Abstract
Objective:
To determine if participation in an online resilience program impacts resilience, stress, and somatic symptoms.
Methods:
Approximately 600 enrollees in the meQuilibrium resilience program received a series of brief, individually prescribed video, and text training modules in a user-friendly format. Regression models tested how time in the program affected change in resilience from baseline and how changes in resilience affected change in stress and reported symptoms.
Results:
A significant dose–response was detected, where increases in the time spent in training corresponded to greater improvements in resilience. Degree of change in resilience predicted the magnitude of reduction in stress and symptoms. Participants with the lowest resilience level at baseline experienced greater improvements.
Conclusion:
Interaction with the online resilience training program had a positive effect on resilience, stress, and symptoms in proportion to the time of use.
Learning Objectives
Become familiar with current evidence linking employee resilience with work-related outcomes, including previous resilience intervention studies.
Describe the online resilience program described in the study, along with the evaluation methods and outcomes used.
Summarize the improvements achieved and the implications for employee resilience interventions.
A growing body of evidence connects employee resilience with important work-related outcomes. As examples, resilience is associated with lower levels of perceived stress,1,2 higher job satisfaction,3,4 and fewer stress-related symptoms (such as chronic pain,5 headaches,6,7and poor sleep quality3). Higher resilience also corresponds to higher levels of productivity, fewer absences, and a lower likelihood of quitting.3,8,9 Additionally, resilience is protective against high-strain jobs, where workers face greater stress from high demands and lower job discretion.3
Scientific understanding of the scope of resilience has evolved over the past decade.10 While early studies focused on resilience as an inherent ability to overcome severe trauma11–14 more recent studies highlighted its value in managing daily stressors.15–17 Further, resilience has become recognized less as an innate characteristic and more as a set of learnable skills that mitigate the experience of stress and speed productive responses when setbacks occur.10,18 Specifically, resilient employees have the ability to apply these positive mental skills—which include emotion control, optimism, self-efficacy, and problem-solving—to remain psychologically robust when faced with challenges or adversity, diminishing the negative effects of stress.8,10,19
For these reasons, academic interest in the psychological construct of resilience has grown over recent years, from approximately 30 peer-reviewed studies per year before 2000, to over 900 in 2016. Among US employers, resilience training is one of fastest growing interventions offered to employees.16,20 Similar to efforts by the military to build resilience in active duty soldiers and family members,21,22 employers are focusing on developing resilience among employees as a competitive advantage.15,17,23–26
A published review of resilience intervention studies between 2003 and 2014 reported inconsistent results, but concluded that some training programs do improve personal resilience and well-being.16 This may in part be due to variance across these studies in how resilience is defined operationally. Several showed positive improvements in resilience following in-person training, specifically in psychological metrics (eg, stress, anxiety),27–29 physical/biological metrics (symptoms and blood markers of stress),30,31 and performance.31,32 One noted limitation was that most interventions were of short duration, delivered over a period of weeks, with limited follow-up periods. Delivery of in-person programs also has disadvantages, including limits on user access (ceilings on number of participants, required participation at a specific time or location, availability of a trained instructor) and higher costs due to low scalability. Authors of the review suggested the need to provide tailored interventions focused on “individual needs.”16
Online delivery of resilience training has the potential of delivering effective training in a more flexible, personalized, and cost-effective way. Only a few studies of online interventions have been conducted, with inconsistent results. One had a very small number of participants and did not measure a significant impact.33 Another did not focus specifically on resilience, and instead used sentiment analysis (answers to open-ended questions are categorized via algorithms as happy or unhappy) to impute increases in positive feelings.34 Thus far, evidence regarding online interventions has been limited.
The current investigation is intended to add to existing literature, by reporting prepost findings for 600 participants in an online resilience program over a period of up to 2.5 years.
METHODS
Subjects
Approximately 600 subjects were recruited to complete a follow-up assessment in October, 2016. Individuals in the employer-sponsored meQuilibrium program who had been enrolled for at least 3 months at the time of recruitment were eligible to complete the follow-up assessment in return for a $15 (Amazon) gift card. Over 50,000 participants were enrolled at the time of recruitment. To maximize variance in exposure to the intervention, initial invitations were stratified across randomly selected program enrollees within three utilization groups (low, medium, and high utilization since enrollment). A total of 699 participants completed the assessment. A total of 65 participants were removed from the final sample due to response patterns to two items that indicated inattention to the survey content. An additional 43 users were removed due to missing values on one or more measures.
Measures
All participants had previously completed a 91-question assessment upon enrollment into the resilience program. Many of the assessment questions drive operational, programmatic rules, such as targeted content and communication. Others form the following scales which we used in the study:
MeQuilibrium Resilience Measure (Resilience)
This 16-item scale consists of four subscales of four items each. Items were scored on a Likert scale on degree of agreement, ranging in value from 1 to 5. Overall resilience was measured as the average score across the 16 items. Internal consistency reliability for the overall scale is α = 0.94. Labels and internal consistency reliability for each of the subscales were as follows: problem solving (α = 0.82), emotion control (α = 0.86), optimism (α = 0.88), and self-efficacy (α = 0.81). Further information about this scale has been reported elsewhere.3
Perceived Stress Measure (Stress)
An 11-item scale was used to measure perceived stress. This scale correlates strongly (0.73) with the Perceived Stress Scale35 and has high internal consistency reliability (α = 0.92). Questions focused on the experience of worry and stress (examples: I have difficulty balancing competing demands in my life; there are times I feel sick with worry). Responses measure degree of agreement, with numbers ranging from 1 to 5. Overall stress was measured as the average score across the 11 items.
Somatic Symptom Measure (Somatic Symptoms)
This scale included four questions regarding self-reported experience of back pain, headaches, neck and shoulder tension, and fatigue. Question responses measured reported frequency of symptoms, with numbers ranging from 1 to 5. Overall symptom frequency was measured as the average score across the four items. This scale has an internal consistency reliability of α = 0.78.
Demographics
Respondents were asked to provide age and sex.
Program Participation (Minutes)
Because each participant receives a tailored prescription for content, participation was measured by time engaged with the product since their enrollment, rather than completion of specific modules or activities. Engagement time only included active time in the product performing activities, not time logged in.
Chesapeake IRB approved this study.
Intervention
The meQuilibrium resilience training program offers digital coaching with over 40 modules based on the science of positive psychology, cognitive behavioral therapy, and mindfulness. A personalized program is tailored for each user based on their specific needs. Based on answers to an intake assessment, the program identifies the root cause of stress for the individual and defines a highly personalized program of coaching and training to build applicable skills. Specifically, the program identifies “resilience gaps” and, through training and interactive exercises, helps each participant reframe his or her thinking along four key dimensions of mind, body, connection, and surroundings. Each individual curriculum offers both fundamental aspects of resilience as well as personally relevant skills and tools to address identified gaps.
Content is offered through a variety of media, including animated and expert videos, podcasts, interactive elements, Q&As, and text. The content library is flexible and easy to browse or filter by wellbeing categories including: positive outlook, motivation, work/life balance, emotion control, mindfulness, and body.
Users have access to over 50 activities, designed to reinforce learning and encourage practice to achieve new habits. Activities range widely in duration from 2-minute concepts to over 15 minutes for facilitated meditations. Users can select the activities that interest them most and schedule them into their day by using a built-in calendar integration feature. Most users also receive regular email updates and reminders to encourage their ongoing participation.
Analytic Methods
Means and standard deviations were calculated for all measures and changes in measures. To determine the effect of program participation on resilience, an ordinary least-squares regression model was run predicting change in resilience (ΔResilience) from minutes in the program (Minutes). An additional model was run predicting ΔResilience from Minutes, while controlling for age and sex. The square of the Minutes variable was also tested to determine if there was a curvilinear relationship between Minutes and ΔResilience. To assess whether the magnitude of change in resilience was influenced by respondents’ pretraining resilience level, a regression model was run predicting ΔResilience from Minutes, level of pre-resilience (Low Pre-Resilience, a binomial indicating below the median on the initial resilience score), and an interaction term of Minutes × Pre-resilience.
To determine whether changes in resilience were associated with changes in other outcomes, general linear models were run with ΔResilience predicting the dependent variables: change in stress (ΔStress) and change in somatic symptoms (ΔSymptoms). These models were also repeated while controlling for age and sex. All statistical analysis was performed using Stata Software V14.1 (StataCorp LP, College Station, TX).36
Graphic illustrations of regression findings were generated by taking the sum-product of model coefficients and set values of independent variables. For example, to show the expected effect of increasing duration of resilience training, change in resilience was calculated by multiplying the Minutes coefficient by 60-minute increments. In these projections, age was set at the mean and sex was set at 0.5 (half male and half female). Some values were converted to percentages by setting pre-resilience to the scale midpoint (3.0) for all participants and 2.5 for those with low pre-resilience. Similarly, expected changes in stress were estimated by multiplying ΔResilience values by its respective model coefficient. Percentage changes were determined according to the scale mid-point (3.0).
RESULTS
Descriptive statistics for all measures are shown in Table 1. Respondents had an average age of 41 years (s.d. = 11.38). Thirty-two percent of respondents were men, 68% were women. Respondents had been enrolled in the program for an average of 9 months (s.d. = 9 months, median = 4 months). Average duration of active participation across all respondents was 91 minutes (s.d. = 121 minutes, median = 45 minutes). Excluding outliers, some above 1000 minutes, the range of participation was 0 to over 600 minutes. This wide variability reflects the intentional recruitment of individuals with both low and high rates of participation in order to assess dose response.
TABLE 1.
Population Characteristics
| Variable | Mean | Standard Deviation |
| Pre-resilience score | 3.58 | 0.67 |
| Prestress score | 3.35 | 0.88 |
| Presomatic symptom score | 3.33 | 1.04 |
| ΔResilience | 0.03 | 0.56 |
| ΔStress | −0.29 | 0.67 |
| ΔSomatic | −0.22 | 0.82 |
| Minutes in program | 91 | 121 |
| Months since enrolled | 9.28 | 9.55 |
| Age (yrs) | 41.25 | 11.38 |
| Male gender (%) | 32% |
Average pre-resilience score was 3.58 (s.d. = 0.67) on a scale of 1 to 5. This is similar to resilience levels measured in an earlier study (mean = 3.6, s.d. = 0.8).3 Average change in resilience (ΔResilience) across all respondents, regardless of minutes spent in the program or pre-resilience score, was 0.03 (s.d. = 0.56, median = 0.07). This equates to a 1% increase.
Preintervention stress and symptom scores were 3.35 (s.d. = 0.88) and 3.33 (s.d. = 1.04), each on a scale of 1 to 5. Average change in stress (ΔStress) and somatic (ΔSomatic) scores across all respondents were −0.29 (s.d. = 0.67) and −0.22 (s.d. = 0.82), or a decrease of 10% and 7%, respectively.
Program Participation and Changes in Resilience, Stress, and Somatic Symptoms
Participation in meQuilibrium training was significantly related to ΔResilience, such that more minutes of training was associated with greater expected ΔResilience (see Table 2, Model 1). Specifically, each additional hour (60 minutes) of training translated into an expected increase of 1.3% in resilience (0.04 score change divided by a scale score of 3). The effect of Minutes on ΔResilience remained significant controlling for age and sex (see Table 2, Model 2). The square of Minutes was not a significant predictor of ΔResilience in any models, and was excluded from the final versions shown in Table 2. Age was significantly and positively related to changes in resilience.
TABLE 2.
Models Predicting Change in Resilience
| Variable in Model | Model 1 | Model 2 | Model 3 |
| Minutes | 0.00065*** | 0.00048* | 0.00044* |
| Age | 0.00634** | 0.00567** | |
| Gender (Male = 1) | 0.00614 | −0.00117 | |
| Low pre-resilience (1) | 0.275** | ||
| Constant | −0.0306 | −0.279** | −0.371** |
*P < 0.05.
**P < 0.01.
***P < 0.001
Having a lower level of resilience at the time of enrollment was a significant predictor of greater improvements in resilience (see Table 2, Model 3). In other words, those whose score was lower in the pretest could be expected to improve their resilience more for each additional hour of training than those with a higher score on the pretest. Because the interaction between Minutes and Low Pre-Resilience was not significant, it was left out of the final version of Model 3.
An illustration of the expected incremental improvement in resilience across the range of participation is shown in Figure 1, where—across all participants—those participating for 3 hours could expect a 2% improvement (from a scale mid-point of 3) in resilience score, while those participating for 8 hours could expect an improvement of 7% in resilience score. For those whose pretraining resilience was below the median, those participating for 3 hours could expect a 9% improvement (from a scale mid-point of 2.5) in resilience score, while those participating for 8 hours could expect a 14% improvement in resilience score.
FIGURE 1.
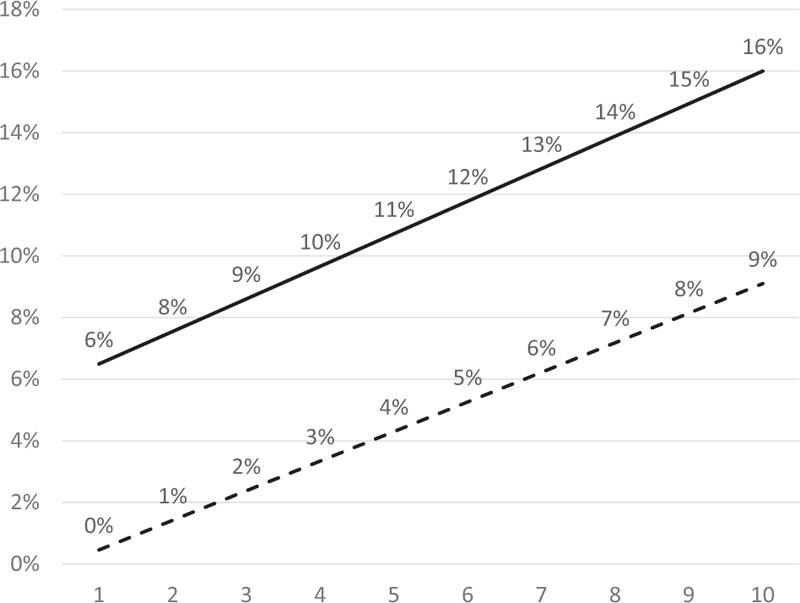
Percent change in resilience score by hours of resilience training. Legend: hours of participation. All participants - - -, participants with low pre-resilience – —.
Increases in resilience scores corresponded to improvements in reported stress and symptoms, controlling for age and sex (see Table 3). Neither age nor sex contributed significantly to these models or altered the coefficients to any noticeable degree. The negative linear relationship between ΔResilience and both outcomes (ΔStress and ΔSomatic) results in an expected incremental reduction in stress and reported symptoms across the range of ΔResilience.
TABLE 3.
Models Predicting Change in Stress and Somatic Symptoms
| Variable in Model | ΔStress | ΔSomatic |
| ΔResilience | −0.432** | −0.347** |
| Age | 0.0050* | −0.0008 |
| Gender (male = 1) | −0.0714 | −0.124 |
| Constant | 0.0936 | 0.277* |
*P < 0.05.
**P < 0.001.
In running calculations (not shown) based on these models, across all participants and using expected improvements in resilience for someone participating for 0 to 10 hours of training, expected decreases in stress would range from 0% to 13%, and expected decreases in somatic symptoms would range from 0% to 9%.
Because those having Low Pre-Resilience could be expected to have larger changes in resilience with each hour of training, predicted reductions in stress and symptoms are also larger. As shown in Figure 2, after 5 hours of training, those with lower pretraining resilience could be expected to report a 15% and 11% decrease in ΔStress and ΔSomatic, respectively.
FIGURE 2.
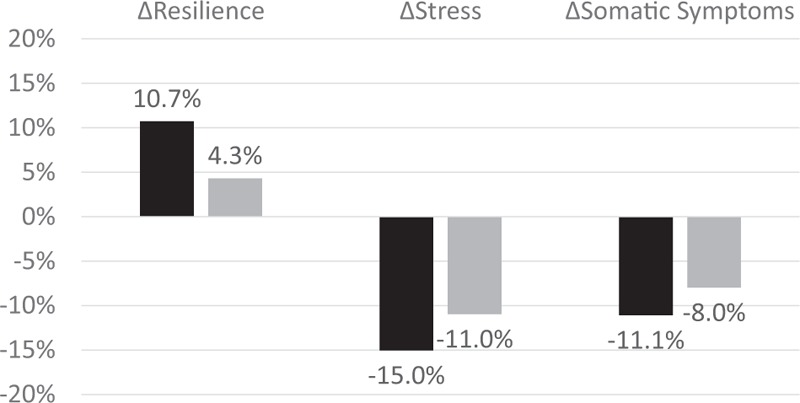
Expected change in stress and symptoms after 5 hours of training.
DISCUSSION
Participants in this study experienced significant improvements in resilience following participation in online training. This finding is consistent with some other resilience studies, where training improved resilience and stress.16,30,32,33 This investigation also found that the improvement in outcomes occurred in direct association with the amount of time spent in online resilience training. Further, reductions in reported stress and somatic symptoms occurred in proportion to improvements in resilience. The relationships were linear, indicating an incremental benefit to training over time.
This dose–response effect supports hypotheses that (a) online resilience training focused on mental skills such as reframing of negative thoughts, self-awareness of emotion, and alternatives for managing difficult challenges, can improve resilience, and (b) that more training equates to greater changes in resilience. This is the first study to document how the degree of exposure to an online resilience intervention influences outcomes, rather than treatment versus control. These results suggest that, logically, those who participate more and return to training modules more often achieve the greatest improvements.
Additionally, the more resilience improved, the more stress and stress-related symptoms declined. This is consistent with previous research indicating that greater resilience is associated with lower levels of stress and stress-related symptoms.1,2,5,6 However, while many previous studies have documented this relationship at a point in time, this study found that changes in resilience corresponded to changes in these outcomes.
Perhaps not surprisingly, those whose resilience was low before enrolling in training (thus, having greater room for improvement) demonstrated greater improvements in resilience, and correspondingly greater decreases in stress, with each additional hour of training. This suggests that those in greatest need of resilience skills received the greatest benefit. This is an important finding indicating that those low in resilience actually utilize the offered program.
Because recruitment did not require a set amount of participation, study participants varied significantly in their use of the online training tools. This provided the ideal mechanism for testing dose–response. Of note, some improvements in resilience occurred even when the duration of training was short. This may reflect the design of the skills training, where specific content segments, including video, were brief but targeted. Also, because skills are assigned individually, emphasizing content areas having greatest relevance to existing gaps in resilience, even initial training sessions had a measurable effect.
Low resilience increases the risk of depression, job burnout, absenteeism, and job impairment, especially in difficult work environments.3 In this study, those with the lowest initial resilience experienced the greatest expected improvements in resilience, stress and somatic symptoms. Logically, low-resilience populations would benefit most from targeted interventions. However, a previous study found that low resilience cannot be presumed based on other known characteristics—notably, almost half of those with college education or high income have below-average resilience.37 This suggests that direct resilience screening could be a beneficial addition to population-based risk-screening programs conducted by employers and health plans. Further, because resilience and its connection to stress has unique value for both health and work performance, resilience training can bridge the efforts of Benefits, Occupational Health and Human Resources in a way that traditional well-being efforts have not.
These findings fill a gap in the literature regarding the effect of ongoing, online resilience training. Previous studies have focused mostly on in-person training programs,16 or those offered over a short-term period, to small groups of employees.33 In the current applied work-setting investigation, participants had training available over an extended period of time (in some cases, years) to be used when it was most relevant and most convenient for their needs and schedules. Because on-demand, online training is customizable and efficient, it can be provided to large numbers of users more economically.
Future research is needed in several areas. First, practitioners need information about the effects of resilience on objective business measures, such as turnover, absence, job performance. Such metrics would further validate self-reported outcomes. Second, it will be important to more carefully investigate the connections between resilience, stress, and work outcomes at the individual level. For example, for a particular person, identify which gaps in resilience affect work the most, and which specific new skills most improve resilience and reduce stress. In addition, questions remain about the positive contagion effects of team resilience. As individuals and leaders become more resilient, how does this affect team and enterprise performance?
Limitations
Participants in this study were self-selected respondents who received an incentive to take a follow-up survey, which limits the generalizability of the results. Any investigation that lacks a control group, as this one did, risks inferring causality when the observed change is due to some other influence. That said, change in resilience was connected to the amount of exposure to the training, not to enrollment, which strengthens the possibility of a causal association.
Another limitation is a lack of specificity of the intervention measure. While the online training is structured to deliver a series of skill-building activities, the specific activities presented to a participant are tailored to each participant's needs. Not all activities have similar duration or complexity. This means the intervention is intentionally not uniform, but instead individualized. Whether some activities have a greater effect than others is not known. Also, while minutes-in-program was the unit of intervention, the longitudinal timeframe of exposure was non-specific because individuals could have had access to the intervention for as little as 2 months or as many as 30 months. Whether the education occurred more or less recently could have impacted its effect.
CONCLUSIONS
Participation in an online resilience training program produced measurable improvements in resilience in proportion to the time spent in training. Improvements in resilience were associated with significant reductions in reported stress and stress-related symptoms. As could be expected, those whose levels of resilience were low before training experienced greater improvements than those whose resilience was high.
Footnotes
Work was funded by meQuilibrium Corporation.
Dr Shatté receives speaking fees for topics related to resilience. Dr Perlman speaks and consults about topics related to resilience. Dr Lynch consults for meQuilibrium and serves on its Board of Directors.
Authors Smith, Shatté, Perlman, Siers, and Lynch have no relationships/conditions/circumstances that present potential conflict of interest.
The JOEM editorial board and planners have no financial interest related to this research.
REFERENCES
- 1.Kwok ST, Wong WN, Lee TY. Effect of resilience on self-perceived stress and experiences on stress symptoms. A surveillance report. Univers J Public Health 2014; 2:64–72. [Google Scholar]
- 2.Beasley M, Thompson T, Davidson J. Resilience in response to life stress: the effects of coping style and cognitive hardiness. Pers Individ Dif 2003; 34:77–95. [Google Scholar]
- 3.Shatté A, Perlman A, Smith B, Lynch WD. The positive effect of resilience on stress and business outcomes in difficult work environments. J Occup Environ Med 2017; 59:135–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Luthans F, Avolio BJ, Avey JB, Norman SM. Positive psychological captial: measurement and relationship with performance and satisfaction. Pers Psychol 2007; 60:541–572. Paper 11. Leadership Institute Faculty Publications. [Google Scholar]
- 5.Bauer H, Emeny RT, Baumert J, Ladwig KH. Resilience moderates the association between chronic pain and depressive symptoms in the elderly. Eur J Pain 2016; 20:1253–1265. [DOI] [PubMed] [Google Scholar]
- 6.Stonnington CM, Kothari DJ, Davis MC. Understanding and promoting resiliency in patients with chronic feadache. Curr Neurol Neurosci Rep 2016; 16:6. [DOI] [PubMed] [Google Scholar]
- 7.Kalapurakkel S, Carpino EA, Lebel A, Simons LE. “Pain can’t stop me”: examining pain self-efficacy and acceptance as resilience processes among youth with chronic headache. J Pediatr Psychol 2015; 40:926–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Avey JB, Reichard RJ, Luthans F, Mhatre KH. Meta-analysis of the impact of positive psychological capital on employee attitudes, behaviors, and performance. Hum Resour Dev Q 2011; 22:127–152. [Google Scholar]
- 9.Luthans F, Avey JB, Avolio BJ, Peterson SJ. The development and resulting performance impact of positive psychological capital. Hum Resour Dev Q 2010; 21:41–67. [Google Scholar]
- 10.Shatté AJ. Pulla V, Shatte’ A, Warren S. Resilience in work and in life. Perspectives on Coping and Resilience. New Delhi: Authors Press Books; 2012. 444–479. [Google Scholar]
- 11.de Terte I, Stephens C, Huddleston L. The development of a three part model of psychological resilience. Stress Health 2014; 30:416–424. [DOI] [PubMed] [Google Scholar]
- 12.Windle G. What is resilience? A review and concept analysis. Rev Clin Gerontol 2011; 21:152–169. [Google Scholar]
- 13.Krell R. Child survivors of the Holocaust—strategies of adaptation. Can J Psychiatry 1993; 38:384–389. [DOI] [PubMed] [Google Scholar]
- 14.Nagata DK, Takeshita YJ. Coping and resilience across generations: Japanese Americans and the World War II internment. Psychoanal Rev 1998; 85:587–613. [PubMed] [Google Scholar]
- 15.Rees CS, Breen LJ, Cusack L, Hegney D. Understanding individual resilience in the workplace: the international collaboration of workforce resilience model. Front Psychol 2015; 6:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Robertson IT, Cooper CL, Sarkar M, Curran T. Resilience training in the workplace from 2003 to 2014: a systematic review. J Occup Organ Psychol 2015; 88:533–562. [Google Scholar]
- 17.Rankin A, Lundberg J, Woltjer R, Rollenhagen C, Hollnagel E. Resilience in everyday operations: a framework for analyzing adaptations in high-risk work. J Cogn Eng Decis Mak 2014; 8:78–97. [Google Scholar]
- 18.Winwood PC, Colon R, McEwen K. A practical measure of workplace resilience: developing the resilience at work scale. J Occup Environ Med 2013; 55:1205–1212. [DOI] [PubMed] [Google Scholar]
- 19.Avey JB, Wernsing TS, Luthans F. Can positive employees help positive organizational change? Impact of psychological capital and emotions on relevant attitudes and behaviors. J Appl Behav Sci 2008; 44:48–70. [Google Scholar]
- 20.Livingston S. Employers turn to resilience-building programs to cut worker stress. Business Insurance; 2015. Available at: http://www.businessinsurance.com/article/20150607/NEWS03/306079981/employers-turn-to-resilience-building-programs-to-cut-worker-stress. Accessed November 4, 2015. [Google Scholar]
- 21.Meadows SO, Miller LL, Robson S. Airman and family resilience: lessons from the scientific literature. RAND Project Air Force Series on Resiliency 2016; Available at: www.rand.org/t/RR106. Accessed September 26, 2016. [PMC free article] [PubMed] [Google Scholar]
- 22.Meredith LS, Sherbourne CD, Gaillot S, et al. Promoting Psychological Resilience in the U.S. Military; 2011. Available at: www.rand.org/content/dam/rand/pubs/.../RAND_MG996.sum.pdf. Accessed September 26, 2016. [PMC free article] [PubMed] [Google Scholar]
- 23.McCann J, Selsky J, Lee J. Building agility resilience and performance in turbulent environments. People Strategy 2009; 32:44–51. [Google Scholar]
- 24.Çam O, Büyükbayram A. The results of nurses’ increasing emotional intelligence and resilience. J Psychiatric Nurs 2015; 6:130–136. [Google Scholar]
- 25.Bardoel EA, Pettit TM, De Cieri H, McMillan L. Employee resilience: an emerging challenge for HRM. Asia Pacific J Hum Resour 2014; 52:279–297. [Google Scholar]
- 26.Spangler NW, Koesten J, Fox MH, Radel J. Employer perceptions of stress and resilience intervention. J Occup Environ Med 2012; 54:1421–1429. [DOI] [PubMed] [Google Scholar]
- 27.Boccuzzi SJ, Wogen J, Fox J, Sung JC, Shah AB, Kim J. Utilization of oral hypoglycemic agents in a drug-insured U.S. population. Diabetes Care 2001; 24:1411–1415. [DOI] [PubMed] [Google Scholar]
- 28.Burton NW, Pakenham KI, Brown WJ. Feasibility and effectiveness of psychosocial resilience training: a pilot study of the READY program. Psychol Health Med 2010; 15:266–277. [DOI] [PubMed] [Google Scholar]
- 29.Bedi A, Schat ACH. Perceptions of organizational politics: a meta-analysis of its attitudinal, health, and behavioural consequences. Can Psychol 2013; 54:246–259. [Google Scholar]
- 30.McCraty R, Atkinson M. Resilience training program reduces physiological and psychological stress in police officers. Global Adv Health Med 2012; 1:44–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arnetz BB, Nevedal DC, Lumley MA, Backman L, Lublin A. Trauma resilience training for police: psychophysiological and performance effects. J Police Crim Psychol 2009; 24:1–9. [Google Scholar]
- 32.Pipe TB, Buchda VL, Launder S, et al. Building personal and professional resources of resilience and agility in the healthcare workplace. Stress Health 2012; 28:11–22. [DOI] [PubMed] [Google Scholar]
- 33.Abbott J-A, Klein B, Hamilton C, Rosenthal A. The impact of online resilience training for sales managers on wellbeing and work performance. Electron J Appl Psychol 2009; 5:89–95. [Google Scholar]
- 34.Carpenter J, Crutchley P, Zilca RD, et al. Seeing the “Big” picture: big data methods for exploring relationships between usage, language, and outcome in internet intervention data. J Med Internet Res 2016; 18:e241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Taylor JM. Psychometric analysis of the ten-item perceived stress scale. Psychol Assess 2015; 27:90–101. [DOI] [PubMed] [Google Scholar]
- 36.Stata Statistical Software [computer program]. Version 14.1. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 37.Shatte’ A, Perlman A, Smith B, Lynch WD. Is Resilience the Result of Higher Education and Income? Investigating the Independent Effect of Resilience on Stress and Work. Boston, MA: New Life Solution, Inc; 2017. [Google Scholar]


