Abstract
Acute basilar artery occlusion (BAO) secondary to emergent large vessel occlusion (ELVO) has an extremely poor natural history, with a reported mortality rate up to 95%. Mechanical thrombectomy in the setting of ELVO is generally performed via a transfemoral approach. However, radial access is increasingly being utilized as an alternative. We report our initial multi-institutional experience using primary radial access in the treatment of acute BAO in nine consecutive cases. Technical success defined as a TICI score of 2B or 3 was achieved in 89% of cases. Average puncture to revascularization time was 35.8 minutes. There were no complications related to radial artery catheterization. We contend radial access should potentially be considered as the first-line approach given inherent advantages over femoral access for mechanical thrombectomy for BAO.
Keywords: Acute stroke, basilar artery occlusion, radial artery
Introduction
Mechanical thrombectomy for acute ischemic strokes has proven benefit over medical management in the treatment of distal internal carotid artery (ICA) and proximal middle cerebral artery (MCA) occlusions. Primary aspiration, stent retrievers or combined techniques are associated with high recanalization rates; routinely >80% at most high-volume centers. Time to recanalization and the degree of recanalization (based on thrombolysis in cerebral infarction (TICI)) grading are independent predictors of a good outcome. One potential target to shorten the time to recanalization is improved access techniques/approaches.
Most centers routinely triage acute ischemic stroke patients with computed tomography angiography (CTA) of the head and neck. Critical evaluation of the cervical vasculature can improve times by helping develop an access strategy focusing on the necessary supporting catheters and selective catheters. Alternatives to the traditional transfemoral approach include transradial and transcervical access, which have not been well described. Transradial approach to the posterior circulation is often facilitated by the natural orientation of the vertebral artery origin to the subclavian artery. Additionally, many operators use smaller guiding catheters for posterior circulation over the anterior circulation approach and a transcervical approach is not technically feasible.
In this study, we present our initial multicenter experience with basilar artery occlusions (BAOs) using a transradial approach with a focus on feasibility, safety, and technical success.
Radial access is increasingly being utilized as an alternative to the femoral approach for complex cerebrovascular intervention. Potential advantages include a lower incidence of access site complications (hematomas and pseudoaneurysms) and shorter procedure times given that vertebral artery access may be facilitated by a radial approach.1–3 We report our initial multi-institutional experience using primary radial access in the treatment of acute BAO in nine consecutive cases.
Methods
Patients
Following informed consent exemption by the respective institutional review boards, retrospective data were collected on all patients who received endovascular mechanical thrombectomy for basilar artery strokes in 2016 via radial access. In all cases radial access was the primary approach utilized, and this decision was made by the performing attending neurointerventionalist based on patient factors and proximal tortuosity based on pre-procedural CTA. All cases were performed under general anesthesia.
Access
In each case, patients were evaluated for distal ulnar-palmar arterial arch patency using a Barbeau test prior to radial artery access.4 All radial artery access procedures were performed with an ultrasound-guided single-wall Seldinger technique using a 0.021 micropuncture and 6 French vascular sheath (Terumo 6 Fr Glidesheath Slender) (see Figure 1). Sheath placement was immediately followed by intra-arterial infusion of 2000 u of heparin (1000 u/ml), 5 mg verapamil (2.5 mg/ml), and 200 mcg of nitroglycerin (100 mcg/ml).
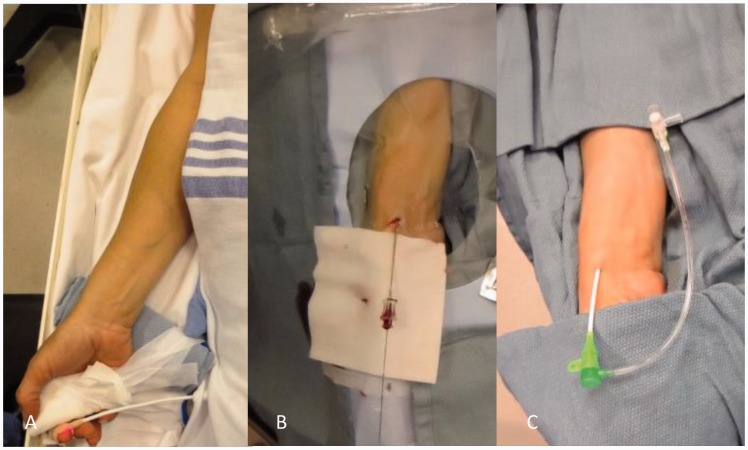
Figure 1.
The patient’s arm is first placed in a supinated position (a). Next, the wrist is slightly hyperextended, supported with a roll behind the wrist and secured with tape across the palm of the hand to the arm-board. Access is obtained using micropuncture needle and wire (b). Needle is removed and the 6-French introducer sheath is advanced over the wire (c). This is followed by infusion of the anti-spasm/occlusion cocktail.
Intervention
Mechanical thrombectomy was performed utilizing a combination of primary aspiration, stent retrievers or combined techniques. Stent retrievers included the Medtronic Solitaire 2 or Stryker Trevo Provue; lesional aspiration with stent retrievers or primary aspiration included use of the Penumbra MAX Reperfusion catheters, and the Penumbra aspiration pump) (see Figure 2).
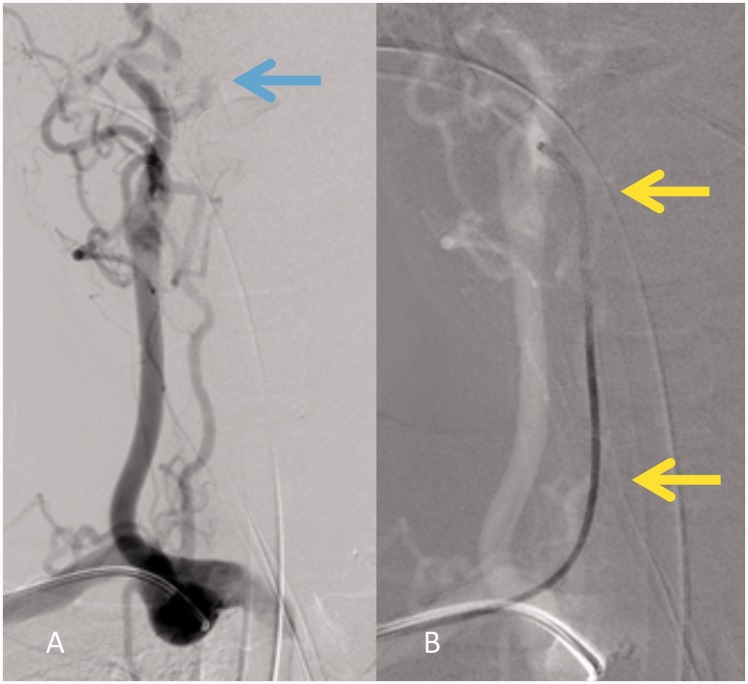
Figure 2.
Right subclavian artery angiogram (a) via a Penumbra ACE 64 Reperfusion catheter demonstrates poor flow in the right vertebral artery V4 segment (blue arrow). Under roadmap guidance (b) the Penumbra catheter (yellow arrows) was easily advanced into the vertebral artery over a Marksman microcatheter with a Fathom microwire.
Hemostasis
Following completion of the procedure the sheath was removed immediately after the intervention and patent hemostasis was achieved utilizing the TR Band radial compression device (Terumo).
Results
Eight patients underwent a total of nine procedures for acute BAOs, which were suspected to be thromboembolic in origin. Of those patients, the average age was 68 years old with a 1:1 male-to-female ratio. There were significant comorbidities in the majority of patients, including hypertension, coronary artery disease, and diabetes (see Table 1).
Table 1.
Comorbidities in the majority of patients, including hypertension, coronary artery disease, and diabetes.
| Age, years | 68.5 |
| SD = 10.2 | |
| Range = 57–80 | |
| Gender | |
| Male | 4 (50%) |
| Female | 4 (50%) |
| BMI | 29.7 |
| SD = 4.9 | |
| Range = 24.1–37.6 | |
| Comorbidity | |
| Hypertension | 8 (100%) |
| Hyperlipidemia | 8 (100%) |
| Diabetes | 6 (75%) |
| Coronary artery disease | 5 (62.5%) |
| Smoker (former or active) | 5 (62.5%) |
| Prior CVA | 2 (25%) |
| Atrial fibrillation | 1 (12.5%) |
| Peripheral vascular disease | 1 (12.5%) |
| Renal failure (GFR < 90 ml/min) | 1 (12.5%) |
| Medication history | |
| Aspirin | 6 (75%) |
| Clopidogrel | 1 (12.5%) |
| Anticoagulation | 1 (12.5%)a |
Noncompliant. BMI: body mass index; CVA: cardiovascular accident; GFR: glomerular filtration rate.
Pre-thrombectomy evaluation revealed a mean National Institutes of Health Stroke Scale (NIHSS) of 21 (see Table 2). Approximately 56% of cases presented with acute ischemic change on CT; however, all cases demonstrated a hyperdense basilar artery sign, with occlusion confirmed by CTA (see Figure 3). A total of 536 minutes elapsed on average from symptom onset until radial artery puncture.
Table 2.
Pre-thrombectomy evaluation mean National Institutes of Health Stroke Scale (NIHSS).
| # | Age (years) | Gender | NIHSS | Last known normal -> puncture (hours) | tPA | Puncture -> recanalization (mins) | Post-TICI | Intervention |
|---|---|---|---|---|---|---|---|---|
| 1 | 57 | F | 11 | 5.85 | No | 16 | 2B | Stent retriever + aspiration |
| 2 | 78 | M | 11 | 6.25 | Yes | 53 | 1 | Primary balloon angioplasty |
| 3 | 63 | M | 31 | 13.40 | No | 24 | 3 | Stent retriever + aspiration |
| 4 | 61 | M | 5 | 17.57 | No | 90 | 2B | Stent retriever |
| 5 | 61 | M | 30 | 2.40 | No | 19 | 2B | Stent retriever |
| 6 | 80 | F | 8 | 13.68 | No | 60 | 2B | Stent retriever + aspiration |
| 7 | 82 | F | 22 | 4.58 | No | 30 | 3 | Aspiration |
| 8 | 69 | F | 36 | 10.17 | No | 8 | 2B | Aspiration |
| 9 | 58 | M | 31 | 6.50 | No | 22 | 3 | Aspiration |
TPA: tPA: tissue plasminogen activator; TICI: thrombolysis in cerebral infarction; F: female; M: male.
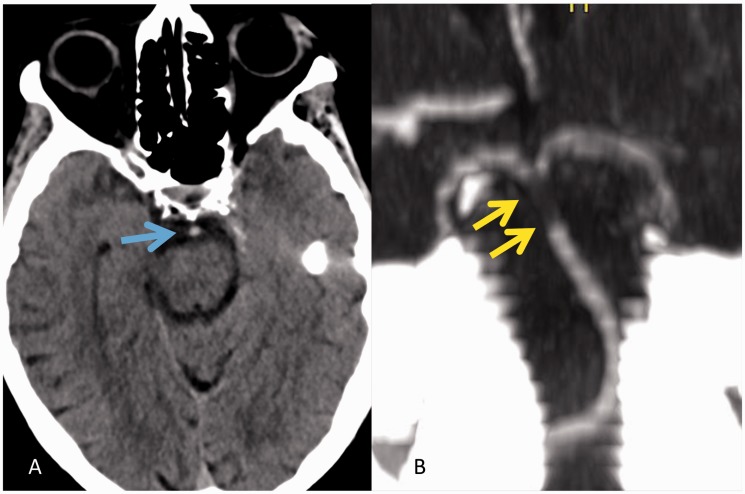
Figure 3.
Non-enhanced head CT (a) demonstrates a hyperdense basilar artery (blue arrow), which in our series was highly predictive of an acute occlusion. Thin-MIP CT angiography (b) image confirms the filling defect in the distal basilar artery (yellow arrow). CT: computed tomography; MIP CT: maximum intensity projection.
Although the left vertebral artery was dominant in one case, the right radial artery was accessed in all cases. All patients had complete BAOs, TICI 0, based on catheter angiography. Of these, 56% of the occlusions were in the distal basilar artery. Technical success defined as a TICI score of 2B or 3 was achieved in 89% of cases (eight out of nine). The one unsuccessful case, patient 2, received balloon angioplasty for a proximal stenosis; however, a thrombectomy system could not be advanced past the stenosis. The average puncture to revascularization time was 35.8 minutes. In three cases, a stent-retriever with lesion aspiration was performed. Aspiration-only (ADAPT) was performed in another three cases. There were no complications related to radial artery catheterization; however, two patients ultimately expired from complications of their stroke.
Discussion
Posterior circulation strokes represent approximately 15% of all ischemic strokes. Acute basilar artery occlusion (BAO) secondary to emergent large vessel occlusion (ELVO) has an extremely poor natural history, with a reported mortality rate up to 95%.5–7 Given its high associated morbidity and mortality, early revascularization may improve outcomes.
Mechanical thrombectomy in the setting of ELVO is generally performed via a transfemoral approach. However, a combination of developmental arch variants, great vessel origin tortuosity, and marked atherosclerotic calcification or occlusion of descending thoracic and abdominal aorta segments contribute to difficult or delayed access to the posterior circulation via a femoral artery approach.
Transradial access is increasingly becoming the standard of care for percutaneous coronary intervention (PCI) in the setting of acute coronary syndrome (ACS) in the United States and is already the standard of care in Europe and Asia. In randomized controlled cardiology trials, radial access is associated with high technical success and low associated complications when compared to transfemoral access.2 Radial access has been shown to have low rates of vascular complications including bleeding, pseudoaneurysm formation, and arterial occlusion.1–3
Radial access has also been adopted in the field of interventional radiology with similar success. A single-center study of 1512 consecutive non-coronary interventions performed via a radial approach demonstrated a 98.2% technical success rate with a 2.5% complication rate.8 Of these patients, one developed a major vascular complication (pseudoaneurysm) and less than 1% (11 patients) developed asymptomatic radial artery occlusion (RAO). RAO is typically asymptomatic because of good distal blood supply through the ulnar artery confirmed in most reported studies with preoperative testing of the distal palmar arch collateral supply.
Experience with a transradial approach for neurovascular procedures is more limited, but has been described as early as 2000.9 Diagnostic angiography, stenting, and coiling of the cerebral vasculature, in particular the vertebrobasilar system, have all been reported via a transradial approach.10 Patients undergoing cerebrovascular procedures have also reported a preference for radial access after previous femoral access.11 Barriers to the radial approach for neurointerventional procedures include lack of physician experience, concern about technical difficulty with selection of cervical and intracranial vasculature, and concern about radial injury and post-procedural hemostasis management. Despite these barriers to radial access in the neurovascular space, we contend radial access should be considered first given inherent advantages over femoral access for mechanical thrombectomy for BAO. Radial access should always be considered in the setting of failed femoral access and based on this initial experience, potentially be considered as the first-line approach. Generally, right radial access is more common for neurovascular procedures as the room (monitors and anesthesia) is generally set up for right common femoral access. In the setting of a hypoplastic right vertebral artery or a vertebral artery that terminates in the right posterior inferior cerebellar artery, primary left radial access can easy be performed. The radial artery can be accessed from the left side of the patient and then the arm secured across the body with tape or a restraint, thereby allowing the operator to work from the right side of the patient.
Recently, Haussen et al. described their experience with radial access in 15 out of 1001 acute ischemic patients.12 Thirteen of these patients underwent radial access in the setting of failed primary femoral access. In only two patients was there failure to engage the clot (hypoplastic radial artery and occlusion of the innominate artery). Successful recanalization (TICI 2B/3) was achieved in 60%; however, the average time from converting from femoral to radial access was 1.9 hours (±1.3 hours) and the average time from radial access to reperfusion was 2.2 hours (±1.0 hours).
In our analysis, we build on the existing literature and also demonstrate that transradial access is technically feasible for acute ischemic stroke interventions, specifically for BAO. Eighty-nine percent of our cases resulted in successful reperfusion, as graded by a TICI score of 2B or higher (see Figure 4). Case 2, which was unsuccessful in recanalization (less than TICI 2B), had a severe stenosis in the proximal basilar artery that despite balloon angioplasty would not dilate enough to allow the stent retriever system to adequately capture the thrombus in the distal basilar artery (see Figure 5). Ultimately a TICI 1 score was achieved. When compared to the results from the MR CLEAN trial, a TICI score of 2b or 3 was achieved in only 58.7% of patients.13 Additionally, our average recanalization times are comparable to the ADAPT FAST study (which used a primary transfemoral approach), of 36 minutes versus 37 minutes, respectively. These results suggest that transradial access for acute treatment of BAO is capable of delivering just as good recanalization outcome in a relatively quick time after arterial puncture.
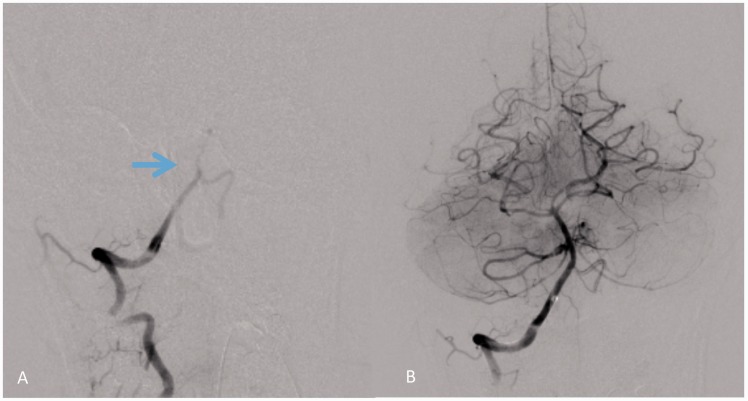
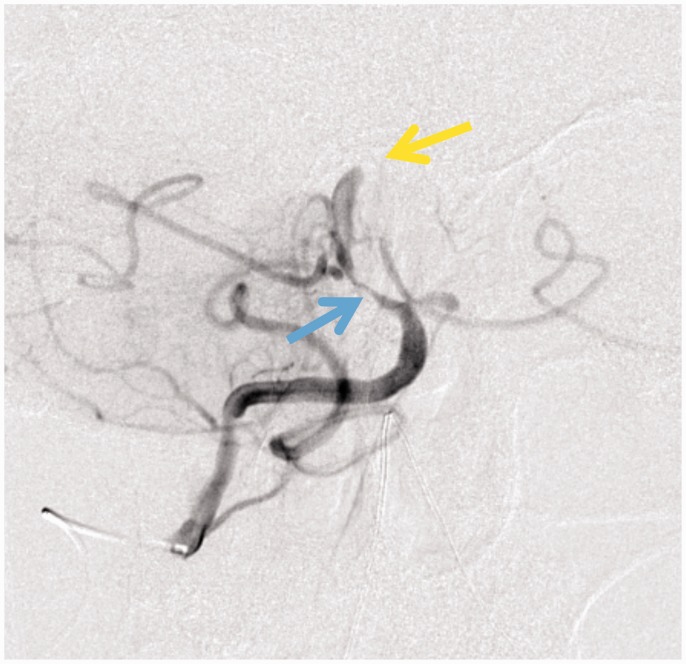
Figure 4.
Right vertebral artery injection (a) demonstrates proximal basilar artery occlusion (blue arrow), TICI 0. Following mechanical thrombectomy via a right radial approach, repeat injection (b) shows complete revascularization of the basilar artery territory, TICI 3. TICI: thrombolysis in cerebral infarction.
Figure 5.
Right vertebral artery injection demonstrates marked basilar artery stenosis (blue arrow) and distal occlusion (yellow arrow). Stenosis prevented advancement of the catheter construct for thrombectomy.
In summary, our initial experience suggests that the use of radial access for acute stroke interventions is technically feasible, associated with low rates of access site complications, and results in rapid recannulization of BAO in the setting of ELVO. In addition, a subset of patients with known challenging aortic arch anatomy (type II/III), atherosclerotic disease/occlusion of iliofemoral arteries, severe tortuosity of the innominate/left subclavian arteries, and morbid obesity may represent a subgroup of patients in whom primary radial access should be considered. The authors would caution that given the time-sensitive nature of the acute ischemic stroke, experience with radial access should be developed during elective routine cases. This experience would allow the angio suite staff to develop an approach to patient setup and preparation as well as allow the neurointerventionalist to develop confidence and strategies for cerebrovascular access with the available catheters and wires unique to each practice.
Conclusions
Radial access maybe a rapid viable approach to mechanical thrombectomy in selected patients with ELVO in the setting of BAO. In our initial experience, radial access was associated with high technical success and no major complications. Future studies should be prospectively designed and include a larger sample to further validate our conclusions.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Brueck M, Bandorski D, Kramer W, et al. A randomized comparison of transradial versus transfemoral approach for coronary angiography and angioplasty. JACC Cardiovasc Interv 2009; 2: 1047–1054. [DOI] [PubMed] [Google Scholar]
- 2.Agostoni P, Biondi-Zoccai GG, de Benedictis ML, et al. Radial versus femoral approach for percutaneous coronary diagnostic and interventional procedures: Systematic overview and meta-analysis of randomized trials. J Am Coll Cardiol 2004; 44: 349–356. [DOI] [PubMed] [Google Scholar]
- 3.Kotowycz MA, Džavík V. Radial artery patency after transradial catheterization. Circ Cardiovasc Interv 2012; 5: 127–133. [DOI] [PubMed] [Google Scholar]
- 4.Barbeau GR, Arsenault F, Dugas L, et al. Evaluation of the ulnopalmar arterial arches with pulse oximetry and plethysmography: Comparison with the Allen’s test in 1010 patients. Am Heart J 2004; 147: 489–493. [DOI] [PubMed] [Google Scholar]
- 5.Israeli-Korn SD, Schwammenthal Y, Yonash-Kimchi T, et al. Ischemic stroke due to acute basilar artery occlusion: Proportion and outcomes. Isr Med Assoc J 2010; 12: 671–675. [PubMed] [Google Scholar]
- 6.Yeung JT. Endovascular revascularization for basilar artery occlusion. Interv Neuroradiol 2015; 3: 31–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lindsberg PJ, Soinne L, Tatlisumak T, et al. Long-term outcome after intravenous thrombolysis of basilar artery occlusion. JAMA 2004; 292: 1862–1866. [DOI] [PubMed] [Google Scholar]
- 8.Posham R, Biederman DM, Patel RS, et al. Transradial approach for noncoronary interventions: A single-center review of safety and feasibility in the first 1,500 cases. J Vasc Interv Radiol 2016; 27: 159–166. [DOI] [PubMed] [Google Scholar]
- 9.Matsumoto Y, Hokama M, Nagashima H, et al. Transradial approach for selective cerebral angiography: Technical note. Neurol Res 2000; 22: 605–608. [DOI] [PubMed] [Google Scholar]
- 10.Bendok BR, Przybylo JH, Parkinson R, et al. Neuroendovascular interventions for intracranial posterior circulation disease via the transradial approach: Technical case report. Neurosurgery 2005; 56: 626. [DOI] [PubMed] [Google Scholar]
- 11.Satti SR, Vance AZ, Golwala SN, et al. Patient preference for transradial access over transfemoral access for cerebrovascular procedures. J Vasc Interv Neurol 2017; 9: 1–5. [PMC free article] [PubMed] [Google Scholar]
- 12.Haussen DC, Nogueira RG, DeSousa KG, et al. Transradial access in acute ischemic stroke intervention. J Neurointerv Surg 2016; 8: 247–250. [DOI] [PubMed] [Google Scholar]
- 13.Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015; 372: 11–20. [DOI] [PubMed] [Google Scholar]