Summary
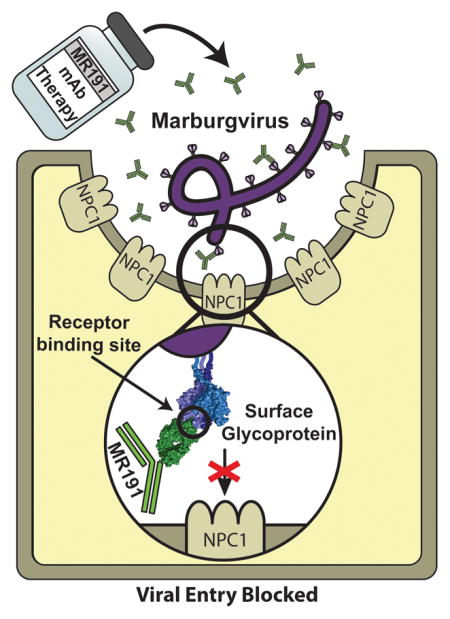
Since its first identification 50 years ago, Marburgviruses have emerged several times, with 83–90% lethality in the largest outbreaks. Although no vaccines or therapeutics are available for human use, the human antibody MR191 provides complete protection in nonhuman primates when delivered several days after inoculation of a lethal marburgvirus dose. The detailed neutralization mechanism of MR191 remains outstanding. Here we present a 3.2 Å crystal structure of MR191 complexed with a trimeric marburgvirus surface glycoprotein (GP). MR191 neutralizes by occupying the conserved receptor-binding site and competing with the host receptor Niemann-Pick C1. The structure illuminates previously disordered regions of GP including the stalk, fusion loop, CX6CC switch, and an N-terminal region of GP2 that wraps about the outside of GP1 to anchor a marburgvirus-specific “wing” antibody epitope. Virus escape mutations mapped far outside the MR191 receptor-binding site footprint suggest a role for these other regions in the GP quaternary structure.
eTOC Blurb
Using structural analysis, King et al. demonstrates how the protective, potentially therapeutic, monoclonal antibody MR191 engages the marburgvirus glycoprotein receptor-binding site. The resulting complex is able to outcompete the host entry receptor NPC1 for viral neutralization. Additionally, the structure illuminates previously disordered, functionally critical regions of the marburgvirus glycoprotein.
Introduction
Filoviruses cause severe disease and have been responsible for multiple outbreaks among both humans and nonhuman primates. Within the filovirus family are three genera: Ebolavirus [which includes Ebola virus (EBOV), Sudan virus (SUDV), Bundibugyo virus, Taï Forest virus and Reston virus], Marburgvirus [which includes Marburg virus (MARV) and Ravn virus (RAVV)], and Cuevavirus. Ebola Virus Disease (EVD) and Marburg Virus Disease (MVD) are clinically similar. MARV was the first filovirus identified, and has re-emerged multiple times since its 1967 discovery. The largest outbreak was nearly 90% lethal (CDC, 2005).
Antibody therapies are a promising avenue for prophylaxis, post-exposure prophylaxis, and therapeutic treatment of emerging viral diseases (Chanock et al., 1993; Zeitlin, Cone and Whaley, 1999; Lachmann, 2012; Burton and Saphire, 2015). One antibody-based therapy, ZMapp™ (Qiu et al., 2014), appeared to be beneficial during the 2013–2016 EVD outbreak although the results did not reach the threshold of statistical significance (Prevail II Group and Multi-National, 2016). None of the antibodies in ZMapp™ reacts with marburgviruses, and at this time, there are no approved treatments available for MVD.
Filoviruses produce enveloped virions that express a single glycoprotein (GP) on the surface. GP is responsible for attachment to and entry of target cells, and is the primary target for antibodies and vaccines (Dye et al., 2012). Filovirus GPs share a common core fold and trimeric organization, but are antigenically distinct. Marburgvirus GPs are only 30% identical to EBOV GP in primary amino acid sequence. The two marburgvirus GPs, however, MARV and RAVV GP, are quite similar to each other in sequence and likely structure, with 78% amino acid identity overall and 90% identity outside the mucin-like domain.
Filovirus GPs are 676–681 amino acids in length and are cleaved in the producer cell to yield two subunits, GP1 and GP2, which remain anchored by a single disulfide bond (Volchkov et al., 1998; Volchkov et al., 2000). The larger GP1 subunit harbors a receptor-binding core, a “glycan cap” subdomain, and a C-terminal, heavily glycosylated mucin-like domain. GP2 contains the membrane fusion machinery, including the internal fusion loop (IFL), two heptad repeat regions (HR1 and HR2), and a transmembrane domain to anchor the protein in the viral membrane (Bukreyev et al., 1993; Feldmann, Klenk and Sanchez, 1993; Lee et al., 2008). After attachment, filoviruses enter cells via macropinocytosis (Nanbo et al., 2010; Saeed et al., 2010; Aleksandrowicz et al., 2011; Mulherkar et al., 2011). Once in the endosome, ebolavirus GPs are cleaved by cathepsins B and/or L (Chandran et al., 2005). Cleavage removes the heavily glycosylated “glycan cap” and mucin-like domains from ebolavirus GP1 and is required to expose the binding site for the entry receptor, Niemann-Pick C1 (NPC1) (Chandran et al., 2005; Schornberg et al., 2006; Hood et al., 2010; Brecher et al., 2012; Marzi, Reinheckel and Feldmann, 2012). Interestingly, marburgviruses use the same NPC1 receptor but do not share the dependence on Cathepsins B and L of ebolaviruses (Gnirss et al., 2012).
The shared NPC1 receptor is an endosomal/lysosomal 13-pass transmembrane protein with three large luminal domains, A, C, and I, of which domain C (NPC1-C) is necessary and sufficient for filovirus binding (Carette et al., 2011; Miller et al., 2012; Gong et al., 2016). Recent work has shown that the interaction between EBOV GP and NPC1-C is mediated by two protruding loops of NPC1-C that engage a hydrophobic pocket on the surface of cleaved GP (GPcl) (Wang et al., 2016). Prior to cleavage, an 86 amino acid “glycan cap” occupies the NPC1-binding site on EBOV GP (Lee et al., 2008). Hence, uncleaved ebolavirus GPs do not bind to NPC1-C (Miller et al., 2012).
Potent antibodies against marburgvirus recently were isolated from circulating B cells in the blood of a human survivor of natural MVD (Flyak et al., 2015). Among these, antibody MR191 was shown to protect non-human primates against a lethal marburgvirus challenge when treatment was initiated as late as five days post-exposure (Mire et al., 2017). In that study, MR191 provided protection superior to that of two other antibodies in the same competition group, MR78 and MR82 (Mire et al., 2017). Here, we present the crystal structure at 3.2 Å resolution, of trimeric, uncleaved, pre-fusion RAVV GP in complex with antibody MR191 (PDB: 6BP2). This structure is higher in resolution than the marburgvirus GP structure previously available. The higher resolution map reveals that the N-terminal region of marburgvirus GP2 wraps around the outside of the GP core, to occupy a position that in ebolaviruses, is instead held by GP1. This newly visualized subdomain of GP2 anchors a marburgvirus-specific “wing” epitope – the only other epitope that has been yet shown to elicit protective antibodies against MVD (Fusco et al., 2015). This structure also now illustrates the complete internal fusion loop, GP1-GP2 disulfide anchor, CX6CC switch region, and HR2 stalk of RAVV GP, all of which were disordered in structures obtained previously. Fundamental differences between marburgvirus and ebolavirus in the organization of the GP2 wing and the glycosylated regions in GP1 help explain why marburgvirus entry is Cathepsin B and L-independent and why it elicits a different pattern of antibody reactivity than ebolaviruses.
Further, the crystal structure illustrates that the potent therapeutic antibody MR191 binds into the receptor-binding site near the apex of GP1. In ebolaviruses, this site is inaccessible due to the position of the glycan cap in the absence of cathepsin cleavage. However, in the marburgvirus GP, the polypeptide region equivalent to the ebolavirus glycan cap appears to be flexible and does not as effectively block access of antibody to the receptor-binding site. MR191 competes with NPC1-C for binding of GP and appears to mimic NPC1-C (Wang et al., 2016) in its attachment. Contact residues for MR191 are also essential for receptor binding and are highly conserved among related filoviruses. The conservation and importance of its binding site suggests that the footprint of MR191 may be somewhat more resistant to mutagenic escape than other, less conserved antibody epitopes. Interestingly, however, those escape mutations that do arise in cell culture occurred in distant sites, suggesting an allosteric conformational change or an as-yet unknown role of these regions in maintenance of GP quaternary structure.
Results
3.2 Å structure of RAVV GP
Recombinant RAVV GP ectodomain, (residues 1–636, with 257–425 deleted to remove the mucin-like domain) was expressed in Drosophila S2 cells, purified, and complexed with Fab fragments of the human MR191 antibody for crystallization. Data to 3.2 Å were collected from cryo-protected crystals at beamline 23-ID-D of the Advanced Photon Source. Residues 33–180 of GP1, 469–629 of GP2, and glycans attached to N94, N171, and N564 were visible. Residues 2–216 of the light chain and 2–227 of the heavy chain of MR191 also were visible. One GP protomer-Fab complex is contained in the asymmetric unit of the P321 crystals, with the biologically relevant trimer formed about a crystallographic three-fold axis (Figure 1 and Table S1).
Figure 1. Structure of RAVV GP-MR191 complex.
Complete RAVV trimeric GP is illustrated in complex with three MR191 Fab fragments. (A) The heavy chain of each Fab (green) binds into the hydrophobic receptor-binding pocket of GP1 (blue). GP2 is colored gold. Visible glycans are colored with carbon atoms blue for those attached to GP1 and gold for those attached to GP2. Oxygen atoms are red. (B) Top view, from antibody perspective looking onto viral surface. (C) Bottom view, viewing from the viral membrane outwards. The trimeric bundle of HR2 helices is visible at center with HR1 to the outside.
The structure illuminates functionally critical regions of a marburgvirus GP that were disordered in the previous marburgvirus GP structure (Figure 2). First, the internal fusion loop (IFL) of GP2 (residues 514–551) can now be traced in its entirety (Figure 2A). The IFL is anchored to the protein core via an anti-parallel β-strand scaffold with a 20-residue loop containing the hydrophobic fusion peptide. The IFL rests in the GP1/GP2 interface of the adjacent protomer in the GP trimer, and is secured by several hydrophobic interactions and hydrogen bonds.
Figure 2. New features of a marburgvirus GP.
New elements revealed in RAVV GP. (A) The internal fusion loop (yellow) is shown coordinating with GP1 of the neighboring monomer within the trimer. The adjacent GP is shown in surface representation and is colored by hydrophobicity. Residues W532, F535, and F536 of the fusion peptide bind into hydrophobic pockets (red). (B) The GP2 wing anchor (orange) fits between GP1 (blue) and GP2 (gold). L490, F474, and F492 form hydrophobic contacts to secure the wing against the GP1-GP2 core. (C) The C-terminal heptad repeat 2 (HR2) of GP2 is resolved to residue 629, and illustrates hydrophobic packing among central residues I613, L616, I620, I624 and I627. The GP1-GP2 disulfide bond (residue C37-C610) is visible in this higher resolution structure.
Second, we can now visualize an N-terminal region of the GP2, beginning 34 residues downstream of the furin cleavage site and including residues 469–478 and 487–498. These residues anchor the marburgvirus-specific “wing” domain, residues 435–500. This site is targeted by marburgvirus-specific protective antibodies (Fusco et al., 2015) and is the only major recognition site of antibodies against marburgviruses yet described beyond the receptor-binding site. We were able to place the GP2 wing anchor at the base of GP unambiguously, packing against the GP1 core directly beneath the C terminus of the fusion loop and the start of heptad repeat 1 (HR1) (Figure 2B). This observation was unexpected, since this same site on the GP1 core of EBOV or SUDV is not bound by any part of GP2, but instead, by residues 32–45 at the N terminus of GP1 (Figure S5). The wing domain is unique to marburgviruses and results from a 76 residue N-terminal shift in the position of the furin cleavage event (R501 in EBOV, but R435 in MARV) which separates the GP1 and GP2 segments. Therefore, residues at the equivalent sequence region in ebolavirus to the marburgvirus “wing” domain are included in the ebolavirus mucin-like domain and attach to the top of GP1 in ebolaviruses, not to GP2 as in marburgviruses.
The crystal structure also revealed the structure of the heptad repeat 2 (HR2) region, which forms the “stalk” between the GP core and the viral membrane (Figure 2C). Here, HR2 forms a three-helix bundle with five hydrophobic residues from each helix facing inward to form a hydrophobic core, likely stabilizing the trimer. Although these residues differ in sequence from those of ebolaviruses, the hydrophobic packing is conserved (Zhao et al., 2016). Further, an N-linked glycosylation sequon is present in the HR2 of all known filoviruses. This glycan has been visualized for EBOV (Zhao et al., 2016) and likely shields a portion of this conserved site from antibody recognition. Although an NXS glycosylation sequon is present in the sequence of all marburgvirus isolates, a glycan is not visible in this structure, and there does not appear to be enough space for a glycan attached at this site to fit within in the crystal packing. It is unknown if this site is glycosylated on authentic marburgvirus particles. Immediately prior to HR2, the CX6CC disulfide-bearing switch region also can be seen in its entirety. The first and second cysteines in this motif (Cys-602 and Cys-609) form an intra-GP2 disulfide bond that anchors the switch region in a 360° turn as it descends downward to the membrane. The third cysteine in this motif (Cys-610) forms the disulfide anchor to GP1 (Cys-37).
Absence of an ordered glycan cap
In all structures of uncleaved, mucin-deleted EBOV or SUDV GP, a “glycan cap” subdomain of GP1 occupies the hydrophobic NPC1-C binding pocket (Lee et al., 2008; Dias et al., 2011; Bale et al., 2012; Misasi et al., 2016; Pallesen et al., 2016; Zhao et al., 2016). The equivalent residues for marburgviruses (174–256) are included in proteins used for crystallization in this study. The RAVV GP was intact and uncleaved, yet a glycan cap was not visible. Instead, these 82 residues, their five predicted N-linked glycans, and four predicted O-linked glycans are disordered and likely occupy the ~90 Å solvent channels between receptor-binding sites in the crystal packing. Marburgviruses and ebolaviruses possess little sequence identity in this region, and this domain of MARV GP is predicted to be more disordered than that of EBOV GP (Figure S2). These observations suggest that these residues of marburgvirus GP diverge structurally from the corresponding domain of ebolaviruses. A great many marburgvirus antibodies have been identified against the hydrophobic trough of the NPC1-C, while no such antibodies are yet described for ebolaviruses, leading to speculation that this site is more exposed in marburgviruses than ebolaviruses. We note here, however, that NPC1-C is unable to bind uncleaved RAVV GP in vitro (Figure 4A). The RAVV glycan cap, although mobile in MR191- and MR78-bound structures, may still partially shield the receptor-binding site. The antibodies may simply better displace the cap than NPC1-C.
Figure 4. MR191 outcompetes NPC1-C.
(A) GP-coated plates were bound to antibody, blocked and then incubated with HA-tagged NPC1-C in 5-fold dilutions. NPC1-C is unable to bind full-length or mucin-deleted RAVV GP ectodomain. It can, however, bind RAVV GP ectodomain from which the glycan cap is removed by limited proteolysis with trypsin. (B) Competition of MR191 with NPC1-C demonstrated by ELISA. Negligible NPC1-C bound in the presence of MR191 (green). The non-competing mAb MR246, directed against another site on RAVV GP (Flyak et al., 2015), is shown as a control (blue).
Interactions of mAb MR191 with RAVV GP
MR191 binds in the NPC1-C binding site of RAVV GP, interacting with both the hydrophobic trough and the crest at the apex of GP1 (Figure 3 and Figure S4). CDRs H3, H2, L3 and L1 participate in this interaction. CDR H3 extends 11 Å into the hydrophobic trough of GP, with antibody residue F100a (Kabat numbering) at its apex interacting with W70, F72, and M154 of RAVV GP (residues equivalent to W86, F88, and I170 in EBOV GP). Along the C-terminal side of the extended CDR H3, residues V100b and W100d of MR191 form additional hydrophobic interactions with the pocket. Further, residue E100c of MR191 CDR H3 forms a hydrogen bond with Q128 of the crest of GP1, which rises above the hydrophobic trough. Four residues of CDR H2 (S52, S54, N56 and Y58) also hydrogen bond to Q128 and to the main chain carbonyls of D99 and P100 of the GP1 crest (Figure 3). The light chain of MR191 forms a mixture of hydrophobic and hydrophilic contacts with the lower and outer rim of the GP trough.
Figure 3. Receptor binding site and crest interactions.
MR191 binds into the receptor-binding site of RAVV GP. (A) CDR H3 of MR191 (green) engages the hydrophobic trough with F100a binding deepest within the pocket. (B) CDR-H2 of MR191 engages the crest of GP. Residues S52, S54, N56, and Y58 form hydrogen bonds with both the main chain of RAVV GP and side chains of Q128 and T98. (C) Mutagenesis of key hydrophobic residues of CDR-H3. Top, MR191 bearing mutations to residue F100a, and bottom, MR191 bearing mutations to W100d evaluated for binding to RAVV GP. A hydrophobic-aromatic residue appears most important for F100a in the receptor-binding site.
Mimicry of, and competition with, NPC1-C
MR191 mimics the interaction made by NPC1-C Loop 2 in which an extended loop bearing a Phe (F100a in MR191, F131 in NPC1-C) at its apex binds into the GP hydrophobic trough (Wang et al., 2016). A Phe also is employed by the related human mAb MR78 (Hashiguchi et al., 2015) and by the EBOV and SUDV glycan caps, which insert into and masks this region prior to cathepsin cleavage (Lee et. al., 2008; Dias et. al., 2011; Bale et. al., 2012; Zhao et. al., 2016). An aromatic residue appears essential for interaction with this conserved filovirus site: mutation of F100a in the MR191 heavy chain to a tyrosine (F100aY) maintained binding to the GP, while mutation to an alanine (F100aA) greatly reduced the strength of the interaction (Figure 3C). Interestingly, however, the other strongly hydrophobic, aromatic residue inserted into the pocket, W100d, did not appear to be as critical for binding (Figure 3C). Based on their binding sites, it is perhaps unsurprising that MR191 outcompetes NPC1-C when assayed in a competition-binding ELISA (Figure 4). These results suggest that MR191 sterically interferes with the binding of NPC1-C as a primary mechanism of neutralization.
Mutagenesis and binding
MR191 and NPC1-C appear to make similar interactions with the hydrophobic trough of filovirus GP, but only MR191 interacts with the crest (positioned above the receptor binding site). We used mutagenesis to probe the antibody-GP interactions and determine which residues are critical for binding MR191 to marburgvirus GP.
In MR191, in addition to the mutants discussed above, we mutated two residues that interact with the hydrophilic rim around the trough (Y91 and T93 in CDR L3), and four residues that interact with the crest above (S52, S54, N56 and Y58 in CDR H2 and E100c in CDR H3). Notably, no single mutation to any residue that makes hydrophilic interactions, whether to the hydrophilic rim or crest, significantly affected binding: T93A and Y91A mutations in the light chain of MR191 and S54A, N56A, Y58A and Y58F mutations in the heavy chain each resulted in binding of GP equivalent to that of wild-type GP (Figure S3). In contrast, MR191 bearing an F100a to Ala point mutation exhibited a 225-fold increase in EC50 compared to that of wild-type MR191 binding (Figure 3). However, replacing F100a with a Tyr residue retained nearly equivalent levels of binding to that of the wild-type mAb. Mutation of the antibody residue W100d did not appear to affect the EC50 of binding.
In GP, we mutated five residues individually, F72A or W70A in the hydrophobic trough and H124S, Q128S, or N129S in the crest, and we created GP with a Q128S/N129S double mutation in the crest. Four of the five single point mutant GPs did not fold well or express, supporting the intolerance of both the trough and crest in this conserved site to mutagenic substitution (Manicassamy et al., 2007). The only mutants of RAVV GP that did express successfully were GPs with Q128S or Q128S/N129S substitutions. Q128S bound MR191 with a 2.5-fold increase in EC50 compared to wild-type, suggesting that interaction of the antibody with this basic crest is important (Figure S3). This interaction is unique to MR191 and is not made by NPC1-C.
Comparing MR191 to the less protective MR82 and MR78 antibodies
MR191 was found to be more protective than MR82 or MR78 after marburgvirus challenge of guinea pigs (Mire et. al., 2017). All three antibodies are contained in the same competition-binding group for interaction with GP, and all three recognize the NPC1-C binding site (Flyak et. al., 2015; Hashiguchi et. al., 2015). Notably, each of these three antibodies failed to neutralize the escape mutant viruses selected with either of the other two mAbs (Flyak et. al., 2015). We sought to determine if there was a functional difference among the mAbs that could be measured in vitro and explain differences in level of in vivo protection. All three antibodies displayed similar ability to activate human NK or dendritic cells and macrophage- or neutrophil-mediated phagocytosis when bound to marburgvirus GP trimers (Figure S1). One difference noticed structurally between MR191 and MR78’s binding modality is that MR191 coordinates the crest of GP much more thoroughly; however, the importance of this interaction is unclear. Some other factor measurable in vivo, such as improved pharmacokinetics or biodistribution, may be responsible for the apparent superiority of MR191.
MR191 escape mutant viruses
Structural modeling suggested that the footprints of MR191 and NPC1-C on marburgvirus GP overlap significantly, and the residues contacted by each are absolutely conserved in all marburgvirus isolates sequenced to date (Figure 5). To identify potential locations of variant GP residues that could mediate escape from recognition by MR191, we selected and analyzed antibody-resistant GP proteins. A chimeric vesicular stomatitis virus (VSV) displaying MARV GP was incubated with serial two-fold dilutions of MR191 in nine independent replicate experiments (Flyak et. al., 2015). Antibody-resistant virus suspensions were collected and the nucleotide sequence of the gene encoding the GP was determined. MR191-resistant VSV-GP viruses were identified in only three replicates, and were more difficult to isolate than for MR72 and MR78 (Flyak et al., 2015). Notably, when escape mutations were identified for MR191, they were not in the receptor-binding site footprint, but instead, in the region corresponding to the glycan cap and the GP2 wing. The fact that escape only arises with substitution in distant, flexible locations suggests a previously unappreciated role of these regions in the quaternary structure of GP, findings which may be relevant in further exploration of synergistic immunotherapeutic cocktails and in vaccine design.
Figure 5. Overlapping footprints of MR191 and NPC1-C.
(A) Superimposed view of MR191 Fab/RAVV GP and NPC1-C/EBOV GP (PDB: 5F1B) (Wang et al., 2016) complexes. Only RAVV GP is illustrated for clarity. (B) Corresponding footprints of MR191 and NPC1-C overlaid on the RAVV GP trimer and colored as in (A) to illustrate overlap between NPC1-C and MR191. (C) Sequence alignment across historic and modern isolates of marburgvirus. Residues are colored as in (A) with MR191-only contacts in red, NPC1-C only contacts (for EBOV) in blue and shared contacts in purple. Contact residues are highly conserved among marburgviruses. Some residues are also conserved with EBOV and SUDV.
Discussion
This 3.2 Å crystal structure illuminates previously disordered regions of RAVV GP including the internal fusion loop, the CX6CC switch region of GP2 and heptad repeat 2 that forms the stalk below the GP base, as well as the anchor point of the marburgvirus-specific GP2 wing, one of two known protective antibody epitopes for marburgvirus. Unexpectedly, the RAVV GP2 wing anchor was found to wrap about the GP core, in place of the N-terminus of GP1 that binds there in all ebolavirus GP structures. A further difference between marburgvirus and ebolavirus is that although the RAVV GP crystallized contains residues in a similar primary sequence region to that of the ebolavirus glycan cap, none of these residues are visible in the structure. Instead, they are disordered, and as a result, the receptor-binding site appears to be exposed even prior to cathepsin cleavage.
These structural disparities between marburgviruses and ebolaviruses likely explain the differences in antibody reactivity and neutralization. Antibodies against the hydrophobic receptor-binding site constitute the majority of known neutralizing antibodies elicited by marburgvirus described thus far (Flyak et. al., 2015; Hashiguchi et. al., 2015), but no such antibodies are yet known to be elicited by ebolaviruses. Further, although MR191 binds both MARV GPcl and EBOV GPcl, as well as full-length MARV GP, it cannot bind or neutralize full-length EBOV GP, suggesting that the ebolavirus glycan cap more effectively occludes the receptor-binding trough from antibody recognition than does the marburgvirus glycan cap (Brecher et al., 2012; Flyak et al., 2015). Further, numerous antibodies are known against the base of ebolavirus GP such as KZ52, 2G4, 4G7 and mAb 114 (Lee et al., 2008; Dias et al., 2011; Murin et al., 2014; Misasi et al., 2016), but no such antibodies have been described for marburgviruses. The marburgvirus “base” equivalent may be occluded or partially occluded by the marburgvirus-specific wing epitope (Fusco et al., 2015).
MVD and EVD have significant outbreak potential, but lack any licensed therapeutics. Antibodies against these viruses may be used for emergency immunotherapy and in design of improved vaccines. MR191 is the only antibody yet demonstrated to confer complete protection to nonhuman primates after symptoms of MVD have developed, as late as five days after challenge (Mire et. al., 2017). A principal concern with use of an antibody monotherapy, however, is the generation of viral escape mutants. MR191 engages the receptor-binding site of marburgvirus GP with CDR H3, mimicking the binding mode of NPC1-C (Figure 3) and with a footprint that overlaps dramatically with that of NPC1-C (Figure 5). All residues that MR191 contacts in GP are conserved among marburgviruses, with no single divergent mutant present in any strain yet sequenced since its original discovery in 1967 (Figure 5). Further, MR191 also binds EBOV GPcl (Bornholdt et al., 2016; Flyak et al., 2015), which is ~70% different in primary sequence from RAVV in the MR191 footprint residues. MR191 thus appears somewhat tolerant of substitution in its footprint and may be more resistant to escape than single antibodies against other sites. Further, most mutations made to residues in its receptor-binding site footprint, result in poorly folded, poorly expressed GP and/or non-rescuable viruses (Manicassamy et. al., 2007). Hence, while MR191 tolerates substitution in its paratope, RAVV GP seems intolerant of substitution in the MR191 epitope.
Here, however, we note that escape mutations, derived from mAb selections using the chimeric VSV, could be generated in areas distant from the receptor-binding site, in the glycan cap equivalent and in the GP2 wing, consistent with previous observations (Flyak et. al., 2015). Interestingly, these mutations suggest an as-yet-unexplored mechanism by which the disordered regions of GP1 and GP2 influence viral entry or the quaternary structure of GP. It is unknown if such mutations would arise in vivo; escape mutations were not identified in nonhuman primates treated with MR191 (Mire et. al., 2017).
The importance of the receptor-binding site to viral entry, the in vivo performance of the antibody in nonhuman primates, and the conservation and relative resistance of the site to substitution suggests that MR191 is an appropriate first immunotherapeutic for development against MVD. Cocktails could be formulated when antibodies against other marburgvirus GP epitopes show success in nonhuman primates.
STAR Methods
Contact for Reagent and Resource Sharing
Correspondence should be directed to Erica Ollmann Saphire (erica@scripps.edu). Requests for MR191 and other antibodies should be directed to James E. Crowe, Jr. (james.crowe@vanderbilt.edu), which can be made available upon request through a Materials Transfer Agreement.
Experimental Model and Subject details
Plant Strains
Nicotiana benthamiana plants were grown for 24–26 d in an enclosed growth room at 22–24 °C as described in Olinger et al., 2012 and below.
Cells
Stable lines were formed using Drosophila Schneider S2 cells grown in Schneider’s Drosophila Medium at 27 °C. S2 cells for protein expression were grown in Insect-XPRESS™ protein-free medium with L-glutamine (Lonza) supplemented with puromycin (6 μg/mL) (InvivoGen) at 27 °C.
Vero-E6 cells for generation and analysis of chimeric VSV escape mutants were obtained from ATCC and maintained in Dulbecco Minimal Essential Medium (DMEM) (ThermoFisher Scientific) supplemented by 10% fetal bovine serum (HyClone) and 1% penicillin-streptomycin at 5% CO2, 37°C.
Method Details
Construction, expression and purification of RAVV GP and MR191
Ravn virus GPΔmuc (including residues 1–636, with 257–425 deleted to remove the mucin-like domain) was expressed in Drosophila Schneider S2 cells. GP was collected by StepTactin affinity purification (GE Healthcare Life Sciences). Removal of the double Strep tag at the enterokinase cleavage site improved crystallization and was achieved by incubation of RAVV GPΔmuc with enterokinase (Invitrogen) at 2.5 U/mg of glycoprotein at 4 °C overnight followed by passage through on a StrepTactin affinity column.
Hybridoma cells expressing human MR191 IgG were generated previously from peripheral blood mononuclear cells (PBMCs) from a donor who contracted MARV infection while visiting the Python Cave in Queen Elizabeth National Park, Uganda in 2008 (Flyak et. al., 2015). For larger scale production of mAbs MR191, MR78, and MR82, the variable region sequences were used as reported and codon optimized. Genes containing these sequences were synthesized (Life Technologies) and subsequently cloned into plant expression vectors (TMV and PVX, Icon Genetics, GmbH) containing codon-optimized human constant regions followed by transformation into Agrobacterium tumefaciens strain ICF320 (Bendandi et al., 2010).
We used the “magnifection” procedure (Marillonnet et al., 2005) with minor modifications for production of mAb. Plants grown for 4 weeks in an enclosed growth room (20–23°C) were used for vacuum infiltration. Equal volumes of Agrobacterium cultures grown overnight were mixed in infiltration buffer (1 mM MES/10 mM MgSO4, pH 5.5), resulting in a 1:1000 dilution for each individual culture. Infiltration solution was transferred into a 20 L custom built (Kentucky Bioprocessing) vacuum chamber. The aerial parts of the plants were inverted into the bacterial/buffer solution. A vacuum of 0.5 bars was applied for 2 min, and the plants were returned to the growth room. Seven days post-infiltration, leaf tissue was extracted in a juicer (Model GS-1000, Green Star) using 250 mL of chilled extraction buffer (100 mM Tris/40 mM ascorbic acid/1 mM EDTA) per kg of green leaf tissue. The extract was clarified by lowering the pH to 4.8 with 1 M phosphoric acid then re-adjusting to pH 7.5 with 2 M Tris base to insolubilize the plant polymers. The supernatant was transferred and centrifuged at 16,000 x g for 30 min. The clarified extract was filtered (0.2 μm) prior to concentration using the Minim Tangential Flow Filtration System (Pall) and then 0.2 μm was filtered immediately prior to loading onto a 5 mL HiTrap MabSelect SuRe (GE Healthcare Life Sciences) Protein A column at 2 mL/min. The column was washed with running buffer (50 mM HEPES/100 mM NaCl, pH 7.5) and eluted with 0.1 M acetic acid, pH 3.0. The resulting eluate was neutralized to pH 7 using 2 M Tris, pH 8.0, and supplemented with Tween 80 to 0.01%. The IgG containing solution was polished via Q filtration (Mustang Acrodisc Q membrane, Pall), aliquoted, and stored at −80°C until use. Fab fragments were generated from purified IgG using 4% w/w papain digestion for six hours, followed by Mono Q anion exchange chromatography (GE Healthcare Life Sciences), and size exclusion chromatography (GE Healthcare Life Sciences).
Preparation and crystallization of GP-antibody complex
For crystallization, purified RAVV GPΔmuc was mixed with a 10-fold excess of MR191 Fab overnight at room temperature. Complexes were separated from unbound antibody and GP via size-exclusion chromatography on Superdex 200 (GE Healthcare Life Sciences) resin. Crystals were grown via sitting-drop vapor diffusion at room temperature using 0.2 μl of protein (7.0 mg/ml, in 10 mM Tris-HCl (pH 7.5), 100 mM NaCl) and 0.2 μl of mother liquor (100 mM HEPES pH 7.5, 5% PEG 3000, 26% PEG 400, 6% Glycerol). Crystals were harvested and flash-cooled immediately in liquid nitrogen without additional cryoprotectant.
X-ray data collection and experimental structure determination
Single-crystal X-ray diffraction data for the RAVV GP-MR191 Fab complex were collected at beamline 23-ID-D (using a Dectris PILATUS3 6M detector) of the Advanced Photon Source (Argonne National Labs, United States). Images were processed and scaled using XDS (Kabsch, 2010). The initial model was determined by molecular replacement in Phaser (McCoy et al., 2007) using the separate molecules of RAVV GPcl and the Fab fragment from PDB ID: 3X2D (Hashiguchi et. al., 2015) as search models. Further model refinement procedures were carried out using Phenix.refine (Adams et al., 2010) and BUSTER software (Bricogne, 1993). Iterative manual model building and correction were performed using COOT (Emsley and Cowtan, 2004). Models constructed using RosettaCM (see below) were used in structure determination of loops. The final structure was refined to Rwork and Rfree of 26.3 and 29.1 respectively, with a root mean square deviation of 0.012 in bond lengths and 1.520 in bond angles. Phenix.rosetta_refine (DiMaio et al., 2013) was used to select rotamers for several ambiguous residues. The quality of the final model was examined using MolProbity (Chen et al., 2010) and simulated annealing composite omit maps generated in Phenix (Adams et al., 2010). The final structure has been deposited to the RCSB Protein Data Bank under ID code 6BP2.
Rosetta modeling of the MR191-RAVV GP complex and Phenix.Rosetta refinement
MR191 modeling and docking studies were performed to assist experimental X-ray structure determination. Unbound MR191 was first modeled by aligning its sequence to known antibody structures using PSIBLAST (Altschul et al., 1990) and comparative modeling was done using RosettaCM (Song et al., 2013). Torsional angle restraints were applied in RosettaCM to remodel the CDR-H3 (Finn et al., 2016). Nine models of MR191, selected for representation of the most significant clusters and lowest energy scores, were docked onto RAVV GP using RosettaDock (Kaufmann et al., 2010; Bender et al., 2016), as rigid bodies allowing a 3 Å translation and 8° rotation to antibody, while keeping GP fixed. Conformational space was constrained by pre-orienting MR191 to the receptor-binding site using observations from electron microscopy (EM). Four of nine potential complex orientations were pursued after relaxation into EM density. For each of the four docking sets, 1,000 models were generated and analyzed for Rosetta total score and binding energy. The CDR conformations from the two lowest energy models assisted in manual structure refinement into the crystallographic data. This procedure was particularly useful in construction of CDR L1 into electron density.
The best-scoring computationally docked complex, however, has MR191 oriented at a different angle than is observed in the crystal structure. This might be due to deviations in the conformation of CDR H3 between the Rosetta model and crystal structure (Figure S4). The Phenix.Rosetta protocol in Rosetta was run on the manually refined MR191-RAVV GP complex structure to predict side chain rotamers that were ambiguous. The low_resolution_refine.xml script (available in Rosetta/main/source/src/apps/public/crystal_refinement) was used with default parameters and talaris2013 score function (DiMaio et al., 2013).
ELISA evaluation of MR191 mutants
The genes encoding MR191 variable regions were synthesized and cloned into a mammalian IgG expression plasmid vector by GenScript Site-directed mutagenesis was performed using QuikChange Lightning Site-Directed Mutagenesis kit (Agilent). Transient expression of MR191 variants was done in Freestyle™ 293-F cells (Thermo Fisher Scientific). MAbs were harvested from filtered supernatants using HiTrap MabSelectSure columns (Life Technologies). ELISA plates were coated with Drosophila S2 cell-expressed Marburgvirus Ravn GPΔmuc at 4 ng/μl. Wild-type or point mutant MR191 were incubated at 25 μg/ml with six subsequent 10-fold dilutions. Binding was detected with HRP-conjugated anti-human Fc secondary antibodies (Thermo Fischer Scientific), and absorbance was measured using a TECAN Spark 10M. Results were analyzed and EC50 values calculated using GraphPad Prism software.
Effector function studies
NK cell activation and degranulation
3 μg/ml of recombinant, trimeric RAVV GP was coated on a Maxisorp ELISA plate. Plates were blocked with 5% BSA prior to addition of antibodies MR191, MR78, or MR82 (range of concentration 5 μg/ml to 0.1 μg/ml) for 2 hours at 37 °C. Human NK cells were enriched from donor peripheral blood by negative selection using RosetteSep (Stem Cell Technologies) followed by ficoll separation and were incubated with IL-15 (1 ng/ml) overnight at 37°C. The antibodies were removed and the wells washed prior to addition of NK cells. The NK cells were added at 2.5 × 104 cells/well in the presence of brefeldin A (Sigma Aldrich), GolgiStop (BD), and anti-CD107a and incubated for 5 hours at 37°C. NK cells were stained for surface markers of NK cells (CD3, CD56, CD16, BD Biosciences), and then stained intracellularly for the production of cytokines and chemokines (IFNγ and MIP-1β, BD Biosciences). Cells were analyzed by flow cytometry on an LSR II flow cytometer (BD Biosciences), and the resulting data were analyzed using FlowJo software.
Antibody-mediated cellular phagocytosis by human monocytes
RAVV GP was biotinylated and conjugated to streptavidin-coated Alexa488 beads (Life Technologies). Antibodies (range of concentration 5 μg/ml to 0.1 μg/ml) were incubated with beads for 2 hours at 37 °C. Human monocytic cells (THP-1) were added at a concentration of 2.5 × 104 cells/well and incubated for approximately 18 hours at 37 °C. Cells were fixed and analyzed by flow cytometry and a phagocytic score was determined using the percentage of FITC+ cells and the mean fluorescent intensity (MFI) of the FITC+ cells.
Antibody-mediated neutrophil phagocytosis
RAVV GP was biotinylated and conjugated to streptavidin-coated Alexa488 beads. mAbs (range of concentration 5 μg/ml to 0.1 μg/ml) were incubated with beads for 2 hours at 37 °C. Human neutrophils freshly isolated from peripheral blood were added at a concentration of 5 × 104 cells/well and incubated for 1 hour at 37 °C. Cells stained for neutrophil markers (neutrophils were defined as high granularity SSC-Ahigh, CD66b+, CD14−, CD3−) were analyzed by flow cytometry. A phagocytic score was determined using the percentage of FITC+ cells and the mean fluorescent intensity (MFI) of the FITC+ cells.
Antibody-dependent dendritic cell phagocytosis
Monocyte-derived dendritic cells (moDC) were generated from CD14+ monocytes isolated from peripheral blood and differentiated into moDC with IL-4 and GM-CSF (Miltenyi Biotec) for 6 days. Differentiation was confirmed by flow cytometry staining of CD14, CD209/DC-SIGN and CD83. Marburgvirus Ravn GP was biotinylated and conjugated to streptavidin-coated Alexa488 beads. Abs (5 μg/ml) were incubated with beads for 2 hours at 37 °C prior to addition of moDCs at 1 × 105 cells/well and incubated with moDCs for an additional 18 hours at 37 °C. moDCs were stained for surface expression of HLA-DR, CD80, and CD86 (BD Biosciences), fixed, and analyzed by flow cytometry. Expression of activation markers was determined for FITC+ moDC by MFI.
Generation of antibody escape mutants
To generate MR191 escape mutants, aliquots containing 100 pfu of chimeric VSV in which G was replaced with GP of MARV strain Uganda 2007 (Flyak et al., 2015) were pre-incubated with serial 2-fold dilutions starting from 200 μg/ml of MR191 mAb for 1 hour at 37 °C, and then inoculated in Vero-E6 cell monolayer cultures in 96-well plates, as multiple independent replicates. After 48 hours, virus samples were harvested and titrated. For each replicate, a virus-positive preparation from the highest antibody concentration was selected for the next passage. After three passages, 200 pfu virus aliquots were pre-incubated with the highest corresponding MR191 concentrations used for the third passage, and inoculated into 24-well plate Vero-E6 cell monolayers. After 24–48 hours, based on observed cytopathic effect, virus samples were harvested and titrated, and the infected cell monolayers were lysed in 1 ml of TRIzol (Life Technologies) and subjected to total RNA isolation and sequencing of the gene encoding MARV GP.
Quantification and Statistical Analysis
Graphpad Prism software was used to determine average values, standard errors, and standard deviations. For each figure, the number of experimental replicates and other information relevant for assessing the accuracy and precision of the analysis are included in the accompanying legend.
Data and Software Availability
The structure factors and experimental model have been deposited in the RCSB Protein Data Bank under ID code 6BP2.
Supplementary Material
Highlights.
3.2 Å structure of mAb MR191 complexed with trimeric marburgvirus surface glycoprotein
MR191 neutralizes by occupying the conserved receptor-binding site
MR191 competes with the host receptor Niemann-Pick C1
Escape mutants map outside the MR191 receptor-binding site suggesting importance of poorly visualized domains in quaternary structure
Acknowledgments
We thank Drs. Zachary Bornholdt and Larry Zeitlin of Mapp Biopharmaceutical for the gift of MR191, MR82 and MR78 IgG and for helpful discussions. R01AI089498 and U19AI109762 (EOS), U19AI109762 (GA), HDTRA1-13-1-0034 (JEC), NIH 1U19AI109711 (JEC and AB), and R21AI121799 (JM) provided financial support. We thank the staff of beamline 23-ID-D of the Advanced Photon Source, and beamline 12-2 of the Stanford Synchrotron Radiation Lightsource for assistance with data collection. This research used resources of the Advanced Photon Source, a U.S. Department of Energy (DOE) Office of Science User Facility operated for the DOE Office of Science by Argonne National Laboratory under Contract No. DE-AC02-06CH11357. Use of the Stanford Synchrotron Radiation Lightsource, SLAC National Accelerator Laboratory, is supported by the U.S. Department of Energy, Office of Science, Office of Basic Energy Sciences under Contract No. DE-AC02-76SF00515. The SSRL Structural Molecular Biology Program is supported by the DOE Office of Biological and Environmental Research, and by the National Institutes of Health, National Institute of General Medical Sciences (including P41GM103393). Coordinates and structure factors for the MR191-RAVV GP complex have been deposited into the Protein Data Bank under accession number 6BP2. In light of the higher resolution map described here, the earlier model of RAVV GP (PDB:3X2D) has been updated and is available at PDB:5UQY. This is manuscript number 29544 from The Scripps Research Institute.
Footnotes
Declaration of Interests:
J.E.C., A.B., A.F., and A.I. are listed as co-inventors for a patent submitted, which includes in part claims relating to MR191. The MR191 antibody has been licensed by Vanderbilt University to a commercial partner.
Author Contributions:
Conceptualization L.B.K., M.L.F., A.B., J.E.C., and E.O.S. Methodology L.B.K., M.L.F., B.G., R.N.K., and A.K.S. Validation R.N.K. and K.M.H. Investigation L.B.K, M.L.F, A.I.F., P.A.I., B.G., and A.K.S. Resources J.E.C. and E.O.S. Writing – Original Draft L.B.K and E.O.S. Writing, Review and Editing - all authors. Visualization L.B.K. and E.O.S. Supervision J.M., G.A., A.B., J.E.C., and E.O.S. Project Administration J.E.C., A.B., and E.O.S., Funding Acquisition J.M., G.A., A.B., J.E.C., and E.O.S.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adams PD, et al. PHENIX: a comprehensive Python-based system for macromolecular structure solution. Acta Crystallogr D. 2010;66(Pt 2):213–221. doi: 10.1107/S0907444909052925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aleksandrowicz P, et al. Ebola virus enters host cells by macropinocytosis and clathrin-mediated endocytosis. J Infect Dis. 2011;204(Suppl):S957–67. doi: 10.1093/infdis/jir326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altschul SF, et al. Basic local alignment search tool. J Mol Bio. 1990;215(3):403–410. doi: 10.1016/S0022-2836(05)80360-2. [DOI] [PubMed] [Google Scholar]
- Bale S, et al. Structural basis for differential neutralization of ebolaviruses. Viruses. 2012;4(4):447–470. doi: 10.3390/v4040447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bendandi M, et al. Rapid, high-yield production in plants of individualized idiotype vaccines for non-Hodgkin’s lymphoma. Ann Oncol. 2010;21(12):2420–2427. doi: 10.1093/annonc/mdq256. [DOI] [PubMed] [Google Scholar]
- Bender BJ, et al. Protocols for Molecular Modeling with Rosetta3 and RosettaScripts. Biochem. 2016;55(34):4748–4763. doi: 10.1021/acs.biochem.6b00444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bornholdt ZA, et al. Host-Primed Ebola Virus GP Exposes a Hydrophobic NPC1 Receptor-Binding Pocket, Revealing a Target for Broadly Neutralizing Antibodies. MBio. 2015;7(1) doi: 10.1128/mBio.02154-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brecher M, et al. Cathepsin cleavage potentiates the Ebola virus glycoprotein to undergo a subsequent fusion-relevant conformational change. J Virol. 2012;86(1):364–372. doi: 10.1128/JVI.05708-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bricogne G. Direct phase determination by entropy maximization and likelihood ranking: status report and perspectives. Acta Crystallogr D. 1993;49(Pt 1):37–60. doi: 10.1107/S0907444992010400. [DOI] [PubMed] [Google Scholar]
- Burton DR, Saphire EO. Swift antibodies to counter emerging viruses. P Natl Acad Sci USA. 2015;112(33):10082–10083. doi: 10.1073/pnas.1513050112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carette JE, et al. Ebola virus entry requires the cholesterol transporter Niemann-Pick C1. Nature. 2011;477(7364):340–343. doi: 10.1038/nature10348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. Brief Report: Outbreak of Marburg Virus Hemorrhagic Fever --- Angola, October 1, 2004 -- March 29, 2005. CDC; 2005. Available at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm54d330a1.htm. [PubMed] [Google Scholar]
- Chandran K, et al. Endosomal proteolysis of the Ebola virus glycoprotein is necessary for infection. Science. 2005;308(5728):1643–1645. doi: 10.1126/science.1110656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chanock RM, et al. Human monoclonal antibody Fab fragments cloned from combinatorial libraries: potential usefulness in prevention and/or treatment of major human viral diseases. Infect Agent Dis. 1993;2(3):118–131. [PubMed] [Google Scholar]
- Chen VB, et al. MolProbity: all-atom structure validation for macromolecular crystallography. Acta Crystallogr D. 2010;66(Pt 1):12–21. doi: 10.1107/S0907444909042073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dias JM, et al. A shared structural solution for neutralizing ebolaviruses. Nat Struct Mol Biol. 2011;18(12):1424–1427. doi: 10.1038/nsmb.2150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiMaio F, et al. Improved low-resolution crystallographic refinement with Phenix and Rosetta. Nat methods. 2013;10(11):1102–1104. doi: 10.1038/nmeth.2648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dye JM, et al. Postexposure antibody prophylaxis protects nonhuman primates from filovirus disease. P Natl Acad Sci USA. 2012;109(13):5034–5039. doi: 10.1073/pnas.1200409109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emsley P, Cowtan K. Coot: model-building tools for molecular graphics. Acta Crystallogr D. 2004;60(Pt 12 Pt 1):2126–2132. doi: 10.1107/S0907444904019158. [DOI] [PubMed] [Google Scholar]
- Feldmann H, Klenk HD, Sanchez A. Molecular biology and evolution of filoviruses. Arch Vir S. 1993;7:81–100. doi: 10.1007/978-3-7091-9300-6_8. [DOI] [PubMed] [Google Scholar]
- Finn JA, et al. Improving Loop Modeling of the Antibody Complementarity-Determining Region 3 Using Knowledge-Based Restraints. PloS one. 2016;11(5):e0154811. doi: 10.1371/journal.pone.0154811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flyak AI, et al. Mechanism of human antibody-mediated neutralization of Marburg virus. Cell. 2015;160(5):893–903. doi: 10.1016/j.cell.2015.01.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Froude JW, et al. Generation and characterization of protective antibodies to Marburg virus. mAbs. 2017;9(4):696–703. doi: 10.1080/19420862.2017.1299848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fusco ML, et al. Protective mAbs and Cross-Reactive mAbs Raised by Immunization with Engineered Marburg Virus GPs. PLoS Path. 2015;11(6):e1005016. doi: 10.1371/journal.ppat.1005016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gnirss K, et al. Cathepsins B and L activate Ebola but not Marburg virus glycoproteins for efficient entry into cell lines and macrophages independent of TMPRSS2 expression. Virology. 2012;424(1):3–10. doi: 10.1016/j.virol.2011.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong X, et al. Structural Insights into the Niemann-Pick C1 (NPC1)-Mediated Cholesterol Transfer and Ebola Infection. Cell. 2016;165(6):1467–1478. doi: 10.1016/j.cell.2016.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Group PIW, Multi-National PIIST. A Randomized, Controlled Trial of ZMapp for Ebola Virus Infection. New Engl J Med. 2016;375(15):1448–1456. doi: 10.1056/NEJMoa1604330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashiguchi T, et al. Structural basis for Marburg virus neutralization by a cross-reactive human antibody. Cell. 2015;160(5):904–912. doi: 10.1016/j.cell.2015.01.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hood CL, et al. Biochemical and structural characterization of cathepsin L-processed Ebola virus glycoprotein: implications for viral entry and immunogenicity. J Virol. 2010;84(6):2972–2982. doi: 10.1128/JVI.02151-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ishida T, Kinoshita K. PrDOS: prediction of disordered protein regions from amino acid sequence. Nucleic Acids Res. 2007;35(Web Server issue):W460–4. doi: 10.1093/nar/gkm363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabsch W. Integration, scaling, space-group assignment and post-refinement. Acta Crystallogr D. 2010;66(Pt 2):133–144. doi: 10.1107/S0907444909047374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufmann KW, et al. Practically useful: what the Rosetta protein modeling suite can do for you. Biochemistry-US. 2010;49(14):2987–2998. doi: 10.1021/bi902153g. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lachmann PJ. The use of antibodies in the prophylaxis and treatment of infections. Emerg Microbes Infec. 2012;1(8):e11. doi: 10.1038/emi.2012.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee JE, et al. Structure of the Ebola virus glycoprotein bound to an antibody from a human survivor. Nature. 2008;454(7201):177–182. doi: 10.1038/nature07082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manicassamy B, et al. Characterization of Marburg virus glycoprotein in viral entry. Virology. 2007;358(1):79–88. doi: 10.1016/j.virol.2006.06.041. [DOI] [PubMed] [Google Scholar]
- Marillonnet S, et al. Systemic Agrobacterium tumefaciens-mediated transfection of viral replicons for efficient transient expression in plants. Nature Biotechnol. 2005;23(6):718–723. doi: 10.1038/nbt1094. [DOI] [PubMed] [Google Scholar]
- Marzi A, Reinheckel T, Feldmann H. Cathepsin B & L are not required for ebola virus replication. PLoS Neglect Trop D. 2012;6(12):e1923. doi: 10.1371/journal.pntd.0001923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCoy AJ, et al. Phaser crystallographic software. J Appl Crystallogr. 2007;40(Pt 4):658–674. doi: 10.1107/S0021889807021206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller EH, et al. Ebola virus entry requires the host-programmed recognition of an intracellular receptor. EMBO J. 2012;31(8):1947–1960. doi: 10.1038/emboj.2012.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mire CE, et al. Therapeutic treatment of Marburg and Ravn virus infection in nonhuman primates with a human monoclonal antibody. Sci Transl Med. 2017;9(384) doi: 10.1126/scitranslmed.aai8711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Misasi J, et al. Structural and molecular basis for Ebola virus neutralization by protective human antibodies. Science. 2016;351(6279):1343–1346. doi: 10.1126/science.aad6117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulherkar N, et al. The Ebola virus glycoprotein mediates entry via a non-classical dynamin-dependent macropinocytic pathway. J Virol. 2011;419(2):72–83. doi: 10.1016/j.virol.2011.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murin CD, et al. Structures of protective antibodies reveal sites of vulnerability on Ebola virus. P Natl Acad Sci USA. 2014;111(48):17182–17187. doi: 10.1073/pnas.1414164111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nanbo A, et al. Ebolavirus is internalized into host cells via macropinocytosis in a viral glycoprotein-dependent manner. PLoS Path. 2010;6(9):e1001121. doi: 10.1371/journal.ppat.1001121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pallesen J, et al. Structures of Ebola virus GP and sGP in complex with therapeutic antibodies. Nat Microbiol. 2016;1(9):16128. doi: 10.1038/nmicrobiol.2016.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu X, et al. Reversion of advanced Ebola virus disease in nonhuman primates with ZMapp. Nature. 2014;514(7520):47–53. doi: 10.1038/nature13777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saeed MF, et al. Cellular entry of ebola virus involves uptake by a macropinocytosis-like mechanism and subsequent trafficking through early and late endosomes. PLoS Path. 2010;6(9):e1001110. doi: 10.1371/journal.ppat.1001110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schornberg K, et al. Role of endosomal cathepsins in entry mediated by the Ebola virus glycoprotein. J Virol. 2006;80(8):4174–4178. doi: 10.1128/JVI.80.8.4174-4178.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song Y, et al. High-resolution comparative modeling with RosettaCM. Structure. 2013;21(10):1735–1742. doi: 10.1016/j.str.2013.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volchkov VE, et al. Processing of the Ebola virus glycoprotein by the proprotein convertase furin. P Natl Acad Sci USA. 1998;95(10):5762–5767. doi: 10.1073/pnas.95.10.5762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volchkov VE, et al. Proteolytic Processing of Marburg Virus Glycoprotein. Virology. 2000;268(1):1–6. doi: 10.1006/viro.1999.0110. [DOI] [PubMed] [Google Scholar]
- Wang H, et al. Ebola Viral Glycoprotein Bound to Its Endosomal Receptor Niemann-Pick C1. Cell. 2016;164(1–2):258–268. doi: 10.1016/j.cell.2015.12.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Ebola virus disease. 2014 Available at: http://www.who.int/mediacentre/factsheets/fs103/en/
- Zeitlin L, Cone RA, Whaley KJ. Using monoclonal antibodies to prevent mucosal transmission of epidemic infectious diseases. Emerg Infect Dis. 1999;5(1):54–64. doi: 10.3201/eid0501.990107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y, et al. Structure of glycosylated NPC1 luminal domain C reveals insights into NPC2 and Ebola virus interactions. FEBS Letters. 2016;590(5):605–612. doi: 10.1002/1873-3468.12089. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.







