Abstract
Purpose
The purpose of this study was to assess the efficacy of orthodontic mini-screws as a modified suture anchor for disc repositioning in cases of internal derangement of the temporomandibular joint.
Patients and Methods
A prospective evaluation of ten patients was undertaken for a period of 6 months using this modified approach from Jan 2014 to Jun 2016. Symptomatic patients with clinical and MRI features suggestive of internal derangement of TMJ and willing to undergo surgical repositioning of articular disc to alleviate symptoms of temporomandibular dysfunction were taken up for the study. Post-operatively, functional outcomes were assessed in terms of reduction in pain, joint movement and absence of joint noise and clicking sounds. Post-operative MRI was used to assess the disc position and morphological changes in the disc and arthritic changes in the condyle.
Results
All patients underwent a surgical repositioning of the anteriorly displaced disc by the modified orthodontic suture anchor. Patients were post-surgically followed up at intervals of 1, 3 and 6 months. Immediate complications in terms of pain, restriction of functional motion and transient facial nerve palsy were noted. Late complications include temporal nerve palsy in one case. All patients experienced significant improvement with good functional outcomes and stable repositioning of disc was noticed at the end of 6 months.
Conclusion
The modified disc repositioning using an orthodontic screw via a mini preauricular approach provided a good functional outcome in all patients as assessed over a period of 6 months. However, the long-term functional sequel of the procedure and changes in the articular disc needs to be assessed.
Keywords: TMJ internal derangement, Disc repositioning, Orthodontic mini-screws
Introduction
Internal derangement is a common intracapsular disorder and is defined as any interference with smooth joint movement. Temporomandibular joint (TMJ) disc displacement (DD) is the most common condition associated with progressive joint dysfunction [1]. With regard to clinical diagnosis and treatment, two predominant stages of internal derangements are distinguished called disc derangement with reduction and disc derangement without reduction.
Partial anterior displacement of the articular disc is the most common sign of joint dysfunction, affecting nearly 40% of the general population [2]. Displacement of the disc can occur at any time of life; it usually follows a traumatic event that causes the condyle–disc relationship to be altered. Disc displacement can incite inflammatory changes that cause osteoarthritis (OA) and progressive degenerative joint disease. These conditions are characterized by deterioration of the articular cartilage, disc, synovium and subchondral bone. Additionally, persistence of the internal derangement will produce condylar remodelling and an overall decrease in condylar height. Often, the extent of degenerative change is proportional to the length of time the disc remains displaced [2].
Though many surgical procedures have been described in the literature, currently the standard open surgical procedure is disc repositioning. Disc repositioning to a more normal anatomical relation with the condyle and fossa is usually undertaken when the disc is displaced [3].
Clinical studies of disc-repositioning surgery have demonstrated a favourable outcome in terms of decreased pain and improved mandibular function in 80–94% of patients [4]. Aim of this study was to assess the efficacy of orthodontic mini-screws as a modified suture anchor for surgical disc repositioning in cases of internal derangement of the temporomandibular joint.
Materials and Methods
This study was conducted on 10 patients (14 joints) who reported to our centre with complaints of pain and dysfunction of the temporomandibular joint between Jan 2014 and Jun 2016. The age group of the patients ranged from 19 to 51 years and included 06 female patients and 04 male patients with a mean age of 33.6 years (Table 1). Two patients underwent bilateral joint surgery, whereas eight had unilateral joint surgery.
Table 1.
Clinical dysfunction index, Di, based on evaluation of five common clinical symptoms (Helkimo 1974)
| Score 0 | Score 1 | Score 5 | |
|---|---|---|---|
| A. Impaired range of movement/mobility index | 06 | 02 | 02 |
| B. Impaired TM joint function | – | 02 | 08 |
| C. Muscle pain | 02 | 05 | 03 |
| D. Temporomandibular joint pain | 01 | 05 | 04 |
| E. Pain on movement of the mandible | 02 | 05 | 03 |
All the patients underwent a thorough pre-operative clinical and MRI evaluation for diagnosis of disc displacement of TMJ. Clinical classification of patients would be as per the RDC/TMD criteria for axis I diagnoses [5]. Objective assessment of patients was undertaken according to the Helkimo anamnestic and clinical dysfunction index [6]. Signs of TMJ dysfunction were assessed as per the objective scale of Helkimo anamnestic and clinical dysfunction index (Table 1). MRI assessment criteria described by Ahmed et al. [7] was used for pre-operative and post-operative assessments.
Orthodontic titanium mini-implants/mini-screws served as bone anchors for repositioning of the meniscus. These self-tapping mini-implants, originally developed for orthodontic anchorage, measured 1.5 mm in diameter and 7.0 mm in length. An eyelet in the screw head allowed for placement of sutures (2-0 nylon) for engaging the disc. Post-operative clinical evaluation was conducted at the end of 1, 3 and 6 months. Post-operative MRI evaluation at the end of 6 months was done to assess the disc shape, position, joint pathology or condylar changes (Table 2).
Table 2.
Comparison of pre-operative and post-opertive clinical dysfunction index scores
| Patient no | Impaired range of movement/mobility index | Impaired TM joint function | Muscle pain | TM joint pain | Pain on movement of the mandible | Total dysfunction score | Post-operative scores at 6 months |
|---|---|---|---|---|---|---|---|
| 1. | 0 | 5 | 1 | 1 | 1 | 8 | 4 |
| 2. | 5 | 5 | 5 | 5 | 5 | 25 | 4 |
| 3. | 0 | 5 | 0 | 1 | 1 | 7 | 2 |
| 4. | 0 | 1 | 5 | 1 | 1 | 8 | 7 |
| 5. | 1 | 5 | 1 | 1 | 0 | 8 | 3 |
| 6. | 0 | 1 | 1 | 1 | 5 | 8 | 0 |
| 7. | 5 | 5 | 1 | 5 | 0 | 16 | 5 |
| 8. | 0 | 5 | 0 | 1 | 1 | 7 | 0 |
| 9. | 0 | 5 | 1 | 5 | 1 | 12 | 3 |
| 10. | 1 | 5 | 5 | 5 | 5 | 21 | 7 |
Surgical Procedure
Under general anaesthesia with nasotracheal intubation, a preauricular incision was marked extending from the root of the helix to the point where the tragus meets the ear lobule. After achieving adequate vasoconstriction, an incision was placed through the skin and subcutaneous tissue, and dissection was extended 2 cm anteriorly in the subcutaneous tissue plane (Fig. 1). The superficial temporal fascia was grasped 5 mm anterior to the tragus with an Adson forceps and a blunt dissection was done in an oblique and superior direction; following the branches of the facial nerves towards the zygomatic arch, exposing the temporal fascia. An incision was placed in the temporalis fascia at this level and extended inferiorly to develop a surgical plane above the capsule of the TMJ. The superior joint space was expanded by application of a mastoid retractor and insufflation of the space with Ringer’s lactate. A T-shaped incision was made with a microsurgical electrode tip with care being taken not to damage the articular disc attached to the capsular ligament. Dissection is performed with a Molt’s elevator liberating the anterior insertion of the articular disc from the preglenoid plane. Disc liberation enabled posterior movement and repositioning of the TMJ disc (Fig. 2).
Fig. 1.

Mini-preauricular incision to expose the superficial temporal fascia
Fig. 2.

Superior joint space exposed
For orthodontic anchor placement, an incision is made on the joint capsule to access the inferior joint space and locating the condylar head. An surgical drill hole was made on the posterior surface of the condyle using a 1.2-mm drill. An orthodontic screw was fixed on to the posterior surface of the condyle, approximately 6–8 mm (Fig. 3) below the posterior slope of the condyle. After fixation of the screw, disc plication was achieved by 2-0 nylon sutures placed on the medial and lateral aspects of the posterior band of the disc (Fig. 4) and engaged to the eyelet of the screw (Fig. 5). The final position and stabilization of the disc was checked by gently translating the condyle forward onto the eminence and back into the fossa. The capsule was closed carefully with No. 4-0 PDS (polydiaxonone) sutures with utmost importance for appropriate wound and synovial membrane tissue healing. Rest of the incision is then closed in layers with 3-0 vicryl and skin approximated with subcuticular 4-0 nylon sutures.
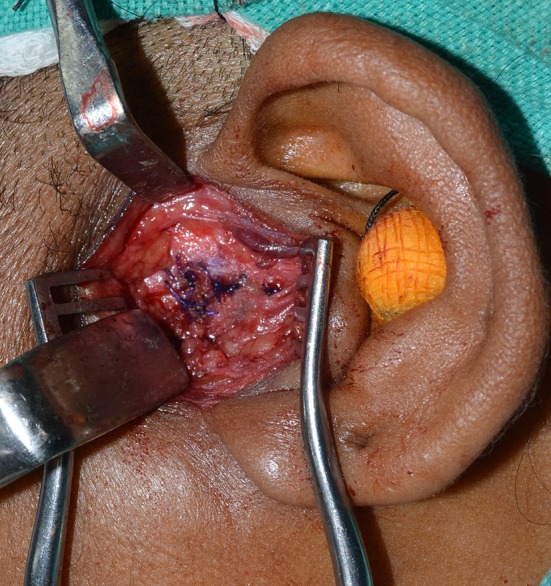
Fig. 3.

Orthodontic mini-screw fixed on the posterior surface of the condyle
Fig. 4.
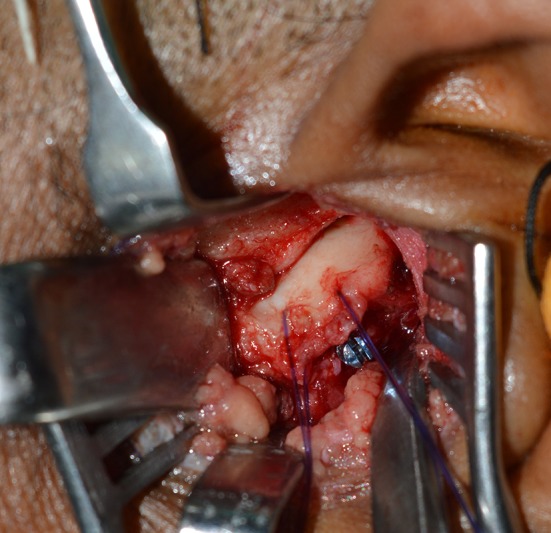
Disc plication was achieved by 2-0 nylon sutures
Fig. 5.
Disc anchored to the orthodontic screw on the posterior surface of the condyle
Results
Ten patients (14 joints) of symptomatic internal derangement underwent surgical repositioning of the disc using an orthodontic mini-screw for various forms of internal derangement of TMJ. Eight patients had unilateral derangement of the disc, whereas two patients had bilateral disc derangement. Three out of the 10 patients had disc displacement without reduction, three patients had disc displacement with reduction, and four patients had non-reducing disc displacement with hypermobility of the joint. Pre-operative clinical dysfunction scores as per the Helkimo index ranged from ranged from 07–25. Clinical dysfunction index showed that six patients had moderate dysfunction of the joint, whereas four patients had severe dysfunction.
All patients showed improvement in their clinical symptoms of pain and dysfunction during the post-operative period. The pre-operative mouth opening of the patients ranged from 23 to 64 mm. Three patients with disc displacement without reduction had a mean pre-operative mouth opening of 25.6 mm which improved to 39.6 mm at the end of 6 months. The mean pre-operative mouth opening of patients with disc displacement with hypermobility was 59.5 mm pre-operatively, and this reduced to a mean mouth opening of 43.5 mm at 6 month post-operative period (Fig. 6). The average laterotrusive excursion (Fig. 7) towards the opposite side ranged at 5 mm, and the mean protrusive movement was 6.5 mm at 6 months post-operatively (Table 3). There was a statistically significant reduction in the mouth opening when compared with a paired t test at the end of 6 months (P value = .001). There was significant reduction in the clinical dysfunction with two patients clinically symptom free five patients with mild dysfunction, and three patients with moderate dysfunction at the end of 6 months.
Fig. 6.

Normal post-operative mouth opening at 6 months
Fig. 7.

Laterotrusive movements towards opposite side at 6 months
Table 3.
Post-operative clinical outcomes in various types of intenal derangement
| S. no. | Age | Diagnosis | Mouth opening (mm) | Mouth opening | Mouth opening | Laterotrusive movements towards opposite side | Protrusive movement | |
|---|---|---|---|---|---|---|---|---|
| Pre-op | 1 month post-op | 6 months post-op | Pre-op | 6 months post-op | 6 months post-op | |||
| 1. | 22 | DdWoR + H | 64 | 38 | 44 | 8 | 6 | 8 |
| 2. | 34 | DdWoR | 23 | 33 | 38 | 2 | 5 | 6 |
| 3. | 26 | DdWoR + H | 55 | 36 | 42 | 9 | 5 | 6 |
| 4. | 19 | DdwR | 44 | 37 | 41 | 7 | 6 | 7 |
| 5. | 37 | DdWoR | 26 | 35 | 39 | 1 | 4 | 5 |
| 6. | 32 | DdwR | 41 | 33 | 39 | 6 | 5 | 7 |
| 7. | 51 | DdWoR + H | 58 | 36 | 43 | 9 | 6 | 8 |
| 8. | 34 | DdwR | 39 | 34 | 38 | 6 | 5 | 6 |
| 9. | 46 | DdWoR + H | 61 | 35 | 45 | 8 | 5 | 7 |
| 10. | 35 | DdWoR | 28 | 37 | 42 | 2 | 5 | 5 |
DdwR disc displacement with reduction, DdWoR disc displacement without reduction, DdWoR + H disc displacement without reduction + hypermobility
Pre-operative MRI assessment showed anterior disc displacement in all 10 cases (Fig. 8). Three patients with non-reducing disc displacement had thinning of the disc pre-operatively and osteoarthritic changes with cupping and deformation of the condylar head. MRI evaluation at the end of 6 months showed stable repositioning of the disc (Fig. 9) in all cases without further progression of arthritic changes in the condyle.
Fig. 8.

Pre-operative MRI showing anterior displacement of disc in closed mouth position
Fig. 9.

Six-month post-operative MRI showing stable position of disc over the surface of the condyle
Discussion
Displacements of the disc can be an acute of chronic event and manifest as reducing or non-reducing disc displacement with reduced mobility or hypermobility. Disc displacements during their natural course can progress to incite inflammatory changes that cause osteoarthritis (OA) and progressive degenerative joint disease characterized by deterioration of the articular cartilage, disc, synovium, and subchondral bone. Additionally, persistence of the internal derangement will produce condylar remodelling and an overall decrease in condylar height [2]. All of our cases had anterior displacement of the disc as assessed clinically and by MRI evaluation, while three cases showed concomitant osteoarthritic features with remodelling changes of the condyle.
All the categories of internal derangements were addressed in our study surgically. The study evaluated the efficacy of disc repositioning and anchorage with an orthodontic mini-screw for the treatment of internal derangement of TMJ. The purpose of surgical intervention was to prevent further disc displacement and simultaneously further prevent degeneration of the disc and arthritic changes in the condyle.
While many treatment modalities have been devised to alleviate the symptoms of TMJ dysfunction, few therapies are directed to correct the actual disease process. Variety of surgical procedures has been mentioned in the literature for to alleviate the symptoms of internal derangement including disc plication, discectomy, condylectomy, condylotomy, and eminectomy [3].
Disc-repositioning surgery can mitigate the degeneration caused by internal derangements by eliminating mechanical interferences and facilitating coordinated joint movement [8]. Appropriate position and morphological preservation of the disc are critical to preventing excess remodelling and degenerative changes within the TM joint [4]. Essentially, the disc acts as a biological cushion between the condyle and fossa and disperses the excessive forces that can promote joint destruction. The rationale for repositioning of the disc in our cases was to remove the mechanical impediment to the condylar movement and allow coordinated movements of the condyle with the disc and prevent further osteoarthritic changes on the condylar surface.
Weinberg and Cousens [9] proposed a technique of discocondylar plication for the surgical correction of the ectopic articular disc by retro positioning the disc and securing it with a Mersilene suture to the lateral surface of the condyle. Mehra and Wolford [1] described a procedure for the treatment of internal derangements of the TMJ in 105 patients, where they used a Mitek screw anchor to reposition the anteriorly displaced disc with 0-Ethibond sutures. Our procedure is similar to the technique described by the same authors, except that we used an orthodontic mini-screw instead of a Mitek screw. Although not designed for temporomandibular joint surgery, we consider the use of a mini-screw for disc anchoring technically more feasible and cost-effective.
We found significant improvement in Clinical dysfunction index as assessed post-operatively, with stable results up to 6-month post-operative period (Table 1). Pre-operatively clinical dysfunction index showed that six patients had moderate dysfunction of the joint, whereas four patients had severe dysfunction. There was significant reduction in the clinical dysfunction at 6 months with two patients clinically symptom free, 05 patients with mild dysfunction, and three patients with moderate dysfunction at the end of 6 months. The gradual increase in the mouth opening from the immediate post-operative to the 6-month follow-up could be attributed to the ensuing laxity of the capsule.
Torres and McCain [10] carried out arthroscopic electrothermal capsulorrhaphy for the treatment of recurrent temporomandibular joint dislocation and concluded that electrothermal shrinkage of the posterior TMJ capsule and attachments effectively limited forward translation of the mandibular condyle and ultimately prevented painful condylar subluxation. In our study, the capsular plication/capsulorrhaphy carried out during capsular closure further “tightens” the capsule, thus preventing dislocation of the condyle from a lax capsule since laxity of the capsule is one of the contributing factors for chronic subluxation.
According to Weinberg and Cousens [9], the technique of meniscocondylar plication, while permitting absolute movement between the disc and the temporal bone, virtually eliminated any relative movement between the disc and the condyle. By reducing the volume of the inferior joint space and increasing the capacity of the superior joint space, it essentially converted a diarthrodial joint to a monoarthrodial joint in which both hinge (ginglymoid) and sliding (arthrodial) condylar movements occurred in the superior joint space [9]. In our study too, anchoring the disc to the condyle essentially confined all condylar movements to the superior joint space.
Fields et al. [11] studied the pull-out strength of Mitek mini-anchors inserted in 20 human cadaver condyles, demonstrating an average pull-out load of 16.0 lb (range 8.5–28.4 lb). The pull-out strength of the orthodontic mini-implants range between 17.8 and 66.3 lb [12], and this strength appeared to be more than adequate to stabilize the disc to the anchor along with condylar movement.
Another factor to be considered in internal derangement is the influence of the muscles of mastication. Omami and Lurie [13], based on MRI findings, classified the anatomy of lateral pterygoid insertion of the superior head as: Type I: the superior head of lateral pterygoid inserted solely into the disc and Type II: the superior head of lateral pterygoid inserted into the disc and condyle. In our study, 2-0 nylon sutures securing the meniscus to the condyle act as artificial ligaments, counterbalancing the influence the lateral pterygoid has on the anterior displacement of the disc and condyle.
Unlike the Mitek screw technique where the screw head is flush with bone, our technique has the disadvantage of the orthodontic mini-screw head protruding from the surface of the condyle, but we have not encountered any complications or interference in condylar function with this. In summary, our technique aims to correct meniscocondylar conflicts by anchoring the disc to the condyle as a single unit minimizing condyle–disc conflicts. A capsulorrhaphy or capsule-tightening procedure performed reinforces the joint capsule around the condyle and disc, maintaining their anatomical relationship. Moreover, the posterior disc repositioning and securing it to the condyle would counter the anterior pull of the lateral pterygoid on the disc and condyle.
Conclusion
Our procedure addresses the fundamental aetiology of meniscocondylar derangement by anchoring the disc to the condyle and correcting condyle–disc disharmony. It is a reliable and cost-effective technique in our set-up with predictable stability as assessed over a period of 6 months. However, long-term changes in the meniscocondylar relationship and degenerative changes that may occur in the articular disc and over the articulating surface of the condyle need to be assessed.
Compliance with Ethical Standards
Conflict of interest
Authors declare that they have no conflict of interest.
References
- 1.Mehra P, Wolford LM. The Mitek mini anchor for TMJ disc repositioning: surgical technique and results. Int J Oral Maxillofac Surg. 2001;30(6):497–503. doi: 10.1054/ijom.2001.0163. [DOI] [PubMed] [Google Scholar]
- 2.Cai XY, Jin JM, Yang C. Changes in disc position, disc length, and condylar height in the temporomandibular joint with anterior disc displacement: a longitudinal retrospective magnetic resonance imaging study. J Oral Maxillofac Surg. 2011;69(11):e340–e346. doi: 10.1016/j.joms.2011.02.038. [DOI] [PubMed] [Google Scholar]
- 3.Quinn PD (1998) Surgery for internal derangements. In: Color atlas of temporomandibular joint surgery. Mosby Co., St Loius, pp 55–99
- 4.Kondoh T, Hamada Y, Kamei K, Seto K. Simple disc reshaping surgery for internal derangement of the temporomandibular joint: 5-year follow-up results. J Oral Maxillofac Surg. 2003;61:41–48. doi: 10.1053/joms.2003.50007. [DOI] [PubMed] [Google Scholar]
- 5.Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord. 1992;6:301–355. [PubMed] [Google Scholar]
- 6.Helkimo M. Studies on function and dysfunction of the masticatory system. Index for anamnestic and clinical dysfunction and occlusal state. Swed Dent J. 1974;67:101–121. [PubMed] [Google Scholar]
- 7.Ahmad M, Hollender L, Anderson Q, Kartha K, Ohrbach R, Trulove E, John M, Schiffman E. Research diagnostic criteria for temporomandibular disorders (RDC/TMD): development of image analysis criteria and examiner reliability for image analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:844–860. doi: 10.1016/j.tripleo.2009.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abramowicz S, Dolwick MF. 20-year follow-up study of disc repositioning surgery for temporomandibular joint internal derangement. J Oral Maxillofac Surg. 2010;68(2):239–242. doi: 10.1016/j.joms.2009.09.051. [DOI] [PubMed] [Google Scholar]
- 9.Weinberg S, Cousens G. Meniscocondylar plication: a modified operation for surgical repositioning of the ectopicmtemporomandibular joint meniscus. Rationale and operative technique. Oral Surg Oral Med Oral Pathol. 1987;63(4):393–402. doi: 10.1016/0030-4220(87)90247-7. [DOI] [PubMed] [Google Scholar]
- 10.Torres DE, McCain JP. Arthroscopic electrothermal capsulorrhaphy for the treatment of recurrent temporomandibular joint dislocation. Int J Oral Maxillofac Surg. 2012;41(6):681–689. doi: 10.1016/j.ijom.2012.03.008. [DOI] [PubMed] [Google Scholar]
- 11.Fields RT, Jr, Cardenas LE, Wolford LM. The pullout force for Mitek mini and micro suture anchor systems in human mandibular condyles. J Oral Maxillofac Surg. 1997;55(5):483–487. doi: 10.1016/S0278-2391(97)90697-2. [DOI] [PubMed] [Google Scholar]
- 12.Pithon MM, Figueiredo DS, Oliveira DD. Mechanical evaluation of orthodontic mini-implants of different lengths. J Oral Maxillofac Surg. 2013;71(3):479–486. doi: 10.1016/j.joms.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 13.Omami G, Lurie A. Magnetic resonance imaging evaluation of discal attachment of superior head of lateral pterygoid muscle in individuals with symptomatic temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114(5):650–657. doi: 10.1016/j.oooo.2012.07.482. [DOI] [PubMed] [Google Scholar]


