Abstract
Objective
Childhood conduct problems are associated with poor functioning in early adulthood. We tested a series of hypotheses to understand the mechanisms underlying this association.
Method
We used data from the Environmental Risk (E-Risk) Longitudinal Twin Study, a birth cohort of 2,232 twins born in England and Wales in 1994 and 1995, followed up to age 18 years with 93% retention. Severe conduct problems in childhood were assessed at ages 5, 7, and 10 years using parent and teacher reports. Poor functioning at age 18 years, including cautions and convictions, daily cigarette smoking, heavy drinking, and psychosocial difficulties, was measured through interviews with participants and official crime record searches.
Results
Participants 18 years old with versus without a childhood history of severe conduct problems had greater rates of each poor functional outcome, and they were more likely to experience multiple poor outcomes. This association was partly accounted for by concurrent psychopathology in early adulthood, as well as by early familial risk factors, both genetic and environmental. Childhood conduct problems, however, continued to predict poor outcomes at age 18 years after accounting for these explanations.
Conclusion
Children with severe conduct problems display poor functioning at age 18 years because of concurrent problems in early adulthood and familial risk factors originating in childhood. However, conduct problems also exert a lasting effect on young people’s lives independent of these factors, pointing to early conduct problems as a target for early interventions aimed at preventing poor functional outcomes.
Key words: conduct problems, functional outcomes, longitudinal, externalizing problems
From Lee Robins’ seminal publication of Deviant Children Grown Up more than 50 years ago1 to a recent meta-analysis of more than 30 empirical studies,2 a wealth of evidence links early childhood conduct problems to poor adult outcomes. The long-term sequelae of conduct problems extend beyond mental illness to encompass poor functioning across other areas of life, such as education and employment, criminal offending, health and well-being, and social relationships.3, 4, 5 Despite the burden that poor functional outcomes place on young adults and public services, little is known about why children with conduct problems fare poorly years later. We tested a series of hypotheses about potential explanations for the link between conduct problems in childhood and worse functioning in early adulthood, at age 18 years.
First, poor functioning in early adulthood may be the result of continuity in psychopathology from child to adult life, rather than a developmental outcome of conduct problems during childhood. Children who display conduct problems are at risk for continuing to exhibit behavioral problems into early adulthood6 and for developing other types of psychopathology, such as depression and anxiety.7 Psychopathology in early adulthood is associated with poor functioning,8, 9 raising the possibility that conduct problems during childhood predict later functioning because of their association with young-adult mental health problems.10 This hypothesis has rarely been tested, because most studies investigating the young-adult sequelae of childhood conduct problems examine mental illness as an outcome alongside poor functioning. To the extent that the association is due to young-adult psychopathology, treating young adults who experience mental health problems will reduce their poor functioning.
Second, childhood conduct problems and poor young-adult functioning may be associated because they share the same risk factors. Children who grow up in socioeconomically disadvantaged families have greater rates of conduct problems compared to their more privileged peers,11 and growing up in poverty is a major risk factor for poor functional outcomes.12, 13 Similar findings have been reported for children exposed to violence at a young age14, 15 or with parents who themselves display psychopathology, such as antisocial behavior or depression.16, 17 Socioeconomic disadvantage, violence exposure, and parental psychopathology could therefore explain why a childhood history of conduct problems is associated with poor functioning.
Third, in addition to well-established risk factors for childhood problems and poor outcomes later in life, there may be additional familial environmental and genetic influences contributing to their association. Twin and adoption studies show that genetic influences and, to a lesser extent, shared environmental influences contribute to childhood conduct problems and young-adult functioning,18, 19, 20 raising the possibility that both originate in the same familial risk factors. By comparing young twins growing up in the same family, who share the same environment and, in the case of identical twins, the same genes, it is possible to capture familial influences and to determine the extent to which children’s conduct problems predict poor outcomes independent of latent familial risks. To the extent that the association is due to well-established familial risk factors and additional familial environmental and genetic influences, interventions aimed at improving the future functioning of children with conduct problems should address factors in a child’s family environment, for example, through work with parents. To the extent that conduct problems in childhood predict outcomes above and beyond these factors, early, individual-level treatment of children’s problem behavior may improve future poor functioning.
We tested these potential explanations in a longitudinal prospective cohort of twin children who have been followed up to age 18 years. We investigated the extent to which childhood conduct problems predicted poor functioning in emerging adulthood. Our focus was on severe conduct problems with an early onset because they have a particularly poor long-term prognosis.21 The outcomes that we examined reflect individuals’ functioning in emerging adulthood across areas in which positive outcomes are critical for successful life-course development, such as attainment, health, and social inclusion. In addition to testing whether childhood conduct problems predicted each outcome separately, we also tested the effect on the accumulation of poor functional outcomes, that is, a cumulative index of poor functioning, because recent evidence has documented that individuals who function poorly in one area often experience difficulties in other areas as well.22
Method
Participants
Participants were members of the Environmental Risk (E-Risk) Longitudinal Twin Study, which tracks the development of a birth cohort of 2,232 British children. The sample was drawn from a larger birth register of twins born in England and Wales in 1994 to 1995.23 Full details about the sample are reported elsewhere.24 Briefly, the E-Risk sample was constructed in 1999 to 2000, when 1,116 families (93% of those eligible) with same-sex 5-year-old twins participated in home-visit assessments. This sample comprised 56% monozygotic (MZ) and 44% dizygotic (DZ) twin pairs; sex was evenly distributed within zygosity (49% male). Families were recruited to represent the UK population of families with newborns in the 1990s, on the basis of residential location throughout England and Wales and mother’s age. Teenage mothers with twins were overselected to replace high-risk families who were selectively lost to the register through nonresponse. Older mothers having twins via assisted reproduction were underselected to avoid an excess of well-educated older mothers. At follow-up, the study sample represents the full range of socioeconomic conditions in the United Kingdom, as reflected in the families’ distribution on a neighborhood-level socioeconomic index.25, 26
Follow-up home visits were conducted when the children were aged 7 (98% participation), 10 (96%), 12 (96%), and 18 (93%) years. At age 18 years, 2,066 participants were assessed, each twin by a different interviewer. The average age at the time of assessment was 18.4 years (SD = 0.36); all interviews were conducted after the 18th birthday. Of the age-18 participants, 70.8% were studying for a degree at university or a vocational qualification, and 56.6% were working. Of the participants, 11.6% were neither studying nor working.
There were no differences between those who did and did not take part at age 18 years in terms of socioeconomic status (SES) assessed when the cohort was initially defined (χ2 = 0.86, p = .65), age-5 IQ scores (t = 0.98, p = .33), or age-5 behavioral or emotional problems (t = 0.40, p = .69 and t = 0.41, p = .68, respectively). The Joint South London and Maudsley and the Institute of Psychiatry Research Ethics Committee approved each phase of the study. Parents gave informed consent, and twins gave assent between 5 and 12 years and then informed consent at age 18 years.
Childhood History of Conduct Problems
When the twins were 5, 7, and 10 years of age, 14 of 15 DSM-IV symptoms of conduct disorder were assessed (forced sexual activity was considered age inappropriate and thus not included) through mothers’ and teachers’ reports of children’s behavioral problems, using the Achenbach family of instruments and DSM-IV items.27, 28, 29 A child was considered to have a given symptom if it was scored as being “very true or often true” (score = 2) in the past 12 months, by either mothers or teachers, to enhance diagnostic validity.30, 31 To focus our analyses on children with moderate to severe conduct problems and following DSM-IV recommendations,29 participants were categorized into those who had not versus had displayed 5 or more symptoms at the age 5-, 7-, or 10-year assessment (n = 307, 14.5%). More detail about the percentage of children meeting this criterion at each age and across ages is provided in Supplement 1, available online. Findings were similar when using different symptom thresholds to categorize participants as having a history of conduct problems (see Tables S1 and S2, available online).
Poor Outcomes in Early Adulthood
We collected information on 10 outcomes that reflected young adults’ poor functioning in areas critical to life-course development. Outcomes and their assessment are described in Table 1 and in Supplement 1, available online. Information on the majority of outcomes was ascertained at the age-18-year interview; cautions and convictions were assessed through UK Police National Computer (PNC) record searches. NEET status (Not in Education, Employment or Training),32 parenthood, daily cigarette smoking, and suicide attempts/self-harm were naturally dichotomous; all other variables were dichotomized. For variables with no predetermined cut-off (drinking, social isolation, and low life satisfaction), we defined poor functioning a priori as being among the 20% highest-scoring participants in an outcome. Findings were similar when using different thresholds (see Table S3, available online).
Table 1.
Descriptive Information for Age-18 Functional Outcomes
| Outcomes | Definition | Prevalence (%) |
||
|---|---|---|---|---|
| Total | Boys | Girls | ||
| NEET | NEET status as self-reported in the age-18 interview | 11.6 | 11.0 | 12.1 |
| Parenthood | Any past live birth or current pregnancy (girls) or having caused a pregnancy that resulted in a live birth (boys) self-reported in the age-18 interview | 2.6 | 1.1 | 4.0 |
| Cautions and convictions | Official record of any UK cautions or convictions, beginning at age 10 through age 19 | 10.2 | 15.4 | 5.5 |
| Overweight | BMI ≥25, assessed at the time of the age-18 interview | 25.8 | 22.7 | 28.7 |
| Daily cigarette smoking | Current, daily smoking self-reported in the age-18 interview | 22.3 | 23.5 | 21.3 |
| Heavy drinking | High (among top 20% of participants) self-reported consumption of alcoholic drinks in a typical week at the time of the age-18 interview | 20.3 | 25.6 | 15.5 |
| Visits to ED | Any visits to an ED within past year, self-reported in the age-18 interview | 20.8 | 22.8 | 19.0 |
| Suicide attempts/self-harm | Any suicide attempts or incidents of self-harm between ages 12 and 18 years, self-reported in the age-18 interview | 14.3 | 10.5 | 17.6 |
| Social isolation | High score (among top 20% of participants) on a self-report scale reverse-coded to assess social isolation at age 18 years | 20.0 | 24.0 | 16.5 |
| Low life satisfaction | High score (among top 20% of participants) on self-report scale reverse-coded to assess low life satisfaction at age 18 years | 18.7 | 19.9 | 17.6 |
Note: Further information on all outcomes is provided in Supplement 1, available online. BMI = body mass index; ED = emergency department; NEET = Not in Education, Employment, or Training.
Young-Adult Psychopathology
During the age-18 interview, we assessed participants’ mental health over the previous 12 months, including depressive disorder, generalized anxiety disorder, posttraumatic stress disorder (PTSD), alcohol dependence, cannabis dependence, and conduct disorder according to DSM-IV33 and attention-deficit/hyperactivity disorder (ADHD) according to DSM-5 criteria.34 Assessments were conducted in face-to-face interviews using the Diagnostic Interview Schedule (DIS).35 We used a summary measure indicating whether participants experienced any of these mental health problems at age 18 years.
Risk Factors for Childhood Conduct Problems and Young-Adult Poor Functioning
Families’ socioeconomic disadvantage was defined at age 5 years using a standardized composite of parents’ income, education, and social class,36 divided into tertiles and reverse coded. Child exposure to violence was indexed by child physical maltreatment and domestic violence by age 5 years, as previously described.6, 37 Briefly, child physical maltreatment by an adult was assessed for each twin during family visits using the standardized clinical protocol from the Multi-Site Child Development Project.38, 39 Interviewers coded the child as having not been, or as having possibly or definitely been, physically harmed on the basis of the mothers’ narrative, with intercoder agreement on 90% of ratings (κ = 0.56). Adult domestic violence was assessed by asking mothers about their own violence toward any partner and about partners’ violence toward them during the 5 years since the twins’ birth, responding “not true” or “true” to questions about 12 acts of physical violence. The measure was dichotomized to reflect whether children lived in homes where there was any versus no adult domestic violence. Parental psychopathology was indexed by parents’ antisocial behavior and mothers’ depression.37, 40 Fathers’ and mothers’ history of antisocial behavior was reported by mothers when children were 5 years old, using the Young Adult Behavior Checklist,41 modified to obtain lifetime data and supplemented with questions from the DIS.35 We combined reports about mothers’ and fathers’ behavior. Mothers’ major depressive disorder since the twins’ birth was assessed when the children were 5 years old according to the DSM-IV,33 using the DIS.35
Statistical Analyses
We tested whether a childhood history of severe conduct problems predicted each poor functional outcome at age 18 separately, and also a cumulative index of poor functioning, using Poisson regression models. We chose Poisson over logistic regression models for the dichotomous outcomes to obtain risk ratios,42 which are a more easily interpretable measure of risk, particularly when outcomes are common. To test whether the effect of childhood conduct problems on functioning was accounted for by young-adult psychopathology and specific family risk factors, we included these as additional predictors in our regression models. We compared results across sex and observed similar patterns of results. We adjusted for sex in all analyses. Standard errors in all models were adjusted for clustering of twins within families. To test whether childhood conduct problems predicted age-18 outcomes within twin pairs growing up in the same family, we used a discordant twin design, with fixed effects models and robust standard errors.43 The resulting estimates indicate whether a twin with a childhood history of conduct problems is more likely to experience poor functional outcomes compared to that individual’s unaffected co-twin, accounting for familywide environmental and, in MZ twins, genetic influences that may increase the risk for both conduct problems and young-adult functional outcomes. Stata version 14.1 was used for all analyses.44
Results
Association Between Childhood Conduct Problems and Poor Functional Outcomes in Early Adulthood
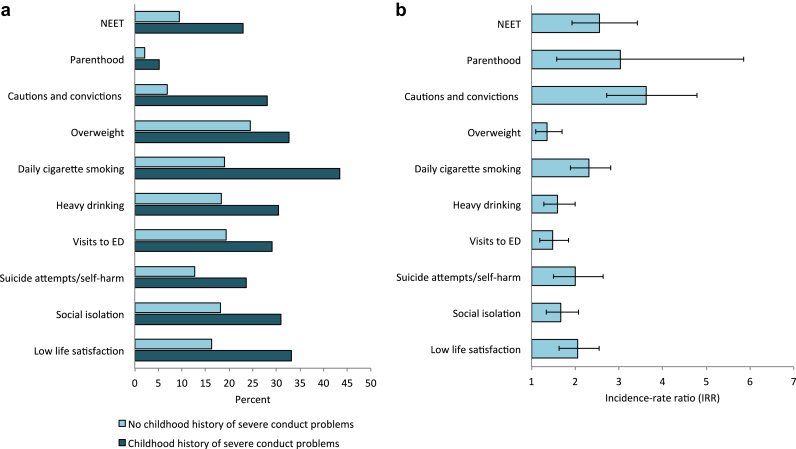
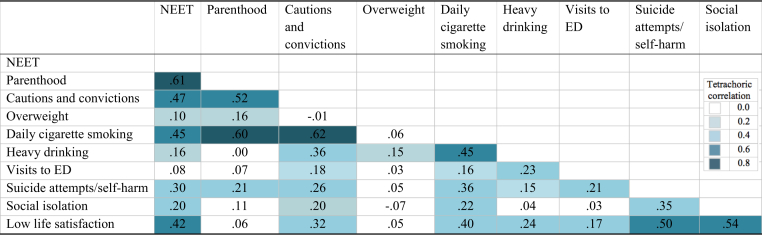
Participants with a childhood history of severe childhood conduct problems were at risk for poor functioning at age 18 years (Figure 1). Risks were elevated across all outcomes, ranging from incidence-rate ratios of 1.36 (for overweight) to 3.62 (for cautions and convictions). Poor functional outcomes were also associated with each other, so that participants with one poor outcome were more likely to display poor functioning in other outcomes (Figure 2). To capture this accumulation, we derived an index of cumulative poor functioning by summing poor outcomes. A childhood history of conduct problems forecast cumulative poor functioning in early adulthood (Table 2, panel A). Closer inspection revealed that the majority of 18-year-olds without a history of conduct problems experienced none or only 1 poor functional outcome (61.6%); few experienced 2 or 3 (28.7%), and fewer experienced 4 or more poor outcomes (9.7%). In contrast, only a minority of those with a history of conduct problems experienced none or 1 poor outcome (25.4%); most of them experienced 2 or 3 (41.7%) or 4 or more poor outcomes (33.0%). This effect was not simply an artifact of childhood conduct problems predicting any one outcome particularly well, as indicated by analyses leaving out 1 outcome at a time (see Table S4, available online). We used the cumulative index of poor functioning in all subsequent analyses.
Figure 1.
Differences in functional outcomes between participants with a childhood history of severe conduct problems and those without. Note: Panel a presents the percentages of 18-year-olds who experienced a poor functional outcome among those with versus without a childhood history of severe conduct problems. Panel b indicates the incidence-rate ratio (interpretable as relative risk42) for experiencing each outcome for those with a childhood history of severe conduct problems. Error bars represent 95% confidence intervals. NEET = not in education, employment or training.
Figure 2.
Heat map illustrating associations among poor functional outcomes, as indicated by tetrachoric correlations. Note: ED = emergency department; NEET = not in education, employment or training.
Table 2.
A Childhood History of Severe Conduct Problems Predicts Poor Cumulative Functioning at Age 18 Years
| Predictor | Bivariate Model |
Multivariate Modelb |
|---|---|---|
| IRR (95% CI) | IRR (95% CI) | |
| Panel A. Does a childhood history of conduct problems predict cumulative poor functioninga at age 18 years? | ||
| Childhood conduct problems | 1.96 (1.75, 2.18) | — |
| Panel B. Is the effect accounted for by young-adult psychopathology? | ||
| Childhood conduct problems | 1.96 (1.75, 2.18) | 1.61 (1.45, 1.79) |
| Young-adult psychopathology | 2.22 (2.03, 2.43) | 2.06 (1.89, 2.25) |
| Panel C. Is the effect accounted for by well-established risk factors? | ||
| Childhood conduct problems | 1.94 (1.74, 2.16) | 1.40 (1.26, 1.56) |
| Young-adult psychopathology | 2.22 (2.03, 2.43) | 1.94 (1.78, 2.12) |
| Socioeconomic disadvantage | 1.41 (1.32, 1.50) | 1.23 (1.16, 1.31) |
| Exposure to violence | 1.50 (1.35, 1.66) | 1.13 (1.02, 1.24) |
| Parental antisocial behavior | 1.27 (1.21, 1.33) | 1.05 (1.00, 1.11) |
| Maternal depression | 1.31 (1.17, 1.46) | 1.04 (0.95, 1.15) |
| Predictor | Fixed-Effects Bivariate Models |
Fixed-Effects Multivariate Models |
|---|---|---|
| IRR (95%CI) | IRR (95%CI) | |
| Panel D. Is the effect accounted for by unmeasured familial risk factors? | ||
| Childhood conduct problems | 1.34 (1.13, 1.59) | 1.30 (1.10, 1.54) |
| Young-adult psychopathology | 1.48 (1.33, 1.66) | 1.47 (1.32,1.64) |
Note: The number of participants within each panel is restricted to participants with nonmissing data on all variables included in the multivariate model within a panel. IRR = incidence-rate ratio.
The cumulative poor functioning measure is the sum of all poor functional outcomes.
Results are adjusted for all other predictors within a panel and for participants’ sex.
Effect of Concurrent Psychopathology in Early Adulthood on the Association Between Conduct Problems and Cumulative Poor Functioning
Participants with a childhood history of severe conduct problems were more likely to experience psychopathology at age 18 years (incidence-rate ratio [IRR] = 1.75, 95% CI = 1.57, 1.96, p < .01). Psychopathology was associated with cumulative poor functioning (Table 2, panel B). Including young-adult psychopathology as a predictor of poor young-adult functioning in our model reduced the effect of childhood conduct problems by approximately one-third; however, it continued to forecast poor functioning, over and above young-adult psychopathology.
Effect of Familial Risk Factors on the Association Between Conduct Problems and Cumulative Poor Functioning
Participants who grew up in socioeconomic disadvantage, had been exposed to violence, or had parents with psychopathology were at greater risk for displaying conduct problems as children (IRR = 1.66, 95% CI 1.40, 1.98, p < .01 for socioeconomic disadvantage; IRR = 2.24, 95% CI = 1.71, 2.94, p < .01 for exposure to violence; IRR = 1.68, 95% CI = 1.54,1.84, p < .01 for parental antisocial behavior; and IRR = 1.62. 95% CI = 1.26, 2.08, p < .01 for maternal depression) and to experience cumulative poor functioning at age 18 years (Table 2, panel C). These factors explained part of the association between childhood conduct problems and cumulative poor functioning, each reducing it by approximately one-fifth. Taken together, familial risk factors accounted for approximately an additional one-fourth of the association, beyond young-adult psychopathology. However, childhood conduct problems continued to predict poor functioning in early adulthood (Table 2, panel C).
Effect of Genetic and Shared Environmental Influences on the Association Between Conduct Problems and Cumulative Poor Functioning
Twin correlations of a childhood history of severe conduct problems (tetrachoric rmz = 0.85 and rdz = 0.62) and cumulative poor functioning at age 18 years (polychoric rmz= 0.67 and rdz = 0.41) were greater in MZ than DZ twins, indicating genetic influences. MZ correlations were less than twice the DZ correlations, indicating shared environmental influences. However, even twins raised in the same families and with the same genetic background differed in whether they had a childhood history of conduct problems and in their cumulative poor functioning, making it possible to test whether conduct problems predicted young-adult outcomes independent of familial influences. The prediction of cumulative poor functioning by childhood conduct problems was reduced when twins within the same family were compared to each other (Table 2, panel D). However, the effect remained significant, indicating that childhood conduct problems predicted poor functioning independent of familywide risk factors. We restricted our analyses to MZ twins to completely account for genetic influences, and found that childhood conduct problems continued to predict poor functioning (IRR = 1.32, 95% CI = 1.11, 1.57, p < .01). Taken together, these findings indicate that children with a history of severe conduct problems remain at greater risk for future poor functioning even after taking into account familywide environmental and genetic risk factors that could explain the association.
Discussion
Previous studies have shown that children with conduct problems are at risk for experiencing poor functional outcomes in adulthood. We extended this research in 2 ways: first, we examined the effect of childhood conduct problems on a cumulative index of poor functioning in emerging adulthood, reflecting outcomes across areas as broad as educational attainment, crime, health, and social relationships. Our findings show that 18-year-olds with a childhood history of severe conduct problems were more likely to experience difficulties across multiple spheres of adult life, more than a decade after they had first displayed conduct problems. The overall effect was modest but pervasive across young-adult outcomes that are not only relevant for individuals’ success during the transition to adulthood but are also part of the foundation for health, attainment, and well-being across the life-course. Second, we examined explanations for the link between conduct problems and later poor functioning. Our findings revealed that children with conduct problems grew up to develop poor functional outcomes partly because they were more likely to experience psychopathology as young adults, and partly because they had been exposed to familial risk factors from early in life, both genetic and environmental. However, conduct problems forecast poor outcomes even after accounting for these explanations, indicating an independent, long-lasting effect. The findings have implications for our understanding of why children with conduct problems are at greater risk for poor outcomes, as well as for interventions aimed at improving young adults’ functioning.
Each of our hypothesized explanatory factors accounted partly for the association between childhood conduct problems and poor young-adult outcomes. It is well established that conduct problems during childhood predict conduct problems and other mental health problems in adulthood,7, 45 and here we have shown that this continuity of problems across time may be partly responsible for the link between a childhood history of conduct problems and age-18 functional impairment. Our findings also suggest that childhood conduct problems and later poor functioning to some extent originate in the same underlying risk factors, both specific, well-established risk factors such as socioeconomic deprivation, and additional, unmeasured influences that we were able to capture through studying twins. These unmeasured familial risk factors may reflect environmental factors such as aspects of parenting or excessive stress that increase risk for childhood conduct problems and for poor functioning in adulthood. Familial risk may also reflect genetically influenced, early-emerging behaviors and characteristics.
Our findings indicate that the presence of severe conduct problems during childhood signal poorer long-term outcomes independent of psychopathology in early adulthood.10, 46 The association was also not explained away by familial risk. These findings suggest that conduct problems at a young age, by themselves, have a lasting, negative, pervasive impact on young-adult outcomes. Conduct problems may do so by interfering with children’s ability to accumulate the human capital needed to become successful young adults. For example, children with conduct problems may be less well integrated into formal institutions and informal social settings that promote skills and positive functioning as children grow up, such as school or friendship groups of well-adjusted peers. Children with conduct problems may become involuntarily excluded from these settings if their behaviors elicit rejection from others,47 or they may withdraw from favorable settings by truanting or associating with peers who also display conduct problems.48 Once children with conduct problems lose contact with settings that promote positive functioning, it may be difficult to catch up in their development of skills needed to succeed in life, leading to pervasive functional impairment even years later.
The findings of our study need to be interpreted in light of some limitations. First, the E-Risk study participants were on the cusp of adulthood. It was not possible to examine negative outcomes that may unfold later in life,49 or life events and experiences such as marriage that may limit the negative effects of conduct problems or improve young adults’ functioning as individuals grow older.50 However, poor functional outcomes in the transition to adulthood are informative because they are a foundation for individuals’ health, attainment, and well-being across the life course. Second, our finding that childhood problems predicted poor adult outcomes within twin pairs does not establish causality. It is possible that factors not shared between twins, such as school experiences, explain the association. However, by taking into account environmental and genetic influences shared between members of a family, the twin comparisons rule out a powerful source of confounding of the association.51 Third, because functional outcomes in young adulthood were all assessed at the same age, we were unable to account for the possibility that a poor outcome in one area may have influenced other poor outcomes to occur. For example, excessive drinking may have led to visits to the emergency department. Fourth, we cannot be certain that our results generalize to singletons. However, twins have been shown to be similar to singletons in the levels and development of behavior problems they experience during childhood.52
Our findings have implications for future research and for interventions. First, future studies could benefit from adopting the approach of summarizing outcomes into a measure of cumulative poor functioning that captures the global impairment of young adults with a history of conduct problems. A cumulative measure empirically reflects the reality that poor functional outcomes are not restricted to any one specific indicator, but aggregate across outcomes.22 It may also help to identify global, underlying pathways that connect childhood conduct problems to pervasive poor functioning. Second, more research is needed to understand the processes through which bouts of severe problem behavior during childhood leave an imprint on children’s lives. Individuals who display stable high levels of conduct problems across development are at greatest risk for poor long-term outcomes,53 but our findings add to a growing evidence base suggesting that bouts of early severe behavior problems still predict poor functioning over and above young-adult problems.10, 46 Third, although there is already strong evidence to support early intervention to limit childhood conduct problems, knowledge about the extent to which different explanations account for the link between childhood conduct problems and functional outcomes is important because it implies different strategies and targets for interventions. Our findings provide further support for comprehensive interventions that address familial risk factors for problem behavior and target children’s conduct problems from early in life onward, to disrupt pathways of cumulative continuity and to improve individual long-term outcomes.54, 55 Because the effects of conduct problems on later outcomes are pervasive, treatment has the potential to reduce economic burden across multiple public sectors,56 such as the judicial system, the health care system, and social services, in addition to improving individuals’ health, attainment, and well-being across the life course.
Acknowledgments
The authors are grateful to the study families and teachers for their participation. The authors thank Michael Rutter, PhD, and Robert Plomin, PhD, of King’s College London, Thomas Achenbach, PhD, of the University of Vermont, for his kind permission to adapt the Child Behavior Checklist, to CACI, Inc., the UK Ministry of Justice, and the members of the E-Risk Study team for their dedication, hard work, and insights.
Footnotes
The Environmental Risk (E-Risk) Longitudinal Twin Study is funded by UK Medical Research Council (UKMRC grant G1002190). Additional support was provided by the US National Institute of Child Health and Development (NICHD grant HD077482) and by the Jacobs Foundation. Dr. Arseneault is the Mental Health Leadership Fellow for the UK Economic and Social Research Council (ESRC). Dr. Fisher is supported by an MQ Fellows Award (MQ14F40).
Disclosure: Drs. Wertz, Agnew-Blais, Caspi, Danese, Fisher, Goldman-Mellor, Moffitt, and Arseneault report no biomedical financial interests or potential conflicts of interest.
Supplement 1
Additional Information About Conduct Problems Across Childhood
The percentage of children displaying 5 or more symptoms of conduct disorder at each age were 9.2% (n = 205) at age 5 years, 6.1% (n = 133) at age 7 years, and 5.5% (n = 118) at age 10 years. In all, 14.5% (n = 307) of the children studied displayed 5 or more symptoms of conduct disorder at 1 or more of these time points. Of these 307 children, 11.7% (n = 36) displayed 5 or more symptoms across all 3 time points; 23.8% (n = 73) of the children displayed 5 or more symptoms at 2 of 3 time points; and 61.9% (n = 190) of the children displayed 5 or more symptoms at only 1 time point. A further 2.6% (n = 8) displayed 5 or more symptoms at 1 or more of 3 time points, but had missing data for other assessment time points. Children who displayed 5 or more symptoms at only 1 time point also had elevated symptoms of conduct disorder at the other time points, compared to those who did not ever display 5 or more symptoms, even though these symptoms did not reach the 5+ threshold.
Description of Poor Functional Outcomes at Age 18 Years
Not in Education, Employment, or Training (NEET)
Participants were classified as Not in Education, Employment, or Training (NEET) if they reported in the age-18-years interview that they were neither studying, nor working in paid employment, nor pursuing a vocational qualification or apprenticeship training.1 Participants were queried to ensure that NEET status was not simply a function of being on summer holiday/vacation, or of being a parent. This operationalization of NEET status follows that used by the UK Office of National Statistics and the International Labor Organization.2 In our cohort, 11.6% of participants were NEET, matching UK national NEET figures.3
Parenthood
Information on parenthood was obtained in the age-18 interview by asking participants about the outcome of any previous pregnancies that they had experienced (for girls) or caused (for boys). Girls were additionally asked whether they were currently pregnant. Participants were classified as parents if a previous pregnancy had resulted in a live birth or if they were currently pregnant. In all, 2.9% of girls and 1.1% of boys had experienced or caused at least 1 pregnancy that had resulted in live birth and 0.9% of participants were pregnant at the age-18 interview. The observed rates match the UK national figures on live births for this age group.4
Cautions and Convictions
Official records of participants’ cautions and convictions were obtained through UK Police National Computer (PNC) record searches conducted in cooperation with the UK Ministry of Justice. Records include complete histories of cautions and convictions for participants cautioned or convicted in the United Kingdom beginning at age 10 years, the age of criminal responsibility. Our data are complete through age 19 years. Cautions and convictions were recoded into a binary variable to reflect whether participants had been cautioned or convicted or not. In all, 10.2% of E-Risk participants had been cautioned or convicted.
Overweight
To assess whether young adults were overweight, trained research workers took anthropometric measurements of participants at the start of the age-18 interview. Body mass index (BMI) was computed as weight in kilograms by height in meters squared, and being overweight was defined as a BMI of ≥25. In all, 25.8% of participants were classified as overweight based on this definition, matching UK national figures for this age group.5
Daily Cigarette Smoking
We assessed cigarette smoking by asking participants about their current smoking habits. Participants who reported that they were currently smoking daily were coded as smokers. Of the participants, 22.3% reported smoking at the time of the interview, matching UK national figures for this age group.6
Heavy Drinking
We assessed alcohol drinking by asking participants: “In a typical week when you had something to drink, how many drinks, in total, would you usually have,” for the period from Monday to Thursdays and from Fridays through Sundays. The term “drink” was explained to mean “a glass of wine, a can or bottle of beer, a ‘shot’ of hard spirits either alone or in a mixed drink, cocktail.” We added the number of drinks from both time periods to obtain drinks per week. We defined heavy drinking as being among the 20% highest scoring participants (equivalent to 14 or more alcoholic drinks per week; see Table S3 for sensitivity tests using different thresholds). This categorization corresponds to UK figures reporting that approximately 15% to 20% of 16- to 24-year-olds consume more than the UK Chief Medical Officer’s recommended limit of 14 units of alcohol per week.7
Suicide Attempts/Self-Harm
At the age-18 interview, participants were interviewed about suicide attempts and self-harm occurring between ages 12 and 18 years. To assess suicide attempts, participants were asked whether they had tried to kill themselves or attempted suicide since age 12. If they answered positively, further questions about the specific events were asked to obtain details and to establish whether they were accompanied by intent to die. To assess self-harm, participants were asked whether they had ever tried to hurt themselves to cope with stress or emotional pain. Responses were combined into 1 dichotomous variable indicating whether the participant had engaged in any suicidal or self-harming behavior. In all, 3.8% of participants had attempted suicide and 14.3% had engaged in self-harm. These rates are slightly lower than UK national figures in 16- to 24-year-olds, which may be explained by different measurement methods and age periods covered.8
Social Isolation
Social isolation was measured using the Multidimensional Scale of Perceived Social Support (MSPSS), which assesses individuals’ access to supportive relationships with family and friends9 with 12 items consisting of statements such as “There is a special person who is around when I am in need” and “I can count on my friends when things go wrong.” Participants rated these statements as “not true” (0), “somewhat true” (1), or “very true” (2). We reversed the scoring of the items so that higher scores reflected greater isolation (Cronbach’s α = .88). We defined social isolation as being among the 20% highest-scoring participants (see Table S3 for sensitivity tests using different thresholds).
Low Life Satisfaction
Participants’ life satisfaction was assessed using the Satisfaction With Life Scale,10 with 5 items such as “The conditions of my life are excellent” and “I am satisfied with my life.” The response format was a 5-point scale ranging from “strongly disagree” (1) to “strongly agree” (5). We reversed the scoring of the items so that higher scores reflected lower life satisfaction. We defined low life satisfaction as being among the 20% highest scoring participants (see Table S3 for sensitivity tests using different thresholds).
Table S1.
Effect of Childhood Conduct Problems on Age-18 Functional Outcomes, Using Different Symptoms Thresholdsa to Identify a Childhood History of Conduct Problems as Well as a Continuous Measure of Conduct Disorder Symptomsb
| Measurement of Childhood History of Conduct Problems |
||||
|---|---|---|---|---|
| 3+ Symptoms (37.8% of Sample) |
4+ Symptoms (23.3% of Sample) |
5+ Symptoms (14.5% of Sample) |
Continuous Measure |
|
| IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | |
| NEET | 1.90 (1.46, 2.48) | 2.07 (1.55, 2.75) | 2.56 (1.92, 3.43) | 1.28 (1.22, 1.35) |
| Parenthood | 2.29 (1.28, 4.09) | 2.07 (1.11, 3.86) | 3.04 (1.58, 5.86) | 1.35 (1.20, 1.52) |
| Cautions and convictions | 2.74 (2.03, 3.71) | 3.33 (2.49, 4.46) | 3.62 (2.73, 4.79) | 1.37 (1.30, 1.44) |
| Overweight | 1.35 (1.13, 1.61) | 1.49 (1.23, 1.80) | 1.36 (1.10, 1.70) | 1.12 (1.06, 1.17) |
| Daily cigarette smoking | 2.08 (1.73, 2.50) | 2.08 (1.72, 2.52) | 2.31 (1.89, 2.82) | 1.26 (1.21, 1.30) |
| Heavy drinking | 1.57 (1.30, 1.90) | 1.63 (1.33, 2.00) | 1.60 (1.29, 2.00) | 1.15 (1.11, 1.21) |
| Visits to ED | 1.18 (.98, 1.41) | 1.20 (.98, 1.47) | 1.48 (1.19, 1.85) | 1.10 (1.04, 1.16) |
| Suicide attempts/self-harm | 1.51 (1.21, 1.90) | 1.53 (1.18, 1.99) | 2.00 (1.51, 2.64) | 1.14 (1.06, 1.22) |
| Social isolation | 1.58 (1.31, 1.92) | 1.50 (1.22, 1.84) | 1.67 (1.34, 2.08) | 1.15 (1.09, 1.21) |
| Low life satisfaction | 1.66 (1.36, 2.04) | 1.87 (1.52, 2.31) | 2.05 (1.64, 2.55) | 1.19 (1.14, 1.25) |
Note: All analyses are adjusted for participants’ sex. ED = emergency department; IRR = incidence-rate ratio; NEET = Not in Education, Employment, or Training.
Participants were categorized as having a childhood history of conduct problems if they displayed equal to or more than the threshold number of conduct disorder symptoms at 1 or more assessment time points during childhood. Results reported in the main article using a threshold of 5+ symptoms are shown in boldface type.
The continuous measure was computed by averaging conduct disorder symptoms across all assessment time points in childhood, for children with valid data at all 3 time points (n = 2,116).
Table S2.
Effect of Childhood Conduct Problems on Cumulative Poor Functioning, Using Different Symptoms Thresholdsa to Identify a Childhood History of Conduct Problems as Well as a Continuous Measure of Conduct Disorder Symptomsb
| Measurement of Childhood History of Conduct Problems |
||||
|---|---|---|---|---|
| 3+ Symptoms |
4+ Symptoms |
5+ Symptoms |
Continuous Measure |
|
| IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | |
| Does a childhood history of conduct problems predict cumulative poor functioning at age 18 years? | ||||
| Effect of conduct problems (adjusted for sex) | 1.65 (1.49, 1.82) | 1.75 (1.58, 1.95) | 1.96 (1.75, 2.18) | 1.20 (1.17, 1.23) |
| Is the effect accounted for by young adult psychopathology? | ||||
| Effect of conduct problems (adjusted for sex and young-adult psychopathology) | 1.49 (1.37, 1.63) | 1.50 (1.37, 1.65) | 1.61 (1.45, 1.79) | 1.15 (1.12, 1.17) |
| Is the effect accounted for by well-established risk factors? | ||||
| Effect of conduct problems (adjusted for sex, young-adult psychopathology and well-established risk factors) | 1.32 (1.21, 1.45) | 1.31 (1.19, 1.45) | 1.40 (1.26, 1.56) | 1.11 (1.08, 1.14) |
| Is the effect accounted for by unmeasured familial risk factors? | ||||
| Effect of conduct problems within twin pairs (adjusted for young-adult psychopathology) | 1.23 (1.08, 1.41) | 1.25 (1.07, 1.45) | 1.30 (1.10, 1.54) | 1.08 (1.01, 1.14) |
Note: IRR = Incidence-rate ratio.
Children were categorized as having a childhood history of conduct problems if they displayed equal to or more than the threshold number of conduct disorder symptoms at 1 or more assessment time points during childhood. Results reported in the main article using a threshold of 5+ symptoms are shown in boldface type.
The continuous measure was computed by averaging conduct disorder symptoms across all assessment time points in childhood, for children with valid data at all 3 time points (n = 2,116).
Table S3.
Effects of a Childhood History of Severe Conduct Problems on Age-18 Functional Outcomes, Using Different Thresholds to Classify Poor Functioning
| Childhood History of Conduct Problems |
|
|---|---|
| IRR (95% CI) | |
| Heavy drinking | |
| 20% Cut-off | 1.60 (1.29, 1.99) |
| 15% Cut-off | 1.65 (1.28, 2.13) |
| 10% Cut-off | 1.71 (1.23, 2.39) |
| Social isolation | |
| 20% Cut-off | 1.67 (1.34, 2.08) |
| 15% Cut-off | 1.86 (1.41, 2.46) |
| 10% Cut-off | 1.96 (1.42, 2.68) |
| Low life satisfaction | |
| 20% Cut-off | 2.05 (1.64, 2.55) |
| 15% Cut-off | 2.05 (1.56, 2.70) |
| 10% Cut-off | 2.10 (1.53, 2.89) |
Note: All analyses are adjusted for participants’ sex. Results reported in the main article using the 20% cut-off are shown in boldface type. IRR = incidence-rate ratio.
Table S4.
Effect of Childhood Conduct Problems on a Measure of Cumulative Poor Functioning at Age 18 Years, Leaving Out 1 Outcome at a Time
| Childhood History of Conduct Problems |
|
|---|---|
| IRR (95% CI) | |
| Cumulative poor functioning | 1.96 (1.75, 2.18) |
| Excluding NEET | 1.92 (1.73, 2.13) |
| Excluding parenthood | 1.92 (1.73, 2.13) |
| Excluding cautions and convictions | 1.87 (1.67, 2.08) |
| Excluding overweight | 2.05 (1.82, 2.31) |
| Excluding daily cigarette smoking | 1.89 (1.70, 2.11) |
| Excluding heavy drinking | 2.00 (1.79, 2.24) |
| Excluding visits to emergency department | 2.03 (1.80, 2.28) |
| Excluding suicide attempts/self-harm | 1.94 (1.74, 2.16) |
| Excluding social isolation | 1.92 (1.73, 2.14) |
| Excluding low life satisfaction | 1.99 (1.77, 2.23) |
Note: All analyses are adjusted for participants’ sex. Results reported in the main article using a measure that includes all outcomes are shown in boldface type. IRR = incidence-rate ratio; NEET = not in education, employment, or training.
References
- 1.Robins L.N. Williams & Wilkins; Baltimore, MD: 1966. Deviant Children Grown Up. [Google Scholar]
- 2.Erskine H.E., Norman R.E., Ferrari A.J. Long-term outcomes of attention-deficit/hyperactivity disorder and conduct disorder: a systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2016;55:841–850. doi: 10.1016/j.jaac.2016.06.016. [DOI] [PubMed] [Google Scholar]
- 3.Burke J.D., Rowe R., Boylan K. Functional outcomes of child and adolescent oppositional defiant disorder symptoms in young adult men. J Child Psychol Psychiatry. 2014;55:264–272. doi: 10.1111/jcpp.12150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fergusson D.M., Horwood L.J., Ridder E.M. Show me the child at seven: the consequences of conduct problems in childhood for psychosocial functioning in adulthood. J Child Psychol Psychiatry. 2005;46:837–849. doi: 10.1111/j.1469-7610.2004.00387.x. [DOI] [PubMed] [Google Scholar]
- 5.Goodman A., Joyce R., Smith J.P. The long shadow cast by childhood physical and mental problems on adult life. Proc Natl Acad Sci U S A. 2011;108:6032–6037. doi: 10.1073/pnas.1016970108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jaffee S.R., Moffitt T.E., Caspi A., Taylor A., Arseneault L. Influence of adult domestic violence on children’s internalizing and externalizing problems: an environmentally informative twin study. J Am Acad Child Adolesc Psychiatry. 2002;41:1095–1103. doi: 10.1097/00004583-200209000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Reef J., van Meurs I., Verhulst F.C., van der Ende J. Children’s problems predict adults’ DSM-IV disorders across 24 years. J Am Acad Child Adolesc Psychiatry. 2010;49:1117–1124. doi: 10.1016/j.jaac.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 8.Fergusson D.M., Goodwin R.D., Horwood L.J. Major depression and cigarette smoking: results of a 21-year longitudinal study. Psychol Med. 2003;33:1357–1367. doi: 10.1017/s0033291703008596. [DOI] [PubMed] [Google Scholar]
- 9.Wittchen H.U., Nelson C.B., Lachner G. Prevalence of mental disorders and psychosocial impairments in adolescents and young adults. Psychol Med. 1998;28:109–126. doi: 10.1017/s0033291797005928. [DOI] [PubMed] [Google Scholar]
- 10.Copeland W.E., Wolke D., Shanahan L., Costello E.J. Adult functional outcomes of common childhood psychiatric problems. JAMA Psychiatry. 2015;72:892–899. doi: 10.1001/jamapsychiatry.2015.0730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bradley R., Corwyn R. Socioeconomic status and child development. Annu Rev Psychol. 2002;53:371–399. doi: 10.1146/annurev.psych.53.100901.135233. [DOI] [PubMed] [Google Scholar]
- 12.Duncan G.J., Ziol-Guest K.M., Kalil A. Early-childhood poverty and adult attainment, behavior, and health. Child Dev. 2010;81:306–325. doi: 10.1111/j.1467-8624.2009.01396.x. [DOI] [PubMed] [Google Scholar]
- 13.Danese A., Moffitt T.E., Harrington H. Adverse childhood experiences and adult risk factors for age-related disease: depression, inflammation, and clustering of metabolic risk markers. Arch Pediatr Adolesc Med. 2009;163:1135–1143. doi: 10.1001/archpediatrics.2009.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jaffee S.R., Caspi A., Moffitt T.E., Taylor A. Physical maltreatment victim to antisocial child: evidence of an environmentally mediated process. J Abnorm Psychol. 2004;113:44–55. doi: 10.1037/0021-843X.113.1.44. [DOI] [PubMed] [Google Scholar]
- 15.Currie J., Spatz Widom C. Long-term consequences of child abuse and neglect on adult economic well-being. Child Maltreat. 2010;15:111–120. doi: 10.1177/1077559509355316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim-Cohen J., Moffitt T.E., Taylor A., Pawlby S., Caspi A. Maternal depression and children’s antisocial behavior: nature and nurture effects. Arch Gen Psychiatry. 2005;62:173–181. doi: 10.1001/archpsyc.62.2.173. [DOI] [PubMed] [Google Scholar]
- 17.Lewinsohn P.M., Olino T.M., Klein D.N. Psychosocial impairment in offspring of depressed parents. Psychol Med. 2005;35:1493–1504. doi: 10.1017/S0033291705005350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Branigan A.R., McCallum K.J., Freese J. Variation in the heritability of educational attainment: an international meta-analysis. Social Forces. 2013;92:109–140. [Google Scholar]
- 19.Rhee S.H., Waldman I.D. Genetic and environmental influences on antisocial behavior: a meta-analysis of twin and adoption studies. Psychol Bull. 2002;128:490–529. [PubMed] [Google Scholar]
- 20.Kendler K.S., Schmitt E., Aggen S.H., Prescott C.A. Genetic and environmental influences on alcohol, caffeine, cannabis, and nicotine use from early adolescence to middle adulthood. Arch Gen Psychiatry. 2008;65:674. doi: 10.1001/archpsyc.65.6.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moffitt T.E. Adolescence-limited and life-course-persistent antisocial behavior: a developmental taxonomy. Psychol Rev. 1993;100:674–701. [PubMed] [Google Scholar]
- 22.Caspi A., Houts R.M., Belsky D.W. Childhood forecasting of a small segment of the population with large economic burden. Nat Hum Behav. 2016;1:1–10. doi: 10.1038/s41562-016-0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Trouton A., Spinath F.M., Plomin R. Twins Early Development Study (TEDS): a multivariate, longitudinal genetic investigation of language, cognition and behavior problems in childhood. Twin Res. 2002;5:444–448. doi: 10.1375/136905202320906255. [DOI] [PubMed] [Google Scholar]
- 24.Moffitt T.E. E-Risk Study Team. Teen-aged mothers in contemporary Britain. J Child Psychol Psychiatry. 2002;43:727–742. doi: 10.1111/1469-7610.00082. [DOI] [PubMed] [Google Scholar]
- 25.Odgers C.L., Caspi A., Bates C.J., Sampson R.J., Moffitt T.E. Systematic social observation of children’s neighborhoods using Google Street View: a reliable and cost-effective method. J Child Psychol Psychiatry. 2012;53:1009–1017. doi: 10.1111/j.1469-7610.2012.02565.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Odgers C.L., Caspi A., Russell M.A., Sampson R.J., Arseneault L., Moffitt T.E. Supportive parenting mediates neighborhood socioeconomic disparities in children’s antisocial behavior from ages 5 to 12. Dev Psychopathol. 2012;24:705–721. doi: 10.1017/S0954579412000326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Achenbach T.M. University of Vermont, Department of Psychiatry; Burlington, VT: 1991. Manual for the Child Behavior Checklist/4-18 and 1991 Profile. [Google Scholar]
- 28.Achenbach T.M. University of Vermont, Department of Psychiatry; Burlington, VT: 1991. Manual for the Teacher’s Report Form and 1991 Profile. [Google Scholar]
- 29.American Psychiatric Association . American Psychiatric Association; Washington, DC: 2000. Diagnostic and Statistical Manual of Mental Disorders (4th ed., Text Rev.) [Google Scholar]
- 30.Bird H.R., Gould M.S., Staghezza B. Aggregating data from multiple informants in child psychiatry epidemiological research. J Am Acad Child Adolesc Psychiatry. 1992;31:78–85. doi: 10.1097/00004583-199201000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Piacentini J.C., Cohen P., Cohen J. Combining discrepant diagnostic information from multiple sources: are complex algorithms better than simple ones? J Abnorm Child Psychol. 1992;20:51–63. doi: 10.1007/BF00927116. [DOI] [PubMed] [Google Scholar]
- 32.Goldman-Mellor S., Caspi A., Arseneault L. Committed to work but vulnerable: self-perceptions and mental health in NEET 18-year olds from a contemporary British cohort. J Child Psychol Psychiatry. 2016;57:196–203. doi: 10.1111/jcpp.12459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.American Psychiatric Association . American Psychiatric Association; Washington, DC: 1994. Diagnostic and Statistical Manual of Mental Disorders (4th ed.) [Google Scholar]
- 34.American Psychiatric Association . American Psychiatric Association; Washington, DC: 2013. Diagnostic and Statistical Manual of Mental Disorders (5th ed.) [Google Scholar]
- 35.Robins L.N., Cottler L., Bucholz K.K., Compton W. Washington University School of Medicine; St Louis, MO: 1995. Diagnostic Interview Schedule for DSM-IV. [Google Scholar]
- 36.Trzesniewski K.H., Moffitt T.E., Caspi A., Taylor A., Maughan B. Revisiting the association between reading achievement and antisocial behavior: new evidence of an environmental explanation from a twin study. Child Dev. 2006;77:72–88. doi: 10.1111/j.1467-8624.2006.00857.x. [DOI] [PubMed] [Google Scholar]
- 37.Jaffee S.R., Caspi A., Moffitt T.E., Polo-Tomás M., Taylor A. Individual, family, and neighborhood factors distinguish resilient from non-resilient maltreated children: a cumulative stressors model. Child Abuse Negl. 2007;31:231–253. doi: 10.1016/j.chiabu.2006.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dodge K.A., Bates J.E., Pettit G.S. Mechanisms in the cycle of violence. Science. 1990;250:1678–1683. doi: 10.1126/science.2270481. [DOI] [PubMed] [Google Scholar]
- 39.Dodge K.A., Pettit G.S., Bates J.E., Valente E. Social information-processing patterns partially mediate the effect of early physical abuse on later conduct problems. J Abnorm Psychol. 1995;104:632–643. doi: 10.1037//0021-843x.104.4.632. [DOI] [PubMed] [Google Scholar]
- 40.Jaffee S.R., Moffitt T.E., Caspi A., Taylor A. Life with (or without) father: the benefits of living with two biological parents depend on the father’s antisocial behavior. Child Dev. 2003;74:109–126. doi: 10.1111/1467-8624.t01-1-00524. [DOI] [PubMed] [Google Scholar]
- 41.Achenbach T.M. University of Vermont; Burlington, VT: 1997. Manual for the Young Adult Self-Report and Young Adult Behavior Checklist. [Google Scholar]
- 42.Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 43.Allison P.D. Sage Publications; Thousand Oaks, CA: 2009. Fixed Effects Regression Models. [Google Scholar]
- 44.StataCorp . StataCorp LP; College Station, TX: 2015. Stata Statistical Software: Release 14. [Google Scholar]
- 45.Lahey B.B., Loeber R., Burke J.D., Applegate B. Predicting future antisocial personality disorder in males from a clinical assessment in childhood. J Consult Clin Psychol. 2005;73:389–399. doi: 10.1037/0022-006X.73.3.389. [DOI] [PubMed] [Google Scholar]
- 46.Moffitt T.E., Caspi A., Harrington H., Milne B.J. Males on the life-course-persistent and adolescence-limited antisocial pathways: follow-up at age 26 years. Dev Psychopathol. 2002;14:179–207. doi: 10.1017/s0954579402001104. [DOI] [PubMed] [Google Scholar]
- 47.Pedersen S., Vitaro F., Barker E.D., Borge A.I.H. The timing of middle-childhood peer rejection and friendship: linking early behavior to early-adolescent adjustment. Child Dev. 2007;78:1037–1051. doi: 10.1111/j.1467-8624.2007.01051.x. [DOI] [PubMed] [Google Scholar]
- 48.Button T.M.M., Corley R.P., Rhee S.H., Hewitt J.K., Young S.E., Stallings M.C. Delinquent peer affiliation and conduct problems: a twin study. J Abnorm Psychol. 2007;116:554–564. doi: 10.1037/0021-843X.116.3.554. [DOI] [PubMed] [Google Scholar]
- 49.Healey A., Knapp M., Farrington D.P. Adult labour market implications of antisocial behaviour in childhood and adolescence: findings from a UK longitudinal study. Appl Econ. 2004;36:93–105. [Google Scholar]
- 50.Jaffee S.R., Lombardi C.M., Coley R.L. Using complementary methods to test whether marriage limits men’s antisocial behavior. Dev Psychopathol. 2013;25:65–77. doi: 10.1017/S0954579412000909. [DOI] [PubMed] [Google Scholar]
- 51.Turkheimer E., Harden K.P. Behavior genetic research methods. In: Reiss H.T., Judd C.M., editors. Handbook of Research Methods in Social and Personality Psychology. Cambridge University Press; New York, NY: 2014. pp. 159–187. [Google Scholar]
- 52.Gjone H., Nøvik T.S. Parental ratings of behaviour problems: a twin and general population comparison. J Child Psychol Psychiatry. 1995;36:1213–1224. doi: 10.1111/j.1469-7610.1995.tb01366.x. [DOI] [PubMed] [Google Scholar]
- 53.Odgers C.L., Moffitt T.E., Broadbent J.M. Female and male antisocial trajectories: from childhood origins to adult outcomes. Dev Psychopathol. 2008;20:673–716. doi: 10.1017/S0954579408000333. [DOI] [PubMed] [Google Scholar]
- 54.Conduct Problems Prevention Research Group (CPPR) The effects of the Fast Track preventive intervention on the development of conduct disorder across childhood. Child Dev. 2011;82:331–345. doi: 10.1111/j.1467-8624.2010.01558.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Heckman J.J. Skill formation and the economics of investing in disadvantaged children. Science. 2006;312:1900–1902. doi: 10.1126/science.1128898. [DOI] [PubMed] [Google Scholar]
- 56.Scott S., Knapp M., Henderson J., Maughan B. Financial cost of social exclusion: follow up study of antisocial children into adulthood. BMJ. 2001;323 doi: 10.1136/bmj.323.7306.191. 191-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
Supplemental References
- 1.Goldman-Mellor S., Caspi A., Arseneault L. Committed to work but vulnerable: self-perceptions and mental health in NEET 18-year olds from a contemporary British cohort. J Child Psychol Psychiatry. 2016;57:196–203. doi: 10.1111/jcpp.12459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.UK Office for National Statistics . UK Office for National Statistics; London, UK: 2013. UK Estimate of Young People Not in Education, Employment or Training. [Google Scholar]
- 3.UK Office for National Statistics . UK Office for National Statistics; London, UK: 2014. Young People Not in Education, Employment or Training (NEET): November 2014. [Google Scholar]
- 4.UK Office for National Statistics . UK Office for National Statistics; London, UK: 2016. Childbearing for Women Born in Different Years. [Google Scholar]
- 5.UK Health and Social Care Information Centre . UK Health and Social Care Information Centre; Leeds, UK: 2015. Health Survey for England, 2014. [Google Scholar]
- 6.UK Health and Social Care Information Centre . UK Health and Social Care Information Centre; Leeds, UK: 2014. Health Survey for England, 2013. [Google Scholar]
- 7.UK Health and Social Care Information Centre . UK Health and Social Care Information Centre; Leeds, UK: 2016. Health Survey for England, 2015. [Google Scholar]
- 8.UK Health and Social Care Information Centre . UK Health and Social Care Information Centre; Leeds, UK: 2016. Adult Psychiatric Morbidity Survey 2014. [Google Scholar]
- 9.Zimet G.D., Dahlem N.W., Zimet S.G., Farley G.K. The Multidimensional Scale of Perceived Social Support. J Pers Assess. 1988;52:30–41. [Google Scholar]
- 10.Diener E., Emmons R.A., Larsen R.J., Griffin S. The Satisfaction With Life Scale. J Pers Assess. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]