Abstract
Background: Women with pre-existing diabetes are at high maternal risk for comorbidities and death, particularly when early prenatal care is not received. Low income is a known barrier to early prenatal care. It is unknown whether recent policies to expand access to prenatal care have reduced income disparities. We hypothesized that income disparities would be minimized and that the odds of receipt of first trimester prenatal care among women with pre-existing diabetes would become similar across income strata over time.
Material and Methods: Using the Colorado birth certificate registry from 2007 to 2014, receipt of prenatal care was assessed retrospectively in 2,497 women with pre-existing diabetes. Logistic regression was used to examine the association between high (>$50,000), medium ($25,000–50,000), and low (<$25,000) income strata and receipt of first trimester prenatal care by birth year, adjusted for demographics.
Results: High, medium, and low income represented 29.5%, 19.0%, and 51.5% of the cohort, respectively. Women with high income were more likely to receive first trimester care than women with low income from 2007 [adjusted odds ratio, 95% confidence interval: 2.16 (1.18, 3.96)] through 2013 [1.66 (1.01, 2.73)], but significant differences were no longer observed in 2014 [1.59 (0.89, 2.84)]. The likelihood of receiving first trimester prenatal care was not significantly different between medium- and low-income strata from 2007 [1.07 (0.66, 1.74)] through 2014 [0.77 (0.48, 1.23)].
Conclusions: From 2007 to 2013, women in Colorado with diabetes were more likely to receive early prenatal care if they were in the highest income stratum than in the lowest stratum. In 2014, receipt of first trimester care became equitable across all income strata. Future work should examine national patterns of income with receipt of prenatal care and outcomes among women with pre-existing diabetes.
Keywords: : pregnancy, socioeconomic status, policy
Introduction
First trimester care is critical in preventing comorbidities associated with pregnancy.1–3 This is especially true among women with pre-existing diabetes who have 11-fold higher risk of intrauterine fetal demise4 and nearly twofold higher risk of pre-eclampsia and death with receipt of late inadequate prenatal care than early or first trimester prenatal care.5,6 Pregnant women with pre-existing diabetes represent 0.4%–1.8% of annual childbirths in the United States.7,8 The majority of this group have type 2 diabetes mellitus,7,9 which is expected to continue rising in prevalence following national trends.10 In prior works, pre-existing diabetes has been associated with lack of early prenatal care.11,12 Meanwhile, there is sparse contemporary data on trends in receipt of early prenatal care among women with pre-existing diabetes; however, there is increasing data regarding barriers to receipt of early prenatal care.6,11
Low income is one of the most cited barriers to obtaining early prenatal care, particularly among women with pre-existing diabetes.13,14 This may be related to variable eligibility for Medicaid across the United States and increased health insurance premiums for childbirth.14 Efforts to improve access to early prenatal care have included state- and national-level policy changes. Specific initiatives in Colorado include prohibition of denial of prenatal care to privately insured women in Colorado in 2010, Colorado Medicaid Expansion in 2013, and the national Affordable Care Act, which prohibited insurance rate increases for pregnancy and provided tax credits for insured women.14–20
Following such policy changes, it was unknown whether income status remains a factor in obtaining early prenatal care. The state of Colorado has a robust data set of birth certificate information that makes it ideal to study trends in receipt of early prenatal care in women with pre-existing diabetes across income strata. We hypothesized that the odds of receipt of first trimester prenatal care among women with pre-existing diabetes across high (>$50,000), medium ($25,000–50,000), and low (<$25,000) annual household incomes would become similar over time.
Methods
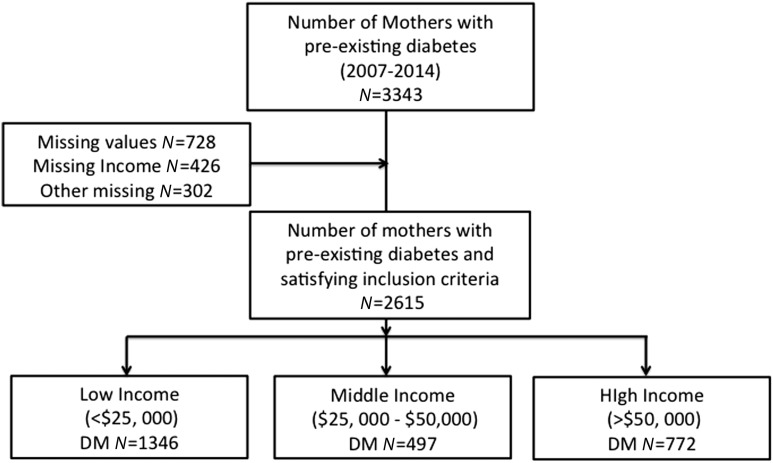
The Colorado birth certificate registry was retrospectively assessed for mothers with pre-existing diabetes (n = 3,343) from 2007 to 2014 (Fig. 1). The Colorado birth certificate registry is maintained by the Colorado Department of Public Health and Environment and uses coding from the Colorado Standard Certificate of Live Births, which include demographics of the mother, pre-existing comorbidities (i.e., yes/no for diabetes prepregnancy), prenatal care, and delivery data. The initial birth certificate was completed by patient self-report and reviewed by hospital administration. Women with missing values for annual household income, race/ethnicity, education, body mass index, maternal age, marital status, month of prenatal care initiation, parity, and Graduated Prenatal Care Utilization Index (GINDEX) were excluded from the study population (n = 726). The final study population included 2,615 women.
FIG. 1.
Flowchart of mothers with pre-existing diabetes included in the Retrospective Cohort Study from Colorado birth certificate data during 2007–2014.
Outcome
The outcome of interest for this study was receipt of the first prenatal care visit during the first trimester.
Predictor variable
The primary explanatory variable was annual household income ascertained from the Colorado birth certificate registry and categorized as high (>$50,000), medium ($25,000–50,000), and low (<$25,000). Income categories were chosen based on known U.S. median household income, and stratification is typical of socioeconomic status literature.21–23
Statistical analysis
We compared baseline characteristics of mothers with pre-existing diabetes by annual household income categories of high, medium, and low. Bivariate analyses were performed on potential covariates associated with receipt of early prenatal care, including race/ethnicity, maternal age, maternal education, insurance, marital status, prepregnancy body mass index, gestational hypertension, prepregnancy hypertension, birth year, and parity.3,5,6,24,25 Categorical variables were compared using chi-squared analyses, and continuous variables were compared using analysis of variance.
Logistic regression models were used to determine the association between income and receipt of first trimester prenatal care. Covariates with significance (p < 0.1) in bivariate analyses were included in the multivariable analyses. Parsimonious models were explored by removal of covariates one at a time using the Akaike Information Criterion. Covariates that were identified as confounders or effect modifiers were retained in the model. The adjusted model included the following covariates: race/ethnicity, insurance, parity, marital status, and maternal age. To explore whether birth year modified the effect of income, an income × birth year interaction term was included. The odds ratio of receipt of first trimester care was obtained annually from 2007 through 2014 in women with high versus low income and in women with medium versus low income. Statistical analyses were performed using SAS 9.4 (Cary, NC), and the significance level was set at 0.05 for all tests.
Results
Differences in demographics were found across annual household income strata. Women with low annual household income were more likely to be of Hispanic/non-Caucasian ethnicity, have less than a high school education, and have Medicaid insurance as the primary source of payment (Table 1).
Table 1.
Demographics of Women with Pre-Existing Diabetes Stratified by Annual Household Income from 2007 to 2014
| <$25,000 n = 1346 (51.5%) | $25–50,000 n = 497 (19.0%) | >$50,000 n = 772 (29.5%) | p-value | |
|---|---|---|---|---|
| Maternal education | <0.0001 | |||
| <High school | 40.0% | 14.7% | 1.7% | |
| High school and/or GED | 27.5% | 23.9% | 9.1% | |
| College and/or technical school | 29.6% | 46.5% | 31.9% | |
| College graduate | 2.9% | 14.9% | 57.4% | |
| Race/ethnicity | <0.0001 | |||
| Non-Hispanic/Latino Caucasian | 27.6% | 52.1% | 76.8% | |
| Hispanic/Latino non-Caucasian | 53.2% | 32.0% | 11.7% | |
| Other | 19.2% | 15.9% | 11.5% | |
| Insurance | <0.0001 | |||
| Medicaid | 79.1% | 32.4% | 2.3% | |
| Private insurance | 12.4% | 53.3% | 92.5% | |
| Self-pay | 2.8% | 1.4% | 0.7% | |
| Other | 5.7% | 12.9% | 9.5% | |
| Marital status | <0.0001 | |||
| Never married | 34.6% | 12.5% | 4.4% | |
| Married | 59.6% | 82.9% | 95.0% | |
| Divorced/separated/widowed | 5.8% | 4.6% | 0.7% | |
| Maternal age* | 29.1 ± 6.3 | 30.4 ± 5.6 | 32.0 ± 4.9 | 0.0002 |
| ≥35 years | 21.0% | 25.4% | 29.0% | |
| Gestational age* | 37.3 ± 2.7 | 37.4 ± 2.2 | 37.4 ± 2.4 | 0.63 |
| Parity | 0.02 | |||
| 0 births | 29.9% | 33.4% | 42.9% | |
| Prepregnancy BMI* | 31.7 ± 7.9 | 31.6 ± 7.5 | 29.4 ± 7.4 | 0.12 |
| Pre-existing hypertension | 11.4% | 11.1% | 7.5% | 0.43 |
| Gestational hypertension | 9.0% | 10.9% | 13.3% | 0.90 |
denotes mean with standard deviation.
BMI, body mass index; GED, general education diploma.
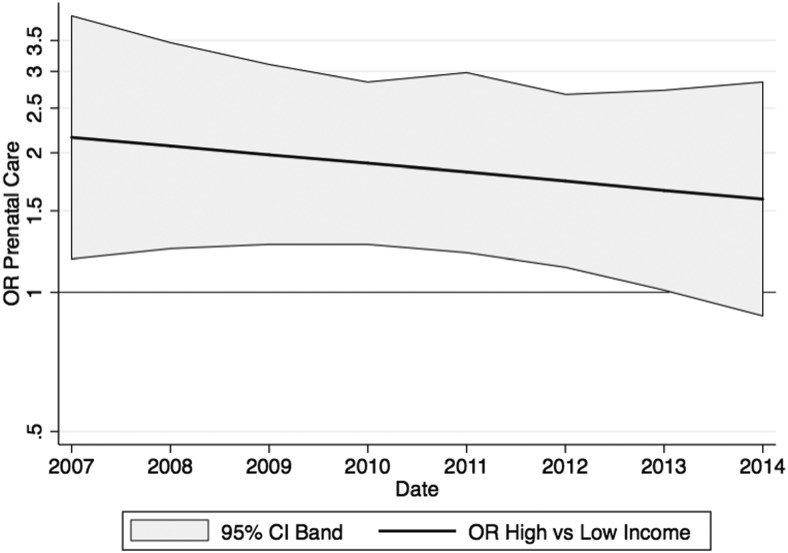
The prevalence of first trimester prenatal care was the highest in women with high annual household income (high income ranges: 87.9%–95.4%; medium income: 70.3%–87.5%; low income: 66.7%–81.9%, Table 2). The unadjusted odds of receiving first trimester prenatal care were higher in women with high income than in women with low income throughout the study (Table 3). After adjusting for race/ethnicity, insurance, parity, marital status, and maternal age, the odds of receiving first trimester prenatal care were higher in women with high income than in women with low income for each year from 2007 to 2013 (Table 3 and Fig. 2) until 2014 when the likelihood of receiving care was similar in both groups [1.59 (0.89, 2.84) for 2014].
Table 2.
Prevalence of Receipt of Early Prenatal Care By Income Strata
| Early prenatal care | |||
|---|---|---|---|
| Year | Low | Middle | High |
| 2007 | 99/134 (73.9%) | 65/78 (83.3%) | 65/73 (89.0%) |
| 2008 | 80/120 (66.7%) | 40/52 (76.9%) | 85/95 (89.5%) |
| 2009 | 127/185 (68.7%) | 51/67 (76.1%) | 82/86 (95.4%) |
| 2010 | 108/153 (70.6%) | 39/49 (79.6%) | 97/105 (92.4%) |
| 2011 | 144/188 (76.6%) | 53/69 (76.8%) | 80/86 (93.0%) |
| 2012 | 153/191 (80.1%) | 44/52 (84.6%) | 102/116 (87.9%) |
| 2013 | 136/193 (70.5%) | 52/74 (70.3%) | 93/100 (93.0%) |
| 2014 | 149/182 (81.9%) | 49/56 (87.5%) | 103/111 (92.8%) |
| Total | 996/1346 (74.0%) | 393/497 (79.1%) | 707/772 (91.6%) |
Table 3.
Odds Ratio of Receipt of Early Prenatal Care Based on Income
| High vs. low income | Medium vs. low income | |||||||
|---|---|---|---|---|---|---|---|---|
| Year | adjOR | 95% CI | unadjOR | 95% CI | adjOR | 95% CI | unadjOR | 95% CI |
| 2007 | 2.16 | (1.18, 3.96) | 4.50 | (2.64, 7.65) | 1.07 | (0.66, 1.74) | 1.77 | (1.13, 2.77) |
| 2008 | 2.07 | (1.24, 3.47) | 4.30 | (2.80, 6.62) | 1.02 | (0.68, 1.53) | 1.63 | (1.14, 2.35) |
| 2009 | 1.98 | (1.27, 3.10) | 4.12 | (2.91, 5.82) | 0.97 | (0.70, 1.36) | 1.51 | (1.13, 2.03) |
| 2010 | 1.90 | (1.27, 2.84) | 3.94 | (2.94, 5.28) | 0.93 | (0.69, 1.25) | 1.40 | (1.09, 1.80) |
| 2011 | 1.82 | (1.22, 2.98) | 3.77 | (2.83, 5.02) | 0.89 | (0.66, 1.18) | 1.30 | (1.00, 1.67) |
| 2012 | 1.74 | (1.13, 2.68) | 3.61 | (2.59, 5.03) | 0.84 | (0.61, 1.17) | 1.20 | (0.89, 1.61) |
| 2013 | 1.66 | (1.01, 2.73) | 3.46 | (2.29, 5.21) | 0.81 | (0.55, 1.19) | 1.11 | (0.77, 1.50) |
| 2014 | 1.59 | (0.89, 2.84) | 3.31 | (1.99, 5.50) | 0.77 | (0.48, 1.23) | 1.03 | (0.65, 1.61) |
Models were adjusted for race/ethnicity, insurance, parity, marital status, maternal age.
Adj, adjusted; CI, confidence interval; unadj, unadjusted.
FIG. 2.
Trends in receipt of first trimester prenatal care among women with high versus low annual household income. The solid black line represents the OR of receipt of first trimester prenatal care for women with high versus low annual household income. The gray shade represents the 95% CI band. CI, confidence interval; OR, odds ratio.
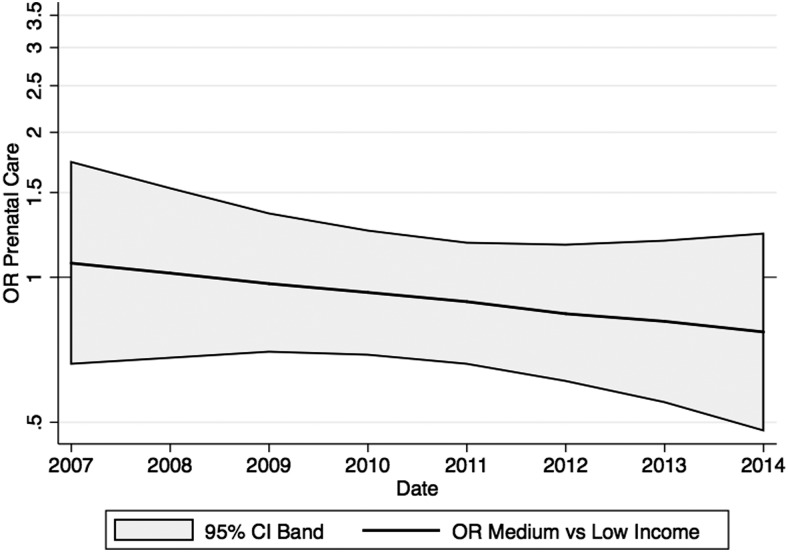
The unadjusted odds of receiving first trimester prenatal care were higher in medium income women than in low income women until 2012 (Table 3). The adjusted odds of receiving first trimester prenatal care were similar among women with medium and low annual household income from 2007 to 2014 (Table 3 and Fig. 3).
FIG. 3.
Trends in receipt of first trimester prenatal care among women with medium versus low annual household income. The solid black line represents the OR of receipt of first trimester prenatal care for women with medium versus low annual household income. The gray shade represents the 95% CI band.
Discussion
During years 2007–2013, low income was associated with reduced likelihood of receipt of early prenatal care among women giving birth in Colorado with pre-existing diabetes. However, in 2014, income differences were no longer present in the likelihood of receipt of early prenatal care in women with pre-existing diabetes. The Colorado birth certificate registry provided the ideal population to study income disparities in women with pre-existing diabetes, given the diverse self-reported income backgrounds and rising prevalence of diabetes.26,27
This is one of the first studies to investigate the likelihood of receipt of early prenatal care among a contemporary cohort of women with pre-existing diabetes. Our results are consistent with National Center for Health Statistics data showing gradual increase in receipt of first trimester prenatal care among all-comer women in Colorado from 69% in 2007 to 73% in 2013.3,24,28–30 Prior studies have demonstrated that access to prenatal care is not equal across socioeconomic status nationally.13,14 In multiple populations, low income and inadequate insurance were described as key barriers to prenatal care in women with pre-existing diabetes living in the United States.11,13 More than 40% of women surveyed through the Colorado Pregnancy Risk Assessment Monitoring System listed low income as the key reason for not obtaining early prenatal care.14 This may contribute to the disproportionately higher rates of morbidity and mortality among women from lower socioeconomic backgrounds.6,14,17,21,26 Heightened public health efforts have sought to assess factors associated with obtaining early prenatal care.
Improving access to prenatal care is of special importance in women with pre-existing diabetes.5,13,31 The incidence of diabetes mellitus in women 20 years of age and older is on the rise at epidemic proportions in the United States.10 Women of childbearing age are at increasingly higher risk for ensuing complications with pregnancy due to comorbidities such as diabetes and increased maternal age.5,32,33 Early prenatal care can reduce poor outcomes in diabetic women.6
Access to prenatal care is a priority across socioeconomic status. Both public and private insurance carriers offered poor prenatal care coverage in Colorado at the start of this study.14 Colorado ranked in the lowest quarter of the nation for providing Medicaid coverage; a greater proportion of women of child-bearing age lacked insurance in Colorado than in the rest of the United States, and private insurers did not provide universal coverage for prenatal care and delivery.14,34 Policy changes at the state and national level are being associated with improved access to care.14 In 2008, CenteringPregnancy, a group clinic visit method, was being used in Colorado at three locations and was expanded further during this study.35 Reports in other cities have demonstrated that this program is effective in increasing access to early prenatal care for low-income populations.36 In 2010, Colorado legislature mandated that private insurers must no longer deny prenatal care to any enrollees.14 Perhaps most relevant to this study, Colorado Medicaid eligibility was expanded to pregnant women from a federal poverty level of 133% to 185% in 2013.19 This corresponds to a woman in a two-person household now having access to Medicaid if her annual household income was >$21,320 but <$29,640.37 In 2014, the national Patient Protection and Affordable Care Act further expanded prenatal care by providing tax credits to reduce insurance premiums for women of child-bearing age and prohibited insurance rate hikes for pregnancy care.14 In sum, the gaps in socioeconomic access to prenatal care are being reduced.14 Changes in insurance likely mediate the increased access to prenatal care across income strata.
Limitations
First, there was an inability to distinguish between type 1 and type 2 diabetes mellitus. Patients with type 1 and type 2 diabetes mellitus have different demographics38 and thus different access to care.39 However, the majority of pre-existing diabetes during pregnancy is secondary to type 2 diabetes mellitus.7,9 Nevertheless, the Centers for Disease Control and Prevention has stressed the importance of prenatal care in pre-existing diabetes irrespective of type.40 Second, socioeconomic status was measured by annual household income in this study. Although the research community disagrees about the appropriate elements to measure socioeconomic status,21 annual household income has been validated as an appropriate derivative from census data.41 This study used self-report of annual household income, which is a better indicator than census report. Although this study was not able to adjust for the number of people living in a household, the annual household income remains a reputable way of describing socioeconomic status. Third, considerations for alternative measures of adequate prenatal care were considered, such as GINDEX, but the accuracy and completion of data collection were in question.42,43 Prevalence of adequate care by GINDEX did not correlate with known national rates.3 Fourth, the results of this study were less generalizable to the entire United States. The education of people living within the state of Colorado is the highest in the country,44 but the annual household income is closer to the national median.22 Finally, the completion and accuracy of the birth certificate data including pre-existing diabetes may vary by facility and year. However, the credibility of this study is increased since state birth certificate registries have been validated for research purposes.45
Conclusions
Early prenatal care is paramount in women with pre-existing diabetes. In the past, low socioeconomic status has been associated with underutilization of prenatal care. The Colorado birth certificate registry has provided the ideal setting to determine whether income remains associated with receipt of prenatal care in women with pre-existing diabetes over time. We found that the receipt of prenatal care was equitable across income strata starting in 2014. This is likely secondary to national and state-wide policy changes, which expanded prenatal care in 2013 and 2014. This study should be performed on a national scale to determine whether access to prenatal care is changing and whether outcomes are improving in women with pre-existing diabetes.
Acknowledgments
Dr. Breathett received support from a T32 training grant (5T32 HL116276-02) and Loan Repayment Award (L60 MD010857) from the National Institute of Health, American Heart Association Strategically Focused Research Network for Heart Failure (16SFRN29640000), and the University of Colorado, Department of Medicine, Health Services Research Development Grant Award.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Kitzmiller JL, Block JM, Brown FM, Catalano PM, Conway DL, Coustan DR, et al. Managing preexisting diabetes for pregnancy. Diabetes Care 2008;31:1060–1079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Carter EB, Tuuli MG, Odibo AO, Macones GA, Cahill AG. Prenatal visit utilization and outcomes in pregnant women with type II and gestational diabetes. J Perinatol 2017;37:122–126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prenatal Care Utilization, Child Health USA 2013 [Internet]. Available from: http://mchb.hrsa.gov/chusa13/health-services-utilization/p/prenatal-care-utilization.html Accessed May18, 2016
- 4.Allen AJ, Snowden JM, Lau B, Cheng Y, Caughey AB. Type-2 diabetes mellitus: Does prenatal care affect outcomes? suggested running head: Treatment of T2DM and perinatal outcomes. J Matern Fetal Neonatal Med 2017;15:1–15 [DOI] [PubMed] [Google Scholar]
- 5.Feig DS, Razzaq A, Sykora K, Hux JE, Anderson GM. Trends in deliveries, prenatal care, and obstetrical complications in women with pregestational diabetes: A population-based study in Ontario, Canada, 1996–2001. Diabetes Care 2006;29:232–235 [DOI] [PubMed] [Google Scholar]
- 6.Chen X-K, Wen SW, Yang Q, Walker MC. Adequacy of prenatal care and neonatal mortality in infants born to mothers with and without antenatal high-risk conditions. Aust N Z J Obstet Gynaecol 2007;47:122–127 [DOI] [PubMed] [Google Scholar]
- 7.Jovanovič L, Liang Y, Weng W, Hamilton M, Chen L, Wintfeld N. Trends in the incidence of diabetes, its clinical sequelae, and associated costs in pregnancy. Diabetes Metab Res Rev 2015;31:707–716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lawrence JM, Contreras R, Chen W, Sacks DA. Trends in the prevalence of preexisting diabetes and gestational diabetes mellitus among a racially/ethnically diverse population of pregnant women, 1999–2005. Diabetes Care 2008;31:899–904 [DOI] [PubMed] [Google Scholar]
- 9.Albrecht SS, Kuklina EV, Bansil P, Jamieson DJ, Whiteman MK, Kourtis AP, et al. Diabetes Trends Among Delivery Hospitalizations in the U.S., 1994–2004. Diabetes Care 2010;33:768–773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benjamin EJ, Blaha MJ, Chiuve S, Cushman M, Das S, Deo R, et al. Heart disease and stroke statistics—2017 update a report from the American Heart Association. Circulation 2017;135:e146–e603 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Robinson M, Wesley M, Bish C, Mohamed A. Barriers to prenatal care for women with pre-existing diabetes in Mississippi [Internet]. American Public Health Association Meeting; 2012. October Available from: https://apha.confex.com/apha/140am/webprogram/Paper262158.html Accessed March25, 2016
- 12.Prenatal Care and Pregnancies Complicated by Diabetes—U.S. Reporting Areas, 1989 [Internet]. Available from: www.cdc.gov/mmwr/preview/mmwrhtml/00019601.htm Accessed February8, 2017 [PubMed]
- 13.Collier SA, Mulholland C, Williams J, Mersereau P, Turay K, Prue C. A qualitative study of perceived barriers to management of diabetes among women with a history of diabetes during pregnancy. J Womens Health 2002 2011;20:1333–1339 [DOI] [PubMed] [Google Scholar]
- 14.Ready, Set, Go! Investing in Infants and Toddlers [Internet]. Colorado Children's Campaign; 2013. August Available from: www.coloradokids.org/wp-content/uploads/2014/12/Ready-Prenatal-Health-and-Care.pdf Accessed May17, 2016
- 15.The WIC Program Background, Trends, and Issues [Internet]. US Department of Agriculture, Economic Research Service; Report No.: 27. Available from: www.ers.usda.gov/media/327957/fanrr27_1_.pdf Accessed May17, 2016
- 16.Rosenbach M, O'Neil S, Cook B, Trebino L, Walker DK. Characteristics, access, utilization, satisfaction, and outcomes of healthy start participants in eight sites. Matern Child Health J 2010;14:666–679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saving Our Nation's Babies The Impact of the Federal Healthy Start Iniative [Internet]. National Healthy Start Association. Department of Health and Human Services; 2011. Available from: www.nationalhealthystart.org/site/assets/docs/NHSA_SavingBabiesPub_2ndED.pdf Accessed February28, 2016
- 18.Aizer A, Grogger J. Parental Medicaid Expansions and Health Insurance Coverage [Internet]. National Bureau of Economic Research; 2003. August Report No.: 9907. Available from: www.nber.org/papers/w9907.pdf Accessed February28, 2016
- 19.Martinez C, Guadarrama M. Child Health Plan Plus and Medicaid Program Changes [Internet]. Colorado Department of Health Care Policy & Financing; 2013. January Available from: www.colorado.gov/pacific/sites/default/files/2013%20Director%20letters%20CHP%2B%20and%20Medicaid%20Changes%20effective%20January%201,%202013.pdf Accessed February28, 2016
- 20.McPherson ME, Gloor PA, Smith LA. Using collaborative improvement and innovation networks to tackle complex population health problems. JAMA Pediatr 2015;169:709–710 [DOI] [PubMed] [Google Scholar]
- 21.Braveman P, Cubbin C, Marchi K, Egerter S, Chavez G. Measuring socioeconomic status/position in studies of racial/ethnic disparities: Maternal and infant health. Public Health Rep 2001;116:449–463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.US Census BureauDID. Income [Internet]. Available from: www.census.gov/hhes/www/income/data/statemedian Accessed March25, 2016
- 23.Real Median Household Incomes for all Racial Groups Remain Well Below Their 2007 Levels [Internet]. Economic Policy Institute. Available from: www.epi.org/blog/real-median-household-incomes-racial-groups Accessed June7, 2015
- 24.Prenatal - First Trimester Care Access [Internet]. Available from: www.hrsa.gov/quality/toolbox/measures/prenatalfirsttrimester Accessed March25, 2016
- 25.Alexander GR, Kogan MD, Nabukera S. Racial differences in prenatal care use in the United States: Are disparities decreasing? Am J Public Health 2002;92:1970–1975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carmen DeNava-Walt, Proctor B. Income and Poverty in the United States: 2014 [Internet]. United States Census Bureau; 2015. September (Current Population Reports). Report No.: P60-252. Available from: wwwcensus.gov/content/dam/Census/library/publications/2015/demo/p60-252.pdf Accessed April18, 2016
- 27.Colorado State Obesity Data, Rates and Trends: The State of Obesity [Internet]. Available from: http://stateofobesity.org/states/co Accessed May17, 2016
- 28.Early prenatal care Colorado | PeriStats | March Of Dimes [Internet]. Available from: www.marchofdimes.org/Peristats/ViewSubtopic.aspx?reg=08&top=5&stop=21&lev=1&slev=4&obj=1 Accessed June17, 2016
- 29.Colorado Health Institute [Internet]. Available from: http://coloradohealthinstitute.org/data-repository/category/colorado-health-report-card/2016 Accessed June17, 2016
- 30.Late or No Prenatal Care [Internet]. Child Trends. 2015. Available from: www.childtrends.org/?indicators=late-or-no-prenatal-care Accessed June17, 2016
- 31.Pregnancy Complications and Perinatal Outcomes Among Women With Diabetes—North Carolina, 1989–1990 [Internet]. Available from: www.cdc.gov/mmwr/preview/mmwrhtml/00022136.htm Accessed March25, 2016 [PubMed]
- 32.Pregnancy Mortality Surveillance System [Internet]. Centers for Disease Control and Prevention; 2016. January Available from: www.cdc.gov/reproductivehealth/maternalinfanthealth/pmss.html Accessed June17, 2016
- 33.Wenger NK. Recognizing pregnancy-associated cardiovascular risk factors. Am J Cardiol 2014;113:406–409 [DOI] [PubMed] [Google Scholar]
- 34.Arellano AR de, Wolfe S. Unsettling Scores, A Ranking of State Medicaid Programs [Internet]. 2007. Available from: www.citizen.org/hrg1807#national_results Accessed May4, 2016
- 35.The 2011 Colorado Health Report Card–Healthy Beginnings—Prenatal Care [Internet]. Available from: www.coloradohealth.org/ReportCard/2011/subdefault.aspx?id=5467 Accessed May17, 2016
- 36.Klima C, Norr K, Vonderheid S, Handler A. Introduction of CenteringPregnancy in a public health clinic. J Midwifery Womens Health 2009;54:27–34 [DOI] [PubMed] [Google Scholar]
- 37.Poverty Guidelines [Internet]. ASPE. 2015. [cited 2016. May 17]. Available from: https://aspe.hhs.gov/poverty-guidelines Accessed May17, 2016
- 38.2014 Statistics Report | Data & Statistics | Diabetes | CDC [Internet]. Available from: www.cdc.gov/diabetes/data/statistics/2014statisticsreport.html Accessed March25, 2016
- 39.Brown AF, Ettner SL, Piette J, Weinberger M, Gregg E, Shapiro MF, et al. Socioeconomic position and health among persons with diabetes mellitus: A conceptual framework and review of the literature. Epidemiol Rev 2004;26:63–77 [DOI] [PubMed] [Google Scholar]
- 40.CDC - Type 1 or Type 2 Diabetes and Pregnancy [Internet]. Available from: www.cdc.gov/pregnancy/diabetes-types.html Accessed March25, 2016
- 41.Foraker RE, Patel MD, Whitsel EA, Suchindran CM, Heiss G, Rose KM. Neighborhood Socioeconomic Disparities and 1-year Case Fatality after Incident Myocardial Infarction: The Atherosclerosis Risk in Communities (ARIC) Community Surveillance (1992–2002). Am Heart J 2013;165:102–107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Concept: Revised-Graduated Prenatal Care Utilization Index (R-GINDEX) [Internet]. Available from: http://mchp-appserv.cpe.umanitoba.ca/viewConcept.php?printer=Y&conceptID=1360 Accessed May17, 2016
- 43.Alexander GR, Kotelchuck M. Quantifying the adequacy of prenatal care: A comparison of indices. Public Health Rep 1996;111:408–419 [PMC free article] [PubMed] [Google Scholar]
- 44.Population estimates, July 1, 2015, (V2015) [Internet]. Available from: www.census.gov/quickfacts/table/PST045215/08 Accessed March9, 2016
- 45.Andrade SE, Scott PE, Davis RL, Li D-K, Getahun D, Cheetham TC, et al. Validity of health plan and birth certificate data for pregnancy research. Pharmacoepidemiol Drug Saf 2013;22:7–15 [DOI] [PMC free article] [PubMed] [Google Scholar]