Abstract
Background
Several studies have raised concerns that future demand for blood products may not be met. The ageing of the general population and the fact that a large proportion of blood products is transfused to elderly patients has been identified as an important driver of blood shortages. The aim of this study was to collect, for the first time, nationally representative data regarding blood donors and transfusion recipients in order to predict the future evolution of blood donations and red blood cell (RBC) use in Switzerland between 2014 and 2035.
Materials and methods
Blood donor and transfusion recipient data, subdivided by the subjects’ age and gender were obtained from Regional Blood Services and nine large, acute-care hospitals in various regions of Switzerland. Generalised additive regression models and time-series models with exponential smoothing were employed to estimate trends of whole blood donations and RBC transfusions.
Results
The trend models employed suggested that RBC demand could equal supply by 2018 and could eventually cause an increasing shortfall of up to 77,000 RBC units by 2035.
Discussion
Our study highlights the need for continuous monitoring of trends of blood donations and blood transfusions in order to take proactive measures aimed at preventing blood shortages in Switzerland. Measures should be taken to improve donor retention in order to prevent a further erosion of the blood donor base.
Keywords: blood donation, RBC use, demographics, Switzerland
Introduction
Several studies have raised concerns that the future demand for blood products may not be met. The ageing of the general population has been identified as an important driver of blood shortages because large proportions of blood products are transfused to elderly patients whereas blood is primarily donated by younger age cohorts1–9.
So far, studies have reported demography-induced increases of red blood cell (RBC) demand in Australia, Germany, France, England and Wales, Ireland, Italy, Japan, Canada, Poland, Russia and the United States of America1,2,4–7. Only one study that assessed future RBC use in the Netherlands showed a declining trend of RBC demand despite an ageing population3.
Forecasts of population growth by the Swiss Federal Statistical Office indicate that, in 2035, more than 1 million men and 1.2 million women in Switzerland will be 65 years or older10. Thus, the absolute number of older people in Switzerland will have more than doubled between 1996 and 2035. Although demographic change in Switzerland may have a substantial impact on RBC demand, no study has so far assessed future RBC demand and supply in Switzerland. Moreover, results from previous studies are not easily transferable between countries. Despite their similar socioeconomic and demographic backgrounds, Denmark, Austria, Switzerland, and the Netherlands differed considerably with respect to the number of transfused RBC units per 1,000 population in 2008 (60, 53, 41 and 34, respectively) and the corresponding number of blood donors per 1,000 population (46, 41, 33 and 24, respectively)11. Furthermore, most previous studies extrapolated RBC use based on constant RBC transfusion rates1,2,4–7 and only one study included trends in RBC use3. However, several studies have shown that recent implementation of restrictive transfusion strategies and patient blood management (PBM) schemes is associated with a reduction in transfused blood products and transfused patients, while mortality and overall morbidity seemed to be at least comparable12–19. Consequently, studies that used constant transfusion rates to forecast future demand may have substantially overestimated RBC demand. Finally, Switzerland currently lacks national data to assess future demand and supply of blood products, i.e. no national datasets are currently available that include age-specific and gender-specific information on transfused patients as well as whole blood donors in Switzerland.
Our study aims were to: (i) establish nationally representative datasets on age-specific and gender-specific use of blood products and whole blood donations in Switzerland and (ii) assess future RBC demand and supply in Switzerland by taking into account demographic trends as well as trends in RBC use.
Materials and methods
Transfusion data
Aggregate data on the total number of blood products issued in Switzerland by the Regional Transfusion Services SRC from 2003 to 2013 were obtained from Swiss Transfusion SRC. Corresponding anonymised microdata on transfused blood products divided according to the age and gender of the recipients were derived from a sample of nine large, acute-care hospitals which accounted for 19% of total national blood product use. In order to describe blood products and blood product recipients in Switzerland by age and gender, data from the included hospitals were extrapolated to the national level by weighting the transfused blood products, i.e. weights were calculated by dividing the total number of blood products issued per product type and year by the corresponding number of transfused blood products. Consequently, age-specific and gender-specific national counts of blood products and blood product recipients represent weighted counts. National RBC, platelet and fresh-frozen plasma transfusion rates were calculated as the mean number of units transfused per 1,000 inhabitants per age group and gender.
Since participating hospitals reflect a non-random sample, microdata on transfused blood products were cross-validated using comparable data from the Netherlands9.
Donation data
In Switzerland, Swiss Transfusion SRC and the Regional Blood Transfusion Services SRC (RBS) are the only institutions entrusted with the collection of homologous blood donations by the Swiss government. We obtained aggregate data on the total number of whole blood donations from 1996 to 2013 from Swiss Transfusion SRC. Corresponding anonymised microdata on whole blood donors aged between 18 and 69 years and successful whole blood donations divided by the donors’ age and gender were obtained from 11 of 13 RBS. On average, the included RBS sample accounted for 87% and the non-reporting blood centres for 13% of national whole blood donations in the study period. Inverse probability weighting was used to extrapolate the data from the 11 RBS to the national level. Hence, age-specific and gender-specific national counts of whole blood donations represent weighted counts. National whole blood donor and whole blood donation rates were calculated as the mean number of whole blood donors and whole blood donations per 1,000 inhabitants per age group and gender.
Demographic data
The Swiss Federal Statistical Office (SFSO) provided past and future information on the age and gender distribution of the permanent resident population of Switzerland. We used the SFSO's reference scenario (A-00-2010) which extrapolates past trends of mortality, birth rates and net migration to estimate the future age and gender composition of the population between 2014 and 203510.
Red blood cell demand model
In order to predict future RBC demand in Switzerland, we assumed that future RBC use will not only be influenced by demographic factors but also by changes in clinical transfusion practice. In recent years, PBM has been implemented in many hospitals and several studies report substantial reductions in the use of blood products as a consequence of PBM12–19.
In order to account for these trends, age-specific and gender-specific RBC transfusion data from 2003 to 2013 were used and a generalised additive model was employed to estimate RBC transfusion rates as a function of age, gender and calendar year3. RBC demand in past and future years was estimated by multiplying age-specific and gender-specific transfusion rates by the corresponding population of permanent residents in the respective year and summing them.
Furthermore, our model assumed that blood products transfused equal blood products issued, i.e. we assumed that all blood products delivered to hospitals were transfused and no loss occurred.
Whole blood donation model
Switzerland’s total number of whole blood donors declined from 341,741 in 1996 to 198,406 in 2013 and the respective whole blood donations declined from 576,529 to 322,910. Similarly, retention rates declined and the median transition time from active to inactive whole blood donor was found to be shorter for more recent blood donor cohorts20. While most previous studies assumed constant whole blood donation rates1,2,4–7 or constant whole blood donor retention rates3, we suggest that assuming constant rates does not adequately capture recent trends in the Swiss blood donor population. Rather, the total number of blood donors reflects donor recruitment efforts and donor management by the blood banks as well as sociodemographic, socioeconomic and sociocultural changes in the general population. The latter changes include a growing number of immigrants, increasing population mobility, and decreasing participation in traditional volunteer organisations, all of which have been found to make recruitment or retention of blood donors more difficult4,21–24.
Age-specific and gender-specific whole blood donations from 1996 to 2013 and exponential smoothing models (ETS) within a univariate time series framework were used to forecast whole blood donation rates25,26. We employed automatic selection of the ETS models, i.e. the algorithm selected an exponential smoothing method among 30 different methods that best fitted the data based on the Akaike information criterion26,27. Whole blood donations of future years were calculated by multiplying age-specific and gender-specific whole blood donation rates by the corresponding population of permanent residents in the respective year and summing them.
Statistical analyses
We used Stata/SE Version 14 (StataCorp, College Station, TX, USA) for statistical analyses and for creating graphs. The whole blood donation model was created using the forecast library in R Version 3.2.3 (The R Foundation for Statistical Computing, Vienna, Austria). For the RBC demand model, the “mgcv” library was used.
Results
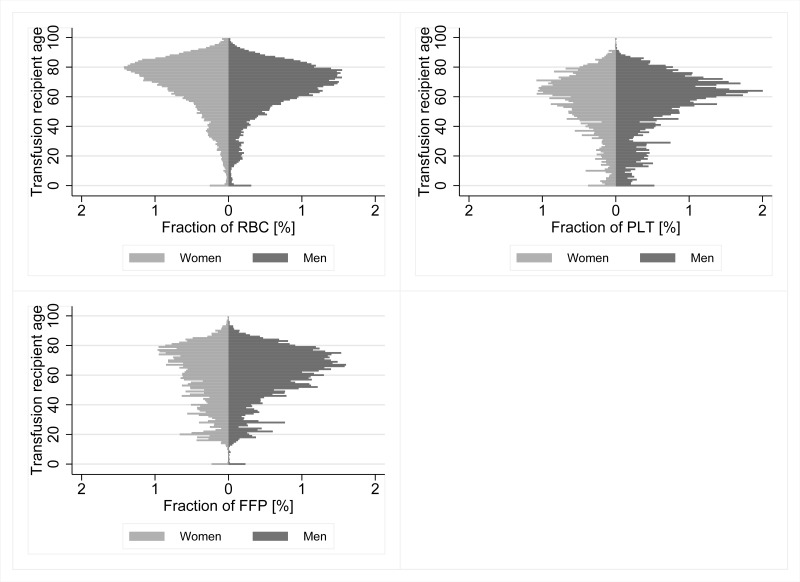
From 2003 to 2013, the Regional Transfusion Services SRC delivered 3,343,734 RBC units, 292,259 platelet units and 710,699 fresh-frozen plasma (FFP) units to hospitals (Table I). Corresponding microdata obtained from the nine participating hospitals contained anonymised information on 179,748 patients who received 802,966 blood products (588,221 RBC units; 78,395 platelet units; 136,350 FFP units). Overall, the included hospitals accounted for 19% of total national blood product use from 2003 to 2013 or, more specifically, 18% of RBC, 27% of platelet and 19% of FFP use. Figure 1 shows weighted national blood product use in Switzerland by recipient age and gender. With the exception of children at age 0, the use of RBC, platelets and FFP tends to increase substantially with age. From 2003 to 2013, 53% of all RBC, 60% of all platelets and 59% of all FFP were transfused to men. Moreover, recipients of 65 years or older received 62% of the RBC, 37% of the platelets and 45% of the FFP. Recipients between 45 and 64 years of age received 25% of the RBC, 37% of the platelets and 33% of the FFP.
Table I.
Coverage of blood product transfusions in the dataset compared to annual blood products issued (BPI) by the Regional Blood Transfusion Services SRC (RBS) in Switzerland1.
| Blood products issued by RBS | Blood product transfusions in dataset | Fraction of BPI covered by dataset | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| RBC | PLT | FFP | RBC | PLT | FFP | % RBC | % PLT | % FFP | |
| 2003 | 308,965 | 18,590 | 81,267 | 43,892 | 4,262 | 12,857 | 14 | 23 | 16 |
| 2004 | 302,820 | 19,081 | 66,309 | 43,447 | 4,759 | 12,476 | 14 | 25 | 19 |
| 2005 | 301,340 | 19,814 | 73,125 | 48,013 | 4,563 | 14,285 | 16 | 23 | 20 |
| 2006 | 302,654 | 21,885 | 74,577 | 57,856 | 7,523 | 14,811 | 19 | 34 | 20 |
| 2007 | 308,470 | 22,937 | 69,822 | 58,549 | 7,965 | 14,933 | 19 | 35 | 21 |
| 2008 | 313,587 | 27,669 | 65,823 | 58,460 | 7,805 | 16,711 | 19 | 28 | 25 |
| 2009 | 311,580 | 29,654 | 70,353 | 60,185 | 7,795 | 11,055 | 19 | 26 | 16 |
| 2010 | 308,599 | 29,938 | 61,571 | 59,330 | 7,686 | 11,447 | 19 | 26 | 19 |
| 2011 | 308,627 | 33,676 | 53,937 | 57,277 | 8,503 | 8,935 | 19 | 25 | 17 |
| 2012 | 297,582 | 34,265 | 49,832 | 56,493 | 9,510 | 10,452 | 19 | 28 | 21 |
| 2013 | 279,510 | 34,750 | 44,083 | 44,719 | 8,024 | 8,388 | 16 | 23 | 19 |
|
| |||||||||
| Total | 3,343,734 | 292,259 | 710,699 | 588,221 | 78,395 | 136,350 | 18 | 27 | 19 |
An unknown but small fraction of BPI is not transfused to patients because of outdating, leakage, lost units and other reasons.
RBC: red blood cells; PLT: platelets; FFP: fresh-frozen plasma.
Figure 1.
Age distribution of blood product recipients 2003–2013.
RBC: red blood cells; PLT: platelets; FFP: fresh-frozen plasma.
Overall, the median age of the RBC transfusion recipients increased from 70 years in 2003 (mean=65.6) to 73 years in 2013 (mean=68.5). The corresponding median age for men was 68 years (mean=63.8) and 71 years (mean=67.3). For women, the median age was 73 years (mean=67.2) and 75 years (mean=69.6).
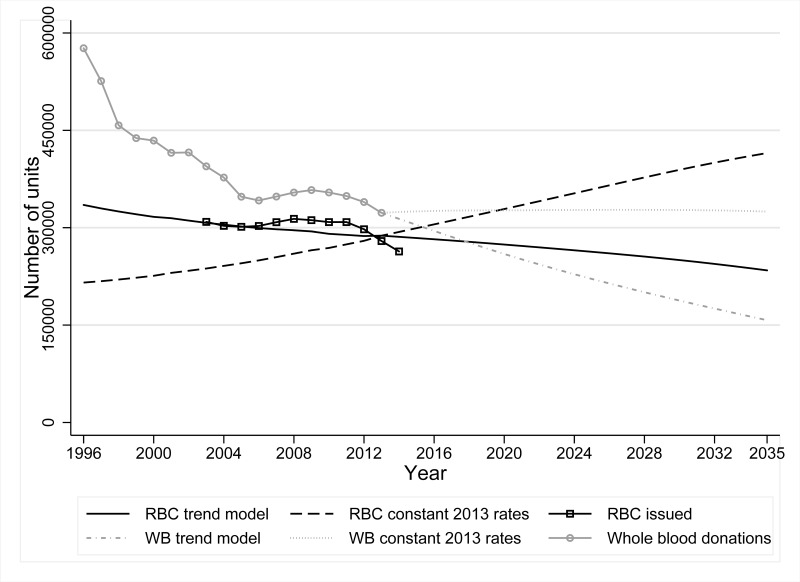
With annual differences of 0.2 to 6.3% between past empirical and predicted RBC demand from 2003 to 2013, the model fit is adequate (Figure 2). Predicted RBC demand decreased by 18.6% from 287,789 to 234,311 units between 2013 and 2035. The overall predicted transfusion rate decreased from 35.8 RBC units per 1,000 inhabitants to 26.5 RBC units per 1,000 inhabitants.
Figure 2.
RBC demand and whole blood donations 1996–2035.
RBC: red blood cells; WB: whole blood.
Conversely, predictions of RBC use with constant 2013 transfusion rates resulted in an inferior fit and predicted an increase of RBC demand from 287,789 to 414,992 units between 2013 and 2035. Constant 2003 transfusion rates also resulted in an inferior fit whereas predicted RBC demand in 2035 was even higher than the demand based on constant 2013 transfusion rates (results not shown).
Between 2013 and 2035 the predicted number of whole blood donations declined by 51.2% from 322,910 to 157,550 or on average by 7,516 donations per year. Thus, predicted whole blood donations were declining much faster than predicted RBC demand. This trend suggests that RBC demand could equal supply by 2018 and could eventually cause an increasing shortfall of up to 77,000 RBC units by 2035 if blood centres do not adjust their operations. If, however, whole blood donations could be sustained at constant 2013 rates, RBC demand would be met up to 2035.
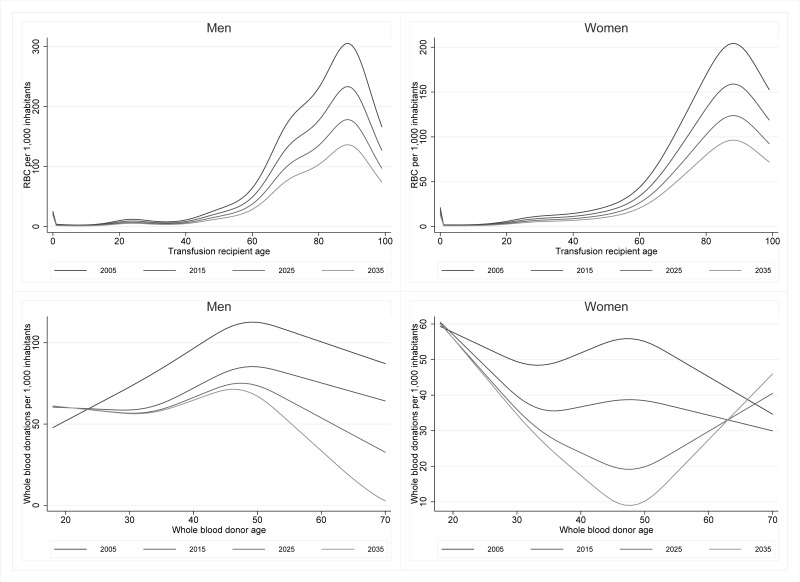
Predicted trends of RBC transfusion rates and whole blood donation rates are explored further in Figure 3. RBC transfusion rates reached their maximum at ages 89 (men) and 88 (women) and continued to decline in all age groups over all years. For men, the maximum RBC transfusion rates were 305 (2005), 233 (2015), 178 (2025), and 136 (2035) RBC units per 1,000 inhabitants. Respective maximum RBC transfusion rates for women were 204, 159, 124, and 96 RBC units per 1,000 inhabitants. Overall, whole blood donation rates also declined over all years but showed age-specific and gender-specific patterns. Donation rates of men first increased with age, reached a maximum around ages 45–50 years and then started to decline again. Over time, donation rates for younger men (18–24 years) were rather stable. Similarly, donation rates of men below 50 years of age were rather stable from 2015–2035 while donation rates for men over 50 declined substantially over all years. For women, donation rates in past years first declined with age, then increased slightly, and then decreased again. However, predicted donation rates 2025–2035 first declined, reached a nadir at around 47 years of age and then increased again. In contrast to donation rates for older men, the rates for older women (60–69 years) were rather stable and even increased slightly over time.
Figure 3.
Red blood cell (RBC) transfusion rates and whole blood donation rates 2005–2035.
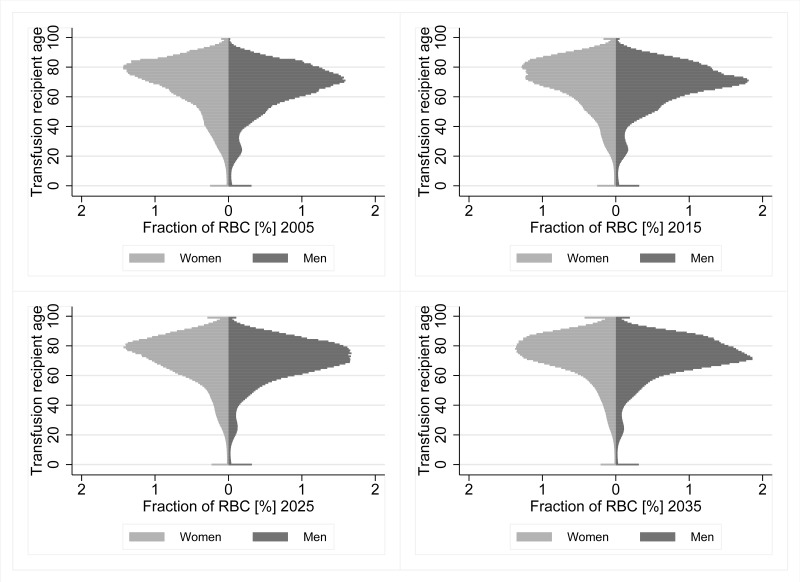
Predicted changes in RBC transfusion rates and predicted changes in whole blood donation rates together with predicted demographic changes determine the age-specific and gender-specific composition and evolution of RBC transfusion recipients and whole blood donors. The proportion of RBC units transfused to men increased slightly from 52.1 (2005) to 54.6% (2035). For men and women, the predicted fraction of RBC units transfused to older people increased substantially (Figure 4). In 2005, 62.8% of RBC units were transfused to recipients 65 years of age or older and 23.9% were transfused to recipients 80 years or older. Respective fractions for the 65+ (80+) age groups were 66.1% (25.7%), 70.0% (29.0%), and 75.3% (33.3%) in 2015, 2025, and 2035.
Figure 4.
Fraction of red blood cell (RBC) transfused by age and gender 2005–2035.
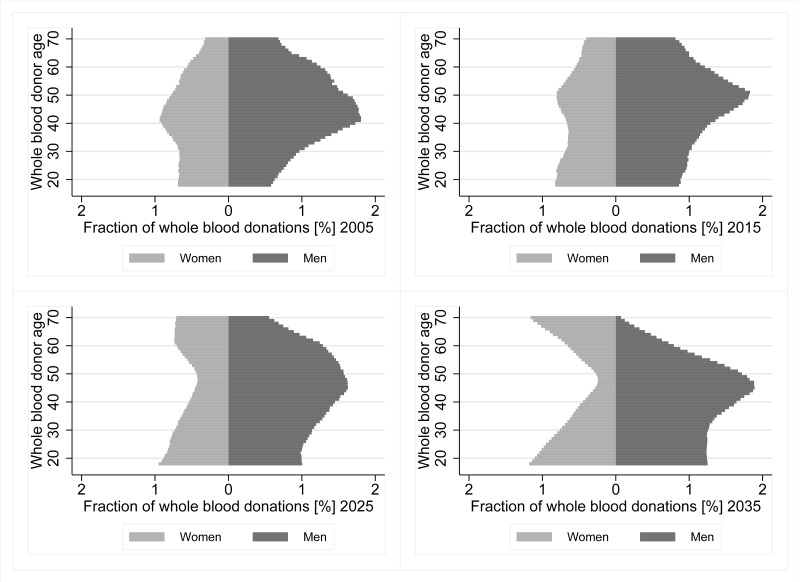
Similarly, the composition of whole blood donations divided by age and gender of the donors was found to evolve substantially over time (Figure 5). The proportion of whole blood donations from women decreased marginally from 36.1 (2005) to 35.5% (2035). However, the fraction of whole blood donations in the age group 18–29 years increased from 17.0% in 2005 to 26.8% in 2035 while the fraction of donations in the age groups 30–49 years and 50–69 years decreased from 47.0 to 41.2% and from 36.0 to 32.0% respectively.
Figure 5.
Fraction of whole blood donations by age and gender 2005–2035.
Discussion
In recent years, several studies have assessed future demand of blood products for Canada4, Germany5–7, Finland2, the Netherlands3, the United Kingdom1,8 or several countries at the same time2. With the exception of one Dutch study conducted by Borkent-Raven, Janssen and van der Poel3 and one study conducted in the North of England by Tinegate and colleagues8, all were assuming constant age-specific and gender-specific transfusion rates and most of them predicted future RBC use based on only one observation year. However, the implementation of restrictive transfusion practice and PBM has reduced the average number of blood products used per patient in many clinical settings12–19, a trend that has been documented on a national level as well3,8. Consequently, the Dutch study found that modelling RBC demand using demographic data alone hugely overestimated future demand3. Our results confirm these findings for Switzerland.
Red blood cell demand
Both, RBC demand and whole blood donation models assume that current trends continue into the future. More specifically, the RBC demand model suggests that the implementation of restrictive transfusion practices and PBM continues to lead to transfusion of fewer blood products and fewer transfused patients. Consequently, the trend in clinical practice counterbalances the demographic trend which suggests that an ageing population requires ever more blood products. The latter effect is illustrated in Figure 2 by the increasing demand of RBC when constant 2013 transfusion rates are assumed. These findings are in line with the results reported by Borkent-Raven and colleagues3. However, demographic trends such as the ageing population of a society can be predicted with less uncertainty than future developments in clinical practice. Moreover, it seems currently unlikely that transfusion rates will drop below a certain threshold in the near future, without putting the population at risk from undersupply. While the assumption of ever decreasing transfusion rates may be too optimistic, a more realistic scenario is that RBC demand continues to decline for some time and then, as soon as the threshold is reached, rises again due to the demographic trend. However, it is currently unclear where this threshold lies since comparable countries in Europe vary greatly with respect to their RBC transfusion rates. The most recently published EDQM country survey 2012 found that in Europe, the average reported use of RBC was 36 units per 1,000 inhabitants with a median of 37 per 1,000 inhabitants28. Among comparable countries, the Netherlands reported the lowest RBC transfusion rate (27 units per 1,000 inhabitants). Assuming that Switzerland’s RBC transfusion rates will approach at least 27 RBC units per 1,000 inhabitants, demographic trends could lead to an increase in RBC demand only after 2035 if the RBC transfusion rates continue to decline as projected by our demand model.
Whole blood donations
The blood donation model also assumed that past trends continue and hence, the number of blood donations continues to decline. Overall, the decline in the number of blood donations is partially attributable to the declining RBC demand of Swiss hospitals. The initial sharp drop in the number of whole blood donations from 1996 to 2000 is mainly attributable to the sale of the Central Laboratory in Bern to Australian CSL Limited in 2000 which resulted in a marked reduction of blood plasma demand. However, even after the year 2000, the projected blood donations were declining much faster than the projected RBC demand. Yet, it is not very likely that the blood transfusion services will just sit there and watch their donor base erode. Instead, it is reasonable to assume that the blood transfusion services will adjust their operations and take all measures to attract and recruit new donors, and to improve donor retention in order to stop or mitigate any further erosion of the blood donor base. In the past years, the number of blood donations has not been much affected by demography or donor recruitment but rather by donor retention. While the number of first-time donors per 1,000 inhabitants and the number of whole blood donations per donor (1.69 and 1.63 in 1996 and 2013, respectively) remained relatively stable over a long period, the number of repeat donors, and consequently the number of total donors per 1,000 inhabitants, declined from 48 donors per 1,000 inhabitants in 1996 to 31 and 25 donors in 2003 and 2013, respectively. As the number of blood donations from the middle age group 26–40 years declined between 1996 (34.2%) and 2013 (24.0%) and new blood donors were mostly recruited from the younger population, the fraction of whole blood donations in the age group 18–29 years is predicted to increase from 17.0% in 2005 to 26.8% in 2035.
In line with these findings, a study focusing on active to inactive donor transition in the Basel region showed that the proportion of inactive donors after just one blood donation increased in successive donor cohorts and similarly, the median active to inactive donor transition time markedly decreased20. Consequently, the RBS and Swiss Transfusion SRC should specifically develop and implement strategies that improve donor retention in order to prevent a further decline of their donor base. Moreover, the impact of demographics on the blood donor base is likely to increase in the near future and beyond. The blood-dependency ratio, i.e. the ratio of the age-eligible to the age-non-eligible donor population, was approximately 0.44 between 1996 and 2013: in other words, for every 44 age-non-eligible inhabitants, there were 100 age-eligible inhabitants aged between 18 and 69 years (eligible donor age limits in Switzerland). By 2035, the blood-dependency ratio will have increased to 0.55 which suggests that the burden on blood donors will increase. Moreover, decreasing proportions of age-eligible blood donors could make recruitment of new donors more difficult and retention and motivation of existing donors more challenging. Furthermore, sociodemographic changes may further intensify the challenges that blood establishments will have to face. Over the last decade, Switzerland has seen a pronounced population growth of roughly 1% per year29, mainly due to immigration. Immigration, however, may pose a double challenge. On the one hand, studies found that immigrants and ethnic minorities have a lower propensity to donate blood4,21–23. On the other hand, the demand for certain (rare) blood groups could increase as people from African or Asian descent more often have O-positive or B-positive blood groups. At the same time, they have a higher risk of sickle-cell disorders and thalassaemias30.
Implications
Given that blood establishments in Switzerland are constantly adjusting their strategies and actions in order to meet the demand for blood products, our whole blood donation model is probably too pessimistic and the “truth” may lie somewhere between the number of donations expected by our trend model and the model with constant 2013 donation rates. Consequently, it is very likely that the potential gap between RBC demand and supply can be closed. However, the number of blood transfusions and the number of blood donations should be closely and continuously monitored in order to prevent blood shortages.
To sum up, our study suggests that if current trends of RBC demand and whole blood donation continue, RBC demand could equal supply by 2018 and could eventually cause an increasing shortfall of up to 77,000 RBC units by 2035 if blood centres do not adjust their operations. However, the assumption of a continuing trend of declining rates of RBC use over more than 20 years seems overly optimistic, while it seems overly pessimistic for the number of whole blood donations made. A more realistic scenario would be that RBC transfusion rates will reach a threshold were no further decline is possible without putting the population at risk of undersupply. At the same time, adaptive strategies and measure taken by blood establishments are likely to stop the erosion of the blood donor base which, in turn, increases the likelihood that RBC demand can be met.
Strengths and limitations
It is a strength of our study that large data samples were used to compile whole blood donor and transfusion recipient datasets weighted to the national level by year, age and gender and that these datasets could be subsequently used to assess past and future trends of blood product use and whole blood donations.
Our study does, however, have several limitations that need to be taken into account. Firstly, the participating hospitals reflect a systematic, non-random sample and hence microdata on transfused blood products divided by the subjects’ age and gender may be biased. However, the participating hospitals included one university hospital (out of 5) and eight large cantonal or regional hospitals (out of 34) that accounted for 18% of national RBC use. Furthermore, all language regions were covered. With the exception of neonates, who were underrepresented in our dataset, we found that the age-specific distribution of RBC use by gender was very similar to the distribution reported by the Dutch PROTON study9. The latter suggests that despite the non-random sample, the data have substantial credibility.
Secondly, we assumed that all RBC issued by the RBS were actually transfused to patients in hospitals. However, blood products may not have been transfused because of outdating, leakage or lost units and we may, therefore, have slightly overestimated the number of transfused RBC.
Thirdly, time-series data for RBC use were available for the period 2003–2013 only. However, our whole blood donation data suggest that RBC use from 1996 to 2003 was substantially higher than after 2003. Consequently, we may have underestimated the yearly decline in RBC transfusion rates.
Fourthly, our RBC demand and whole blood donation models both assume that current trends will continue. However, it is not clear whether future clinical transfusion practice will continue to reduce the number of RBC needed or whether new therapies will even lead to an increased RBC demand or whether RBC transfusion rates will remain constant, once that a certain threshold is reached. Similarly, blood establishments and their recruitment and retention strategies and programmes will have an impact on the future number of blood donors and blood donations.
Fifthly, many interdependent and dynamic factors affect both the supply of and demand for RBC. Hence, future trends in blood use may be impossible to predict with any mathematical model.
Conclusions
Our study highlights the need for continuous monitoring of trends in blood donations and blood transfusions in order to take proactive measures aimed at preventing blood shortages in Switzerland. Measures should also be taken to improve donor retention in order to prevent a further substantial erosion of blood donations and the blood donor base.
Acknowledgements
This study was supported by Stiftung Lindenhof, grant number 13-04-F.
Footnotes
Authorship contribution
TV drafted the text. All Authors critically reviewed the text and provided additional thoughts and input.
The Authors declare no conflict of interests.
References
- 1.Currie CJ, Patel TC, McEwan P, et al. Evaluation of the future supply and demand for blood products in the United Kingdom National Health Service. Transfus Med. 2004;14:19–24. doi: 10.1111/j.0958-7578.2004.00475.x. [DOI] [PubMed] [Google Scholar]
- 2.Ali A, Auvinen MK, Rautonen J. The aging population poses a global challenge for blood services. Transfusion. 2010;50:584–8. doi: 10.1111/j.1537-2995.2009.02490.x. [DOI] [PubMed] [Google Scholar]
- 3.Borkent-Raven BA, Janssen MP, Van Der Poel CL. Demographic changes and predicting blood supply and demand in the Netherlands. Transfusion. 2010;50:2455–60. doi: 10.1111/j.1537-2995.2010.02716.x. [DOI] [PubMed] [Google Scholar]
- 4.Drackley A, Newbold KB, Paez A, et al. Forecasting Ontario’s blood supply and demand. Transfusion. 2012;52:366–74. doi: 10.1111/j.1537-2995.2011.03280.x. [DOI] [PubMed] [Google Scholar]
- 5.Greinacher A, Fendrich K, Alpen U, et al. Impact of demographic changes on the blood supply: Mecklenburg-West Pomerania as a model region for Europe. Transfusion. 2007;47:395–401. doi: 10.1111/j.1537-2995.2007.01129.x. [DOI] [PubMed] [Google Scholar]
- 6.Greinacher A, Fendrich K, Brzenska R, et al. Implications of demographics on future blood supply: a population-based cross-sectional study. Transfusion. 2011;51:702–9. doi: 10.1111/j.1537-2995.2010.02882.x. [DOI] [PubMed] [Google Scholar]
- 7.Greinacher A, Fendrich K, Hoffmann W. Demographic changes: the impact for safe blood supply. Transfus Med Hemother. 2010;37:141–8. doi: 10.1159/000313949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tinegate H, Chattree S, Iqbal A, et al. Ten-year pattern of red blood cell use in the North of England. Transfusion. 2013;53:483–9. doi: 10.1111/j.1537-2995.2012.03782.x. [DOI] [PubMed] [Google Scholar]
- 9.Borkent-Raven BA, Janssen MP, van der Poel CL, et al. The PROTON study: profiles of blood product transfusion recipients in the Netherlands. Vox Sang. 2010;99:54–64. doi: 10.1111/j.1423-0410.2010.01312.x. [DOI] [PubMed] [Google Scholar]
- 10.Swiss Federal Statistical Office. Szenarien zur Bevölkerungsentwicklung der Schweiz 2010–2060. Neuchâtel: SFSO; 2010. [Accessed on 11/10/2015]. Available at: http://www.bfs.admin.ch/bfs/portal/de/index/news/publikationen.html?publicationID=3989. [Google Scholar]
- 11.Janssen MP, Behr-Gross ME. Trends and observations on the collection, testing and use of blood and blood components in Europe. 2001–2008 report. Strasbourg: Directorate for the quality of medicines and healthcare of the Council of Europe (EDQM); 2014. [Google Scholar]
- 12.Surial B, Burkhart A, Terliesner N, et al. Adherence to transfusion guidelines: are we prepared for the Smarter Medicine or Choosing Wisely initiative? Swiss Med Wkly. 2015;145:w14084. doi: 10.4414/smw.2015.14084. [DOI] [PubMed] [Google Scholar]
- 13.Holst LB, Petersen MW, Haase N, et al. Restrictive versus liberal transfusion strategy for red blood cell transfusion: systematic review of randomised trials with meta-analysis and trial sequential analysis. BMJ. 2015;350:h1354. doi: 10.1136/bmj.h1354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim Y, Spolverato G, Lucas DJ, et al. Red cell transfusion triggers and postoperative outcomes after major surgery. J Gastrointest Surg. 2015;19:2062–73. doi: 10.1007/s11605-015-2926-9. [DOI] [PubMed] [Google Scholar]
- 15.Gross I, Seifert B, Hofmann A, et al. Patient blood management in cardiac surgery results in fewer transfusions and better outcome. Transfusion. 2015;55:1075–81. doi: 10.1111/trf.12946. [DOI] [PubMed] [Google Scholar]
- 16.So-Osman C, Nelissen RG, Koopman-van Gemert AW, et al. Patient blood management in elective total hip- and knee-replacement surgery (part 2): a randomized controlled trial on blood salvage as transfusion alternative using a restrictive transfusion policy in patients with a preoperative hemoglobin above 13 g/dl. Anesthesiology. 2014;120:852–60. doi: 10.1097/ALN.0000000000000135. [DOI] [PubMed] [Google Scholar]
- 17.So-Osman C, Nelissen RG, Koopman-van Gemert AW, et al. Patient blood management in elective total hip- and knee-replacement surgery (Part 1): a randomized controlled trial on erythropoietin and blood salvage as transfusion alternatives using a restrictive transfusion policy in erythropoietin-eligible patients. Anesthesiology. 2014;120:839–51. doi: 10.1097/ALN.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 18.Gombotz H, Rehak PH, Shander A, et al. Blood use in elective surgery: the Austrian benchmark study. Transfusion. 2007;47:1468–80. doi: 10.1111/j.1537-2995.2007.01286.x. [DOI] [PubMed] [Google Scholar]
- 19.Gombotz H, Rehak PH, Shander A, et al. The second Austrian benchmark study for blood use in elective surgery: results and practice change. Transfusion. 2014;54:2646–57. doi: 10.1111/trf.12687. [DOI] [PubMed] [Google Scholar]
- 20.Volken T, Buser A, Holbro A, et al. Blood donor to inactive donor transition in the Basel region between 1996 and 2011: a retrospective cohort study. Vox Sang. 2015;109:155–62. doi: 10.1111/vox.12269. [DOI] [PubMed] [Google Scholar]
- 21.Lattimore S, Wickenden C, Brailsford SR. Blood donors in England and North Wales: demography and patterns of donation. Transfusion. 2015;55:91–9. doi: 10.1111/trf.12835. [DOI] [PubMed] [Google Scholar]
- 22.Shaz BH, James AB, Hillyer KL, et al. Demographic patterns of blood donors and donations in a large metropolitan area. J Natl Med Assoc. 2011;103:351–7. doi: 10.1016/s0027-9684(15)30316-3. [DOI] [PubMed] [Google Scholar]
- 23.Veldhuizen IJ, Doggen CJ, Atsma F, et al. Donor profiles: demographic factors and their influence on the donor career. Vox Sang. 2009;97:129–38. doi: 10.1111/j.1423-0410.2009.01201.x. [DOI] [PubMed] [Google Scholar]
- 24.Smith A, Matthews R, Fiddler J. Blood donation and community: exploring the influence of social capital. Int J Soc Inquiry. 2011;4:45–63. [Google Scholar]
- 25.Hyndman RJ, Akram M, Archibald BC. The admissible parameter space for exponential smoothing models. AISM. 2008;60:407–26. [Google Scholar]
- 26.Hyndman RJ, Koehler AB, Snyder RD, et al. A state space framework for automatic forecasting using exponential smoothing methods. Int J Forecasting. 2002;18:439–54. [Google Scholar]
- 27.Burkom HS, Murphy SP, Shmueli G. Automated time series forecasting for biosurveillance. Stat Med. 2007;26:4202–18. doi: 10.1002/sim.2835. [DOI] [PubMed] [Google Scholar]
- 28.van Hoeven LR, Janssen MP, Rautmann G. The collection, testing and use of blood and blood components in Europe EDQM 2012 report. Strasbourg: Directorate for the quality of medicines and healthcare of the Council of Europe (EDQM); 2015. [Google Scholar]
- 29.Swiss Federal Statistical Office. Bevölkerungsstand und Bevölkerungswachstum. 2016. [Accessed on 10/02/2016]. Available at: http://www.bfs.admin.ch/bfs/portal/de/index/themen/01/02/blank/key/bevoelkerungsstand.html.
- 30.Modell B, Darlison M. Global epidemiology of haemoglobin disorders and derived service indicators. Bulletin of the World Health Organization. 2008. [Accessed on 03/02/2016]. Available at: http://www.who.int/bulletin/volumes/86/6/06-036673/en/ [DOI] [PMC free article] [PubMed]