Abstract
Background
Intracranial atherosclerotic disease may result in ischemic infarction and has a high rate of recurrent ischemic strokes despite medical therapy. Patients who fail medical therapy may undergo endovascular treatment with cerebral artery angioplasty and possible Wingspan stent placement. We present a unique case of Wingspan delivery microcatheter fracture that resulted in a retained foreign body and an endovascular salvage maneuver.
Case description
An elderly patient presented with an acute ischemic stroke due to a severe stenosis in the proximal left middle cerebral artery (MCA). The patient failed non-invasive medical treatment and underwent endovascular treatment with angioplasty and Wingspan stent placement. Following Wingspan stent deployment, the stent delivery catheter fractured, and the retained catheter fragment resulted in MCA occlusion. The foreign body was retrieved by balloon catheter inflation within an intermediate catheter adjacent to the proximal end of the fractured catheter and removal of the entire construct (TRAP technique).
Conclusions
Wingspan delivery microcatheter fracture is a rare event. The TRAP technique may be used for successful retrieval of a retained foreign body.
Keywords: Stroke, intracranial atherosclerotic disease, angioplasty, Wingspan, foreign body
Background
Ischemic stroke is caused by occlusion of a cerebral artery due to a thromboembolic event or in situ thrombosis of an intracranial artery. Ischemic stroke secondary to intracranial atherosclerotic disease (ICAD) may be caused by thrombosis of a diseased cerebral artery, a thromboembolic event secondary to ICAD plaque rupture, or ischemia secondary to poor perfusion.1 ICAD accounts for 5–10% of ischemic strokes in North America and up to 50% of ischemic strokes worldwide.2 ICAD is initially treated with non-invasive medical therapy that seeks to reduce the risk of cerebral infarction.1,3 However, patients who develop cerebral infarction or ongoing transient ischemic attacks despite optimal medical therapy may be considered for more aggressive treatment by cerebral angioplasty and/or cerebral artery stent placement.1,3,4 Wingspan (Boston Scientific) is a self-expanding nitinol stent approved for the treatment of ICAD patients with cerebral artery narrowing of at least 50% and symptoms referable to this stenosis despite maximum medical therapy. Cerebral angioplasty may also be performed either as monotherapy treatment of ICAD or as adjunctive treatment prior to Wingspan stent placement.4–6
We describe a patient with an acute ischemic stroke due to ICAD treated with Wingspan stent placement. Wingspan deployment was complicated by fracture of the delivery microcatheter, which was retained as a foreign body in the middle cerebral artery (MCA). We describe a unique technique (TRAP) for retrieval of the fractured microcatheter.
Case description
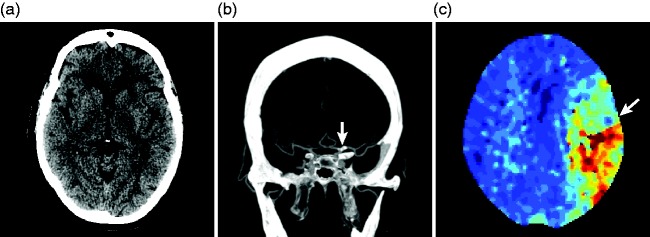
An elderly patient with a past medical history of hyperlipidemia, hypertension, and hypothyroidism presented to our emergency department with new right facial droop, speech impairment, and mild right-sided weakness. Initial National Institutes of Health Stroke Scale (NIHSS) score was 8. The time of symptom onset was unknown, so intravenous tissue plasminogen activator was not administered. Initial imaging showed no acute ischemic infarction on head computed tomography (CT) or computed tomographic perfusion (CTP), a densely calcified carotid terminus and M1 segment of the MCA with an associated severe stenosis on computed tomographic angiography (CTA), and a perfusion deficit on CTP (Figure 1). These imaging findings were interpreted as cerebral artery narrowing due to ICAD with a possible superimposed partially occlusive thrombus. A calcified thrombus as a cause of the stroke was also considered, but this diagnosis was less likely based upon the non-invasive imaging appearance.
Figure 1.
Presentation CT, CTA, and CTP in a patient with left MCA ICAD.
(a) Non-contrast head CT does not show any evidence of acute ischemic infarction. (b) Maximum-intensity projection images from a CTA demonstrate a calcified lesion with an associated severe stenosis in the left ICA terminus and M1 segment of the left MCA (arrow). (c) Time-to-maximum images from CTP demonstrate a perfusion deficit in the left MCA territory (arrow).
After a discussion with the patient’s family, who wished to be conservative, initial medical treatment was initiated with aspirin 325 mg, clopidogrel 600 mg loading dose, and blood pressure augmentation to a systolic blood pressure of 160–180 mm Hg per the recommendation of the treating neurointerventionalist and neurologist. The patient rapidly improved, with resolution of the speech impairment and restoration of full strength in the right arm and leg. However, several hours later, the patient developed weakness in the right upper and lower extremity. Repeat imaging by CT, CTA, and CTP was stable. The patient was deemed to have failed medical therapy, likely due to pial collateral vessel failure, and the patient’s family requested more aggressive treatment. The patient was transferred to the neurointerventional suite for endovascular treatment.
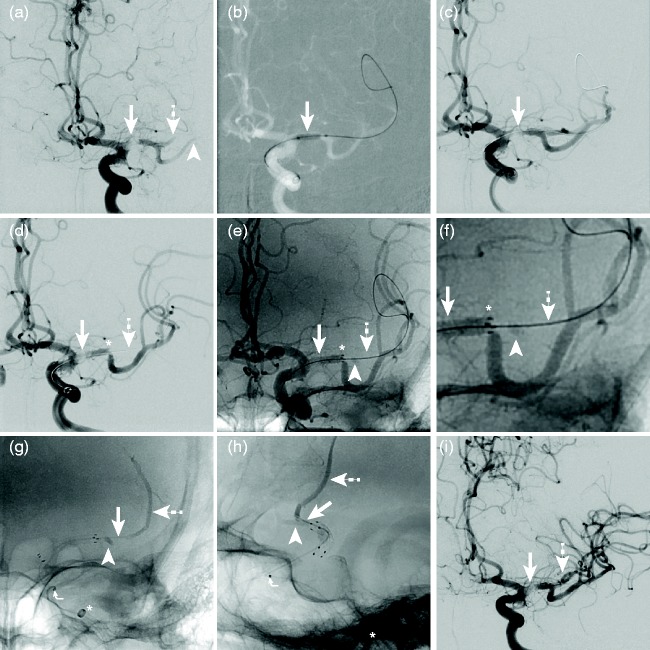
The right common femoral artery was accessed with a 6-French shuttle SL sheath (Cook Medical, Bloomington, IN). The cervical left internal carotid artery (ICA) was selected with a 5-French Berenstein catheter, and a left ICA digital subtraction angiography (DSA) showed severe narrowing within M1 segment of the left MCA with an associated filling defect extending from the left ICA terminus to the proximal M1 segment (Figure 2). The DSA appearance was consistent with either thrombosis of an underlying ICA terminus/M1 segment stenosis or a calcified embolus. Given that the lesion might represent a calcified embolus, aspiration thrombectomy with a large bore catheter (5-Max ACE, Penumbra Inc., Alameda, CA) was performed. However, this approach was unsuccessful, and the lesion remained unchanged after two aspiration attempts. The lesion was felt to be too high-risk to cross with a stentriever device given the risk of vessel rupture. The decision was made to perform angioplasty of the stenosis and thrombus with possible Wingspan stent placement in the event of angioplasty failure to improve flow to the left MCA.
Figure 2.
Cerebral angioplasty and Wingspan placement for left M1 stenosis treatment with retained foreign body.
Images (a)–(g) and (i) are in the anteroposterior (AP) projection. Image (h) is in the lateral projection. (a) Left ICA DSA demonstrates a partially occlusive filling defect and stenosis within the left ICA terminus and left M1 segment (arrow). Poor filling of the superior (dashed arrow) and inferior (arrowhead) post-bifurcation M1 segments is noted. (b) A balloon microcatheter is inflated across the left ICA terminus/M1 stenosis (arrow). (c) DSA following angioplasty demonstrates improved flow through the treated left ICA terminus/M1 stenosis (arrow). (d)–(f) Subtracted (d), unsubtracted (e), and magnified unsubtracted (f) angiographic images after Wingspan placement show an improved caliber of the left ICA terminus/M1 segment (arrows, (d)–(f)). The superior post-bifurcation M1 segment is now occluded (dashed arrows, (d)–(f)) distal to the Wingspan (*, (d)–(f)), and the microwire remains present within this segment. A new triangular density (arrowhead, (e), (f)) is present near the origin of the occluded post-bifurcation M1 segment. ((g), (h)) Unsubtracted AP (g) and lateral (h) views during Navien (*, (g), (h)) flushing demonstrates contrast opacification of a retained Wingspan delivery microcatheter fragment. A proximal marker in the retained catheter (curved arrow, (g), (h)) is present, and contrast (dashed arrows, (g), (h)) extends through the distal tip of the retained catheter (arrows, (g), (h)). The retained distal catheter tip abuts the triangular density identified after Wingspan deployment (arrowhead, (g), (h)). (i) Left ICA following successful retrieval of the fractured delivery catheter shows improved flow through the left ICA terminus/M1 stenosis (arrow) and recanalization of the post-bifurcation M1 segment that supplies the superior division (dashed arrow).
A 5-French Navien intermediate catheter (Medtronic Inc., Irvine, CA) was introduced through the shuttle sheath and positioned in the cavernous ICA. Next, a 2 × 8 mm percutaneous coronary balloon catheter was introduced into the Navien over a Synchro microwire, and the microwire and balloon were positioned across the stenosis in the left M1 segment. Gentle angioplasty to nominal pressure was then performed for treatment of the left M1 stenosis as previously described.4 A post-angioplasty DSA showed a mild improvement in the caliber of left MCA with a persistent severe stenosis, and it was felt that a superior and more durable result would be obtained by placement of a Wingspan stent.
The balloon catheter was removed, and a 2.5 × 15 mm Wingspan stent was easily advanced across the left M1 stenosis over the Synchro microwire. The stent was deployed across the M1 stenosis without difficulty (Figure 2). The microwire was left in position, and the Wingspan delivery microcatheter was removed.
A post-stent deployment angiogram demonstrated significant improvement in the caliber of the left ICA terminus and M1 segment. However, there was new non-filling of the post-bifurcation M1 segment that supplied the left MCA superior division (Figure 2). Careful inspection of the unsubtracted images demonstrated a new triangular radiopaque density distal to the Wingspan stent within proximal aspect of the now occluded post-bifurcation M1 segment (Figure 2). In addition, a linear radiopaque foreign body was identified that extended from the Wingspan stent proximally to the mid-section of the Navien intermediate catheter lumen proximally (Figure 2). Flushing of the Navien with heparinized saline after this angiogram identified a retained microcatheter fragment with its distal tip lodged in the origin of the occluded post-bifurcation M1 segment (Figure 2). Contrast from the prior angiographic run had filled this fractured microcatheter fragment and was expunged into the left MCA superior division following flushing of the Navien (Figure 2). All equipment was then examined on the back table, and it was determined that the Wingspan stent delivery microcatheter had fractured. A significant length (approximately 25 cm) of the distal aspect of this catheter and the nose cone were missing, which accounted for the new radiopaque foreign body in the patient.
A snare device to retrieve the foreign body was considered, but it was felt that capturing the proximal end of the fractured catheter within the Navien would be difficult. We used the following method, which we have termed “TRAP,” to retrieve the fractured catheter fragment (Supplementary Videos 1 and 2). The previously used coronary balloon catheter was advanced through the Navien such that it was immediately adjacent to the proximal aspect of the fractured microcatheter. The balloon catheter was then firmly inflated within the Navien such that the fractured microcatheter was trapped between the inflated balloon and inner wall of the Navien. The Navien distal access catheter was carefully withdrawn into the 6 French 80 cm shuttle sheath and removed from the patient. The entirety of the retained foreign body was removed from the patient with the Navien intermediate catheter. The balloon was then deflated, and the length of retained fractured catheter was compared with the other section of the delivery catheter. It was determined that the entire length of the Wingspan delivery catheter had been recovered. A post-retrieval cerebral angiogram demonstrated complete recanalization within the post-bifurcation M1 segment that supplied the superior division.
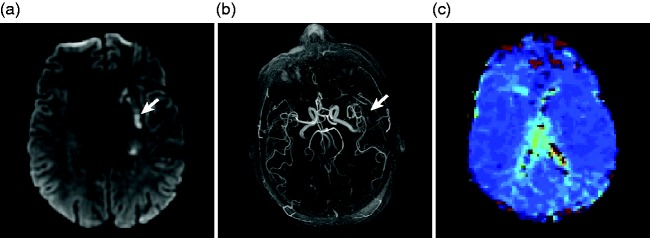
Following the procedure, the patient improved neurologically, and there was no increase in the size of infarction on MRI (Figure 3). The patient was discharged on post-operative day 6 with a stable neurological exam of NIHSS of 6. At 3 months of follow-up, the patient had improved to a NIHSS of 2 and a modified Rankin Scale score of 1.
Figure 3.
MRI, MR angiogram, and MR perfusion following Wingspan placement and foreign body retrieval.
(a) Diffusion-weighted imaging shows a small cerebral infarction in the left cerebral corona radiata (arrow) and caudate. (b) Maximum-intensity projection images from a MR angiogram demonstrate excellent flow-related signal in the left MCA vessels (arrow). (c) Time-to-maximum images from MR perfusion demonstrate no residual perfusion deficit in the left MCA territory.
Discussion
Symptomatic ICAD may result in ischemic infarction and has a high rate of recurrent ischemic strokes despite medical therapy.5,7 In the Warfarin-Aspirin Symptomatic Intracranial Disease (WASID) trial, 21–22% of patients presenting with high grade stenosis experienced recurrent stroke in the ipsilateral territory within 2 years, despite treatment with aspirin or warfarin.7 The Stenting and Aggressive Medical Management for Preventing Recurrent Stroke in Intracranial Stenosis (SAMMPRIS) trial randomized patients with ICAD to medical therapy or endovascular treatment with angioplasty and possible Wingspan stent placement.8 The SAMMPRIS trial was halted after an interim analysis showed that the frequency of cerebral infarction and death was markedly lower with aggressive medical management (5.8%) than with endovascular treatment with angioplasty and Wingspan stent placement (14.7%).8 The medical management arm in SAMMPRIS was treated with aspirin, clopidogrel, and high-dose atorvastatin, and ischemic infarction and death occurred with a lower frequency than was anticipated.8 Current medical management of ICAD is largely based on the medical arm of SAMMPRIS.1 The safety of endovascular ICAD treatment has subsequently been questioned due to the high periprocedural rates of stroke and death in the SAMMPRIS trial,8 and the Food and Drug Administration (FDA) has limited the indications for the Wingspan stent. However, in patients with ICAD who have ischemic stroke or transient ischemic attacks while on maximal medical therapy, endovascular treatment with angioplasty and possible Wingspan stent placement may be considered by most neurointerventionalists.
Here we describe a patient who underwent endovascular treatment of ICAD with angioplasty and Wingspan stent placement. Following successful stent deployment, we identified fracture of the Wingspan stent delivery catheter that resulted in occlusion of post-bifurcation M1 segment. The cause of the delivery catheter fracture is unclear. The arterial stenosis was easily crossed by the microwire and the Wingspan stent delivery catheter, and the stent deployed smoothly and without difficulty. Prior reports of Wingspan stent system fracture may suggest that there is a low, but real, risk of failure of this product during device deployment.
Wingspan stent system fracture and temporary retention of the nose cone of the Wingspan system has been described in two different patients.9 However, it is unclear from these reports whether the stent itself fractured or whether the delivery catheter fractured. Furthermore, the maneuvers undertaken to salvage these endovascular complications were not described.9 To our knowledge, we describe the first clear report of Wingspan delivery catheter fracture. We recommend careful inspection of the Wingspan delivery catheter after stent deployment to identify this potential complication. Additionally, Wingspan should always be used with foreknowledge of the FDA’s requirements and advice.
Retained catheter fragments may be retrieved using snares.10 In our patient, the proximal end of the fractured delivery catheter remained in the Navien intermediate catheter, and the use of a snare to retrieve the catheter was felt to be technically challenging. The use of our newly described TRAP technique was effective in retrieving the fractured catheter fragment, which resulted in restoration of flow to the left MCA.
Our patient made an excellent neurologic recovery and continues to do well after treatment. In describing this case, we hope to make neurointerventionalists aware of possible Wingspan delivery catheter fracture and to provide them with a unique method of foreign body retrieval.
Conclusions
Cerebral artery angioplasty and possible Wingspan stent placement for the treatment of ischemic stroke due to ICAD may result in good clinical outcomes. Although rare, fracture of the Wingspan stent delivery system may result in a retained foreign body. The TRAP technique is effective for retained microcatheter fragment retrieval.
Supplementary Material
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Heit JJ and Wintermark M. New developments in clinical ischemic stroke prevention and treatment and their imaging implications. J Cereb Blood Flow Metab. Epub ahead of print 1 January 2017. DOI: 10.1177/0271678X17694046. [DOI] [PMC free article] [PubMed]
- 2.Gorelick PB, Wong KS, Bae HJ, et al. Large artery intracranial occlusive disease: A large worldwide burden but a relatively neglected frontier. Stroke 2008; 39(8): 2396–2399. [DOI] [PubMed] [Google Scholar]
- 3.Qureshi AI, Caplan LR. Intracranial atherosclerosis. Lancet 2014; 383(9921): 984–998. [DOI] [PubMed] [Google Scholar]
- 4.Marks MP, Marcellus M, Norbash AM, et al. Outcome of angioplasty for atherosclerotic intracranial stenosis. Stroke 1999; 30(5): 1065–1069. [DOI] [PubMed] [Google Scholar]
- 5.Fiorella D, Levy EI, Turk AS, et al. US multicenter experience with the wingspan stent system for the treatment of intracranial atheromatous disease: Periprocedural results. Stroke 2007; 38(3): 881–887. [DOI] [PubMed] [Google Scholar]
- 6.Zhang L, Huang Q, Zhang Y, et al. Wingspan stents for the treatment of symptomatic atherosclerotic stenosis in small intracranial vessels: Safety and efficacy evaluation. AJNR Am J Neuroradiol 2012; 33(2): 343–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chimowitz MI, Lynn MJ, Howlett-Smith H, et al. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. The New England journal of medicine. 2005; 352(13): 1305–1316. [DOI] [PubMed] [Google Scholar]
- 8.Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, Lane BF, et al. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med 2011; 365(11): 993–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yu SC, Leung TW, Lee KT, et al. Learning curve of Wingspan stenting for intracranial atherosclerosis: Single-center experience of 95 consecutive patients. J Neurointerv Surg 2014; 6(3): 212–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Funatsu A, Kobayashi T, Nakamura S. Successful retrieval of a broken intravascular ultrasound catheter tip in the coronary artery. J Invasive Cardiol 2010; 22(10): E197–200. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.