Abstract
Background
Endodontic treatment is usually indicated when teeth with periapical lesions are encountered. However, sometimes root canal treatment results in failure. In that case, one of the treatment choices is retreatment by an orthograde approach. Surgical endodontic therapy is also an alternative to preserve the tooth. Various techniques have been suggested in the literature which has more predictable results. The introduction of modern surgical techniques have enhanced the results of apical surgery procedures. Operating microscopes, magnifying loupes, microinstruments, ultrasonic tips, and biologically acceptable root-end filling materials (such as MTA and SuperEBA) have been introduced to this field with the modern technique, thus the success rates of modern apical surgery has increased significantly.
Objective
The aim of the present study was to evaluate the clinical and radiographic outcomes and periotest values of apical surgery treatment.
Methods
A total of 112 teeth were included. SuperEBA and MTA were used as root-filling materials. The recorded parameters were gender, age, location of the tooth, the presence/absence of a post, coronal restoration of the tooth, previous surgical/nonsurgical treatment of the tooth, the size of periapical lesions, histopathology of periapical lesions, smoking habits. Also the periotest values were recorded.
Results
The overall success rate was 88.4%. With regard to the evaluated variables, only one parameter (tooth type) was found statistically significant. Although the periotest values were decreased after 6 months compared to immediately postoperative measurements, the values were still significantly higher than preoperative measurements.
Conclusion
In this study, apical surgery performed with the modern instruments has significantly successful results with 88.4% success rate.
Keywords: MTA, Apical surgery, Periotest, Super-EBA
Introduction
Endodontic treatment is usually performed in teeth with periapical lesions [1]. In some cases, root canal treatment can result in failure. The main factors of endodontic failure are microbial infection in the root canal system and/or the periradicular area [2, 3]. The clinician thinks that the direct causes of endodontic failures are procedural errors such as broken instruments, perforations, overfilling, underfilling, and ledges [3]. Nevertheless, there are some cases in which the treatment has followed the highest technical standards and yet treatment can result in failure [3]. They include microbial factors, comprising extraradicular and/or intraradicular infections, and intrinsic or extrinsic nonmicrobial factors [3]. In case of failure, one of the treatment choices is retreatment by an orthograde approach [1]. However, when a nonsurgical attempt proves unsuccessful or is contraindicated, surgical endodontic therapy is indicated to obtain an apical seal and save the tooth [1, 4, 5].
The main goal of surgical endodontic treatment is to prevent the invasion of bacteria and their by-products from the root canal system into the periradicular tissues of teeth with apical periodontitis [2]. Various techniques have been suggested that provide apical surgery procedures to become easier to perform, ensure safer treatment outcomes for the patients and has more predictable results [6]. For years, the modern approach for root-end filling was accepted to be the traditional approach with round surgical burs and amalgam [6, 7]. The preparation of root-end cavities with burs brings about some problems such as difficult access to the apices of the roots, inability to prepare a cavity parallel to the canal, and the risk of perforation of the root [7]. The success rates of traditional techniques reported approximately 59% [4]. Apical surgery has changed substantially in the last 20 years with the implementation of modern surgical techniques. Use of the operating microscope, magnifying loupes, microinstruments, ultrasonic tips, and more biologically acceptable root-end filling materials (such as MTA and Super-EBA) has been introduced with this modern technique, and the success rate of modern apical surgery has increased approximately 90% [4, 8].
Increase in tooth mobility is ineluctable, and mobility changes over time are an interesting clinical success criteria considered after apical surgery. The periotest was first introduced by Schulte and Lukas [9] as a reproducible and basic method for measurement of tooth mobility. It also provides a reliable evaluation of treatment outcomes in the fields of periodontology, implantology, traumatology, and orthodontics. Schulte et al. studied the relationship between periotest values and marginal bone loss of teeth [9] and showed high correlation between the parameters.
To our knowledge, there are not any studies in the English literature that include periotest measurements for tooth treated by apical surgery. The aim of the present study was to evaluate the clinical and radiographic outcomes of apical surgery treatment and measure periotest values of the teeth treated by a modern instrument.
Materials and Methods
Patient Selection and Inclusion/Exclusion Criteria
In this clinical study, data were collected in the Gazi University, Faculty of Dentistry, Department of Oral and Maxillofacial Surgery, between September 2014 and October 2015. This study was approved by Gazi University Institutional Review Board and Ministry of Health. Patients were informed in detail about the surgical procedure and were instructed about postoperative care, follow-up examinations, and alternative treatment options available to them. Informed written signed consent was acquired from all participants according to the Declaration of Helsinki. Inclusion criteria were as follows: patients with a noncontributory medical history; patients older than 18 years old; teeth without a periapical lesion, no mobility and normal pocket depth, but unresolved symptoms after nonsurgical approaches have been exhausted; teeth with small periapical lesions together with clinical symptoms, normal periodontal probing depth and no mobility; teeth that have a large periapical lesion progressing coronally but without periodontal pocket and mobility.
The following exclusion criteria were applied: patients under 18 years old; patients that were nursing or pregnant; teeth with pathoses associated with horizontal or vertical root fracture; more than 5 mm of periodontal attachment and bone loss detected by periodontal probing; teeth with perforation of cervical or lateral canal walls.
Of the 150 teeth that had undergone an apical surgery during the study period, the following exclusions were made: root resorption 4%, vertical root fractures 4.6%, and teeth not in the recall time after surgery 16.6%. Finally, 112 teeth were applicable for the study and subjected to further analysis. Prognostic evaluation factors and results for these 112 teeth are summarized in Table 1. A total of 112 patients were included. The recorded parameters were gender, age, location of the tooth, the presence or absence of a post, coronal restoration of the tooth, previous surgical or nonsurgical treatment of the tooth, the size of periapical lesions, histopathology of periapical lesions, smoking habits. Also the periotest values were recorded from all teeth which were subjected to apical surgery.
Table 1.
Treatment outcome of apical surgery
| Final outcome | n | % |
|---|---|---|
| Healed | 99 | 88.4 |
| Healing | 3 | 2.7 |
| Persistent diseases | 10 | 8.9 |
| Total | 112 | 100.0 |
Surgical Procedures
Surgical procedure was performed using an operation loupe (Seiler Dental Loupe, St. Louis, MO) with magnification of 3.5X to provide optimum magnification and illumination. Operation loupe was used throughout the operation including osteotomies, root-end resections, root inspections, root-end preparations, root-end fillings, and suturings. Incisions and elevation of flaps were not performed under the operation loupe.
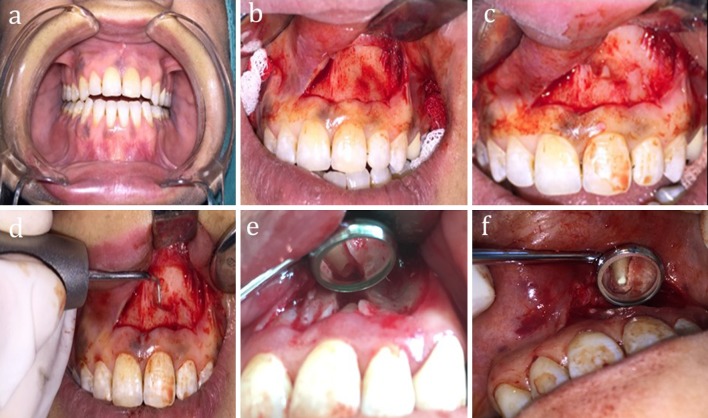
Before the operation, the oral region was isolated by sterile cover. Mucogingival flap type was used for the surgery. A full-thickness mucoperiosteal flap was elevated under local anesthesia containing 2% lidocaine with 1:80.000 adrenaline. After the elevation of mucoperiosteal flap, osteotomy was performed to remove bone overlying the root apices. After the osteotomy, the periradicular tissues of the root apex were gently curetted and were sent for biopsy. In order to provide a clearer analysis, methylene blue was applied to the surgical site. After the inspection of the surgical field, a 3-mm section of the root tip was resected. Root was resected at 0- or near 0-degree bevels; the resected surface and external root surfaces were then examined to check for the presence of cracks and isthmuses. If the crack could not be removed completely without compromising retention of the tooth, the surgery was abandoned and an extraction was indicated instead. If an isthmus was seen between the canals, the root-end preparation included the isthmus. Hemostasis was achieved by applying pressure with small gauzes soaked in adrenaline. Root-end preparations were performed depth of 3 mm with surgical microretro tips (SONICflex retro, KaVo, Biberach/Riss, Germany) in a surgical sonic unit (KaVo SONICflex, KaVo GmbH, Biberach, Germany). The cavity was rinsed with sterile water. After the preparation of root-end cavity, root-end filling was performed. MTA (MTA-Angelus®, Angelus Odonto-Logika, Londrina, Paraná, Brazil) (56 teeth) or Super-EBA (Super-EBA, Harry J. Bosworth Co, Skokie, IL) (56 teeth) was used as root-end filling material. When MTA was used as a root-end filling material, it was placed into the root-end cavity with a microplugger (Retro-filling Plugger, Hu-Friedy Mfg. Co, Chicago). In case of Super-EBA used as root-end filling material, it was placed into the root-end cavity with a microplugger as MTA. The same procedure was performed in cases which received previous periradicular surgery, having no root-end filling materials. The flap was replaced using 5.0 monofilament sutures (suture size 5.0 nonabsorbable monofilament black, Solmed Pty Limited, Penrith). The sutures were removed 6 or 7 days after the surgical intervention (Fig. 1).
Fig. 1.
Stages of apical surgery and root-end filling procedures (a–f)
Medication
All patients were given nonsteroidal analgesic (Majezik), and patients were instructed to rinse their mouth twice daily with 0.1% chlorhexidine digluconate for 10 days. Antibiotics were prescribed starting 1 day before surgery and during the 4 days postoperatively (1 g amoxicillin every 12 h or alternatively 150 mg clindamycin every 6 h).
Clinical and Radiographic Evaluation
The postoperative clinical examination procedures were applied such as the presence of specific signs and/or symptoms, loss of function, tenderness to percussion, tenderness to palpation, subjective discomfort, excess tooth mobility, sinus tract formation, signs of infection or swelling, sinusitis, paresthesia, soft tissue scarring or discoloration, and periodontal pocket formation and follow-up sensitivity of adjacent teeth to electrical pulp testing.
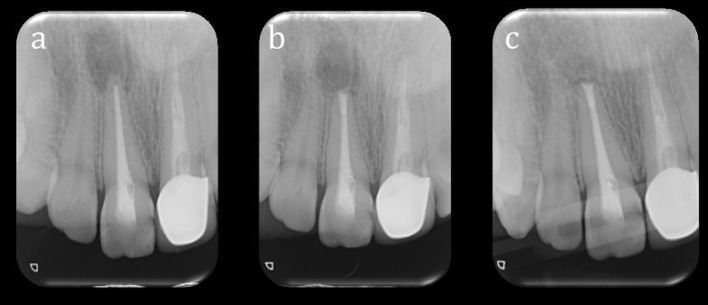
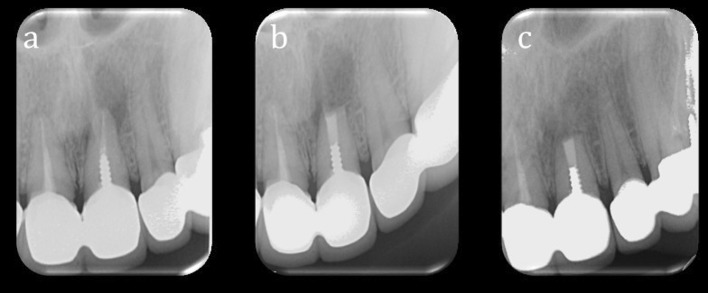
The postoperative radiographs taken at 6 months were evaluated independently by two examiners using the criteria established by Rud et al. [10] (Figs. 2, 3). The two examiners standardized the evaluation criteria before case analyses. Any disagreement regarding the clinical outcome was resolved by discussion until an agreement was reached. The following healing classification was used based on the criteria proposed by Rud et al. [10]:
Complete healing Reformation of an intact lamina dura around the root.
Incomplete healing Rarefaction has either decreased in size or remained stationary. Bone structures may be present within the rarefaction. The rarefaction is irregular in shape and may be located asymmetrically around the root apex. An isolated rarefaction (scar tissue) may be present in the bone.
Uncertain healing Rarefaction has decreased in size. The rarefaction is circular in shape and is located symmetrically around the root apex.
Unsatisfactory healing Rarefaction has increased in size.
Fig. 2.
Preoperative (a), immediately postoperative (b) and 6 months postoperative (c) periapical radiographs of a patient included in this study
Fig. 3.
Preoperative (a), immediately postoperative (b) and 6 months postoperative (c) periapical radiographs of another patient included in this study
Assessment of Outcome
After clinical and radiographic evaluation, outcomes of the cases were grouped into the following three categories using criteria proposed by Friedman [11]:
Healed Absence of clinical signs and symptoms and radiographic classification of complete healing or incomplete healing.
Healing Absence of clinical signs and symptoms and radiographic classification of uncertain healing.
Persistent disease The presence of the clinical signs and symptoms and/or radiographic classification of unsatisfactory healing.
Statistical Analysis
The influence of the predictors was analyzed by Pearson’s Chi-square, Monte Carlo simulation, or Fisher’s exact tests. All hypotheses were tested at 0.05 significance level using IBM SPSS Statistics 20.0 software (IBM SPSS Inc., Chicago, IL, USA).
The evaluation criteria prior to the case analyses were standardized by two examiners so that the results could be evaluated based on the same methods and conditions. Cohen’s kappa statistical analysis was used to measure interexaminer reliability. Any disagreement resulted in joint evaluation until an agreement was reached.
Results
There was high agreement between the observers with respect to the evaluation of the outcome of surgery (k = 1; p = 0.0001). The overall success rate was 88.4% (Table 1). With regard to the evaluated variables, only one parameter (tooth location) was found statistically significant. Maxillary teeth were more likely to be healed compared with mandibular teeth (p = 0.0001). Similarly, anterior teeth were more likely to be healed compared with posterior teeth (p = 0.0006) (Table 2). Other predictors investigated including root-end filling material (p = 0,639), gender (p = 0.401), age (p = 0.819), preoperative signs and symptoms (p = 0.348), apical resurgery (p = 0.436), preoperative status of root canal filling (p = 0.307), previous initial endodontic treatment or retreatment (p = 0.771), histopathological examination of periapical lesions (p = 0.534), presence or absence of post (p = 0.605) had no significant effect on the outcome of apical surgery (Tables 2, 3).
Table 2.
Prognostic factors affecting treatment outcome
| Final outcome | Chi-square | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Healed | Healing | Persistent disease | Total | ||||||||
| n | % | n | % | n | % | n | % | Chi-square | P | ||
| Root-end filling material | Super-EBA | 48 | 85.7 | 2 | 3.6 | 6 | 10.7 | 56 | 100 | M | 0.639 |
| MTA | 51 | 91.1 | 1 | 1.8 | 4 | 7.1 | 56 | 100 | |||
| Total | 99 | 88.4 | 3 | 2.7 | 10 | 8.9 | 112 | 100 | |||
| Age | 16–30 | 44 | 68 | 1 | 2 | 5 | 10 | 50 | 100 | M | 0.819 |
| 31–50 | 40 | 86.9 | 2 | 4.4 | 3 | 6.7 | 45 | 100 | |||
| 51–65 | 15 | 86.2 | 0 | 0 | 2 | 11.8 | 17 | 100 | |||
| Total | 99 | 86.4 | 3 | 2.7 | 10 | 8.9 | 112 | 100 | |||
| Gender | Female | 42 | 91.3 | 0 | 0 | 4 | 8.7 | 46 | 100 | M | 0.401 |
| Male | 57 | 86.4 | 3 | 4.5 | 6 | 9.1 | 66 | 100 | |||
| Total | 99 | 88.4 | 3 | 2.7 | 10 | 8.9 | 112 | 100 | |||
| Tooth location | Max. | 84 | 96.6 | 0 | 0 | 3 | 3.4 | 87 | 100 | M | 0.0001 |
| Mand. | 15 | 60 | 3 | 12 | 7 | 28 | 25 | 100 | |||
| Total | 99 | 88.4 | 3 | 2.7 | 10 | 8.9 | 112 | 100 | |||
| Tooth location | Anterior | 85 | 93.4 | 2 | 2.2 | 4 | 4.4 | 91 | 100 | M | 0.0006 |
| Posterior | 14 | 66.7 | 1 | 4.8 | 6 | 28.6 | 21 | 100 | |||
| Total | 99 | 88.4 | 3 | 2.7 | 10 | 8.9 | 112 | 100 | |||
| Tooth location | Max. anterior | 74 | 97.4 | 0 | 0 | 2 | 2.6 | 76 | 100 | M | 0.0001 |
| Max. posterior | 10 | 90.9 | 0 | 0 | 1 | 9.1 | 11 | 100 | |||
| Mand. anterior | 11 | 73.3 | 2 | 13.3 | 2 | 13.3 | 15 | 100 | |||
| Mand posterior | 4 | 40 | 1 | 10 | 5 | 50 | 10 | 100 | |||
| Total | 99 | 88.4 | 3 | 2.7 | 10 | 8.9 | 112 | 100 | |||
Table 3.
Prognostic factors affecting treatment outcome
| Final outcome | Chi-square | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Healed | Healing | Persistent disease | Total | ||||||||
| n | % | n | % | n | % | n | % | Chi-square | P | ||
| Presence of post | Presence | 18 | 81.8 | 1 | 4.5 | 3 | 13h6 | 22 | 100 | M | 0.605 |
| Absence | 81 | 90 | 2 | 2.2 | 7 | 7.8 | 90 | 100 | |||
| Total | 99 | 88.4 | 3 | 2.7 | 10 | 8.9 | 112 | 100 | |||
| Preoperative status of root canal filling | Good | 38 | 82.6 | 2 | 4.3 | 6 | 13 | 46 | 100.0 | M | 0.307 |
| Not good | 61 | 92.4 | 1 | 1.5 | 4 | 6.1 | 66 | 100.0 | |||
| Total | 99 | 88.4 | 3 | 2.7 | 10 | 8.9 | 112 | 100.0 | |||
| Apical resurgery | Re-surgery | 16 | 80 | 1 | 5 | 3 | 15 | 20 | 100 | M | 0.436 |
| First surgery | 83 | 90.2 | 2 | 2.2 | 7 | 7.6 | 92 | 100 | |||
| Total | 99 | 86.4 | 3 | 2.1 | 10 | 8.9 | 112 | 100 | |||
| Previous initial endodontic treatment or retreatment | First treatment | 64 | 90.1 | 2 | 2.8 | 5 | 7 | 71 | 100 | M | 0.771 |
| Retreatment | 35 | 85.4 | 1 | 2.4 | 5 | 12.2 | 41 | 100 | |||
| Total | 99 | 88.4 | 3 | 2.7 | 10 | 8.9 | 112 | 100 | |||
| Histopathological examination | Granuloma | 46 | 86.8 | 1 | 1.9 | 6 | 11.3 | 53 | 100 | M | 0.534 |
| Cyst | 23 | 85.2 | 2 | 7.4 | 2 | 7.4 | 27 | 100 | |||
| Other | 8 | 80 | 0 | 0 | 2 | 20 | 10 | 100 | |||
| Total | 77 | 85.6 | 3 | 3.3 | 10 | 11.1 | 90 | 100 | |||
| Preoperative signs and symptoms | Presence | 39 | 83 | 2 | 4.3 | 6 | 12.8 | 47 | 100 | M | 0.348 |
| Absence | 60 | 92.3 | 1 | 1.5 | 4 | 6.2 | 65 | 100 | |||
| Total | 99 | 88.4 | 3 | 2.7 | 10 | 8.9 | 112 | 100 | |||
Periotest values were measured preoperative, postoperative, and 6 months after surgery, respectively. In our study, tooth mobility significantly increased after the surgery according to presurgical results. At the 6-month follow-up appointment, a significant decrease in mobility was discovered in comparison with posttreatment results. Although a reduction in mobility was discovered after 6 months, the obtained values compared to preoperative values were still considerably high (Table 4).
Table 4.
Comparative evaluation of periotest values prior to, immediately after and 6 months after surgery
| Periotest | Wilcoxon | |||||||
|---|---|---|---|---|---|---|---|---|
| n | Mean | Median | Minimum | Maximum | 55 | z | P | |
| Preop B/L(Periotest) | 112 | 3 | 3 | 1 | 5 | 1 | −9.3 | 0.0001 |
| Postop B/L(Periotest) | 112 | 7 | 7 | 5 | 9 | 1 | ||
| Preop B/L(Periotest) | 112 | 3 | 3 | 1 | 5 | 1 | −8.9 | 0.0001 |
| Postop 6 month B/L(Periotest) | 112 | 5 | 5 | 3 | 8 | 1 | ||
| Postop B/L(Periotest) | 112 | 7 | 7 | 5 | 9 | 1 | −9.5 | 0.0001 |
| Postop 6 month B/L(Periotest) | 112 | 5 | 5 | 3 | 8 | 1 | ||
Discussion
Apical surgery has been a procedure that is resorted as the last option before tooth extraction with unpredictable outcomes. Today, apical surgery has advanced to become a modern technique which has good results with regard to treatment of endodontic lesions with predictable healing patterns [12].
In 1997, Kim et al. recommended the use of modern apical surgery instead of traditional root-end surgery. Both techniques aim to obtain good periapical healing results; however, they are significantly different from each other considering the methods used [8].
In a recent meta-analysis and systematic review [6], the mean clinical success rates for traditional root-end surgery were reported to be 59% (rates ranging from 43.5 to 75%). In contrast, recent studies about apical surgery show success rate ranging from 89 to 100%. Considering these factors all teeth included in this study were applied apical surgery with modern instruments.
Outcomes were categorized as healed, healing, or persistent disease. Patient without clinical symptoms and patients with complete or incomplete radiographic groups were classified as successful. In this short-term clinical study, the percentage of teeth assessed as healed, healing, and persistent disease were 88.4, 2.7, and 8.9%, respectively. The success rate 6 months after the surgery was found to be 88.4%. This is similar to the results of other studies performed using magnification, ultrasonic surgical tips, and filling materials such as Super-EBA or MTA [13].
The most commonly studied intraoperative factor is the effect of the root-end filling material, and the most commonly used materials are biocompatible materials such as Super-EBA and MTA. In the literature, in vitro and ex vivo studies comparing MTA and Super-EBA showed that Super-EBA is inferior to MTA [8]. In vitro and ex vivo studies are easier to perform and allow for a more objective evaluation of the effectiveness of a material. However, these studies are performed under conditions that differ from those found in actual surgical practice. Moreover, the human body has a natural ability to heal mild inflammation and adapt foreign materials. Therefore, they cannot reflect the influence of clinical conditions [8]. Moreover, in the literature, Super-EBA was reported over 90% clinical success. Thus, in this study Super-EBA and MTA were used as a retrograde filling material [8]. In many clinical studies, use of Super-EBA and MTA has shown similar clinical results [14]. In our study, a success rate of 85.7% (56 teeth) for MTA and 91.1% (56 teeth) for Super-EBA was achieved. The statistical analysis of the success rates did not exert any significant difference between the groups.
When previous studies about apical surgery were examined [12–19], parameters such as gender, age, location of the tooth, the presence or absence of a post, coronal restoration of the tooth, previous surgical or nonsurgical treatment of the tooth, the size of periapical lesions, histopathology of periapical lesions, smoking habits, and preoperative signs and symptoms were reported to be potential prognostic factors that might affect the clinical results. These prognostically effective parameters were also recorded in this study, and their effects on the success of the apical surgery were evaluated. Moreover, periotest values were recorded preoperatively, postoperatively, and 6 months after the surgery for each tooth that was operated. To our knowledge, there are not any studies in the English literature that include periotest measurements for apical surgery applied tooth. Thus, this is the first study to be published in the English literature that evaluates periotest values after apical surgery.
After apical surgery, increase in tooth mobility is ineluctable and mobility changes over time are an interesting clinical success criteria considered after apical surgery. Measuring tooth mobility and especially assessing changes in mobility is rather difficult. Luxation is the most commonly used method to detect tooth mobility. This is because the recommendations for evaluating tooth mobility are insufficient, nonscientific, and highly subjected to individual variation [9]. Since there was need for a numerical assessment of tooth mobility to help assess changes after the apical surgery, a periotest was used. It is an electronic device that measures the damping characteristics of the periodontium and provides an objective measurement [9]. The periotest was first introduced by Schulte and Lukas [9] as a reproducible and basic method for measurement of tooth mobility. In this study, the periotest device was selected to measure tooth mobility because of its widespread use in daily practice. It also provides a reliable evaluation of treatment outcomes in the fields of periodontology, implantology, traumatology, and orthodontics [9]. Long-term data on periotest have shown that it can be an objective clinical measurement of the stability of bone-implant anchorage [20]. In the literature, periotest was used to measure implant stability and found a direct correlation between periotest values (PTV) and the degree of initial osseointegration [20]. It was further suggested that PTV should be included in the current success criteria [20]. In this study, we aim to test our hypothesis on correlation between apical surgery and tooth mobility before surgery and 6 months after surgery by using periotest device. In our study, tooth mobility significantly increased after the surgery according to presurgical results. At the 6-month follow-up appointment, a significant decrease in mobility was discovered in comparison with posttreatment results. Although a reduction in mobility was discovered after 6 months, the obtained values compared to preoperative values were still considerably high. Six monthly data on short-term results showed us some improvement, but mobility values have not yet been returned to the beginning of treatment.
In the present study, parameters such as patient age and gender were of no importance with regard to the outcome of apical surgery; this finding is consistent with other studies [15, 21, 22]. However, in a retrospective study by Song et al. [16], it was stated that after 4 years of follow-up better outcomes were achieved in female patients. Similar results and success rates were achieved in all age and gender groups proving that this technique may be used in all age and gender groups.
The success rates obtained in this study were 97.4% for anterior maxillary teeth, 90.9% for posterior maxillary teeth, 73.3% for anterior mandibular teeth, and 40% for posterior mandibular teeth. Among all groups, anterior maxillary teeth were found to have the highest success rates. These data are consistent with the results of Penarrocha et al. [23]. In our study, success rates were found to be 96.6% for maxillary teeth, 60% for mandibular teeth and compared to mandibular teeth maxillary teeth showed statistically significant higher success rates. This result is similar to the results of studies performed by Song et al. [17] and Testori et al. [24]. In this study, anterior maxillary teeth were found to have statistically significant success rates in comparison with anterior mandibular teeth. Likewise, posterior maxillary teeth showed statistically significant higher success rates compared to posterior mandibular teeth. Success rates were 93.4% for anterior teeth and 66.7% for posterior teeth in our study. We believe that this finding may be a result of better sight of vision and easier access to the apices of maxillary teeth and thus better apical seal [15]. Anterior teeth showed statistically significant higher success rates in comparison with posterior teeth. These data were consistent with the data reported by Kreisler et al. [18] and Song et al. [17]. Low success rates in the posterior region may be attributed to difficulty in access and complicated anatomical properties of the posterior teeth [15].
Song et al. [16] stated that the outcome of the apical surgery is not influenced by preoperative signs and symptoms. Von Arx et al. [22] reported that pain and tenderness at the initial examination were shown to be effective only in the 1-year prognosis after apical surgery; however, after 5-year follow-up these findings lost their prognostic value [19]. In the present study, the outcome of endodontic microsurgery was not affected by the preoperative signs and symptoms similar to the previous study [16, 19]. In the literature, initial apical surgery shows better prognosis compared to resurgery [16, 19], but not in all cases were these findings statistically significant. In the present study, first-time apical surgery demonstrated better clinical results with a statistically insignificant higher success rate of 90.2% in comparison with the 80% success rate of resurgery. However, Gagliani et al. [25] reported significantly different success rates, with complete healing achieved in 59% of the resurgery cases compared to 86% of the cases treated with single surgical procedure. Interestingly, Song et al. [26] reported considerably higher success rate of endodontic microsurgery such as 92.9% as opposed to other studies in the literature [22]. Lower success rates were achieved in the resurgery cases included in this study. This might be due to the fibrotic changes that occur after the first surgery, excess shortening of the root after the second surgery, and possible damage in the lingual or palatal bone caused by the second osteotomy.
In the present study, the final treatment result was not significantly affected by the previously done root canal treatment. This finding is in correlation with other studies performed on this subject [22, 27]. These results suggest that no matter the quality of the root canal treatment done previously; when modern apical surgery is performed achieving an optimal seal, high success rates may be achieved. Likewise, as stated by Song et al. [16], previously done endodontic treatment or retreatment had no distinct effect.
Although Maddalone and Gagliani [28] showed a higher success rate of 95.3% in healthy teeth, compared to 87.5% in teeth restored with the aid of a post, this finding has not yet been supported by other researchers [16, 19, 21]. In the present study, no relation was found between the healing rate and the existence of a post or screw.
In this study, teeth with lesions were biopsied for histopathological examination. Periapical lesion histopathology was evaluated by the World Health Organization classification [29]. Histopathological investigation was performed after 80.3% of the all teeth. Most of the lesions were granulomas, but 30% were diagnosed as periapical cysts. In our study, the histopathological diagnosis of the lesions was not found to be associated with the success or failure of the treatment. The overall treatment outcome in the present population was not significantly influenced by the presence of either a granuloma or a cyst, which is consistent with previous studies [27, 30].
Apical surgery performed with the modern instruments has significantly successful results [4, 8]. In our study, a success rate of 88.4% was achieved. According to this study, especially maxillary teeth were found more successful results than mandibular teeth. Similarly, anterior teeth were found more successful results for posterior teeth. Apical surgical procedures can be safely performed in these regions, but in the posterior mandible region alternative therapies should be considered. Moreover, there are a lot of parameters that affect the surgical outcomes. Considering the results obtained in this clinical study, we believe that there is need for more investigation regarding this subject.
Compliance with Ethical Standards
Conflict of interest
All the authors declare that they have no conflict of interest.
Ethical Standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Contributor Information
Faruk Öğütlü, Phone: +903122034142, Email: drfarukogutlu@gmail.com.
İnci Karaca, Phone: +903122034328, Email: incirana@yahoo.com.
References
- 1.Shahi S, Rahimi S, Yavari HR, Shakouie S, Nezafati S, Abdolrahimi M. Sealing ability of white and gray mineral trioxide aggregate mixed with distilled water and 0.12% chlorhexidine gluconate when used as root-end filling materials. J Endod. 2007;33:1429–1432. doi: 10.1016/j.joen.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 2.Pecora CN, Baskaradoss JK, Al-Sharif A, Al-Rejaie M, Mokhlis H, Al-Fouzan K, et al. Histological evaluation of the root apices of failed endodontic cases. Saudi Endod J. 2015;5:120. doi: 10.4103/1658-5984.155450. [DOI] [Google Scholar]
- 3.Siqueira J. Aetiology of root canal treatment failure: why well-treated teeth can fail. Int Endod J. 2001;34:1–10. doi: 10.1046/j.1365-2591.2001.00396.x. [DOI] [PubMed] [Google Scholar]
- 4.Setzer FC, Kohli MR, Shah SB, Karabucak B, Kim S. Outcome of endodontic surgery: a meta-analysis of the literature—part 2: comparison of endodontic microsurgical techniques with and without the use of higher magnification. J Endod. 2012;38:1–10. doi: 10.1016/j.joen.2012.03.027. [DOI] [PubMed] [Google Scholar]
- 5.Abu-Melha AS. Root amputation and bone grafting of failed apicoectomy of mesiobuccal root of maxillary first molar. Saudi Endod J. 2012;2:147. doi: 10.4103/1658-5984.112709. [DOI] [Google Scholar]
- 6.Setzer FC, Shah SB, Kohli MR, Karabucak B, Kim S. Outcome of endodontic surgery: a meta-analysis of the literature—part 1: comparison of traditional root-end surgery and endodontic microsurgery. J Endod. 2010;36:1757–1765. doi: 10.1016/j.joen.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 7.Liu Z, Zhang D, Li Q, Xu Q. Evaluation of root-end preparation with a new ultrasonic tip. J Endod. 2013;39:820–823. doi: 10.1016/j.joen.2013.03.004. [DOI] [PubMed] [Google Scholar]
- 8.Song M, Kim E. A prospective randomized controlled study of mineral trioxide aggregate and super ethoxy–benzoic acid as root-end filling materials in endodontic microsurgery. J Endod. 2012;38:875–879. doi: 10.1016/j.joen.2012.04.008. [DOI] [PubMed] [Google Scholar]
- 9.Schulte W, d’Hoedt B, Lukas D, Maunz M, Steppeler M. Periotest for measuring periodontal characteristics–correlation with periodontal bone loss. J Periodontal Res. 1992;27:184–190. doi: 10.1111/j.1600-0765.1992.tb01667.x. [DOI] [PubMed] [Google Scholar]
- 10.Rud J, Andreasen J, Jensen JM. Radiographic criteria for the assessment of healing after endodontic surgery. Int J Oral Surg. 1972;1:195–214. doi: 10.1016/S0300-9785(72)80013-9. [DOI] [PubMed] [Google Scholar]
- 11.Friedman S. The prognosis and expected outcome of apical surgery. Endodontic Topics. 2005;11:219–262. doi: 10.1111/j.1601-1546.2005.00187.x. [DOI] [Google Scholar]
- 12.Serrano-Giménez M, Sánchez-Torres A, Gay-Escoda C. Prognostic factors on periapical surgery: a systematic review. Med Oral Patol Oral Cir Bucal. 2015;20:e715. doi: 10.4317/medoral.20613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lui J-N, Khin M-M, Krishnaswamy G, Chen N-N. Prognostic Factors Relating to the Outcome of Endodontic Microsurgery. J Endod. 2014;40:1071–1076. doi: 10.1016/j.joen.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 14.Çalışkan M, Tekin U, Kaval M, Solmaz M. The outcome of apical microsurgery using MTA as the root-end filling material: 2-to 6-year follow-up study. Int Endod J. 2016;49:245–254. doi: 10.1111/iej.12451. [DOI] [PubMed] [Google Scholar]
- 15.von Arx T, Penarrocha M, Jensen S. Prognostic factors in apical surgery with root-end filling: a meta-analysis. J Endod. 2010;36:957–973. doi: 10.1016/j.joen.2010.02.026. [DOI] [PubMed] [Google Scholar]
- 16.Song M, Jung I-Y, Lee S-J, Lee C-Y, Kim E. Prognostic factors for clinical outcomes in endodontic microsurgery: a retrospective study. J Endod. 2011;37:927–933. doi: 10.1016/j.joen.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 17.Song M, Kim SG, Lee S-J, Kim B, Kim E. Prognostic factors of clinical outcomes in endodontic microsurgery: a prospective study. J Endod. 2013;39:1491–1497. doi: 10.1016/j.joen.2013.08.026. [DOI] [PubMed] [Google Scholar]
- 18.Kreisler M, Gockel R, Aubell-Falkenberg S, Kreisler T, Weihe C, Filippi A, et al. Clinical outcome in periradicular surgery: effect of patient- and tooth-related factors—a multicenter study. Quintessence Int. 2013;44(1):53–60. doi: 10.3290/j.qi.a28742. [DOI] [PubMed] [Google Scholar]
- 19.von Arx T, Jensen SS, Hänni S, Friedman S. Five-year longitudinal assessment of the prognosis of apical microsurgery. J Endod. 2012;38:570–579. doi: 10.1016/j.joen.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 20.Atsumi M, Park S-H, Wang H-L. Methods used to assess implant stability: current status. Int JOMI. 2007;22:743–754. [PubMed] [Google Scholar]
- 21.Tsesis I, Rosen E, Schwartz-Arad D, Fuss Z. Retrospective evaluation of surgical endodontic treatment: traditional versus modern technique. J Endod. 2006;32:412–416. doi: 10.1016/j.joen.2005.10.051. [DOI] [PubMed] [Google Scholar]
- 22.von Arx T, Jensen SS, Hänni S. Clinical and radiographic assessment of various predictors for healing outcome 1 year after periapical surgery. J Endod. 2007;33:123–128. doi: 10.1016/j.joen.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 23.Peñarrocha M, Martí E, García B, Gay C. Relationship of periapical lesion radiologic size, apical resection, and retrograde filling with the prognosis of periapical surgery. J Oral Maxillofac Surg. 2007;65:1526–1529. doi: 10.1016/j.joms.2006.10.058. [DOI] [PubMed] [Google Scholar]
- 24.Testori T, Capelli M, Milani S, Weinsteind RL. Success and failure in periradicular surgeryA longitudinal retrospective analysis. JOOO. 1999;87:493–498. doi: 10.1016/s1079-2104(99)70250-7. [DOI] [PubMed] [Google Scholar]
- 25.Gagliani M, Gorni F, Strohmenger L. Periapical resurgery versus periapical surgery: a 5-year longitudinal comparison. Int Endod J. 2005;38:320–327. doi: 10.1111/j.1365-2591.2005.00950.x. [DOI] [PubMed] [Google Scholar]
- 26.Song M, Shin S-J, Kim E. Outcomes of endodontic micro-resurgery: a prospective clinical study. J Endod. 2011;37:316–320. doi: 10.1016/j.joen.2010.11.029. [DOI] [PubMed] [Google Scholar]
- 27.Wälivaara D-Å, Abrahamsson P, Fogelin M, Isaksson S. Super-EBA and IRM as root-end fillings in periapical surgery with ultrasonic preparation: a prospective randomized clinical study of 206 consecutive teeth. JOOO. 2011;112:258–263. doi: 10.1016/j.tripleo.2011.01.016. [DOI] [PubMed] [Google Scholar]
- 28.Maddalone M, Gagliani M. Periapical endodontic surgery: a 3 year follow up study. Int Endod J. 2003;36:193–198. doi: 10.1046/j.1365-2591.2003.00642.x. [DOI] [PubMed] [Google Scholar]
- 29.Kramer IR, Pindborg JJ, Shear M. Histological typing of odontogenic tumours. Berlin: Springer; 1992. [DOI] [PubMed] [Google Scholar]
- 30.Rubinstein RA, Kim S. Short-term observation of the results of endodontic surgery with the use of a surgical operation microscope and Super-EBA as root-end filling material. J Endod. 1999;25:43–48. doi: 10.1016/S0099-2399(99)80398-7. [DOI] [Google Scholar]