Abstract
Skeletal surveys (SSs) have been identified as a key component of the evaluation for suspected abuse in young children, but variability in SS utilization has been reported. Thus, we aimed to describe the utilization patterns, yield, and risks of obtaining SS in young children through a systematic literature review. We searched PubMed/MEDLINE and CINAHL databases for articles published between 1990 and 2016 on SS. We calculated study-specific percentages of SS utilization and detection of occult fractures and examined the likelihoods that patient characteristics predict SS utilization and detection of occult fractures. Data from 32 articles represents 64,983 children < 60 months old. SS utilization was high (85%–100%) in studies of infants evaluated by a child protection team for suspected abuse and/or diagnosed with abuse except in one study of primarily non-pediatric hospitals. Greater variability in SS utilization was observed across studies that included all infants with specific injuries, such as femur fractures (0%-77%), significant head injury (51%-82%), and skull fractures (41%-86%). Minority children and children without private insurance were evaluated with SS more often than white children and children with private insurance despite lack of evidence to support this practice. Among children undergoing SS, occult fractures were frequently detected among infants with significant head injury (23%-34%) and long bone fractures (30%) but were less common in infants with skull fractures (1%-6%). These findings underscore the need for interventions to decrease disparities in SS utilization and standardize SS utilization in infants at high risk of having occult fractures.
Keywords: skeletal survey, systematic review, child abuse, occult injury, fracture
The skeletal survey (SS), a series of radiographs of the entire body, is a key component of the evaluation of suspected physical abuse, as it can identify occult fractures. Identification of occult fractures characteristic of inflicted trauma can confirm concerns for abuse and enable protection of the child from further harm. In addition, dating the fractures can sometimes help determine the timing of the abuse. For these reasons, the American Academy of Pediatrics (AAP; 1991) published a policy in 1991 recommending that clinicians perform a SS in all cases of suspected physical abuse in children < 2 years old and on a case-by-case basis for children 2 to 5 years old. The AAP (2000; 2009; (Christian & Committee on Child Abuse and Neglect, 2015)) reaffirmed their SS recommendations in 2000, 2009 and 2015. Since 1997, the American College of Radiology (ACR) and The Society for Pediatric Radiology (2006; 2011; 2014; 2016) have also published practice parameters recommending that SSs be performed in infants and young children who are suspected victims of abuse. However, in clinical practice, determining which young, injured children warrant evaluation for suspected abuse and a SS can be challenging.
As a result, disparities by race and socioeconomic status as well as variation across high-risk groups in SS performance in young, injured children have been described (Higginbotham et al., 2014; Lane, Rubin, Monteith, & Christian, 2002; Lindberg, Beaty, Juarez-Colunga, Wood, & Runyan, 2015; Rangel et al., 2009; Wood et al., 2012). These disparities and variation in SS performance may contribute to missed opportunities to diagnose abuse and protect children from further harm. Retrospective studies suggest that between 13% and 39% of young children with abusive injuries had missed opportunities for diagnosis of abuse, and as a result, 17-28% of these children suffered additional injuries from ongoing abuse (Jenny, Hymel, Ritzen, Reinert, & Hay, 1999; Oral, Blum, & Johnson, 2003; Oral, Yagmur, Nashelsky, Turkmen, & Kirby, 2008; Pierce et al., 2008; Ravichandiran et al., 2010; Thorpe, Zuckerbraun, Wolford, & Berger, 2014). To inform the development of interventions aimed at decreasing these disparities, increasing appropriate use of SS, and ensuring timely and accurate diagnosis of abuse, we sought to answer the following questions: To what extent are there variation and disparities in which young, injured children are evaluated with SS, and in what subpopulations are SS evaluations appropriate? A better understanding of the current utilization, benefits, and risks of obtaining SS in the evaluation of young, injured children is important for understanding the gaps in current practice and determining appropriate use of SS (as determined by the benefits and risks of SS in each subpopulation). Thus, we aimed to describe the utilization patterns (percentages of children who are evaluated), yield (percentages of children with occult fractures detected), and risks of obtaining SS in young, injured children through a systematic review of the literature.
Methods
Search Strategy
We performed a systematic review of the literature on the areas listed in our aims using a pre-specified protocol with inclusion and exclusion criteria (available upon request) and developed this article using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. We searched PubMed/MEDLINE and CINAHL databases for studies published in English between January 1990 and December 2016 using the search terms listed in Appendix 1. Studies were also identified by reviewing reference lists of articles identified during the search.
Study Selection
We included observational studies (including cross sectional and cohort, prospective and retrospective), but excluded surveys, reviews, editorials, textbooks, and unpublished literature. Studies were included if the majority of subjects were ≤ 60 months old or if the data for the subset of children ≤ 60 months old could be extracted. We chose a cutoff age of 60 months, since SSs are not recommended for children older than 60 months (5 years). Studies including fewer than 5 children ≤ 60 months old evaluated with SS were excluded, as such a small sample size would provide unstable study-specific estimates. Titles and abstracts of studies were screened by one of four reviewers (CP, JW, MG, or KK), and non-relevant studies were eliminated (see Figure 1). Full articles for relevant studies were assessed for eligibility by two reviewers (CP, JW) in an unblinded, standardized manner, with disagreements resolved by consensus.
Figure 1.
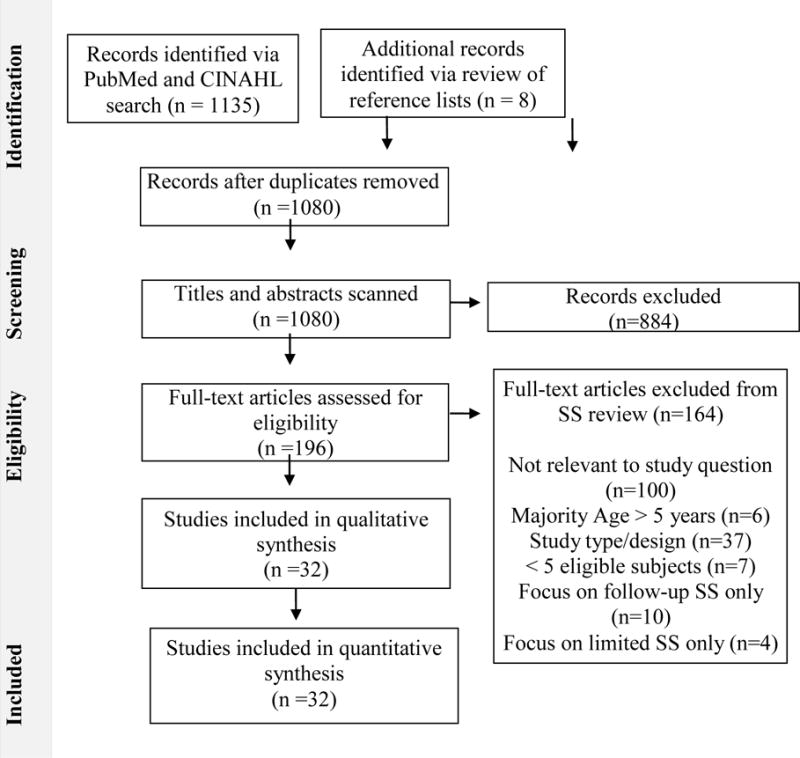
Flow of study identification, screening, eligibility assessment and inclusion. Although some studies could have been excluded for multiple reasons, each study is only listed once in the list of reasons for exclusion. Excluded study types/designs included reviews, editorials, and case reports.
Data Extraction, Assessment of Methodological Quality, and Analysis
Two reviewers (CP, JW) independently identified potential sources of bias and extracted the following information using a standardized form: 1) study population characteristics (ages, injury presentations, sample size, study location, and dates), 2) inclusion and exclusion criteria for subjects, 3) imaging methods and interpretation, 4) number of subjects who were evaluated with SS and who had positive SSs (occult fracture(s) detected on initial SS, and in some cases a composite of the findings of both initial and follow-up SS), and 5) risks of SS. In addition, the reviewers contacted the authors of publications for additional information as needed. The reviewers independently categorized the overall study methodology as A, B, or C using the rating presented in Table 1.
Table 1.
Study Methodology Rating Scale
| A | Prospective study |
| B | Retrospective data analysis with clearly defined sources/criteria |
| C | Retrospective data analysis with unclear sources/criteria |
Note. This scale was adapted from a previously published scale (Paine, Fakeye, Christian, & Wood, 2016).
The two reviewers evaluated risk of bias by assessing whether 1) the study population was representative of the general population of children ≤ 60 months old who were evaluated with SS of the age group and/or injury type specified in the study (selection bias) and 2) the selection criteria used were clearly presented in the article (reporting bias). Disagreements between reviewers were resolved through discussion and consensus.
The percentage of subjects who were evaluated with an initial SS and percentage of subjects undergoing an initial SS who had occult fractures detected were calculated with 95% confidence intervals (CIs) for each relevant study. The study-specific positive likelihood and negative likelihood ratios for the associations of demographic and clinical characteristics with SS performance and detection of occult fractures were also computed. Likelihood ratios report the likelihood of an outcome based on the sensitivity and specificity of the test. We reported the likelihood of SS utilization and likelihood of a positive SS if the characteristic was present (LR+) and if the characteristic was absent (LR−). Formulae described by Simel, Samsa, and Matchar (1991) were applied to calculate 95% CIs for likelihood ratios. All analyses were performed using Stata 12 (StataCorp, College Station, TX). We chose not to perform a meta-analysis due to the heterogeneity of study populations and methodologies.
Results
Search Results
The database search and reference review identified 1,080 non-duplicate citations, of which 196 were deemed relevant after review of the titles and abstracts and 32 met inclusion criteria after review of the full article (see Figure 1). Of these, 10 provided data only on utilization, seven provided data only on yield, 12 provided data on both utilization and yield, and three provided data on risks. Although our study criteria included ages up to 60 months, the studies that met our inclusion and exclusion criteria included only ages up to 59 months. Details of the imaging methods and interpretation methods used were so scarcely described that we only presented and compared the imaging methods of the three radiation studies in Appendix C. Of the studies on utilization and yield of SS, two studies were prospective and were categorized as ‘A,’ 18 were categorized as ‘B,’ and nine were categorized as ‘C’ (see Appendix B). Of the radiation risk studies, one was categorized as ‘A,’ and two were categorized as ‘C’ (see Appendix C). Of the studies on utilization and yield of SS, 15 had representative study populations, and 15 had clear selection criteria.
Skeletal Survey Utilization
Description of studies
Data on SS utilization represents 62,226 children aged 0-59 months (see Appendix 2). The inclusion and exclusion criteria varied across studies, with 4 including all children with suspected or diagnosed with abuse (Belfer, Klein, & Orr, 2001; Hansen & Campbell, 2009; Hicks & Stolfi, 2007; Lindberg, Berger, Reynolds, Alwan, & Harper, 2014), 6 including children evaluated for suspected abuse with specific injuries or presentations (Carrim, Arbabi, & Long, 2012; Deye, Berger, & Lindberg, 2013; Ghahreman, Bhasin, Chaseling, Andrews, & Lang, 2005; Harper, Feldman, Sugar, Anderst, & Lindberg, 2014; Jackson et al., 2015; Lindberg et al., 2012), 10 including all children with specific injuries or presentations regardless of whether abuse was suspected (Anderst, 2008; Higginbotham et al., 2014; Hymel et al., 2015; Lane et al., 2002; Laskey, Stump, Hicks, & Smith, 2013; Lindberg et al., 2015; Rangel et al., 2009; Shelmerdine, Das, Ingram, & Negus, 2014; Wood et al., 2009; Wood et al., 2010), and 2 including some combination of these populations (Wood et al., 2012; Wood, French, et al., 2015). All 22 studies included infants, but the upper age limit ranged from 5 to 59 months.
Evaluation for suspected or diagnosed physical abuse: skeletal survey utilization among infants < 12 months old
In 4 studies that included all infants < 12 months old with any type of injury from suspected or diagnosed abuse at pediatric hospitals (see Figure 2A), the percentage who were evaluated with SS ranged from 85% to 99% (Hansen & Campbell, 2009; Hicks & Stolfi, 2007; Lindberg et al., 2014; Wood et al., 2012). A much lower percentage of infants diagnosed with abuse (58%) were evaluated with SS in a study of primarily non-pediatric hospitals (Wood, French, et al., 2015). Study-specific SS utilization percentages were also high in studies of infants with specific injuries referred to a child protection team (CPT) for evaluation of suspected or diagnosed abuse, including infants with retinal hemorrhages (100%; Carrim et al., 2012), skull fracture (94%; Deye et al., 2013), bruising (91% to 94%; Harper et al., 2014; Jackson et al., 2015), and burns (89%; Hicks & Stolfi, 2007).
Figure 2A.
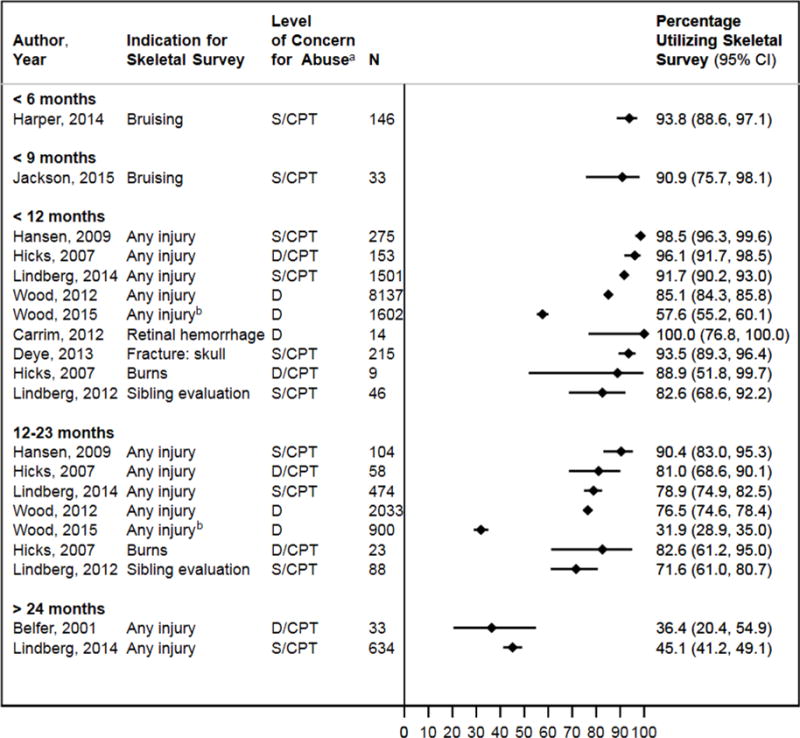
Skeletal Survey Utilization in Young Children Who Were Evaluated for and/or Diagnosed with Physical Abuse. Percentage of children who underwent skeletal survey, grouped by subject age. With the exception of the studies by Wood et al. (2012 and 2015) which used ICD-9-CM codes to identify children diagnosed with abuse, the study population of each study was children evaluated by a child protection team. Abbreviations: CI, confidence interval; N, sample size. a Abuse level of concern was categorized as “S” for suspected if all children undergoing skeletal survey for suspected abuse were included or was categorized as “D” for diagnosed if only children receiving a diagnosis of abuse were included. In addition, CPT indicates that only children referred to a child protection team were included. b Unlike other studies, the study population in Wood 2015 was evaluated primarily at non-pediatric hospitals.
Evaluation for suspected or diagnosed abuse: skeletal survey utilization among toddlers ≥ 12 months old
For children 12–23 months old with any type of injury from suspected or diagnosed abuse, SS utilization ranged from 77% to 90% in studies at pediatric centers (Hansen & Campbell, 2009; Hicks & Stolfi, 2007; Lindberg et al., 2014; Wood et al., 2012), but was only 32% in the study of primarily non-pediatric hospitals (see Figure 2A; Wood, French, et al., 2015). For children > 24 months old with suspected or diagnosed abuse at pediatric hospitals, SS utilization ranged from 36% to 45% (Belfer et al., 2001; Lindberg et al., 2014).
In 2 studies that did not break down the data by age groups, SS utilization ranged from 65% to 92% for children < 48 months old diagnosed with AHT (Belfer et al., 2001; Ghahreman et al., 2005) and was 79% for children < 48 months old with abusive fractures (Belfer et al., 2001).
Evaluation due to specific injuries for which abuse may or may not have been considered: skeletal survey utilization among infants <12 months old
Twelve studies provided SS utilization data for all children with specific presentations, regardless of whether abuse was suspected (see Figure 2B). For infants < 12 months old, SS utilization was lowest in infants with bruising, burns, or minor head injuries (13%-21%; Anderst, 2008; Lindberg et al., 2015) and highest in infants with significant head injuries treated at pediatric centers (59%-82%; Hymel et al., 2015; Lindberg et al., 2015; Rangel et al., 2009; Wood et al., 2012; Wood et al., 2010). In two studies of infants with any of type fracture, 11% and 60% were evaluated with SS (Higginbotham et al., 2014; Shelmerdine et al., 2014). SS utilization percentage for infants with long bone fractures, including humerus and femur fractures, ranged from 0% to 77% across studies (Lane et al., 2002; Lindberg et al., 2015; Shelmerdine et al., 2014; Wood et al., 2012; Wood, French, et al., 2015). In two studies of infants < 12 months old with skull fracture without associated intracranial hemorrhage, 41% of infants underwent SS, but in a third study at an institution with a protocol requiring SS performance in this population, 86% of infants ≤ 18 months old had a SS (Laskey et al., 2013; Lindberg et al., 2015; Wood et al., 2009).
Figure 2B.
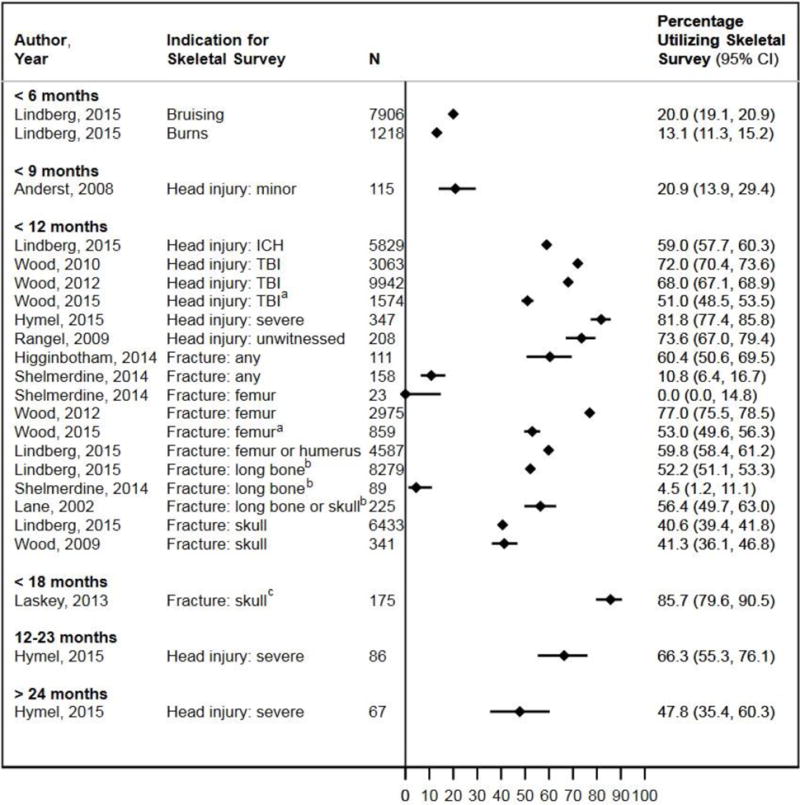
Skeletal Survey Utilization in All Young Children with Specific Injury Presentations. Percentage of children who underwent skeletal survey, grouped by injury type. Abbreviations: CI, confidence interval; ICH, intracranial hemorrhage; N, sample size; TBI, traumatic brain injury. a Evaluated primarily at non-pediatric hospitals. bLong bone was defined as femur, humerus, ulna, radius, tibia, and/or fibula. c The institutional protocol required skeletal survey performance in infants ≤ 18 months old with isolated skull fractures. Based on the data provided by the authors, we estimated that the SS utilization percentage for infants < 12 months old in this study would be between 89% and 95%.
Evaluation due to specific injuries for which abuse may or may not have been considered: skeletal survey utilization among toddlers ≥ 12 months old
Only one study provided data on SS utilization in injured children older than 12 months. In a study of children with severe head injury, SS utilization was 66% in children 12-23 months old and 48% in children 24-35 months old (see Figure 2B; Hymel et al., 2015).
Skeletal survey utilization among siblings and household contacts of physically abused children
In a single study that included data from 20 centers on siblings and other household contacts of physically abused children evaluated by CPTs, 83% of infants < 12 months old and 72% of children 12-23 months old were evaluated with SS (see Figure 2A; Lindberg et al., 2012).
Demographic characteristics associated with skeletal survey utilization
Younger age was associated with higher probability of SS evaluation in 6 of 7 studies comparing ages <12 months to 12–23 months (see Table 2; Hansen & Campbell, 2009; Hicks & Stolfi, 2007; Hymel et al., 2015; Lindberg et al., 2014; Lindberg et al., 2012; Wood et al., 2012; Wood, French, et al., 2015). Gender was not consistently associated with SS utilization (Anderst, 2008; Lindberg et al., 2012; Rangel et al., 2009; Wood et al., 2010). In 4 of 7 studies, children with public insurance or no insurance were more likely to undergo SS than children with private insurance (Anderst, 2008; Lane et al., 2002; Laskey et al., 2013; Lindberg et al., 2012; Rangel et al., 2009; Wood et al., 2009; Wood et al., 2010). In 2 of 3 studies that analyzed the relationship between insurance status and SS utilization in multivariate analyses (Lane et al., 2002; Wood et al., 2009; Wood et al., 2010), public or no insurance remained positively associated with SS utilization after controlling for age, race, and injury severity (Wood et al., 2009; Wood et al., 2010). In 5 of 6 studies, black or minority children were more likely to be evaluated for occult fractures than white children (Lane et al., 2002; Laskey et al., 2013; Lindberg et al., 2012; Rangel et al., 2009; Wood et al., 2009; Wood et al., 2010). In a study by Anderst (2008), Hispanic ethnicity was not associated with SS utilization. In a study by Higginbotham (2014) for which the raw data were unavailable, prior to implementation of a child abuse screening guideline, government insurance/uninsured status was associated with an increased odds of SS performance compared to the private insurance, but there were no differences by race.
Table 2.
Association of Demographic and Clinical Characteristics with Likelihood of Skeletal Survey Utilization
| Characteristics | Skeletal Survey Indication | Study | LR+ (95% CI)a | LR− (95% CI)a | pa |
|---|---|---|---|---|---|
| Age (months) | |||||
| 0-5 vs. 6-11 | Siblingsb | Lindberg, 2012 | 1.5 (0.6–3.9) | 0.7 (0.4–1.3) | 0.44 |
| 0-5 vs. 6-11 | Suspected abuse | Lindberg, 2014 | 1.2 (1.0–1.4) | 0.8 (0.6–1.0) | 0.037 |
| 0-5 vs. 6-11 | Fracture: isolated skull | Wood, 2009 | 0.9 (0.8–1.1) | 1.1 (0.9–1.4) | 0.41 |
| 0-6 vs. 7-11 | Head injury: ICH | Wood, 2010 | 1.0 (0.9–1.0) | 1.1 (0.9–1.2) | 0.28 |
| 0-11 vs. 12-23 | Suspected abuse | Hansen, 2009 | 2.6 (1.1–6.0) | 0.4 (0.2–0.5) | <0.001 |
| 0-11 vs. 12-23 | Diagnosed abuse | Hicks, 2007 | 2.1 (1.1–4.1) | 0.4 (0.2–0.6) | 0.001 |
| 0-11 vs. 12-23 | Head injury: severe | Hymel, 2015 | 1.2 (1.1–1.4) | 0.5 (0.4–0.8) | 0.002 |
| 0-11 vs. 12-23 | Siblingsb | Lindberg, 2012 | 1.6 (0.8–3.0) | 0.8 (0.6–1.1) | 0.21 |
| 0-11 vs. 12-23 | Suspected abuse | Lindberg, 2014 | 1.4 (1.3–1.6) | 0.5 (0.4–0.6) | <0.001 |
| 0-11 vs. 12-23 | Diagnosed abuse | Wood, 2012 | 1.1 (1.1–1.2) | 0.7 (0.6–0.7) | <0.001 |
| 0-11 vs. 12-23 | Diagnosed abuse | Wood, 2015 | 1.5 (1.4–1.5) | 0.5 (0.4–0.6) | <0.001 |
| 0-11 vs. 12-35 | Fracture: skull or long bone | Lane, 2002 | 1.4 (1.2–1.6) | 0.6 (0.5–0.8) | <0.001 |
| 12-23 vs. 24-35 | Head injury: severe | Hymel, 2015 | 1.4 (1.0–1.9) | 0.7 (0.5–0.9) | 0.021 |
| 12-23 vs. 24-35 | Suspected abuse | Lindberg, 2014 | 1.4 (1.2–1.6) | 0.7 (0.6–0.8) | <0.001 |
| Gender | |||||
| Male vs. female | Head injury: minor | Anderst, 2008 | 1.1 (0.8–1.4) | 0.9 (0.7–1.3) | 0.60 |
| Male vs. female | Siblingsb | Lindberg, 2012 | 1.5 (0.8–2.8) | 0.8 (0.6–1.1) | 0.19 |
| Male vs. female | Head injury: unwitnessed | Rangel, 2009 | 1.2 (0.9–1.6) | 0.8 (0.6–1.1) | 0.17 |
| Male vs. female | Head injury: ICH | Wood, 2010 | 0.9 (0.9–1.0) | 1.1 (1.0–1.2) | 0.012 |
| Insurancec | |||||
| Public/none vs. private insurance | Head injury: minor | Anderst, 2008 | 1.1 (0.9–1.3) | 0.9 (0.6–1.4) | 0.63 |
| Public/none vs. private insurance | Fracture: skull or long bone | Lane, 2002 | 1.6 (1.3–1.9) | 0.6 (0.4–0.7) | <0.001 |
| Public/none vs. private insurance | Fracture: isolated skull | Laskey, 2013 | 1.3 (0.9–2.0) | 0.6 (0.4–1.0) | 0.073 |
| Public/none vs. private insurance | Siblingsb | Lindberg, 2012 | 1.0 (0.9–1.1) | 1.7 (0.4–7.3) | 0.73 |
| Public/none vs. private insurance | Head injury: unwitnessed | Rangel, 2009 | 3.0 (1.8–4.8) | 0.4 (0.3–0.5) | <0.001 |
| Public/none vs. private insurance | Fracture: isolated skull | Wood, 2009 | 1.4 (1.1–1.8) | 0.7 (0.6–0.9) | 0.002 |
| Public/none vs. private insurance | Head injury: ICH | Wood, 2010 | 1.5 (1.4–1.6) | 0.4 (0.4–0.5) | <0.001 |
| Race/ethnicity | |||||
| Hispanic vs. non-Hispanic | Head injury: minor | Anderst, 2008 | 0.8 (0.7–1.1) | 1.4 (1.0–2.1) | 0.10 |
| Minority vs. white | Fracture: skull or long bone | Lane, 2002 | 2.0 (1.6–2.5) | 0.5 (0.4–0.6) | <0.001 |
| Minority vs. white | Fracture: isolated skull | Laskey, 2013 | 0.9 (0.4–1.9) | 1.0 (0.8–1.3) | 0.78 |
| Minority vs. white | Siblingsb | Lindberg, 2012 | 1.7 (1.0–2.8) | 0.7 (0.5–0.9) | 0.027 |
| Black vs. white | Head injury: unwitnessed | Rangel, 2009 | 3.4 (1.3–9.1) | 0.8 (0.7–0.9) | 0.006 |
| Black vs. white | Fracture: isolated skull | Wood, 2009 | 1.3 (1.0–1.8) | 0.8 (0.7–1.0) | 0.043 |
| Black vs. white | Head injury: ICH | Wood, 2010 | 2.0 (1.6–2.4) | 0.8 (0.7–0.8) | <0.001 |
| Type of Injury | |||||
| Burnsc vs. other | Diagnosed abuse | Hicks, 2007 | 0.5 (0.2–1.1) | 1.2 (0.9–1.7) | 0.15 |
| Bruisingd vs. other | Suspected abuse | Harper, 2014 | 1.2 (0.6–2.2) | 1.0 (0.9–1.1) | 0.73 |
| Head Injury Characteristics | |||||
| CT findings: positive vs. negative | Head injury: minor | Anderst, 2008 | 3.6 (2.6–4.9) | 0.4 (0.3–0.6) | <0.001 |
| Severe vs. mild/moderate | Head injury: ICH | Wood, 2010 | 1.6 (1.5–1.9) | 0.7 (0.7–0.8) | <0.001 |
| Severe vs. mild/moderate | Head injury: unwitnessed | Rangel, 2009 | 1.2 (0.9–1.7) | 0.8 (0.6–1.1) | 0.27 |
| Skull fracture: present vs. absent | Head injury: ICH | Wood, 2010 | 3.0 (2.7–3.4) | 0.4 (0.4–0.5) | <0.001 |
| Complex vs. simple skull fracture | Fracture: isolated skull | Wood, 2009 | 1.1 (0.9–1.5) | 0.9 (0.8–1.1) | 0.32 |
| Additional Injuries Present | |||||
| Yes vs. no | Fracture: isolated skull | Wood, 2009 | 6.4 (1.4–29.1) | 0.9 (0.9–1.0) | 0.009 |
| Yes vs. no | Head injury: ICH | Wood, 2010 | 2.7 (1.9–3.8) | 0.9 (0.9–1.0) | <0.001 |
| Red Flags on History | |||||
| Red flag for abusee: yes/no | Fracture: isolated skull Wood, 2009 | 3.4 (2.4–4.9) | 0.6 (0.5–0.7) | <0.001 | |
| Delay in seeking care ≥6 hours: yes/no | Head injury: minor | Anderst, 2008 | 3.0 (1.9–4.7) | 0.7 (0.6–0.9) | <0.001 |
| No history of trauma: yes/no | Head injury: minor | Anderst, 2008 | 6.2 (2.6–14.5) | 0.8 (0.7–1.0) | <0.001 |
| Hospital Clinical Guideline | |||||
| Present vs. none | Fracture: any | Higginbotham, 2014 | 1.7 (1.3–2.2) | 0.5 (0.4–0.6) | <0.001 |
| Present vs. none | Head injury: unwitnessed | Rangel, 2009 | 2.0 (1.0–4.2) | 0.9 (0.8–1.0) | 0.0495 |
Note. Abbreviations: CI, confidence interval; CT, computed tomography; LR, likelihood ratio; ICH, intracranial hemorrhage.
Calculated using a two-sided chi square test or, when a cell count was < 10, two-sided Fisher’s exact test. P value of 0.05 or less considered statistically significant.
Study included siblings and other household contacts of children diagnosed with physical abuse.
Injury was the primary reason for abuse consultation. All children were diagnosed with abuse.
Bruising was isolated. All children < 6 months old and were evaluated for suspected physical abuse.
Red flag for abuse was defined as delay in seeking care >72 hours, no history of trauma, changing or conflicting history, or past child protective services report.
Clinical characteristics associated with skeletal survey utilization
In 2 of 3 studies of children with head injuries, increased injury severity was associated with increased SS performance (see Table 2; Anderst, 2008; Rangel et al., 2009; Wood et al., 2010). The presence of “red flags” for abuse (e.g. delay in seeking care, unknown injury mechanism, etc.) in 2 studies (Anderst, 2008; Wood et al., 2009) and the finding of additional injuries on physical exam in 2 studies (Wood et al., 2009; Wood et al., 2010) were associated with increased SS utilization. Two studies assessed the impact of implementation of a local clinical SS guideline for infants with specific injuries and found statistically significant increases in SS use (Higginbotham et al., 2014; Rangel et al., 2009).
Yield of SS: Detection of Occult Fractures on Skeletal Survey
Description of studies
Data on frequencies of positive SS represents 6,459 children aged 0-59 months who were evaluated with SS (see Appendix 2). The inclusion and exclusion criteria varied, with 9 studies including all children evaluated for and/or diagnosed with abuse regardless of injury type or reason for presentation (Barber, Perez-Rossello, Wilson, & Kleinman, 2015; Barber, Perez-Rossello, Wilson, Silvera, & Kleinman, 2013; Belfer et al., 2001; Day, Clegg, McPhillips, & Mok, 2006; Duffy, Squires, Fromkin, & Berger, 2011; Hansen & Campbell, 2009; Hicks & Stolfi, 2007; Karmazyn, Lewis, Jennings, Hibbard, & Hicks, 2011; Lindberg et al., 2014), and 10 studies including only children with specific injuries or presentations who were evaluated for and/or diagnosed with abuse (Deye et al., 2013; Fagen, Shalaby-Rana, & Jackson, 2015; Ghahreman et al., 2005; Harper et al., 2014; Hymel et al., 2015; Laskey et al., 2013; Lindberg et al., 2012; Rangel et al., 2009; Ravichandiran et al., 2010; Wood et al., 2009). All 19 studies included infants 0-5 months old, but the upper age limit ranged from 5 to 59 months.
Detection of occult fractures on skeletal surveys performed in infants < 12 months old
In studies that presented data for infants < 12 months old with any type of presenting injury who underwent SS, occult fractures were detected in 13%-26% of infants evaluated for suspected abuse and 31% of infants diagnosed with abuse in one study (see Figure 3; Barber et al., 2015; Belfer et al., 2001; Day et al., 2006; Duffy et al., 2011; Hansen & Campbell, 2009; Hicks & Stolfi, 2007; Karmazyn et al., 2011; Lindberg et al., 2014). Among studies of infants with specific injuries evaluated for suspected abuse, occult fractures were frequently detected among infants with head injury (23%-34%; Barber et al., 2015; Hymel et al., 2015; Rangel et al., 2009), long bone fractures (30%; Barber et al., 2015), all types of abusive fracture (47%; Ravichandiran et al., 2010), or abusive burns (35%-38%; Fagen et al., 2015; Hicks & Stolfi, 2007) and were less common in the infants with skull fractures without significant intracranial hemorrhage (1%-6%; Deye et al., 2013; Laskey et al., 2013; Wood et al., 2009). For infant siblings of abused children evaluated with a SS, 17% to 34% had occult fractures (Barber et al., 2015; Lindberg et al., 2012).
Figure 3.
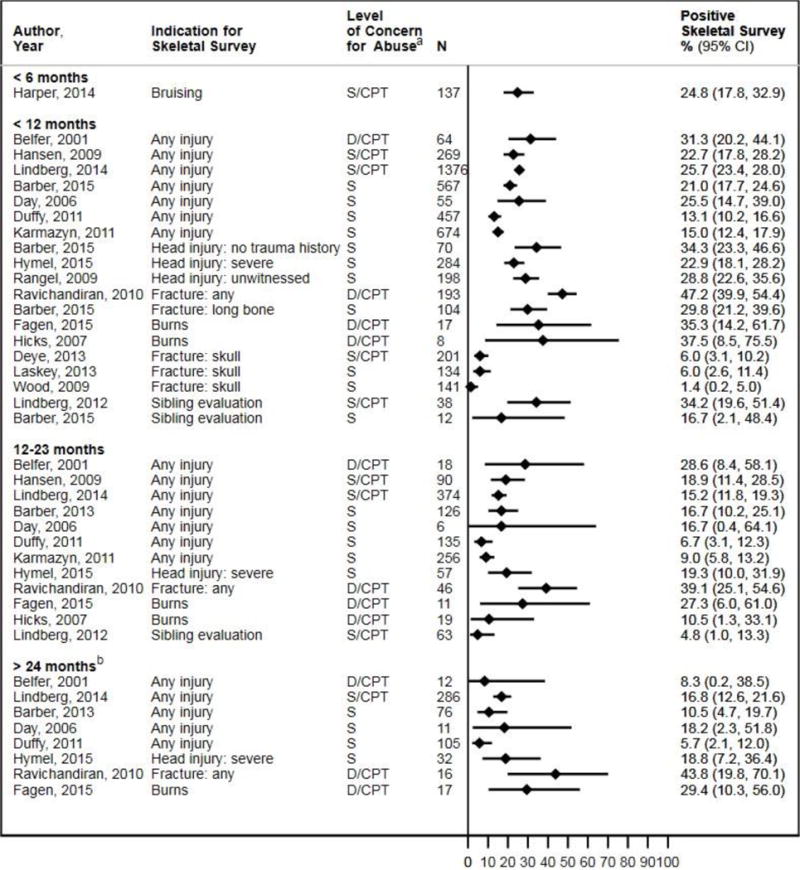
Percentage of Children with Positive Skeletal Survey by Age, Indication, and Level of Concern for Abuse. Percentage of children undergoing initial skeletal survey who had a positive skeletal survey (occult fracture(s) detected on skeletal survey), grouped by subject age. Abbreviations: CI, confidence interval; N, sample size. a Abuse level of concern was categorized as “S” for suspected if all children undergoing skeletal survey for suspected abuse were included or was categorized as “D” for diagnosed if only children receiving a diagnosis of abuse were included. In addition, CPT indicates that only children referred to a child protection team were included. b The upper limit of this age category varied across studies.
Detection of occult fractures on skeletal surveys performed in toddlers 12-23 months old
For studies that included all injuries and presentations in toddlers 12-23 months old, 7%-19% of toddlers with suspected abuse and 29% of toddlers with diagnosed abuse had positive SSs (see Figure 3; Barber et al., 2013; Belfer et al., 2001; Day et al., 2006; Duffy et al., 2011; Hansen & Campbell, 2009; Karmazyn et al., 2011; Lindberg et al., 2014). Among toddlers with severe head injury, an abusive fracture evaluated by a CPT, or abusive burns, 19% (Hymel et al., 2015), 39% (Ravichandiran et al., 2010), and 11-27% (Fagen et al., 2015; Hicks & Stolfi, 2007), respectively, had occult fractures. Among siblings of abused children evaluated by a CPT, 5% had occult fractures (Lindberg et al., 2012).
Detection of occult fractures on skeletal surveys performed in children ≥ 24 months old
For studies that included all injuries and presentations in children age ≥ 24 months, 6%-18% of those with suspected abuse and 8% of those diagnosed with abuse had occult fractures (see Figure 3; Barber et al., 2013; Belfer et al., 2001; Day et al., 2006; Duffy et al., 2011; Lindberg et al., 2014). Among children ≥ 24 months old with severe head injury, an abusive fracture evaluated by a CPT, or abusive burns, 19% (Hymel et al., 2015), 44% (Ravichandiran et al., 2010), and 29% (Fagen et al., 2015), respectively, had occult fractures.
Two additional studies provided data on positive SS percentages but did not break down the data by age groups. Among children < 48 months old evaluated by a CPT, 35% of those with AHT, 19% of those with abusive intracranial injury, 31% of those with abusive fractures, and 7% of those with abusive burns had occult fractures (Belfer et al., 2001; Ghahreman et al., 2005).
Demographic and clinical characteristics associated with positive skeletal survey
Infants < 6 months old were more likely to have occult fractures than infants 6 to 11 months old in 2 of 4 studies (see Table 3; Duffy et al., 2011; Laskey et al., 2013; Lindberg et al., 2014; Lindberg et al., 2012). Age < 12 months was associated with higher probability of positive SS in four of 12 studies (Barber et al., 2015; Barber et al., 2013; Belfer et al., 2001; Day et al., 2006; Duffy et al., 2011; Fagen et al., 2015; Hansen & Campbell, 2009; Hicks & Stolfi, 2007; Hymel et al., 2015; Karmazyn et al., 2011; Lindberg et al., 2014; Lindberg et al., 2012; Ravichandiran et al., 2010). Gender and race were not associated with likelihood of occult fractures in two studies (Day et al., 2006; Rangel et al., 2009). Infants with public or no insurance were more likely to have occult fractures than infants with private insurance in one study of infants with unwitnessed head injuries (Rangel et al., 2009). Lone bone fractures were associated with a higher likelihood of occult fractures than other injuries evaluated in one study (Barber et al., 2015). In two studies of infants with skull fractures, the complexity of the skull fracture did not affect likelihood of occult fractures, but the presence of “red flags” for abuse was associated with increased likelihood for occult fractures in one of the studies (Deye et al., 2013; Laskey et al., 2013).
Table 3.
Association of Demographic and Clinical Characteristics with Likelihood of Positive Skeletal Survey
| Characteristics | Skeletal Survey Indication | Study | LR+ (95% CI)a | LR− (95% CI)a | pa |
|---|---|---|---|---|---|
| Age (months) | |||||
| 0–5 vs. 6–11 | Suspected abuse | Duffy, 2011 | 1.3 (1.1–1.5) | 0.5 (0.3–0.9) | 0.005 |
| 0–5 vs. 6–11 | Siblingsb | Lindberg, 2012 | 1.3 (0.8–2.2) | 0.6 (0.3–1.6) | 0.49 |
| 0–5 vs. 6–11 | Suspected abuse | Lindberg, 2014 | 1.1 (1.0–1.2) | 0.8 (0.7–1.0) | 0.020 |
| 0–5 vs. 6–11 | Fracture: isolated skull | Laskey, 2013 | 1.5 (1.3–1.7) | 0.0 (NA) | 0.11 |
| 0–11 vs. 12–23 | Suspected abuse | Barber, 2013/2015c | 1.0 (1.0–1.1) | 0.8 (0.5–1.3) | 0.31 |
| 0–11 vs. 12–23 | Diagnosed abuse | Belfer, 2001 | 1.0 (0.8–1.3) | 0.9 (0.3–2.6) | 1.00 |
| 0–11 vs. 12–23 | Suspected abuse | Day, 2006 | 1.1 (0.9–1.3) | 0.6 (0.1–4.6) | 1.00 |
| 0–11 vs. 12–23 | Suspected abuse | Duffy, 2011 | 1.1 (1.0–1.3) | 0.5 (0.3–1.0) | 0.046 |
| 0–11 vs. 12–23 | Abusive burns | Fagen, 2015 | 1.2 (0.6–2.1) | 0.8 (0.3–2.3) | 1.00 |
| 0–11 vs. 12–23 | Suspected abuse | Hansen, 2009 | 1.1 (0.9–1.2) | 0.8 (0.5–1.3) | 0.45 |
| 0–11 vs. 12–23 | Abusive burns | Hicks, 2007 | 2.6 (0.9–7.6) | 0.5 (0.2–1.6) | 0.14 |
| 0–11 vs. 12–23 | Head injury: | Hymel, 2015 | 1.0 (0.9–1.2) | 0.8 (0.5–1.5) | 0.55 |
| 0–11 vs. 12–23 | Suspected abuse | Karmazyn, 2011 | 1.1 (1.0–1.3) | 0.6 (0.4–0.9) | 0.016 |
| 0–11 vs. 12–23 | Siblingsb | Lindberg, 2012 | 2.8 (1.8–4.1) | 0.3 (0.1–0.7) | <0.001 |
| 0–11 vs. 12–23 | Suspected abuse | Lindberg, 2014 | 1.1 (1.1–1.2) | 0.6 (0.5–0.8) | <0.001 |
| 0–11 vs. 12–23 | Fracture: abusive | Ravichandiran, 2010 | 1.1 (0.9–1.2) | 0.8 (0.4–1.3) | 0.33 |
| 12–23 vs. 24–35 | Suspected abuse | Day, 2006 | 1.0 (0.2–4.6) | 1.0 (0.2–4.6) | 1.00 |
| 12–23 vs. 24–35 | Head injury: severe | Hymel, 2015 | 1.0 (0.7–1.5) | 1.0 (0.5–2.0) | 1.00 |
| 12–23 vs. 24–35 | Suspected abuse | Lindberg, 2014 | 1.0 (0.8–1.2) | 1.0 (0.8–1.4) | 0.82 |
| 12–23 vs. 24–35 | Fracture: abusive | Ravichandiran, 2010 | 1.0 (0.7–1.3) | 1.2 (0.5–2.7) | 0.77 |
| 12–23 vs. 24–48 | Suspected abuse | Barber, 2013/2015c | 1.2 (0.9–1.6) | 0.7 (0.4–1.3) | 0.29 |
| 12–23 vs. 24–48 | Diagnosed abuse | Belfer, 2001 | 1.7 (0.9–3.1) | 0.4 (0.1–2.3) | 0.33 |
| 12–23 vs. 24–59 | Suspected abuse | Duffy, 2011 | 1.1 (0.7–1.6) | 0.9 (0.5–1.7) | 0.80 |
| 12–23 vs. 24–59 | Abusive burns | Fagen, 2015 | 0.9 (0.3–2.7) | 1.0 (0.5–2.0) | 1.00 |
| Gender | |||||
| Male vs. female | Suspected abuse | Day, 2006 | 1.1 (0.7–1.9) | 0.9 (0.5–1.6) | 0.78 |
| Male vs. female | Head injury: unwitnessed | Rangel, 2009 | 1.0 (0.8–1.2) | 1.1 (0.7–1.5) | 0.79 |
| Insurance | |||||
| Public/none vs. private insurance | Head injury: unwitnessed | Rangel, 2009 | 1.4 (1.2–1.6) | 0.4 (0.2–0.7) | 0.001 |
| Race/ethnicity | |||||
| Black vs. white | Head injury: unwitnessed | Rangel, 2009 | 0.8 (0.4–1.4) | 1.1 (0.9–1.3) | 0.39 |
| Injury Typed | |||||
| Fracture (non-skull) vs. other | Suspected abuse | Barber, 2015 | 1.5 (1.1–2.1) | 0.8 (0.7–1.0) | 0.02 |
| Long bone fracture vs. othere | Suspected abuse | Barber, 2015 | 1.8 (1.3–2.5) | 0.8 (0.7–0.9) | 0.002 |
| Bruisingf vs. other | Suspected abuse | Harper, 2014 | 0.9 (0.6–1.2) | 1.0 (1.0–1.1) | 0.39 |
| Burns vs. other | Diagnosed abuse | Hicks, 2007 | 0.7 (0.3–1.8) | 1.0 (0.9–1.2) | 0.63 |
| Head Injury Characteristics | |||||
| Complex vs. simple skull fracture | Isolated skull fracture | Deye, 2013 | 0.6 (0.2–2.2) | 1.1 (0.9–1.5) | 0.74 |
| Complex vs. simple skull fracture | Isolated skull fracture | Laskey, 2013 | 0.6 (0.1–4.1) | 1.1 (0.8–1.4) | 1.00 |
| Severe vs. mild/moderate | Head injury: unwitnessed | Rangel, 2009 | 1.7 (1.3–2.1) | 0.5 (0.3–0.8) | <0.001 |
| Red Flags on History | |||||
| Red flag for abuseg: yes/no | Isolated skull fracture | Laskey, 2013 | 2.4 (1.6–3.6) | 0.3 (0.1–1.1) | 0.01 |
Note. Abbreviations: CI, confidence interval; LR, likelihood ratio.
Calculated using a two-sided chi square test or, when a cell count was < 10, two-sided Fisher’s exact test. P value of 0.05 or less considered statistically significant.
Study included siblings and other household contacts of children diagnosed with physical abuse.
Data presented in Barber, 2013 and Barber, 2015 were combined in this analysis, as they are for different age groups of the same study population and use the same definition of positive SS.
Injuries were not isolated, and children may have had > 1 presentation for which they underwent SS unless otherwise noted.
Children who had their initial SS performed at an institution other than the study institution were excluded from this analysis.
Bruising was not accompanied by other injuries. All children were < 6 months old.
Red flag for abuse is defined as no history of trauma, changing or conflicting histories, delay in care > 72 hours, prior CPS history, and/or additional injuries concerning for abuse.
Risks of Skeletal Survey: Radiation Exposure
Only radiation exposure was described as a risk of SS (see Appendix 5; Berger, Panigrahy, Gottschalk, & Sheetz, 2016; Drubach et al., 2010; Jha et al., 2013). In one study, at least 21 images were obtained from each patient evaluated with SS, including oblique views of the ribs (Drubach et al., 2010). The authors estimated the effective radiation doses for their standard and high-detail SSs range from 0.15 to 0.45 mSv for a 9-kg patient. In the second study, Jha et al. (2013) reported that the subset of patients representative of the cohort aged 0-24 months had 12-18 images performed and were exposed to 0.729 to 4.842 mGy cm2 (dose-area product) of radiation but did not state what standard equipment settings were used. In the third study, Berger et al. (2016) measured the effective radiation dose of a 15-view SS to be 0.2 mSv in a simulation using a neonatal phantom, Monte Carlo software, and digital radiography. Other risks of SS were not reported.
Discussion
Summary of Results and Implications
Skeletal survey utilization among children evaluated for abuse
Our systematic review identified 32 studies describing the utilization, yield, and radiation risks of SS in young children. In keeping with the AAP and ACR guidelines, all but one study reported high percentages of SS performance among children less than 2 years old who were referred to a CPT team for evaluation of suspected abuse and/or received a diagnosis of physical abuse. In these studies, SSs were performed in 85%-100% of infants and 77%-90% of one-year-olds evaluated for suspected or diagnosed abuse (Carrim et al., 2012; Deye et al., 2013; Hansen & Campbell, 2009; Hicks & Stolfi, 2007; Lindberg et al., 2014; Wood et al., 2012). Notably, the majority of the studies were conducted at pediatric institutions. The single study reporting low percentages of SSs performance among children receiving a diagnosis of abuse (58% in infants and 32% in one-year-olds) used data from a cohort of primarily non-pediatric hospitals (Wood, French, et al., 2015). These findings suggest that although compliance with national recommendations to perform a SS in children < 2 years old with suspected or diagnosed abuse is generally high at pediatric institutions, there is a great need for improvement in some non-pediatric centers.
Skeletal survey utilization among children with specific injuries
In contrast to the overall high percentages of SS performance among infants and young toddlers with an identified concern for abuse, striking variation in percentages of SS performance was observed across studies that included all children presenting with specific injuries, including fractures and head injuries. Study-specific percentages of SS performance ranged from 0%-77% for infants with femur fractures (Lindberg et al., 2015; Shelmerdine et al., 2014; Wood et al., 2012; Wood, French, et al., 2015), 5%-56% for infants with all types of long bone fractures (Lane et al., 2002; Lindberg et al., 2015; Shelmerdine et al., 2014), and 41%-86% for infants with skull fractures (Laskey et al., 2013; Lindberg et al., 2015; Wood et al., 2009). Among infants with significant head injuries, study-specific percentages of SS performance ranged of 51%-82% (Lindberg et al., 2015; Rangel et al., 2009; Wood et al., 2012; Wood, French, et al., 2015; Wood et al., 2010). These results highlight the variability that exists in the approach to evaluation for possible abuse in young, injured children. The low percentage of infants with significant head injury (such as traumatic brain injury) and/or long bone fractures evaluated with SS in some studies raises concern for under-evaluation and missed opportunities to diagnose abuse.
Demographic characteristics associated with skeletal survey utilization and yield
Our review also demonstrated that black children and children with public or no insurance were evaluated with SS more often than white infants and infants with private insurance, respectively (Higginbotham et al., 2014; Lane et al., 2002; Lindberg et al., 2012; Rangel et al., 2009; Wood et al., 2009; Wood et al., 2010). However, black infants had similar likelihood of having a positive SS compared to white infants (Rangel et al., 2009). Poverty, associated with public or no insurance, is a well-known risk factor for child maltreatment (Cancian, Slack, & Yang, 2010; Eckenrode, Smith, McCarthy, & Dineen, 2014); however, basing decisions regarding SS utilization on socioeconomic status is unethical and may lead to both over-evaluation in some populations as well as under-evaluation in other populations. These findings support Lane and Dubowitz’s 2007 study that demonstrated through a survey of orthopedists that subjective biases influenced their decisions to evaluate for and report child abuse.
All of the studies identified in this review included infants. Because the upper age limit varied, less information was available on the utilization and yield of SS in children over age 12 months and, in particular, children over 24 months of age. A relationship between younger age and increased likelihood of a positive SS was observed in only four of the 12 studies. Despite the inconsistency, this relationship is noteworthy considering that SS was used more selectively in older children than in younger children. Of the studies with statistically significant likelihood ratios, all demonstrated decreased SS yield with increased age.
Skeletal survey yield
The yield of the SSs was high across studies, with occult fractures revealed in 13%-26% of infants and in 7%-19% of children 12 to 23 months old with any injury presentation undergoing a SS for suspected abuse (Barber et al., 2015; Barber et al., 2013; Day et al., 2006; Duffy et al., 2011; Hansen & Campbell, 2009; Karmazyn et al., 2011; Lindberg et al., 2014). The observed high yield of the SSs supports the AAP and ACR recommendations for performing SS in children less than 2 years old with concerns for physical abuse. An even higher percentage of SSs were positive in studies focusing on suspected abuse in infants with fractures (47%; Ravichandiran et al., 2010), including long bone fractures (30%; Barber et al., 2015), and significant head injuries (23%-34%; Barber et al., 2015; Hymel et al., 2015; Rangel et al., 2009). The increased yield among infants with fractures and infants with significant head injuries suggests that these are high-risk populations for which a more standardized approach to SS performance may be warranted. The lowest yield of SS with only 1%-6% revealing occult fractures was observed in infants with skull fractures without associated significant intracranial hemorrhage (Deye et al., 2013; Laskey et al., 2013; Wood et al., 2009). A 6% yield of occult fractures is not insignificant and may be sufficient to justify SS in this population. However, a more targeted approach to SS utilization in this population could also be considered.
Skeletal survey risks
Radiation exposure was the only risk of SS identified in the literature review, with three studies providing information on it. The ACR placed SS in the same radiation level category as head computed tomography with a pediatric effective dose of range of 0.3-3 mSv (American College of Radiology & The Society for Pediatric Radiology, 2016). This dose has been estimated to place children < 5 years old at a 2 in 10,000 lifetime risk of developing leukemia (Miglioretti et al., 2013), although this risk may be overestimated (Journy et al., 2015; Slovis, Strouse, & Strauss, 2015). The studies identified in this review reported a lower range of 0.15-0.45 mSv for the radiation effective dose of a SS (Berger et al., 2016; Drubach et al., 2010). Thus, the radiation risk of SS is low and should not prevent clinicians from ordering a SS for a patient with a high risk of occult fractures from abuse.
Future Directions
Implementation of injury- and age-specific abuse evaluation clinical pathways is one proven strategy for addressing the observed disparities and variation in SS utilization and increasing appropriate SS utilization, as demonstrated by two studies (Higginbotham et al., 2014; Rangel et al., 2009). While it is acknowledged that increased SS utilization could lead to decreased yield, the study that measured yield demonstrated that the yield remained the same even though utilization had increased (Rangel et al., 2009), suggesting that the institution may be identifying more children with occult fractures. In addition, evidence-based implementation methods, such as decision support tools, may further increase success of the clinical guidelines (Prior, Guerin, & Grimmer-Somers, 2008). Results from this literature review inform the development of such pathways. Despite recent publication of evidence-informed SS guidelines for children < 2 years old with fractures, bruises, or intracranial hemorrhage (Paine, Scribano, Localio, & Wood, 2016; Wood et al., 2014; Wood, Fakeye, et al., 2015), question and controversy regarding the content of child abuse pathways remain. Thus, there is a need for more hospitals to implement and evaluate evidence-informed SS guidelines to standardize SS utilization, determine the optimal guidelines for various populations, and ultimately decrease the number of missed cases of abuse.
Limitations
This review has several limitations. First, most of the included studies were retrospective and, as a result, subjects were not clinically evaluated in a consistent manner (e.g., various numbers of radiographs were performed), possibly contributing to detection bias in yield. The variation in SS utilization percentages across studies, age groups, and injury groups may have influenced the occult fracture percentages, since centers that only evaluated the highest-risk populations with SS would be more likely to detect occult fractures than centers that had a lower threshold for ordering SS. Second, the inclusion and exclusion criteria and ascertainment methods varied across studies and injury groups. For example, among studies that included children evaluated for suspected abuse, some included all children evaluated for suspected abuse while others included only children evaluated by a CPT. Third, many studies had small sample sizes, limiting their power to detect differences in the characteristics of children evaluated with SS and diagnosed with occult fractures. Fourth, many of the studies presented data on children with multiple injury presentations, which may create bias when comparing injuries and their associations with occult fractures. For studies that included children with multiple injury presentations, we performed calculations on injury type only for those whose primary reason for obtaining a SS was presented. In addition, injury categories were not always consistently defined across studies, making it difficult to compare certain populations. Lastly, nine studies introduced selection bias and nine studies introduced reporting bias which may have influenced the results.
Conclusion
This review highlights the need for improved standardization of SS utilization in young children with injuries in order to increase SS utilization in infants with high-risk injuries, such as long bone fractures and unwitnessed or severe head injuries, and decrease racial and socioeconomic disparities in SS utilization. Implementation of injury- and age-specific SS guidelines hold promise for achieving these goals. Further study on the effectiveness and any unintended consequences of SS guideline implementation is needed. Our review also reveals a need for improved standardization in reporting the methods and results of studies evaluating SS utilization and yield. Studies should clearly report how SSs were performed (e.g. number of x-rays), who was included, and what percentage of children with suspected physical abuse were evaluated with SS. Lastly, multi-center studies are needed to detect differences in outcomes between populations and to account for hospital-level characteristics, such as availability of resources (e.g. child abuse experts, radiology staff, and x-ray equipment) and hospital policies to identify victims of child abuse or to reduce use of radiation.
Supplementary Material
Acknowledgments
This review was funded by grant 1K23HD071967 from the National Institute of Child Health and Human Development grant. Dr. Wood’s institution has received payment for court testimony that she has provided in cases of suspected child abuse for which she has been involved in the care of the child and subpoenaed to testify. We would like to acknowledge Melisa (Ayse) Gebizlioglu and Kurt Koehler for their assistance with screening abstracts and titles for studies that were not relevant and Ms. Gebizlioglu for her assistance with assessing the full manuscripts of relevant studies for eligibility.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors do not have conflicts of interest to disclose.
References
References marked with an asterisk indicate studies included in the systematic review.
- American Academy of Pediatrics. Diagnostic imaging of child abuse. Pediatrics. 1991;87(2):262. [PubMed] [Google Scholar]
- American Academy of Pediatrics. Diagnostic imaging of child abuse. Pediatrics. 2000;105(6):1345–1348. doi: 10.1542/peds.105.6.1345. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatrics. Diagnostic imaging of child abuse. Pediatrics. 2009;123(5):1430–1435. doi: 10.1542/peds.2009-0558. [DOI] [PubMed] [Google Scholar]
- American College of Radiology & The Society for Pediatric Radiology. ACR practice guideline for skeletal surveys in children. 2006 Retrieved from Reston, VA: http://www.acr.org/SecondaryMainMenuCategories/quality_safety/guidelines/dx/musc/skeletal_surveys.aspx.
- American College of Radiology & The Society for Pediatric Radiology. ACR-SPR practice guideline for skeletal surveys in children. 2011 Retrieved from http://www.acr.org/~/media/ACR/Documents/PGTS/guidelines/Skeletal_Surveys.pdf.
- American College of Radiology & The Society for Pediatric Radiology. ACR–SPR practice parameter for skeletal surveys in children. 2014 Retrieved from http://www.acr.org/~/media/ACR/Documents/PGTS/guidelines/Skeletal_Surveys.pdf.
- American College of Radiology & The Society for Pediatric Radiology. ACR Appropriateness Criteria: Suspected Physical Abuse-Child. 2016 Retrieved from https://acsearch.acr.org/docs/69443/Narrative/
- *.Anderst JD. Assessment of factors resulting in abuse evaluations in young children with minor head trauma. Child Abuse Negl. 2008;32(3):405–413. doi: 10.1016/j.chiabu.2007.06.007. [DOI] [PubMed] [Google Scholar]
- *.Barber I, Perez-Rossello JM, Wilson CR, Kleinman PK. The yield of high-detail radiographic skeletal surveys in suspected infant abuse. Pediatr Radiol. 2015;45(1):69–80. doi: 10.1007/s00247-014-3064-3. [DOI] [PubMed] [Google Scholar]
- *.Barber I, Perez-Rossello JM, Wilson CR, Silvera MV, Kleinman PK. Prevalence and relevance of pediatric spinal fractures in suspected child abuse. Pediatr Radiol. 2013;43(11):1507–1515. doi: 10.1007/s00247-013-2726-x. [DOI] [PubMed] [Google Scholar]
- *.Belfer RA, Klein BL, Orr L. Use of the skeletal survey in the evaluation of child maltreatment. Am J Emerg Med. 2001;19(2):122–124. doi: 10.1053/ajem.2001.21345. [DOI] [PubMed] [Google Scholar]
- *.Berger RP, Panigrahy A, Gottschalk S, Sheetz M. Effective Radiation Dose in a Skeletal Survey Performed for Suspected Child Abuse. J Pediatr. 2016;171:310–312. doi: 10.1016/j.jpeds.2016.01.017. [DOI] [PubMed] [Google Scholar]
- Cancian M, Slack KS, Yang MY. The Effect of Family Income on Risk of Child Maltreatment. Madison, WI: University of Wisconsin-Madison Institute for Research and Policy; 2010. [Google Scholar]
- *.Carrim ZI, Arbabi EM, Long VW. Presumed non-accidental injury with retinal haemorrhages–findings from a tertiary referral centre in the United Kingdom. Brain Inj. 2012;26(13–14):1716–1722. doi: 10.3109/02699052.2012.722261. [DOI] [PubMed] [Google Scholar]
- Christian CW, Committee on Child Abuse and Neglect The evaluation of suspected child physical abuse. Pediatrics. 2015;135(5):e1337–1354. doi: 10.1542/peds.2015-0356. [DOI] [PubMed] [Google Scholar]
- *.Day F, Clegg S, McPhillips M, Mok J. A retrospective case series of skeletal surveys in children with suspected non-accidental injury. J Clin Forensic Med. 2006;13(2):55–59. doi: 10.1016/j.jcfm.2005.08.001. [DOI] [PubMed] [Google Scholar]
- *.Deye KP, Berger RP, Lindberg DM. Occult abusive injuries in infants with apparently isolated skull fractures. J Trauma Acute Care Surg. 2013;74(6):1553–1558. doi: 10.1097/TA.0b013e31828b7fc4. [DOI] [PubMed] [Google Scholar]
- *.Drubach LA, Johnston PR, Newton AW, Perez-Rossello JM, Grant FD, Kleinman PK. Skeletal trauma in child abuse: detection with 18F-NaF PET. Radiology. 2010;255(1):173–181. doi: 10.1148/radiol.09091368. [DOI] [PubMed] [Google Scholar]
- *.Duffy SO, Squires J, Fromkin JB, Berger RP. Use of skeletal surveys to evaluate for physical abuse: analysis of 703 consecutive skeletal surveys. Pediatrics. 2011;127(1):e47–52. doi: 10.1542/peds.2010-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckenrode J, Smith EG, McCarthy ME, Dineen M. Income inequality and child maltreatment in the United States. Pediatrics. 2014;133(3):454–461. doi: 10.1542/peds.2013-1707. [DOI] [PubMed] [Google Scholar]
- *.Fagen KE, Shalaby-Rana E, Jackson AM. Frequency of skeletal injuries in children with inflicted burns. Pediatr Radiol. 2015;45(3):396–401. doi: 10.1007/s00247-014-3163-1. [DOI] [PubMed] [Google Scholar]
- *.Ghahreman A, Bhasin V, Chaseling R, Andrews B, Lang EW. Nonaccidental head injuries in children: a Sydney experience. J Neurosurg. 2005;103(3 Suppl):213–218. doi: 10.3171/ped.2005.103.3.0213. [DOI] [PubMed] [Google Scholar]
- *.Hansen KK, Campbell KA. How useful are skeletal surveys in the second year of life? Child Abuse Negl. 2009;33(5):278–281. doi: 10.1016/j.chiabu.2008.10.002. [DOI] [PubMed] [Google Scholar]
- *.Harper NS, Feldman KW, Sugar NF, Anderst JD, Lindberg DM. Additional injuries in young infants with concern for abuse and apparently isolated bruises. J Pediatr. 2014;165(2):383–388 e381. doi: 10.1016/j.jpeds.2014.04.004. [DOI] [PubMed] [Google Scholar]
- *.Hicks RA, Stolfi A. Skeletal surveys in children with burns caused by child abuse. Pediatr Emerg Care. 2007;23(5):308–313. doi: 10.1097/01.pec.0000270174.39228.30. [DOI] [PubMed] [Google Scholar]
- *.Higginbotham N, Lawson KA, Gettig K, Roth J, Hopper E, Higginbotham E, Garcia NM. Utility of a child abuse screening guideline in an urban pediatric emergency department. J Trauma Acute Care Surg. 2014;76(3):871–877. doi: 10.1097/TA.0000000000000135. [DOI] [PubMed] [Google Scholar]
- *.Hymel KP, Herman BE, Narang SK, Graf JM, Frazier TN, Stoiko M, Wang M. Potential Impact of a Validated Screening Tool for Pediatric Abusive Head Trauma. J Pediatr. 2015;167(6):1375–1381 e1371. doi: 10.1016/j.jpeds.2015.09.018. [DOI] [PubMed] [Google Scholar]
- *.Jackson J, Miller M, Moffatt M, Carpenter S, Sherman A, Anderst J. Bruising in Children: Practice Patterns of Pediatric Hematologists and Child Abuse Pediatricians. Clin Pediatr (Phila) 2015;54(6):563–569. doi: 10.1177/0009922814558249. [DOI] [PubMed] [Google Scholar]
- Jenny C, Hymel KP, Ritzen A, Reinert SE, Hay TC. Analysis of missed cases of abusive head trauma. JAMA. 1999;281(7):621–626. doi: 10.1001/jama.281.7.621. doi:joc80101 [pii] [DOI] [PubMed] [Google Scholar]
- *.Jha P, Stein-Wexler R, Coulter K, Seibert A, Li CS, Wootton-Gorges SL. Optimizing bone surveys performed for suspected non-accidental trauma with attention to maximizing diagnostic yield while minimizing radiation exposure: utility of pelvic and lateral radiographs. Pediatr Radiol. 2013;43(6):668–672. doi: 10.1007/s00247-012-2614-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Journy N, Rehel JL, Ducou Le Pointe H, Lee C, Brisse H, Chateil JF, Bernier MO. Are the studies on cancer risk from CT scans biased by indication? Elements of answer from a large-scale cohort study in France. Br J Cancer. 2015;112(1):185–193. doi: 10.1038/bjc.2014.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Karmazyn B, Lewis ME, Jennings SG, Hibbard RA, Hicks RA. The prevalence of uncommon fractures on skeletal surveys performed to evaluate for suspected abuse in 930 children: should practice guidelines change? AJR Am J Roentgenol. 2011;197(1):W159–163. doi: 10.2214/ajr.10.5733. [DOI] [PubMed] [Google Scholar]
- Lane WG, Dubowitz H. What factors affect the identification and reporting of child abuse-related fractures? Clin Orthop Relat Res. 2007;461:219–225. doi: 10.1097/BLO.0b013e31805c0849. [DOI] [PubMed] [Google Scholar]
- *.Lane WG, Rubin DM, Monteith R, Christian CW. Racial differences in the evaluation of pediatric fractures for physical abuse. JAMA. 2002;288(13):1603–1609. doi: 10.1001/jama.288.13.1603. [DOI] [PubMed] [Google Scholar]
- *.Laskey AL, Stump TE, Hicks RA, Smith JL. Yield of skeletal surveys in children </= 18 months of age presenting with isolated skull fractures. J Pediatr. 2013;162(1):86–89. doi: 10.1016/j.jpeds.2012.06.038. [DOI] [PubMed] [Google Scholar]
- *.Lindberg DM, Beaty B, Juarez-Colunga E, Wood JN, Runyan DK. Testing for Abuse in Children With Sentinel Injuries. Pediatrics. 2015;136(5):831–838. doi: 10.1542/peds.2015-1487. [DOI] [PubMed] [Google Scholar]
- *.Lindberg DM, Berger RP, Reynolds MS, Alwan RM, Harper NS. Yield of skeletal survey by age in children referred to abuse specialists. J Pediatr. 2014;164(6):1268–1273 e1261. doi: 10.1016/j.jpeds.2014.01.068. [DOI] [PubMed] [Google Scholar]
- *.Lindberg DM, Shapiro RA, Laskey AL, Pallin DJ, Blood EA, Berger RP. Prevalence of abusive injuries in siblings and household contacts of physically abused children. Pediatrics. 2012;130(2):193–201. doi: 10.1542/peds.2012-0085. [DOI] [PubMed] [Google Scholar]
- Miglioretti DL, Johnson E, Williams A, Greenlee RT, Weinmann S, Solberg LI, Smith-Bindman R. The use of computed tomography in pediatrics and the associated radiation exposure and estimated cancer risk. JAMA Pediatr. 2013;167(8):700–707. doi: 10.1001/jamapediatrics.2013.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oral R, Blum KL, Johnson C. Fractures in young children: are physicians in the emergency department and orthopedic clinics adequately screening for possible abuse? Pediatr Emerg Care. 2003;19(3):148–153. doi: 10.1097/01.pec.0000081234.20228.33. [DOI] [PubMed] [Google Scholar]
- Oral R, Yagmur F, Nashelsky M, Turkmen M, Kirby P. Fatal abusive head trauma cases: consequence of medical staff missing milder forms of physical abuse. Pediatr Emerg Care. 2008;24(12):816–821. doi: 10.1097/PEC.0b013e31818e9f5d. [DOI] [PubMed] [Google Scholar]
- Paine CW, Scribano PV, Localio R, Wood JN. Development of Guidelines for Skeletal Survey in Young Children With Intracranial Hemorrhage. Pediatrics. 2016 doi: 10.1542/peds.2015-3024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce MC, Kaczor K, Acker D, Carle M, Webb T, Brenze AJ. Bruising Missed as a Prognostic Indicator of Future Fatal and Near-Fatal Physical Child Abuse. Pediatric Academic Societies. 2008 Retrieved from http://www.abstracts2view.com/pasall/view.php?nu=PAS08L1_3204.
- Prior M, Guerin M, Grimmer-Somers K. The effectiveness of clinical guideline implementation strategies–a synthesis of systematic review findings. J Eval Clin Pract. 2008;14(5):888–897. doi: 10.1111/j.1365-2753.2008.01014.x. [DOI] [PubMed] [Google Scholar]
- *.Rangel EL, Cook BS, Bennett BL, Shebesta K, Ying J, Falcone RA. Eliminating disparity in evaluation for abuse in infants with head injury: use of a screening guideline. J Pediatr Surg. 2009;44(6):1229–1234. doi: 10.1016/j.jpedsurg.2009.02.044. discussion 1234–1235. [DOI] [PubMed] [Google Scholar]
- *.Ravichandiran N, Schuh S, Bejuk M, Al-Harthy N, Shouldice M, Au H, Boutis K. Delayed identification of pediatric abuse-related fractures. Pediatrics. 2010;125(1):60–66. doi: 10.1542/peds.2008-3794. [DOI] [PubMed] [Google Scholar]
- *.Shelmerdine SC, Das R, Ingram MD, Negus S. Who are we missing? Too few skeletal surveys for children with humeral and femoral fractures. Clin Radiol. 2014;69(12):e512–516. doi: 10.1016/j.crad.2014.08.014. [DOI] [PubMed] [Google Scholar]
- Simel DL, Samsa GP, Matchar DB. Likelihood ratios with confidence: sample size estimation for diagnostic test studies. J Clin Epidemiol. 1991;44(8):763–770. doi: 10.1016/0895-4356(91)90128-v. doi:0895-4356(91)90128-V. [DOI] [PubMed] [Google Scholar]
- Slovis TL, Strouse PJ, Strauss KJ. Radiation Exposure in Imaging of Suspected Child Abuse: Benefits versus Risks. J Pediatr. 2015;167(5):963–968. doi: 10.1016/j.jpeds.2015.07.064. [DOI] [PubMed] [Google Scholar]
- Thorpe EL, Zuckerbraun NS, Wolford JE, Berger RP. Missed opportunities to diagnose child physical abuse. Pediatr Emerg Care. 2014;30(11):771–776. doi: 10.1097/PEC.0000000000000257. [DOI] [PubMed] [Google Scholar]
- *.Wood JN, Christian CW, Adams CM, Rubin DM. Skeletal surveys in infants with isolated skull fractures. Pediatrics. 2009;123(2):e247–252. doi: 10.1542/peds.2008-2467. [DOI] [PubMed] [Google Scholar]
- Wood JN, Fakeye O, Feudtner C, Mondestin V, Localio R, Rubin DM. Development of guidelines for skeletal survey in young children with fractures. Pediatrics. 2014;134(1):45–53. doi: 10.1542/peds.2013-3242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood JN, Fakeye O, Mondestin V, Rubin DM, Localio R, Feudtner C. Development of hospital-based guidelines for skeletal survey in young children with bruises. Pediatrics. 2015;135(2):e312–320. doi: 10.1542/peds.2014-2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Wood JN, Feudtner C, Medina SP, Luan X, Localio R, Rubin DM. Variation in occult injury screening for children with suspected abuse in selected US children’s hospitals. Pediatrics. 2012;130(5):853–860. doi: 10.1542/peds.2012-0244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Wood JN, French B, Song L, Feudtner C. Evaluation for occult fractures in injured children. Pediatrics. 2015;136(2) doi: 10.1542/peds.2014-3977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Wood JN, Hall M, Schilling S, Keren R, Mitra N, Rubin DM. Disparities in the evaluation and diagnosis of abuse among infants with traumatic brain injury. Pediatrics. 2010;126(3):408–414. doi: 10.1542/peds.2010-0031. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


