Introduction
Myiasis is a pathogenic condition found in live humans and animals caused by various species of dipteran larvae. Chrysomya bezziana, also known as old world screwworm, is an obligate parasite in mammals and is known to infest wounds. A case of nasal myiasis by this species in a patient from rural South India is being reported.
Case report
A 50-year-old female patient, residing in a rural area, presented with history of nasal obstruction for three months and one episode of epistaxis. Three days prior, she noticed maggots emerging out of her nose. She had no diagnosed or clinically evident nasal pathology. The patient had Type 2 diabetes mellitus with poor medication compliance.
On examination, she was a poorly nourished woman with pallor and periorbital edema. She had no icterus, clubbing, or lymphadenopathy. Examination of the nose showed a large septal perforation involving both the cartilaginous and bony parts. There were multiple maggots in both nasal cavities (Fig. 1). Nasal endoscopy showed destruction of middle and inferior turbinates on the right side. The mucosa was unhealthy with necrotic tissue and mucopurulent discharge. A noncontrast computed tomography of nose and paranasal sinuses revealed destruction of bony septum, and the superior, middle, and inferior turbinate on the right side with breach of lamina papyracea on both sides with no evidence of orbital cellulitis or abscess (Fig. 2).
Fig. 1.
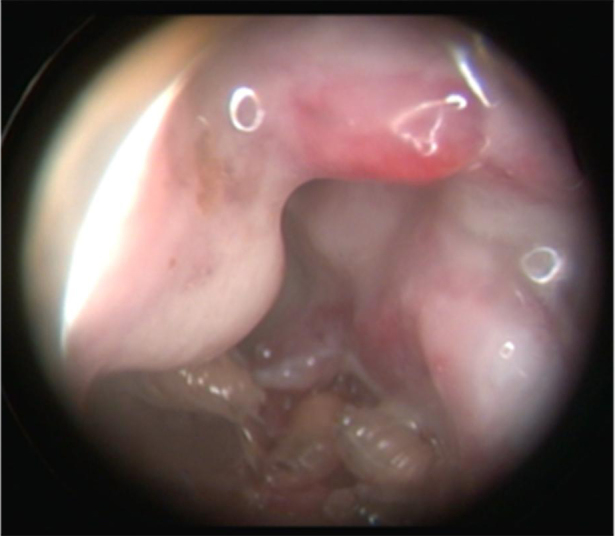
Endoscopic view – maggots in nasal cavity.
Fig. 2.
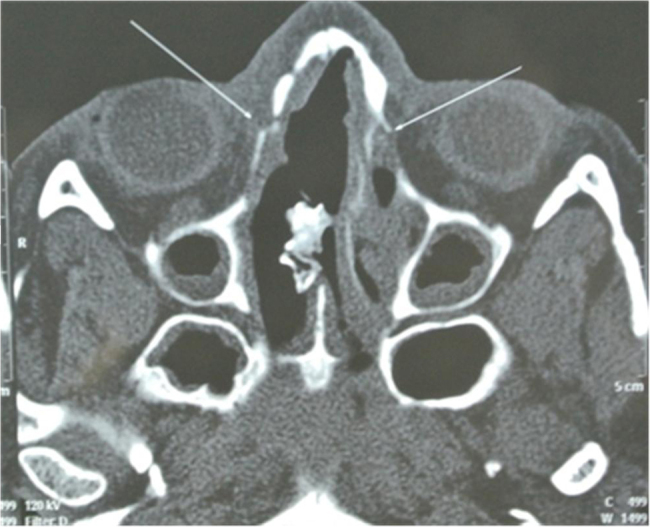
Computed tomography scan showing septal perforation and breach in lamina papyracea.
Biochemical tests showed raised blood sugar levels and deranged renal parameters. The patient was treated with parenteral broad-spectrum antibiotics. Turpentine oil was instilled locally, and maggots were removed manually under endoscopic visualization and regular nasal toilet was done. Glycemic control was achieved with regular insulin in the dosage of 12 units–12 units–10 units subcutaneously. On entomological examination, the maggot (Fig. 3) was identified as larva of C. bezziana. Histopathological examination of the nasal mucosa showed nonspecific inflammation. The patient was discharged after 10 days and followed up after one week and monthly for six months. There was no recurrence of myiasis on follow-up.
Fig. 3.

Maggot of Chrysomya bezziana.
Discussion
Nasal myiasis is common in tropical and subtropical areas of the world. The disease occurs equally in both genders and is usually seen in those over 50 years of age.1 The patients usually present with epistaxis, nasal obstruction, rhinorrhea with fetid odor, facial pain, and headache. The predisposing factors include poor hygiene, underlying diseases like atrophic rhinitis, chronic rhinosinusitis, infective conditions like tuberculosis, leprosy, syphilis, malignancies, systemic diseases like diabetes mellitus, and other conditions causing immunosuppression.
Flies, attracted by odoriferous lesions, deposit their eggs on surfaces contaminated with blood or mucous.2 C. bezziana females lay 150–500 eggs at sites of wounds or in body orifices, which hatch after 18–24 h. Eggs can be inadvertently transferred to other sites by the patient's own fingers.3 On hatching, maggots penetrate deep into the host tissues. The larvae feed on the host tissue for five to seven days while they complete their development. Larvae, while feeding on infected or necrotic tissues, release toxins, which result in progression of necrosis. The pupal stage lasts for seven to nine days in tropical conditions, but up to eight weeks in the subtropical winter months.
C. bezziana is a cause of obligatory myiasis in nose, ear, face, gums, and serous cavities.4 This fly is widely distributed in Asia, tropical Africa, India, and Papua New Guinea (Fig. 4). C. bezziana differs from other maggot infestations by its ability to cause tissue invasion even without pre-existing necrosis. The larvae of C. bezziana burrow deep into the host's healthy living tissue in a screw-like fashion feeding on living tissue, which may be responsible for the septal perforation and destruction of turbinates in this case.
Fig. 4.

Geographic distribution of Chrysomya bezziana.
Source: Spradbery JP. A Manual for the Diagnosis of the Screw-Worm Fly. Canberra, Australia: Division of Commonwealth Scientific and Industrial Research Organization, Division of Entomology; 1991. p. 64. ISBN: 0 643 05268 2.
Treatment comprises systemic and local measures, with the standard treatment being manual removal of maggots.5 Nasal endoscopy enables removal of maggots under vision and thus helps in better clearance.6 Systemic antibiotics are given to combat secondary infections.
As environmental sanitation is important in controlling the population of the flies and thereby myiasis, importance of public education about myiasis as well as maintenance of a high level of environmental health standards is imperative.7
Conclusion
Nasal myiasis, a disease of tropical countries, affects patients having predisposed diseases and poor hygiene. The larvae of C. bezziana have the ability to cause significant tissue destruction by invasion.
Conflicts of interest
The authors have none to declare.
References
- 1.Sharma H., Dayal D., Agrawal S.P. Nasal myiasis: review of 10 years experience. J Laryngol Otol. 1989;103:489–491. doi: 10.1017/s0022215100156695. [DOI] [PubMed] [Google Scholar]
- 2.Manfirm A.M., Cury A., Demeneghi P., Jotz G., Roithmann R. Nasal myiasis: case report and literature review. Int Arch Otorhinolaryngol. 2007;11:74–79. [Google Scholar]
- 3.Arora S., Sharma J.K., Pippal S.K., Sethi Y., Yadav A. Clinical etiology of myiasis in ENT: a reterograde period-interval study. Braz J Otorhinolaryngol. 2009;75(3):356–361. doi: 10.1016/S1808-8694(15)30651-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sood V.P., Kakkar P.K., Vattal V.L. Myiasis in otorhinolaryngology with entomological aspects. J Laryngol Otol. 1976;90:393–399. doi: 10.1017/s0022215100082219. [DOI] [PubMed] [Google Scholar]
- 5.Sinha V., Shah S., Ninama M. Nasal myiasis. J Rhinol. 2006;13(2):120–123. [Google Scholar]
- 6.Ranga R.K., Yadav S.P.S., Goyal A., Agrawal A. Endoscopic management of nasal myiasis: a 10 years experience. Clin Rhinol Int J. 2013;6(1):58–60. [Google Scholar]
- 7.Babamahmoudi F., Rafinejhad J., Enayati A. Nasal myiasis due to Lucilia sericata (Meigen, 1826) from Iran: a case report. Trop Biomed. 2012;29(1):175–179. [PubMed] [Google Scholar]


