Abstract
BACKGROUND:
As the rapid growth of the elderly population and the increased prevalence of Alezheimer’s Disease and related disorders, there is an increasing need for effective cognitive screening. The Mini Mental State Examination (MMSE) is the most frequently used screening test of cognitive impairment because of its convenience. The Montreal Cognitive Assessment-Indonesian Version (MoCA-INA) has been validated and recently been used as a cognitive screening tool.
OBJECTIVES:
The aim of this study was to compare the MMSE and MoCA-INA scores and to determine the correlation between the MMSE and MoCA-INA scores in elderly.
MATERIAL AND METHODS:
This was a cross-sectional study including 83 elderly subjects from November 2016 until June 2017. We performed MMSE and MoCA-INA for assessment of cognitive function and the time between each test was at least 30 minutes.
RESULTS:
The study included 83 subjects which were consisted of 46 (55.4%) males and 37 (44.6%) females. The mean age was 69.19 ± 4.23 ranging from 65 to 79 years old. The average MMSE scores was 24.96 ± 3.38 (range 14 to 30). The average MoCA-INA scores was 21.06 ± 4.56 (range 5 to 30). The Pearson correlation coefficient between the scores was 0.71 (p<0.005). There were no significant differences of both scores based on history of hypertension, diabetes mellitus and previous stroke, but there was a significant difference in MMSE scores based on level of education.
CONCLUSION:
The MoCA-INA score showed a good correlation with the MMSE score. Both tests showed comparable results but MoCA-INA showed lower average with wider range of scores.
Keywords: MMSE, MoCA-INA, Cognitive screening, Elderly
Introduction
As our population grows older, the issue of screening for dementia and cognitive impairment will become increasingly important because of the increase incidence of Alzheimer’s disease (AD) and related disorders. Improvements in survival rates following stroke will also increase the incidence of vascular and post-stroke cognitive impairment, as approximately 30% of stroke survivors will develop a progressive dementia [1].
Alzheimer’s disease (AD) is a chronic, debilitating condition causing significant disease burden and mortality in elderly. The health and economic impact of AD has led to a pressing need to prevent or slow disease onset and progression, and recent research efforts have focused on the transitional period from normal cognitive aging to dementia. This transition period, namely mild cognitive impairment (MCI), is signified by a measurable deterioration in cognitive function that is greater than expected based on an individual’s age and education but which has not meaningfully affected a person’s daily functioning [2, 3].
Mild cognitive impairment is common in elderly patients and can impact on prognosis and quality of life. The areas of cognitive impairment that occur at this stage primarily involve attention, verbal fluency, executive function and visuo-spatial skills, which differs from the language and memory skills that are commonly associated with dementia [5].
Cognitive screening tools in the elderly are important for the purpose of identifying the presence of cognitive impairment. Neuropsychological testing is the gold-standard for assessing dementia and cognitive impairment, but it is time-consuming and requires highly trained assessors. The Mini Mental State Examination (MMSE) is the most frequently used screening test of cognitive impairmens of AD [5], mainly because of its convenience but not sensitive, as it is influenced by age, socio-economic status and level of education. It assesses primarily language and memory skills and has been found to be insensitive to detecting mild cognitive impairment [4]. Cognitive performance as measured by the MMSE varies within the normal population by age and education [6]. The Montreal Cognitive Assessment (MoCA), has been developed as a brief cognitive screening tool to detect mild-moderate cognitive impairment. It has been found to have high sensitivity and specificity for the detection of mild cognitive impairment [4, 7]. The MoCA assess several cognitive domains including executive fuction, visuospatial function, attention and concentration, memory, languange, calculation and orientation [7]. The Indonesian version of MoCA, namely MoCA-INA has been developed and validated in Indonesia and so it can be used as a cognitive screening tool [8]. The aim of this study was to compare the MMSE and MoCA-INA scores and to determine the correlation between the MMSE and MoCA-INA scores in elderly subjects.
Method
This was a cross sectional study involving 83 subjects which were recruited from the Memory Clinic Neurology Department Adam Malik General Hospital Medan North Sumatera Indonesia, between November 2016 and June 2017. Inclusion criteria were age more than 65 years-old, compos mentis and fully cooperative, speak Bahasa Indonesia fluently, able to read and write, and gave written consent to be included in the study. Subjects who were medically unstable (delirium) or other psychiatric disorders, had an aphasia were excluded from the study. All subjects underwent physical and neurologic examination and cognitive assessment including Mini Mental State Examination (MMSE) and Montreal Cognitive Assessment-Indonesian Version (MoCA-INA). The time between each test was at least 30 minutes. Demographic information was collected including age, sex, occupation, level of education, history of stroke, hypertension and diabetes mellitus. The MMSE and MoCA-INA Scores were obtained. All statistical procedures were performed with SPSS. The correlation between MMSE and MoCA-INA Scores was measured using the Pearson correlation. Both scores were also compared based on level of education. The study was performed with approval obtained from the Health Research Ethical Committee Medical Faculty of Universitas Sumatera Utara/H. Adam Malik General Hospital.
Results
A total of 83 subjects were studied. The average age of subjects was 69.19 years old, ranging from 65 to 79 years old. There were 46 (55.4%) males and 37 (44.6%) females. Most of the subjects had level of education of high school (43 subjects, 51.8%). There were 26 subjects (31.3 %) with history of hypertension, 17 (20.5%) with Diabetes Mellitus and 11 subjects (13.3%) with history of previous stroke. The demographic characteristics are shown in Table 1.
Table 1.
Demographic characteristics
| Characteristic | Number (%) (n = 83) |
|---|---|
| Sex | |
| Male | 46 (55.4) |
| Female | 37 (44.6) |
| Age, mean ± SD, years | 69.19 ± 4.23 |
| Age group, years | |
| 65-69 | 53 (63.9) |
| 70-74 | 18 (21.7) |
| 75-79 | 12 (14.5) |
| Occupation | |
| Employee | 16 (19.3) |
| Housewive | 20 (24.1) |
| Entrepreneur | 13 (15.7) |
| Farmer | 4 (4.8) |
| Unemployed | 30 (36.1) |
| Level of education | |
| Elementary School | 15 (11.3) |
| Junior High school | 19 (14.3) |
| High School | 63 (47.4) |
| College/University | 36 (27.1) |
| History of Diabetes Mellitus | |
| Yes | 17 (20.5) |
| No | 66 (79.5) |
| History of Hypertension | |
| Yes | 26 (31.3) |
| No | 57 (68.7) |
| History of Previous Stroke | |
| Yes | 11 (13.3) |
| No | 72 (86.7) |
| MMSE | |
| < 24 | 31 (37.3) |
| ≥ 24 | 52 (62.7) |
| Moca-INA Score | |
| < 26 | 71 (85.5) |
| ≥ 26 | 12 (14.5) |
The average MMSE score was 24.96 ± 3.38 (range 14 to 30). The average MoCA-INA score was 21.06 ± 4.56 (range 5 to 30). Both scores showed comparable result but MoCA-INA showed lower average and a broader range of scores. Comparison between the MMSE and MoCA-INA Score is shown in Table 2.
Table 2.
Comparisan between the MMSE and MoCA-INA Score
| Score | Mean | SD | Median | Range |
|---|---|---|---|---|
| MMSE | 24.96 | 3.38 | 25 | 14-30 |
| Moca-INA | 21.06 | 4.56 | 21 | 5-30 |
The Pearson’s correlation coefficient between the scores was 0.71 (p < 0.005). A graph showing the comparison between the MMSE and MoCA-INA scores based on age groups is shown in Figure 1. There were no significant differences of both scores based on history of hypertension, diabetes mellitus and previous stroke, but there was a significant difference in MMSE scores based on level of education, but not in MoCA-INA score (Table 3).
Figure 1.
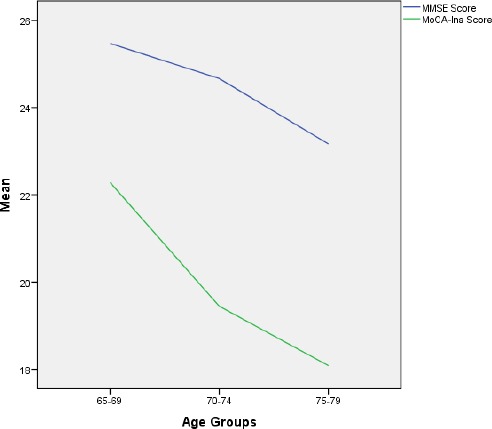
A graph showing the comparison between the MMSE and MoCA scores based on age groups
Table 2.
Comparison between the MMSE and MoCA-INA Score
| Level of Education | MMSE Score | MoCA-INA Score | ||||
|---|---|---|---|---|---|---|
| Mean | SD | P | Mean | SD | p | |
| Elementary | 21.40 | 2.96 | 0.007* | 16.60 | 5.12 | 0.133 |
| Junior High School | 24.67 | 3.36 | 22.00 | 3.24 | ||
| Junior High School | 24.67 | 3.36 | 22.00 | 3.24 | ||
| College/University | 23.96 | 3.58 | 20.87 | 4.24 | ||
One-way ANOVA;
Post-hoc LSD: elementary vs high school p = 0.003; high school vs college p = 0.015.
Table 3
One-way ANOVA. *Post-hoc LSD: elementary vs. high school p = 0.003; high school vs. college p = 0.015.
Discussion
As the rapid growth of the elderly population and the increased prevalence of AD and related disorders, there is an increasing need for effective cognitive screening. This study compared the MMSE and MoCA-INA scores as cognitive screening tools. The Indonesian version of MoCA has been validated and said to be applicable for assessment of cognitive function. There are several adjusments of MoCA-INA compared to the original version in assessment of naming, memory and delayed recall and language function because of transcultural validation [8]. The results showed that The MoCA-INA and MMSE showed comparable results but MoCA-INA showed lower average with wider range of scores. This finding has also been observed in a study by Ohta et al which compared Japanese version of MMSE and MoCA scores in 304 patients with Parkinson’s disease. They found the MMSE and MoCA scores were 26.3 ± 3.6 (range 12-30) and 20.9 ± 5.0 (range 5-30), respectively [9]. A study by Aggarwal et al also found lower MoCA score (22.2 ± 5.1) if compared with MMSE (26.5 ± 3.5) [4].
This finding reflects the MoCA-INA as a more challenging test that includes executive function, higher level languange and complex visuospatial processing that enable it to detect mild impairment or certain domain of cognitive function, if compared to MMSE. The MMSE has both a ‘ceiling’ and ‘floor’ effect: a score of 30 does not always mean normal cognitive function and a score of zero does not mean an absolute absence of cognition. It does not contain much capacity to test frontal/executive or viusospasial (typically right parietal) functions. The pentagon task of the MMSE simply requires the patient to copy the image and does not assess planning skills [10].
This is in line with several previous studies that compared the MMSE and MoCA as cognitive screening tool in differentiating dementia from MCI and normal cognitive aging. A study conducted by Roalf et al in 321 AD patients, 126 MCI and 140 healthy controls found that the MoCA is superior to the MMSE as a global assessment tool, particularly in discerning earlier stages of cognitive decline. In addition, the author found that overall diagnostic accuracy improved when the MMSE or MoCA was combined with an informant-based functional measure [2]. In a study involving 219 healthy control, 299 MCI and 100 AD cases, in which the author analyzed the relationship between the MoCA and MMSE scores, it was found that both tools were more similar for dementia cases, but MoCA distributed MCI cases across a broader score range with less ceiling effect [11]. The MOCA is a useful brief screening tool for the detection of mild dementia or MCI. With a cut-off score of 26, the MMSE had a sensitivity of 17% to detect subjects with MCI, whereas the MoCA detected 83% [12]. The MoCA showed a high sensitivity (0.94) compared to MMSE (0.66) in detecting post stroke cognitive impairment [13].
This study found the differences in MMSE score based on level of education, while the MoCA-INA did not show any significant difference. This finding could also support the superiority of MoCA-INA than MMMSE. MoCA has also been found to be superior to MMSE in assessing cognitive impairment in several other conditions. Wong et al carried out a prospective onservational and diagnostic accuracy study on aneurysmal subarachnoid hemorrhage, The MoCA and MMSE were administered 2-4 weeks and 1 year after ictus. They found that both tools were succesful in differentiating between patients with and without cognitive impairment but at 1 year post-ictus, the MoCA produced higher area under the curve scores for cognitive impairment than the MMSE [14]. MoCA was also found to be more sensitive and reliable than MMSE in testing the cognitive status in epilepsy population with phenytoin monotherapy [15]. The MoCA, but not the MMSE, has adequate psychometric properties as a screening instrument for the detection of mild cognitive impairment or dementia in Parkinson disease [16].
Several advantages of the MMSE includes being the most widely used and studied worldwide and often used as reference for comparative evaluations of other assessments. Its limitations are : education/age/language/culture bias; ceiling effect; best performance for at least moderate cognitive performance. Advantages of the MoCA include being designed to test for mild cognitive impairment and tests many separate domains. Its limitations are: lacks of studies in general practice settings; education bias (≤12 years), limited use and evidence due to published data relatively new (2005) [17].
This study also found a good correlation between the MMSE and MoCA-INA scores (r = 0.71 (p < 0.005). This finding is consistent with several previous studies about correlation between these scores in different clinical setting, such as in an inpatient rehabilitation (r = 0.695, p < 0.003) 4 and in Parkinson’s disease patients (r = 0.74, p < 0.001) 9 and in a clinical cohort (r = 0.82, p < 0.001) [18].
We used cut point of 24 for the MMSE and 26 for the MoCA in this study, so score equal to or less than 24 on the MMSE or less than 26 on the MoCA showed cognitive impairment. Although optimum sensitivity and specificity of the MMSE probably vary depending on the patien’s age and education level, a large body of literature suggests that a general cut point of 23/24 or 24/25 is appropriate for most primary care populations [3, 6].
Interestingly in this study, the proportion of subjects with cognitive impairment found to be higher than normal subjects. Although this could be attributed to history of previous disease (stroke, hypertension and diabetes mellitus), we did not find any statistical differences between these groups indicating the importance of screening for cognitive function in every day clinical practice. Early detection of cognitive impairment that indicates transition to AD may improve diagnosis and lead to better management of the disease. The basic purpose of cognitive screening tests is to indicate a likelihood of cognitive impairment which can be inferred from comparing the patient’s score to reference norms. A very impaired score, along with supporting history and clinical findings may lead a clinician to make a diagnosis, while a borderline score may need a further investigation Cognitive screening test is not intended to substitute a full neuropsychlogical assessment but it can be used to obtain a key for impaired cognitive domain in a patient.
Footnotes
Funding: This research did not receive any financial support.
Competing Interests: The authors have declared that no competing interests exist.
References
- 1.Cullen B, O'Neill B, Evans JJ, et al. A review of screening tests for cognitive impairment. J Neurol Neurosurg Psychiatry. 2007;78:790–9. doi: 10.1136/jnnp.2006.095414. https://doi.org/10.1136/jnnp.2006.095414 PMid:17178826 PMCid:PMC2117747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roalf DR, Moberg PJ, Xie SX, et al. Comparative accuracies of two common screening instruments for classification of Alzheimer's disease, mild cognitive impairment, and healthy aging. Alzheimer's & Dementia. 2012:1–9. doi: 10.1016/j.jalz.2012.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moyer VA. Screening for Cognitive Impairment in Older Adults:U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2014;160:791–7. doi: 10.7326/M14-0496. https://doi.org/10.7326/M14-0496 PMid:24663815. [DOI] [PubMed] [Google Scholar]
- 4.Aggarwal A, Kean E. Comparison of the Folstein Mini Mental State Examination (MMSE) to the Montreal Cognitive Assessment (MoCA) as a Cognitive Screening Tool in an Inpatient Rehabilitation Setting. Neuroscience & Medicine. 2010;1:39–42. https://doi.org/10.4236/nm.2010.12006. [Google Scholar]
- 5.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state.”A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. https://doi.org/10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 6.Sjahrir H, Ritarwan K, Tarigan S, Rambe AS, Lubis ID, Bhakti I. The mini mental state examination in healthy individuals in Medan Indonesia by age and education level. Neurol J Southeast Asia. 2001;6:19–22. [Google Scholar]
- 7.Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S, Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA:a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–9. doi: 10.1111/j.1532-5415.2005.53221.x. https://doi.org/10.1111/j.1532-5415.2005.53221.x PMid:15817019. [DOI] [PubMed] [Google Scholar]
- 8.Husein N, Silvia L, Yetty R dkk. Uji Validitas dan Reabilitas Montreal Cognitive Assessment Versi Indonesia (MoCA-Ina) Untuk Skrining Gangguan Fungsi Kognitif. Neurona Neuro Sains. 2010;27(4):15–22. [Google Scholar]
- 9.Ohta K, Osada T, Shinohara Y, Suzuki N, Takahashi K, Seki M, et al. Comparing the Montreal Cognitive Assessment with Mini-Mental State Examination in japanese parkinson's disease patients. Neurology and Clinical Neuroscience. 2014;2:44–49. https://doi.org/10.1111/ncn3.80. [Google Scholar]
- 10.Woodford HJ, George J. Cognitive assessment in the elderly:a review of clinical methods. Q J Med. 2007;100:469–484. doi: 10.1093/qjmed/hcm051. https://doi.org/10.1093/qjmed/hcm051 PMid:17566006. [DOI] [PubMed] [Google Scholar]
- 11.Trzepacz PT, Hochstetler H, Wang S, et al. Relationship between the Montreal Cognitive Assessment and Mini-mental State Examination for assessment of mild cognitive impairment in older adults. BMC Geriatrics. 2015;15:107. doi: 10.1186/s12877-015-0103-3. https://doi.org/10.1186/s12877-015-0103-3 PMid:26346644 PMCid:PMC4562190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith T, Gildeh N, Holmes C. The Montreal Cognitive Assessment:Validity and Utility in a Memory Clinic Setting. Can J Psychiatry. 2007;52(5):329–32. doi: 10.1177/070674370705200508. https://doi.org/10.1177/070674370705200508 PMid:17542384. [DOI] [PubMed] [Google Scholar]
- 13.Godefroy O, Fickl A, Roussel M, Auribault C, Bugnicourt JM, Lamy C, et al. Is the Montreal Cognitive Assessment superior to the Mini-Mental State Examination to detect poststroke cognitive impairment? A study with neuropsychological evaluation. Stroke. 2011;42:1712–1716. doi: 10.1161/STROKEAHA.110.606277. https://doi.org/10.1161/STROKEAHA.110.606277 PMid:21474808. [DOI] [PubMed] [Google Scholar]
- 14.Wong GK, Lam SW, Wong A, Ngai K, Poon WS, Mok V. Comparison of montreal cognitive assessment and mini-mental state examination in evaluating cognitive domain deficit following aneurysmal subarachnoid haemorrhage. PLoS One. 2013;8(4):e59946. doi: 10.1371/journal.pone.0059946. https://doi.org/10.1371/journal.pone.0059946 PMid:23573223 PMCid:PMC3616097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nathami R, Amirthalingam P, Mukunthu, et al. Sensitivity of Montreal Cognitive Assessment in Comparison with Mini MentalStatus Examination in Testing Cognitive Status in Epilepsy Patients with Phenytoin Monotherapy. AJPCT. 2015;3(03):237–244. [Google Scholar]
- 16.Hoops S, Nazem S, Siderowf AD, et al. Validity of the MoCA and MMSE in the detection of MCI and dementia inParkinson disease. Neurology. 2009;73:1738–1745. doi: 10.1212/WNL.0b013e3181c34b47. https://doi.org/10.1212/WNL.0b013e3181c34b47 PMid:19933974 PMCid:PMC2788810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cordell CB, Borson S, Boustani M, Chodosh J, Reben D, Verghese J, et al. Alzheimer's association recommendations for operationalizing the detection of cognitive impairment during the Medicare Annual Wellness Visit in primary care setting. Alzheimer's & Dementia. 2013;9:141–150. doi: 10.1016/j.jalz.2012.09.011. https://doi.org/10.1016/j.jalz.2012.09.011 PMid:23265826. [DOI] [PubMed] [Google Scholar]
- 18.Roalf DR, Moore TM, Hamilton DM, Wolk DA, Arnold SE, Weintraub DA, et al. Bridging cognitive screening tests in neurologic disorders:A crosswalk between the short Montreal Cognitive Assessment and Mini-Mental State Examination. Alzheimer's & Dementia. 2017:1–6. doi: 10.1016/j.jalz.2017.01.015. https://doi.org/10.1016/j.jalz.2017.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]


