Abstract
Background
Tuberculosis of spine is known as tubercular spondylitis or Pott's spine. The vertebral involvement leads to various pathological processes such as abscess formation, cord compression, and gibbus deformity. Magnetic Resonance Imaging (MRI) is the imaging modality of choice which not only helps in diagnosing a case of Pott's spine but also gives valuable information about its impending complications, thereby, aiding in management of these cases.
Methods
In this study, MRI scans of 80 proven cases of tubercular spondylitis were studied retrospectively for the various pathological processes affecting the spine.
Results
Of the 80 cases included in this study, 68.8% of cases were male and 31.2% of cases were females. Majority of cases were seen in 21–40 yrs age group. Lumbar vertebrae were more commonly affected than the dorsal vertebrae. Contiguous two vertebral involvement was the most common pattern, and skip lesions were seen in 5% of cases. Pre-, paravertebral and epidural soft tissue component was seen in 96.25% and 62.5% of cases, respectively. Intervertebral disc Involvement was noted in 95% of cases, and cord edema was seen in 15% of cases.
Conclusion
Tubercular spondylitis or Pott's spine is an extrapulmonary form of tuberculosis which affects the spine. MRI is the imaging modality of choice not only in diagnosing the condition but also in guiding the surgical management. The cases of spinal tuberculosis were systematically analyzed for various pathological lesions which are produced in the spine as the disease progresses.
Keywords: Tuberculosis, Spine, MRI
Introduction
Tuberculosis (TB) is a bacterial infection caused by Mycobacterium tuberculosis.1 It generally affects the lungs, but can also affect other parts of the body. When the infection spreads outside the lungs, it is called extrapulmonary tuberculosis. The tubercle bacillus reaches vertebrae through hematogenous route most commonly via venous plexus of Batson usually secondary to an extra spinal source of infection.2 The tubercular infection of the spine is better known as Pott's spine after it was first described in 1779 by Percivall Pott.3 It first affects the anterior aspect of the vertebral body adjacent to the subchondral plate. It spreads from there to involve the adjacent intervertebral discs.4 Apart from the clinical signs and symptoms, laboratory test are used to diagnose tuberculosis of spine but the imaging (Radiograph, Computed tomography (CT) and Magnetic Resonance Imaging (MRI)) is the mainstay in diagnosis and management of spinal tuberculosis. Though CT is considered better for imaging of bones, but in spinal tuberculosis MRI has proved to be the modality of choice because of its multiplanar capability and inherent ability to demonstrate the soft tissue and marrow involvement better than CT. It not only demonstrates the bony spinal involvement but also the involvement of the cord which may get affected secondarily.
Materials and methods
Aim of this study was to retrospectively analyze the pattern of involvement of the spine and its complications in patients of spinal tuberculosis who underwent MRI as a diagnostic workup. This study was done in Department of Radiodiagnosis and Imaging of a tertiary care teaching hospital in Pune. MRI scans of all the histopathologically proven cases of Pott's spine done between June 2011 and June 2015 were included in the study. 80 cases were included in this study, in which tubercular infection was proven by Ziehl Neelsen stain, culture or showed histopathological evidence of caseating granuloma either before or after the MRI scan. CT or ultrasound guided aspiration of collection/pus was done where it was indicated. In all operated cases, histopathological examination of tissue was done to confirm the diagnosis. All age groups of patients and both sexes were included in the study, while repeat scans of same patients were excluded from the study. The scans were done on 1.5T Siemens Somatom Symphony, Germany MRI machine. We followed our institutional MR Protocol for spine which is mentioned in Table 1. MR myelogram in sag and coronal planes was done to see significant canal compromise. Spine was evaluated for involvement of site and number of vertebral bodies. The vertebral bodies were assessed for marrow edema on T1W and (Short T1 inversion recovery) STIR images, continuity of end plates, wedging/collapse or deformity on Sag and Cor T1W, T2W and STIR sequences. Posterior cortex was studied for posterior bulge or retropulsion. Intervertebral disc was assessed for increase or decrease in height, signal intensity, and post contrast enhancement. The altered signal intensity and erosion or destruction of posterior elements were assessed on sagittal and axial images. The pre-, paravertebral and epidural soft tissue component and Psoas collection were assessed and documented. The spinal cord was assessed for cord edema or compression.
Table 1.
MR protocol for spine.
| Plane | Sequence |
|---|---|
| Sagittal | T2W (screening of whole spine) T1W, T2W (Affected spine) STIR, Pre contrast FS Myelogram |
| Coronal | STIR Myelogram |
| Axial | T1W T2W |
| Multiplanar (axial, coronal, sagittal) | Post contrast fat sat |
Results
The study included 80 cases of spinal tuberculosis, out of which 55 (68.8%) cases were males and 25 cases (31.2%) were females. Maximum number of cases 22 (27.5%) were observed in 21–30 years age group (Table 2) with almost equal number of cases in 31–40 and 51–60 yrs age group. Majority of cases involved adjacent 2 vertebral bodies (66.25%), followed by involvement of 3 vertebral bodies (12.5%), single vertebral body involvement was seen in 5% of cases and more than 5 vertebrae were involved in 6.25% of cases (Table 3). Most commonly affected vertebrae were Lumbar vertebrae in 38 (47.5%) of cases followed by dorsal vertebrae in 25 (31.25%) of cases (Table 4). Dorsolumbar (D12-L1) and Lumbosacral (L5-S1) spine was affected in 8 (10%) and 6 (7.5%) cases respectively (Table 4). There were no cases involving the cervicodorsal spine in this study. Skip lesions or noncontiguous involvement was noted in 4 (5%) cases. Involvement of intervertebral disc was noted in 76 (95%) of cases (Table 5). Pre- and paravertebral soft tissue component was seen in 77 (96.25%) of cases, while an epidural component was seen in 50 (62.5%) cases (Table 5). Myelographic cutoff due to epidural component was seen in 16 (20%) cases. Posterior elements showed inflammatory marrow edema, erosion or destruction in 30 (37.5%) cases (Table 5). Cord edema with compression was seen in 12 (15%) cases and Psoas abscess was observed in 20 (25%) cases (Table 5). Gibbus deformity was seen in 22 (27.5%) cases (Table 5). Paraparesis and quadriparesis were seen in 9 (11.25%) cases and 3 (3.75%) cases, respectively. Compressive neuropathy in lower limbs was seen in 17 (21.2%) cases. Cauda equina syndrome was seen in 6 (7.5%) cases.
Table 2.
Age wise distribution of cases.
| Age group (in years) | No of cases (%) |
|---|---|
| 0–10 | 0 (0%) |
| 11–20 | 01 (1.25%) |
| 21–30 | 22 (27.5%) |
| 31–40 | 18 (22.5%) |
| 41–50 | 8 (10%) |
| 51–60 | 17 (21.25%) |
| 61–70 | 10 (12.5%) |
| 71–80 | 4 (5%) |
Table 3.
Affected vertebrae.
| No of vertebrae | No of cases (%) |
|---|---|
| 01 | 4 (5%) |
| 02 | 53 (66.25%) |
| 03 | 10 (12.5%) |
| 04 | 8 (10%) |
| 05 | 5 (6.25%) |
Table 4.
Pattern of vertebral column involvement.
| Cervical | 3 (3.75%) |
| Cervicodorsal | 0 (0%) |
| Dorsal | 25 (31.25%) |
| Dorsolumbar | 8 (10%) |
| Lumbar | 38 (47.5%) |
| Lumbosacral | 6 (7.5%) |
Table 5.
Various pathologies in Pott's spine.
| IV disc involvement | 76 (95%) |
| Pre/paravertebral component | 77 (96.25%) |
| Epidural component | 50 (62.5%) |
| Cord edema/compression | 12 (15%) |
| Psoas abscess | 20 (25%) |
| Posterior elements involved | 30 (37.5%) |
| Gibbus deformity | 22 (27.5%) |
Discussion
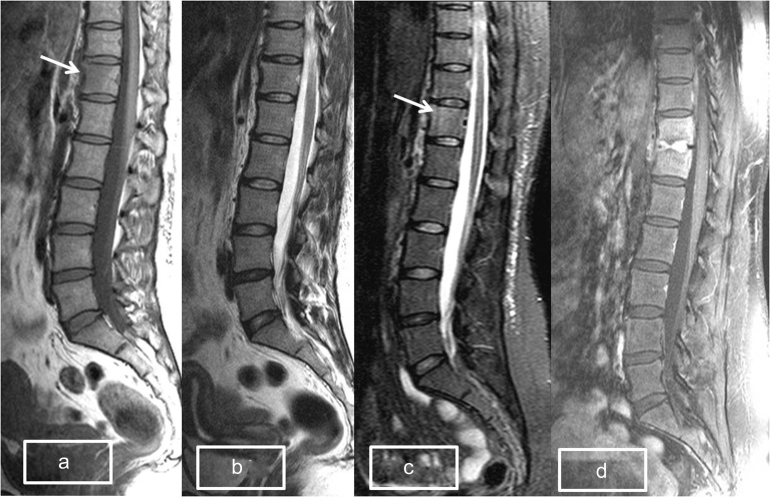
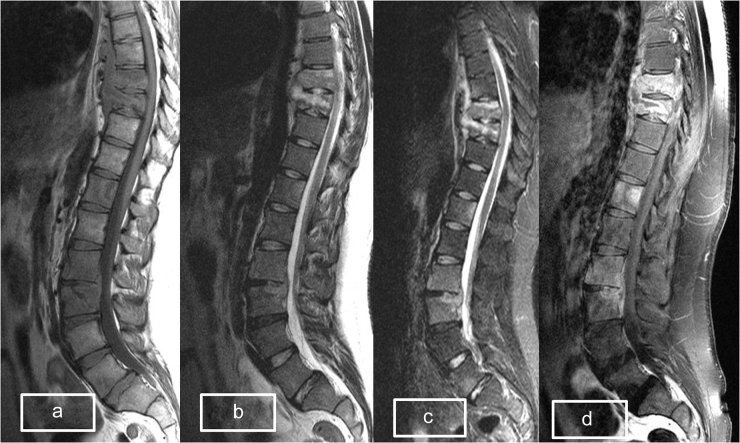
Musculoskeletal system is affected approximately 10–15% of cases of extrapulmonary tuberculosis. Pott's spine is the commonest manifestation of musculoskeletal tuberculosis, accounting for approximately 40–50% of cases.5 Though it can affect all age groups of patients; however, most of the patients in this study (50% cases) were in the 21–40 yrs age group followed by 33.75% cases in 51–70 yrs age group. This suggests that in developing nation like India the most economically productive age group is also the most vulnerable. In this study the most commonly affected were lumbar vertebrae followed by dorsal vertebrae, however dorsolumbar spine has been reported to be the most common site in many studies.2 Early marrow edema is demonstrated as diffuse hypointensity on T1W images and as hyperintensity on STIR images and can be missed on T2W images (Fig. 1a–c). However, post contrast images will demonstrate marrow enhancement of the affected vertebra (Fig. 1d). Therefore, if a tubercular pathology is suspected during MRI study it is suggested that screening of whole spine should be carried out with Sag post contrast T1W fat sat sequence to pick up subtle lesions. Presence of pre or paravertebral soft tissue component clinches the diagnosis in favor of tuberculosis. Single vertebral and skip lesions are atypical presentations of the spinal tuberculosis. Increased incidence of single vertebral involvement in this study can be explained from the fact that all these cases underwent early MRI evaluation and the infection probably had not tracked subligamentously to involve the contiguous vertebra or had not completely involved the intervertebral disc. Skip lesions or noncontiguous vertebral tuberculosis (Fig. 2a–d) occurs due to hematogenous spread through the vertebral venous system that spreads the infection to multiple vertebrae. This is responsible for central focus of infection in these cases as compared to the anterior subchondral involvement of the vertebral body which occurs in the arterial arcade that forms a rich vascular plexus.6 Sinan et al.,7 found the involvement of the intervertebral disc in 72% of the cases, however in this study intervertebral (IV) disc involvement was seen in 95% of the cases. The increased incidence of IV disc involvement in our study could be explained due to use of intravenous contrast agent in our study which shows enhancement of the involved IV disc (Fig. 1d). This we feel it is more sensitive than the T2W/STIR hyperintensity demonstrated by the affected disc on non-contrast study.
Fig. 1.
(a) T1W Sag image showing hypointense signal in the anterior subchondral region of D12 vertebral body (arrow) suggestive of early marrow edema. (b) T2W image in same patient does not show any significant abnormality in the D12 vertebral body. (c) STIR Sag image showing subtle marrow hyperintensity in D12 vertebral body suggesting marrow edema. (d) Post contrast Sag T1 fat sat image of the same patient after one month without treatment now shows marked enhancement of D11 and D12 vertebral bodies and the IV disc.
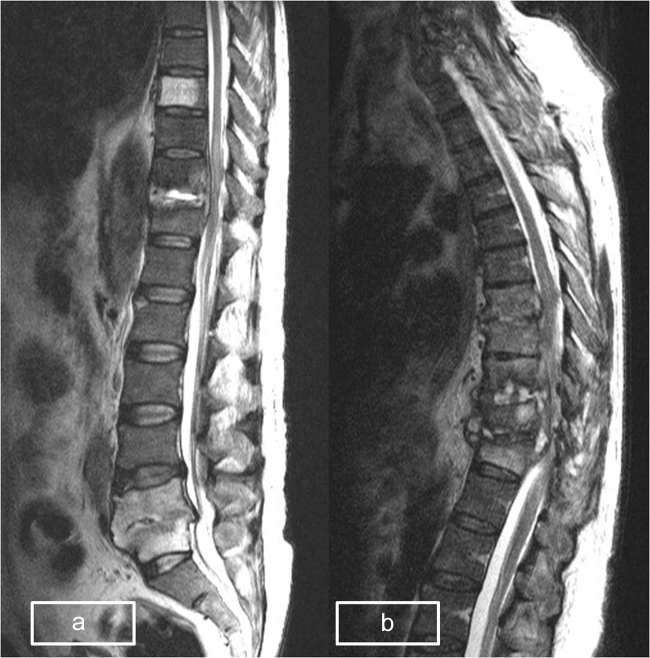
Fig. 2.
(a–c) Sag T1W, T2W, and STIR images show skip lesions with altered marrow signal intensity (hypointense on T1W and hyperintense on T2W/STIR) in dorsal and lumbar vertebrae with prevertebral component at D8-9 level. (d) Sag post contrast image shows noncontiguous enhancement of the affected vertebral bodies. Note relatively preserved IV disc except involvement of L2-3 disc.
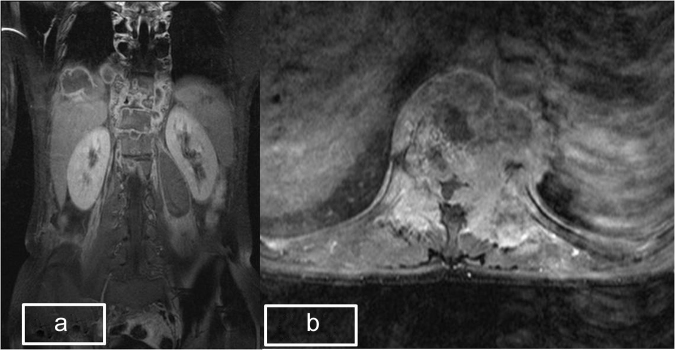
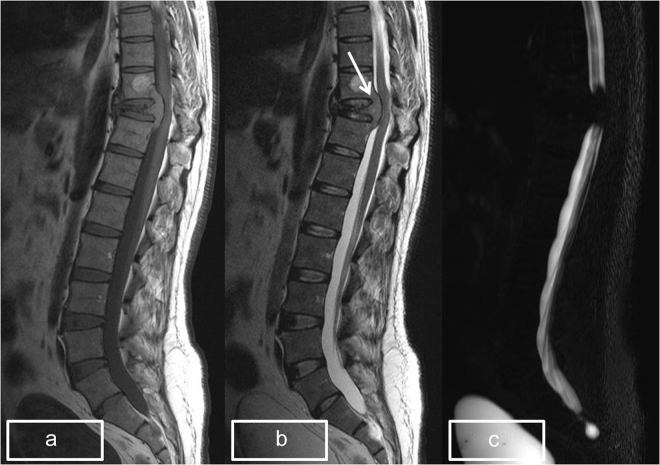
Pre and paravertebral soft tissue component in tubercular spondylitis can be solid in cases of granulomatous inflammation or can be cystic collection due to abscess formation, in this study 77 (96.25%) cases showed a pre or paravertebral soft tissue component which is almost similar to the study by Gehlot et al. who reported a pre and paraspinal abscess in 98.5% of their cases.8 T2W/STIR images demonstrate the collection easily but a caseating paravertebral soft tissue component is best demonstrated on post contrast T1W fat sat images (Fig. 3a). Psoas abscess was seen in 25% of our cases whereas Owolabi et al.9 reported it in only 3% of the cases. Psoas abscess is a complication of tubercular spondylitis which occurs due to tracking of pre or paravertebral abscess along the Psoas muscle. It is seen as hypointense lesion on T1W images and as hyperintense collection on T2W/STIR images. But the best way to demonstrate a Psoas abscess is post contrast T1W fatsat sequence which shows the abscess as central non enhancing area with peripheral wall enhancement (Fig. 3a). Epidural soft tissue component or collection is a dreaded complication of tubercular spondylitis as it may lead to compression of thecal sac and cause cord compression. It is seen as hypointense lesion on T1W images and appears hyperintense on T2W/STIR sequences (Fig. 4a–c). On post contrast images it may be seen as soft tissue enhancement or collection with rim enhancement. In this study epidural component was seen in 62.5% of cases. Posterior elements of vertebrae include pedicle, transverse process, laminae, spine, and the articular facets. Involvement of posterior elements is not common in tubercular spondylitis but was seen in 37.5% of the cases in this study which is a significant finding, considering the widely held belief that tuberculosis rarely affects the posterior elements.10 The commonest involvement is of the pedicle which is usually in continuation with the vertebral body as it is rare to come across involvement of posterior elements in isolation (Fig. 3b). In this study we did not come across any case with isolated involvement of posterior elements. Gibbus in latin means “hump” or “hunch”. Gibbus deformity is seen commonly in involvement of lower dorsal and upper lumbar vertebrae, it was seen in this study in 27.5% of cases, it occurs due to collapse of the vertebral bodies. Cord edema or compression in Pott's spine can occur due to epidural collection or retropulsion of collapsed vertebra and is a surgical emergency as it may lead to paraplegia or quadriplegia depending on the site of affection. In this study, cord edema/compression was found in 15% of the cases (Fig. 5a and b). It is important to look for cord edema or compression whenever epidural component or retropulsion is seen and best way to look for it is in Sag and Axial T2W images and augmented by STIR images in cases of ambiguity.
Fig. 3.
(a) Coronal images showing bilateral paravertebral and Psoas abscess in left Psoas muscle. (b) Axial post contrast image shows destruction of bilateral pedicles and transverse processes with soft tissue component.
Fig. 4.
(a–c) Sag T1, T2, and myelogram images showing soft tissue epidural component (arrow) causing cord compression and complete myelographic cut off at D10 level.
Fig. 5.
(a) Sag T2W image shows tubercular spondylitis of D10-11 with epidural component and cord edema. Evidence of old Pott's spine is seen at L5-S1 level. Incidentally noted is hemangioma of D8 vertebral body. (b) Sag T2W image shows multiple vertebral body involvement of dorsal spine with compression of the cord.
Most of the cases of tuberculosis of spine undergo repeated MRI to study the effect of Anti tubercular treatment (ATT) on these cases. Reduction in marrow edema, appearance of sclerosis seen as hypointensity in all sequences, loss of T2W hyperintensity of IV disc and reduction in pre, paravertebral and epidural soft tissue component are some of the features of healing Pott's spine. But we feel that the healing is better assessed on post contrast MRI. Reduction in the vertebral and IV discal enhancement, reduction in paravertebral or epidural soft tissue component and abscesses are best demonstrated on post contrast images and can be compared with previous post contrast study for assessing the response to the treatment (Fig. 6a–c).
Fig. 6.
(a) Sag post contrast image of patient as in Fig. 3e shows enhancement of D11 and D12 vertebral body and the intervening IV disc. (b) Sag T1W image after treatment with ATT for 9 months show sclerosis and fatty infiltration of marrow. (c) Sag post contrast images after treatment with ATT for 9 months show minimal residual enhancement in the D11 & D12 vertebral bodies and the IV disc suggestive of resolving infection.
Limitations of study were inability to follow up all cases and Immune status of patients was not known in all cases.
Conclusion
Tubercular spondylitis or Pott's spine is an extrapulmonary form of tuberculosis which affects the spine. The vertebral body and IV disc get involved early in the disease and can result in various complications such as cord compression with disastrous consequences. MRI is considered to be imaging modality of choice as it not only demonstrates the bony involvement but also the associated complications such as pre-, paravertebral and epidural abscesses and cord edema. MRI also helps in guiding the surgical management of a case of tuberculosis of spine. Even though plain MRI is enough to diagnose most of the cases but use of contrast delineates the extent of disease better and helps in prognostication in sequential MRI after treatment.
Conflicts of interest
The authors have none to declare.
References
- 1.Cambau E., Drancourt M. Steps towards the discovery of Mycobacterium tuberculosis by Robert Koch, 1882. Clin Microbiol Infect. 2014;20(March (3)):196–201. doi: 10.1111/1469-0691.12555. [DOI] [PubMed] [Google Scholar]
- 2.Burrill J., Williams C.J., Bain G. Tuberculosis: a radiologic review. Radiographics. 2007;27(5):1255–1273. doi: 10.1148/rg.275065176. [DOI] [PubMed] [Google Scholar]
- 3.Tuli S.M. Tuberculosis of the spine: a historical review. Clin Orthop Relat Res. 2007;460:29–38. doi: 10.1097/BLO.0b013e318065b75e. [DOI] [PubMed] [Google Scholar]
- 4.Rasouli M.R., Mirkoohi M., Vaccaro A.R. Spinal tuberculosis: diagnosis and management. Asian Spine J. 2012;6(December (4)):294–308. doi: 10.4184/asj.2012.6.4.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chauhan A., Gupta B.B. Spinal tuberculosis. Indian Acad Clin Med. 2007;8:110–114. [Google Scholar]
- 6.Garg R.K., Somvanshi D.S. Spinal tuberculosis: a review. J Spinal Cord Med. 2011;34(5):440–454. doi: 10.1179/2045772311Y.0000000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sinan T., Al-Khawari H., Ismail M. Spinal tuberculosis: CT and MRI feature. Ann Saudi Med. 2004;24(6):437–441. doi: 10.5144/0256-4947.2004.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gehlot P.S., Chaturvedi S., Kashyap R., Singh V. Pott's spine retrospective analysis of MRI scans of 70 cases. J Clin Diagn Res. 2012;6(November (9)):1534–1538. doi: 10.7860/JCDR/2012/4618.2552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Owolabi L.F., Nagoda M.M., Samaila A.A., Aliyu I. Spinal tuberculosis in adults: a study of 87 cases in Northwestern Nigeria. Neurol Asia. 2010;15(3):239–244. [Google Scholar]
- 10.Moorthy S., Prabhu N.K. Spectrum of MR imaging findings in spinal tuberculosis. Am J Roentgenol. 2002;179(October (4)):979–983. doi: 10.2214/ajr.179.4.1790979. [DOI] [PubMed] [Google Scholar]