Abstract
Background
Knee laxity in the setting of suspected ACL injury is frequently assessed through physical examination using the Lachman, pivot-shift, and anterior drawer tests. The degree of laxity noted on these examinations may influence treatment decisions and prognosis.
Hypothesis
We hypothesized that increased pre-operative knee laxity would be associated with increased risk of subsequent revision ACL reconstruction and poorer patient-reported outcomes two years postoperatively.
Study design
Cohort study.
Methods
From an ongoing prospective cohort study, 2333 patients who underwent primary isolated ACL reconstruction without collateral or posterior cruciate ligament injury were identified. Patients reported by the operating surgeons as having an International Knee Documentation Committee Grade D Lachman, anterior drawer, or pivot-shift examination were classified as having a high-grade laxity. Multiple logistic regression modeling was used to evaluate whether having high-grade pre-operative laxity was associated with increased odds of undergoing revision ACL reconstruction within two years of the index procedure, controlling for patient age, sex, Marx activity level, level of competition, and graft type. Multiple linear regression modeling was used to evaluate whether having high-grade pre-operative laxity was associated with poorer IKDC or KOOS-QOL scores at a minimum 2 years postoperative, controlling for baseline score, patient age, ethnicity, sex, BMI, marital status, smoking status, sport participation, competition level, Marx activity rating score, graft type, and articular cartilage and meniscus status.
Results
Pre-reconstruction laxity data were available for 2325 patients (99.7%). Two year revision data were available for 2259 patients (96.8%) and patient-reported outcomes were available for 1979 patients (84.8%). High-grade pre-operative laxity was noted in 743 patients (31.9%). The mean postoperative IKDC score was 81.8 ± 15.9 and the mean KOOS-QOL score was 72.0 ± 22.0. The presence of high-grade pre-reconstruction laxity was associated with significantly increased odds of ACL graft revision (OR=1.87, 95% CI: 1.19 – 2.95, p = 0.007). The presence of high-grade pre-reconstruction laxity was not associated with any difference in postoperative IKDC (β = −0.56, p = 0.44) or KOOS-QOL (β = 0.04, p = 0.97).
Conclusion
The presence of high-grade pre-reconstruction knee laxity as assessed by manual physical examination under anesthesia is associated with significantly increased odds of revision ACL surgery, but has no association with patient-reported outcome scores at 2 years following ACL reconstruction.
Introduction
The anterior cruciate ligament (ACL) is frequently injured in young, athletic patient populations. Knee laxity in the setting of a possible ACL injury is frequently assessed by the treating physician through physical examination using the Lachman,33 pivot-shift,8, 16 and anterior drawer tests.20 These physical examination tests frequently demonstrate increased laxity when the ACL is ruptured, but the degree of increased laxity varies from patient to patient. In addition to aiding the physician in correctly diagnosing an ACL injury, the degree of laxity noted on these examinations may influence treatment decisions and prognosis.10, 17
Patients with a relatively high degree of knee laxity after sustaining an ACL injury may represent a subset of patients with concomitant injuries in addition to the ACL tear.19 Prior work has demonstrated that patients with lateral meniscus injury are more likely to demonstrate a higher-grade pivot shift, while medial meniscus injury is associated with increased anterior laxity.24 In addition to meniscal injury, increased laxity may also be associated with increased risk of capsular injury, particularly in the anterolateral aspect of the knee.32, 34 This high-grade laxity patient population may be at increased risk for poor outcome following ACL reconstruction and may therefore represent a population in which the performance of additional stabilization procedures may improve outcomes.17, 30
The purpose of this study was to determine whether high-grade laxity of the injured knee as assessed by the surgeon during an exam under anesthesia prior to ACL reconstruction is associated with revision risk or patient-reported outcomes following ACL reconstruction. We hypothesized that increased pre-operative knee laxity would be associated with increased risk of revision ACL reconstruction and poorer patient-reported outcomes at two years postoperative.
Methods
Patients
Institutional Review Board approval was obtained at participating institutions. From an ongoing prospective cohort study, 2859 patients who underwent ACL reconstruction between 2002 and 2008 were identified. Following exclusion of those undergoing revision surgery (321) or simultaneous bilateral reconstructions (13), as well as those with associated grade 2 or 3 collateral ligament injuries (167) or PCL tears (25); 2333 patients were eligible for inclusion in the study (Figure 1).
Figure 1.
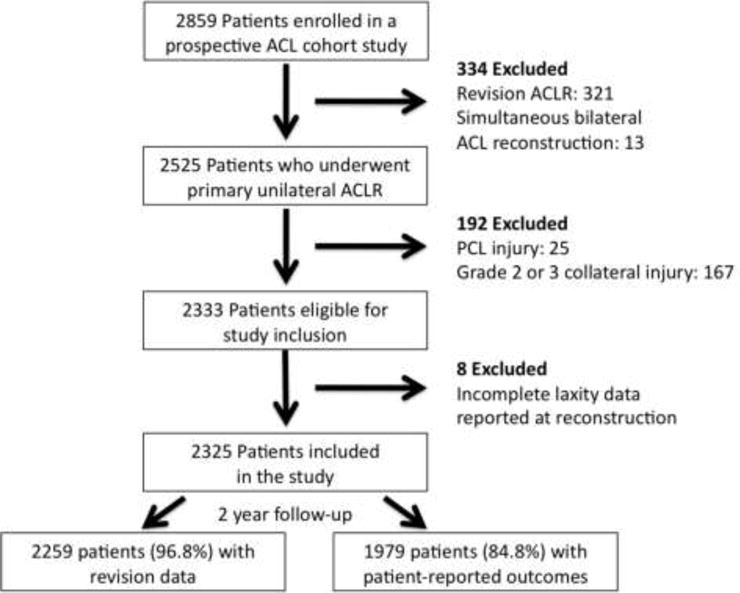
Flowchart demonstrating the selection of patients for study inclusion as well as loss to follow-up.
Data Extraction
Demographic data (age, sex, ethnicity, marital status, and body mass index [BMI]); smoking status; knee laxity during examination under anesthesia prior to ACL reconstruction; sport at injury; level of competition; graft type; information regarding meniscus and articular cartilage status; pre-operative and 2 year postoperative subjective International Knee Documentation Committee (IKDC),11 Knee injury and Osteoarthritis Outcome Score Knee-Related Quality of Life (KOOS-QOL),28 and Marx activity rating scores;23 and the incidence of subsequent revision ACL reconstruction were collected. Ethnicity was recorded and collapsed into the categories of white, black, other, or unknown. Marital status was recorded as single, married, or other. Smoking status was classified as either recent smoker (current smoker or quit within 6 months) or not recent smoker (nonsmoker or quite greater than 6 months ago). Sport at injury was classified as football, soccer, basketball, other, or none. Level of competition was dichotomized as competitive (high school, collegiate, or professional) or recreational. Graft type was classified as patellar tendon autograft, hamstring tendon autograft, quadriceps autograft, or allograft. Hybrid grafts containing both autograft and allograft material were classified as allografts. Meniscus status was determined at the end of the index procedure and classified as intact, meniscectomy (partial or complete), meniscus repair, or untreated stable tear for both the medial and lateral meniscus. Articular cartilage status in each of the three compartments (medial, lateral, patellofemoral) was assessed according to the modified Outerbridge Classification.26 Due to poor reported reliability of differentiation between grade 2 and 3 lesions,22 the grade for each compartment was dichotomized based on the worst score in that compartment as low- (modified Outerbridge 0 or 1) or high-grade (modified Outerbridge 2, 3, or 4) cartilage injury. Knee laxity was assessed according to the IKDC classification system (Table 1).9 Patients noted by the operating surgeon to have a Lachman or anterior drawer examination greater than 10mm different from the contralateral side, or a 3+ pivot-shift were classified as having high-grade laxity.
Table 1.
Interational Knee Documentation Committee (IKDC) Classification of Knee Laxity
| Grade A | Grade B | Grade C | Grade D | |
|---|---|---|---|---|
| Lachman | 0 to 2 mm | 3 to 5 mm | 6 to 10 mm | > 10 mm |
| Anterior Drawer | 0 to 2 mm | 3 to 5 mm | 6 to 10 mm | >10 mm |
| Pivot-Shift | Equal | Glide | Clunk | Gross |
Statistics
Multiple logistic regression modeling was used to evaluate whether high-grade pre-reconstruction laxity was associated with risk of subsequent revision ACL reconstruction. Other variables evaluated as potential confounders or effect modifiers of the relationship of interest included patient age, sex, ethnicity, smoking status, marital status, and BMI; Marx activity rating score at reconstruction; sport at injury; level of competition; graft type; medial and lateral meniscus status; and articular cartilage status. A forward selection modeling procedure was utilized with variables sequentially added to the model and kept in the model if they resulted in a change in the odds ratio of the variable of interest of greater than 0.05. The final model included patient age, sex, BMI, Marx activity rating score, level of competition, and graft type. The presence of interactions between all included predictors was evaluated and no significant interactions were identified. Based on the 8 degrees of freedom required to model these potential predictor variables, the 94 “events” (revision ACL reconstructions) recorded during the 2 year follow-up period provided sufficient power for this analysis. The analysis was repeated using high-grade Lachman, high-grade pivot-shift, and high-grade anterior drawer as the dependent variable.
Multiple linear regression modeling was used to evaluate whether high-grade pre-reconstruction laxity was associated with subjective IKDC score or KOOS-QOL at two years postoperative, controlling for baseline score; patient age, sex, ethnicity, smoking status marital status, and BMI; Marx activity rating score at reconstruction; sport at injury; level of competition; graft type; medial and lateral meniscus status; and articular cartilage status. The presence of interactions between all included predictors was evaluated and no significant interactions were identified. The analysis was repeated using high-grade Lachman, high-grade pivot-shift, and high-grade anterior drawer as the dependent variable.
Results
Complete pre-reconstruction laxity data were available for 2325 patients (99.7%) that formed the study cohort. Baseline patient characteristics are summarized in Table 2. At total of 743 of 2325 patients (32.0%) demonstrated high-grade laxity on at least one physical examination test (Figure 2). High-grade pivot-shift was most common, which occurred in 617 patients (30.0% of females, 23.6% of males), with a high-grade Lachman noted in 334 patients (14.8% of females, 13.9% of males) and a high-grade anterior drawer noted in 233 patients (10.7% of females, 9.4% of males).
Table 2.
Patient Characteristics (n = 2325 patients)
| Age (Mean ± SD) | 26.7 ± 11.1 years |
|---|---|
| Sex | Male: 1302 (56.0%) Female: 1023 (44.0%) |
| Ethnicity | White: 1929 (83.0%) Black: 195 (8.4%) Other: 193 (8.3%) Unknown: 8 (0.3%) |
| Marital Status | Single: 1500 (64.5%) Married: 656 (28.2%) Other: 84 (3.6%) Unknown: 85 (3.7%) |
| Body Mass Index | 25.5 ± 4.9 kg/m2 |
| Smoking Status | Nonsmoker: 2033 (87.4%) Smoker: 280 (12.0%) Unknown: 12 (0.6%) |
| Sport at Injury | Basketball: 508 (21.8%) Football: 299 (12.9%) Soccer: 372 (16.0%) Other: 791 (34.0%) None: 355 (15.3%) |
| Level of Competition | Competitive: 917 (39.4%) Recreational: 1394 (60.0%) Unknown: 14 (0.6%) |
| Graft Type | BTB Autograft: 1037 (44.7%) Hamstring Autograft: 881 (37.9%) Quadriceps Autograft: 3 (0.1%) Allograft: 404 (17.4%) |
| Medial Meniscus Status | Intact: 1389 (59.7%) Meniscectomy: 431 (18.5%) Repaired: 371 (16.0%) Stable Untreated Tear: 130 (5.6%) Unknown: 3 (0.1%) |
| Lateral Meniscus Status | Intact: 1217 (52.3%) Meniscectomy: 688 (29.6%) Repaired: 163 (7.0%) Stable Untreated Tear: 257 (11.1%) |
| Medial Articular Cartilage Status (Modified Outerbridge) | Grade 0 or 1: 1796 (77.2%) Grade2, 3, or 4: 529 (22.8%) |
| Lateral Articular Cartilage Status (Modified Outerbridge) | Grade 0 or 1: 1835 (78.9%) Grade2, 3, or 4: 490 (21.2%) |
| Patellofemoral Articular Cartilage Status (Modified Outerbridge) | Grade 0 or 1: 1858 (79.9%) Grade2, 3, or 4: 467 (20.1%) |
Figure 2.
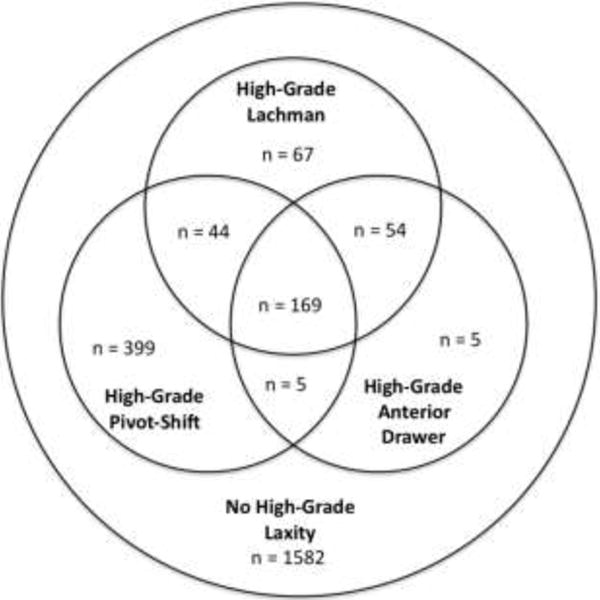
Venn diagram demonstrating the distribution of patients with high-grade laxity by physical examination test.
Two-year revision data were available for 2259 patients (96.8%) and patient-reported outcomes were available for 1979 patients (84.8%). ACL graft revision was performed in 94 patients (4.2%). Revision was performed in 39 patients (5.4%) in the high-grade laxity group and 55 patients without high-grade laxity (3.6%). In the multiple logistic regression model, the presence of high-grade pre-reconstruction laxity on at least one physical examination test was associated with significantly increased odds of ACL graft revision (OR=1.87, 95% CI: 1.19 – 2.95, p = 0.007). Similarly, high-grade pivot-shift (OR=1.84, p = 0.011) and Lachman (OR=2.27, p = 0.003) were associated with increased risk of revision. The relationship between high-grade anterior drawer and revision surgery did not reach statistical significance (OR=1.70, p = 0.12) (Table 2). Those with high-grade laxity on any two or all three of the physical examination tests also demonstrated increased odds of revision surgery (Table 3). The finding that no modeled interactions between predictor variables were statistically significant indicates that patient age, sex, BMI, Marx activity rating score, level of competition, and graft type did not influence failure risk in the high-grade laxity group more or less than in the other patients in the study.
Table 3.
Relationships between high-grade pre-reconstruction knee laxity and revision ACL surgery
| High-grade laxity | Odds Ratio | 95% Confidence Interval | Significance |
|---|---|---|---|
| 3+ Pivot-shift | 1.84 | 1.15 – 2.95 | p = 0.011 |
| Lachman > 10mm | 2.27 | 1.32 – 3.90 | p = 0.003 |
| Anterior Drawer > 10mm | 1.70 | 0.87 – 3.32 | p = 0.12 |
| Any one of the above | 1.87 | 1.19 – 2.95 | p = 0.007 |
| Any two of the above | 2.28 | 1.26 – 4.13 | p = 0.006 |
| All three of the above | 2.07 | 1.00 – 4.30 | p = 0.05 |
The mean postoperative IKDC score was 81.8 ± 15.9 and the mean KOOS-QOL score was 72.0 ± 22.0. The mean IKDC score was 82.1 ± 15.6 in the high-grade laxity group and 81.4 ± 16.5 in the group without high-grade laxity. The mean KOOS-QOL score was 72.0 ± 21.9 in the high-grade laxity group and 71.9 ± 22.0 in the group without high-grade laxity. In the multiple linear regression model, the presence of high-grade pre-reconstruction laxity was not associated with any difference in postoperative IKDC (β = −0.56, p = 0.44) or KOOS-QOL (β = 0.04, p = 0.97). Similarly, no association was found between these patient-reported outcome scores and high-grade pivot-shift, Lachman, or anterior drawer (Table 4).
Table 4.
Relationships between high-grade pre-reconstruction knee laxity and patient-reported outcomes at 2 years postoperative
| High-grade laxity | Regression Coefficient (β) | 95% Confidence Interval | Significance |
|---|---|---|---|
| Subjective IKDC Score | |||
| 3+ Pivot-shift | −0.46 | −1.99 – 1.06 | p = 0.55 |
| Lachman > 10mm | −0.56 | −2.46 – 1.34 | p = 0.56 |
| Anterior Drawer > 10mm | −0.34 | −2.54 – 1.86 | p = 0.76 |
| Any of the above | −0.56 | −2.01 – 0.88 | p = 0.44 |
| KOOS-QOL | |||
| 3+ Pivot-shift | 0.57 | −1.65 – 2.79 | p = 0.61 |
| Lachman > 10mm | 0.24 | −2.53 – 3.03 | p = 0.86 |
| Anterior Drawer > 10mm | −0.47 | −3.69 – 2.74 | p = 0.77 |
| Any of the above | 0.04 | −2.09 – 2.14 | p = 0.97 |
IKDC = International Knee Documentation Committee
KOOS-QOL = Knee injury and Osteoarthritis Outcome Score – Knee-Related Quality of Life
Discussion
The key finding of this study is that the presence of high-grade pre-operative knee laxity as assessed by manual physical examination under anesthesia was associated with significantly increased odds of revision ACL surgery within 2 years. We are aware of no previous studies that evaluate this relationship. Knee laxity should be considered along with other previously identified risk factors including age,1, 14, 29 graft factors (autograft versus allograft7, 13, 14 and hamstring graft size18, 21), and activity level1, 14 when assessing risk of revision ACL surgery.
The increased risk of revision surgery in the high-grade laxity patient population makes this population an important group for further study. These patients may represent a subset of patients in whom to study the efficacy of ancillary stabilization procedures that could augment standard intra-articular ACL reconstruction. Some authors have suggested that additional augmentation procedures in such patients to control high-grade laxity may improve outcomes.17, 25 These extra-articular procedures have seen increased interest in recent years30 following wide dissemination of the anatomy and function of the anterolateral ligament of the knee,3, 34 but high-quality data are lacking regarding surgical indications and outcomes. Further studies evaluating the effects of the addition of extra-articular procedures to intra-articular ACL reconstruction should carefully evaluate and consider pre- and postoperative knee laxity.
Two prior studies have evaluated the influence of pre-operative anterior knee laxity on patient-reported outcomes. Eitzen et al. reported no correlation between preoperative anterior tibial translation (measured with a KT-2000 arthrometer) and Cincinnati knee score at two years postoperative.6 Heijne et al. noted an association between increased preoperative anterior tibial translation and lower KOOS quality of life subscale scores at one year postoperative in a univariable model; however, when they performed multivariable modeling, they did not find any correlation between pre-operative laxity and outcome.10 These studies both involve relatively few patients that may be subject to beta error (Eitzen et al., n=60; Hiejne et al., n=64); however, the finding that pre-operative knee laxity does not influence patient-reported outcomes is confirmed by the current study. Other previously described factors including age, BMI, smoking status, articular cartilage and meniscus status are the major predictors of patient-reported outcomes following ACL reconstruction.5
The strengths of this study include a large sample size, which allowed for robust logistic regression analysis, and prospective data collection, which resulted in a very complete dataset. The data were collected by 17 surgeons at multiple institutions, making them broadly generalizable. Further, the physical examination tests utilized to assess laxity in this study are in broad clinical use, making the findings highly relevant to practicing surgeons. This study utilizes a patient cohort in which predictors in revision surgery have been extensively analyzed,14 but is the first to evaluate the potential influence of pre-operative physical examination findings on outcome of ACL reconstruction in this population.
This study has limitations. First, quantitative instrumentation was not used to measure pre-reconstruction knee laxity. Knee laxity was quantified by the treating physician during the exam under anesthesia at the time of the surgery, using the IKDC classification system. Patients reported by the operating surgeon as having a Lachman or anterior drawer examination greater than 10 mm difference from the contralateral side were classified as having a high-grade Lachman or anterior drawer respectively. Previous studies in conscious patients have demonstrated variable inter-rater reliability when using this system to assess laxity in ACL deficient knees. 12, 15, 27, 35 A portion of this variability is likely due to patients’ guarding 31 and exam under anesthesia may be more reliable, particularly in regards to the pivot-shift.4 While limited, these assessments do represent the method of laxity assessment most frequently used by surgeons when they make treatment decisions, making the data highly relevant. An additional limitation is the lack of post-reconstruction data regarding knee laxity. It is unknown whether patients with high-grade pre-operative laxity continue to have increased laxity following surgery. Such data could provide insight into the mechanism underlying the increased failure risk in this population and provide more insight into potential treatment options. Finally, an assessment of patients’ overall ligamentous laxity with a Beighton score2 or similar test would have allowed more analysis of whether the increased failure risk associated with increased laxity is related to injury factors only affecting the knee or related to generalized ligamentous laxity.
Conclusion
The presence of high-grade pre-operative knee laxity as assessed by manual physical examination under anesthesia is associated with significantly increased odds of revision ACL surgery, but has no association with patient-reported outcome scores at 2 years following ACL reconstruction.
What is known about the subject
Physical examination tests frequently demonstrate increased laxity when the ACL is ruptured, but the degree of increased laxity varies from patient to patient.
What this study adds to existing knowledge
High-grade pre-reconstruction knee laxity is associated with significantly increased odds of revision ACL surgery. There is no association with patient-reported outcome scores at 2 years.
References
- 1.Andernord D, Desai N, Bjornsson H, Ylander M, Karlsson J, Samuelsson K. Patient predictors of early revision surgery after anterior cruciate ligament reconstruction: a cohort study of 16,930 patients with 2-year follow-up. Am J Sports Med. 2015 Jan;43(1):121–127. doi: 10.1177/0363546514552788. [DOI] [PubMed] [Google Scholar]
- 2.Beighton P, Solomon L, Soskolne CL. Articular mobility in an African population. Ann Rheum Dis. 1973 Sep;32(5):413–418. doi: 10.1136/ard.32.5.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J. Anatomy of the anterolateral ligament of the knee. J Anat. 2013 Oct;223(4):321–328. doi: 10.1111/joa.12087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Donaldson WF, 3rd, Warren RF, Wickiewicz T. A comparison of acute anterior cruciate ligament examinations. Initial versus examination under anesthesia. Am J Sports Med. 1985 Jan-Feb;13(1):5–10. doi: 10.1177/036354658501300102. [DOI] [PubMed] [Google Scholar]
- 5.Dunn WR, Wolf BR, Harrell FE, Jr, Reinke EK, Huston LJ, Spindler KP. Baseline predictors of health-related quality of life after anterior cruciate ligament reconstruction: a longitudinal analysis of a multicenter cohort at two and six years. J Bone Joint Surg Am. 2015 Apr 1;97(7):551–557. doi: 10.2106/JBJS.N.00248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eitzen I, Holm I, Risberg MA. Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br J Sports Med. 2009 May;43(5):371–376. doi: 10.1136/bjsm.2008.057059. [DOI] [PubMed] [Google Scholar]
- 7.Engelman GH, Carry PM, Hitt KG, Polousky JD, Vidal AF. Comparison of allograft versus autograft anterior cruciate ligament reconstruction graft survival in an active adolescent cohort. Am J Sports Med. 2014 Oct;42(10):2311–2318. doi: 10.1177/0363546514541935. [DOI] [PubMed] [Google Scholar]
- 8.Galway HR, MacIntosh DL. The lateral pivot shift: a symptom and sign of anterior cruciate ligament insufficiency. Clin Orthop Relat Res. 1980 Mar-Apr;(147):45–50. [PubMed] [Google Scholar]
- 9.Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3–4):226–234. doi: 10.1007/BF01560215. [DOI] [PubMed] [Google Scholar]
- 10.Heijne A, Ang BO, Werner S. Predictive factors for 12-month outcome after anterior cruciate ligament reconstruction. Scand J Med Sci Sports. 2009 Dec;19(6):842–849. doi: 10.1111/j.1600-0838.2008.00852.x. [DOI] [PubMed] [Google Scholar]
- 11.Irrgang JJ, Anderson AF, Boland AL, et al. Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med. 2001 Sep-Oct;29(5):600–613. doi: 10.1177/03635465010290051301. [DOI] [PubMed] [Google Scholar]
- 12.Johnson DS, Ryan WG, Smith RB. Does the Lachman testing method affect the reliability of the International Knee Documentation Committee (IKDC) Form? Knee Surg Sports Traumatol Arthrosc. 2004 May;12(3):225–228. doi: 10.1007/s00167-003-0475-3. [DOI] [PubMed] [Google Scholar]
- 13.Kaeding CC, Aros B, Pedroza A, et al. Allograft Versus Autograft Anterior Cruciate Ligament Reconstruction: Predictors of Failure From a MOON Prospective Longitudinal Cohort. Sports Health. 2011 Jan;3(1):73–81. doi: 10.1177/1941738110386185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Spindler KP. Risk Factors and Predictors of Subsequent ACL Injury in Either Knee After ACL Reconstruction: Prospective Analysis of 2488 Primary ACL Reconstructions From the MOON Cohort. Am J Sports Med. 2015 Jul;43(7):1583–1590. doi: 10.1177/0363546515578836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lange T, Freiberg A, Droge P, Lutzner J, Schmitt J, Kopkow C. The reliability of physical examination tests for the diagnosis of anterior cruciate ligament rupture–A systematic review. Man Ther. 2015 Jun;20(3):402–411. doi: 10.1016/j.math.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 16.Larson RL. Physical examination in the diagnosis of rotatory instability. Clin Orthop Relat Res. 1983 Jan-Feb;(172):38–44. [PubMed] [Google Scholar]
- 17.Lerat JL, Mandrino A, Besse JL, Moyen B, Brunet-Guedj E. Effect of external extra-articular ligament plasty on the results of anterior cruciate ligament reconstruction with patellar tendon, a 4 years follow-up. Rev Chir Orthop Reparatrice Appar Mot. 1997;83(7):591–601. [PubMed] [Google Scholar]
- 18.Magnussen RA, Lawrence JT, West RL, Toth AP, Taylor DC, Garrett WE. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy. 2012 Apr;28(4):526–531. doi: 10.1016/j.arthro.2011.11.024. [DOI] [PubMed] [Google Scholar]
- 19.Magnussen RA, Reinke EK, Huston LJ, Hewett TE, Spindler KP. Factors Associated With High-Grade Lachman, Pivot Shift, and Anterior Drawer at the Time of Anterior Cruciate Ligament Reconstruction. Arthroscopy. 2016 Jan 25; doi: 10.1016/j.arthro.2015.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Malanga GA, Andrus S, Nadler SF, McLean J. Physical examination of the knee: a review of the original test description and scientific validity of common orthopedic tests. Arch Phys Med Rehabil. 2003 Apr;84(4):592–603. doi: 10.1053/apmr.2003.50026. [DOI] [PubMed] [Google Scholar]
- 21.Mariscalco MW, Flanigan DC, Mitchell J, et al. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: a Multicenter Orthopaedic Outcomes Network (MOON) Cohort Study. Arthroscopy. 2013 Dec;29(12):1948–1953. doi: 10.1016/j.arthro.2013.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marx RG, Connor J, Lyman S, et al. Multirater agreement of arthroscopic grading of knee articular cartilage. Am J Sports Med. 2005 Nov;33(11):1654–1657. doi: 10.1177/0363546505275129. [DOI] [PubMed] [Google Scholar]
- 23.Marx RG, Stump TJ, Jones EC, Wickiewicz TL, Warren RF. Development and evaluation of an activity rating scale for disorders of the knee. Am J Sports Med. 2001 Mar-Apr;29(2):213–218. doi: 10.1177/03635465010290021601. [DOI] [PubMed] [Google Scholar]
- 24.Musahl V, Citak M, O’Loughlin PF, Choi D, Bedi A, Pearle AD. The effect of medial versus lateral meniscectomy on the stability of the anterior cruciate ligament-deficient knee. Am J Sports Med. 2010 Aug;38(8):1591–1597. doi: 10.1177/0363546510364402. [DOI] [PubMed] [Google Scholar]
- 25.Noyes FR, Barber SD. The effect of an extra-articular procedure on allograft reconstructions for chronic ruptures of the anterior cruciate ligament. J Bone Joint Surg Am. 1991 Jul;73(6):882–892. [PubMed] [Google Scholar]
- 26.Outerbridge RE. The etiology of chondromalacia patellae. 1961. Clin Orthop Relat Res. 2001 Aug;(389):5–8. doi: 10.1097/00003086-200108000-00002. [DOI] [PubMed] [Google Scholar]
- 27.Peeler J, Leiter J, MacDonald P. Accuracy and reliability of anterior cruciate ligament clinical examination in a multidisciplinary sports medicine setting. Clin J Sport Med. 2010 Mar;20(2):80–85. doi: 10.1097/JSM.0b013e3181ceca45. [DOI] [PubMed] [Google Scholar]
- 28.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)–development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998 Aug;28(2):88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 29.Schlumberger M, Schuster P, Schulz M, et al. Traumatic graft rupture after primary and revision anterior cruciate ligament reconstruction: retrospective analysis of incidence and risk factors in 2915 cases. Knee Surg Sports Traumatol Arthrosc. 2015 Sep 26; doi: 10.1007/s00167-015-3699-0. [DOI] [PubMed] [Google Scholar]
- 30.Sonnery-Cottet B, Thaunat M, Freychet B, Pupim BH, Murphy CG, Claes S. Outcome of a Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction Technique With a Minimum 2-Year Follow-up. Am J Sports Med. 2015 Jul;43(7):1598–1605. doi: 10.1177/0363546515571571. [DOI] [PubMed] [Google Scholar]
- 31.Tanaka M, Vyas D, Moloney G, Bedi A, Pearle AD, Musahl V. What does it take to have a high-grade pivot shift? Knee Surg Sports Traumatol Arthrosc. 2012 Apr;20(4):737–742. doi: 10.1007/s00167-011-1866-5. [DOI] [PubMed] [Google Scholar]
- 32.Terry GC, Norwood LA, Hughston JC, Caldwell KM. How iliotibial tract injuries of the knee combine with acute anterior cruciate ligament tears to influence abnormal anterior tibial displacement. Am J Sports Med. 1993 Jan-Feb;21(1):55–60. doi: 10.1177/036354659302100110. [DOI] [PubMed] [Google Scholar]
- 33.Torg JS, Conrad W, Kalen V. Clinical diagnosis of anterior cruciate ligament instability in the athlete. Am J Sports Med. 1976 Mar-Apr;4(2):84–93. doi: 10.1177/036354657600400206. [DOI] [PubMed] [Google Scholar]
- 34.Vincent JP, Magnussen RA, Gezmez F, et al. The anterolateral ligament of the human knee: An anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc. 2012;20(1):147–152. doi: 10.1007/s00167-011-1580-3. [DOI] [PubMed] [Google Scholar]
- 35.Wiertsema SH, van Hooff HJ, Migchelsen LA, Steultjens MP. Reliability of the KT1000 arthrometer and the Lachman test in patients with an ACL rupture. Knee. 2008 Mar;15(2):107–110. doi: 10.1016/j.knee.2008.01.003. [DOI] [PubMed] [Google Scholar]


