Abstract
Background
Over 70,000 nonfatal firearm injuries occur in the US annually, frequently leaving victims injured with retained bullets. The long-term psychological risks associated with retained bullets remains unstudied. By serving as a constant reminder of injury, we hypothesized that the presence of retained bullets after firearm injury is associated with increased PTSD and depression symptom severity.
Methods
We conducted a prospective cohort study (2013–2015) of Black male survivors of firearm injury at an urban Level I trauma center. Interviews, questionnaires and validated survey tools for PTSD (PCL-5) and depression (QIDS-SR16) to assess severity of symptoms were administered 3 months post-injury. Clinical characteristics and symptom severity scores were compared with respect to retained bullets using Wilcoxon Rank Sum tests and linear regression.
Results
Of 139 participants, 101(73%) had retained bullets. The cohort was young (mean age 26 years), educated (82% high school or greater) yet unemployed (53%) and with multiple injuries (median [IQR] no. of GSWs 2 [1–3]). There was no difference in age, education, employment status, number of gunshot wounds, operative procedures, pain, hospital or ICU LOS between groups (p>0.05). Patients with retained bullets less often rated their health as “very good” or “excellent” (10% vs 29%, p=0.046). Of those working prior to injury (n=47), 61% with retained bullets had not returned to work compared to 33% without retained bullets (p=0.027). No difference in PCL-5 scores [30.9 (SD 18.9) vs 27.9 (SD 18.6), p=0.470] was observed, but patients with retained bullets had greater mean QIDS-SR16 scores [10.7 (SD 6.2) vs 7.8 (SD 6.1), p=0.038] than those without. After controlling for injury severity, number of wounds, marital status and education level, multiple linear regression analysis determined that retained bullets (β=3.52; p=0.017) were associated with more severe depressive symptoms.
Conclusion
Retained bullets are associated with adverse psychological consequences after firearm injury. To improve recovery and to aid in clinical management decisions, clinicians should consider both the psychological and physical effects of retained bullets in survivors of firearm injury.
Keywords: firearm injury, gun violence, depressive symptoms, PTSD, retained bullet
Introduction
Firearm violence represents an ongoing public health crisis in the United States of America. Nearly 32,000 individuals die annually as a result of firearm violence, with homicides of young adults 15–30 years of age accounting for approximately one third of these deaths [1]. An additional 100,000 individuals are non-fatally injured by firearms each year [1, 2]. There is no current standard medical practice to remove bullets after a firearm injury, as research addressing the physiologic and psychological effects of retained bullets among survivors is limited. The general rule at many medical institutions, including the study institution, is to leave bullets in place after injury unless they are or become easily accessible (superficial or during laparotomy), potentially morbid (close proximity to nerves or vessels), symptomatic, or per patient request.
Previous studies examining the potential physiologic risks of retained bullets have found such issues as elevated serum lead levels [3–6], secondary osteoarthritis [7, 8], chronic pain [9], infection [10–12], and neurogenic claudication and radiculopathy [13]. Often a bullet will be excised if an apparent medical benefit (e.g. treating injury-site chronic pain or preventing lead toxicity) [14], but there is a paucity of data regarding the psychological consequences of retained bullets to date. The removal of the retained bullet for any such non-physiologic reason depends on patient and surgeon agreement given a patient’s risk profile, without any universal, standard or evidence-based guidelines.
To this end, we hypothesized that the presence of retained bullets is associated with increased symptom severity of PTSD or depression, perhaps by serving as a reminder of the traumatic event. Our primary study objective was to determine whether survivors of firearm injury with retained bullets have increased severity of psychological symptoms (i.e. PTSD and depression) compared to survivors without retained bullets.
Methods
Patient Population
A large, prospective cohort study examining recovery patterns of Black men after all-causes of injury was conducted at our institution from 2013–2016. We performed a subgroup analysis of adult (age ≥ 18 years), Black, male patients who sustained injuries related to gunshot wounds. Men who were: (1) younger than 18 years of age, (2) unable or refused informed consent, (3) currently receiving treatment for PTSD or depression, (4) in police custody or (5) who sustained injuries unrelated to gunshot wounds were not eligible for study participation.
Procedure
This study was approved by the Institutional Review Board of the University of Pennsylvania. Patients who met eligibility criteria during their index hospitalization were informed of the study, had all questions answered, and provided written informed consent. An initial interview was conducted when patients were medically stable and clinically able to participate and demographics, injury-related, and other study-related data were obtained. The presence of a retained bullet was defined as a dominant metallic foreign object seen on radiographic imaging (i.e. X-ray or computed tomography). Follow-up interviews were administered at 3 months post-hospital discharge in the participant’s home. Participants received at $30 gift card at the completion of the intake interview and a $50 gift card at the completion of the 3 month post-discharge interview.
Survey Instruments
Validated survey instruments to evaluate our primary study outcomes of PTSD and depression after firearm injury were included at the 3-month follow-up interviews. This 3-month time frame was selected because it allows sufficient time to diagnose depression and PTSD; diagnosis of Major Depression requires the presence of symptoms for 2 weeks whereas diagnosis of PTSD requires symptoms to persist longer than one month [15].
The PTSD Check List – 5 (PCL-5) is a validated 20-item self-reported instrument used to screen for post-traumatic stress disorder [16, 17]. The instrument assesses the symptoms of PTSD as defined by the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) criteria. Total scores range from 0 to 80. Answers for each question were summed for a total symptom severity score. Higher scores on the 0–80 scale indicate greater symptom severity.
The Quick Inventory of Depressive Symptomatology – Self Report (QIDS-SR16) is a validated 16-item patient-administered instrument used to screen for the nine defining symptom domains of a major depressive episode [18, 19]. These domains include sleep, weight, psychomotor changes, depressed mood, decreased interest, fatigue, guilt, concentration, and suicidal ideation. Higher scores on the 0–27 scale indicate greater symptom severity.
Statistical Methods
Data were entered into REDCap, a secure data management system. Demographic, injury characteristics, and symptom severity were compared with respect to the presence or absence of retained bullets. In our institution, bulletectomies are offered and performed based on both the preferences of the surgeon and the patient and the risk-benefit analysis of the procedure. As a proxy for the risk-benefit analysis, the severity of the injury was measured using number of GSWs, injury severity score (ISS), hospital course, and pain scores.
Categorical variables were described as frequencies and compared with Chi-Square tests while continuous variables were described using means with standard deviations or medians with interquartile ranges, and compared with t-tests or Wilcoxon rank sum tests, as appropriate. Multivariable linear regressions models were constructed to examine the effect of retained bullets on the primary outcomes of PTSD and depression symptom severity. The regression models included an indicator variable for having a retained bullet, while also adjusting for education level, marital status, injury severity, how much pain relief was received, and number of wounds. All analyses were conducted in SPSS 20.0 and STATA 15 with two-sided tests of hypotheses and a p-value of <0.05 as the criterion for statistical significance.
Results
The study sample included 139 participants. The cohort was young with a mean age of 28 (SD 10) years, educated (82% high school degree or higher) yet unemployed (53%) with multiple gunshot wound injuries (median [IQR] no. of GSWs 2 [1–3]; no. of interventions 8 [4–14]; ISS 10 [5–17]).
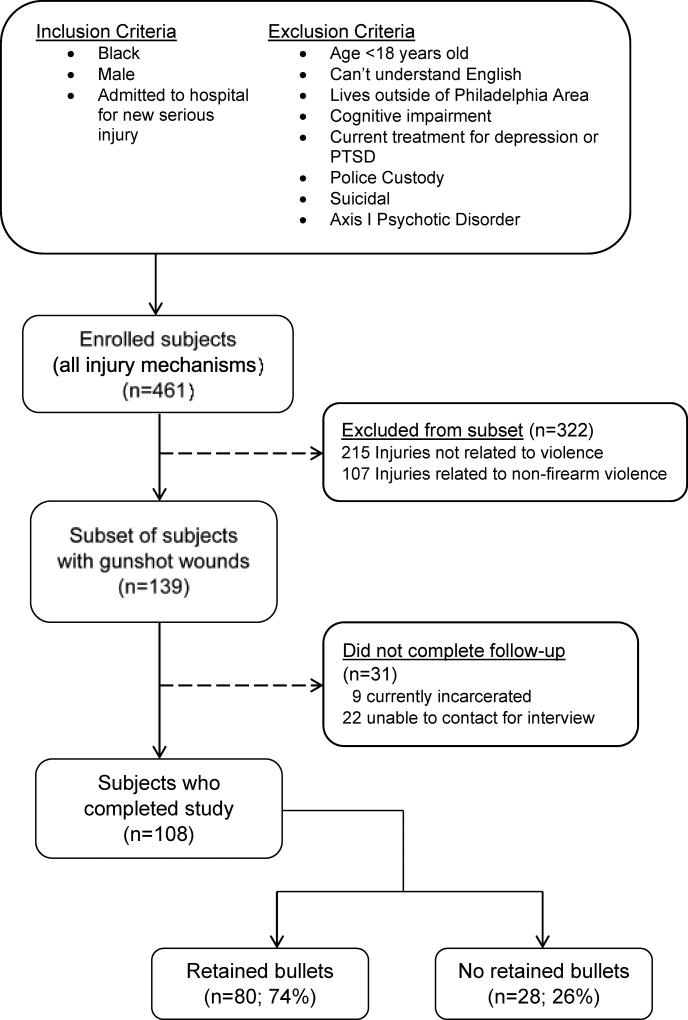
One hundred and eight (78%) of the 139 completed follow-up. Of those who completed follow-up, 80 (74%) had retained bullets (Figure 1). Loss to follow-up was due to incarceration (n=9) and inability to contact participant (n=22). No significant differences were found in demographic characteristics between those retained in the study and those lost to follow-up (Table 1). During the index hospitalization initial assessment, participants with retained bullets (n=80) were compared to those without retained bullets (n=28). There were no differences with respect to age, education level, employment status, number of gunshot wounds, operative procedures, pain or hospital LOS between study groups. Participants with retained bullets had a lower ISS score (p=0.026) than those without retained bullets (Tables 1 and 2).
Figure 1.
Study design of patient population.
Table 1.
Demographic data of study populations at baseline, including men who were lost to follow-up.
| No Retained Bullets N= 28 |
Retained Bullets N=80 |
Lost to Follow-Up N=31 |
p- value* |
|
|---|---|---|---|---|
| Age in years: Mean (SD) | 28.6 (9.7) | 29.0 (11.0) | 25.6 (7.2) | 0.28 |
| Marital Status at baseline: N (%) | 0.14 | |||
| Married/Living w Partner | 5 (18%) | 26 (33%) | 13 (42%) | |
| Not Married/Living w Partner | 23(82%) | 54 (67%) | 18(58%) | |
| High school degree and higher: N (%) | 24 (86%) | 63 (79%) | 27 (87%) | 0.62 |
| Employment status at Baseline: N (%) | 0.36 | |||
| Full-time | 3 (11%) | 24 (30%) | 7 (23%) | |
| Part-time | 6 (21%) | 14 (18%) | 4 (13%) | |
| Unemployed | 19 (68%) | 37 (46%) | 18 (58%) | |
| Student | 0 (0%) | 4 (5.0%) | 2 (6%) | |
| Retired | 0 (0%) | 1 (1%) | 0 (0%) | |
| Previously diagnosed with depression: N (%) | 5 (18%) | 13 (16%) | 5 (16%) | 0.98 |
| Previously diagnosed with PTSD: N (%) | 2 (7%) | 4 (5%) | 3(10%) | 0.66 |
| Previously diagnosed with anxiety: N (%) | 1 (4%) | 6 (7%) | 3 (10%) | 0.66 |
p-value is provided for comparison of study group versus individuals lost to follow-up
Table 2.
Clinical course in patients with and without retained bullets during index hospitalization
| No RB n=28 |
RB n=80 |
p-value | |
|---|---|---|---|
| Injury Severity Score (ISS); mean (SD) | 9.1 (8.1) | 13.8 (9.7) | 0.026 |
| Number of gunshot wounds | 2(1;2) | 2(1;4) | 0.853 |
| No. of Operative Procedures/Interventions | 6(3;12.8) | 8(4;14) | 0.425 |
| Vent Days | 0(0;0.8) | 0(0;1) | 0.567 |
| ICU Length of stay (days) | 0(0;1) | 0(0;2) | 0.650 |
| Hospital length of stay (days) | 6(2;8.8) | 7(3;12) | 0.212 |
| How much pain relief did you receive? (0–10 scale representing % relief) | 6(5;9.3) | 6.5(3.3;8) | 0.484 |
Three months following hospital discharge, participants with retained bullets less often rated their health as Excellent or Very Good as compared to those without retained bullets (10% vs 29%) and more often rated their health as Good, Fair or Poor (90% vs 71%; p=0.046) (Table 3). Moreover, participants with retained bullets who were employed at baseline were less likely to be back to their previous employment without change than those without retained bullets after firearm injuries (p=0.027) (Table 3).
Table 3.
Mental health and quality of life outcomes in patients with and without retained bullets at three months post hospital discharge
| No Retained Bullets n=28 |
Retained Bullets n=80 |
p-value | |
|---|---|---|---|
| QIDS-SR Score (Depression): mean (SD) | 7.9(6.1) | 10.7(6.2) | 0.038 |
| PCL-C Score (DSM-V PTSD): mean (SD) | 27.9(18.6) | 30.9(18.9) | 0.470 |
| In general, would you say your health is: | 0.046 | ||
| Excellent/Very Good | 8 (29%) | 8 (10%) | |
| Good/Fair/Poor | 20 (71%) | 72 (90%) | |
| Health compared to last year | 0.233 | ||
| Better | 3 (11%) | 10 (13%) | |
| Same | 10 (36%) | 14 (18%) | |
| Worse | 15 (54%) | 56 (70%) | |
| Are you back to the same work that you were doing before your injury? (If employed at baseline, n=47) | n=9 | n=38 | 0.027 |
| No | 3 (33%) | 23 (61%) | |
| Part-time only | 2 (22%) | 3 (8%) | |
| Yes, but with limitations | 0(0%) | 8(21%) | |
| Yes, with no changes | 4 (44%) | 4(11%) |
We then assessed PTSD and depression symptom severity at three months post hospital discharge. No significant difference in PCL-5 scores for PTSD (p=0.470) was observed between groups. Participants with retained bullets had more severe symptoms of depression as reflected by QID-SR16 scores [mean 10.7 (SD 6) vs 7.8 (SD 6), p=0.038] than those without, with an effect size of 0.45.
Controlling for injury severity, number of wounds, marital status and education at time of index hospitalization, the adjusted multiple linear regression analysis indicated that retained bullets (β=3.52; p=0.017) and number of wounds (β=0.99; p=0.019) were associated with more severe depressive symptoms at three months post hospital discharge and explained 17% of the variance in depression scores. (Table 4). The adjusted multiple linear regression analysis found no association with severity of PTSD symptoms at three months post hospital discharge.
Table 4.
Linear regression model for effect of retained bullets on depression symptom severity (QIDS-SR) at three months post hospital discharge (n=94)
| Variable | β | Sig | 95% CI |
|---|---|---|---|
| Injury Severity Score | 0.05 | .458 | (−0.08 – .182) |
| Number of wounds | 0.99 | .019 | (.164 – 1.81) |
| Relationship Status ** | −1.60 | .239 | (−4.27 – 1.08) |
| Education*** | −1.41 | .358 | (−4.45 – 1.63) |
| How much pain relief did you receive? (0–10 scale representing % relief) | −0.04 | .832 | (−0.40 – .324) |
| Presence of retained bullet | 3.52 | .017 | (0.63 – 6.40) |
Relationship status: Married/living with partner vs. all others
Education: High school or greater vs. Non-HS
Discussion
Retained bullets are common after firearm injury but few reports have described their impact on survivors. While current literature indicates that retained bullets should be removed for particular physiologic indications [3–14], to our knowledge, the current report is the first study to suggest a psychological benefit to having no retained bullets. The most important finding of our study is that the presence of a retained bullet was associated with more severe depressive symptoms in Black men who sustained firearm injuries. Specifically, men with retained bullets had depressive severity scores 3.5 points higher than those without retained bullets when controlling for other variables. Our results suggest that there may be value in removing retained bullets.
Previous studies demonstrate a link between traumatic injury and psychological disorders. Post-injury psychological disorders are associated with poor quality of life, increased substance abuse, poor coping strategies, impaired functional ability and adverse health outcomes [20, 21]. In a systematic review by Wiseman et al, depression was found in 28–42% of injury survivors [20]. Despite comprehensive screening measures, follow-up studies indicate that few survivors receive treatment for their psychological symptoms— which may contribute to adverse health outcomes and quality of life [22]. Not only did our study participants with retained bullets experience more severe symptoms of depression and poorer quality of life as compared to participants without retained bullets, our results indicate that participants with retained bullets were less likely to return their baseline employment status, an indication of functional status.
In this paper, we focused on severity of psychological symptoms rather than DSM-5 diagnoses. Based on previous work by our group, post-injury psychological symptom severity is associated with suboptimal recovery after injury [23].
Although our research did not demonstrate an association between retained bullets and PTSD, previous studies have indicated that PTSD is prevalent and that depression and PTSD are often co-morbid conditions that may impact outcomes after injury [24]. Shih et al. found that nearly one-third (31%) of survivors of traumatic physical injury requiring hospitalization screened positive for PTSD at 6 months following discharge [24]. It is plausible that a greater time lapse from injury to assessment is needed to discern a difference attributable to the retained bullet itself rather than the act of being shot and injured by a firearm.
The findings of this study provide a first glimpse at the potential impact of retained bullets on post-injury psychological symptoms and merit future study. The implications of this research are important, and if confirmed in future studies, point to potential benefits to patient care, injury prevention strategies and advocacy. Mental illness is associated with increased risks of injury recidivism [25–27]. Wan et al. determined 42% of individuals with a diagnosis of mental illness, defined as depression, psychosis, schizophrenia, anxiety disorder or any combination, experienced recurrent injury compared to 10% in individuals without a diagnosis of mental illness [26]. In another study identifying risk factors for injury recidivism using a population sample from the Medical Expenditure Panel Survey, Alghnam et al. determined that recidivists were more likely to have a positive screen for depression than non-recidivists [27]. By better managing risk factors for depression, such as retained bullets, we suggest an opportunity to intervene and potentially interrupt the cycle of recurrent violence.
Study results should be interpreted within the context of study limitations. We were unable to obtain 3-month outcome data on all study participants. Missing data reduced the number of participants included in the regression analysis which may have reduced statistical power. Contrary to other research on retained bullets, our study collected data in a prospective fashion with 78% retention at 3-month follow-up. Our cohort included only Black male survivors, who comprise the overwhelming majority of those injured from firearm violence both at our institution and in urban America. Thus, our results should be extrapolated to other population with caution.
In addition, this study was associated with diminutive harm to participants. There was minimal risk that the interview itself would worsen psychologic outcomes, as it has been shown that seriously injured urban Black males participate in clinical research as a means of human and therapeutic connection [28]. Further, the follow-up interviews did not focus on the bullet injury itself, but rather the psychologic symptoms of the patient, thereby reducing potential triggers or memories of the retained bullets.
Given the established association between retained bullets and depression symptoms severity, the specific management of bullets should be reconsidered. Future research should aim to understand the burden of retained bullets from an epidemiologic perspective – determining prevalence, costs, interventions, outcomes and impact of retained bullets from the perspective of the injured through qualitative research.
Conclusion
Our results demonstrate that retained bullets are associated with more severe symptoms of depression after firearm injury. Study results suggest that clinicians should consider both the psychological and physical effects of retained bullets in survivors of firearm injury. Regular screening for depression and PTSD along with a multidisciplinary approach including mental health professionals may prove beneficial to patient care, injury prevention strategies and advocacy for those with retained bullets after firearm injury.
Acknowledgments
Funding: Research reported in this publication was supported by the National Institute of Nursing Research of the National Institutes of Health under Award Number R01NR013503 (PI: Richmond). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
In addition, the authors would like to acknowledge Jessica Webster, senior research coordinator, for her outstanding management of the study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Prior Abstract Presentation: 46th Annual Meeting of the Society of Critical Care Medicine, January 2017.
References
- 1.CDC. Injury Prevention & Control: Data & Statistics (WISQARS) http://www.cdc.gov/injury/wisqars/ed2016.
- 2.Annest JL, Mercy JA, Gibson DR, Ryan GW. National estimates of nonfatal firearm-related injuries. Beyond the tip of the iceberg. JAMA. 1995;273:1749–54. [PubMed] [Google Scholar]
- 3.McQuirter JL, Rothenberg SJ, Dinkins GA, Kondrashov V, Manalo M, Todd AC. Change in blood lead concentration up to 1 year after a gunshot wound with a retained bullet. Am J Epidemiol. 2004;159:683–92. doi: 10.1093/aje/kwh074. [DOI] [PubMed] [Google Scholar]
- 4.Fiorica V, Brinker JE. Increased lead absorption and lead poisoning from a retained bullet. J Okla State Med Assoc. 1989;82:63–7. [PubMed] [Google Scholar]
- 5.Farrell SE, Vandevander P, Schoffstall JM, Lee DC. Blood lead levels in emergency department patients with retained lead bullets and shrapnel. Acad Emerg Med. 1999;6:208–12. doi: 10.1111/j.1553-2712.1999.tb00157.x. [DOI] [PubMed] [Google Scholar]
- 6.Linden MA, Manton WI, Stewart RM, Thal ER, Feit H. Lead poisoning from retained bullets. Pathogenesis, diagnosis, and management. Ann Surg. 1982;195:305–13. doi: 10.1097/00000658-198203000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rehman MA, Umer M, Sepah YJ, Wajid MA. Bullet-induced synovitis as a cause of secondary osteoarthritis of the hip joint: A case report and review of literature. J Med Case Rep. 2007;1:171. doi: 10.1186/1752-1947-1-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Primm DD. Lead arthropathy -- progressive destruction of a joint by a retained bullet. Case report. J Bone Joint Surg Am. 1984;66:292–4. [PubMed] [Google Scholar]
- 9.Mazotas IG, Hamilton NA, McCubbins MA, Keller MS. The long-term outcome of retained foreign bodies in pediatric gunshot wounds. J Trauma Nurs. 2012;19:240–5. doi: 10.1097/JTN.0b013e31827757a7. [DOI] [PubMed] [Google Scholar]
- 10.Spitz DJ, Ouban A. Meningitis following gunshot wound of the neck. J Forensic Sci. 2003;48:1369–70. [PubMed] [Google Scholar]
- 11.Sarmiento JM, Yugueros P, Garcia AF, Wolff BG. Bullets and their role in sepsis after colon wounds. World J Surg. 1997;21:648–52. doi: 10.1007/s002689900288. [DOI] [PubMed] [Google Scholar]
- 12.Poret HA, Fabian TC, Croce MA, Bynoe RP, Kudsk KA. Analysis of septic morbidity following gunshot wounds to the colon: the missile is an adjuvant for abscess. J Trauma. 1991;31:1088–94. discussion 94–5. [PubMed] [Google Scholar]
- 13.Ajmal S, Enam SA, Shamim MS. Neurogenic claudication and radiculopathy as delayed presentations of retained spinal bullet. Spine J. 2009;9:e5–8. doi: 10.1016/j.spinee.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 14.Riehl JT, Sassoon A, Connolly K, Haidukewych GJ, Koval KJ. Retained bullet removal in civilian pelvis and extremity gunshot injuries: a systematic review. Clin Orthop Relat Res. 2013;471:3956–60. doi: 10.1007/s11999-013-3260-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hunt JC, Sapp M, Walker C, Warren AM, Brasel K, deRoon-Cassini TA. Utility of the injured trauma survivor screen to predict PTSD and depression during hospital admission. J Trauma Acute Care Surg. 2017;82:93–101. doi: 10.1097/TA.0000000000001306. [DOI] [PubMed] [Google Scholar]
- 16.Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. J Trauma Stress. 2015;28:489–98. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- 17.Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, et al. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in veterans. Psychol Assess. 2016;28:1379–91. doi: 10.1037/pas0000254. [DOI] [PubMed] [Google Scholar]
- 18.Surís A, Holder N, Holliday R, Clem M. Psychometric validation of the 16 Item Quick Inventory of Depressive Symptomatology Self-Report Version (QIDS-SR16) in military veterans with PTSD. J Affect Disord. 2016;202:16–22. doi: 10.1016/j.jad.2016.05.029. [DOI] [PubMed] [Google Scholar]
- 19.Cameron IM, Crawford JR, Cardy AH, du Toit SW, Lawton K, Hay S, et al. Psychometric properties of the Quick Inventory of Depressive Symptomatology (QIDS-SR) in UK primary care. J Psychiatr Res. 2013;47:592–8. doi: 10.1016/j.jpsychires.2013.01.019. [DOI] [PubMed] [Google Scholar]
- 20.Wiseman T, Foster K, Curtis K. Mental health following traumatic physical injury: an integrative literature review. Injury. 2013;44:1383–90. doi: 10.1016/j.injury.2012.02.015. [DOI] [PubMed] [Google Scholar]
- 21.Greenspan AI, Kellermann AL. Physical and psychological outcomes 8 months after serious gunshot injury. J Trauma. 2002;53:709–16. doi: 10.1097/00005373-200210000-00015. [DOI] [PubMed] [Google Scholar]
- 22.Richmond TS, Ruzek J, Ackerson T, Wiebe DJ, Winston F, Kassam-Adams N. Predicting the future development of depression or PTSD after injury. Gen Hosp Psychiatry. 2011;33:327–35. doi: 10.1016/j.genhosppsych.2011.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jacoby SF, Shults J, Richmond TS. The effect of early psychological symptom severity on long-term functional recovery: A secondary analysis of data from a cohort study of minor injury patients. Int J Nurs Stud. 2017;65:54–61. doi: 10.1016/j.ijnurstu.2016.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shih RA, Schell TL, Hambarsoomian K, Belzberg H, Marshall GN. Prevalence of posttraumatic stress disorder and major depression after trauma center hospitalization. J Trauma. 2010;69:1560–6. doi: 10.1097/TA.0b013e3181e59c05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cunningham RM, Carter PM, Ranney M, Zimmerman MA, Blow FC, Booth BM, et al. Violent reinjury and mortality among youth seeking emergency department care for assault-related injury: a 2-year prospective cohort study. JAMA Pediatr. 2015;169:63–70. doi: 10.1001/jamapediatrics.2014.1900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wan JJ, Morabito DJ, Khaw L, Knudson MM, Dicker RA. Mental illness as an independent risk factor for unintentional injury and injury recidivism. J Trauma. 2006;61:1299–304. doi: 10.1097/01.ta.0000240460.35245.1a. [DOI] [PubMed] [Google Scholar]
- 27.Alghnam S, Tinkoff GH, Castillo R. Longitudinal assessment of injury recidivism among adults in the United States: findings from a population-based sample. Inj Epidemiol. 2016;3:5. doi: 10.1186/s40621-016-0071-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bruce MM, Ulrich CM, Kassam-Adams N, Richmond TS. Seriously Injured Urban Black Men's Perceptions of Clinical Research Participation. J Racial Ethn Health Disparities. 2016;3:724–30. doi: 10.1007/s40615-015-0191-y. [DOI] [PMC free article] [PubMed] [Google Scholar]