30 Four studies were conducted in Europe,22,25,27,29 4 in North America,13,28,30,31 1 in New Zealand,26 and 1 included data from 4 countries.3 The studies included patients from a diverse range of surgical specialties. Seven studies reported on 30-day mortality,3,13,22,25–27,29 2 on 90-day mortality,28,31 and 1 on inpatient mortality.30
TABLE 1.
Characteristics of Elective Surgery Studies
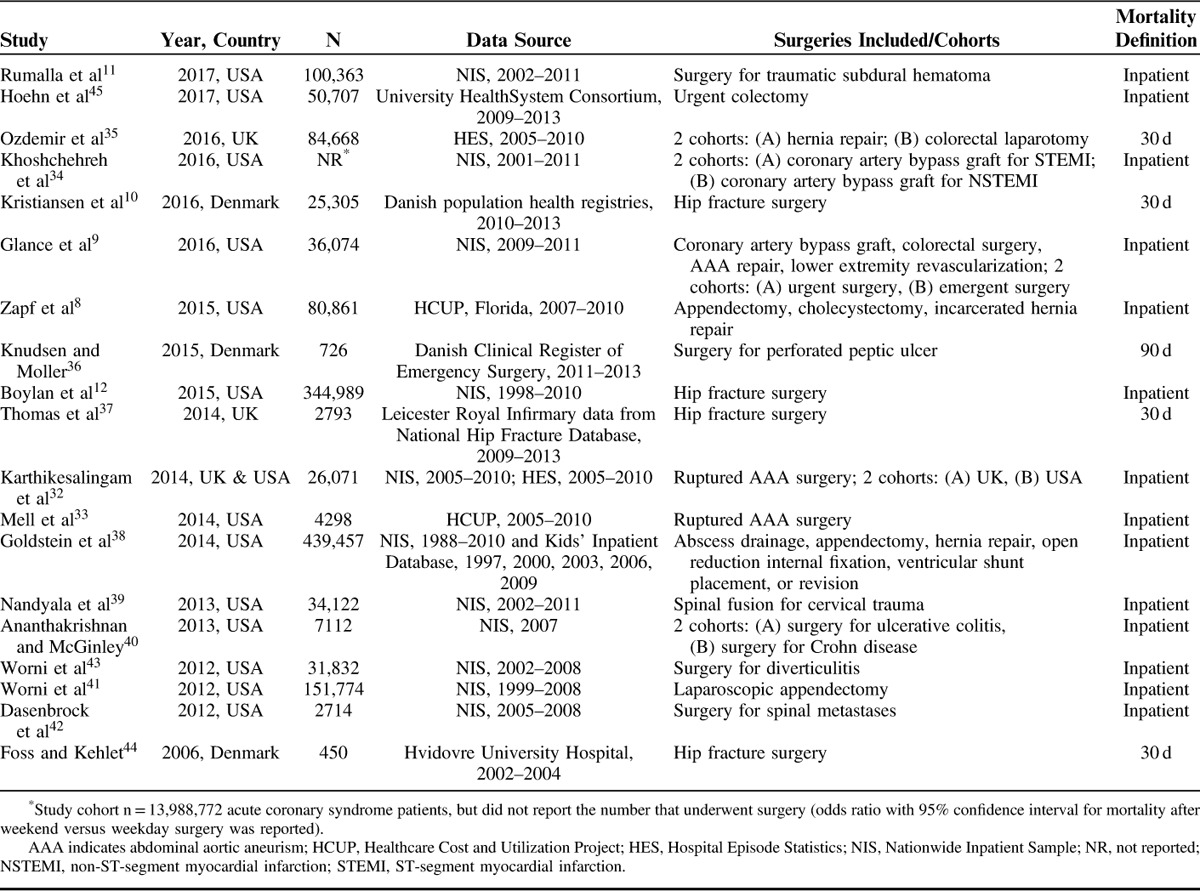
The 19 studies that reported on urgent or emergent surgery patients (Table 2) had sample sizes ranging from 450 to 439,457 patients. Seventeen of the studies were multicenter8–12,32–36,38–43,45 and 2 were single center.37,44 Thirteen studies were conducted in the United States,8,9,11,12,33,34,38–43,45 5 were conducted in Europe,10,35–37,44 and 1 included patients from both Europe and the United States.32 The surgical specialties represented included general surgery, orthopedic surgery, vascular surgery, cardiac surgery, and neurosurgery. Fourteen studies reported on inpatient mortality,8,9,11,12,32–34,38–43,45 4 on 30-day mortality,10,35,37,44 and 1 on 90-day mortality.36
TABLE 2.
Characteristics of Urgent/Emergent Surgery Studies
Risk of Bias Assessment
The majority of included studies were classified as low risk (as specified in eTable 2, Supplemental Digital Content 1, http://links.lww.com/MLR/B514) for participation bias, attrition bias, outcome measurement bias, and statistical analysis bias (eTable 3, Supplemental Digital Content 1, http://links.lww.com/MLR/B514). Fifteen of the 29 included studies were classified as low risk for bias in confounding measurement and account.
Mortality by Day of the Week of Elective Surgery
Data from 10 of the elective surgery cohorts, including >5,718,008 patients, were pooled in our main elective surgery analysis (Fig. 1). The pooled ORs for mortality after elective surgery relative to surgery on Monday were 1.04 (95% CI=0.97–1.11; I2=32.0%) for Tuesday surgery, 1.08 (95% CI=0.98–1.19; I2=53.7%) for Wednesday surgery, 1.12 (95% CI=1.03–1.22; I2=44.5%) for Thursday surgery, and 1.24 (95% CI=1.10–1.38; I2=82.6%) for Friday surgery. The 3 cohorts excluded from the main analysis reported on patients that were potentially included in larger studies. In a series of sensitivity analyses where data from each of the excluded cohorts was substituted in the place of data from the larger included studies, similar patterns of sequentially higher odds estimates for mortality as the week progressed from Monday to Friday were noted (eFigs. 2–4, Supplemental Digital Content 1, http://links.lww.com/MLR/B514).
FIGURE 1.
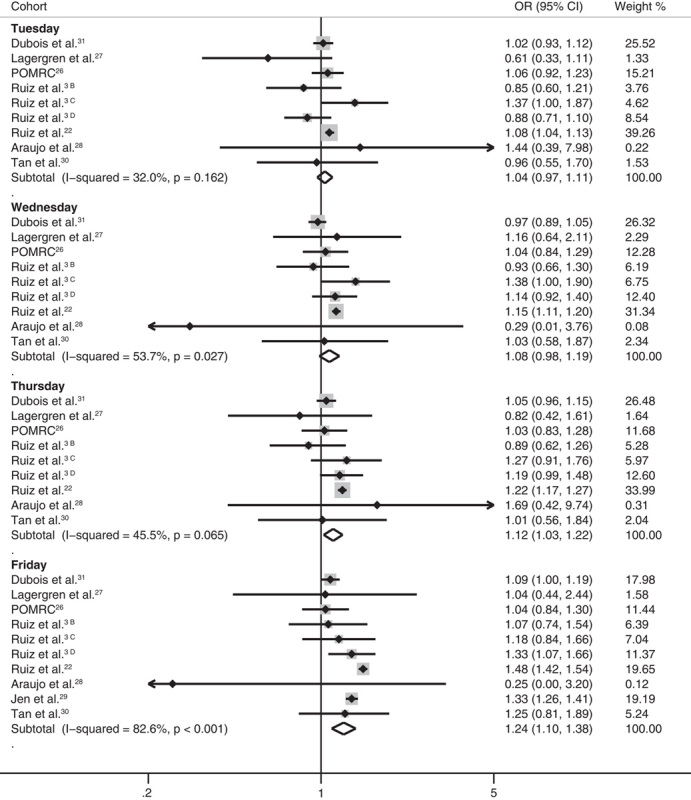
Forest plots of ORs for mortality after elective surgery on Tuesday, Wednesday, Thursday, and Friday relative to Monday. B,C,D Discrete cohorts from single study as specified in Table 1. Solid diamonds represent point estimates, lines represent 95% CIs, shaded boxes represent percentage weight contributed by the study, and open diamonds represent pooled estimates (centered on the point estimate with a length representing the pooled 95% CI). CI indicates confidence interval; OR, odds ratio.
Mortality for Weekend Versus Weekday Admission for Urgent/Emergent Surgery
Data from 20 urgent/emergent surgery cohorts including >1,303,083 patients were pooled in the main urgent/emergent surgery analysis (Fig. 2). The pooled OR for mortality after urgent/emergent surgery for patients admitted on the weekend relative to weekdays was 1.27 (95% CI=1.08–1.49; I2=96.9%). The 4 cohorts excluded from the main analysis reported on patients that were potentially included in larger studies. In a series of sensitivity analyses where data from each of the excluded cohorts was substituted in the place of data from the larger included studies, significant associations between weekend admission and mortality remained present (eFigs. 5–7, Supplemental Digital Content 1, http://links.lww.com/MLR/B514).
FIGURE 2.
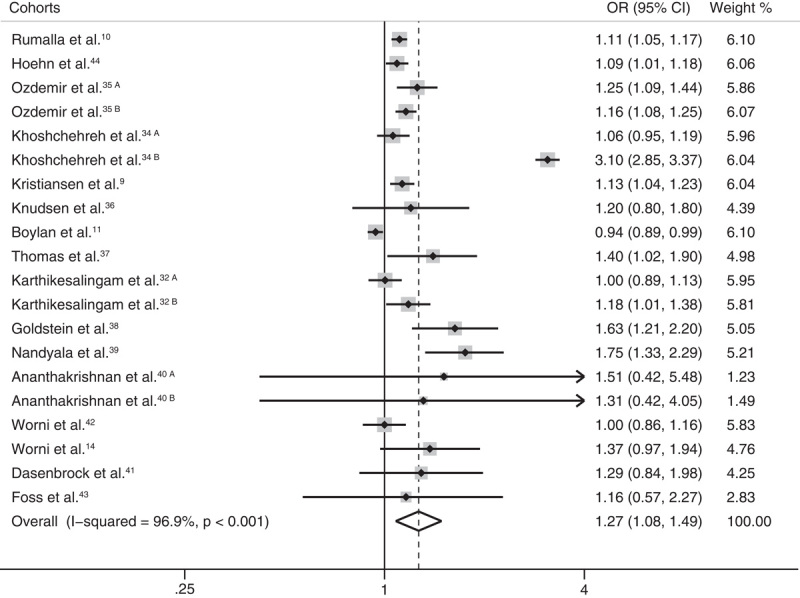
Forest plot of OR for mortality after admission for urgent/emergent surgery on the weekend relative to weekdays. A,B Discrete cohorts from single studies as specified in Table 2. Solid diamonds represent point estimates, lines represent 95% CIs, shaded boxes represent percentage weight contributed by the study, and open diamond represents pooled estimate (centered on the point estimate with a length representing the pooled 95% CI). CI indicates confidence interval; OR, odds ratio.
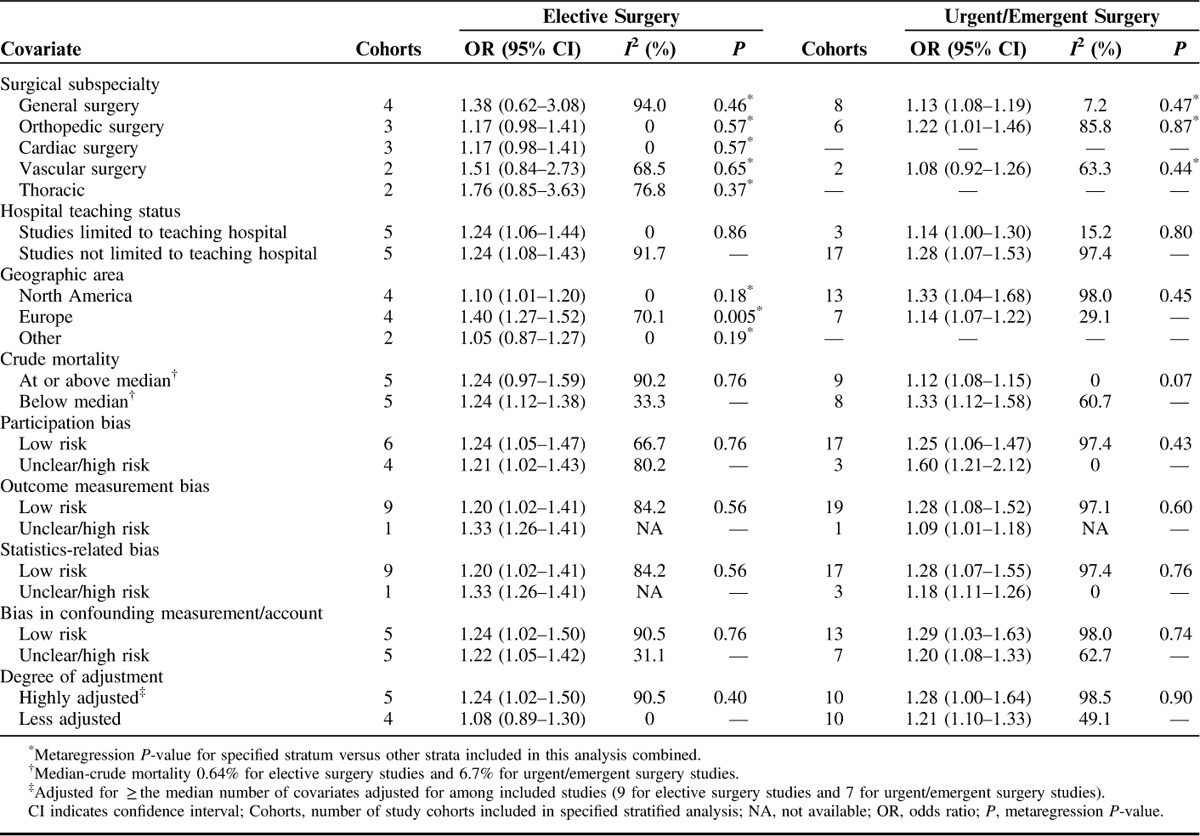
Stratified Meta-Analysis and Metaregression
To explore the heterogeneity observed in the associations with mortality for elective surgeries on Friday relative to Monday and for urgent/emergent surgeries on the weekend relative to weekdays, we performed a series of stratified analyses and metaregression analyses across several clinical and study design features (Table 3). For elective surgeries, the OR for mortality after surgery on Friday relative to Monday was higher among studies conducted in Europe (OR=1.40; 95% CI=1.27–1.52; I2=70.1%) than studies conducted in North America (OR=1.10; 95% CI=1.01–1.20; I2=0%) or other geographic areas (OR=1.05; 95% CI=0.87–1.27; I2=0%) (metaregression P-value for Europe relative to North America/other combined=0.005). For urgent/emergent surgeries, the OR for mortality after admission for surgery on the weekend relative to weekdays was higher among studies with a low-crude mortality rate (OR=1.33; 95% CI=1.12–1.58; I2=60.7%) than among studies with a high-crude mortality rate (OR=1.12; 95% CI=1.08–1.15; I2=0%) (metaregression P=0.07) after studies were dichotomized based on crude mortality (at or above median vs. below median). No other statistically significant differences were noted between strata for either the elective surgery or urgent/emergent surgery analyses based on hospital teaching status, surgical specialty, risk of bias, or degree of statistical adjustment.
TABLE 3.
Stratified Analyses and Metaregression of Elective Surgery Mortality Data for Friday Relative to Monday Operations and of Urgent/Emergent Surgery Mortality Data for Weekend Admission Relative to Weekday Admission
Analysis for Small Study Effects
Funnel plots of ORs for mortality after elective surgery on Friday relative to Monday and for urgent/emergent surgery admission on the weekend relative to weekdays are shown in eFigure 8 (Supplemental Digital Content 1, http://links.lww.com/MLR/B514). The result of the Egger test was not statistically significant for the elective surgery analysis (P=0.12) or the urgent/emergent surgery analysis (P=0.54). Duval and Tweedie trim and fill analyses, which adjust for small study effects potentially due to publication bias, computed an adjusted OR for mortality after elective surgery on Friday relative to Monday of 1.24 (95% CI=1.10–1.38) and an adjusted OR for mortality after weekend admission relative to weekday admission for surgery of 1.27 (95% CI=1.08–1.49). These results are identical to the results computed in the main analyses.
DISCUSSION
In this systematic review and meta-analysis, we synthesized data from 29 studies that included over 8 million patients to examine for associations suggestive of a weekend effect impacting surgical care. We found that short-term mortality estimates after weekday elective surgery increased in a graded manner as the weekend approached and were statistically significantly higher for surgery on Thursday and Friday, relative to surgery on Monday. Specifically, we observed that the pooled odds of short-term mortality after elective surgery on Thursday and Friday were 12% and 24% higher, respectively, than for surgery conducted on Monday. We also found that admission for urgent or emergent surgery on the weekend was associated with 27% higher pooled odds of short-term mortality relative to admission for such surgery on weekdays. Collectively, these findings lend support to the presence of a weekend effect in surgical care.
We conducted our analyses among elective surgical patients by comparing mortality after surgery on each day of the week from Monday to Friday, rather than for weekends versus weekdays, to mitigate the potential for selection bias in comparisons. Weekend elective surgeries are uncommon at many institutions,3,6,13 and patients selected for such procedures may have differing levels of surgical urgency and risk profiles relative to weekday elective patients.3,13 The causality of the strong associations between weekend elective surgery and postoperative mortality demonstrated in previous analyses may therefore be questioned.3,6,13 Our study, which showed that postoperative mortality is higher for surgeries performed late in the week, relative to early in the week, is much less vulnerable to selection bias and still provides support for a weekend effect as patients who undergo surgery late in the week experience the most critical period of their postoperative course14 on the weekend.
We observed statistical heterogeneity in our analyses of both elective and urgent/emergent surgery. Such heterogeneity is not uncommon in meta-analyses of cohort studies where populations and designs are variable. We examined potential underlying reasons for this heterogeneity by performing stratified analysis and metaregression based on hospital teaching status, surgical specialty, geographic area of the source cohort, crude mortality rate of the cohort, and various measures of risk of bias. We explored these variables based on clinical plausibility and the ability to ascertain them from the published studies. For example, it is plausible that teaching hospitals may have better in-house weekend staffing, which could mitigate a weekend effect, or that certain surgical subspecialties are more vulnerable to a weekend effect based on more urgent care requirements in the early postoperative course. Despite the plausibility of such relationships we did not identify evidence of modification of the association between weekend care and mortality based on hospital teaching status, surgical subspecialty, or any of the various measures of bias assessed. In our stratified analyses and metaregression, Friday relative to Monday elective operations were associated with higher odds of short-term mortality in European studies than in studies conducted in North America or other regions of the world. In our urgent/emergent analysis, weekend relative to weekday admission for surgery was associated with higher odds of short-term mortality among cohorts with low-crude mortality rates (used as a marker of surgical risk within the cohort) relative to cohorts with high-crude mortality rates. These finding should be interpreted with caution however, as differences between strata could be representative of other study level differences between patient groups studied, rather than differences attributable to the variables in question. Given the heterogeneity we observed, it remains possible that the weekend effect is modified by factors that were not assessed in our study.
Although this is the largest and most comprehensive analysis of the subject of the weekend effect in surgery, it has several important limitations. First, the majority of the included cohort studies were conducted in the United States or the United Kingdom. This limits the generalizability of our findings to institutions located elsewhere in the world. Second, although we assessed the influence of adjustment for potential confounding variables in our metaregression analyses and noted no evidence of modification of mortality estimates, it remains possible that residual unmeasured confounding could have biased our results. Finally, and most importantly, our results demonstrate the presence of an association between weekend surgical care and mortality, but do not and cannot indicate the underlying cause for such an association given the observational design of the included studies.
Others have suggested6,38 that the weekend effect may result from systemic differences at institutional levels in the manner in which care is delivered on weekends relative to weekdays.
We agree that such a mechanism is plausible. Differences in hospital staffing and resource availability on the weekends relative to weekdays could, for example, lead to suboptimal care and poor outcomes. The hypothesis that the weekend effect results from institutional factors is supported by the results of one study of surgery patients that used extended median length of stay as a surrogate marker for the weekend effect and suggested that it could be overcome by the presence of specific hospital resources such as increased nurse-to-bed ratio, full adoption of an electronic medical record, a home health program, and a pain management program.46 However, we caution against overinterpretation of the findings of our meta-analysis by policy makers. Data from studies of nonsurgical patients have suggested that the weekend effect may be mediated in part by differences in admission acuity, differences in case-mix, or administrative data coding discrepancies.47,48 One study included in our analysis did find that admission acuity was higher and the probability of operative management was lower for traumatic subdural hematoma patients admitted on weekends relative to weekdays.11 Whether or not similar differences in weekend versus weekday acuity or probability of operative management exist for other groups of surgery patients is unknown. Further study in this area is necessary to identify causality, by characterizing avoidable deaths and developing and testing effective strategies to mitigate preventable deaths at times and places when availability of care providers is reduced. Such knowledge will be important to inform any future policy changes addressing surgical care on weekends and to avoid the considerable controversy that has surrounded administrative decisions prompted by prior reports of this association.49
CONCLUSIONS
This systematic review and meta-analysis of 29 studies that includes over 8 million patients demonstrates that mortality estimates increase in a graded manner after elective surgery for each day of the week approaching the weekend and are higher after admission for urgent or emergent surgery on the weekend relative to weekdays. These results are consistent with the presence of a weekend effect in surgical care. Future studies should focus on clarifying the contributing factors to poor outcomes and developing strategies to potentially improve safety and mitigate adverse events associated with weekend surgical care.
Supplementary Material
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.
ACKNOWLEGMENTS
The authors thank Diane Lorenzetti (Department of Community Health Sciences, University of Calgary, Calgary, Canada) for her advice with our search strategy as well as Dr Takuya Ishikawa (Department of Medicine, Foothills Medical Centre, Calgary, Canada) for screening Japanese articles for potential inclusion.
Footnotes
S.A.S. and J.M.Y. contributed equally.
K.L.T. is supported by fellowship awards from Canadian Institutes of Health Research and Alberta Innovates—Health Solutions.
The authors declare no conflict of interest.
REFERENCES
- 1.Sorita A, Ahmed A, Starr SR, et al. Off-hour presentation and outcomes in patients with acute myocardial infarction: systematic review and meta-analysis. BMJ. 2014;348:f7393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cavallazzi R, Marik PE, Hirani A, et al. Association between time of admission to the ICU and mortality: a systematic review and metaanalysis. Chest. 2010;138:68–75. [DOI] [PubMed] [Google Scholar]
- 3.Ruiz M, Bottle A, Aylin PP. The Global Comparators project: international comparison of 30-day in-hospital mortality by day of the week. BMJ Qual Saf. 2015;24:492–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345:663–668. [DOI] [PubMed] [Google Scholar]
- 5.Zare MM, Itani KM, Schifftner TL, et al. Mortality after nonemergent major surgery performed on Friday versus Monday through Wednesday. Ann Surg. 2007;246:866–874. [DOI] [PubMed] [Google Scholar]
- 6.Aylin P, Alexandrescu R, Jen MH, et al. Day of week of procedure and 30 day mortality for elective surgery: retrospective analysis of hospital episode statistics. BMJ. 2013;346:f2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aylin P. Making sense of the evidence for the “weekend effect”. BMJ. 2015;351:h4652. [DOI] [PubMed] [Google Scholar]
- 8.Zapf MAC, Kothari AN, Markossian T, et al. The weekend effect in urgent general operative procedures. Surgery. 2015;158:508–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Glance LG, Osler T, Li Y, et al. Outcomes are worse in US patients undergoing surgery on weekends compared with weekdays. Med Care. 2016;54:608–615. [DOI] [PubMed] [Google Scholar]
- 10.Kristiansen NS, Kristensen PK, Norgard BM, et al. Off-hours admission and quality of hip fracture care: a nationwide cohort study of performance measures and 30-day mortality. Int J Qual Health Care. 2016;28:324–331. [DOI] [PubMed] [Google Scholar]
- 11.Rumalla K, Reddy AY, Bijilani P, et al. Surgical treatment of traumatic subdural hematoma: weekday versus weekend admission. Ann Neurol. 2015;78:324–331. [Google Scholar]
- 12.Boylan MR, Rosenbaum J, Adler A, et al. Hip fracture and the weekend effect: does weekend admission affect patient outcomes? Am J Orthop. 2015;44:458–464. [PubMed] [Google Scholar]
- 13.McIsaac DI, Bryson GL, van Walraven C. Elective, major noncardiac surgery on the weekend: a population-based cohort study of 30-day mortality. Med Care. 2014;52:557–564. [DOI] [PubMed] [Google Scholar]
- 14.Cavaliere F, Conti G, Costa R, et al. Intensive care after elective surgery: a survey on 30-day postoperative mortality and morbidity. Minerva Anestesiol. 2008;74:459–468. [PubMed] [Google Scholar]
- 15.Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008–2012. [DOI] [PubMed] [Google Scholar]
- 16.Egger M, Smith GD, Altman DG. Systematic Reviews in Health Care : Meta-Analysis in Context, 2nd ed London: BMJ; 2001. [Google Scholar]
- 17.Hayden JA, Cote P, Bombardier C. Evaluation of the quality of prognosis studies in systematic reviews. Ann Intern Med. 2006;144:427–437. [DOI] [PubMed] [Google Scholar]
- 18.DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–188. [DOI] [PubMed] [Google Scholar]
- 19.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. The Cochrane Collaboration. 2011. Version 5.1.0. [Google Scholar]
- 20.Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.von Elm E, Poglia G, Walder B, et al. Different patterns of duplicate publication: an analysis of articles used in systematic reviews. JAMA. 2004;291:974–980. [DOI] [PubMed] [Google Scholar]
- 22.Ruiz M, Bottle A, Aylin PP. Exploring the impact of consultants’ experience on hospital mortality by day of the week: a retrospective analysis of hospital episode statistics. BMJ Qual Saf. 2015;25:337–344. [DOI] [PubMed] [Google Scholar]
- 23.Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. [DOI] [PubMed] [Google Scholar]
- 25.Vohra RS, Pinkney T, Evison F, et al. Influence of day of surgery on mortality following elective colorectal resections. Br J Surg. 2015;102:1272–1277. [DOI] [PubMed] [Google Scholar]
- 26.Perioperative Mortality Review Committee (POMRC). Perioperative mortality in New Zealand: fifth report of the perioperative mortality review committee. Wellington: Health Quality & Safety Commission; 2016. [Google Scholar]
- 27.Lagergren J, Mattsson F, Lagergren P. Weekday of oesophageal cancer surgery in relation to early postoperative outcomes in a nationwide Swedish cohort study. BMJ Open. 2016;6:e011097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Araujo RL, Karkar AM, Allen PJ, et al. Timing of elective surgery as a perioperative outcome variable: analysis of pancreaticoduodenectomy. HPB (Oxford). 2014;16:250–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jen MH. Day of week of procedure and 30-day in-hospital mortality for elective surgery. Value Health. 2012;15:A81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tan PJ, Xu M, Sessler DI, et al. Operation timing does not affect outcome after coronary artery bypass graft surgery. Anesthesiology. 2009;111:785–789. [DOI] [PubMed] [Google Scholar]
- 31.Dubois L, Vogt K, Vinden C, et al. Association between day of the week of elective surgery and postoperative mortality. CMAJ. 2017;189:E303–E309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Karthikesalingam A, Holt PJ, Vidal-Diez A, et al. Mortality from ruptured abdominal aortic aneurysms: clinical lessons from a comparison of outcomes in England and the USA. Lancet. 2014;383:963–969. [DOI] [PubMed] [Google Scholar]
- 33.Mell MW, Wang NE, Morrison DE, et al. Interfacility transfer and mortality for patients with ruptured abdominal aortic aneurysm. J Vasc Surg. 2014;60:553–557. [DOI] [PubMed] [Google Scholar]
- 34.Khoshchehreh M, Groves EM, Tehrani D, et al. Changes in mortality on weekend versus weekday admissions for acute coronary syndrome in the United States over the past decade. Int J Cardiol. 2016;210:164–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ozdemir BA, Sinha S, Karthikesalingam A, et al. Mortality of emergency general surgical patients and associations with hospital structures and processes. Br J Anaesth. 2016;116:54–62. [DOI] [PubMed] [Google Scholar]
- 36.Knudsen NV, Moller MH. Association of mortality with out-of-hours admission in patients with perforated peptic ulcer. Acta Anaesthesiol Scand. 2015;59:248–254. [DOI] [PubMed] [Google Scholar]
- 37.Thomas CJ, Smith RP, Uzoigwe CE, et al. The weekend effect: short-term mortality following admission with a hip fracture. Bone Joint J. 2014;96-B:373–378. [DOI] [PubMed] [Google Scholar]
- 38.Goldstein SD, Papandria DJ, Aboagye J, et al. The “weekend effect” in pediatric surgery—increased mortality for children undergoing urgent surgery during the weekend. J Pediatr Surg. 2014;49:1087–1091. [DOI] [PubMed] [Google Scholar]
- 39.Nandyala SV, Marquez-Lara A, Fineberg SJ, et al. Comparison of perioperative outcomes and cost of spinal fusion for cervical trauma: weekday versus weekend admissions. Spine (Phila Pa 1976). 2013;38:2178–2183. [DOI] [PubMed] [Google Scholar]
- 40.Ananthakrishnan AN, McGinley EL. Weekend hospitalisations and post-operative complications following urgent surgery for ulcerative colitis and Crohn’s disease. Aliment Pharmacol Ther. 2013;37:895–904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Worni M, Ostbye T, Gandhi M, et al. Laparoscopic appendectomy outcomes on the weekend and during the week are no different: a national study of 151,774 patients. World J Surg. 2012;36:1527–1533. [DOI] [PubMed] [Google Scholar]
- 42.Dasenbrock HH, Pradilla G, Witham TF, et al. The impact of weekend hospital admission on the timing of intervention and outcomes after surgery for spinal metastases. Neurosurgery. 2012;70:586–593. [DOI] [PubMed] [Google Scholar]
- 43.Worni M, Schudel IM, Ostbye T, et al. Worse outcomes in patients undergoing urgent surgery for left-sided diverticulitis admitted on weekends vs weekdays: a population-based study of 31 832 patients. Arch Surg. 2012;147:649–655. [DOI] [PubMed] [Google Scholar]
- 44.Foss NB, Kehlet H. Short-term mortality in hip fracture patients admitted during weekends and holidays. Br J Anaesth. 2006;96:450–454. [DOI] [PubMed] [Google Scholar]
- 45.Hoehn RS, Hanseman DJ, Chang AL, et al. Surgeon characteristics supersede hospital characteristics in mortality after urgent colectomy. J Gastrointest Surg. 2017;21:23–32. [DOI] [PubMed] [Google Scholar]
- 46.Kothari AN, Zapf MAC, Blackwell RH, et al. Components of hospital perioperative infrastructure can overcome the weekend effect in urgent general surgery procedures. Ann Surg. 2015;262:683–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Meacock R, Anselmi L, Kristensen SR, et al. Higher mortality rates amongst emergency patients admitted to hospital at weekends reflect a lower probability of admission. J Health Serv Res Policy. 2017;22:17–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Li L, Rothwell PM, Oxford Vascular S. Biases in detection of apparent “weekend effect” on outcome with administrative coding data: population based study of stroke. BMJ. 2016;353:i2648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Craven D. The statistical sins of Jeremy Hunt. BMJ. 2015;351:h6358. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's website, www.lww-medicalcare.com.


