Abstract
Translation research in occupational safety and health is the application of scientific investigative approaches to study how the outputs of basic and applied research can be effectively translated into practice and have an impact. This includes the study of the ways in which useful knowledge and interventions are disseminated, adopted, implemented, and institutionalized. In this paper, a 4-stage framework (Development, Testing, Institutionalization, and Evaluation) is presented. Translation research can be used to enhance the use and impact of occupational safety and health knowledge and interventions to protect workers. This type of research has not received much attention in the occupational safety and health field. However, in contemporary society, it is critical to know how to make an impact with the findings and outputs of basic and applied research. This paper provides a novel framework for consideration of how to advance and prioritize translation research for occupational safety and health.
Keywords: dissemination, intervention, research-to-practice
1 | INTRODUCTION
The occupational safety and health (OSH) research field historically has focused more on the etiologic end of the research-to-practice (r2p) continuum than on the implementation and impact end.1–4 This also has been the case in medicine and public health fields.5–7 There has been a call to increase efforts to investigate factors that enhance or limit the development, transfer, and use of OSH risk factor and intervention information and technology, thus ensuring that these outputs lead to improvements in worker health.1–4,8–13
There is an extensive amount of OSH research and developed knowledge that is not applied. For example, much is known about the cause and prevention of occupational hearing loss, but it is still one of the most prevalent occupational illnesses.14 Similarly, workers are still exposed to lead, one of the oldest known toxicants, at levels much higher than recommended.15 The list of known but uncontrolled or inappropriately controlled hazards is long and growing, even though risk management techniques are known.16–18 Consequently, there is value in studying factors that influence the uptake and use of new and extant research findings.
The purpose of this paper is to develop a framework, or basic conceptual structure, for the consideration and promotion of translation research in the OSH field. The framework could be used by OSH organizations, defined here to include academics, government agencies, trade associations, unions, insurers and NGOs (nongovernmental organizations) to consider, conduct, and benefit from translation research. Although the components of this framework are not novel, their adaptation for OSH research is a new and needed perspective.
1.1 | Foundation, scope, and nomenclature for translation research
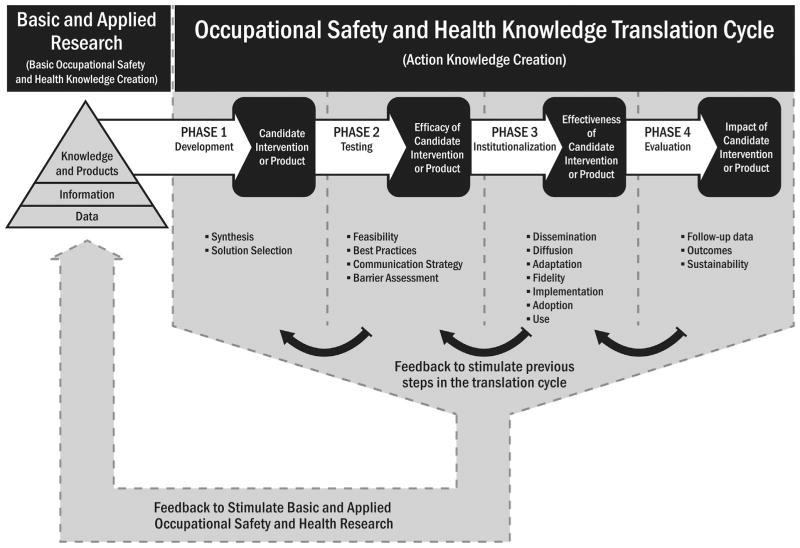
The subject of translation research is the nature and drivers of translation processes and barriers to them. Translation research encompasses the scientific study of factors that optimize closing the gap between new or extant research findings and guidance, and real-work practices, outcomes, and impacts in the workplace (Figure 1). As such, translation research has three aspects: it is a set of methodologies, a body of substantive scientific knowledge, and a perspective for viewing a continuum of research efforts from the identification of hazard and risks, through intervention to impact.6,7,19–35
FIGURE 1.
Conceptual framework for translation research in occupational safety and health
Translation research is a multidisciplinary field of research composed of such disciplines as intervention effectiveness research,9,36 implementation research,5,37 health communication, and dissemination research,38–42 evaluation research,126 knowledge utilization,9,24,36,41,43,44 diffusion of innovations research,38–40 social marketing and commercial marketing,40,45,46 and surveillance and economic evaluation.47–52 However, application of these and related approaches in the OSH field has been limited and as Rantanen1 has noted, “such research on research is relatively scarce and even the paradigm for such studies is not well developed.”
Quite often the phrase “translation research” has been used to describe the systematic effort to convert basic research outputs into practical applications to enhance human health and well-being.53 As such it is frequently referred to as “translational research” or “translational science.”54 Various journals or programs refer to the term “translational” in the title (eg, American Journal of Translational Research), and the National Institutes of Health (NIH) has the National Center for Advancing Translational Sciences. Generally, these uses of the phrase translational research refer to harnessing knowledge from basic medical science to bring it to clinical practice (so called bench-to-bedside models). In contrast, we define the phrase “translation research” to refer to the study of the process of moving “research-to-practice-to-impact” and the methods, barriers and facilitators and context (social, political, organizational, etc.) encountered in this process.55 However it should be noted that in the literature the two descriptors of research (translation and translational) overlap.56 In this article, we use “translation research” generally to refer to the study of the processes that move research/innovations from adoption, to implementation to maintenance/institutionalization in the workplace.
1.2 | Adaptation to the OSH field
The translational model (bench to bedside) for clinical medicine may be adapted to the OSH field.5,21,23,25,28,36,43,44,57–60 The objectives of using this translational model are to identify important basic or etiologic findings and subsequent interventions and to study how they can best be applied to address workers’ occupational safety and health.
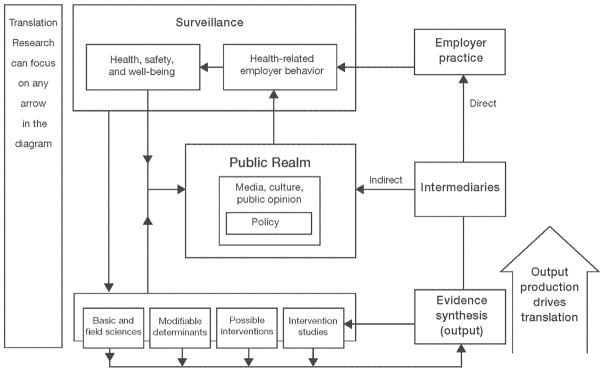
Additionally, there may be a need to consider iterative and bidirectional processes, which are integral to OSH translation. This need to consider iterative processes has been captured conceptually in a translation research model for public health developed by Ogilvie et al, which provides an integral role for surveillance in assessing impact and identifying modifiable determinants.25
Translation research in OSH is envisioned to be theory-based and model-based, drawing on the demand and control model,61 health belief model62 the transtheoretical model of change,40 Precede-Proceed model,63 health promotion model,64 and social cognitive theory,65 among others. Such research can occur at any of the connecting arrows in Figure 2. We have modified Figure 2 to include employers and intermediaries, so that it also connotes that there are many stakeholders (ie, employers, business owners, labor organizations, resource managers) in OSH with differing agendas and concerns.
FIGURE 2.
Critical focus points for translation research in occupational safety and health
Taking into account the strengths of the clinical and public health models, we propose a framework (shown in Figure 1 and Table 1) for translation research for the OSH field that encompasses adaptations of the four traditional stages of translation research to optimize the development and dissemination of research outputs in ways that motivate target audiences concerned with worker health and safety to adopt, implement, and sustain change to improve workplace safety and health.30,89 This framework (Figure 1, Table 1) builds on the NIH model,90,91 interpreted by Khoury et al,23 as well as the Noonan and Emshoff model,55 the public health model of Ogilvie et al,25 Knowledge to Action (KTA) and Knowledge Transfer and Exchange (KTE) models,20,92,93 and the extensive portrayal of OSH translation research in the commercial fishing industry by Lucas et al.60 The framework utilizes a linear pathway from underlying basic or applied OSH information and knowledge to impact, with a continuous cycle of feedback loops to stimulate research at all points along the pathway. A linear pathway is used to represent a holistic view of the potential intended direction from each translation research stage and the underlying risk being reduced (eg, hearing loss, musculoskeletal disorders, respiratory disease) to the final eradication or control of that risk (ie, reductions in mortality, morbidity, and injury).
TABLE 1.
Examples of translation research for different types of hazards
| Physical agent: noise-induced hearing loss | |||
|---|---|---|---|
| Stage | Description | Reference | |
| 0a | Hazard/Problem Identification | Occupational noise-induced hearing loss | Dobie66; Hager67 |
| 1 | Development | Development of protocol for testing hearing protection Devices | Berger et al68 |
| 2 | Testing | Hearing protector effectiveness study | Morata69; Murphy et al70 |
| 3 | Institutionalization | Identifying attitude and behaviors associated with wearing hearing protection | Stephenson and Stephenson71; Bocksteel et al72 |
| 4 | Evaluation | Impact of hearing conservation on incidence of hearing loss | Davies, et al73; Masterson et al14 |
| Hazardous substance: silicosis in mining | |||
| 0 | Hazard/problem identification | Identification of silicosis in mining | Wagner74 |
| 1 | Development | Development of an intervention | Cecala and O’Brien75 |
| 2 | Testing | Testing worker response to intervention | Haas et al76 |
| 3 | Institutionalization | Development of guidelines for widespread use | Reed et al77 |
| 4 | Evaluation | Utilization of on-going or new surveillance data to determine impact | Need studies of use of interventions, studies of silicosis prevalence, incidence, mortality |
| Psychosocial hazard: stress | |||
| 0 | Hazard/problem identification | Identification of stress hazards in healthcare workers | Bourbonnais et al78 |
| 1 | Development | Development of interventions in healthcare | Bourbonnais et al79 |
| 2 | Testing | Testing the effects of modifying the psychosocial work Environment | Jimmieson et al80 |
| 3 | Institutionalization | Systematic review of effectiveness of various interventions | Ruotsalainen et al81 |
| 4 | Evaluation | Surveillance | Dollard et al82 |
| Safety hazard: Winch entanglements resulting in severe traumatic injuries and fatalities | |||
| 0 | Hazard/problem identification | Identification of injuries involving winches | NIOSH83 |
| 1 | Development | Development of anxillary stopping switch | Lincoln et al84; Lincoln et al85 |
| 2 | Testing | Testing interventions in target users | Levin et al., 86; Lincoln et al85 |
| 3 | Institutionalization | Examing methods of implementation | Teske and Victoroff87 |
| 4 | Evaluation | Surveillance of injuries | National Institute for Occupational Safety and Health (NIOSH)88 |
0a Stage 0 is the basic or applied research finding that becomes the focus for study in stages 1–4 of the translation research framework. It is not part of that framework.
The framework utilizes a variety of different disciplines and approaches to learn how best to put research into practice. Translation research efforts can now close the gap between basic and applied research outputs and OSH impact by studying the best ways that validated candidate interventions, research findings, and authoritative recommendations can systematically and sustainably be moved to adoption in ways that address workplace health and safety problems.
1.3 | Objectives of translation research for occupational safety and health
There are two proposed objectives of the framework for translation research. The first is to develop generalizable knowledge related to the research-to-practice continuum for the OSH field. The second is to apply this generalizable knowledge whenever possible to provide feedback to organizations that develop or use OSH information (ie, OSH organizations) and investigators to improve their efforts.
Important translation research should include studies that:
Examine how best to facilitate and optimize awareness among key audiences of OSH organizations’ activities and outputs94–95;
Investigate methods to improve decision makers’ (eg, employers) ability to act upon authoritative recommendations and guidance (research-to-practice);
Increase researchers’ responsiveness to and collaboration with stakeholders (eg, employers and workers), so that the information and advice end users receive fit their needs, priorities, and circumstances (practice-to-research)63;
Explore what motivates partners, stakeholders, and intermediaries to more effectively seek, model, and communicate credible OSH organizations’ recommendations and guidance to others;
Identify barriers as well as solutions for overcoming these barriers in political, social, and economic systems that inhibit the translation of practices or technologies into the workplace;
Assess readiness of the target audience to receive this guidance, and shed light on the factors that facilitate or hinder adoption decisions.38,39,96
Evaluate the implementation of evidence-based programs, including whether and how they are implemented with fidelity (ie, as designed) and adaptations made to the original program.
Assess the impact of interventions and practices on workers’ morbidity, mortality, and well-being.
1.4 | Framework for translation research in the occupational safety and health field
Levels of implementation of research findings, technological innovations, and recommendations, as well as guidance focused on worker health and safety, remain suboptimal across many industrial sectors.3,15,97 Information is necessary, but insufficient, for facilitating behavior change in the workplace,98 and it is known that simply sharing knowledge about new discoveries on websites, publishing and disseminating technical reports and journal articles, and presenting at conferences is inadequate to change OSH investment and practice on a large scale.2,99 Therefore, for promising practices to be enacted on a large-scale, it is critical to explore the characteristics of an innovation, the characteristics of an adopting organization (and the individuals within that organization), and their interactions that predict the uptake and maintenance of that innovation.38,55,96,100 Without a stronger focus on translation research, the OSH field may continue the processes of knowledge creation without adequate attention to what creates effective uptake of research outputs and how to best execute the translation process.
The framework for translation research in OSH proposed here was developed by an internal NIOSH workgroup with expertise in such fields as intervention effectiveness research, implementation science, communication and diffusion research, program evaluation, and impact evaluation among others. The NIOSH workgroup surveyed the relevant literature on translation research frameworks and adapted the existing NIH framework to include elements of other frameworks including the KTA,92 and Noonan and Emshoff models,55 the KTE approach of Lavis et al20 and Estabrooks and Glasgow,101 and the interpretation by Lucas et al.60
As stated earlier, an objective of applying these research efforts to the outcome end of the research-to-practice continuum is to develop relevant, generalizable, and specific knowledge on how to obtain optimal impact of research outputs. Common challenges in pursuing this objective includes: (1) Defining subcategories of intermediate and end outcomes; (2) Studying how decision-makers (employers, insurers, government agencies) get and use OSH information and the barriers they encounter; and (3) Identifying which approaches work and do not work in achieving impact of OSH research outputs. This framework requires the development of a comprehensive OSH research agenda focused on high-priority translation research goals.
2 | FOUR STAGES OF TRANSLATION RESEARCH IN OSH
A prerequisite for effective translation research in OSH is to take a holistic view of the potential pathway from each OSH basic research result to reduction of underlying OSH risk to the final eradication or control of that problem. Within that pathway, it is possible to conceptualize four stages of translation research. The pathway is multidimensional in that each stage of translation research may not lead specifically to the next stage but may provide useful information for practitioners of r2p to construct and implement impact-generating efforts and practices. Translation research is intentionally portrayed with linear models because it is goal oriented. Thus each study at each stage needs to be viewed as part of a continuum of efforts to reach the goal of reduced burden of the hazard or problem identified. This linear view does not preclude extensive feedback to various prior stages but the overall direction is toward a goal of reducing a specific risk. Table 1 shows examples of the four stages (Development, Testing, Institutionalization, and Evaluation) of research for four different types of hazards. Prior to the four stages, is stage 0 (referred to in Table 1 as Hazard/Problem Identification), which is the performance of basic and applied research that leads to the identification of hazards and risks, or to the indication of a solution or intervention that is needed or could be developed.
2.1 | Stage 1: Development
This initial stage is the assessment of technology, equipment, program designs, measures, or analyses needed to develop interventions from, or applications of, basic research.22 Here, the subject of study is the first step in moving the outputs of OSH research into a trialable prototype or program. For example, in seeking a solution to the problem of the inability to measure effectiveness of hearing protection as it is used on worksites, NIOSH scientists created and tested within their laboratories a laptop-based system capable of conducting onsite fit testing of hearing protection.102 They then created a candidate, potentially marketable, invention that employers could use to gather information about the effectiveness of the hearing protection being used by their workforce in real time. Small pilot testing on a limited “proof of concept” basis occurred at this stage, to inform the process of refining a marketable invention derived from laboratory-based knowledge of hearing protection effectiveness measurement. Reports were published in the peer-reviewed literature and presented at key conferences.103 Developing marketable interventions requires obtaining feedback from potential users of the interventions as well as evaluating economic, social, and cultural appeal. Many, if not most, OSH researchers currently address workplace health and safety hazards through this level of research. Another example is the development of the NIOSH ladder safety application (app) for smartphones,104 which has subsequently become the subject of stage 2 and 3 translation research efforts.
Additionally, related training and health communication research occurs in the OSH field complementary to this stage and can be thought of as developmental, assessing the options for audience segmentation, channels of dissemination, message design, forms of delivery of messages, or usability studies before technology is finalized.4,99,105
Researchers may conduct studies that result in the production of health communication products in a variety of formats (written, web, video, social media). There are still many research gaps relating to the investigation of factors that affect how research findings can be optimally “written” and presented in a variety of formats and messages to motivate policy makers, OSH professionals, and decision makers (including workers and employers) in businesses.
Stage 1 translation research supports and informs the scaling up of basic research outputs toward efficacy research in stage 2. This work could also resolve critical translation research questions related to optimal “dosage” of interventions. Other activities include developing options for the packaging, transmission, and dissemination of workplace OSH guidance and interventions.
For example, NIOSH produces significant model training programs and products that are typically turned over to study partners on a small scale or published for distribution on a website. Training research that identifies and investigates gaps in knowledge associated with refresher training is needed to improve evidence-based guidance about the frequency, level of engagement, and modality of training methods. Similarly, all industries are utilizing online training as a way to impart knowledge, but there is a gap in the understanding of factors critical to effective online training. Research on transfer of training is an example of translation research.105
Laboratory-based translation research is by definition generally at the stage 1 level although other stages may come into play over time. Critical issues to consider in stage 1 translation research include: What are the greatest needs within the OSH organization to assist laboratory investigators in moving their discoveries and recommendations out of the laboratory? Can OSH organizations identify promising solutions bogged down in stage 1 or clearly ready for a stage 2 trial?
2.2 | Stage 2: Testing
This second stage should capture and analyze evidence-based success stories, including case studies, pilot work, and small intervention studies that can be scalable into stage 3 intervention effectiveness trials. There is a persistent need in OSH research to document, validate, replicate, and/or generalize isolated OSH successes to gather evidence needed to justify a stage 3 large scale effort. Research at this level should involve significant interaction between researchers and users leading to exchanges of information, synthesis of evidence, and dialogue with key partners about feasibility of recommendations, including cost benefit analyses on a local scale.
Stage 2 research assesses the efficacy and potential value of a new finding, invention, process, training program, or intervention for larger scale OSH application or practice to a targeted work sector, or for a targeted health outcome across sectors. Thus testing stage research seeks to assess the internal validity of the research by examining whether the promising laboratory or pilot effort is effective in the workplace. The goal of this step is to gather formal evidence that a new process, training program, workplace intervention, authoritative recommendation, or technology can be feasibly utilized in an effective manner with a targeted workplace or workplaces. In other words, it serves as an experimental opportunity to assess the potential future impact of large-scale utilization of the program or process.
For example, a current NIOSH translation research study is focusing on a major employer to test a new approach to training temporary workers before their placement on job sites. Another study is exploring work with insurers to test a new mobile phone application designed to provide on-worksite guidance to safe work practices for addressing common hazards in residential construction. Outputs at this level may include peer-reviewed publications and government reports, training products, or technology ready for widespread use. Stage 2 research may also focus on enablers, barriers to action, and the characteristics of the innovation and the adopting organization which may inform efforts to scale up the intervention. Similarly, research in OSH is needed to shed light on the predictors of effective program implementation. As Fixsen et al, point out in their extensive review, implementing a program effectively is as important as implementing an effective program. A more detailed discussion of these points is provided under stage 3 below.5
Most OSH field intervention, training, and outreach studies completed in the past could be considered as stage 2 translation research. Most have been conducted on a limited basis with an industry partner, at a few companies, or with limited workplace samples. Typically, results from those studies are published in the peer-reviewed literature and perhaps products are handed off to participating partners, but with that, the OSH research organization efforts usually end. There is a need for further research emphasis and activity beyond the publication stage. Translation research fills this gap. Translation researchers should convene periodically to identify those successful (eg, published evidence-based) small scale studies that warrant scaling up to a nationwide or industry-wide intervention and that serve as potential process models. When promising interventions are noted, prioritized funding could be utilized to move them into stage 3 studies.
2.3 | Stage 3: Institutionalization
The third stage of the translation research framework involves studies of evidence-based technology and recommendations into well accepted OSH practice, through large-scale delivery, dissemination, and diffusion research.17,28,47,60,106,107 The emphasis now is on external validity, resolving implementation challenges, and ensuring that an intervention or recommendation actually works within and can be integrated into a broad range of workplace settings. It should be noted that, although internal validity criteria are important for measuring translation research outcomes, studies specifically designed to maximize external validity and that provide estimates of the effectiveness of an intervention across target populations, cultural contexts, delivery agents, and modalities are currently limited and more are needed to expand the public health evidence base.7,63,108,109 Studies at this stage involve identifying methods for overcoming diffusion and utilization obstacles and opening channels to ensure OSH products and guidance are integrated and utilized in a sustainable way by targeted industries on a sector or national scale. In this stage, smaller successful interventions validated through stage 2 studies may be scaled up so that they reach all or nearly all targeted workers.
2.3.1 | Uptake
Research is needed in the OSH field related to why and how new programs, practices and policies are taken up by stakeholders. Scientific support for the effectiveness of an intervention is just one of a set of perceived attributes that can affect adoption decisions.39 When considering uptake of innovations, business enterprises engage in a complex cost-benefit analysis as to the risk and advantages of change. Stakeholders may prioritize factors such as compatibility with existing programs, cost-effectiveness, the values of individuals within the organization and the culture of the organization, and relative advantage over other programs when making adoption decisions.38,109 Furthermore, as Weiner points out, organizational readiness for change must be gauged to determine the extent to which employers and employees within organizations are “psychologically and behaviorally” prepared to make the changes in policies, practices and processes that are necessary to enact an innovation and to support its on-going use.96
Once innovative OSH programs are put into place, translation research is needed to understand the factors that lead to sucessful implementation of innovations. As Durlak and DuPre37 note in their extensive review of nearly 500 non-occupational implementation studies, the magnitude of mean effect sizes are at least two to three times higher when programs are carefully implemented than when implementation is incomplete or unsuccessful. The fidelity of program implementation is also a critical aspect for exploration, and one that is not often a focus of OSH research. The concept of fidelity, sometimes called adherence, integrity, or program “dosage,” is a determination of how well a program is delivered as it was designed (and tested in the efficacy stage).110 Durlak and DuPre reported evidence from 59 quantitative studies confirming that higher levels of implementation are in general associated with better outcomes, particularly when fidelity or dosage is assessed.37
By necessity, work at this level involves working with intermediaries already serving targeted employers, workers, and workplaces to understand their motivation to engage in new or additional OSH activities and finding ways to integrate new knowledge or technology into their existing programs and practices in a sustainable manner. Very little OSH work has been conducted at stages 3 and 4.28,89,107,111 One stage 3 example is a NIOSH partnership with the Mexican consulates and Mexican Ministry of Health to integrate information and guidance about OSH into all of their consulate educational programs.112,113 While initial work (stage 2) was conducted in several consulates to test and fine tune messages and approach, scaled up interventions and guidance (stage 3) have involved all 50 consulates with the goal of reaching all Mexican immigrants served by those consulates with basic OSH information.
2.3.2 | Barrier assessments
Across multiple domains of OSH research, barrier assessments are a critical focus for stage 3 translation research (as well as stage 2 translation research). Common barriers such as lack of reporting on moderating variables or lack of evidence of sustainability are reported in the medical translation research literature and related to health education and health promotion programs.7,22 This literature may provide indications of external barriers preventing OSH translation as well. There is a need to assess and document barriers to and facilitators of institutionalizing and sustaining new recommendations, training, or technology leading to generalizable knowledge that in time should measurably improve the health and safety of workers.
Thus investigations should be developed to look at OSH professional provider motivation/behavior and attitudes; factors affecting gatekeepers of information (employers, unions, service providers, suppliers) and new work practices; organizational structures that either encourage or discourage change; adequacy and usability of information systems; lack of incentives or strong disincentives; key decision makers; and financial barriers.11,20,34,47,60,100,114 It may also be fruitful to conduct research regarding internal threats to OSH translation processes, motivational factors, or systems that inhibit translation activity within work organizations. For example, a new project called “Increasing Adoption of Safety Technologies in Commercial Fishing” will conduct translation research to improve adoption of existing NIOSH engineering interventions to protect deckhands from winch entanglements.87
Stage 3 translation research should also: 1) explore means to overcome such barriers and 2) determine effective methods to identify and incentivize, key decision-makers, and intermediaries influencing large scale intervention effectiveness. In essence, stage 3 research should effect widespread change through participant leadership and involvement—discovering who the “right” people are and what they want.6,115 Indeed, it is in stage 3 institutionalization research where the most critical knowledge gaps remain, and where the OSH field stands to benefit the most from translation research.
A critical tool that can be used in stages 3 and 4 translation research is the use of systematic reviews. These reviews are means to evaluate how well interventions and plans are being implemented and their impact on various scales.32,81,116–119 The use of systematic reviews in occupational safety and health is increasing and it will drive translation research.119
2.4 | Stage 4: Evaluation
Stage 4 seeks to investigate the “real world” health, safety, economic, and well-being impacts of integrating these new OSH discoveries and interventions into large scale practice. Stage 4 emphasizes research specifically focusing on the impact of translation efforts on workplace illnesses, injuries, and fatalities; thus, this stage should complement surveillance efforts. A good example of stage 4 translation research was described by Lucas et al.60 It involved analysis of fatality and survival data for commercial fishing vessels during the period 1991–1997. The study found that “decedents of vessel disasters were less likely than survivors to have received safety training, supporting the hypothesis that training improves survival.19”
Evaluation stage translation research includes a persistent yet critical need to assess real-world effects of an OSH organization’s outputs in short-, medium-, and long-term time frames. This type of work is among the most challenging in OSH research, but OSH organizations can begin to better measure their impact if they can: (1) develop and test methods to assess impact at various time points in the future; (2) utilize ongoing surveillance and retrospective studies to assess impact; (3) utilize systematic reviews and meta-analyses to determine if these are real-world evaluations and what they indicate for worker safety and health116,119; (4) incorporate findings from impact assessments so that new “impact-making” efforts can be developed; and (5) engage their stakeholders in the evaluation process, (eg, monitoring PPE sales, documenting expansion of technology distribution networks or identifying reductions in policy holder workers’ compensation claims). Additionally, there is a knowledge gap related to identifying clear causal links between OSH organizations’ research translation efforts and related improvements in health and safety outcomes. Thus, evaluation stage translation research efforts should also include specific attention to levels of fidelity and adaptation of interventions as they are adopted into large-scale use.
Important for stage 4 translation research is the need to answer three data availability and use questions: In what way can translation research efforts utilize economic and epidemiological/surveillance outcome data? Are there obvious and fruitful collaborations, especially for stage 4 efforts? Can OSH organizations improve data collection related to translation research in their applied and public health practice efforts. Specifically, can they standardize elements to capture process and outcome data, facilitate economic analysis, validate quality of data, and determine how to gather and use after-action reports, grant reports, and other evidence-based performance measures?
3 | CONCLUSION: USING THE FRAMEWORK
The development of evidence-based guidelines, new findings and interventions, and novel technologies is a continually evolving process. The four stages of translation research (Figure 1 and Table 1) can at times overlap and provide feedback loops to previous stages which can inform improvements in knowledge uptake.
In all instances, translation research should remain focused on solutions, that is, understanding how best to reduce the risk of a workplace safety and health problem, how to change less effective workplace practices, and how to overcome barriers to adoption of new information and integration of new workplace practices. Efforts should be directed toward those technologies, interventions, and guidance that are scalable, and might be feasibly expected to provide optimal workplace health for many. OSH translation research should emphasize investigating effectiveness (ie, evidence under real-life conditions), and should be broadly thought of as encompassing multifactorial elements that may be drawn from work in biological, engineering, industrial hygiene, psychosocial, economic, legal, cultural, manufacturing, and marketing as well as other possible domains—as all have an impact on workers, employers, and workplaces. Translation research at its best also should study transferability—the successful application to diverse workplace settings.120 This emphasis on transferability does not ignore factors specific to success in certain workplace settings, but emphasizes a goal of conducting translation research with maximum potential to generalize across workplaces. This also makes particular interventions easier to disseminate, for example, personal flotation device manufacturers are more likely to invest in designing and distributing better products if their consumer population includes more than just commercial fishermen.60
Translation research should become an integral part of the complex feedback loop that characterizes the OSH field’s value to the nation. As such, translation research should be focused on areas where there is a large burden on workers, employers, and society in terms of morbidity, mortality, cost, and distress or where there is the greatest opportunity for success.16,121–125 Translation research findings stand to add significant value by informing and optimizing the work of OSH research, communication efforts, direct product disseminations, and technology transfer. This program of research should increase the likelihood that OSH organizations’ effective, science-based OSH information, and technology is sought and used by others who are in a position to make changes in workplaces. This research should also ensure that OSH organizations partner with effective and influential stakeholders and intermediaries in ways that maximize the impact of the organizations’ production and dissemination of scientific information and technology. Each translation effort or approach studied should drive new translation research through lessons learned, development of novel methodologies and metrics, and validation of evolving mediums and channels for outreach. Ultimately, translation research needs to focus on whether the outputs of OSH organizations make a difference. Do they have an impact on health, safety, economics, and well-being? For translation research to take hold and grow there will be a need to shift some research investments to the more distal areas of the research-to-practice continuum.
The framework proposed here requires the development of an effort within the OSH field to nuture, promote, and coordinate translation research. This framework was developed because there is a pressing need to focus on the last steps in the process of applying knowledge to protect the health, safety and well-being of workers. Translation research can be helpful in meeting this need.
Acknowledgments
National Institute for Occupational Safety and Health (NIOSH).
The authors thank the following for comments on earlier drafts: Linda Goldenhar, Julie Sorensen, James Emshoff, and thanks to Nicole Romero for graphic support and Amanda Keenan and Amanda Stammer for processing support.
FUNDING
This work was conducted at the National Institute for Occupational Safety and Health.
Footnotes
AUTHORS’ CONTRIBUTIONS
Paul Schulte and Carol Stephenson chaired a working group of the authors and developed the first draft. Thomas Cunningham revised the manuscript. All authors participated in the development of concepts used in the paper and in the editing.
ETHICS APPROVAL AND INFORMED CONSENT
Not applicable.
DISCLOSURE (AUTHORS)
The authors report no conflicts of interest.
DISCLOSURE BY AJIM EDITOR OF RECORD
Rodney Ehrlich declares that he has no conflict of interest in the review and publication decision regarding this article.
DISCLAIMER
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health.
References
- 1.Rantanen J. Research challenges arising from changes in work life. Scand J Work Environ Health. 1999;25:473–483. doi: 10.5271/sjweh.469. [DOI] [PubMed] [Google Scholar]
- 2.Schulte PA, Okun A, Stephenson CM, et al. Information dissemination and use: critical components in occupational safety and health. Am J Ind Med. 2003;44:515–531. doi: 10.1002/ajim.10295. [DOI] [PubMed] [Google Scholar]
- 3.National Research Council (NRC) Evaluating Occupational Health and Safety Research Programs: Framework and Next Steps. Washington, DC: National Academies Press; 2009. [PubMed] [Google Scholar]
- 4.Gillen M. The NIOSH construction program: research to practice, impact and developing a national construction agenda. J Safety Res. 2010;41:289–299. doi: 10.1016/j.jsr.2010.04.002. [DOI] [PubMed] [Google Scholar]
- 5.Fixsen DL, Naoom SF, Blase KA, Friedman RM, Wallace F. Implementation research: a synthesis of the literature. Tampa, FL: University of South Florida, Louis de la Parte Florida Mental Health Institute, The National Implementation Research Network; 2005. FMHI Publication No. 231. [Google Scholar]
- 6.Rohrbach LA, Grana R, Sussman S, Valente TW. Type II translation: transportion prevention interventions to real-world settings. Eval Health Prof. 2006;29:302–333. doi: 10.1177/0163278706290408. [DOI] [PubMed] [Google Scholar]
- 7.Glasgow RE, Emmons KM. How can we increase the translation of research into practice? Types of evidence needed. Annu Rev Public Health. 2007;28:413–433. doi: 10.1146/annurev.publhealth.28.021406.144145. [DOI] [PubMed] [Google Scholar]
- 8.GPRA Modernization Act of2010. PL 111–352, Jan 4:2011.
- 9.Goldenhar LM, LaMontagne AD, Katz T, Heany C, Landbergis P. The intervention research process in occupational safety and health: an overivew from the National Occupational Research Agenda Intervention Effectiveness Research team. J Occup Environ Med. 2001;43:616–622. doi: 10.1097/00043764-200107000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Howard J. Informing public health policy and practice: the strategic management of research processes and organizations. Governance. 2009;22:203–216. http://evidencebasedliving.human.cornell.edu/2010/08/18/what-is-translation. [Google Scholar]
- 11.Desmarais L, Lortie M. La dynamique du transfert des connaissances: une perspective centrée sur l’usager. The dynamics of knowledge transfer: a user-centered perspective. The workplace collection of chair in health and safety in the workplace management. Quebec, QC: Presses de l’université Laval; 2011. [Google Scholar]
- 12.CPWR (The Center for Construction Research and Training) [Accessed December 12, 2016];R2p Tools: Roadmaps. 2014 Available at: http://www.cpwr.com/research/r2p-tools-roadmaps.
- 13.Research to practice (r2p) roadmap: guidance document for general industry. University of California; Berkeley: 2014. [Accessed December 12, 2016]. LOHP-Labor Occupational Health Program. Available at: http://lohp.org/research-to-practice-r2p-roadmap/ [Google Scholar]
- 14.Masterson EA, Deddens JA, Themann CL, Bertke S, Calvert GM. Trends in worker hearing loss by industry sector, 1981–2010. Am J Ind Med. 2015;58:392–401. doi: 10.1002/ajim.22429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Alarcon WA. Elevated blood lead levels among employed adults – United States, 1994–2013. MMWR. 2016;63:59–65. doi: 10.15585/mmwr.mm6355a5. [DOI] [PubMed] [Google Scholar]
- 16.Takala J, Hämäläinen P, Saarela KL, et al. Global estimates of burden of injury and illness at work in 2012. J Occup Environ Hyg. 2014;11:326–337. doi: 10.1080/15459624.2013.863131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Urbina I. New York Times. Mar 30, 2013. As OSHA emphasizes safety, long-term health risks fester. [Google Scholar]
- 18.Deveau M, Chen CP, Johanson G, et al. The global landscape of occupational exposure limits-implementation of harmonization principles to guide limit selection. J Occup Environ Hyg. 2015;12:S127–S144. doi: 10.1080/15459624.2015.1060327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Perkins R. Evaluation of an Alaskan marine safety training program. Public Health Rep. 1995;110:701–702. [PMC free article] [PubMed] [Google Scholar]
- 20.Lavis JN, Roberston D, Woodside JM, McDeod CB, Abelson J. How can research organizations more effectively transfer research knowledge to decision makers? Milbank Q. 2003;81:221–248. doi: 10.1111/1468-0009.t01-1-00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Woolf SH. The meaning of translational research and why it matters. JAMA. 2008;299:211–213. doi: 10.1001/jama.2007.26. [DOI] [PubMed] [Google Scholar]
- 22.Sussman S, Valente TW, Rohrbach LA, Skara S, Pentz MA. Translation in the health professions: converting science into action. Eval Health Prof. 2006;29:7–32. doi: 10.1177/0163278705284441. [DOI] [PubMed] [Google Scholar]
- 23.Khoury MJ, Gwinn M, Yoon PW, Dowling N, Moore CA, Bradley L. The continuum of translation research in genomic medicine: how can we accelerate the appropriate integration of human genome discoveries into health care and disease prevention? Genet Med. 2007;9:665–674. doi: 10.1097/GIM.0b013e31815699d0. [DOI] [PubMed] [Google Scholar]
- 24.Estabrooks CA, Derksen Z, Winther C, et al. The intellectual structure and substance of the knowledge utilization field: a longitudinal author co-citation analysis, 1945–2004. Implement Sci. 2008;3:49. doi: 10.1186/1748-5908-3-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ogilvie D, Craig P, Griffin S, Macintyre S, Wareham NJ. A translational framework for public health research. BMC Public Health. 2009;9:116. doi: 10.1186/1471-2458-9-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Green LW, Kreuter MW. Health Education Planning: A Diagnostic Approach. 3. Mountain View CA: Mayfield; 1999. [Google Scholar]
- 27.Khoury MJ, Gwinn M, Ioannidis JPA. The emergence of translational epidemiology: from scientific discovery to population health impact. Am J Epidemiol. 2010;172:517–524. doi: 10.1093/aje/kwq211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sorensen JA, Jenkins PL, Bayes B, Clark S, May JJ. Cost-effectiveness of a ROPS socail marketing campaign. J Agric Saf Health. 2010;16:31–40. doi: 10.13031/2013.29247. [DOI] [PubMed] [Google Scholar]
- 29.Wharf Higgins J. Navigating through translational research: a social marketing compass. Health Mark Q. 2011;28:1–15. doi: 10.1080/07359683.2010.495302. [DOI] [PubMed] [Google Scholar]
- 30.Williams VL, Eiseman E, Landrer E, Adamon DM. Demonstrating and Communicating Research Impact: Preparing NIOSH Programs for External Review. Santa Monica: Rand Corporation; 2009. [Google Scholar]
- 31.Straus SE, Graham ID, Mazmanian PE. Knowledge translation: resolving the confusion. J Contin Educ Health Prof. 2006;26:3–4. doi: 10.1002/chp.45. [DOI] [PubMed] [Google Scholar]
- 32.Van Eerd D, Cole D, Keown E . Report on Knowledge Transfer and Exhange Practices: a Systmeatic Review of the Quality and Types of Instruments Used to Assess KTE Implementation and Impact. Toronto: Institute for Work and Health; 2011. [Google Scholar]
- 33.Grimshaw JM, Eccles MD, Lavis JN, Hill SJ, Squires JE. Knowledge translation of research findings. Implement Sci. 2012;7:50. doi: 10.1186/1748-5908-7-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lortie M, Desmarais L, Cheikh F, Laroche É, Faurie I. Le transfert de connaissances au RRSSTQ: bilan et perspectives [Knowledge transfer to the RRSSTQ: evaluation and perspectives.] Relat Ind/Ind Relat. 2013;68:567–589. [Google Scholar]
- 35.Nilsen P. Making sense of implementation theories, models, and frameworks. Implement Sci. 2015;10:53. doi: 10.1186/s13012-015-0242-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schulte PA, Goldenhar LM, Connally LB. Intervention research: science, skills, and strategies. Am J Ind Med. 1996;29:285–288. doi: 10.1002/(SICI)1097-0274(199604)29:4<285::AID-AJIM1>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 37.Durlak JA, DuPre EP. Implementation matters: a review of research on the influence of implementation on program outcomes and factors affecting implementation. Am J Community Psychol. 2008;41:327–350. doi: 10.1007/s10464-008-9165-0. [DOI] [PubMed] [Google Scholar]
- 38.Rogers EM. Diffusion of Innovations. 3. New York: Free Press; 1983. [Google Scholar]
- 39.Dearing JW, Kreuter MW. Designing for diffusion: how can we increase uptake of cancer communication innovations? Patient Educ Couns. 2010;81:S100–S110. doi: 10.1016/j.pec.2010.10.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Booth-Butterfield S, Welbourne J, Williams C, Lewis V. Formative field experiments of a NIOSH alert to reduce the risks to firefighters from structural collapse: applying the cascade framework. Health Commun. 2007;22:79–88. doi: 10.1080/10410230701310331. [DOI] [PubMed] [Google Scholar]
- 41.Real K. Information seeking and workplace safety: a field application of the risk perception attitude framework. J Appl Commun Res. 2008;36:339–359. [Google Scholar]
- 42.Prochaska J, DiClemente C. Transtheoretical therapy: toward a more integrative model of change. Psychother-Theor Res. 1982;19:276–288. [Google Scholar]
- 43.Weiss C. The many meanings of research utilization. Public Admin Rev. 1979;39:426–431. [Google Scholar]
- 44.Dannenberg AL, Bhatia R, Cole BL, et al. Growing the field of health impact assessment in the United States: an agenda for research and practice. Am J Public Health. 2006;96:262–270. doi: 10.2105/AJPH.2005.069880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Saunders SG, Barrington DJ, Sridharan S. Redefining social marketing: beyond behavioral change. J Social Marketing. 2015;5:160–168. [Google Scholar]
- 46.Reid DA, Plank RE. Fundamentals of Business Marketing Research. New York: Haworth Press; 2004. [Google Scholar]
- 47.Verbeek J, Pulliainen M, Kankaanpää E, Taimela S. Transferring results of occupational safety and health cost-effectiveness studies from one country to another—a case study. Scand J Work Environ Health. 2010;36:305–312. doi: 10.5271/sjweh.3070. [DOI] [PubMed] [Google Scholar]
- 48.Asfaw A, Pana-Cryan R, Bashnell T, Sauter S. Musculoskeletal disorders and associated healthcare costs among family members of injured workers. Am J Ind Med. 2015;58:1205–1216. doi: 10.1002/ajim.22500. [DOI] [PubMed] [Google Scholar]
- 49.Dorman P. InFocus Program on SafeWork, International Labour Oranization. Working Paper. Geneva: International Labour Organization; 2000. The Economics of Safety, Health and Well-Being at Work: An Overview. Available at: http://www.ilo.org/safework/info/publications/WCMS_110382/lang-en/index.htm. [Google Scholar]
- 50.Sas K, Suarez A. Priorities for occupational safety and health research in Europe: 2013–2020. Luxembourg: European Agency for Safety and Health at Work; 2013. [Google Scholar]
- 51.Elsler D, Eeckelaert L. Factors influencing the transferability of occupational safety and health economic incentive schemes between different countries. Scand J Work Environ Health. 2010;36:325–331. doi: 10.5271/sjweh.3062. [DOI] [PubMed] [Google Scholar]
- 52.Tompa E, Trevithick S, McLeod C. Systematic review of the prevention incentives of insurance and regulatory mechanisms for occupational health and safety. Scand J Work Environ Health. 2007;33:85–95. doi: 10.5271/sjweh.1111. [DOI] [PubMed] [Google Scholar]
- 53.Wethington E. What is translation research. Cornell University; 2010. [Accessed December 12, 2016]. Available at: http://evidencebasedliving.human.cornell.edu/2010/08/18/what-is-translational-research/ [Google Scholar]
- 54.Coller BS. Translational research: forging a new cultural identity. Mt Sinai J Med. 2008;75:478–487. doi: 10.1002/msj.20064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Noonan RK, Emschoff JG. Translating research to practice: putting “what works” to work. In: DiClemente RJ, Salazar LF, Crosby RA, editors. Health Behavior Theory for Public Health: Principles, Foundations, and Applications. Burlington, MA: Jones and Bartlett Learning; 2013. pp. 309–334. [Google Scholar]
- 56.Molas-Gallart J, D’Este P, Llopis O, Rafols I. Towards an alternative framework for the evaluation of translational research initiatives. Res Evaluat. 2016;25:235–243. [Google Scholar]
- 57.Huberman M. Research utilization: the state of the art. Knowledge Policy. 1994;7:13–33. [Google Scholar]
- 58.Schulte PA, Lentz TJ, Anderson VP, Lamborg AD. Knowledge management in occupational hygiene: the United States example. Ann Occup Hyg. 2004;48:583–594. doi: 10.1093/annhyg/meh061. [DOI] [PubMed] [Google Scholar]
- 59.Kuruvilla S, Mays N, Pleasant A, Walt G. Describing the impact of health research: a Research Impact Framework. BMC Health Serv Res. 2006;6:134. doi: 10.1186/1472-6963-6-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lucas DL, Kincl LD, Bovbjerg VE, Lincoln JM. Application of a translational research model to assess the progress of occupational safety research in the international commercial fishing industry. Saf Sci. 2014;64:71–81. [Google Scholar]
- 61.Karasek RA. Job demands, job decision latitude, and mental strain: implications for job redesign. Admin Sci Quart. 1979;25:285–308. [Google Scholar]
- 62.Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q. 1984;11:1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- 63.Green LW, Ottoson JM, Garcia C, Hiatt RA. Diffusion theory and knowledge dissemination utilization, and integration in public health. Annu Rev Public Health. 2009;30:151–174. doi: 10.1146/annurev.publhealth.031308.100049. [DOI] [PubMed] [Google Scholar]
- 64.Pender NJ. Health Promotion in Nursing. Norwalk, CT: Appleton-Century-Crofts; 1982. [Google Scholar]
- 65.Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol. 2001;52:1–26. doi: 10.1146/annurev.psych.52.1.1. [DOI] [PubMed] [Google Scholar]
- 66.Dobie RA. Medical-Legal Evaluation of Hearing Loss. New York: Van Nostrand Reinhold; 1993. pp. 1–3. [Google Scholar]
- 67.Hager LD. BLS occupational hearing loss report for 2007. CAOHC Update. 2009;21:7–9. Available at: http://www.caohc.org/updatearticles/spring09.pdf. [Google Scholar]
- 68.Berger EH, Franks JR, Behar A, et al. Development of a new standard laboratory protocol for estimating field attenuation of hearing protection devices. Part III. The validity of using subject-fit data. J Acoust Soc Am. 1998;103:665–672. doi: 10.1121/1.423236. [DOI] [PubMed] [Google Scholar]
- 69.Morata TC, Themann CL, Randolph RF, Verbsky BL, Byrne DC, Reeves ER. Working in noise with a hearing loss: perceptions from workers, supervisors, and hearing conservation program managers. Ear Hear. 2005;26:529–545. doi: 10.1097/01.aud.0000188148.97046.b8. [DOI] [PubMed] [Google Scholar]
- 70.Murphy WJ, Davis RR, Byrne DC, Franks JR. Advanced hearing protector study. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; NIOSH EPHB Report No. 312-11a; 2007. [Google Scholar]
- 71.Stephenson CM, Stephenson MR. Hearing loss prevention for carpenters. Part I—using health communication and health promotion models and health to develop training that works. Noise Health. 2011;13:113–121. doi: 10.4103/1463-1741.77207. [DOI] [PubMed] [Google Scholar]
- 72.Bockstael A, De Bruyne L, Vinck B, Botteldooren D. Hearing protection in industry companies policy and workers perception. Int J Ind Ergon. 2013;43:512–517. [Google Scholar]
- 73.Davies H, Marion S, Teschke K. The impact of hearing conservation programs on incidence of noise-induced hearing loss in Canadian workers. Am J Ind Med. 2008;51:923–931. doi: 10.1002/ajim.20634. [DOI] [PubMed] [Google Scholar]
- 74.Wagner GR. The inexcusable persistence of silicosis. Am J Public Health. 2005;85:1346–1347. doi: 10.2105/ajph.85.10.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Cecala AB, O’Brien AD. Here comes the Helmet-CAM: a recent advance in techology can improve how mine operators investigate and assess respirable dust. Rock Prod. 2014;117:26–30. [Google Scholar]
- 76.Haas EJ, Willmer D, Cecala AB. Formative research to reduce mine worker respirable silica dust exposure: a feasibility study to integrate technology into behavioral interventions. Pilot Feasibility Stud. 2016;2:6. doi: 10.1186/s40814-016-0047-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Reed WR, Kwitowski AJ, Helfrich WJ, Cecala AB, Joy GJ. Guidelines for performing a helmet-CAM respirable dust survey and conducting subsequent analysis with the Enhanced Video Analysis of Dust Exposures (EVADE) software. Pittsburgh, PA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 2014. DHHS (NIOSH) Publication No. 2014-133. [Google Scholar]
- 78.Bourbonnais R, Comeau M, Vézina M. Job strain and evolution of mental health among nurses. J Occup Health Psychol. 1999;4:92–107. doi: 10.1037//1076-8998.4.2.95. [DOI] [PubMed] [Google Scholar]
- 79.Bourbonnais R, Brisson C, Vinet A, Vézina M, Lower A. Development and implementation of a participative intervention to improve the psychosocial work environment and mental health in an acute care hospital. Occup Environ Med. 2006;63:326–334. doi: 10.1136/oem.2004.018069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jimmieson NL, Hobman EV, Tucker MK, Bordia P. Change in psychosocial work factors predicts follow-up employee strain: an examination of Australian employees. J Occup Environ Med. 2016;58:1002–1013. doi: 10.1097/JOM.0000000000000827. [DOI] [PubMed] [Google Scholar]
- 81.Ruotsalainen JH, Verbeek JH, Mariné A, Serra C. Preventing occupational stress in healthcare workers. Cochrane Database Syst Rev. 2015;4:D002892. doi: 10.1002/14651858.CD002892.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dollard M, Skinner N, Tuckey MR, Bailey T. National surveillance of psychosocial risk factors in the workplace: an international overview. Work Stress. 2007;21:1–29. [Google Scholar]
- 83.National Institute for Occupational Safety and Health (NIOSH) Commercial fishing vessel shipper dies after being pulled into a deck winch–Alaska. Anchorage, AK: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health, Fatality Assessment and Control Evaluation (FACE) Program, State FACE Reports—Alaska; 1995. Report No. FACE AK-95-23. Available at: https://wwwn.cdc.gov/NIOSH-FACE/Default.cshtml?Category=0000&Category2=ALL&State=AK&Submit=Submit. [Google Scholar]
- 84.Lincoln JM, Lucas DL, McKibbin RW, Woodward CC, Bevan JE. Reducing commercial fishing deck hazards with engineering solutions for winch design. J Safety Res. 2008;39:231–235. doi: 10.1016/j.jsr.2008.02.027. [DOI] [PubMed] [Google Scholar]
- 85.Lincoln JM, Woodward CC, King GW, Case SL, Lucas DL, Teske TD. Preventing fatal winch entanglements in the US southern shrimp fleet: a research to practice approach. J Safety Res. 2017;60:119–123. doi: 10.1016/j.jsr.2016.12.007. [DOI] [PubMed] [Google Scholar]
- 86.Levin JL, Gilmore K, Wickman A, et al. Workplace safety interventions for commercial fishermen of the gulf. J Agromedicine. 2016;21:178–189. doi: 10.1080/1059924X.2016.1143430. [DOI] [PubMed] [Google Scholar]
- 87.Teske TD, Victoroff T. Study in progress. Anchorage, AK: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health (NIOSH); 2017. Increasing adoption of safety technologies in commercial fishing. [Google Scholar]
- 88.Centers for Disease Control and Prevention (CDC) Fatal and nonfatal injuries involving fishing vessel winches–Southern shrimp fleet, United States, 2000–2011. MMWR. 2013;62:157–160. [PMC free article] [PubMed] [Google Scholar]
- 89.Sorensen JA, Brewer DD, Wyckoff L, Horsman M, Scott E, May JJ. Building safety partnerships using social network analysis. Soc Mar Q. 2013;19:67–75. [Google Scholar]
- 90.Zerhouni EA. Medicine. The NIH Roadmap Sci. 2003;302:63–72. doi: 10.1126/science.1091867. [DOI] [PubMed] [Google Scholar]
- 91.Westfall JM, Mold J, Fagnan L. Practice-based research—“Blue highways” on the NIH roadmap. JAMA. 2007;297:403–406. doi: 10.1001/jama.297.4.403. [DOI] [PubMed] [Google Scholar]
- 92.Graham ID, Logan J, Harrison MB, et al. Lost in knowledge translation: time for a map? J Contin Educ Health Prof. 2006;26:13–24. doi: 10.1002/chp.47. [DOI] [PubMed] [Google Scholar]
- 93.Wilson KM, Brady TJ, Lesesne C on behalf of the NCCDPHP Work Group on Translation. An organizing framework for translation in public health: the Knowledge to Action Framework. Prev Chronic Dis. 2011;8:A46. [PMC free article] [PubMed] [Google Scholar]
- 94.Tinc PJ, Ayers P, May JJ, et al. Implementing a national tractor safety program: using “Whole System in a Room” to mobilize partners and implement solutions. J Agromedicine. 2016;21:127–131. doi: 10.1080/1059924X.2016.1142916. [DOI] [PubMed] [Google Scholar]
- 95.Hudson H, Hall J. Value of social media in reaching and engaging employers in Total Worker Health. J Occup Environ Med. 2013;55:S78–S81. doi: 10.1097/JOM.0000000000000035. [DOI] [PubMed] [Google Scholar]
- 96.Weiner BJ. A theory of organizational readiness for change. Implement Sci. 2009;4:67. doi: 10.1186/1748-5908-4-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.McCullagh MC, Banerjee T, Yang J, Bernick J, Duffy S, Redman R. Gender differences in using hearing protection devices among farm operators. Noise Health. 2016;18:368–375. doi: 10.4103/1463-1741.195803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kerner JF. Knowledge translation versus knowledge integration: a “funder’s” perspective. J Contin Educ Health Prof. 2006;26:72–80. doi: 10.1002/chp.53. [DOI] [PubMed] [Google Scholar]
- 99.Welbourne J, Booth-Butterfield S. Using the theory of planned behavior and a stage model of persuasion to evaluate a safety message for firefighters. Health Commun. 2005;18:141–154. doi: 10.1207/s15327027hc1802_3. [DOI] [PubMed] [Google Scholar]
- 100.Maxfield AM, Lewis MJ, Tisdale JA, Lachenmayr S, Lum M. Effects of a preventive message in the organizational context: occupational latex allergy in hospitals. Am J Ind Med. 1999;36:125–127. doi: 10.1002/(sici)1097-0274(199909)36:1+<125::aid-ajim44>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 101.Estabrooks PA, Glasgow RE. Translating effective clinic-based physical activity interventions into practice. Am J of Prev Med. 2006;31:S45–S56. doi: 10.1016/j.amepre.2006.06.019. [DOI] [PubMed] [Google Scholar]
- 102.National Institute for Occupational Safety and Health (NIOSH) A story of impact: measuring how well earplugs work. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 2015. DHHS (NIOSH) Publication No. 2015-181. Available at: http://www.cdc.gov/niosh/docs/2015-181/pdfs/fy15_well-fit_impact_sheet2.pdf. [Google Scholar]
- 103.Murphy WJ, Themann CL, Murata TK. Hearing protector fit testing with off-shore oil-rig inspectors in Louisiana and Texas. Int J of Audiol. 2016;55:688–698. doi: 10.1080/14992027.2016.1204470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Simeonov P, Hsiao H, Powers J. Ladder Safety— Development of the First NIOSH Smartphone app. National Occupational Injury Research Symposium 2015, (NOIRS 2015); May 19–21, 2015; Kingwood, West Virginia. Morgantown, WV: National Institute for Occupational Safety and Health; 2015. p. 108. [Google Scholar]
- 105.Burke LA, Hutchins HM. Training transfer: an integrative literature review. Hum Resour Dev Rev. 2007;6:263–296. [Google Scholar]
- 106.Kristensen TS. Intervention studies in occupational epidemiology. Occup Environ Med. 2005;62:205–210. doi: 10.1136/oem.2004.016097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Jenkins PL, Sorensen JA, Yoder A, et al. Prominent barriers and key motivators to installing ROPS: an analysis of survey responses from Pennsylvania and Vermont. J Agric Saf and Health. 2012;18:103–112. doi: 10.13031/2013.41328. [DOI] [PubMed] [Google Scholar]
- 108.Glasgow RE, Klesges LM, Dzewaltowski DA, Bull SS, Estabrooks P. The future of health behavior change research: what is needed to improve translation of research into health promotion practice? Ann Behav Med. 2004;27:3–12. doi: 10.1207/s15324796abm2701_2. [DOI] [PubMed] [Google Scholar]
- 109.Brownson RC, Kreuter MW, Arrington B, True WR. Translating scientific discoveries into public health action: how can schools of public health move us forward? Public Health Rep. 2006;121:97–103. doi: 10.1177/003335490612100118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Mihalic SF, Fagan AA, Argamaso S. Implementing the LifeSkills Training drug prevention program: factors related to implementation fidelity. Implement Sci. 2008;3:5. doi: 10.1186/1748-5908-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Evanoff B, Wolf L, Aton E, Cano J, Collins J. Reduction in injury rates in nursing personnel through introducation of mechanical lifts in the workplace. Am J Ind Med. 2003;44:451–457. doi: 10.1002/ajim.10294. [DOI] [PubMed] [Google Scholar]
- 112.National Institute for Occupational Safety and Health (NIOSH) Protect yourself at work. Cincinnati, OH: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Institute for Occupational Safety and Health; 2015a. [Accessed December 12, 2016]. Available at: http://www.cdc.gov/niosh/topics/protejase/?s_cid=3ni7d2blogprotenglish. [Google Scholar]
- 113.Flynn MA, Check P, Eggerth DE, Tonda J. Improving occupational safety and health among Mexican immigrant workers: a binational collaboration. Supplement on Applying Social Determinates of Health to Public Health Practice. Public Health Rep. 2013;129:33–38. doi: 10.1177/00333549131286S306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Israel BA, Baker EA, Goldenhar LM, Heaney CA, Schurman SJ. Occupational stress, safety, and health: conceptual framwork and principles for effective prevention interventions. J Occup Health Psychol. 1996;1:261–286. doi: 10.1037//1076-8998.1.3.261. [DOI] [PubMed] [Google Scholar]
- 115.Smith B. Can social marketing be everything to everyone? Soc Mar Q. 2008;14:91–93. [Google Scholar]
- 116.Rivara FP, Thompson DC. Prevention of falls in the construction industry: evidence for program effectiveness. Am J Prev Med. 2000;18:23–26. doi: 10.1016/s0749-3797(00)00137-9. [DOI] [PubMed] [Google Scholar]
- 117.Montaro D, Hoven H, Siegrist J. Effects of organizational-level interventions at work on employees’ health: a systematic review. BWC Public Health. 2014;14:135. doi: 10.1186/1471-2458-14-135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Cochrane. [Accessed May 17, 2017];Cochrane Work. 2017 Available at: http://work.cochrane.org/
- 119.Howard J, Piacentino J, Schulte P, MacMahon K. Using systematic review in occupational safety and health. Am J Ind Med. 2017 doi: 10.1002/ajim.22771. https://doi.org/10.1002/ajim.22771. [DOI] [PubMed]
- 120.Cambon L, Minary L, Ridde V, Alla F. Transferability of interventions in health education: a review. BMC Public Health. 2012;12:497. doi: 10.1186/1471-2458-12-497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Dembe AE. The social consequences of occupational injuries and illnesses. Am J Ind Med. 2001;40:403–417. doi: 10.1002/ajim.1113. [DOI] [PubMed] [Google Scholar]
- 122.Schulte PA. Characterizing the burden of occupational disease and injury. J Occup Environ Med. 2005;47:607–622. doi: 10.1097/01.jom.0000165086.25595.9d. [DOI] [PubMed] [Google Scholar]
- 123.Zaloghnja E, Miller TR, Waehrer G. The impact of occupational injury reduction on the US economy. Am J Ind Med. 2006;49:719–727. doi: 10.1002/ajim.20353. [DOI] [PubMed] [Google Scholar]
- 124.Leigh JP. Economic burden of occupational injury and illness in the United States. Milbank Q. 2011;89:728–772. doi: 10.1111/j.1468-0009.2011.00648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Schulte PA, Pana-Cryan R, Schnorr T, et al. An approach to assess burden of work-related injury, disease, distress. Am J Pub Health. 2017;107:1051–1057. doi: 10.2105/AJPH.2017.303765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Centers for Disease Control and Prevention (CDC) Framework for program evaluation in public health. MMWR. 1999;48:1–40. [Google Scholar]