Abstract
Perioperative echocardiography, especially transesophageal echocardiography, is of paramount importance in evaluating and managing refractory hypotension, a potential cause of which is systolic anterior motion (SAM) of anterior mitral leaflet. Dynamically moving anterior mitral valve leaflet towards the left ventricular outflow tract (LVOT) is described as SAM. Although SAM was initially observed in patients with hypertrophic cardiomyopathy, it can also be seen in patients with complex dynamic anatomy of the left ventricle. Interestingly, SAM may or may not give rise to clinically significant LVOT obstruction. Hence, it is of paramount importance for perioperative physician to know such ‘dynamic SAM’ which can potentially and significantly affect and alter perioperative management.
Keywords: Systolic anterior motion, HOCM, MR, LVOT
In hypertrophic cardiomyopathy (HCM), papillary muscle displacement along with associated leaflet elongation can contribute to systolic anterior motion (SAM). Septal hypertrophy in HCM narrows left ventricular outflow tract (LVOT) and creates Venturi effect during systole dragging mitral valve into the LVOT.1 Mitral valve has adaptive reserve which prevents SAM. Systolic anterior motion is a result of complex geometric interaction between mitral valve components requiring significant Venturi and drag forces in the presence of good functioning left ventricle (LV). Disruption in dynamic mitral valvular apparatus, eg, after mitral valve repair can produce SAM. ‘Drag’ phenomenon is believed to be the most predominant cause of SAM, rather than Venturi.
Predisposing factors that cause SAM are (1) excessive anterior or posterior leaflet tissue; (2) any anatomical or surgical translocation of the mitral valve anteriorly; (3) aortomitral angle <120° (Figure 1; Supplementary Clip 1); (4) pathological or post-surgical correction elongation of the anterior leaflet; (5) annular undersizing in mitral valve repair; (6) chordal anomalies such as elongation and buckling; (7) surgical chordal interventions such as transection, translocation, and reimplantation; (8) anterior and medial displacement of the papillary muscles; (9) bulging subaortic septum; (10) absolute height of the posterior leaflet (>1.5 cm); (11) anterior to posterior leaflet height ratio (<1.4); and (12) minimum distance from the coaptation point to the septum (C-Sept, <2.5 cm).2
Figure 1.
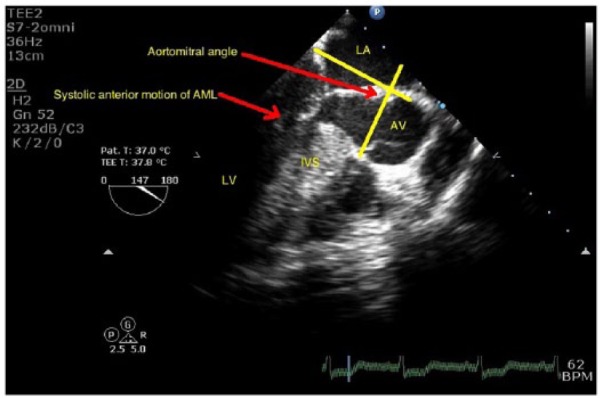
Transesophageal echocardiography midesophageal long-axis view showing systolic anterior motion of anterior mitral leaflet, bulging of interventricular septum, and aortomitral angle. AV indicates atrioventricular; IVS, interventricular septum; LA, left atrium.
In non-HCM hypertrophied ventricles, SAM peak is observed at the end of systole; however, SAM peaks in midsystole in patients with HCM.3 Systolic anterior motion of mitral leaflet is more likely to happen when anatomically susceptible heart is subjected to permissive physiological conditions that provoke SAM: ie, reduced preload, increased inotropic state, and decreased afterload.
Systolic anterior motion of the mitral valve can be graded echocardiographically:
No mitral leaflet-septal contact, minimum distance between the mitral valve and the ventricular septum during systole = 10 mm;
No mitral leaflet-septal contact, minimum distance between the mitral valve and the ventricular septum during systole <10 mm;
Brief mitral leaflet-septal contact (<30% of systole time);
Prolonged mitral leaflet-septal contact (>30% of systole time).
Complex congenital conditions such as accessory papillary muscle, cleft anterior mitral leaflet, subaortic stenosis,4 and transposition of the great arteries5 can also present SAM. Systolic anterior motion in post–aortic valve replacement (AVR) patients with pre-existing aortic stenosis can be observed due to drag on the anterior mitral leaflet because of raised blood velocity in the LVOT and small hypertrophied LV cavity.6 Paradoxically, SAM is uncommon in post-AVR patients operated for aortic regurgitation due to dilated LV with increased distance between mitral valve and LVOT and compensatory hypervolemia seen in these patients.7 Takotsubo cardiomyopathy rarely can present with SAM and left ventricular outflow tract obstructions because of mid and apical hypokinesia and compensatory basal hyperkinesias.8 Patients with diabetes may manifest SAM in the context of LV hypertrophy due to hyperdynamic state by raised β-adrenoreceptor sensitivity.9 Dobutamine stress echocardiography has also been reported to cause SAM by alteration of pathoanatomical features of mitral valve.10 It is like unmasking of anatomical features eliciting systolic movement of anterior mitral leaflet into LVOT.2 Post–myocardial infarction (MI) change in LV geometry due to opposition of hyperkinetic and hypokinetic regions after acute MI can sometimes result in SAM.11 This is clinically important because vasodilator and inotropic agents used in cardiogenic shock can actually worsen hemodynamics in such patients. Judicious use of β-blocker may benefit such patients.2 General anaesthesia, by its effect of vasodilation and hypovolemia, can sometimes provoke SAM even in the absence of any cardiac abnormality.2,12 Certain cardiac surgical procedures such as mitral valve repair can cause severe systolic anterior motion of mitral apparatus resulting in grade 2 to 4 mitral regurgitation (MR) with reported incidence of 9.1%. However correction of hyperdynamic status resolved SAM and reduced MR in more than half of these patients without further operative interventions.13
Risk assessment in patients with SAM is essential to decide WHICH SAM is clinically significant. Some methods are suggested: (1) tests to ameliorate SAM – administer fluid and vasopressor and look for reduction in SAM; (2) test to provoke SAM – administer nitroglycerin and rapid ventricular pacing and look for LVOT gradient.2
Pathophysiology of SAM clearly indicates that anatomically susceptible heart when subjected to hypovolemia, tachycardia, and reduced afterload can easily cause LV outflow obstruction with refractory hypotension. In patients with only mild SAM and MR, conservative medical therapy by volume administration, vasoconstriction, and β-blocker can be used to stabilize the patient. However, in cases with moderate or severe SAM and MR, medical therapy may be able to reduce SAM, but surgical options to address the underlying pathology causing SAM should be preferred to avoid long-term detrimental outcomes.2 It is essential for the perioperative physician to be aware of the variety of underlying conditions causing SAM and its clinical significance.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: MR and AM have conceptualised and written the manuscript. BS has edited the paper.
References
- 1. Lefebvre XP, He S, Levine RA, Yoganathan AP. Systolic anterior motion of the mitral valve in hypertrophic cardiomyopathy: an in vitro pulsatile flow study. J Heart Valve Dis. 1995;4:422–423. [PubMed] [Google Scholar]
- 2. Ibrahim M, Rao C, Ashrafian H, Chaudhry U, Darzi A, Athanasiou T. Modern management of systolic anterior motion of the mitral valve. Eur J Cardiothorac Surg. 2012;41:1260–1270. doi: 10.1093/ejcts/ezr232. [DOI] [PubMed] [Google Scholar]
- 3. Doi YL, McKenna WJ, Oakley CM, Goodwin JF. ‘Pseudo’ systolic anterior motion in patients with hypertensive heart disease. Eur Heart J. 1983;4:838–845. [DOI] [PubMed] [Google Scholar]
- 4. Iwata Y, Imai Y, Shin’oka T, Kurosawa H. Subaortic stenosis associated with systolic anterior motion. Heart Vessels. 2008;23:436–439. [DOI] [PubMed] [Google Scholar]
- 5. Zurick AO, III, Menon V. Dynamic outflow tract obstruction in congenitally corrected transposition of the great arteries. Int J Cardiovasc Imaging. 2010;26:617–619. [DOI] [PubMed] [Google Scholar]
- 6. Xu J, Wen J, Shu L, Liu C, Zhang J, Zhao W. Mechanism and correlated factors of SAM phenomenon after aortic valve replacement. J Huazhong Univ Sci Technolog Med Sci. 2007;27:72–74. [DOI] [PubMed] [Google Scholar]
- 7. Routledge T, Nashef SA. Severe mitral systolic anterior motion complicating aortic valve replacement. Interact Cardiovasc Thorac Surg. 2005;4:486–487. [DOI] [PubMed] [Google Scholar]
- 8. Dorfman TA, Iskandrian AE, Aqel R. An unusual manifestation of Takotsubo cardiomyopathy. Clin Cardiol. 2008;31:194–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Maraud L, Gin H, Roudaut R, Aubertin J, Bricaud H. Echocardiographic study of left ventricular function in type 1 diabetes mellitus: hypersensitivity of beta-adrenergic stimulation. Diabetes Res Clin Pract. 1991;11:161–168. [DOI] [PubMed] [Google Scholar]
- 10. Henein MY, O’Sullivan C, Sutton GC, Gibson DG, Coats AJ. Stress-induced left ventricular outflow tract obstruction: a potential cause of dyspnea in the elderly. J Am Coll Cardiol. 1997;30:1301–1307. [DOI] [PubMed] [Google Scholar]
- 11. Haley JH, Sinak LJ, Tajik AJ, Ommen SR, Oh JK. Dynamic left ventricular outflow tract obstruction in acute coronary syndromes: an important cause of new systolic murmur and cardiogenic shock. Mayo Clin Proc. 1999;74:901–906. [DOI] [PubMed] [Google Scholar]
- 12. Luckner G, Margreiter J, Jochberger S, et al. Systolic anterior motion of the mitral valve with left ventricular outflow tract obstruction: three cases of acute perioperative hypotension in noncardiac surgery. Anesth Analg. 2005;100:1594–1598. [DOI] [PubMed] [Google Scholar]
- 13. Freeman WK, Schaff HV, Khandheria BK, et al. Intraoperative evaluation of mitral valve regurgitation and repair by transesophageal echocardiography: incidence and significance of systolic anterior motion. J Am Coll Cardiol. 1992;20:599–609. [DOI] [PubMed] [Google Scholar]


