Abstract
Objectives
The aims of the research are to examine the problems of abnormal menopausal women: the relationship between depression and menopausal-specific quality of life (MENQOL)-symptoms among postmenopausal women; the association of MENQOL-symptoms between pre- and postmenopausal female society in Bangladeshi real community.
Methods
This cross sectional study was conducted on 435 women of Tangail, aged (≥ 17) years, using a structured questionnaire where is inaacluded the information of MENQOL and one of the main outcomes “depression” is measured by beck depression inventory.
Results
Menopausal status and MENQOL symptoms (except pain) are significantly (P < 0.05) associated. By using post-hoc analysis, the proportion of menopausal women, classified as having a depressive mood of early menopause is significantly higher than natural-menopause. Among postmenopausal women, there is a significant correlation between “concentration problem” and “depression”. Here mean depression score (29.40 ± 6.42) of menopausal women who have any difficulty in concentrating is higher than mean depression score (20.89 ± 6.64) of menopausal women who have no difficulty in concentrating. Another six factors (osteoporosis, heart-beating, fatigue, pressure, tingling, headaches) of MENQOL-symptoms were significantly correlated with depression and P-values are 0.000, 0.000, 0.000, 0.033, 0.006, and 0.002, respectively. Finally the presence of “difficulty in concentrating” and “fatigue” are strongly associated factors with depression score (P < 0.001).
Conclusions
The early postmenopausal women have to face more psychological problems (e.g., depression) compare to others. Among postmenopausal women, there is no significant relation between depression and vasomotor symptom (e.g., hot-flashes) perspective to menopausal female society of Bangladesh.
Keywords: Bangladesh, Depression, Menopause, Quality of life
Introduction
The quality of life (QOL) based on health-related issues is a multidimensional health concept that includes social, physical, and mental day-to-day functional areas of life.1,2 Besides, it encompasses several significant domains like subjective well-being role disability and psychological functions. Every woman has a significant experience of QOL after menopause. In menopause, a woman passes about a third of her own life with the heightening life expectancy.3 All women recognize the term menopause in their life when their regular menstrual cycle has stopped for one year. So, menopause is a reproductive phenomenon.3 If menopause has happened in abnormal time then every women have to face much difficulties in QOL. It is also well known that every menopausal symptom have effect on QOL of pre and postmenopausal women. But it varies according to life style; vasomotor symptoms have lower impact on QOL of Asian menopausal women compare to western.4,5 In addition, North American and European menopausal women show higher rates of symptoms than Asian menopausal women.6 It is nicely showed that the reasons behind those differences were possibly cultural or genetically.6,7,8
The impact of menopause on QOL is a consequence of social, physical and mental changes. It is highly visible that socio-economic and cultural factors influence the menopausal transition.7 But it varies from region to region, country to country according to their culture. Like, in western countries, night sweating, hot flushes are the major menopausal symptoms of women but not in Asia.5 So the vasomotor symptoms as well as natural menopausal time have been varied from one cultural region to another. The 45 to 55 years range is called natural menopausal time of a women.9 But perspective to Bangladesh, 40 to 50 years range is treated as natural menopausal time.10 In the research work, before 45 years of a menopausal women treated as early postmenopausal candidate and after 50 years of a menopausal women is treated as late postmenopausal candidate. Every menopausal woman faces many psychological as well as physical problems.3 But premenopausal or postmenopausal women may be facing more or less difficulties of QOL. For menopause, postmenopausal women have to face indicative impacts on her social, daily and sexual life.11,12 Several health criteria like insomnia, tiredness, hot flashes, sweats, hair loss etc. are changed significantly in her body. Besides, having depressive mood among postmenopausal women is a subject of debate for decades. Postmenopausal women have more depressive mood which was found in earlier clinic based study.13 On the other hand, different community based study shows that depression is not more frequent in peri- or postmenopausal women.14,15
Actually, depression is a crippling condition leads to indicative societal, personal and economic costs.16 A several number of both prospective and cross-sectional studies have inquired a potential affiliation between the risks for depressive symptoms or major depressive disorder (MDD; new onset or recurrent) and distinguishable menopause staging.17 Bromberger et al.18 concluded in their study that transition of menopause considered as a vulnerable period to MDD recurrence, while two important risk factors (health factors and vasomotor symptoms) should be considered first lifetime-onset of MDD during midlife. Juang et al.19 also concluded that post- and perimenopausal women with hot flashes were affiliated with depressive and anxious symptoms in East Asian population.
But there are published very few articles by indicating QOL of menopausal women. In Southeast Asia20 menopausal symptoms have not been excessively studied like Western countries. Perspective to developing country like Bangladesh, the documentations about menopausal women are very poor. In 2016, Ahmed et al.10 provided the information about QOL of menopausal women in Bangladesh. But they did not work on premenopausal women and there was not shown the relationship between pre- and postmenopausal women's altitude and QOL. Though this research is an advancement of Ahmed's work, the aim of this research is to examine the problems of abnormal menopausal women in a Bangladeshi real community and also investigate the relationship between pre and postmenopausal women's altitude and QOL. In addition, another major purpose of the present study was to examine whether the relationship between depression and menopausal-specific QOL (MENQOL) symptoms (vasomotor, psychological and physical) exists or not among postmenopausal women in Bangladesh.
Materials and Methods
1. Subjects and sample design
This cross-sectional study was conducted among rural women in Tangail district in Bangladesh. On the basis of area, Tangail district is the greatest district of Dhaka division and one of the central regions of Bangladesh. Also it is the second greatest district of Dhaka division by population. The study mainly adopted cluster sampling procedure in which villages were to be counted as a cluster. A total of 10 clusters were proposed for the survey. The clusters were selected using systematic probability proportionate to size sampling procedure. A total of 435 responders aged (≥ 17) years were collected. Actually sample size was determined by using,
| n = z2 [p(1−p)/d2] |
Where,
n = sample size
z = two-sided normal variate at 95% confidence level (1.96)
P = indicator percentage
d = precision.
By applying this formula the minimum required sample was 384. In this study, data were collected from 435 women by face to face interview method on the basis of a structured questionnaire. Interviews were conducted between participant and well-trained interviewer. Classification and menopausal definition of the data: In first stage of this study, we classified the total completed participants into two groups such as “premenopausal women” and “postmenopausal women”. This classification is defined according to other study conducted on women in Bangladesh.21 Premenopausal women indicated those women who had regular menstrual bleeding during last one year and postmenopausal women were defined as those who had ascertained that their last menstrual bleeding happened at least 1 year previously. Women were defined as perimenopausal if they had experienced irregular menstrual cycles within last 1 year or last menses to be 3 months previously but less than 12 months.
In second stage, postmenopausal women were classified in three groups concerning to our objectives. These were “Early postmenopausal women”, “Natural postmenopausal women”, “Late postmenopausal women”. Women were included in early postmenopausal group whose menstruation cycles stopped before 45 years old, whose cycles were stopped between 45 to 50 years old they were included in natural postmenopausal group and late postmenopausal women were indicated those women whose cycles were stopped after 50 years old. The classifications we made according to several studies.3,9,22
Instruments and assessment of depression: The structured questionnaire was developed in 3 steps. In first step, the study was included the information of the participants on the basis of socio-economic characteristics; in second step, we included the information of MENQOL;23 in third step the information of depression were collected according to Beck depression inventory.24 MENQOL consists of four domains i.e vasomotor, physical, psychological and sexual. It was applied in several worldwide studies like Thailand,25 Europe,26 Asian women.27 Here we ignored sexual domain in our study because of reluctance of participants about these types of questions.
In Beck depression inventory, there were 21 questions. On the basis of these questions, four categories were developed (such as “no depression”, “mild depression”, “moderate depression” and “severe depression”). For our convenience, we made two categories (depressed and mild depressed). “Moderate depression” and “severe depression” were included in depressed group. “No depression” and “mild depression” were included in mild depressed group. Beck depression scale was converted in Bangla language which was approved by the doctor of Bangabandhu Sheikh Mujib Medical University (BSMMU). The study was approved by the local committees at the participating centers and “Bio-photomatiχ” Research and Ethics Committee, Mawlana Bhashani Science and Technology University.
2. Data cleaning
Data is inconsistent, noisy and incomplete in the existed world.28,29 Raw data is highly susceptible to missing values or inconsistency and affected the result analysis process. So, data cleaning is a mandatory step for mining or statistical analysis.30,31 At the primary stage we collected information from 435 women for the study. Then we excluded 23 data because of missing values. Also we ignored the data of perimenopausal women, divorced women and those women who had history of hysterectomy. We didn't get those women who had the case of surgical menopause during our data collection time. So our final participants were 346 women.
3. Statistical Analysis
For statistical analysis we have used SPSS for windows version 20 (SPSS Inc., Chicago, IL, USA). In this study, first descriptive results and χ2 test for (2 × 2) table for the completed data were determined where all categorical variables were dichotomous. Then we used χ2 test of homogeneity and post-hoc test (also known as pairwise comparisons). Furthermore, bonferroni adjustment to correct multiple comparisons was included. We have also used point-biserial correlation and hierarchical regression in this research. All required assumptions were checked before and we considered P < 0.05 value as statistically significant result.
Results
1. Characteristics of the study population
The age range of total postmenopausal women was 40 to 90 years where the mean ± standard deviation (SD) age was 60.78 ± 10.24 years and the age range of premenopausal women was 19 to 25 years with mean ± SD age was 22.83 ± 1.12. Among 206 postmenopausal women, 69 women had knowledge about menopause. Mean ± SD age difference from their husband was 12.27 ± 4.17 which is not shown in the Table.
2. MENQOL symptoms
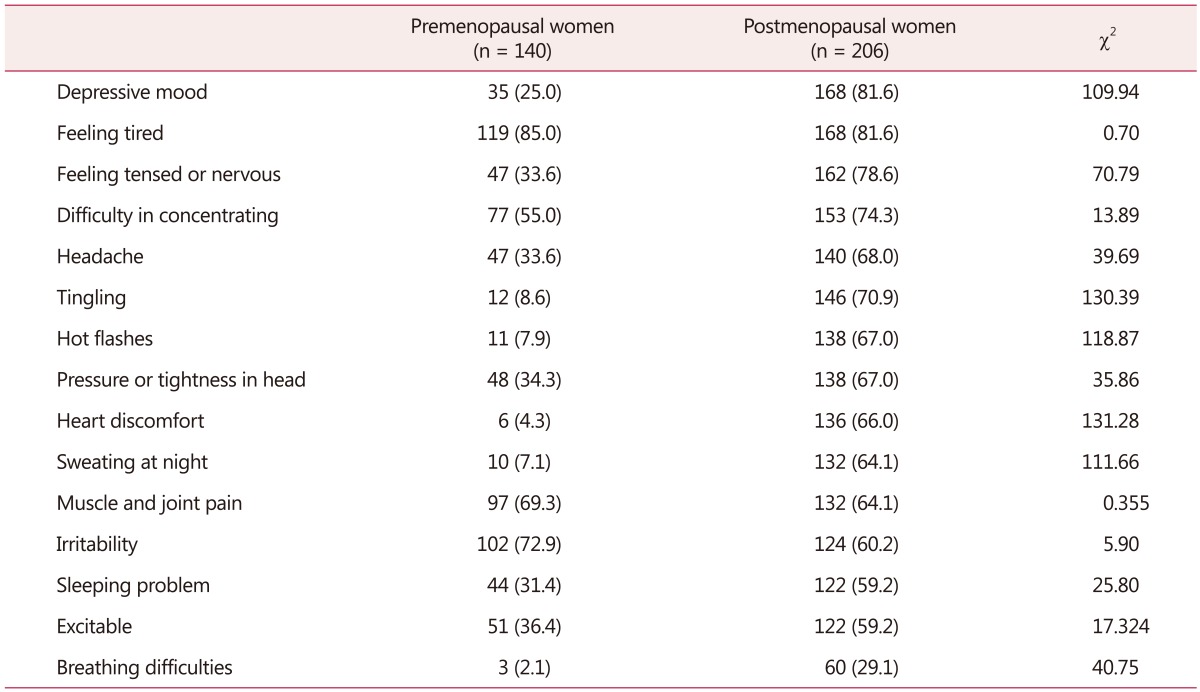
Table 1 represents frequencies of the menopausal symptoms and χ2 value that represents the association of the symptoms between two groups (premenopausal women and postmenopausal women). Here 69.3% women are abided by muscle and joint pain among premenopausal women and 64.1% women are abided among postmenopausal women. Individual measures of association between menopausal status and all other symptoms except muscle and joint pain are significantly (P < 0.05) associated.
Table 1. Frequency distribution and association about menopause-specific quality of life questionnaire symptoms between premenopausal and post-menopausal women.
The data is presented as n (%)
3. Depression in early (< 45) menopausal women
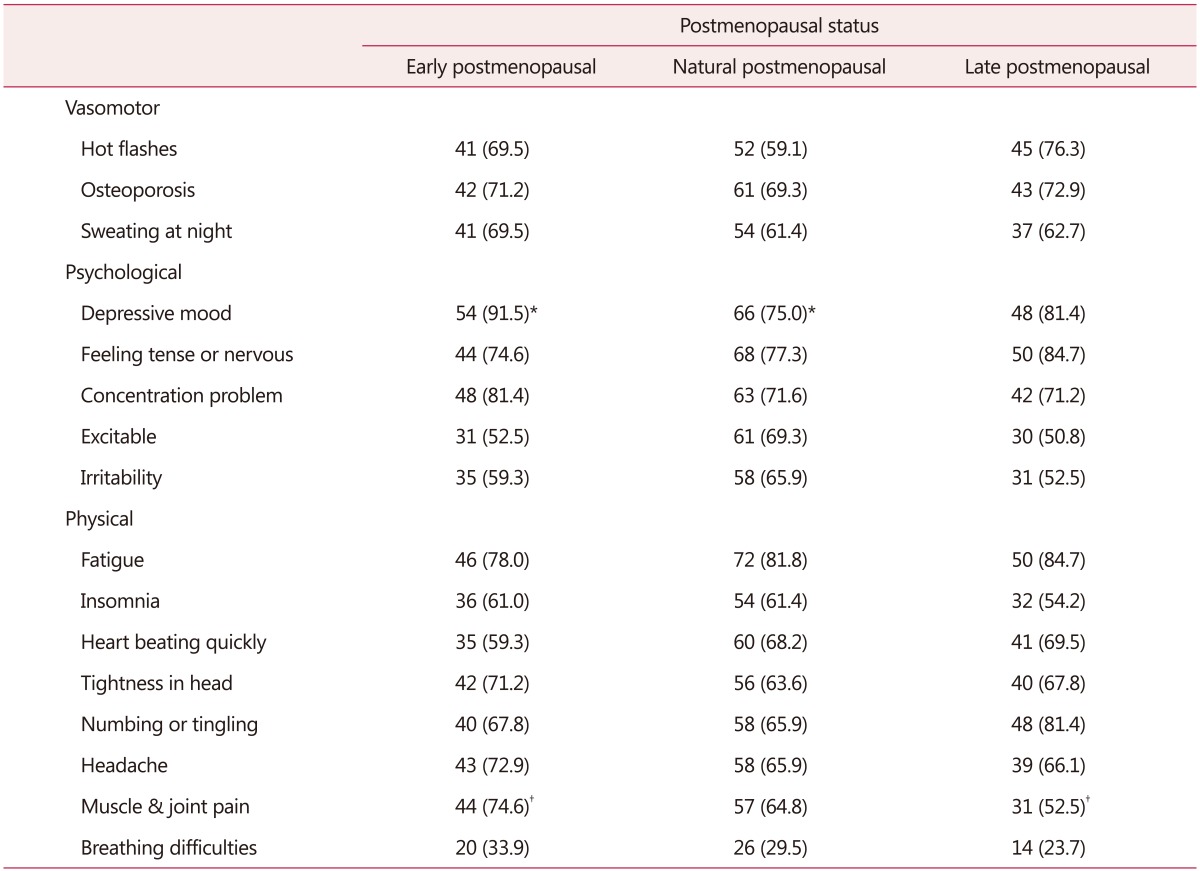
Table 2 shows the result of χ2 test of homogeneity. It is explored that the proportional differences lie between three menopausal age groups i.e., early menopausal women (< 45 years), natural menopausal women (45–50 years), late menopausal women (> 50 years). On the basis of post-hoc analysis, the proportion of menopausal women classified as having depressive mood of early age at menopause was significantly higher than normal age at menopause, P < 0.05. The proportion of women classified as having depressive mood at normal age of menopause was not significantly different with the late age at menopause, P > 0.05. Again the proportion of menopausal women classified as having muscle and joint pain of early age at menopause was significantly higher than late age at menopause, P < 0.05 and there was no significant proportional different between early age at menopause and normal age at menopause, P > 0.05.
Table 2. Comparisons about menopause-specific quality of life questionnaire symptoms among three groups of post-menopausal women.
The data is presented as n (%)
*Significant difference P < 0.05 between early and natural postmenopausal
†Significant difference P < 0.05 between early and late postmenopausal
4. Depressive mood effect on QOL among
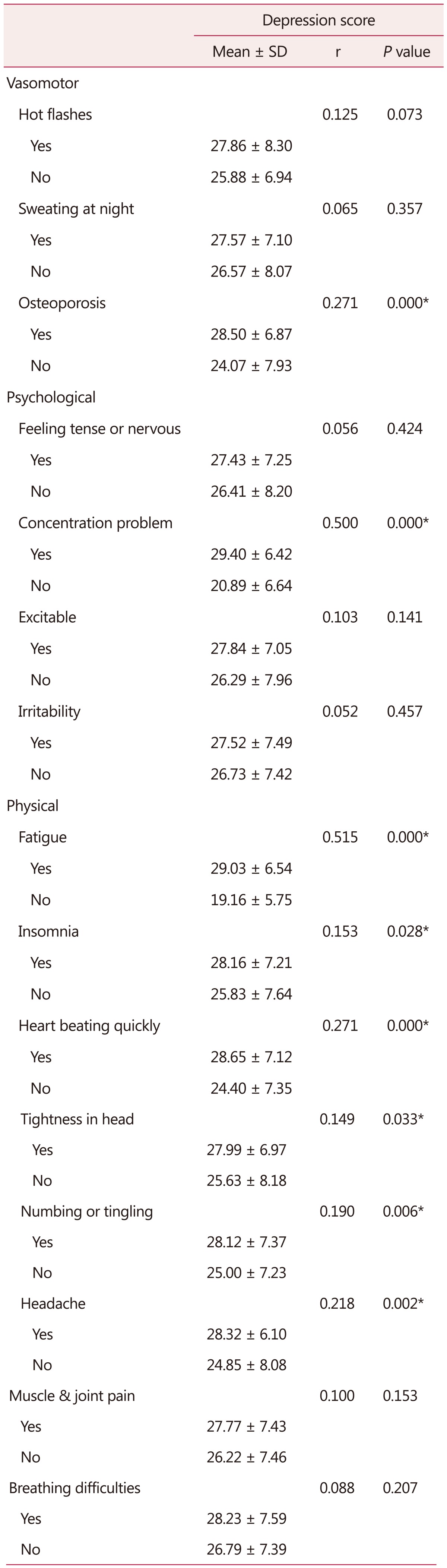
A point-biserial correlation has been run individually between Beck depression score and MENQOL symptoms of menopausal women in Bangladesh. There are eight factors significantly (P < 0.05) correlated with depression which is shown in Table 3. Among them one factor is in vasomotor symptoms, one factor is in psychological symptoms and six factors are in physical symptoms. In vasomotor symptoms only osteoporosis is significantly (P = 0.000, P < 0.05) correlated with depression score. There were 146 women who have osteoporosis and their mean depression score (28.50 ± 6.87) was higher than mean depression score (24.07 ± 7.93) of 60 women who didn't have osteoporosis. In psychological symptoms, there was significant correlation between “difficulty in concentrating” and “depression”, P-value is 0.000 (P < 0.05). Here mean depression score (29.40 ± 6.42) of menopausal women who have difficulty in concentrating is higher than mean depression score (20.89 ± 6.64) of menopausal women who have no difficulty in concentrating. Another six factors (heart beating quickly, fatigue, pressure or tightness in head or body, numbing or tingling, headaches) of physical symptoms are significantly correlated with depression score and P-values are (0.000, 0.000, 0.033, 0.006, 0.002) respectively. Total result of point-biserial correlation is shown in Table 3.
Table 3. Correlation between depression score and menopause-specific quality of life questionnaire symptoms.
*Significant
SD: standard deviation
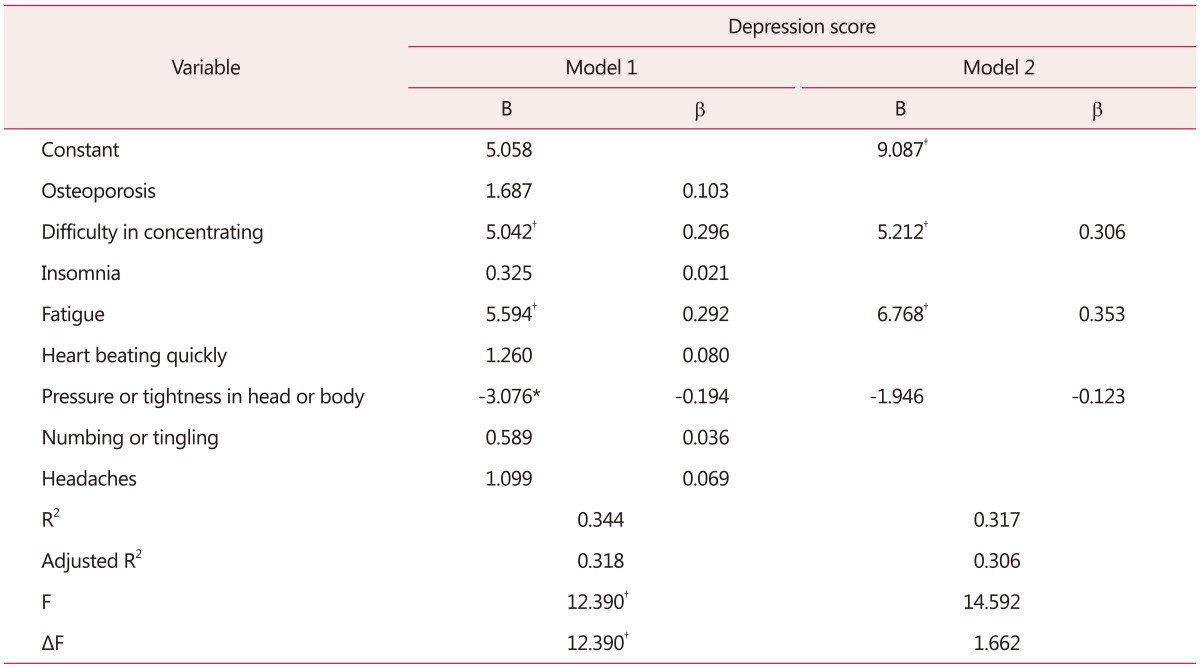
5. Relationship of depression, fatigue, concentration problem
We have carried out hierarchical multiple regression to ensure that which factors are severally consociated with the depression scores (Table 4). The several factors have been chosen which are individually correlated with depression score (Table 3). The presence of “difficulty in concentrating” and “fatigue” are strongly associated factors with depression score (P < 0.001). “Pressure or tightness in head or body” is also an associated factor with depression score. It is the result of model 1 in Table 4. In model 2 of Table 4, we have included only three factors which show significant association in model 1. The results are explored that two factors are strongly associated with depression score except “pressure or tightness in head or body”. Model 1 and Model 2 both are statistically significantly predicts the depression score (For model 1, F = 12.390; P = 0.000 and for model 2, F = 14.592; P = 0.000). The analysis of variance Table is not shown here.
Table 4. Hierarchical regression model of variables and their association with depression score of beck depression scale.
*P < 0.05
†P < 0.001
B: unstandardized regression coefficient, β: standardized regression coefficient, R2: squared multiple correlation coefficient, F: Fisher ratio
Discussion
In this study, the mean ages of the early menopausal women, natural menopausal women and late menopausal women were 55.37 years, 62.75 years and 63.25 years respectively and the overall mean ± SD age of total menopausal women was 60.78 ± 10.24 years which is greater than the other studies in other places21,32,33 across Bangladesh, in British women (50 ± 4.9 years),34 and the age range of premenopausal women was 19 to 25 years with mean ± SD age was 22.83 ± 1.12. It is lower than other study conducted on rural women in Bangladesh (31.36 years).21 There are three groups of postmenopausal women in this study. Among them 59 women are in early (< 45 years) postmenopausal group, 88 women are in normal (45–50 years) postmenopausal group, 59 women are in late (> 50 years) menopausal group. Comparatively it is higher than the study of urban women of extreme northern India.3
From Table 1 we have got that postmenopausal women are more depressed than premenopausal women perspective to Bangladeshi women. This result is different from the study of Juang et al.19 as they revealed that depression is not associated with menopausal status and the study of Cheng et al.1 found that fewer postmenopausal women had depression because of menopause and both study were conducted on middle aged women of Taiwan. On the other hand our findings are also similar to other studies carried on in Bangladesh33 and also other worldwide studies.16,18,35 So, depressive mood is a significant symptom for postmenopausal women compared to premenopausal women in case of women in Bangladesh.
On the other hand, no significant results have found in case of muscle and joint pain among menopausal symptoms perspective to Bangladeshi postmenopausal women compared to premenopausal women. In the study, the information of perimenopausal women was not included. But Islam et al.36 included perimenopausal women in their study which was conducted on Bangladeshi women, got joint pain as significant symptoms for both perimenopausal and postmenopausal women compared to premenopausal women. In our study, we have got that 35.9% postmenopausal women and 21.4% premenopausal women have faced muscle and joint pain. But there was no significant proportional difference between two groups. Except muscle and joint pain, all other symptoms (vasomotor, psychological and physical) of QOL are significant for postmenopausal women compared to premenopausal women. This result shows similarity to other study of Asian countries like.3,7,33
The study has determined proportional differences among three postmenopausal groups (early postmenopausal, natural postmenopausal and late postmenopausal) in case of MENQOL symptoms. Hence, the result also shows that early postmenopausal group has more depressed than natural postmenopausal group. With our best knowledge, this is the meaningful unique outcome and comparison among early three postmenopausal groups perspective to menopausal female society of Bangladesh. So, early postmenopausal women have to face so many difficulties in psychological (e.g., depressive mood) perspective. There is another significant proportional difference exist between early and late postmenopausal group with respect to muscle and joint pain.
In addition, it is also investigated that how depressive mood influence the QOL among postmenopausal women in the study. Juang et al.19 showed in their study that there is a significant relation between vasomotor symptoms and depressive mood. They seemed that night sweating may be caused of insomnia. That's why they confounded night sweating with insomnia in their analysis. In the study, we have used χ2 test between insomnia and sweating at night and have got insignificant (P > 0.05) result between them. So, sweating at night with insomnia is not confounded in our analysis. From Table 3 it can be said that there is no significant relationship between vasomotor symptoms (hot flashes, night sweating) and depressive mood. Though Juang et al.19 used hospital anxiety and depression scale (HADS) for measuring anxiety and depression score, while we have used Beck depression inventory for measuring depression of the participants. Another study said that there is strong positive relationship between depression and osteoporosis.37 Any significant (P = 0.073) relationship between “hot flashes” and “depression” among postmenopausal women are not found in this research. Meanwhile, we have obtained significant relationship between osteoporosis and depression. So, perspective to Bangladeshi women, there is no significant relationship between “hot flashes” and “depression” among postmenopausal women.
The result of hierarchical regression have showed that fatigue and concentration problem are associated significantly with depression among postmenopausal women even after controlling all other factors (those were individually correlated with depression). In psychological point of view, there is relation between fatigue and depression;38,39 between concentration problem and depression.40 Finally it can be concluded that there is strong association between fatigue and depressed postmenopausal women; between concentration problem and depressed postmenopausal women perspective Bangladesh. The findings show the similarities among the women of Kinmen island,2 European women,41 Ecuadorian women,42 Italian women,43 Canadian women,44 Iranian women.45
This study has some limitations like other cross sectional studies. Comparatively a small number of data were collected for the study. For large number of data from different places the frequency of QOL symptoms of menopausal women might be changed. The age range of premenopausal women was 19 to 25. Results might be changed for large age range of premenopausal women. The information about osteoporosis was not collected from premenopausal women.
Conclusion
On the basis of the study, it can be concluded that early postmenopausal women faced so many difficulties psychologically (e.g., depression). Among postmenopausal women depression is associated with fatigue and concentration problem. But there is no significant relation between vasomotor symptom (e.g., hot flashes) and depression perspective to rural postmenopausal women in Tangail district in Bangladesh. In addition, the final result suggested that psychological symptoms are strongly correlated with menopausal women and have significant impact on QOL of early postmenopausal women than late postmenopausal women perspective to Bangladesh.
Acknowledgement
The authors are grateful to the participants who contributed to this research.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Cheng MH, Lee SJ, Wang SJ, Wang PH, Fuh JL. Does menopausal transition affect the quality of life? A longitudinal study of middle-aged women in Kinmen. Menopause. 2007;14:885–890. doi: 10.1097/GME.0b013e3180333a58. [DOI] [PubMed] [Google Scholar]
- 2.Fuh JL, Wang SJ, Lee SJ, Lu SR, Juang KD. Quality of life and menopausal transition for middle-aged women on Kinmen island. Qual Life Res. 2003;12:53–61. doi: 10.1023/a:1022074602928. [DOI] [PubMed] [Google Scholar]
- 3.Sharma S, Tandon VR, Mahajan A. Menopausal symptoms in urban women. JK Sci. 2007;9:13–17. [Google Scholar]
- 4.Tang GW. The climacteric of Chinese factory workers. Maturitas. 1994;19:177–182. doi: 10.1016/0378-5122(94)90069-8. [DOI] [PubMed] [Google Scholar]
- 5.Boulet MJ, Oddens BJ, Lehert P, Vemer HM, Visser A. Climacteric and menopause in seven South-east Asian countries. Maturitas. 1994;19:157–176. doi: 10.1016/0378-5122(94)90068-x. [DOI] [PubMed] [Google Scholar]
- 6.Dennerstein L. Well-being, symptoms and the menopausal transition. Maturitas. 1996;23:147–157. doi: 10.1016/0378-5122(95)00970-1. [DOI] [PubMed] [Google Scholar]
- 7.Ayranci U, Orsal O, Orsal O, Arslan G, Emeksiz DF. Menopause status and attitudes in a Turkish midlife female population: an epidemiological study. BMC Womens Health. 2010;10:1. doi: 10.1186/1472-6874-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brown DE, Sievert LL, Morrison LA, Reza AM, Mills PS. Do Japanese American women really have fewer hot flashes than European Americans? The Hilo Women's Health Study. Menopause. 2009;16:870–876. doi: 10.1097/gme.0b013e31819d88da. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.World Health Organization. Research on the menopause in the 1990s: Report of a WHO scientific group. Geneva, CH: World Health Organization; 1994. [PubMed] [Google Scholar]
- 10.Ahmed K, Jahan P, Nadia I, Ahmed F, Abdullah Al E. Assessment of menopausal symptoms among early and late menopausal midlife Bangladeshi women and their impact on the quality of life. J Menopausal Med. 2016;22:39–46. doi: 10.6118/jmm.2016.22.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kwak EK, Park HS, Kang NM. Menopause knowledge, attitude, symptom and management among midlife employed women. J Menopausal Med. 2014;20:118–125. doi: 10.6118/jmm.2014.20.3.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim HK, Kang SY, Chung YJ, Kim JH, Kim MR. The recent review of the genitourinary syndrome of menopause. J Menopausal Med. 2015;21:65–71. doi: 10.6118/jmm.2015.21.2.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ihezue UH, Kumaraswamy N. Prevalence of depressive symptoms among patients attending a general outpatient clinic. Acta Psychiatr Scand. 1986;73:395–398. doi: 10.1111/j.1600-0447.1986.tb02701.x. [DOI] [PubMed] [Google Scholar]
- 14.Matthews KA, Wing RR, Kuller LH, Meilahn EN, Kelsey SF, Costello EJ, et al. Influences of natural menopause on psychological characteristics and symptoms of middle-aged healthy women. J Consult Clin Psychol. 1990;58:345–351. doi: 10.1037//0022-006x.58.3.345. [DOI] [PubMed] [Google Scholar]
- 15.Mitchell ES, Woods NF. Symptom experiences of midlife women: observations from the Seattle Midlife Women's Health Study. Maturitas. 1996;25:1–10. doi: 10.1016/0378-5122(96)01047-x. [DOI] [PubMed] [Google Scholar]
- 16.Soares CN. Depression and menopause: Current knowledge and clinical recommendations for a critical window. Psychiatr Clin North Am. 2017;40:239–254. doi: 10.1016/j.psc.2017.01.007. [DOI] [PubMed] [Google Scholar]
- 17.Bromberger JT, Kravitz HM, Chang YF, Cyranowski JM, Brown C, Matthews KA. Major depression during and after the menopausal transition: Study of Women's Health Across the Nation (SWAN) Psychol Med. 2011;41:1879–1888. doi: 10.1017/S003329171100016X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bromberger JT, Schott L, Kravitz HM, Joffe H. Risk factors for major depression during midlife among a community sample of women with and without prior major depression: are they the same or different? Psychol Med. 2015;45:1653–1664. doi: 10.1017/S0033291714002773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Juang KD, Wang SJ, Lu SR, Lee SJ, Fuh JL. Hot flashes are associated with psychological symptoms of anxiety and depression in peri- and post- but not premenopausal women. Maturitas. 2005;52:119–126. doi: 10.1016/j.maturitas.2005.01.005. [DOI] [PubMed] [Google Scholar]
- 20.Rahman SA, Zainudin SR, Mun VL. Assessment of menopausal symptoms using modified Menopause Rating Scale (MRS) among middle age women in Kuching, Sarawak, Malaysia. Asia Pac Fam Med. 2010;9:5. doi: 10.1186/1447-056X-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jesmin S, Islam AM, Akter S, Islam MM, Sultana SN, Yamaguchi N, et al. Metabolic syndrome among pre- and post-menopausal rural women in Bangladesh: result from a population-based study. BMC Res Notes. 2013;6:157. doi: 10.1186/1756-0500-6-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Panay N. Menopause and the postmenopausal women. In: Edmonds DK, editor. Dewhurst's textbook of obstetrics and gynaecology. 7th ed. London, UK: Blackwell Publishing; 2007. pp. 479–494. [Google Scholar]
- 23.Nisar N, Sohoo NA. Frequency of menopausal symptoms and their impact on the quality of life of women: a hospital based survey. J Pak Med Assoc. 2009;59:752–756. [PubMed] [Google Scholar]
- 24.Beck AT, Steer RA, Brown GK. Beck depression inventory-II. San Antonio, TX: The Psychological Corporation; 1996. [Google Scholar]
- 25.Peeyananjarassri K, Cheewadhanaraks S, Hubbard M, Zoa Manga R, Manocha R, Eden J. Menopausal symptoms in a hospital-based sample of women in southern Thailand. Climacteric. 2006;9:23–29. doi: 10.1080/13697130500487422. [DOI] [PubMed] [Google Scholar]
- 26.Dodin S, Lemay A, Jacques H, Légaré F, Forest JC, Mâsse B. The effects of flaxseed dietary supplement on lipid profile, bone mineral density, and symptoms in menopausal women: a randomized, double-blind, wheat germ placebo-controlled clinical trial. J Clin Endocrinol Metab. 2005;90:1390–1397. doi: 10.1210/jc.2004-1148. [DOI] [PubMed] [Google Scholar]
- 27.Limpaphayom KK, Darmasetiawan MS, Hussain RI, Burriss SW, Holinka CF, Ausmanas MK. Differential prevalence of quality-of-life categories (domains) in Asian women and changes after therapy with three doses of conjugated estrogens/medroxyprogesterone acetate: the Pan-Asia Menopause (PAM) study. Climacteric. 2006;9:204–214. doi: 10.1080/13697130600722520. [DOI] [PubMed] [Google Scholar]
- 28.Ahmed K, Emran AA, Jesmin T, Mukti RF, Rahman MZ, Ahmed F. Early detection of lung cancer risk using data mining. Asian Pac J Cancer Prev. 2013;14:595–598. doi: 10.7314/apjcp.2013.14.1.595. [DOI] [PubMed] [Google Scholar]
- 29.Ahmed K, Jesmin T, Rahman MZ. Early prevention and detection of skin cancer risk using data mining. Int J Comput Appl. 2013 doi: 10.5120/10065-4662. [DOI] [PubMed] [Google Scholar]
- 30.Asaduzzaman S, Chakraborty S, Hossain MG, Bashar MI, Bhuiyan T, Paul BK, et al. Hazardous consequences of polygamy, contraceptives and number of childs on cervical cancer in a low incoming country: Bangladesh. Cumhuriyet Univ Fac Sci. 2016;37:74–84. [Google Scholar]
- 31.Ahmed K, Asaduzzaman S, Bashar MI, Hossain G, Bhuiyan T. Association assessment among risk factors and breast cancer in a low income country: Bangladesh. Asian Pac J Cancer Prev. 2015;16:7507–7512. doi: 10.7314/apjcp.2015.16.17.7507. [DOI] [PubMed] [Google Scholar]
- 32.Rahman S, Salehin F, Iqbal A. Menopausal symptoms assessment among middle age women in Kushtia, Bangladesh. BMC Res Notes. 2011;4:188. doi: 10.1186/1756-0500-4-188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tanira S, Wazed F, Sutlana A, Amin R, Sutlana K, Ahmad S. Knowledge, attitude and experience of menopause an urban based study in Bangladesh. J Dhaka Med Coll. 2009;18:33–36. [Google Scholar]
- 34.Lawlor DA, Ebrahim S, Smith GD. The association of socioeconomic position across the life course and age at menopause: the British Women's Heart and Health Study. BJOG. 2003;110:1078–1087. [PubMed] [Google Scholar]
- 35.Freeman EW, Sammel MD, Lin H, Nelson DB. Associations of hormones and menopausal status with depressed mood in women with no history of depression. Arch Gen Psychiatry. 2006;63:375–382. doi: 10.1001/archpsyc.63.4.375. [DOI] [PubMed] [Google Scholar]
- 36.Islam RM, Bell RJ, Billah B, Hossain MB, Davis SR. Prevalence and severity of vasomotor symptoms and joint pain in women at midlife in Bangladesh: a population-based survey. Menopause. 2016;23:731–739. doi: 10.1097/GME.0000000000000615. [DOI] [PubMed] [Google Scholar]
- 37.Gold DT, Solimeo S. Osteoporosis and depression: a historical perspective. Curr Osteoporos Rep. 2006;4:134–139. doi: 10.1007/s11914-996-0021-6. [DOI] [PubMed] [Google Scholar]
- 38.Janardhan V, Bakshi R. Quality of life in patients with multiple sclerosis: the impact of fatigue and depression. J Neurol Sci. 2002;205:51–58. doi: 10.1016/s0022-510x(02)00312-x. [DOI] [PubMed] [Google Scholar]
- 39.Roscoe JA, Morrow GR, Hickok JT, Mustian KM, Griggs JJ, Matteson SE, et al. Effect of paroxetine hydrochloride (Paxil) on fatigue and depression in breast cancer patients receiving chemotherapy. Breast Cancer Res Treat. 2005;89:243–249. doi: 10.1007/s10549-004-2175-1. [DOI] [PubMed] [Google Scholar]
- 40.Arnau RC, Meagher MW, Norris MP, Bramson R. Psychometric evaluation of the Beck Depression Inventory-II with primary care medical patients. Health Psychol. 2001;20:112–119. doi: 10.1037//0278-6133.20.2.112. [DOI] [PubMed] [Google Scholar]
- 41.Glaus A, Boehme C, Thurlimann B, Ruhstaller T, Hsu Schmitz SF, Morant R, et al. Fatigue and menopausal symptoms in women with breast cancer undergoing hormonal cancer treatment. Ann Oncol. 2006;17:801–806. doi: 10.1093/annonc/mdl030. [DOI] [PubMed] [Google Scholar]
- 42.Chedraui P, Hidalgo L, Chavez D, Morocho N, Alvarado M, Huc A. Quality of life among postmenopausal Ecuadorian women participating in a metabolic syndrome screening program. Maturitas. 2007;56:45–53. doi: 10.1016/j.maturitas.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 43.Genazzani AR, Nicolucci A, Campagnoli C, Crosignani P, Nappi C, Serra GB, et al. Assessment of the QoL in Italian menopausal women: comparison between HRT users and non-users. Maturitas. 2002;42:267–280. doi: 10.1016/s0378-5122(02)00067-1. [DOI] [PubMed] [Google Scholar]
- 44.Blumel JE, Castelo-Branco C, Binfa L, Gramegna G, Tacla X, Aracena B, et al. Quality of life after the menopause: a population study. Maturitas. 2000;34:17–23. doi: 10.1016/s0378-5122(99)00081-x. [DOI] [PubMed] [Google Scholar]
- 45.Shobeiri F, Jenabi E, Hazavehei SM, Roshanaei G. Quality of life in postmenopausal women in Iran: A populationbased study. J Menopausal Med. 2016;22:31–38. doi: 10.6118/jmm.2016.22.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]