Abstract
Adolescent-onset major depressive disorder (MDD) is associated with an increased risk of recurrent depressive episodes, suicidal behaviors, and psychiatric morbidity throughout the lifespan. The objective of the present study was to investigate brain structural and functional changes in adolescent patients with MDD. Furthermore, we aimed to clarify the influence of early-life stress on brain function and structure. The study investigated adolescent patients with severe MDD (n=20, mean age=16.0, range=15–18 years) and a control sample of matched healthy adolescents (n=21, mean age=16.6, range=15–18 years). Functional MRI data were obtained using a face-matching paradigm to investigate emotion processing. Structural MRI data were analyzed using voxel-based morphometry (VBM). In line with previous studies on adult MDD, adolescent patients showed elevated amygdala activity to negative and reduced amygdala activity to positive emotional stimuli. Furthermore, MDD patients showed smaller hippocampal volumes compared to healthy adolescents. Higher levels of childhood maltreatment were associated with smaller hippocampal volumes in both depressed patients and healthy controls, whereby no associations between amygdala reactivity and childhood maltreatment were found. Our results suggest that hippocampal alterations in youth MDD patients may at least partly be traced back to higher occurrence of early-life adverse experiences. Regarding the strong morphometric impact of childhood maltreatment and its distinctly elevated prevalence in MDD populations, this study provides an alternative explanation for frequently observed limbic structural abnormalities in depressed patients.
Introduction
Major depressive disorder (MDD) is one of the most debilitating diseases worldwide (World Health Organization, 2001). In particular, adolescent-onset MDD is associated with increased risk of recurrent depressive episodes, suicidal behaviors, and psychiatric morbidity throughout the lifespan (Kessler and Walters, 1998). This underscores the importance to improve treatment and prevention. Although, our knowledge regarding neurobiological markers has increased for adult MDD, there is still a need for a more detailed understanding of the etiology, developmental psychopathology and biological implications in youth and adolescents.
In last two decades, an increasing amount of knowledge regarding neurobiological markers has been gained, pointing to functional and structural alterations in limbic and prefrontal cortical regions in adult patients with MDD (Du et al, 2012). In particular, amygdala dysfunction—including abnormally increased activation to negative (mood-congruent) stimuli—has been repeatedly reported for MDD (Epstein et al, 2006; Abler et al, 2007; Peluso et al, 2009; Stuhrmann et al, 2011). Furthermore, adult MDD patients show brain structural abnormalities, with volume reductions in the hippocampus and anterior cingulate gyrus (ACC) being among the most consistent findings (Arnone et al, 2012a). However, adult neurobiological findings may not be directly applicable to youth depression due to the high neuroplasticity and variability of brain development in adolescence.
While a large body of literature exists for adult MDD, fewer neuroimaging studies have directly investigated child or adolescent patients with MDD. To date, only a handful of studies have investigated emotion processing in depression during childhood and adolescence using neuroimaging techniques. These studies provide evidence that an increased amygdala reactivity to emotional—particularly to negative—stimuli is already present in adolescent subjects with MDD (Yang et al, 2010; Mingtian et al, 2012; Tao et al, 2012; Gaffrey et al, 2013; Hall et al, 2014) and that this increased sensitivity of the limbic system is positively associated with severity of depression (Mingtian et al, 2012) as well as with disruptions in parent-reported emotion regulation and negative affect (Gaffrey et al, 2013). Regarding brain structure, both depressed and healthy adolescents with high risk of depression show volume reduction within the hippocampal formation (Rosso et al, 2005; Rao et al, 2010), similar to findings in adults.
It is a well-documented fact that early abuse experiences increase the risk of developing depression in later life (Stirling and Amaya-Jackson, 2008). It is assumed that early-life stress leads to a sensitization of the limbic system even to mild stress, increasing the susceptibility to develop or maintain a depression. This is supported by a recent study reporting that hippocampal alterations in MDD patients may at least partly be traced back to higher occurrence of adverse experiences in early life (Opel et al, 2014). However, to date only one study has investigated the association between brain structure, early-life stress, and depression in adolescents, supporting the idea that the effects of early-life adversity on depression are partially mediated by smaller hippocampal volumes (Rao et al, 2010). However, this association, recently identified in healthy adults (Dannlowski et al, 2012, 2013), is less clear in healthy adolescents, especially in younger age (Teicher and Samson, 2016). In summary, there is broad evidence suggesting that chronic stress in early periods of life alters the physiological brain structural development. In turn, these structural alterations and dysfunctional neuroendocrine response to stressful life-events could be an important factor in the development of stress-related psychiatric disorders—particularly depression—in later life by increasing the vulnerability to the onset, as well as to an unfavorable course of mental illness. However, the underlying biological mechanisms and mediating pathways still need to be clarified. Hence, the main aim of this study is to bring maltreatment, depression, brain structure, and brain function together using two MRI methods (VBM and functional MRI) in a homogenous sample of adolescents.
Hence, the goals of the present study are:
To investigate brain functional changes to emotional stimuli in adolescents with MDD showing an early onset of depression;
To investigate brain structural alterations in adolescents with MDD compared to HC;
To investigate the effects of early-life stress on the brain functional and structural alterations in MDD.
In accordance with previous studies, we hypothesized an elevated limbic activity to negative stimuli, as well as structural reductions in hippocampal and the ACC in adolescents with MDD. Furthermore, we expected both functional and structural changes to be influenced by childhood maltreatment experiences, irrespective of diagnosis.
Materials and methods
Participants and Study Design
The present cross-sectional study comprised 20 adolescent patients with severe MDD (mean age=16.00 years, SD=1.03, range=15–18 years), and n=21 age (T(df=39)=−1.74, P=0.09) and sex (χ2(df=1)=1.45, P=0.23) matched healthy controls (HC, mean age=16.57 years, SD=1.08, range=15–18 years). Structural and functional data were obtained using a MRI at 3T. The patients were recruited through the inpatient service of the Department of Child and Adolescent Psychiatry, University of Muenster. HC were recruited through public notices and newspaper announcements. Diagnoses were verified employing the structured clinical interview for DSM-IV (Wittchen et al, 1997). All patients suffered from a current major depressive episode and fulfilled the criteria of MDD. Six patients were currently treated with antidepressants, two patients with antipsychotics (haloperidol equivalent=1 mg according to Andreasen et al, 2010) and 12 patients were medication-naive (see Table 1 for details). Only two patients had prior antidepressant treatment. In order to assess the severity of depressive symptoms, the hamilton rating scale of depression (HDRS; Hamilton, 1960) and the Beck Depression Inventory (BDI; Beck and Steer, 1987) were used. The Childhood Trauma Questionnaire (CTQ; Bernstein et al., 1994) was administered to assess maltreatment during childhood. Exclusion criteria for all participants were any neurological abnormalities, organic mental disorders, brain injuries or MRI contraindications. For HC, any lifetime psychiatric disorder was an exclusion criterion. For patients, lifetime substance related disorders, bipolar disorders, schizophrenia, and other psychotic disorders were exclusion criteria. The study was approved by the local IRB, and all participants provided written informed consent before participation.
Table 1. Sociodemographic and Clinical Characteristics.
|
MDD Sample (n=20) |
HC sample (n=21) |
t-tests/χ2-test | P-value | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Sociodemographic characteristics | ||||||
| Age | 16.00 | 1.03 | 16.57 | 1.08 | T(df=39)=−1.74 | 0.09 |
| Sex (m/f) | 5/15 | 9/12 | χ2(df=1)=1.45 | 0.23 | ||
| Questionnaires | ||||||
| BDI | 27.55 | 11.61 | 1.29 | 2.67 | T(df=39)=10.10 | <0.01 |
| HDRS | 19.95 | 2.84 | 0.57 | 0.98 | T(df=39)=29.45 | <0.01 |
| CTQ | 44.55 | 12.42 | 30.38 | 5.47 | T(df=39)=4.77 | <0.01 |
| Clinical characteristics | ||||||
| Number of depressive episodes | 1.80 | 0.83 | ||||
| Duration of illness (months) | 31.50 | 20.35 | ||||
| Time since first inpatient treatment (months) | 26.79 | 26.29 | ||||
| Lifetime duration of inpatient treatment (weeks) | 27.85 | 19.71 | ||||
| Duration of index episode (weeks) | 32.38 | 18.18 | ||||
| Medical Characteristics | Dose | |||||
| Fluoxetine | 3 | 20 mg/day | ||||
| Citalopram | 3 | 20 mg/day | ||||
| Quetiapine | 1 | 25 mg/day | ||||
| Risperidone | 1 | 1 mg/day | ||||
| No Medication | 12 | |||||
Abbreviations: CTQ, childhood trauma questionnaire; HC, healthy controls; BDI, Beck depression inventory; HDRS, Hamilton depression rating scale; MDD, major depressive disorder.
Paradigm
Paradigm
A frequently used face-matching fMRI paradigm (Redlich et al, 2015a, 2015b) has been used to investigate emotion processing with a few modifications. A set of happy, negative (angry, fear) and neutral faces from the NimStim battery were used (Tottenham et al, 2009). The paradigm consisted of five blocks of a sensorimotor control task alternating with four blocks of a face-processing task. During the face-processing task, participants viewed a trio of faces and selected 1 of 2 faces (bottom) that was identical to the target face (top). Each face-processing block consisted of twelve images, balanced for target gender and emotion (negative, happy, and neutral). Equally during the sensorimotor control blocks, the participants viewed a trio of geometric shapes (circles and ellipses) and selected 1 of 2 shapes (bottom) that was identical to the target shape (top). Each sensorimotor control block consisted of 12 shape trios. All blocks were preceded by an instruction (‘Match faces’ or ‘Match shapes’ in German) that lasted 2 s. In the face-processing blocks, each of the 12 face trios was presented for 2 s with a variable inter-stimulus interval of 1–5 s (mean, 3 s), for a total block length of 62 s. In the sensorimotor control blocks, each of the 12 shape trios was presented for 2 s with a fixed inter-stimulus interval of 1 s, for a total block length of 38 s. The total task time was 438 s. Participant performance (accuracy and reaction time) was recorded.
Functional MRI
Acquisition and preprocessing
Our functional and structural MRI methods and statistical approach followed standardized published protocols (Opel et al, 2015; Redlich et al, 2015a, 2015b, 2017). Briefly, T2* functional data were acquired with a 3-Tesla scanner (Gyroscan Intera 3T, Philips Medical Systems, Best, NL) using a single-shot echoplanar sequence, with parameters selected to minimize distortion in the region of central interest, while retaining an adequate signal-to-noise ratio (S/N) and T2* sensitivity. Volumes consisting of 34 slices were acquired (matrix 64 × 64, resolution 3.6 × 3.6 × 3.6 mm; TR=2.1 s, TE=30 ms, FA=90°). The slices were tilted by 25° from the AC/PC line in order to minimize drop-out artifacts in the mediotemporal and orbitofrontal regions. The data were analyzed using statistical parametric mapping software (SPM8, Welcome Department of Cognitive Neurology, London, UK; http://www.fil.ion.ucl.ac.uk/spm). Preprocessing of functional data included realignment, unwarping, and spatial normalization of each participant’s functional images to the Montreal Neurological Institute International Consortium (MNI) for Brain Mapping template. For brain functional analysis, three adolescents with MDD and one HC had to be excluded due to excessive head movement (exclusion criterion 3 mm/3°). Images were smoothed with a Gaussian kernel of 6 mm full width at half-maximum (FWHM).
First-level analyses
The onsets and durations of the experimental conditions (positive, negative, and neutral) were modeled by using a canonical hemodynamic response function in the context of a GLM, and the model was corrected for serial correlations. A high-pass filter of 128 s was used to remove low-frequency noise. For each subject, two contrast images were generated in each individual first-level analysis (negative>neutral, positive>neutral) in order to investigate our research objective.
Statistical analyses functional data
In order to investigate our research objectives, we conducted a 2 (group=MDD vs HC) × 2 (condition=positive>neutral vs negative>neutral) ANOVA using a full-factorial model, with group as the between-subjects factor and emotion valence as the within-subjects factor. Age and sex were included as confounding covariates. To explore the nature of the interaction, post hoc analyses were conducted. First, we conducted a whole-brain. To address our hypotheses on differential amygdala responsiveness, region of interest (ROI) analyses were additionally performed on the bilateral amygdala. A mask for the bilateral amygdala was created with the aid of the Wake Forest University PickAtlas (Maldjian et al, 2003) according to the AAL-atlas definitions (Tzourio-Mazoyer et al, 2002). Significance thresholds for multiple testing were obtained at the cluster-level by threshold-free cluster enhancement as a non-parametric approach, which is implemented in the TFCE-toolbox (http://dbm.neuro.uni-jena.de/tfce/tfce_r121.zip). We consequently established a conservative FWE-corrected threshold of P<.05 obtained by 5000 permutations per test.
In order to analyze the potential associations between brain function, sociodemographic, and clinical data, respectively, the mean cluster values of potential interaction were extracted and associated with covariates using either Spearman’s rho correlations (age, duration of illness, duration of index episode) or t-test for independent samples (sex, medication yes/no).
Structural MRI
Data acquisition and preprocessing
T1-weighted high resolution anatomical images were acquired (Gyroscan Intera 3T, Philips Medical Systems, Best, NL) with a 3D fast gradient echo sequence (‘Turbo Field Echo’, TFE), TR=7.4 ms, TE=3.4 ms, FA=9°, two signal averages, inversion prepulse every 814.5 ms, acquired over a field of view of 256(FH) × 204(AP) × 160(RL) mm, phase encoding in AP and RL direction, reconstructed to cubic voxels of 0.5 × 0.5 × 0.5 mm. The VBM8-toolbox (http://dbm.neuro.uni-jena.de/vbm) was used for preprocessing the structural images with default parameters as described before (Opel et al, 2016; Redlich et al, 2016; Stacey et al, 2016). Briefly, images were bias-corrected, tissue classified, and normalized to MNI-space using linear (12-parameter affine) and nonlinear transformations, within a unified model including high-dimensional DARTEL-normalization and smoothed with a Gaussian kernel of 8 mm full width half maximum (FWHM).
Statistical analyses structural data
In order to investigate potential structural differences, a t-test was conducted for independent samples (HC vs MDD) with age and sex as confounding covariates. First, a whole-brain analysis including full brain volumes was conducted. Second, in order to test our hypotheses, the restricted ROI analyses of the bilateral hippocampus and Anterior Cingulate Gyrus (ACC) were performed according to the AAL-atlas definitions (Tzourio-Mazoyer et al, 2002, for a visual guide of conducted ROI's please see Supplementary Figure 1). Again, a rigorous FWE-corrected threshold of P<0.05 was applied using the TFCE toolbox, as described above.
Finally, the potential associations between brain structure and covariates—the mean cluster values were extracted and associated with covariates using either Spearman’s rho correlations (age, duration of illness, duration of index episode) or t-test for independent samples (sex, medication yes/no).
Associations between Brain Structure, Brain Function, and Childhood Maltreatment
In order to determine the influence of childhood maltreatment on gray-matter volume, the mean gray-matter values of the resulting cluster of the hippocampus were extracted and then separately correlated with CTQ scores for adolescents with both MDD and HC. Additionally, correlation analysis was conducted for the combined sample. To investigate the association between functional amygdala reactivity and childhood maltreatment, the mean contrast values of the resulting cluster of the amygdala of the 2 × 2 ANOVA were extracted. The individual contrast values were again correlated with the CTQ scores for the two samples separately and jointly. All correlation analyses were performed using Spearman's rho due to non-normality distributions (HC=Kolmogorov–Smirnov (df=21)=0.193, P=0.40, Shapiro-Wilk(df=21)=0.808, P<0.01; MDD=Kolmogorov–Smirnov (df=20)=0.146, P=0.20; Shapiro-Wilk(df=20)=0.887, P=0.02).
Results
Behavioral Performance in the fMRI Experiment
The mean accuracy rates in the shape condition were 96.8% for adolescent patients (SD=3.7%) and 96.8% for HC (SD=2.5%). The mean accuracy rates for the face condition were 94.9% for adolescent patients (SD=4.3%) and 96.0% for HC (SD=4.9%). The analysis of accuracy rates using a 2 (group=MDD, HC) × 2 (condition=faces, shapes) ANOVA with repeated measures yielded neither a significant interaction (F(1;39)=3.69; P=0.06) nor a main effect (group F(1;35)=1.52; P=0.42; condition F(1;35)=3.35; P=0.75). The analysis of reaction times using a 2 (group=MDD, HC × 2 (condition=faces, shapes) ANOVA with repeated measures yielded a significant main effect of condition (F(1;35)=185.19; P<0.01). Post hoc analyses revealed significantly shorter reaction times to shapes compared to faces (T(36)=13.67; P<0.01; HC=T(19)=9.15, P<0.01; MDD=T(16)=9.31, P>0.01). Again, neither a main effect of group (F(1;39)=1.39; P=0.25) nor an interaction effect between group and condition (F(1;39)=0.77; P=0.39) was found.
Emotion Processing—Functional MRI
The analysis of whole-brain data yielded no significant cluster. The ROI analysis of the 2 × 2 full-factorial model yielded a significant main effect of condition (x=−28, y=0, z=−14, F(1, 68)=13.51, TFCE=74.75, k=29, PFWE=0.019) resulting from an overall increased amygdala reactivity to negative stimuli, compared to positive stimuli, driven by the MDD sample (x=−22, y=−8, z=−14, T(14)=4.79, TFCE=145.61, k=61, PFWE=0.005). There was no significant main effect of group.
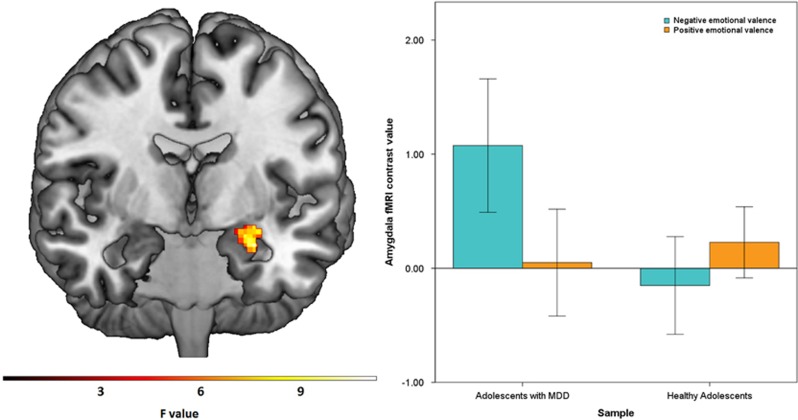
Furthermore, the analysis revealed an interaction effect of the group (MDD vs HC) by condition (positive vs negative) within the amygdala (x=−28, y=−4, z=−20, F(1, 68)=11.24, TFCE=709.89, k=5, PFWE=0.027), resulting from an increased amygdala activity in reaction to negative faces (x=30, y=−2, z=−14, T(34)=3.48, TFCE=65.62, k=12, PFWE=0.012) and a decreased amygdala activity to positive faces (x=−20, y=−6, z=−12, T(34)=3.53, TFCE=48.13, k=34, PFWE=0.001) in adolescents with MDD, compared to HC (see Figure 1).
Figure 1.
Coronal view (Montreal-Neurological-Institute coordinate y=−3) depicts the interaction effect of group (MDD versus HC) by condition (positive vs negative) within the amygdala (F(1, 68)=11.24, TFCE=709.89, k=5, PFWE=0.027), resulting from an increased amygdala activity in reaction to negative faces (T(34)=3.48, TFCE=65.62, k=12, PFWE=0.012) and a decreased amygdala activity to positive faces (T(34)=3.53, TFCE=48.13, k=34, PFWE=0.001) in adolescents with MDD compared to HC. For display reasons, the statistical threshold was set to P<0.05, uncorrected. Right: bar graphs depicting the estimated contrast values of the amygdala subdivided by group (MDD, HC) for the negative emotional valence (blue) and the positive emotion valence (orange) condition. Error bars (±2 SE). MDD, major depressive disorder; HC, healthy controls. A full color version of this figure is available at the Neuropsychopharmacology journal online.
The analysis of covariates showed no significant associations between amygdala reactivity and age (rspearman=−.16, P=0.34), sex (T(df=35)=−1.5, P=0.63), duration of illness (rspearman=−.13, P=0.62) or duration of index episode (rspearman=−.19, P=0.47). Furthermore, there was no significant differences between amygdala reactivity and medication on group level (T(df=15)= −4.8, P=0.64).
Voxel Based Morphometry—Structural MRI
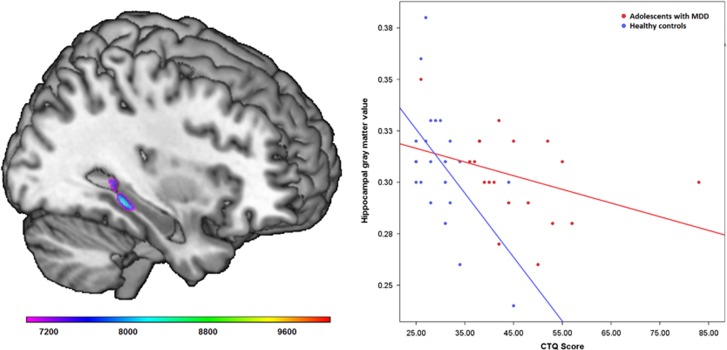
The analysis of structural data yielded no significant differences on whole-brain level. The hippocampal ROI analysis yielded significant gray-matter volume reductions in the bilateral hippocampal formation in adolescents with MDD compared to HC (left: x=−26, y=−36, z=6, T(37)=4.29, TFCE=11 817.37, k=25, PFWE=0.022; right: x=33, y=−33, z=−9, T(37)=4.68, TFCE=8992.14, k=54, PFWE=0.040). No significant differences were found for the ACC. The analysis of covariates showed no significant associations between hippocampal volume and age (rspearman=0.21, P=0.20), sex (T(df=39)=−4.9, P=0.63), duration of illness (rspearman=−.11, P=0.64), duration of index episode (rspearman=0.03, P=0.90) or medication (T(df=18)=0.39, P=0.70).
Associations between Brain Structure, Brain Function, and Childhood Maltreatment
The correlation analysis of structural data for the combined sample yielded a negative association between hippocampal volume and CTQ scores (rspearman=−.43, P=0.005). Further analysis revealed that this association is present in both HC (rspearman=−.45, P=0.039) and in adolescents with MDD (rspearman=−.46, P=0.042), indicating that this association is independent of diagnosis (see Figure 2).
Figure 2.
Associations between brain structure, diagnosis, and childhood maltreatment. Left: coronal view (Montreal-Neurological-Institute coordinate at x=33) depicting significant gray-matter volume reductions in the bilateral hippocampal formation in adolescents with major depressive disorder compared to healthy controls (color bar: TFCE score, PFWE=0.05, k=53 voxel). Right: scatter plot depicting the association between gray-matter volume and Childhood-Trauma-Questionnaire scores for MDD patients (red) and healthy controls (blue). A full color version of this figure is available at the Neuropsychopharmacology journal online.
In order to further investigate the association between CTQ, hippocampal volume, and diagnosis, we followed two strategies: First, a logistic regression model was used with CTQ scores and hippocampal volume as independent regressors and diagnosis as binary dependent output variable. The model explained 47.1% of the variance of MDD diagnosis, revealing a strong association between CTQ scores and diagnosis of MDD (β(df=1)=−309, P=0.001) and CTQ scores and hippocampal volume (β(df=1)=−312, P=0.013). However, the association between diagnosis of MDD and hippocampal volume disappeared controlling for CTQ. Second, in order to further prove the competing effects of group and childhood maltreatment, a second SPM model was performed, identical to Paragraph 3.3, but now additionally controlling for CTQ scores. We hypothesized that group differences between MDD and healthy controls are strongly diminished or even disappear if childhood maltreatment is included as a covariate. Indeed, when accounting for CTQ scores as additional covariates in the ANCOVA from Paragraph 3.3, no significant group differences between MDD and HC could be observed any longer. Taken together, this indicates that hippocampal volume does not seem to act as mediator between childhood maltreatment and MDD and provides support for the interpretation that hippocampal volume is mainly explained by CTQ scores instead of MDD diagnosis.
The analysis of the functional data and childhood maltreatment data revealed no significant associations between CTQ scores and amygdala reactivity to negative or positive faces, neither for the combined nor for both samples separately (Ps>.1).
Discussion
In sum, the present study provides three major findings. First, adolescents with MDD show an elevated degree of amygdala activity in reaction to negative stimuli. This is in line with results of previous studies (Yang et al, 2010; Mingtian et al, 2012; Tao et al, 2012; Gaffrey et al, 2013; Hall et al, 2014). Second, depressed adolescents show a smaller hippocampal volume compared to healthy adolescents. Third, high levels of childhood maltreatment are associated with smaller hippocampal volumes in both depressed patient and healthy controls. In contrast, there were no significant associations between CTQ scores and functional amygdala activity to either positive or negative emotional stimuli.
In line with previous studies in adults (Victor et al, 2010; Stuhrmann et al, 2013), we found an increased amygdala activity in reaction to emotional negative stimuli and a decreased amygdala activity to positive stimuli in adolescents with MDD compared to HC. This might reflect an cognitive processing bias in subjects with depression according to cognitive theories of depression, suggesting potentiation of negative affective information and attenuation of positive information (Beck, 2008; Stuhrmann et al, 2013). This is further in line with the conclusion that amygdala hyperactivity in response to negative faces in studies with adolescent MDD patients are consistent with those with adults (Tao et al, 2012; Kerestes et al, 2014). In contrast to the results of previous studies on healthy adults (Dannlowski et al, 2013) and adolescents (Teicher and Samson, 2016), we did not find an association between childhood maltreatment and amygdala reactivity to emotional stimuli for either MDD patients or HC. This finding might indicate that amygdala reactivity rather represent a state effect of depression instead of a trait effect of early maltreatment which finds further support by studies showing a normalization after antidepressant treatment (Fu et al, 2004; Arnone et al, 2012b; Williams et al, 2015). The analyses of brain structural data were in line with similar findings in adult patients. Compared to healthy subjects, a smaller hippocampal GM volume already seems to be present in adolescents with MDD representing an early onset of depression. However, we did not find any differences in ACC volumes—as previous reported in meta-analyses (Arnone et al., 2012a)—when comparing patients with MDD and HC. A possible explanation of this finding might be that most patients in our sample showed a first episode, as previous meta-analyses reported gray-matter reduction in ACC, mostly observed in samples that included multi-episode patients. This suggests a possible progression of abnormalities in these regions over time which received additional support from longitudinal work (Frodl et al, 2008a; Bora et al, 2012).
Our regression analysis further revealed that this hippocampal gray-matter volume loss seems to be at least partly a result of early-life stress rather than MDD diagnosis itself, which is in line with the findings of previous studies in adults (Vythilingam et al, 2002; Teicher et al, 2012; Opel et al, 2014) and youth (Rao et al, 2010). This suggests that a small hippocampus volume seems to represent a trait marker—apparent before the onset of disease—rather than a state marker of depression. Further evidence for this assumption is given by genetic studies showing that several putative genetic risk variants have been associated with hippocampal structure (Baune et al, 2012; Dannlowski et al, 2015). However, this conclusion does not necessarily exclude the possibility that further depressive episodes and adult life stress extend this primary hippocampal volume reduction. In particular, a chronic course of depression seems to influence the hippocampal structure negatively with time (Bell-McGinty et al, 2002; Videbech and Ravnkilde, 2004; Frodl et al, 2008b), most probably due to neurotoxic effects of prolonged and repeated cortisol release in depressed patients (Sapolsky, 2000; Dohm et al, 2017). Nevertheless, a smaller hippocampal volume seems to be already present before onset of depression, and therefore needs special consideration. Clinically, this implies that children and young people who have experienced childhood maltreatment and show corresponding neurobiological markers might benefit from special attention in order to avert a potential onset of a depression. A prevention strategy should preferably aim to reduce a further loss of hippocampal volume through additional stressors to avoid further increase in the vulnerability to depression. One approach to accomplish this goal might be psychotherapy, pharmacotherapy and other treatments—even before onset of depression—to reduce the limbic sensitivity and normalize the hippocampus volume, as recently shown by several studies in adults (Harmer et al, 2006; Redlich et al, 2016; Arnone et al, 2013). Another approach could aim to reduce glucocorticoid levels using anti-glucocorticoid agents and antagonists, as already tested in patients with depression. This therapy is still at a proof-of-concept stage (Gallagher et al, 2008). First results are promising and might offer options to prevent a further hippocampal volume loss, given the presumption that high levels of corticosteroids are neurotoxic. However, future investigations are needed to prove the clinical utility of these drugs in the treatment of mood disorders. The benefit of such a treatment must be confirmed with great certainty to justify a treatment that abides by ethical requirements.
The major strength of the study is the investigation of the relations between brain structure, brain function, depression, and maltreatment using two MRI methods (VBM and functional MRI) in a homogenous sample. Despite the evident results, some limitations of this study must be acknowledged. First, the rather modest sample size was sufficient to detect differences between the patient samples and controls, but might have been a reason why we were not able to detect linear associations between maltreatment and brain function. Furthermore, traumatic experiences in childhood were assessed by means of a self-reporting measure retrospectively. Severe depressed subjects may have had a negative recall bias. While we do not assume this to be a major problem, future prospective studies could definitely rule out this possibility. Although very challenging, future studies should aim to specifically recruit healthy controls with higher levels of adversity (eg matched to the MDD sample). Finally, due to the cross-sectional design of the study, we can only draw limited conclusions about causal associations between childhood maltreatment, brain structure, and function. Again, there is an urgent need for longitudinal studies to investigate this relationship, preferably starting in early childhood.
Conclusions
In sum, these findings give further evidence that smaller hippocampal volumes in depression seem to represent a consequence of early childhood maltreatment, potentially increases the risk of developing a depressive disorder. This underlines the importance of prevention of a potential onset of depression, particularly in children and young people who have experienced childhood maltreatment or neglect. In future, apart from family and childhood maltreatment anamnesis, additional information about the hippocampal morphometry might enable us to identify high-risk subjects and to develop preventive measures for those high-risk subjects even before the onset of depression.
Funding and disclosure
The study was supported by grants of the Innovative Medizinische Forschung (PO211206 to CP, RE111604 to RR and RE111722 to RR), and the German Research Foundation (DFG; grant FOR 2107; DA1151/5-1 to UD). VA is a member of the advisory board of, or has given presentations on behalf of, the following companies: Astra-Zeneca, Janssen-Organon, Lilly, Lundbeck, Servier, Pfizer, Otsuka, and Trommsdorff. HK has received consultation fees from MR:comp GmbH, Testing Services for MR Safety. These affiliations are of no relevance to the work. The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on the Neuropsychopharmacology website (http://www.nature.com/npp)
Supplementary Material
References
- Abler B, Erk S, Herwig U, Walter H (2007). Anticipation of aversive stimuli activates extended amygdala in unipolar depression. J Psychiatr Res 41: 511–522. [DOI] [PubMed] [Google Scholar]
- Andreasen NC, Pressler M, Nopoulos P, Miller D, Ho B-C (2010). Antipsychotic dose equivalents and dose-years: a standardized method for comparing exposure to different drugs. Biol Psychiatry 67: 255–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnone D, McIntosh AM, Ebmeier KP, Munafò MR, Anderson IM (2012. a). Magnetic resonance imaging studies in unipolar depression: systematic review and meta-regression analyses. Eur Neuropsychopharmacol 22: 1–16. [DOI] [PubMed] [Google Scholar]
- Arnone D, McKie S, Elliott R, Juhasz G, Thomas EJ, Downey D et al (2013). State-dependent changes in hippocampal grey matter in depression. Mol Psychiatry 18: 1265–1272. [DOI] [PubMed] [Google Scholar]
- Arnone D, McKie S, Elliott R, Thomas EJ, Downey D, Juhasz G et al (2012. b). Increased amygdala responses to sad but not fearful faces in major depression: relation to mood state and pharmacological treatment. Am J Psychiatry 169: 841–850. [DOI] [PubMed] [Google Scholar]
- Baune BT, Konrad C, Grotegerd D, Suslow T, Ohrmann P, Bauer J et al (2012). Tumor necrosis factor gene variation predicts hippocampus volume in healthy individuals. Biol Psychiatry 72: 655–662. [DOI] [PubMed] [Google Scholar]
- Beck AT (2008). The evolution of the cognitive model of depression and its neurobiological correlates. Am J Psychiatry 165: 969–977. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA (1987) Beck Depression Inventory: manual. The Psychological Corporation, Harcourt Brace Jovanovich: San Antonio. [Google Scholar]
- Bell-McGinty S, Butters MA, Meltzer CC, Greer PJ, Reynolds CF, Becker JT (2002). Brain morphometric abnormalities in geriatric depression: long-term neurobiological effects of illness duration. Am J Psychiatry 159: 1424–1427. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L, Handelsman L, Foote J, Lovejoy M, Wenzel K et al (1994). Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry 151: 1132–1136. [DOI] [PubMed] [Google Scholar]
- Bora E, Fornito A, Pantelis C, Yücel M (2012). Gray matter abnormalities in major depressive disorder: a meta-analysis of voxel based morphometry studies. J Affect Disord 138: 9–18. [DOI] [PubMed] [Google Scholar]
- Dannlowski U, Grabe HJ, Wittfeld K, Klaus J, Konrad C, Grotegerd D et al (2015). Multimodal imaging of a tescalcin (TESC)-regulating polymorphism (rs7294919)-specific effects on hippocampal gray matter structure. Mol Psychiatry 20: 398–404. [DOI] [PubMed] [Google Scholar]
- Dannlowski U, Kugel H, Huber F, Stuhrmann A, Redlich R, Grotegerd D et al (2013). Childhood maltreatment is associated with an automatic negative emotion processing bias in the amygdala. Hum Brain Mapp 34: 2899–2909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dannlowski U, Stuhrmann A, Beutelmann V, Zwanzger P, Lenzen T, Grotegerd D et al (2012). Limbic scars: long-term consequences of childhood maltreatment revealed by functional and structural magnetic resonance imaging. Biol Psychiatry 71: 286–293. [DOI] [PubMed] [Google Scholar]
- Dohm K, Redlich R, Zwitserlood P, Dannlowski U (2017). Trajectories of major depression disorders: A systematic review of longitudinal neuroimaging findings. Aust N Z J Psychiatry 51: 441–454 in press. [DOI] [PubMed] [Google Scholar]
- Du MY, Wu QZ, Yue Q, Li J, Liao Y, Kuang WH et al (2012). Voxelwise meta-analysis of gray matter reduction in major depressive disorder. Prog Neuropsychopharmacol Biol Psychiatry 36: 11–16. [DOI] [PubMed] [Google Scholar]
- Epstein J, Pan H, Kocsis JH, Yang Y, Butler T, Chusid J et al (2006). Lack of ventral striatal response to positive stimuli in depressed versus normal subjects. Am J Psychiatry 163: 1784–1790. [DOI] [PubMed] [Google Scholar]
- Frodl T, Koutsouleris N, Bottlender R, Born C, Jäger M, Scupin I et al (2008. a). Depression-related variation in brain morphology over 3 years: effects of stress? Arch Gen Psychiatry 65: 1156–1165. [DOI] [PubMed] [Google Scholar]
- Frodl T, Koutsouleris N, Bottlender R, Born C, Jäger M, Scupin I et al (2008. b). Depression-related variation in brain morphology over 3 years: effects of stress? Arch Gen psychiatryeneral Psychiatry 65: 1156–1165. [DOI] [PubMed] [Google Scholar]
- Fu CHY, Williams SCR, Cleare AJ, Brammer MJ, Walsh ND, Kim J et al (2004). Attenuation of the neural response to sad faces in major depression by antidepressant treatment: a prospective, event-related functional magnetic resonance imaging study. Arch Gen Psychiatry 61: 877–889. [DOI] [PubMed] [Google Scholar]
- Gaffrey MS, Barch DM, Singer J, Shenoy R, Luby JL (2013). Disrupted amygdala reactivity in depressed 4- to 6-year-old children. J Am Acad Child Adolesc Psychiatry 52: 737–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher P, Malik N, Newham J, Young AH, Ferrier IN, Mackin P (2008). Antiglucocorticoid treatments for mood disorders. Cochrane Database Syst Rev 1CD005168. [DOI] [PubMed] [Google Scholar]
- Hall LMJ, Klimes-Dougan B, Hunt RH, Thomas KM, Houri A, Noack E et al (2014). An fMRI study of emotional face processing in adolescent major depression. J Affect Disord 168: 44–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamilton M (1960). A rating scale for depression. J Neurol Neurosurg 23: 56–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harmer CJ, Mackay CE, Reid CB, Cowen PJ, Goodwin GM (2006). Antidepressant drug treatment modifies the neural processing of nonconscious threat cues. Biol Psychiatry 59: 816–820. [DOI] [PubMed] [Google Scholar]
- Kerestes R, Davey CG, Stephanou K, Whittle S, Harrison BJ (2014). Functional brain imaging studies of youth depression: a systematic review. NeuroImage Clin 4: 209–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Walters EE (1998). Epidemiology of DSM-III-R major depression and minor depression among adolescents and young adults in the National Comorbidity Survey. Depress Anxiety 7: 3–14. [DOI] [PubMed] [Google Scholar]
- Maldjian JA, Laurienti PJ, Kraft RA, Burdette JH (2003). An automated method for neuroanatomic and cytoarchitectonic atlas-based interrogation of fMRI data sets. Neuroimage 19: 1233–1239. [DOI] [PubMed] [Google Scholar]
- Mingtian Z, Shuqiao Y, Xiongzhao Z, Jinyao Y, Xueling Z, Xiang W et al (2012). Elevated amygdala activity to negative faces in young adults with early onset major depressive disorder. Psychiatry Res 201: 107–112. [DOI] [PubMed] [Google Scholar]
- Opel N, Redlich R, Grotegerd D, Dohm K, Haupenthal C, Heindel W et al (2015). Enhanced neural responsiveness to reward associated with obesity in the absence of food-related stimuli. Hum Brain Mapp 36: 2330–2337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opel N, Redlich R, Zwanzger P, Grotegerd D, Arolt V, Heindel W et al (2014). Hippocampal Atrophy in Major Depression: a Function of Childhood Maltreatment Rather than Diagnosis? Neuropsychopharmacology 39: 2723–2731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opel N, Zwanzger P, Redlich R, Grotegerd D, Dohm K, Arolt V et al (2016). Differing brain structural correlates of familial and environmental risk for major depressive disorder revealed by a combined VBM/pattern recognition approach. Psychol Med 46: 277–290. [DOI] [PubMed] [Google Scholar]
- Peluso MAM, Glahn DC, Matsuo K, Monkul ES, Najt P, Zamarripa F et al (2009). Amygdala hyperactivation in untreated depressed individuals. Psychiatry Res 173: 158–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao U, Chen L-A, Bidesi AS, Shad MU, Thomas MA, Hammen CL (2010). Hippocampal changes associated with early-life adversity and vulnerability to depression. Biol Psychiatry 67: 357–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redlich R, Bürger C, Dohm K, Grotegerd D, Opel N, Zaremba D et al (2017). Effects of electroconvulsive therapy on amygdala function in major depression—a longitudinal fMRI study. Psychol Med 47: 2166–2176. [DOI] [PubMed] [Google Scholar]
- Redlich R, Grotegerd D, Opel N, Kaufmann C, Zwitserlood P, Kugel H et al (2015. a). Are you gonna leave me? Separation Anxiety is associated with increased amygdala responsiveness and volume. Soc Cogn Affect Neurosci 10: 278–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redlich R, Opel N, Grotegerd D, Dohm K, Zaremba D, Bürger C et al (2016). Prediction of individual response to electroconvulsive therapy via machine learning on structural magnetic resonance imaging data. JAMA Psychiatry 73: 557–564. [DOI] [PubMed] [Google Scholar]
- Redlich R, Stacey D, Opel N, Grotegerd D, Dohm K, Kugel H et al (2015. b). Evidence of an IFN-gamma by early life stress interaction in the regulation of amygdala reactivity to emotional stimuli. Psychoneuroendocrinology 62: 166–173. [DOI] [PubMed] [Google Scholar]
- Rosso IM, Cintron CM, Steingard RJ, Renshaw PF, Young AD, Yurgelun-Todd DA (2005). Amygdala and hippocampus volumes in pediatric major depression. Biol Psychiatry 57: 21–26. [DOI] [PubMed] [Google Scholar]
- Sapolsky RM (2000). The possibility of neurotoxicity in the hippocampus in major depression: a primer on neuron death. Biol Psychiatry 48: 755–765. [DOI] [PubMed] [Google Scholar]
- Stacey D, Redlich R, Buschel A, Opel N, Grotegerd D, Zaremba D et al (2016). TNF receptors (TNFR) 1 and 2 exert distinct region-specific effects on striatal and hippocampal grey matter volumes (VBM) in healthy adults - Revision. Genes Brain Behav 16: 352–360 in press. [DOI] [PubMed] [Google Scholar]
- Stirling J, Amaya-Jackson L (2008). Understanding the behavioral and emotional consequences of child abuse. Pediatrics 122: 667–673. [DOI] [PubMed] [Google Scholar]
- Stuhrmann A, Dohm K, Kugel H, Zwanzger P, Redlich R, Grotegerd D et al (2013). Mood-congruent amygdala responses to subliminally presented facial expressions in major depression: associations with anhedonia. J Psychiatry Neurosci 37: 249–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuhrmann A, Suslow T, Dannlowski U (2011). Facial emotion processing in major depression: a systematic review of neuroimaging findings. Biol Mood Anxiety Disord 1: 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tao R, Calley CS, Hart J, Mayes TL, Nakonezny PA, Lu H et al (2012). Brain activity in adolescent major depressive disorder before and after fluoxetine treatment. Am J Psychiatry 169: 381–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teicher MH, Anderson CM, Polcari A (2012). Childhood maltreatment is associated with reduced volume in the hippocampal subfields CA3, dentate gyrus, and subiculum. Proc Natl Acad Sci U S A 109: E563–E572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teicher MH, Samson JA (2016). Annual research review: enduring neurobiological effects of childhood abuse and neglect. J Child Psychol Psychiatry 57: 241–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tottenham N, Tanaka JW, Leon AC, McCarry TW, Nurse M, Hare TA et al (2009). The NimStim set of facial expressions: judgments from untrained research participants. Psychiatry Res 168: 242–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tzourio-Mazoyer N, Landeau B, Papathanassiou D, Crivello F, Etard O, Delcroix N et al (2002). Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. Neuroimage 15: 273–289. [DOI] [PubMed] [Google Scholar]
- Victor TA, Furey ML, Fromm SJ, Ohman A, Drevets WC (2010). Relationship between amygdala responses to masked faces and mood state and treatment in major depressive disorder. Arch Gen Psychiatry 67: 1128–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Videbech P, Ravnkilde B (2004). Hippocampal volume and depression: a Meta-Analysis of MRI Studies. Am J Psychiatry 161: 1957–1966. [DOI] [PubMed] [Google Scholar]
- Vythilingam M, Heim C, Newport J, Miller AH, Anderson E, Bronen R et al (2002). Childhood trauma associated with smaller hippocampal volume in women with major depression. Am J Psychiatry 159: 2072–2080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams LM, Korgaonkar MS, Song YC, Paton R, Eagles S, Goldstein-Piekarski A et al (2015). Amygdala reactivity to emotional faces in the prediction of general and medication-specific responses to antidepressant treatment in the randomized iSPOT-D trial. Neuropsychopharmacology 40: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wittchen H-U, Wunderlich U, Gruschwitz S, Zaudig M (1997) Strukturiertes Klinisches Interview für DSM-IV. Hogrefe: Goettingen. [Google Scholar]
- World Health Organization (2001) Mental health: new understanding, new hope. World Health Organization: Geneva, Switzerland. [Google Scholar]
- Yang TT, Simmons AN, Matthews SC, Tapert SF, Frank GKW, Max JE et al (2010). Adolescents with major depression demonstrate increased amygdala activation. J Am Acad Child Adolesc Psychiatry 49: 42–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.