Introduction
Dyshidrosiform bullous pemphigoid (DP) is an unusual localized variant of bullous pemphigoid (BP), first described by Levine et al1 in 1979. It presents with a persistent and recurrent vesicobullous eruption, sometimes hemorrhagic, localized to the soles and/or palms. Since the clinical manifestations of DP are similar to those of pompholyx or bullous tinea pedis, which are more common and benign dermatologic diseases, a proper diagnosis could be delayed. We report the case of an 82-year-old man affected by DP who was treated for months for pompholyx and bullous tinea pedis with dermatophytid reaction.
Case report
An 82-year-old man presented with a few-months’ history of recurrent itchy vesicobullous eruption localized to the soles and the palms. First diagnosed in another center with pompholyx, the patient was treated with topical betamethasone with temporary benefit, but the symptoms soon recurred. Direct microscopic examination of a potassium hydroxide preparation and the fungal culture of skin scrapings yielded positive results, and a diagnosis of bullous tinea pedis with dermatophytid reaction was made. Although 1-month therapy with daily itraconazole 100 mg, potassium permanganate solution 1 in 10,000 soaks, chlorquinaldol 2% in petrolatum, and nitrate econazole 1% cream was started, only a slight improvement was noted. When the patient presented to our clinic, multiple tense vesiculobullae (some hemorrhagic) on the nonerythematous skin of the palms, the soles, and lateral surfaces of both hands and feet were present (Fig 1). No mucosal or other cutaneous involvement was observed, and the Nikolsky sign was negative. Mycologic examination with potassium hydroxide preparation and a fungal culture from skin scrapings found no trace of fungal elements. The patient denied consistent exposure to allergens or products that might induce persistent contact dermatitis. A skin biopsy from the lateral foot skin was performed. The histopathologic finding revealed focal spongiosis tending to form focally subepidermal clefts and a predominantly eosinophilic dermal infiltration, which is consistent with early BP lesions (Fig 2). Direct immunofluorescence of the perilesional skin disclosed continuous linear deposits of IgG along the dermoepidermal junction and blister roof staining within separate portions of biopsy (Fig 3). An enzyme-linked immunosorbent assay found circulating antibodies to BP180 (71.0 U/mL; normal values, <9 U/mL) and BP230 (85.2 U/mL; normal values, <9 U/mL). A diagnosis of DP was made. The patient was treated with topical betamethasone and prednisone 50 mg/day, which resulted in a marked clinical improvement with no new blister formation. The systemic steroid dose was then gradually tapered. Eight months later, the patient remains in good condition.
Fig 1.
Multiple tense vesiculobullae of dyshidrosiform pemphigoid, some of them hemorrhagic, on nonerythematous skin on the soles and the lateral surfaces of feet.
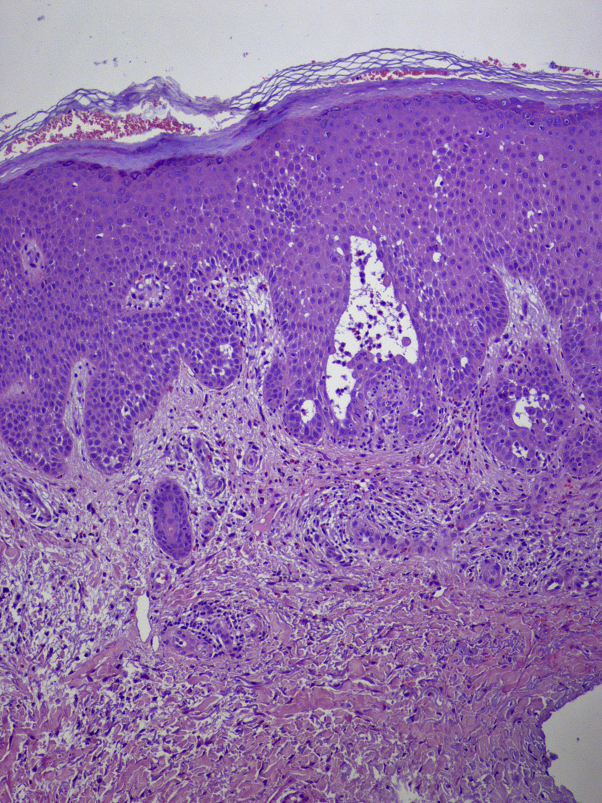
Fig 2.
Histopathologic findings show focal spongiosis tending to form focally subepidermal clefts and a predominantly eosinophilic dermal infiltration, consistent with bullous pemphigoid. (Hematoxylin-eosin stain; original magnification: ×20.) A high-resolution version of this slide for use with the Virtual Microscope is available as eSlide: VM04193.
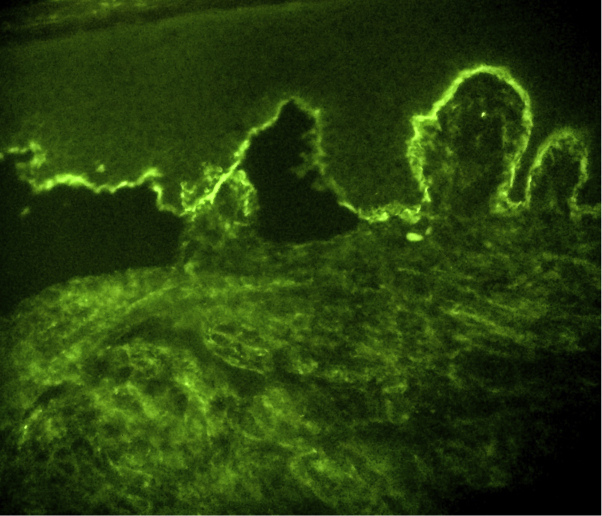
Fig 3.
Direct immunofluorescence of the perilesional skin shows continuous linear deposits of IgG along the dermoepidermal junction, consistent with bullous pemphigoid. Note the staining pattern of the blister roof within separate portions of biopsy, further supporting BP diagnosis.
Discussion
DP is a rare variant of localized BP, which Levine et al1 first reported in 1979. It presents with a persistent and recurrent vesicobullous eruption localized to the soles and/or palms, often misleading clinicians to diagnose pompholyx or bullous tinea pedis.2 When present, the hemorrhagic character of the bullae could be an important clue for dermatologists,3 but only a skin biopsy revealing the typical pathologic hallmarks of BP,2, 4 direct immunofluorescence, and the assays for the evaluation of circulating antibodies to BP180 and BP230 allowed a correct diagnosis. To the best of our knowledge, only 31 cases of DP have been reported in the literature so far. However, since the diagnosis of DP may be misleading, the disease prevalence could have been underestimated. In a clinical report by Chang et al,5 3 of 86 patients with BP could have a dyshidrosiform type. Most of the cases of DP are described in elderly patients, but Caldarola et al6 and Lupi et al7 reported 2 cases in young adults. DP's pathologic mechanism is currently unknow. Levine et al1 proposed that an inflammatory process, such as tinea pedis, could uncover antigens usually protected from antibody recognition. Interestingly, our patient reported traces of a fungal infection only in the first mycologic examination. The first result may have been a false-positive, or the oral itraconazole treatment may have led to the infection resolution. According to the literature, mycologic research has been performed only in 2 other reported cases, both with negative results.6, 7 Therefore, further studies are needed to determine the disease's exact pathogenesis. Initially reported as a localized variant of BP, it has been shown that DP may precede or occur concomitantly with generalized lesions of classic BP, ranging from urticarial plaques to bullae and erosions.3, 7, 8 Consequently, a follow-up examination is mandatory. DP has generally proved very responsive to topical steroids, at least temporarily. This fact may also have contributed to underdiagnosis, as cases that respond to topical steroids alone are unlikely to undergo a further workup with biopsy and immunofluorescence studies. Although low-dose oral steroid therapy has been used primarily for systemic treatment, other therapies include dapsone, cyclophosphamide, azathioprine, methotrexate, and erythromycin. The condition has subsided in all cases reported in the literature as well as in our patient.
In conclusion, clinicians should be aware that an unusually persistent or recurrent pompholyx-like eruption on the palms and/or the soles, especially if hemorrhagic and particularly in elderly patients, may conceal BP.
Footnotes
Funding sources: None.
Conflicts of interest: None declared.
References
- 1.Levine N., Freilich A., Barland P. Localized pemphigoid simulating dyshidrosiform dermatitis. Arch Dermatol. 1979;115(3):320–321. [PubMed] [Google Scholar]
- 2.Rongioletti F., Parodi A., Rebora A. Dyshidrosiform pemphigoid. Report of an additional case. Dermatologica. 1985;170(2):84–85. [PubMed] [Google Scholar]
- 3.Descamps V., Flageul B., Vignon-Pennamen D. Dyshidrosiform pemphigoid: report of three cases. J Am Acad Dermatol. 1992;26(4):651–652. doi: 10.1016/s0190-9622(08)80798-0. [DOI] [PubMed] [Google Scholar]
- 4.Scola F., Telang G.H., Swartz C. Dyshidrosiform pemphigoid. J Am Acad Dermatol. 1995;32(3):516–517. doi: 10.1016/0190-9622(95)90092-6. [DOI] [PubMed] [Google Scholar]
- 5.Chang Y.T., Liu H.N., Wong C.K. Bullous pemphigoid–a report of 86 cases from Taiwan. Clin Exp Dermatol. 1996;21(1):20–22. [PubMed] [Google Scholar]
- 6.Caldarola G., Fania L., Cozzani E., Feliciani C., De Simone C. Dyshidrosiform pemphigoid: a well-defined clinical entity? Eur J Dermatol. 2011;21(1):112–113. doi: 10.1684/ejd.2010.1172. [DOI] [PubMed] [Google Scholar]
- 7.Lupi F., Masini C., Ruffelli M., Cianchini G. Dyshidrosiform palmoplantar pemphigoid in a young man: response to dapsone. Acta Derm Venerol. 2010;90(1):80–81. doi: 10.2340/00015555-0734. [DOI] [PubMed] [Google Scholar]
- 8.Patrizi A., Rizzoli L., Benassi L., Neri I. Another case of dyshidrosiform pemphigoid. J Eur Acad Dermatol Venereol. 2003;17(3):370. doi: 10.1046/j.1468-3083.2003.00792_17.x. [DOI] [PubMed] [Google Scholar]