Key Clinical Message
Even if gossypibomas are extremely rare in the Oro‐Maxillofacial region, they should be evoked in bizarre tumors when repeated histology tests are not contributive, especially in patients with a history of dento‐sinusal surgery. As it is recommended in general surgery, gauzes should be carefully counted when used in dentistry.
Keywords: Foreign bodies, foreign body reaction, gossypiboma, hard palate, paranasal sinus, reconstructive surgical procedures
Background
Gossypiboma or textiloma defines a mass inside the body composed of retained surgical gauze or sponge surrounded by an inflammatory foreign body reaction 1. Very few cases involving the maxillary sinuses were reported 1, 2, 3, 4, 5. The authors describe a case of a cancer‐like gossypiboma of the paranasal sinus that extended to the nasal fossa, the orbit, and the oral cavity. They present the trilayer reconstruction technique they elaborated to reconstruct the loss of 1/3 of the hard palate.
Case Presentation
An 85‐year‐old male was sent to the Oral and Maxillofacial Unit for an enormous tumor of the right paranasal sinus.
His medical history included the following: high blood pressure controlled by medication, treatment by aspirin 150 mg/day for 6 years, complete exeresis of a right paranasal basal cell carcinoma of the skin (1.2 cm in diameter) eleven years before, and some repetitive episodes of epistaxis that usually benefitted from a bilateral nasal packing using gauzes provided with fatty ointment Biogaze® (Bottu Pharmaceuticals, Casablanca, Morocco).
The patient presented with a facial CT scan that showed a large osteolytic tumor of the right maxillary sinus (Fig. 1). Thoraco‐abdominal CT scan was normal. Biopsies were performed by the ENT team through nasal endoscopy. The samples’ histology examination revealed necrosis and inflammatory tissues. New sets of biopsies were performed using a Caldwell–Luc approach. The histological findings showed no different features. Although no histological signs of malignancy were reported, the tumor showed a very aggressive behavior. It spread rapidly through the site of the meatotomy and the vestibular incision. Within a few days, the tumor had invaded the right nasal fossa and a large part of the oral cavity, inducing a destruction of 1/3 of the oral cavity's roof in its lateral part (hard palate; Fig. 2). The histological tests raised suspicion regarding the presence of Candida Albicans and Actinomyces, but specific cultures were all negative. The patient, however, was put under antifungal and antibiotic treatments without any improvement. During the screening time, bleeding from the nose and the oral cavity was accompanying the growing of the tumor. The patient suffered some episodes of severe anemia (hemoglobin concentration: 5–6 g/dL) that necessitated blood transfusion. The growth of the tumor toward the pharynx was so impressive (Fig. 3) that the patient showed rapidly increasing signs of respiratory discomfort and frequent episodes of coughing.
Figure 1.

Facial CT scan using contrast‐enhancing agent and showing an osteolytic tumor starting in the right maxillary sinus and measuring 60 × 57 × 55 mm.
Figure 2.

Facial MRI using gadolinium and showing the extension of the tumor to the orbit, the nasal fossa and the oral cavity and the destruction of the right lateral one‐third of the palate.
Figure 3.

The development of the tumor in the oral cavity and toward the pharynx. We can notice the swelling of the right cheek.
Considering the imminent risk of asphyxiation, the patient was admitted to the operating theater where he underwent an oral and pharyngeal tumor removal under local anesthesia. The specimen (Fig. 4) was then sent to the laboratory. The histological examination found necrosis, inflammatory tissue, and fabric fibers suggesting the presence of the remains of gauze (Gossypiboma; Fig. 5).
Figure 4.

The specimen after the tumor was removed from inside the oral cavity and the pharynx.
Figure 5.

Microscopique picture of the specimen showing a fabric fiber surrounded by inflammatory tissue.
The patient was then prepared for a second surgery under general anesthesia 2 weeks later. A right paranasal approach with a back cut in the right lower eyelid was performed. The infraorbital nerve was exposed and protected. The gossypiboma partially destroyed the anterior and the medial paranasal sinus bony walls. The floor of the sinus was completely destroyed, and only the orbital floor's periosteum was left intact. The complete removal of the tumor was performed using a submucoperiosteal dissection (Fig. 6A and B).
Figure 6.
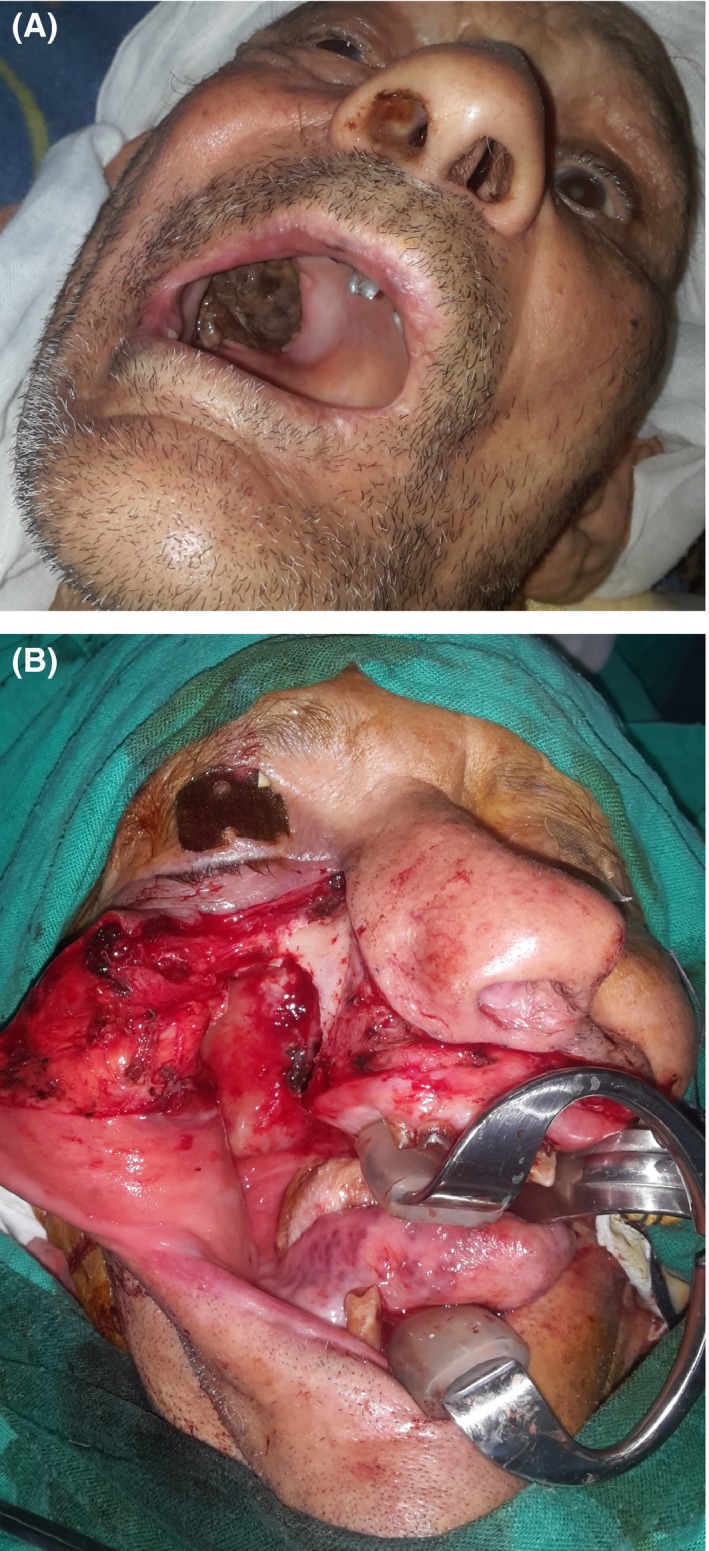
(A) Aspect before the second surgery. (B) Peroperative aspect of the surgical site after the gossypiboma was removed using a submucoperiosteal dissection of the maxillary sinus.
A trilayer reconstruction of the defect of the lateral one‐third of the hard palate was immediately performed using the following: a flap of the remaining nasal wall mucosa to create the upper layer (sinusal floor mucosa), a flap of the buccal fat pad to create the intermediate layer, and a mucosal cheek flap harvested above the level of the parotid duct to create the lower layer (palatal mucosa; Fig. 7A–E).
Figure 7.

(A) The remaining nasal mucosa was used to create a new upper layer for the palate. The buccal fat pad is dissected. (B) The buccal fat pad was flattened and spread under the new sinus floor mucosa. (C) A mucosal flap was harvested from the cheek above the level of the Stensen's duct to form the oral roof mucosa. Transfixing sutures ensure the good contact between the three layers. (D) Final external aspect with the tumor that has been removed. (E) Continuous sutures ensure a good contact of the oral cavity roof mucosa (picture taken 3 days after the surgery).
Saline solution spray was indicated for nasal and sinusal cleaning. Nose blowing was prohibited for 15 days. The immediate follow‐up was uneventful, and the patient was discharged 5 days after surgery.
A monthly follow‐up was scheduled, including clinical examinations and plain X‐rays. No complication was noticed.
Six months after the surgery, the oral cavity's roof is still completely closed (Fig. 8A and B). An MRI showed clear right paranasal sinus and nasal fossa with a large communication between them. There are no signs of recurrence. There is still persistent thickening of the sphenoidal sinus mucosa (Fig. 9).
Figure 8.

(A) External aspect 6 months after surgery: The right eye ball which was deported upward is returning to its normal position. (B) Oral view of the palate: 6 months after the surgery, the palate is still completely closed.
Figure 9.

Facial MRI performed 6 months after the surgery and showing empty right sinus and nasal fossa. A thickening of the sphenoid sinus mucosa is remaining.
Discussion and Conclusions
Using the keywords “gossypiboma” and “paranasal sinuses,” only five case reports were found on PubMed. They are listed in the reference section of this article 1, 2, 3, 4, 5. All the patients whose cases were reported in those articles had undergone surgery on the maxilla prior to the appearance of the symptoms: Three of them benefitted from a Caldwell–Luc approach, one underwent a tooth extraction and the last one benefitted from a cyst enucleation of the maxilla using an unknown approach. One of the peculiarities of the case presented in the current paper is that the patient doesn't recall any surgery on his maxilla. The authors see three possibilities for fabric fibers to be located inside the patient's maxillary sinus: 1/Some gauze or cotton sponge may have been forgotten during the skin surgery the patient underwent eleven years ago, or 2/As the patient is edentulous, a gauze may have been left after a tooth extraction, or at last 3/Some fabric fibers may have passed from the nasal fossa to the sinus during a forced nasal packing. Although these three possibilities are very improbable, there are no other elements in the patient's history that can explain the presence of fabric fibers inside his paranasal sinus. A tooth extraction that could have caused an oroantral communication should have shown clinical expressions soon after its occurrence and the patient should have remembered infectious episodes of the extraction site. It is also very unlikely that a blunt foreign body‐like gauze or cotton deepened through the skin toward the sinus and passed through the bone instead of reaching the surface of the skin or infecting it and leaving a fistula. Finally, it is uncommon for a foreign body to pass from the nasal fossa to the ipsilateral maxillary sinus in a reversed way. A case report showed that foreign bodies in the paranasal sinus are also subject to the mucociliary action that conveys mucus centripetally toward the primary ostium 6.
Another peculiarity of this case is that the gossypiboma mimicked a malignant tumor in its radiological features and in its clinical behavior: Osteolysis, massive bleeding, and rapid spreading especially after each biopsy. Discussions took place between Oral and Maxillofacial surgeons, ENT surgeons, and Oncology staff to establish a way to clear up the matter. Eventually, the fact that the tumor threatened the airway by surging toward the pharynx urged the first author to remove the oral portion of it. The histological analysis of this big portion of the tumor established the diagnosis and decided for the next steps to undertake.
Almost one‐third of the hard palate was destroyed by the expansion of the tumor. The fact that the patient is edentulous made a prosthetic solution difficult. The surgical repair of the hard palate was then indicated. It was conducted in a very simple manner. A trilayer reconstruction was performed using three locoregional flaps to ensure a tension‐free closure and thus to lower the risk of fistula. Pedicled buccal fat pads are frequently reported in the reconstruction of oral defects. They show rapid epithelialization when used alone and were reported to cover defects of the maxilla up to 6 cm long 7. The first author of this article believes the buccal fat pad is the key of this reconstruction thanks to its good blood supply. It played the role of a reliable support for the mucosal flaps that were harvested. Finally, the trilayer reconstruction as described allowed for the repair to provide a solution close to the normal anatomy.
Authorship
AG: treated the patient and collected the patient's data and consent. MK: collected the references. AG and MK: discussed the diagnosis and wrote the paper.
Availability of Data and Material
All the information and proofs needed are available from the corresponding author on reasonable request.
Consent for Publication
The patient consents for his pictures and information to be published. A signed consent can be provided if requested.
Conflict of Interest
None declared.
Acknowledgment
The authors thank Prof. Fouad Kettani (Laboratoire d'Anatomie Pathologique Nations Unies, Rabat, Morocco) for providing the microscopic picture used as Figure 5 and Dr. Bradley Fisher (Department of Oral and Maxillofacial Surgery, Dalhousie University, Halifax NS, Canada) for his help in editing the paper.
Clinical Case Reports 2018; 6(1): 71–77
References
- 1. Kim, K. S. 2014. Changes in computed tomographyfindings according to the chronicity of maxillary sinus gossypiboma. J. Craniofac. Surg. 25:e330–e333. [DOI] [PubMed] [Google Scholar]
- 2. Alves‐de‐Oliveira, C. N. , Pimenta‐do‐Amaral T. M., Ribeiro‐Souto G., and Alves‐Mesquita R.. 2014. Gossypiboma in the oral region: Case report and literature review. J. Clin. Exp. Dent. 6:e444–e447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pons, Y. , and Schouman T.. 2010. Maxillary sinus textiloma: a case report. J. Med. Case Rep. 4:288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mohanavalli, S. , David J. J., and Gnanam A.. 2011. Rare foreign bodies in oro‐facial regions. Indian J. Dent. Res. 22:713–715. [DOI] [PubMed] [Google Scholar]
- 5. Pekanan, P. , Wichiwaniwate P., and Thanomkiat W.. 1996. Retained gauze in the sinonasal cavities: plain film and CT findings. Neuroradiology 38:381–382. [DOI] [PubMed] [Google Scholar]
- 6. Pang, K. P. , Siow J. K., and Tan H. M.. 2005. Migration of a foreign body in the maxillary sinus illustrating natural mucociliary action. Med. J. Malaysia 60:523–525. [PubMed] [Google Scholar]
- 7. Jain, M. K. , Ramesh C., Sankar K., and Lokesh Babu K. T.. 2012. Pedicled buccal fat pad in the management of oroantral fistula: a clinical study of 15 cases. Int. J. Oral Maxillofac. Surg. 41:1025–1029. [DOI] [PubMed] [Google Scholar]


