Abstract
The high rate of mortality associated with cancer is due to its inherent nature to metastasize. Perineural invasion (PNI) is a relatively rare mode of metastasis, and a distinct pathologic entity that can be observed in the absence of lymphatic or vascular invasion which is still shrouded by mystery. PNI is a marker of poor prognosis. Despite increasing recognition of this metastatic process, there has been little progress in the understanding of mechanisms behind PNI. The purpose of this article is to make surgeons aware of caudad to cephalad metastasis of oral cancer along trigeminal nerve.
Keywords: Perineural invasion, Metastasis, Oral cancer
Introduction
Squamous cell carcinoma (SCC) of the oral cavity is very common in India and sixth most common malignancy worldwide [1]. Metastasis is the biggest hurdle in the treatment of oral cancer. What is metastasis—it is the ability of malignant cells to break themselves from the primary lesion, invade the basal lamina, dodge host defences, disseminate via lymphatic or the hematogenous route, and establish a new niche at a secondary site [2].
Perineural invasion (PNI) is distinct from lymphatic or vascular invasion and may be the reason of seeding of cells to non-contiguous regions, thus lead to loco-regional recurrence [3].
Cruveilhier in 1835 first discovered PNI of tumor cells, when he reported invasion of mammary carcinoma into facial nerve [4]. In 2011 PNI, was included among the high-risk parameters in the new 7th edition AJCC staging system for cSCC [5].
Perineural invasion is a subject of controversy among pathologist. According to Dunn et al. [6] PNI is defined as the presence of malignant cells in the perineural space with total or near total circumferential involvement of the nerve. Liebig et al. [7] have put forth the most widely agreed description of PNI: Tumors in close proximity to a nerve that involve one-third of its circumference and or the presence of tumor cells within any of the three layers of the nerve sheath.
Trigeminal nerve is most vulnerable for PNI as it gives cutaneous innervation to major region of the head and neck [8], as is observed in our case.
We report of a rare incidence of spread of oral buccal mucosa cancer along the peripheral branches of trigeminal nerve to the intracranial sites.
Case Report
We present a case of 45 year old female with a chief complaint of burning sensation on chewing food since 2 months. On examination a 3 cm lesion was seen on the left lower buccal mucosa involving the attached gingiva extending from second premolar to second molar. Biopsy revealed moderately differentiated squamous cell carcinoma. The treatment done was supraomohyoid neck dissection with segmental mandibulectomy and reconstruction with titanium plates. Post-operative healing was satisfactory. However after 7 days post-op, patient started complaining of neuralgia type of pain and described the pain as ants crawling on her left side of face, along the distribution of trigeminal nerve. The patient was referred to neurology centre where she was diagnosed with Trigeminal Neuralgia. But the pain kept on worsening and patient also complained of diminishing vision in left eye, which prompted us to advise the patient MRI scan. The scan revealed an infiltration of tumor cells along the trigeminal nerve till the cavernous sinus (Figs. 1, 2, 3). As the tumor had extensively infiltrated surrounding areas and could not be surgically resected, the patient was referred for radiotherapy. Here she was subjected to a dose of 58 Gy over 28 days.
Fig. 1.
Post gadolinium enhanced axial image shows thickened trigeminal nerve (red circle) with extension into the orbit along opthalmic nerve (blue arrow)
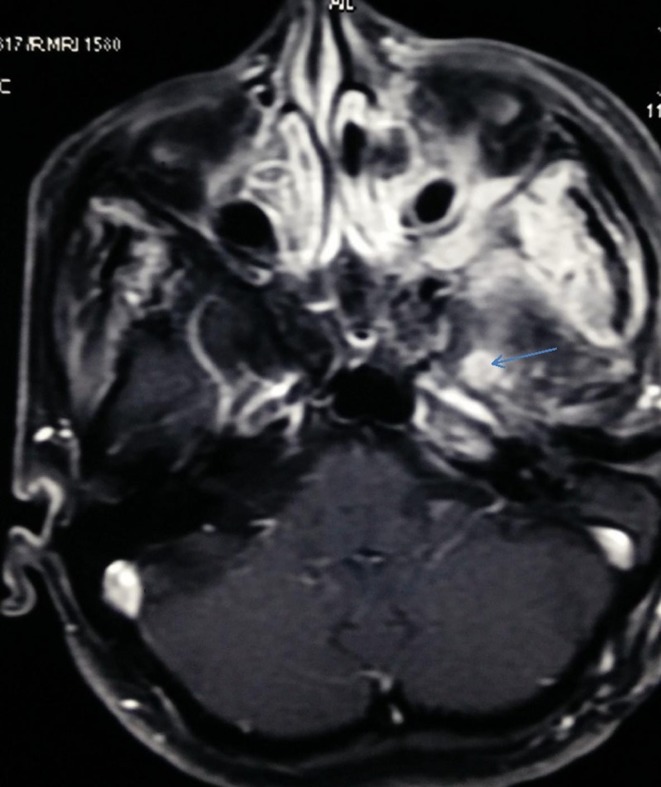
Fig. 2.
Post gadolinium enhanced axial section shows thickening of trigeminal nerve (blue arrow)
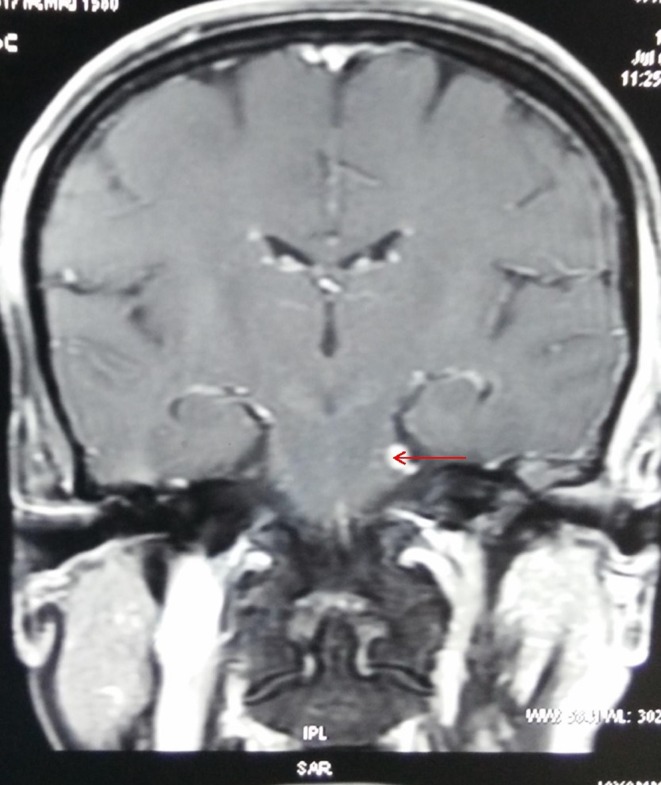
Fig. 3.
Post gadolinium enhanced coronal section shows thickening of trigeminal nerve (red arrow)
Discussion
The diagnosis and treatment of PNI in head and neck cancer is a challenge for the clinicians. Tumors more than 2 cm in the cephalic region have a greater propensity for PNI due to rich cutaneous innervation [9]. The tumor cells first invade the peripheral cutaneous nerves which then metastasise along the larger nerves and eventually inflict the brainstem. Perineural invasion usually occurs in a centripetal fashion, though centrifugal involvement has also been described. PNI is divided as ‘incidental PNI’ and ‘clinical PNI’ [4]. PNI without the presence of preoperative symptoms is “incidental” or microscopic (mPNI), as the diagnosis is made on biopsy. When patients with carcinomas develop symptoms such as paresthesia, hypesthesia, pain in the distribution of a trigeminal nerve branch, or facial weakness then it is clinical PNI (cPNI). Early symptoms can be noted only if the clinician suspects PNI, otherwise it is usually missed. If untreated, symptoms progress to pain, numbness and/or motor deficits afflicting the distribution of the affected cranial nerve. PNI is often misdiagnosed as Bell palsy or trigeminal neuralgia, which delays the diagnosis by 6 months to 2 years [8].
Pathogenesis
Though CRUVEILHEIR, identified PNI more than 150 years ago, but the mechanism of PNI is still controversial. Plethora of theories tried to explain the pathology of PNI. Earlier, it was though that cancer cells extend along planes of least resistance, that is by proliferation through the loose connective tissue sheath of the perineurium or via the lymphatics of the epineurium. These theory was discarded because the ultra-structural scans of the nerve sheath revealed that perineurium is a tightly adherent and selective barrier between nerves and surrounding tissue. Tumor cells invade the perineurium in a direct and continuous manner, and gets fused with layers of the endoneurium. Also, lymphatic channels are absent in perineurium and endoneurium [1, 4].
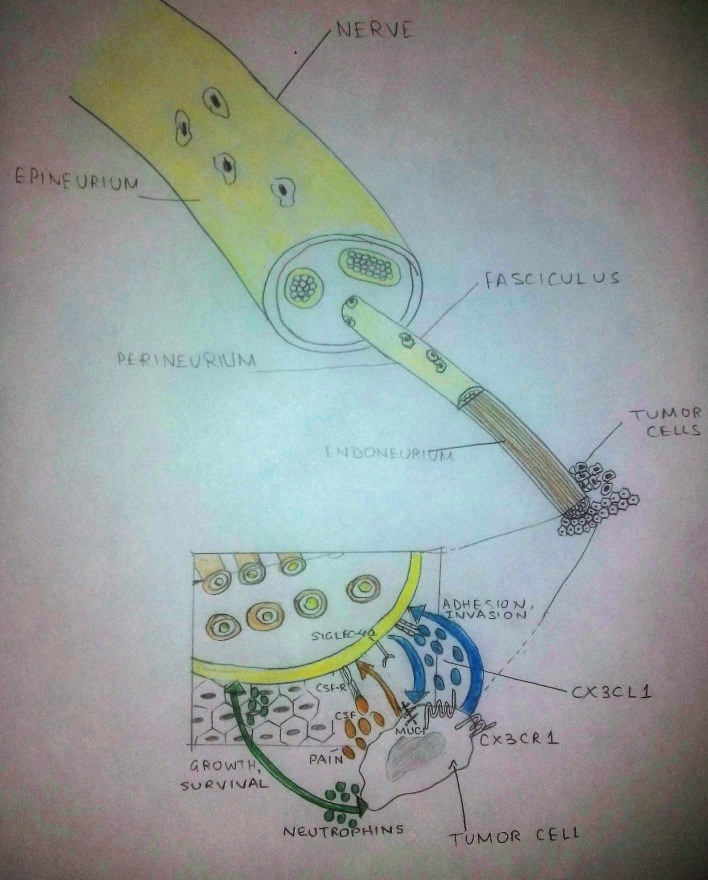
Continuous research have emphasized that the tumor microenvironment plays a central role to promote PNI by providing signals (Fig. 4) [4]. Nerve growth factor/tyrosine kinase A, neural cell adhesion molecule (N-CAM), claudin1, laminin5, telencephalin (ICAM-5), and many other factors promote, cancer cell metastasis towards and along the nerve trunk within the perineural space [1, 4]. Cranial nerves that shows features of PNI on MRI scan, should be thoroughly evaluated [4]. Hi-resolution focused gadolinium enhanced MRI detects PNI with precision. The obliteration of fat plane surrounding the cranial nerve, enhancement with or without enlargement of the nerve, mass in the cavernous sinus or Meckel cave are signs of PNI on imaging and sometimes indirect signs of PNI seen are denervation of a group of muscles supplied by the cranial nerve [10]. Advanced imaging modalities, positron emission tomography/computed tomography (PET/CT) with 2-[fluorine 18]fluoro- 2-deoxy-d-glucose (FDG) has been proved fundamental in the detection of PNI. Based on imaging grading of PNI has been done. (Table 1) which has a significant prognostic implication.
Fig. 4.
Sketch diagram showing interaction between the nerve fibers and tumor cells in the pathogenesis of perineural invasion. Molecules involved in this interaction include the chemokine Fractalkine/Neurotactin (CX3CL1) expressed by neurons and its receptor CX3CR1 on tumor cells and membranebound glycoproteins (SIGLEC-4a) binding to tumor mucins (MUC-1). Neurotropins secreted by neural and tumor cells sustain growth and survival of both intratumoral nerves and cancer cells. Colony stimulating factors (G and GM-CSF) secreted by tumor cells sensitize neural cells expressing their receptors (CSFR), affecting pain perception
Table 1.
Grading of PNI based on extent of invasion as seen on radiographic image
| Grade | Zone involved | Zonal anatomy involved in PNI |
|---|---|---|
| Grade 1 | Zone 1 | Ophthalmic-superior orbital fissure Maxillary-foramen rotundum Mandibular-foramen ovale |
| Grade 2 | Zone 2 | From zone 1 to gasserian ganglion |
| Grade 3 | Zone 3 | Extension into the brain cisterns and brain stem with involvement of zones 1 and 2 |
Treatment/Prognosis
Perineural invasion leads to greater recurrence rate and poor prognosis as compared to patients without PNI. Jambusaria et al. documented a 84 % of 5-year disease specific survival in patients with PNI versus 96 % in those without. Compared to patients without PNI, PNI is associated with a higher rate of recurrence and 5-year disease specific death. Local site relapse is most common, and most relapses occur within 2-4 years after initial resection. Clinical PNI patients have an increased rate of relapse compared to those with mPNI. Garcia-Serra et al., reported local control, cause specific survival and overall survival of 87, 65 and 50 % respectively over a 5-year follow up on 59 patients with mPNI compared to 55, 59 and 55 % on 76 patients with cPNI treated with surgery and postoperative radiotherapy. Imaging positive cPNI patients have highest rates of local recurrence, 43-75 versus 24 % and lower rates of disease-specific survival, 56-61 versus 100 % compared to image negative patients. Miller [11], also found a significant correlation between PNI, nodal status and T stage of primary tumor.
15–20 % of patients with PNI are at increased risk of nodal metastases and adjuvant radiation therapy (RT) is always recommended [4]. In practice, the patients with SCC and microscopic PNI are subjected to prophylactic postoperative RT to prevent recurrence. Clinical PNI has worse prognosis but management is less controversial. Aggressive Resection and postoperative RT is the mainstay of treatment. Based on the location and extent of the tumor, the RT dose is fixed. Patients are treated with hyperfractionation at 1.2 Gy per fraction twice daily to doses in the range of 64.8–74.4 Gy postoperatively (depending on the margins) and 74.4 Gy for definitive RT. Even though the regional nodes are clinically uninvolved, they are given prophylactic RT due to relatively high risk of subclinical disease. No evidence is there for using adjuvant chemotherapy in patients with PNI [5].
Conclusion
Treatment failures in patients with oral squamous cell carcinoma are primarily due to loco-regional recurrence and distant metastasis. PNI represents a least understood phenomenon of metastasis and has very poor prognosis. The radiologist and the surgeon should be highly suspicious of perineural involvement when evaluating cancers that occur in close proximity, with one or more cranial nerves in the head and neck region.
Acknowledgments
No funding is or was obtained by any author from any sources.
Compliance with Ethical Standards
Conflict of interest
All the authors declared that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Contributor Information
R. Keerthi, Email: 29.keerthi@gmail.com
Abhishek Dutta, Email: drabhishekmaxfac23@gmail.com.
Shruthi Agarwal, Email: shruthi86dec@gmail.com.
Vikram Kani, Email: vikramarunachalam@gmail.com.
Abhishek Khatua, Email: abhishekkhatua@gmail.com.
References
- 1.Binmadi NO, Basile JR. Perineural invasion in oral squamous cell carcinoma: a discussion of significance and review of the literature. Oral Oncol. 2011;47:1005–1010. doi: 10.1016/j.oraloncology.2011.08.002. [DOI] [PubMed] [Google Scholar]
- 2.Haddad RI, Shin DM. Recent advances in head and neck cancer. N Engl J Med. 2008;359:1143–1154. doi: 10.1056/NEJMra0707975. [DOI] [PubMed] [Google Scholar]
- 3.Rapidis AD, Givalos N, Gakiopoulou H, Faratzis G, Stavrianos SD, Vilos GA, et al. Adenoid cystic carcinoma of the head and neck. Clinicopathological analysis of 23 patients and review of the literature. Oral Oncol. 2005;41:328–335. doi: 10.1016/j.oraloncology.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 4.Gaddikeri S, Bhrany S, Anzai Y. Perineural invasion of skin cancers in the head and neck: an uncommon phenomenon revisited. Otolaryngology. 2014 [Google Scholar]
- 5.Mendenhall WM, Ferlito A, Takes RP, Bradford CR, Corry J, Fagan JJ, et al. Cutaneous head and neck basal and squamous cell carcinomas with perineural invasion. Oral Oncol. 2012;48:918–922. doi: 10.1016/j.oraloncology.2012.02.015. [DOI] [PubMed] [Google Scholar]
- 6.Dunn M, Morgan MB, Beer TW. Perineural invasion: identification, significance and a standardized definition. Dermatol Surg. 2009;35:214–221. doi: 10.1111/j.1524-4725.2008.34412.x. [DOI] [PubMed] [Google Scholar]
- 7.Liebig C, Ayala G, Wilks JA, Berger DH, Albo D. Perineural invasion in cancer: a review of the literature. Cancer. 2009;115:3379–3391. doi: 10.1002/cncr.24396. [DOI] [PubMed] [Google Scholar]
- 8.Mendenhall WM, Amdur RJ, Hinerman RW, Werning JW, Malyapa RS, et al. Skin cancer of the head and neck with perineural invasion. Am J Clin Oncol. 2007;30:93–96. doi: 10.1097/01.coc.0000251224.16075.60. [DOI] [PubMed] [Google Scholar]
- 9.Lawrence N, Cottel WI. Squamous cell carcinoma of skin with perineural invasion. J Am Acad Dermatol. 1994;31:30–33. doi: 10.1016/S0190-9622(94)70131-8. [DOI] [PubMed] [Google Scholar]
- 10.Gandhi MR, Panizza B, Kennedy D. Detecting and defining the anatomic extent of large nerve perineural spread of malignancy: comparing “targeted” MRI with the histologic findings following surgery. Head Neck. 2011;33:469–575. doi: 10.1002/hed.21470. [DOI] [PubMed] [Google Scholar]
- 11.Miller ME, Palla B, Chen Q, Elashoff DA, Abemayor E, Maie A. A novel classification system for perineural invasion in noncutaneous head and neck squamous cell carcinoma: histologic subcategories and patient outcomes. Am J Otolaryngol-Head Neck Med Surg. 2012;33:212–215. doi: 10.1016/j.amjoto.2011.06.003. [DOI] [PubMed] [Google Scholar]