Abstract
Introduction
Technological advances in 3D printing can dramatically improve orthognathic surgical planning workflow. Custom positioning and cutting guides enable intraoperative reproduction of pre-planned osteotomy cuts and can result in greater surgical accuracy and patient safety.
Objectives
This short paper describes the use of freeware (some with open-source) combined with in-house 3D printing facilities to produce reliable, affordable osteotomy cutting guides.
Methods
Open-source software (3D Slicer) is used to visualise and segment three-dimensional planning models from imported conventional computed tomography (CT) scans. Freeware (Autodesk Meshmixer ©) allows digital manipulation of maxillary and mandibular components to plan precise osteotomy cuts. Bespoke cutting guides allow exact intraoperative positioning. These are printed in polylactic acid (PLA) using a fused-filament fabrication 3D printer. Fixation of the osteotomised segments is achieved using plating templates and four pre-adapted plates with planned screw holes over the thickest bone. We print maxilla/ mandible models with desired movements incorporated to use as a plating template.
Results
A 3D printer capable of reproducing a complete skull can be procured for £1000, with material costs in the region of £10 per case. Our production of models and guides typically takes less than 24 hours of total print time. The entire production process is frequently less than three days. Externally sourced models and guides cost significantly more, frequently encountering costs totalling £1500–£2000 for models and guides for a bimaxillary osteotomy.
Conclusion
Three-dimensional guided surgical planning utilising custom cutting guides enables the surgeon to determine optimal orientation of osteotomy cuts and better predict the skeletal maxilla/mandible relationship following surgery. The learning curve to develop proficiency using planning software and printer settings is offset by increased surgical predictability and reduced theatre time, making this form of planning a worthy investment.
Keywords: Orthognathic, 3D printing, Osteotomy, Surgical cutting guides
Introduction
Technological advances in three-dimensional (3D) printing and the availability of open-source software can dramatically improve orthognathic surgical planning workflow. Custom cutting and positioning guides enable intra-operative reproduction of pre-planned osteotomy cuts. Superior accuracy, better post-operative outcomes and increased patient safety are principle benefits.
Traditionally, obtaining custom guides is an expensive, protracted undertaking that requires design and production by remote technicians. We describe a cost-effective method of in-house 3D printing facilities to produce reliable, affordable custom guides.
Materials and Methods
Patients undergoing planning require pre-operative cone-beam or conventional computed tomography (CT). The CT dataset is exported in Digital Imaging and Communications in Medicine (DICOM) format. Image manipulation software (3D Slicer) is used to visualise and segment 3D planning models which are exported as triangular meshes into mesh manipulation software (Autodesk Meshmixer ©). Using this software, the meshes may be cut, joined and manipulated in virtual 3D space.
Osteotomy cuts can be performed using inbuilt functions. Bespoke cutting guides (Figs. 1, 2, 3) precisely adapt to the patient’s unique anatomical features (buccal shelf, piriform fossa, root form, etc.) allowing exact intra-operative positioning. Guides are printed in polylactic acid (PLA) using a fused filament fabrication 3D printer.
Fig. 1.
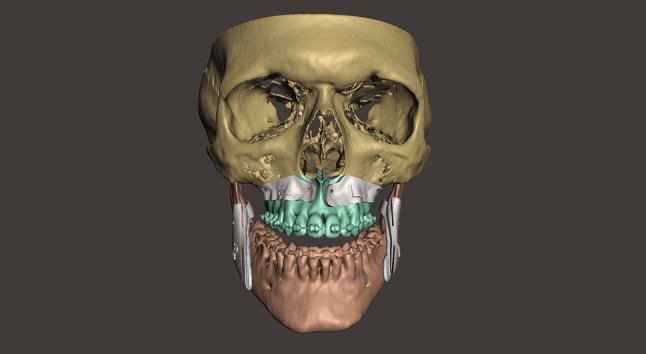
Digital planning model with osteotomy cutting guides positioned
Figs. 2, 3.

Intra-operative placement of maxillary cutting guide: thickness and edge angle can be varied
Fixation of the osteotomised segments is achieved using titanium plates which have been pre-adapted using a 3D printed plating template. This template incorporates the exact movements made with the 3D-planned screw holes that were incorporated into the cutting guides. The screw holes for the plates are incorporated into the cutting guide and drilled into the plating template when the cutting guide is tested for stability. The plates are then adapted to the template and screwed in position. Both plates and plating template are sent for sterilisation. When the cutting guides are applied intra-operatively, the screw holes are initially secured with 1.2- or 1.7-mm titanium screws. The guide is then removed, and the adapted plate utilises the same holes secured with 2.0-mm screws. We have had no problems with stability.
Occlusal splints are not required to maintain the maxillary position. The mandibular position is determined by the surgical plan and quality of the orthodontics. Good occlusal intercuspation will mean that no occlusal splint is required and minor occlusal adjustments can be made post-operatively.
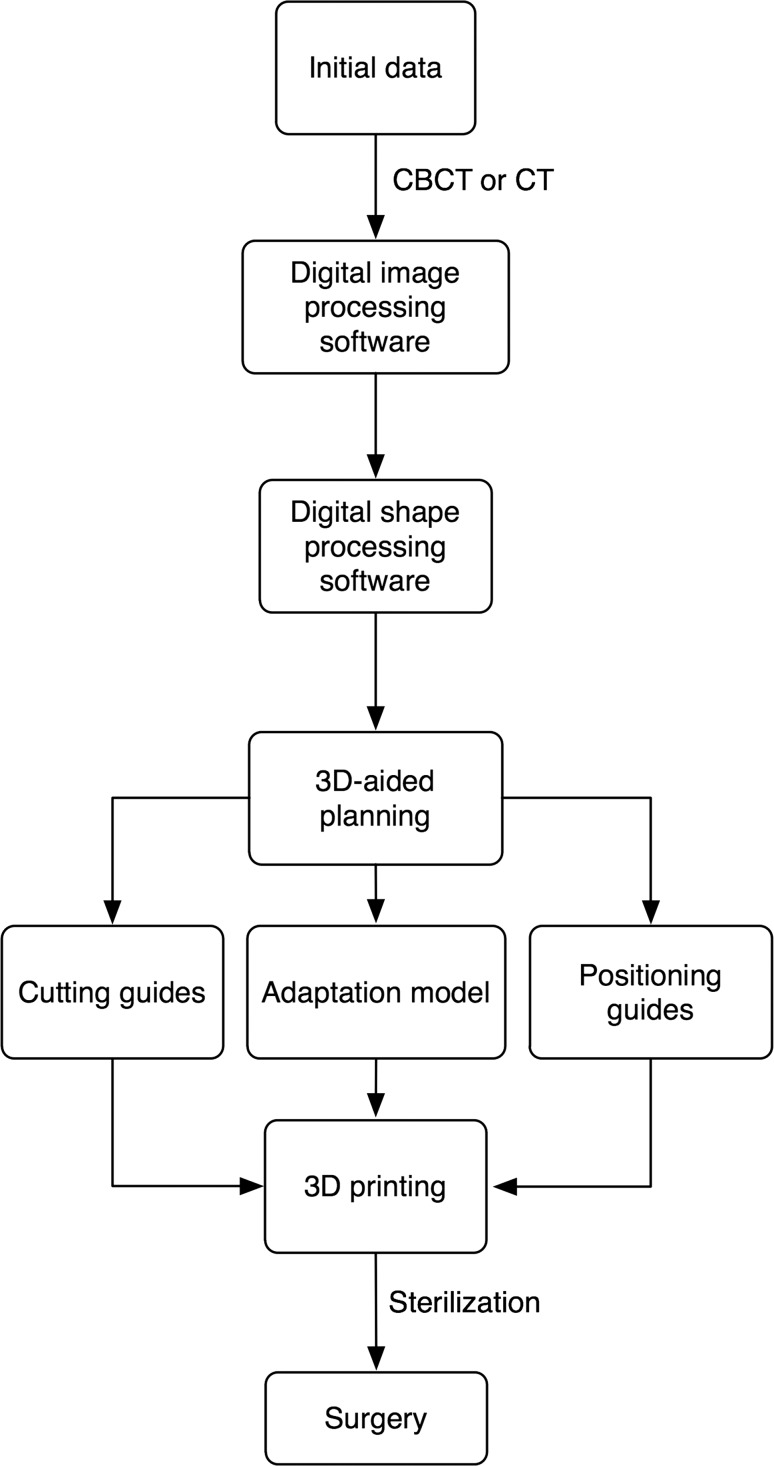
A simple workflow was developed (see Fig. 4), allowing junior and senior colleagues to plan their osteotomies.
Fig. 4.
Simple workflow demonstrates process from imaging through planning and printing to surgery
Discussion
Three-dimensional (3D) guided orthognathic surgical planning utilising custom cutting guides may well become the “gold standard” enabling the surgeon to determine optimal orientation of osteotomy cuts and better predict the skeletal maxilla/mandible relationship following surgery.
Planning lateral cephalograms or panoramic views are redundant using this method as a CT scan can easily be reformatted to provide both views if required and additionally provides the actual soft tissue profile rather than relying on hand tracing which is prone to error, especially in patients with significant asymmetry. More experience in planning in 3D means that reformatting to old two-dimensional views is seldom necessary. The entire production process is frequently less than 3 days, including 36 h for model and guide printing followed by ethylene oxide sterilisation at a regional sterilisation centre.
The integration of independent 3D guided orthognathic planning adds a further dimension to junior training roles, whilst its wafer-less technique reduces the workload for prosthetists. Anecdotally, our custom guides reduce operative duration, anaesthetic time and theatre costs. Independent planning allows direct communication with prosthetists allowing quick alterations. Patient confidentiality is maintained as no patient identifiable information is externalised.
A 3D printer with a print volume capable of reproducing a complete skull can be procured for £1000, with material costs in the region of £10 per case. The print time depends on the desired print quality. Our production of models and guides typically take less than 24-h total print time. Externally sourced models and guides cost significantly more, with frequently encountered costs totalling £1500–£2000 for models and guides for a bimaxillary osteotomy. Total production time, including scheduled video conferencing, can exceed a week excluding sterilisation.
There are technical limitations; useful software features such as collision detection found in expensive commercial software require custom code to be written if required using the software described. Also, printer settings take time to understand. The learning curve to develop proficiency using planning software is offset by increased surgical predictability and reduced theatre time, making this form of planning a worthy investment.
Compliance with ethical standards
Conflict of interest
The authors have no conflict to declare.
Ethics statement/confirmation of patients’ permission
No ethical approval required.