Abstract
Human leukocyte antigen-G (HLA-G) is a non-classical HLA molecule, predominantly expressed in cytotrophoblast cells to protect the fetus during pregnancy. Notably, a high frequency of HLA-G expression has been observed in a wide variety of cancer types in previous studies. Furthermore, HLA-G expression in cancer has been considered to be detrimental, since it can protect cancer cells from natural killer cell cytotoxic T lymphocyte-mediated destruction, promote tumor spreading and shorten the survival time of patients by facilitating tumor immune evasion. In addition, HLA-G polymorphisms have been investigated in numerous types of cancer and are considered as risk factors and predictive markers of cancer. This review focuses on HLA-G expression and its polymorphisms in cancer, analyzing the mechanisms of HLA-G in promoting cancer development, and evaluating the potential and value of its clinical application as a diagnostic and prognostic biomarker, or even as a prospective therapeutic target in certain types of tumors.
Keywords: human leukocyte antigen-G, cancer, genetic polymorphism, immune evasion, tumor development, therapeutic target
1. Introduction
Human leukocyte antigen-G (HLA-G), a non-classical major histocompatibility complex class I (MHC-I) antigen, has well-recognized tolerogenic properties (1). HLA-G has been detected under physiological conditions in fetal tissues, adult immune-privileged organs and cells of the hematopoietic lineage (1), as well as under pathological conditions in cancer, viral infections, inflammatory diseases, autoimmune diseases and transplantation (2).
HLA-G was first detected at the maternal-fetal interface in the trophoblast, possibly performing a role in the modulation of the maternal immune system during pregnancy (3). The expression of HLA-G in fetal tissue successfully suppressed the local immune response in the placenta, therefore inducing maternal-fetal tolerance, preventing the fetus from being recognized as a non-self tissue and protecting it from lysis mediated by natural killer (NK) cells (4). Similarly, HLA-G expression in tumors can also protect cancer cells from NK cell and cytotoxic T lymphocyte (CTL)-mediated destruction (5). In this context, HLA-G expression may be a mechanism used by cancer cells to escape host immune surveillance.
Differing from classical HLA, the HLA-G gene presents limited coding region variability (6). Variation at the 5′ upstream regulatory region (5′URR) and 3′ untranslated region (3′UTR) has been observed most frequently (6). Several lines of evidence have indicated that HLA-G polymorphisms affect the expression level of HLA-G, the production of different isoforms and the pattern of alternative splicing (7,8). Polymorphisms in HLA-G have been studied in pathophysiological conditions, revealing that HLA-G polymorphisms are associated with numerous types of disorders, including pre-eclampsia (9), recurrent spontaneous abortion (10), asthma (11), systemic lupus erythematosus (12) and pemphigus vulgaris (13). In addition, several isolated segments of the HLA-G gene have been studied in different tumor types and were identified to be associated with tumor progression (14).
The present review discusses HLA-G expression and its gene polymorphisms in tumors, and analyzes its underlying mechanisms in promoting tumor development. Furthermore, the possible clinical applications of HLA-G (or sHLA-G) as a diagnostic and prognostic biomarker for cancer, and as a potential therapeutic target for cancer biotherapy are considered.
2. Structure and physiology of HLA-G
HLA-G is a MHC-I antigen encoded by a gene on chromosome 6 at region 6p21.3 (15). It has been termed as a non-classical HLA class I molecule, since it differs from classical HLA class I molecules due to its unique promoter region, limited polymorphism, restricted tissue distribution and immunosuppressive function (16). The structure of HLA-G is different to HLA class I (17). The main difference resides in the presence of a stop codon in exon 6, which generates a shorter HLA-G protein compared with the classical HLA-G class I molecule (17). Compared with the high incidence of polymorphism in classical HLA class I molecules, HLA-G exhibits limited genetic polymorphism with only 50 alleles, which are distributed within the α1, α2 and α3 domains (15). HLA-G consists of seven isoforms, including four membrane-bound isoforms (HLA-G1-HLA-G4) and three secreted isoforms (sHLA-G; HLA-G5-HLA-G7), which are generated by alternate splicing of primary transcripts (18). sHLA-Gs contain an intron 4-encoded stop codon, resulting in the lack of transmembrane domain (19). Membrane-bound HLA-G1 and its soluble counterpart, HLA-G5 have been most studied in tissues or cells of organisms (1). In addition, sHLA-G molecules may also be shed via the proteolytic cleavage of membrane-bound HLA-G1 (20). Therefore, sHLA-G consists of sHLA-G1 and HLA-G5, of which HLA-G5 is the primary component (20). HLA-G1 and HLA-G5 are composed of heavy chains consisting of three globular domains (α1, α2, α3), which non-covalently bind to β2-microglobulin (β2-m), and a nonapeptide, while the other isoforms lacking one or two globular domains can bind neither β2-m nor present peptides (21).
In healthy individuals, HLA-G was first detected in extra-villous cytotrophoblast at the maternal-fetal interface, being regarded as a molecule that modulates the maternal immune system during pregnancy (3). It is also expressed by amnion epithelial cells, endothelial cells of fetal blood vessels in the placenta, erythroblasts, macrophages, antigen-presenting cells and dendritic cells (DCs), as well as by immune-privileged organs of adults, including the thymus, cornea and pancreatic islets (22). Additionally, ectopic HLA-G expression can be induced in various pathological conditions, including cancer, viral infections, inflammatory diseases, viral infections, autoimmune diseases and transplantation (1).
Considered as immunomodulatory molecules, HLA-G antigens can induce immunological tolerance by inhibiting certain immune-competent cells (22). The immune-suppressive function of HLA-G antigens may be mediated by binding membrane-bound and sHLA-G to their specific inhibitory receptors (23). Regarding these receptors, HLA-G antigens preferentially act as ligands for immunoglobulin-like transcript 2 (ILT2) and immunoglobulin-like transcript 4 (ILT4) (23). ILT2 is expressed by B cells/T cells/NK cells/monocytes/DCs, and ILT4 is presented on monocytes/macrophages/DCs (24,25). In addition, HLA-G antigens were also reported to be ligands for the killer cell immunoglobulin-like receptor [KIR2DL4/p49 (CD158d)], which is expressed on NK cells (26). The direct interactions between HLA-G proteins and their specific inhibitory receptors promote the maintenance of tolerance at different stages of the immune response, consisting of differentiation, proliferation, cytolysis and cytokine secretion (27). It was also demonstrated that HLA-G could modulate the differentiation of DCs by interacting with ILT4, which requires the interleukin (IL)-6-signal transducer and activator of transcription 3 (STAT3) signaling pathway and results in the recruitment of Src homology region 2 domain-containing phosphatase (SHP)-1 and SHP-2 protein tyrosine phosphatases (28). Furthermore, the cell cycle of human-activated T cells can be suppressed by activating SHP-2 phosphatase and inhibiting the mechanistic target of rapamycin pathway mediated by HLA-G (29). Notably, HLA-G may upregulate the inhibitory receptors in immune cells, which may precede an immune response and be involved in immune escape mechanisms by increasing their activation thresholds (30).
In addition to these direct effects, HLA-G can implement its indirect immune-inhibitory function through the expression of non-classical HLA class I molecule HLA-E (16,31). HLA-E can directly bind the peptides derived from HLA-G, and the HLA-E/peptide complexes can interact with the inhibitory receptor CD94/NKG2A, which is predominantly expressed on NK cells (31). Thus, the effect of HLA-E on immune cells is of great importance for the inhibition of NK and T cell reactivity (31). Indeed, HLA-G-mediated immune tolerance may be extended to induce regulatory T cells (Tregs), a subpopulation of T cells possessing abilities to modulate the immune system, abrogate the autoimmune reaction and maintain the tolerance-to-self antigens (32). For instance, in the presence of HLA-G, CD4+ and CD8+ T cells may lose their capability to respond to antigenic stimulation and be differentiated into Tregs (32).
3. HLA-G expression and plasma sHLA-G levels in cancer and their association with clinical parameters
Since the ectopic expression of HLA-G in tumor cells was first described in melanoma by Paul et al (5) in 1998, a high frequency of HLA-G expression and plasma sHLA-G levels have been observed successively in different solid tumor types, as well as in hematological malignancies, including melanoma (33,34), breast cancer (35–44), lung cancer (45–49), hepatocellular carcinoma (50–53), colorectal cancer (49,54–58), gastric cancer (49,59–61), esophageal carcinoma (49,62–65), nasopharyngeal carcinoma (66), laryngeal lesions (67), bladder transitional cell carcinoma (68), renal cell carcinoma (69–72), cervical cancer (73), thyroid carcinoma (74,75), neuroblastoma (76,77), glioblastoma (78–81) and myeloid leukemia (82). HLA-G expression in various cancer types is listed in Table I, and data regarding plasma sHLA-G levels detected by ELISA are presented in Table II. As shown in Table II, in the majority of cancer types, serum sHLA-G levels were significantly higher in patients with cancer compared with in the healthy controls. Notably, sHLA-G levels were similar between patients with bladder transitional cell carcinoma (TCC) and healthy controls (68).
Table I.
HLA-G expression in different cancer types.
| Tumor type | Method | Total number | HLA-G+ number | HLA-G+, % | (Refs.) |
|---|---|---|---|---|---|
| Melanoma | IHC | 79 | 22 | 28.0 | (33) |
| Breast cancer | IHC | 52 | 31 | 59.6 | (35) |
| IHC | 38 | 22 | 58.0 | (36) | |
| IHC | 36 | 14 | 36.0 | (37) | |
| IHC | 58 | 41 | 70.7 | (38) | |
| IHC | 235 | 155 | 66.0 | (39) | |
| IHC | 667 | 400 | 60.0 | (40) | |
| IHC | 45 | 28 | 62.0 | (41) | |
| IHC | 45 | 29 | 64.4 | (42) | |
| Lung cancer | IHC | 34 | 9 | 26.0 | (45) |
| IHC | 106 | 79 | 75.0 | (46) | |
| IHC | 101 | 42 | 41.6 | (47) | |
| Hepatocellular carcinoma | IHC | 173 | 99 | 57.0 | (50) |
| IHC | 219 | 110 | 50.2 | (51) | |
| WB | 36 | 24 | 66.7 | (52) | |
| Colorectal cancer | RT-PCR | 39 | 34 | 87.0 | (54) |
| IHC | 201 | 130 | 64.6 | (55) | |
| IHC | 251 | 51 | 20.3 | (56) | |
| IHC | 102 | 72 | 70.6 | (57) | |
| Gastric cancer | IHC | 160 | 113 | 71.0 | (59) |
| IHC | 179 | 89 | 49.7 | (60) | |
| IHC | 52 | 16 | 31.0 | (61) | |
| Esophageal carcinoma | IHC | 121 | 110 | 90.9 | (62) |
| IHC | 79 | 52 | 65.8 | (63) | |
| IHC | 60 | 40 | 75.0 | (64) | |
| IHC | 60 | 42 | 70.0 | (65) | |
| Nasopharyngeal carcinoma | IHC | 552 | 437 | 79.2 | (66) |
| Laryngeal lesions | IHC | 109 | / | / | (67) |
| Bladder TCC | IHC | 75 | 51 | 68.0 | (68) |
| Renal cell carcinoma | IHC | 18 | 11 | 61.0 | (69) |
| IHC | 38 | 29 | 76.0 | (70) | |
| Clear cell renal carcinoma | IHC | 12 | 7 | 58.0 | (71) |
| IHC | 95 | 47 | 49.5 | (72) | |
| Cervical lesions | IHC | 129 | 81 | 62.8 | (73) |
| PT | IHC | 70 | 30 | 44.3 | (74) |
| IHC | 72 | 56 | 77.8 | (75) | |
| FTC | IHC | 19 | 17 | 90.0 | (75) |
| Neuroblastoma | IHC | 12 | 0 | 0.0 | (76) |
| FC | 9 | 9 | 100.0 | (77) | |
| Glioblastoma | IHC | 5 | 4 | 80.0 | (78) |
| IHC | 26 | 15 | 58.0 | (79) | |
| IHC | 39 | 25 | 64.0 | (80) | |
| IHC | 108 | 65 | 60.2 | (81) |
HLA-G, human leukocyte antigen-G; IHC, immunohistochemistry; WB, western blot analysis; RT-PCR, reverse transcription-polymerase chain reaction; FC, flow cytometry; TCC, transitional cell carcinoma of the human bladder; PTC, papillary thyroid cancer; FTC, follicular thyroid cancer.
Table II.
Plasma sHLA-G level detected by ELISA.
| Tumor type | Number (α/β)a | sHLA-G concentrate (α' vs. β')b | (Refs.) |
|---|---|---|---|
| Melanoma | 190/126 | 41.95±2.15 vs. 22.92±1.51 ng/mlc | (34) |
| Breast cancer | 80/80 | 117.2 vs. 10.1 U/mld | (43) |
| 120/40 | 70.59 vs. 46.05 U/mld | (44) | |
| 92/70 | 82.19 vs. 9.65 U/mld | (38) | |
| 44/48 | 0.78 vs. 0.43 µg/mlc | (39) | |
| 45/40 | 35 vs. 7.6 ng/md | (42) | |
| 120/40 | 70.59 vs. 46.05 U/mld | (44) | |
| Lung cancer | 91/150 | 32.0 vs. 20.4 U/mld | (47) |
| 137/84 | 34 vs. 14 ng/mld | (48) | |
| 43/120 | 64 vs. 34 U/mld | (49) | |
| Thyroid cancer | 183/245 | 42.9 vs. 8.5 U/mld | (83) |
| Hepatocellular carcinoma | 19/86 | 92.49 vs. 9.29 U/mld | (51) |
| 36/25 | 132.6 vs. 47.0 U/mld | (52) | |
| 80/50 | 178.8 vs. 6.8 U/mld | (53) | |
| Colorectal cancer | 144/60 | 124.3 vs. 25 U/mld | (58) |
| 37/129 | 84 vs. 34 U/mld | (49) | |
| Gastric cancer | 58/64 | 130 vs. 38 U/mld | (60) |
| 28/120 | 73 vs. 34 U/mld | (49) | |
| Esophageal carcinoma | 41/153 | 152.4 vs. 8.9 U/mld | (63) |
| 58/120 | 77 vs. 34 U/mld | (49) | |
| 60/28 | 15.04 vs. 6.81 U/mld | (65) | |
| Bladder TCC | 15/105 | 10.75 vs. 8.69 U/mld | (68) |
| Clear cell renal carcinoma | 16/144 | 39.5 vs. 19.2 U/mld | (72) |
| Neuroblastoma | 53/53 | 26.1±6.97 vs. 4.409±0.808 ng/mlc | (76) |
| AML | 47/37 | 16.23±6.17 vs. 52.8±32.7 ng/mlc | (82) |
| ALL | 28/37 | 16.23±6.17 vs. 63.4±35.8 ng ng/mlc | (82) |
α represents the number of tumor patients, β represents the number of healthy controls.
α' represents the plasma sHLA-G level of tumor patients and β' represents the plasma sHLA-G level of healthy controls.
Quantitative variables are expressed as the mean ± standard error of the mean.
Quantitative variables are expressed as median levels. TCC, transitional cell carcinoma; AML, acute myeloid leukemia; ALL, acute lymphoblastic leukemia; sHLA-G, soluble iman leukocyte antigen-G.
However, the associations between increased HLA-G expression and the clinical parameters of patients with cancer remain conflicting. Although there was a significant association between increased HLA-G expression levels and certain clinical parameters, including advanced disease stage, poor histological grade, higher tumor grade, presence of metastasis, shorter survival time, greater tumor size, tumor recurrence or tumor invasion in many types of tumors (27), the association was not detected in other tumors, including bladder TCC (68) and acute myeloid leukemia (82). Although several studies have demonstrated that high serum sHLA-G levels were associated with aggressive behavior in cancer, histological type, tumor-node-metastasis stage or a shorter survival time of patients suffering from breast cancer, papillary thyroid carcinoma (PTC) and lung cancer among others, no clear associations were identified between the plasma sHLA-G levels and the clinicopathological parameters in colorectal cancer, hepatocellular carcinoma, esophageal carcinoma, renal cell carcinoma and gastric cancer (38,43,45,83). Notably, numerous factors may affect sHLA-G expression (65,82). The upregulated plasma IL-10 level in primary esophageal squamous cell carcinoma was determined to be associated with high sHLA-G levels (65). In addition, sHLA-G levels have been established as associated with the deficiency of anterior myelodysplasia along with higher leukocytosis in acute myeloid leukemia (82). Notably, contradictions exist in the same type of tumor between different studies. For instance, Kren et al (70) confirmed that HLA-G is upregulated in renal cell carcinoma tissues and that it is associated with a worse prognosis. By contrast, Reimers et al (84) reported that weak HLA-G expression was associated with a poor prognosis and a significantly worse survival. These contradictions may possibly be attributed to differing ethnicities in the patient cohorts, varied criteria of patient selection, the methods used and factitious surgical errors.
4. HLA-G polymorphisms promote cancer development
Compared with classical HLA, the HLA-G gene presents limited coding region variability (6). However, variations at the 5′URR and at the 3′UTR have been observed in numerous previous studies (6,85–87). Recently, a number of studies indicated that HLA-G polymorphisms are associated with HLA-G expression (41), cancer susceptibility (88–91) and cancer development (86).
Although it remains a controversial issue as to where HLA-G transcription begins, the polymorphisms at the 5′URR and haplotypes at the 3′UTR are considered to affect HLA-G expression (7). In healthy Brazilian and French individuals, the 14-bp del/del genotype exhibited higher sHLA-G levels compared with the 14-bp ins/ins genotype (85). Additionally, in patients with invasive ductal carcinoma, 14-bp ins/del polymorphisms may induce a higher expression of the HLA-G molecule compared with 14-bp ins/ins and 14-bp del/del polymorphisms (41). The differential expression levels were attributed to the fact that polymorphic sites at the 5′URR coincided with the known transcription factor binding sites, and that the polymorphic sites at 3′UTR affect mRNA stability and the binding of specific microRNAs (85).
It has previously been demonstrated that 14-bp polymorphisms may be a genetic risk factor for susceptibility to several types of cancer (87,88,91). A study in Australia and New Zealand identified an association between heterozygote carriers of the HLA-G 14-bp ins/del polymorphism and decreased risk of neuroblastoma (88). Another study demonstrated that the 14-bp del allele may promote human papillomavirus infection and the 14-bp del/+3142C haplotype may be involved in invasive cervical cancer (ICC) development (91). In addition, in Brazilian patients who smoke, the polymorphic 14-bp ins/ins genotype and 14-bp ins/+3142 G haplotypes were associated with an increased risk of high-grade squamous intraepithelial lesion (HSIL) and a higher risk of developing ICC, while the 14-bp del/del genotype and 14-bp del/+3142G haplotypes were associated with a lower risk of HSIL and cervical cancer (86). By contrast, no significant differences in the +14/−14 bp polymorphism frequencies were observed between patients with PTC and the healthy control group. However, the association between 14-bp polymorphisms and cancer susceptibility is discrepant in distinct ethnic populations. The presence of the HLA-G 3′UTR 14-bp sequence was observed to be associated with a reduced risk of breast cancer susceptibility in HLA-G-expressing tissues in Southeastern Iranian (92) and Korean patients (43). However, the association between HLA-G 3′UTR 14-bp sequence and breast cancer susceptibility was not observed in Brazilian patients with breast cancer (93). In addition, the 14-bp del/del allele was revealed to increase hepatocellular carcinoma (HCC) susceptibility in Brazilian (94) and Chinese (87) patients, but the variation was not associated with HLA-G expression and susceptibility to HCC in Korean patients (95).
Other polymorphisms of HLA-G have also been investigated. In Canadian populations with cervical cancer, the homozygous genotype form of the HLA-G*01:01:02, -G*01:06 and -G*3′UTR 14-bp insertions were identified to be associated with a significantly increased risk for invasive cancer, compared with the wild-type heterozygous form of the HLA-G*01:01:01 allele (89). Evaluating the effect of HLA-G polymorphism occurrence on nasopharyngeal carcinoma (NPC) susceptibility in Tunisian patients, researchers observed that the lle110 allele was associated with fewer lymph node metastases and an increased number of patients with higher tumor stages, and the occurrence of codon 130C deletion reduced the disease-free and overall survival rates of patients with NPC (90). To date, and to the best of our knowledge, HLA-G polymorphisms have not been investigated in a number of tumor types, including lung cancer, gastric cancer, colorectal cancer, melanoma, renal cell carcinoma and glioblastoma.
Therefore, HLA-G polymorphisms may be risk factors and predictive markers for several types of cancer. However, the conflicting results regarding the association between HLA-G polymorphisms and cancer susceptibility indicate that additional studies consisting of populations from different ethnicities and larger sample sizes are required.
5. HLA-G is involved in cancer development
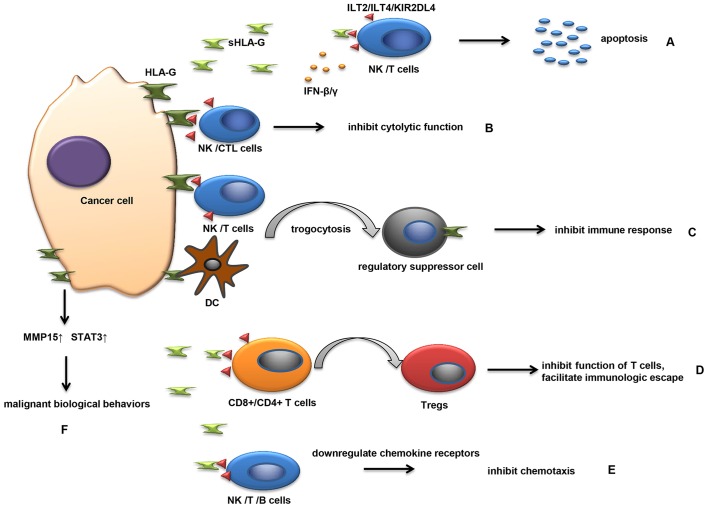
Since HLA-G expression was observed in various types of cancer, the roles of HLA-G in promoting cancer progression were investigated in a number of studies (17,96–98). Studies revealed that HLA-G and sHLA-G have multiple mechanisms of involvement in the development of malignancies (Fig. 1).
Figure 1.
HLA-G and sHLA-G ae involved in the development of malignancies in multiple ways. (A) sHLA-G released by cancer cells binds to the receptors on NK cells and T cells, leading to the apoptosis of immune cells. (B) The interaction between HLA-G on cancer cells and its receptors on NK/CTL cells directly inhibit the function of activated immune cells. (C) During cell-cell contact, cancer cells transfer HLA-G-containing membrane patches to activated NK/DC/T cells. NK/DC/T cells that receive HLA-G temporarily behave as regulatory suppressor cells and acquire the ability to inhibit immune responses. (D) In the presence of sHLA-G, CD4+ and CD8+ T cells lose their capability to respond to antigenic stimulation and differentiate into Tregs, which can inhibit T cell function and facilitate immunological escape. (E) sHLA-G can inhibit the chemokine receptors expressed on NK/T/B cells by interacting with ILT2 on cells. Losing the ability of chemotaxis, NK/T/B cells cannot migrate to pathological tissues and cannot regulate a series of immunological responses. (F) HLA-G may be involved in the invasiveness and metastasis of tumor progression by increasing the expression of MMPs and STAT3. HLA-G, human leukocyte antigen-G; sHLA-G, soluble HLA-G; NK, natural killer; CTL, cytotoxic T lymphocyte; DC, dendritic cell; MMP, matrix metalloproteinase; STAT3, signal transducer and activator of transcription 3l ILT2, immunoglobulin-like transcript 2; Tregs, regulatory T cells; Ifn, interferon.
Available evidence has demonstrated that HLA-G may be actively involved in the immune escape mechanism of tumor cells (17). Cancer immunoediting is an important host protection process (97). In this process, the immune surveillance can be divided into three essential steps, including an elimination phase, equilibrium phase and escape phase (97), and HLA-G is involved in each of these three phases (2). Several adaptive/innate immunizing molecules and cells are involved in inhibiting the elimination of tumor cells (98). As mentioned earlier, HLA-G could bind to its special receptors on immune effector cells, thereby blocking the proliferation and lytic function of uterine and peripheral NK cells in a physiological context (4). Similarly, sHLA-G released by cancer cells can bind to the receptors on NK cells and T cells, leading to the apoptosis of immune cells (Fig. 1A). HLA-G expression in tumors such as hepatocellular carcinoma, glioma, melanoma, renal, ovarian and lung carcinoma can also protect cancer cells from NK and CTL-mediated destruction (99,100) (Fig. 1B). In addition, plasmatic sHLA-G molecules secreted by melanoma M8 cells functionally and potently inhibit NK cell cytotoxicity by weakening the lytic granules polarization toward the target cells (101). The formation of HLA-G and its soluble counterpart, HLA-G5, can be increased by numerous pro-inflammatory cytokines from the tumor microenvironment, including interferon (IFN)-β and IFN-γ, which enhance the protection of tumor cells from NK cell-mediated cytolysis (62). HLA-G can affect the equilibrium phase by allowing cancer cell persistence, resulting in the selection of tumor cells with reduced immunogenicity (102). Tumor development primarily occurs in the evasion phase (103); in this phase, tumor cells tend to express only HLA-G on the cell surface, and not molecules essential to immune recognition, leading to the rapid growth of tumor cells and the creation of a hypoxic microenvironment. Furthermore, the hypoxic microenvironment and cytokines derived by tumor-like transforming growth factor-β and IL-10 in this phase can upregulate HLA-G expression (104). Estrogenic G-protein-coupled estrogen receptor-1 signaling can trigger HLA-G expression by inhibiting miR148a in breast cancer cells (105). These mechanisms modulated by HLA-G are considered to facilitate the escape of tumor cells from the antigen-specific immune response and to create a microenvironment suitable for tumor cells (98).
Notably, HLA-G can be transferred from one HLA-G-expressing cell to another, a phenomenon defined as trogocytosis (106) (Fig. 1C). In this manner, cancer cells transfer HLA-G-containing membrane patches to activated NK cells (106). NK cells receiving the HLA-G temporarily behave as regulatory suppressor cells, and acquire the ability to inhibit immune responses such as prohibiting the proliferation of immune cells and inhibiting the cytotoxic effector of neighboring NK cells (106,107). T cells and DCs may also possess regulatory properties subsequent to acquiring HLA-G antigens from malignant plasma cells, providing another novel mechanism for escaping effective immune surveillance (108). Similarly, the HLA-G-negative tumor cells in the vicinity of HLA-G-positive cells can be protected in this way (1). Therefore, this phenomenon may be an important mechanism underlying immune inhibition in physical conditions as well as in pathological conditions.
During tumor development, immune cells are able to infiltrate tumors and participate in tumor formation and progression (22,98). Tregs are one type of tumor-infiltrating lymphocyte, which serve an important role in immunologic escape of tumor cells. High tumor-infiltrating Tregs are associated with the poor prognosis of human malignant tumors (98). Tregs can be induced by HLA-G not only under physiological conditions but also pathological conditions (22). Several studies have elucidated the association between HLA-G and Tregs in malignant diseases (38,60,61). It has been observed that the proportion of CD4+CD25+FoxP3+ Tregs was markedly increased in the plasma of breast cancer patients when compared with that in the plasma of healthy controls, and the increase was strongly associated with sHLA-G levels (38). In gastric cancer, a significant positive association between HLA-G expression and the presence of tumor-infiltrating Tregs was observed in tumor tissues (60). When gastric cancer cells were co-cultured with human peripheral blood mononuclear cells in vitro, HLA-G overexpression in gastric cancer cells significantly enhanced the number of Tregs (60). In addition, a negative correlation between HLA-G expression and the number of CD8+ T lymphocytes was observed in gastric tumor tissues using immunohistochemistry (61). This may be attributed to CD8+ T lymphocyte differentiation into Tregs, induced by HLA-G (Fig. 1D). Taken together, these results indicate that HLA-G may be associated with tumor progression and may be involved in tumor evasion by inducing the production of Tregs.
Another mechanism by which sHLA-G promotes cancer development is to inhibit the chemokine receptors expressed on NK/T/B cells (Fig. 1E), which can regulate the migration and recruitment of these cells by binding with chemotactic cytokines (109). Several studies have demonstrated that sHLA-G reduces the expression of CCR2/CXCR3/CXCR5 on T cells, downregulates CCR2/CXCR3/CX3CR1/CXCR5 expression on NK cells and inhibits CXCR4/CXCR5 expression on B cells by interacting with ILT2 (109–111). Following the loss of chemotaxic ability, NK/T/B cells cannot migrate to pathological tissues and consequently cannot regulate a series of immunological responses (109).
Furthermore, a previous study (96) determined that HLA-G may be involved in the invasion and metastasis stages of tumor progression (Fig. 1F). In ovarian carcinoma, HLA-G expression is closely associated with matrix metalloproteinase-15 (MMP-15) expression (100). Knockdown of MMP-15 expression significantly decreases the migration potential and tumor metastasis of HO-8910 ovarian serous cystadenocarcinoma cells (100). In JEG-3 gestational choriocarcinoma cells, downregulating HLA-G expression notably suppressed the activation of STAT3 and the invasion capacity of cancer cells (112). These data indicate that HLA-G may regulate the malignant biological behavior of cancer cells by affecting STAT3 activation and MMP-15 expression.
In addition, in vivo evidence of the immunosuppression function of HLA-G in tumors was provided by a number of studies. HLA-G may interact with the murine-paired immunoglobulin-like receptor-B, ortholog of human ILT receptors, enabling the role to be investigated in vivo (113). Agaugué et al (114) first established a HLA-G+ xenotumor mouse model by subcutaneously injecting M8-HLA-G1 tumor cells into immunocompetent mice. This demonstrated that HLA-G serves a crucial role in immune evasion and promotes tumor expansion in vivo by depleting peripheral T cells and increasing blood myeloid-derived CD11b(+) Gr1(+) PIR-B(+) suppressor cells (114). In another study, researchers injected syngeneic hβ2m+ HLA-G5+ tumor cells (tumor cells co-expressing HLA-G5 and human β2-microglubulin) or hβ2m+ HLA-G5− tumor cells into immunocompetent mice (115). The results indicated that secreted HLA-G5 protected hβ2m+ HLA-G5+ tumor cells against immune rejection elicited by hβ2 m, thereby permitting the immunogenic tumors to grow in a similar manner to poorly immunogenic tumors (115). These data highlight the crucial role of HLA-G in tumor immune surveillance and malignant disease progression.
6. Role of HLA-G in the diagnosis of cancer
As aforementioned, HLA-G expression levels in tumor tissue samples and high levels of sHLA-G in plasma samples, all obtained from patients with various types of cancer, have previously been detected, and high expression was determined to be significantly associated with high histological grade, lymph node metastasis, advanced clinical stage and a poor prognosis (96). Therefore, the application of HLA-G as a diagnostic and prognostic biomarker of cancer has been proposed.
Studies have demonstrated that HLA-G expression was higher in malignant lesions compared with that in benign hyperplasias (73,75). In thyroid tissues, the percentage of cell staining for HLA-G antigen in PTC, follicular thyroid carcinomas and follicular adenomas (FA) was significantly higher than in colloid goiter and histologically normal thyroid glands (75). In cervical cancer lesions, HLA-G expression was increased in patients with invasive cervical cancer compared with that in patients with CIN III, and HLA-G expression was more frequently observed in cancer lesions from patients with a higher FIGO stage of cancer (73). In liver tissues, HLA-G expression was identified in the primary sites of HCC, but not detected in benign lesions represented by liver cirrhosis (LC) (52). ELISA assay also showed that the plasma sHLA-G level in patients with HCC was higher than in LC (52). These results indicated that HLA-G and sHLA-G may be involved in tumorigenesis and tumor development, which provides the basis for their purpose as indicators of early diagnosis.
HLA-G expression may also be a prognostic predictor of carcinoma following curative resection (50). For instance, high expression levels of HLA-G in hepatocellular carcinoma are independently associated with the shortening of overall survival times and an increase in tumor recurrence (50). In addition, patients with high HLA-G levels and a high Tregs:CD8+ ratio exhibited ≥3 times increased risk of tumor relapse and mortality, compared with those without (50). Therefore, the combination of HLA-G expression and the Tregs:CD8+ ratio served as an improved prognosticator (50). In colorectal cancer, patients with HLA-G expression in tissue have a significantly shorter survival time compared with those patients with HLA-G negative, indicating that HLA-G may be an independent prognostic factor for colorectal cancer (55).
In addition, HLA-G expression in tissues and sHLA-G concentrations in body fluids were useful for the prediction and diagnosis of cancer patients with various subtypes (44,116). When sHLA-G plasma level was detected in 120 patients with breast cancer, Provatopoulou et al (44) found that sHLA-G levels were closely associated with histological type: sHLA-G expression in patients with mixed type co-existing ductal and lobular breast lesions was significantly higher than patients with pure ductal carcinoma or pure lobular neoplasia. Furthermore, the expression of HLA-G was significantly higher in non-luminal subtypes of invasive ductal breast carcinoma compared with in luminal subtypes (116).
Therefore, HLA-G/sHLA-G could be used as biomarkers to diagnose cancer in the early stages, to predict the prognosis of cancer patients and be used as subsidiary indicators to distinguish various cancer subtypes of cancer. Additionally, as aforementioned, HLA-G polymorphisms may be useful in the diagnosis of cancer.
7. HLA-G as a potential therapeutic target in cancer
In accordance with the important role of HLA-G in promoting tumor evolution and progression, targeting HLA-G has been deemed to be a novel innovative therapeutic strategy in cancer (99,114). In human HCC cell lines, when HLA-G expression is diminished by applying the vectors containing small interfering RNA specifically targeting the HLA-G gene, a significant increase in NK cell-mediated lysis occurs, which prevents tumor progression (99). In xenotumor mouse models, blocking HLA-G using a specific antibody successfully inhibits the development of the tumor (114). Additional studies and clinical trials are required to demonstrate the value of HLA-G in targeted cancer therapy.
However, a noteworthy phenomenon to consider is that several therapeutics may induce HLA-G-negative tumors to express HLA-G, and thus contribute to cancer recurrence (34,81). For example, a multicentric study has demonstrated that high expression levels of HLA-G in glioblastoma may be induced by combined 5-aza-2′-deoxycytidine and interferon-γ treatments in vitro (81). Melanoma patients undergoing INF-α immunotherapy exhibited significantly enhanced increases in the serum sHLA-G level (34). Furthermore, it was demonstrated that HLA-G1 expression may modulate the radiosensitivity of human tumoral cell lines: HLA-G1 expressing cells had a higher radiosensitivity in human melanoma M8 and human erythroleukemia K562 cell lines (117). Thus, identification of HLA-G status may be conducive to improved selection of cancer patients who could benefit from more tailored immunological therapy or neoadjuvant biological therapy.
8. Conclusion
In conclusion, HLA-G is a potent immune-inhibitory molecule in healthy individuals and in pathological organisms. Although the frequency of HLA-G/sHLA-G expression and its association with clinical parameters varies between different cancer types, and even between different studies of the same tumor type, HLA-G expression in tumors has been considered to be detrimental. However, studies with a larger number of populations from different ethnicities are required.
Considering the ectopic expression of HLA-G and its gene polymorphisms in tumors, it is promising that membrane-bound and sHLA-G could be a potential diagnostic biomarker to identify tumors and to monitor disease stage. Since HLA-G has been demonstrated to be an important molecule in tumor immune escape and cancer development, blockade of HLA-G expression or elimination of HLA-G-expressing cancer cells may be important to the efficacy of anticancer therapies. Thus far, several molecular inhibitors have demonstrated their ability to specifically target the HLA-G gene; however, additional studies involving higher animals and clinical trials involving humans are required in order for these inhibitors targeting HLA-G to be used clinically.
Acknowledgements
The present study was financially supported by the National Natural Science Foundation of China (grant no. 81372334).
References
- 1.Carosella ED, Favier B, Rouas-Freiss N, Moreau P, Lemaoult J. Beyond the increasing complexity of the immunomodulatory HLA-G molecule. Blood. 2008;111:4862–4870. doi: 10.1182/blood-2007-12-127662. [DOI] [PubMed] [Google Scholar]
- 2.Amiot L, Ferrone S, Grosse-Wilde H, Seliger B. Biology of HLA-G in cancer: A candidate molecule for therapeutic intervention? Cell Mol Life Sci. 2011;68:417–431. doi: 10.1007/s00018-010-0583-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jiang F, Zhao H, Wang L, Guo X, Wang X, Yin G, Hu Y, Li Y, Yao Y. Role of HLA-G1 in trophoblast cell proliferation, adhesion and invasion. Biochem Biophys Res Commun. 2015;458:154–160. doi: 10.1016/j.bbrc.2015.01.085. [DOI] [PubMed] [Google Scholar]
- 4.Rouas-Freiss N, Kirszenbaum M, Dausset J, Carosella ED. Fetomaternal tolerance: Role of HLA-G molecule in the protection of the fetus against maternal natural killer activity. C R Acad Sci III. 1997;320:385–392. doi: 10.1016/S0764-4469(97)85026-3. (In French) [DOI] [PubMed] [Google Scholar]
- 5.Paul P, Rouas-Freiss N, Khalil-Daher I, Moreau P, Riteau B, Le Gal FA, Avril MF, Dausset J, Guillet JG, Carosella ED. HLA-G expression in melanoma: A way for tumor cells to escape from immunosurveillance; Proc Natl Acad Sci USA; 1998; pp. 4510–4515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Castelli EC, Mendes-Junior CT, Veiga-Castelli LC, Roger M, Moreau P, Donadi EA. A comprehensive study of polymorphic sites along the HLA-G gene: Implication for gene regulation and evolution. Mol Biol Evol. 2011;28:3069–3086. doi: 10.1093/molbev/msr138. [DOI] [PubMed] [Google Scholar]
- 7.Rousseau P, Le Discorde M, Mouillot G, Marcou C, Carosella ED, Moreau P. The 14 bp deletion-insertion polymorphism in the 3′ UT region of the HLA-G gene influences HLA-G mRNA stability. Hum Immunol. 2003;64:1005–1010. doi: 10.1016/j.humimm.2003.08.347. [DOI] [PubMed] [Google Scholar]
- 8.Castelli EC, Mendes-Junior CT, Deghaide NH, de Albuquerque RS, Muniz YC, Simões RT, Carosella ED, Moreau P, Donadi EA. The genetic structure of 3′untranslated region of the HLA-G gene: Polymorphisms and haplotypes. Genes Immun. 2010;11:134–141. doi: 10.1038/gene.2009.74. [DOI] [PubMed] [Google Scholar]
- 9.Hylenius S, Andersen AM, Melbye M, Hviid TV. Association between HLA-G genotype and risk of pre-eclampsia: A case-control study using family triads. Mol Hum Reprod. 2004;10:237–246. doi: 10.1093/molehr/gah035. [DOI] [PubMed] [Google Scholar]
- 10.Pandey MK, Rani R, Agrawal S. An update in recurrent spontaneous abortion. Arch Gynecol Obstet. 2005;272:95–108. doi: 10.1007/s00404-004-0706-y. [DOI] [PubMed] [Google Scholar]
- 11.Tahan F, Patiroglu T. Plasma soluble human leukocyte antigen G levels in asthmatic children. Int Arch Allergy Immunol. 2006;141:213–216. doi: 10.1159/000095290. [DOI] [PubMed] [Google Scholar]
- 12.Consiglio CR, Veit TD, Monticielo OA, Mucenic T, Xavier RM, Brenol JC, Chies JA. Association of the HLA-G gene +3142C>G polymorphism with systemic lupus erythematosus. Tissue Antigens. 2011;77:540–545. doi: 10.1111/j.1399-0039.2011.01635.x. [DOI] [PubMed] [Google Scholar]
- 13.Gazit E, Slomov Y, Goldberg I, Brenner S, Loewenthal R. HLA-G is associated with pemphigus vulgaris in Jewish patients. Hum Immunol. 2004;65:39–46. doi: 10.1016/j.humimm.2003.09.019. [DOI] [PubMed] [Google Scholar]
- 14.Dias FC, Castelli EC, Collares CV, Moreau P, Donadi EA. The Role of HLA-G molecule and HLA-G gene polymorphisms in tumors, viral hepatitis, and parasitic diseases. Front Immunol. 2015;6:9. doi: 10.3389/fimmu.2015.00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Koller BH, Geraghty DE, DeMars R, Duvick L, Rich SS, Orr HT. Chromosomal organization of the human major histocompatibility complex class I gene family. J Exp Med. 1989;169:469–480. doi: 10.1084/jem.169.2.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morandi F, Pistoia V. Interactions between HLA-G and HLA-E in Physiological and Pathological Conditions. Front Immunol. 2014;5:394. doi: 10.3389/fimmu.2014.00394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carosella ED, Rouas-Freiss N, Tronik-Le Roux D, Moreau P, LeMaoult J. HLA-G: An immune checkpoint molecule. Adv Immunol. 2015;127:33–1444. doi: 10.1016/bs.ai.2015.04.001. [DOI] [PubMed] [Google Scholar]
- 18.Carosella ED, Moreau P, Le Maoult J, Le Discorde M, Dausset J, Rouas-Freiss N. HLA-G molecules: From maternal-fetal tolerance to tissue acceptance. Adv Immunol. 2003;81:199–252. doi: 10.1016/S0065-2776(03)81006-4. [DOI] [PubMed] [Google Scholar]
- 19.Fujii T, Ishitani A, Geraghty DE. A soluble form of the HLA-G antigen is encoded by a messenger ribonucleic acid containing intron 4. J Immunol. 1994;153:5516–5524. [PubMed] [Google Scholar]
- 20.Park GM, Lee S, Park B, Kim E, Shin J, Cho K, Ahn K. Soluble HLA-G generated by proteolytic shedding inhibits NK-mediated cell lysis. Biochem Biophys Res Commun. 2004;313:606–611. doi: 10.1016/j.bbrc.2003.11.153. [DOI] [PubMed] [Google Scholar]
- 21.Ishitani A, Geraghty DE. Alternative splicing of HLA-G transcripts yields proteins with primary structures resembling both class I and class II antigens; Proc Natl Acad Sci USA; 1992; pp. 3947–3951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Curigliano G, Criscitiello C, Gelao L, Goldhirsch A. Molecular pathways: Human leukocyte antigen G (HLA-G) Clin Cancer Res. 2013;19:5564–5571. doi: 10.1158/1078-0432.CCR-12-3697. [DOI] [PubMed] [Google Scholar]
- 23.Gao GF, Willcox BE, Wyer JR, Boulter JM, O'Callaghan CA, Maenaka K, Stuart DI, Jones EY, van der Merwe PA, Bell JI, Jakobsen BK. Classical and nonclassical class I major histocompatibility complex molecules exhibit subtle conformational differences that affect binding to CD8alphaalpha. J Biol Chem. 2000;275:15232–15238. doi: 10.1074/jbc.275.20.15232. [DOI] [PubMed] [Google Scholar]
- 24.Colonna M, Samaridis J, Cella M, Angman L, Allen RL, O'Callaghan CA, Dunbar R, Ogg GS, Cerundolo V, Rolink A. Human myelomonocytic cells express an inhibitory receptor for classical and nonclassical MHC class I molecules. J Immunol. 1998;160:3096–3100. [PubMed] [Google Scholar]
- 25.Borges L, Cosman D. LIRs/ILTs/MIRs, inhibitory and stimulatory Ig-superfamily receptors expressed in myeloid and lymphoid cells. Cytokine Growth Factor Rev. 2000;11:209–217. doi: 10.1016/S1359-6101(00)00007-1. [DOI] [PubMed] [Google Scholar]
- 26.Yan WH, Fan LA. Residues Met76 and Gln79 in HLA-G alpha1 domain involve in KIR2DL4 recognition. Cell Res. 2005;15:176–182. doi: 10.1038/sj.cr.7290283. [DOI] [PubMed] [Google Scholar]
- 27.González A, Rebmann V, LeMaoult J, Horn PA, Carosella ED, Alegre E. The immunosuppressive molecule HLA-G and its clinical implications. Crit Rev Clin Lab Sci. 2012;49:63–84. doi: 10.3109/10408363.2012.677947. [DOI] [PubMed] [Google Scholar]
- 28.Liang S, Ristich V, Arase H, Dausset J, Carosella ED, Horuzsko A. Modulation of dendritic cell differentiation by HLA-G and ILT4 requires the IL-6-STAT3 signaling pathway; Proc Natl Acad Sci USA; 2008; pp. 8357–8362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ketroussi F, Giuliani M, Bahri R, Azzarone B, Charpentier B, Durrbach A. Lymphocyte cell-cycle inhibition by HLA-G is mediated by phosphatase SHP-2 and acts on the mTOR pathway. PLoS One. 2011;6:e22776. doi: 10.1371/journal.pone.0022776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.LeMaoult J, Zafaranloo K, Le Danff C, Carosella ED. HLA-G up-regulates ILT2, ILT3, ILT4, and KIR2DL4 in antigen presenting cells, NK, cells and T cells. FASEB J. 2005;19:662–664. doi: 10.1096/fj.04-1617fje. [DOI] [PubMed] [Google Scholar]
- 31.Gooden MJ, van Hall T. Infiltrating CTLs are bothered by HLA-E on tumors. Oncoimmunology. 2012;1:92–93. doi: 10.4161/onci.1.1.17961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.LeMaoult J, Krawice-Radanne I, Dausset J, Carosella ED. HLA-G1-expressing antigen-presenting cells induce immunosuppressive CD4+ T cells; Proc Natl Acad Sci USA; 2004; pp. 7064–7069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ibrahim EC, Aractingi S, Allory Y, Borrini F, Dupuy A, Duvillard P, Carosella ED, Avril MF, Paul P. Analysis of HLA antigen expression in benign and malignant melanocytic lesions reveals that upregulation of HLA-G expression correlates with malignant transformation, high inflammatory infiltration and HLA-A1 genotype. Int J Cancer. 2004;108:243–250. doi: 10.1002/ijc.11456. [DOI] [PubMed] [Google Scholar]
- 34.Ugurel S, Rebmann V, Ferrone S, Tilgen W, Grosse-Wilde H, Reinhold U. Soluble human leukocyte antigen-G serum level is elevated in melanoma patients and is further increased by interferon-alpha immunotherapy. Cancer. 2001;92:369–376. doi: 10.1002/1097-0142(20010715)92:2<369::AID-CNCR1332>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 35.da Silva GB, Silva TG, Duarte RA, Neto NL, Carrara HH, Donadi EA, Gonçalves MA, Soares EG, Soares CP. Expression of the Classical and Nonclassical HLA molecules in breast cancer. Int J Breast Cancer. 2013;2013:250435. doi: 10.1155/2013/250435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Elliott RL, Jiang XP, Phillips JT, Barnett BG, Head JF. Human leukocyte antigen G expression in breast cancer: Role in immunosuppression. Cancer Biother Radiopharm. 2011;26:153–157. doi: 10.1089/cbr.2010.0924. [DOI] [PubMed] [Google Scholar]
- 37.Lefebvre S, Antoine M, Uzan S, McMaster M, Dausset J, Carosella ED, Paul P. Specific activation of the non-classical class I histocompatibility HLA-G antigen and expression of the ILT2 inhibitory receptor in human breast cancer. J Pathol. 2002;196:266–274. doi: 10.1002/path.1039. [DOI] [PubMed] [Google Scholar]
- 38.Chen HX, Lin A, Shen CJ, Zhen R, Chen BG, Zhang X, Cao FL, Zhang JG, Yan WH. Upregulation of human leukocyte antigen-G expression and its clinical significance in ductal breast cancer. Hum Immunol. 2010;71:892–898. doi: 10.1016/j.humimm.2010.06.009. [DOI] [PubMed] [Google Scholar]
- 39.He X, Dong DD, Yie SM, Yang H, Cao M, Ye SR, Li K, Liu J, Chen J. HLA-G expression in human breast cancer: Implications for diagnosis and prognosis, and effect on allocytotoxic lymphocyte response after hormone treatment in vitro. Ann Surg Oncol. 2010;17:1459–1469. doi: 10.1245/s10434-009-0891-9. [DOI] [PubMed] [Google Scholar]
- 40.de Kruijf EM, Sajet A, van Nes JG, Natanov R, Putter H, Smit VT, Liefers GJ, van den Elsen PJ, van de Velde CJ, Kuppen PJ. HLA-E and HLA-G expression in classical HLA class I-negative tumors is of prognostic value for clinical outcome of early breast cancer patients. J Immunol. 2010;185:7452–7459. doi: 10.4049/jimmunol.1002629. [DOI] [PubMed] [Google Scholar]
- 41.Ramos CS, Gonçalves AS, Marinho LC, Gomes Avelino MA, Saddi VA, Lopes AC, Simões RT, Wastowski IJ. Analysis of HLA-G gene polymorphism and protein expression in invasive breast ductal carcinoma. Hum Immunol. 2014;75:667–672. doi: 10.1016/j.humimm.2014.04.005. [DOI] [PubMed] [Google Scholar]
- 42.Sayed D, Badr G, Maximous D, Mikhail NN, Abu-Tarboush F, Alhazza IM. HLA-G and its relation to proliferation index in detection and monitoring breast cancer patients. Tissue Antigens. 2010;75:40–47. doi: 10.1111/j.1399-0039.2009.01393.x. [DOI] [PubMed] [Google Scholar]
- 43.Jeong S, Park S, Park BW, Park Y, Kwon OJ, Kim HS. Human leukocyte antigen-G (HLA-G) polymorphism and expression in breast cancer patients. PLoS One. 2014;9:e98284. doi: 10.1371/journal.pone.0098284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Provatopoulou X, Kalogera E, Sagkriotis A, Zagouri F, Nonni A, Zografos GC, Gounaris A. Soluble human leukocyte antigen-G expression in patients with ductal and lobular breast malignancy. Anticancer Res. 2012;32:1021–1026. [PubMed] [Google Scholar]
- 45.Urosevic M, Kurrer MO, Kamarashev J, Mueller B, Weder W, Burg G, Stahel RA, Dummer R, Trojan A. Human leukocyte antigen G up-regulation in lung cancer associates with high-grade histology, human leukocyte antigen class I loss and interleukin-10 production. Am J Pathol. 2001;159:817–824. doi: 10.1016/S0002-9440(10)61756-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Yie SM, Yang H, Ye SR, Li K, Dong DD, Lin XM. Expression of human leucocyte antigen G (HLA-G) is associated with prognosis in non-small cell lung cancer. Lung Cancer. 2007;58:267–274. doi: 10.1016/j.lungcan.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 47.Lin A, Zhu CC, Chen HX, Chen BF, Zhang X, Zhang JG, Wang Q, Zhou WJ, Hu W, Yang HH, et al. Clinical relevance and functional implications for human leucocyte antigen-g expression in non-small-cell lung cancer. J Cell Mol Med. 2010;14:2318–2329. doi: 10.1111/j.1582-4934.2009.00858.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Schütt P, Schütt B, Switala M, Bauer S, Stamatis G, Opalka B, Eberhardt W, Schuler M, Horn PA, Rebmann V. Prognostic relevance of soluble human leukocyte antigen-G and total human leukocyte antigen class I molecules in lung cancer patients. Hum Immunol. 2010;71:489–495. doi: 10.1016/j.humimm.2010.02.015. [DOI] [PubMed] [Google Scholar]
- 49.Cao M, Yie SM, Liu J, Ye SR, Xia D, Gao E. Plasma soluble HLA-G is a potential biomarker for diagnosis of colorectal, gastric, esophageal and lung cancer. Tissue Antigens. 2011;78:120–128. doi: 10.1111/j.1399-0039.2011.01716.x. [DOI] [PubMed] [Google Scholar]
- 50.Cai MY, Xu YF, Qiu SJ, Ju MJ, Gao Q, Li YW, Zhang BH, Zhou J, Fan J. Human leukocyte antigen-G protein expression is an unfavorable prognostic predictor of hepatocellular carcinoma following curative resection. Clin Cancer Res. 2009;15:4686–4693. doi: 10.1158/1078-0432.CCR-09-0463. [DOI] [PubMed] [Google Scholar]
- 51.Lin A, Chen HX, Zhu CC, Zhang X, Xu HH, Zhang JG, Wang Q, Zhou WJ, Yan WH. Aberrant human leucocyte antigen-G expression and its clinical relevance in hepatocellular carcinoma. J Cell Mol Med. 2010;14:2162–2171. doi: 10.1111/j.1582-4934.2009.00917.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang Y, Ye Z, Meng XQ, Zheng SS. Expression of HLA-G in patients with hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int. 2011;10:158–163. doi: 10.1016/S1499-3872(11)60025-8. [DOI] [PubMed] [Google Scholar]
- 53.Park Y, Park Y, Lim HS, Kim YS, Hong DJ, Kim HS. Soluble human leukocyte antigen-G expression in hepatitis B virus infection and hepatocellular carcinoma. Tissue Antigens. 2012;79:97–103. doi: 10.1111/j.1399-0039.2011.01814.x. [DOI] [PubMed] [Google Scholar]
- 54.Fukushima Y, Oshika Y, Nakamura M, Tokunaga T, Hatanaka H, Abe Y, Yamazaki H, Kijima H, Ueyama Y, Tamaoki N. Increased expression of human histocompatibility leukocyte antigen-G in colorectal cancer cells. Int J Mol Med. 1998;2:349–351. doi: 10.3892/ijmm.2.3.349. [DOI] [PubMed] [Google Scholar]
- 55.Ye SR, Yang H, Li K, Dong DD, Lin XM, Yie SM. Human leukocyte antigen G expression: As a significant prognostic indicator for patients with colorectal cancer. Mod Pathol. 2007;20:375–383. doi: 10.1038/modpathol.3800751. [DOI] [PubMed] [Google Scholar]
- 56.Zeestraten EC, Reimers MS, Saadatmand S, Goossens-Beumer IJ, Dekker JW, Liefers GJ, van den Elsen PJ, van de Velde CJ, Kuppen PJ. Combined analysis of HLA class I, HLA-E and HLA-G predicts prognosis in colon cancer patients. Br J Cancer. 2014;110:459–468. doi: 10.1038/bjc.2013.696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Guo ZY, Lv YG, Wang L, Shi SJ, Yang F, Zheng GX, Wen WH, Yang AG. Predictive value of HLA-G and HLA-E in the prognosis of colorectal cancer patients. Cell Immunol. 2015;293:10–16. doi: 10.1016/j.cellimm.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 58.Zhu CB, Wang CX, Zhang X, Zhang J, Li W. Serum sHLA-G levels: A useful indicator in distinguishing colorectal cancer from benign colorectal diseases. Int J Cancer. 2011;128:617–622. doi: 10.1002/ijc.25372. [DOI] [PubMed] [Google Scholar]
- 59.Yie SM, Yang H, Ye SR, Li K, Dong DD, Lin XM. Expression of human leukocyte antigen G (HLA-G) correlates with poor prognosis in gastric carcinoma. Ann Surg Oncol. 2007;14:2721–2729. doi: 10.1245/s10434-007-9464-y. [DOI] [PubMed] [Google Scholar]
- 60.Du L, Xiao X, Wang C, Zhang X, Zheng N, Wang L, Zhang X, Li W, Wang S, Dong Z. Human leukocyte antigen-G is closely associated with tumor immune escape in gastric cancer by increasing local regulatory T cells. Cancer Sci. 2011;102:1272–1280. doi: 10.1111/j.1349-7006.2011.01951.x. [DOI] [PubMed] [Google Scholar]
- 61.Tuncel T, Karagoz B, Haholu A, Ozgun A, Emirzeoglu L, Bilgi O, Kandemir EG. Immunoregulatory function of HLA-G in gastric cancer. Asian Pac J Cancer Prev. 2013;14:7681–7684. doi: 10.7314/APJCP.2013.14.12.7681. [DOI] [PubMed] [Google Scholar]
- 62.Yie SM, Yang H, Ye SR, Li K, Dong DD, Lin XM. Expression of HLA-G is associated with prognosis in esophageal squamous cell carcinoma. Am J Clin Pathol. 2007;128:1002–1009. doi: 10.1309/JNCW1QLDFB6AM9WE. [DOI] [PubMed] [Google Scholar]
- 63.Lin A, Zhang X, Zhou WJ, Ruan YY, Xu DP, Wang Q, Yan WH. Human leukocyte antigen-G expression is associated with a poor prognosis in patients with esophageal squamous cell carcinoma. Int J Cancer. 2011;129:1382–1390. doi: 10.1002/ijc.25807. [DOI] [PubMed] [Google Scholar]
- 64.Hu J, Li L, Liu Y, Chen Y, Liu C, Liang W, Zhao J, Zou H, Cui X, Qi Y, et al. Overexpression of HLA-G Is positively associated with Kazakh esophageal squamous cell carcinoma in Xinjiang, China. Viral Immunol. 2013;26:180–184. doi: 10.1089/vim.2012.0085. [DOI] [PubMed] [Google Scholar]
- 65.Zheng J, Xu C, Chu D, Zhang X, Li J, Ji G, Hong L, Feng Q, Li X, Wu G, et al. Human leukocyte antigen G is associated with esophageal squamous cell carcinoma progression and poor prognosis. Immunol Lett. 2014;161:13–19. doi: 10.1016/j.imlet.2014.04.007. [DOI] [PubMed] [Google Scholar]
- 66.Cai MB, Han HQ, Bei JX, Liu CC, Lei JJ, Cui Q, Feng QS, Wang HY, Zhang JX, Liang Y, et al. Expression of human leukocyte antigen G is associated with prognosis in nasopharyngeal carcinoma. Int J Biol Sci. 2012;8:891–900. doi: 10.7150/ijbs.4383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Silva TG, Crispim JC, Miranda FA, Hassumi MK, de Mello JM, Simões RT, Souto F, Soares EG, Donadi EA, Soares CP. Expression of the nonclassical HLA-G and HLA-E molecules in laryngeal lesions as biomarkers of tumor invasiveness. Histol Histopathol. 2011;26:1487–1497. doi: 10.14670/HH-26.1487. [DOI] [PubMed] [Google Scholar]
- 68.Gan LH, Huang LF, Zhang X, Lin A, Xu DP, Wang Q, Wang TJ, Yan WH. Tumor-specific upregulation of human leukocyte antigen-G expression in bladder transitional cell carcinoma. Hum Immunol. 2010;71:899–904. doi: 10.1016/j.humimm.2010.06.012. [DOI] [PubMed] [Google Scholar]
- 69.Ibrahim EC, Guerra N, Lacombe MJ, Angevin E, Chouaib S, Carosella ED, Caignard A, Paul P. Tumor-specific up-regulation of the nonclassical class I HLA-G antigen expression in renal carcinoma. Cancer Res. 2001;61:6838–6845. [PubMed] [Google Scholar]
- 70.Kren L, Valkovsky I, Dolezel J, Capak I, Pacik D, Poprach A, Lakomy R, Redova M, Fabian P, Krenova Z, Slaby O. HLA-G and HLA-E specific mRNAs connote opposite prognostic significance in renal cell carcinoma. Diagn Pathol. 2012;7:58. doi: 10.1186/1746-1596-7-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ibrahim EC, Allory Y, Commo F, Gattegno B, Callard P, Paul P. Altered pattern of major histocompatibility complex expression in renal carcinoma: Tumor-specific expression of the nonclassical human leukocyte antigen-G molecule is restricted to clear cell carcinoma while up-regulation of other major histocompatibility complex antigens is primarily distributed in all subtypes of renal carcinoma. Am J Pathol. 2003;162:501–508. doi: 10.1016/S0002-9440(10)63844-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Li BL, Lin A, Zhang XJ, Zhang X, Zhang JG, Wang Q, Zhou WJ, Chen HX, Wang TJ, Yan WH. Characterization of HLA-G expression in renal cell carcinoma. Tissue Antigens. 2009;74:213–221. doi: 10.1111/j.1399-0039.2009.01302.x. [DOI] [PubMed] [Google Scholar]
- 73.Li XJ, Zhang X, Lin A, Ruan YY, Yan WH. Human leukocyte antigen-G (HLA-G) expression in cervical cancer lesions is associated with disease progression. Hum Immunol. 2012;73:946–949. doi: 10.1016/j.humimm.2012.07.041. [DOI] [PubMed] [Google Scholar]
- 74.Nunes LM, Ayres FM, Francescantonio IC, Saddi VA, Avelino MA, Alencar Rde C, Silva RC, Meneghini AJ, Wastowski IJ. Association between the HLA-G molecule and lymph node metastasis in papillary thyroid cancer. Hum Immunol. 2013;74:447–451. doi: 10.1016/j.humimm.2012.12.012. [DOI] [PubMed] [Google Scholar]
- 75.de Figueiredo Feitosa NL, Crispim JC, Zanetti BR, Magalhães PK, Soares CP, Soares EG, Neder L, Donadi EA, Maciel LM. HLA-G is differentially expressed in thyroid tissues. Thyroid. 2014;24:585–592. doi: 10.1089/thy.2013.0246. [DOI] [PubMed] [Google Scholar]
- 76.Morandi F, Levreri I, Bocca P, Galleni B, Raffaghello L, Ferrone S, Prigione I, Pistoia V. Human neuroblastoma cells trigger an immunosuppressive program in monocytes by stimulating soluble HLA-G release. Cancer Res. 2007;67:6433–6441. doi: 10.1158/0008-5472.CAN-06-4588. [DOI] [PubMed] [Google Scholar]
- 77.Morandi F, Scaruffi P, Gallo F, Stigliani S, Moretti S, Bonassi S, Gambini C, Mazzocco K, Fardin P, Haupt R, et al. Bone marrow-infiltrating human neuroblastoma cells express high levels of calprotectin and HLA-G proteins. PLoS One. 2012;7:e29922. doi: 10.1371/journal.pone.0029922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wiendl H, Mitsdoerffer M, Hofmeister V, Wischhusen J, Bornemann A, Meyermann R, Weiss EH, Melms A, Weller M. A functional role of HLA-G expression in human gliomas: An alternative strategy of immune escape. J Immunol. 2002;168:4772–4780. doi: 10.4049/jimmunol.168.9.4772. [DOI] [PubMed] [Google Scholar]
- 79.Kren L, Muckova K, Lzicarova E, Sova M, Vybihal V, Svoboda T, Fadrus P, Smrcka M, Slaby O, Lakomy R, et al. Production of immune-modulatory nonclassical molecules HLA-G and HLA-E by tumor infiltrating ameboid microglia/macrophages in glioblastomas: A role in innate immunity? J Neuroimmunol. 2010;220:131–135. doi: 10.1016/j.jneuroim.2010.01.014. [DOI] [PubMed] [Google Scholar]
- 80.Kren L, Slaby O, Muckova K, Lzicarova E, Sova M, Vybihal V, Svoboda T, Fadrus P, Lakomy R, Vanhara P, et al. Expression of immune-modulatory molecules HLA-G and HLA-E by tumor cells in glioblastomas: An unexpected prognostic significance? Neuropathology. 2011;31:129–134. doi: 10.1111/j.1440-1789.2010.01149.x. [DOI] [PubMed] [Google Scholar]
- 81.Wastowski IJ, Simões RT, Yaghi L, Donadi EA, Pancoto JT, Poras I, Lechapt-Zalcman E, Bernaudin M, Valable S, Carlotti CG, Jr, et al. Human leukocyte antigen-G is frequently expressed in glioblastoma and may be induced in vitro by combined 5-aza-2′-deoxycytidine and interferon-γ treatments: Results from a multicentric study. Am J Pathol. 2013;182:540–552. doi: 10.1016/j.ajpath.2012.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gros F, Sebti Y, de Guibert S, Branger B, Bernard M, Fauchet R, Amiot L. Soluble HLA-G molecules increase during acute leukemia, especially in subtypes affecting monocytic and lymphoid lineages. Neoplasia. 2006;8:223–230. doi: 10.1593/neo.05703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Dardano A, Rizzo R, Polini A, Stignani M, Tognini S, Pasqualetti G, Ursino S, Colato C, Ferdeghini M, Baricordi OR, Monzani F. Soluble human leukocyte antigen-g and its insertion/deletion polymorphism in papillary thyroid carcinoma: Novel potential biomarkers of disease? J Clin Endocrinol Metab. 2012;97:4080–4086. doi: 10.1210/jc.2012-2231. [DOI] [PubMed] [Google Scholar]
- 84.Reimers MS, Engels CC, Putter H, Morreau H, Liefers GJ, van de Velde CJ, Kuppen PJ, Prognostic value of HLA class I, HLA-E, HLA-G and Tregs in rectal cancer A retrospective cohort study. Bmc Cancer. 2014;14:486. doi: 10.1186/1471-2407-14-486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Martelli-Palomino G, Pancotto JA, Muniz YC, Mendes-Junior CT, Castelli EC, Massaro JD, Krawice-Radanne I, Poras I, Rebmann V, Carosella ED, et al. Polymorphic sites at the 3′ untranslated region of the HLA-G gene are associated with differential hla-g soluble levels in the Brazilian and French population. PLoS One. 2013;8:e71742. doi: 10.1371/journal.pone.0071742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Silva ID, Muniz YC, Sousa MC, Silva KR, Castelli EC, Filho JC, Osta AP, Lima MI, Simões RT. HLA-G 3′UTR polymorphisms in high grade and invasive cervico-vaginal cancer. Hum Immunol. 2013;74:452–458. doi: 10.1016/j.humimm.2012.11.025. [DOI] [PubMed] [Google Scholar]
- 87.Jiang Y, Chen S, Jia S, Zhu Z, Gao X, Dong D, Gao Y. Association of HLA-G 3′ UTR 14-bp insertion/deletion polymorphism with hepatocellular carcinoma susceptibility in a Chinese population. Dna Cell Biol. 2011;30:1027–1032. doi: 10.1089/dna.2011.1238. [DOI] [PubMed] [Google Scholar]
- 88.Lau DT, Norris MD, Marshall GM, Haber M, Ashton LJ. HLA-G polymorphisms, genetic susceptibility, and clinical outcome in childhood neuroblastoma. Tissue Antigens. 2011;78:421–427. doi: 10.1111/j.1399-0039.2011.01781.x. [DOI] [PubMed] [Google Scholar]
- 89.Ferguson R, Ramanakumar AV, Koushik A, Coutlée F, Franco E, Roger M, Biomarkers of Cervical Cancer Risk Study Team Human leukocyte antigen G polymorphism is associated with an increased risk of invasive cancer of the uterine cervix. Int J Cancer. 2012;131:E312–E319. doi: 10.1002/ijc.27356. [DOI] [PubMed] [Google Scholar]
- 90.Ghandri N, Gabbouj S, Farhat K, Bouaouina N, Abdelaziz H, Nouri A, Chouchane L, Hassen E. Association of HLA-G polymorphisms with nasopharyngeal carcinoma risk and clinical outcome. Hum Immunol. 2011;72:150–158. doi: 10.1016/j.humimm.2010.10.006. [DOI] [PubMed] [Google Scholar]
- 91.Xu HH, Shi WW, Lin A, Yan WH. HLA-G 3′ untranslated region polymorphisms influence the susceptibility for human papillomavirus infection. Tissue Antigens. 2014;84:216–222. doi: 10.1111/tan.12359. [DOI] [PubMed] [Google Scholar]
- 92.Eskandari-Nasab E, Hashemi M, Hasani SS, Omrani M, Taheri M, Mashhadi MA. Association between HLA-G 3′UTR 14-bp ins/del polymorphism and susceptibility to breast cancer. Cancer Biomark. 2013;13:253–259. doi: 10.3233/CBM-130364. [DOI] [PubMed] [Google Scholar]
- 93.Rolfsen GB, Castelli EC, Donadi EA, Duarte RA, Soares CP. HLA-G polymorphism and breast cancer. Int J Immunogenet. 2014;41:143–148. doi: 10.1111/iji.12092. [DOI] [PubMed] [Google Scholar]
- 94.Teixeira AC, Mendes-Junior CT, Souza FF, Marano LA, Deghaide NH, Ferreira SC, Mente ED, Sankarankutty AK, Elias-Junior J, Castro-e-Silva O, et al. The 14bp-deletion allele in the HLA-G gene confers susceptibility to the development of hepatocellular carcinoma in the Brazilian population. Tissue Antigens. 2013;81:408–413. doi: 10.1111/tan.12097. [DOI] [PubMed] [Google Scholar]
- 95.Kim SK, Chung JH, Jeon JW, Park JJ, Cha JM, Joo KR, Lee JI, Shin HP. Association between HLA-G 14-bp insertion/deletion polymorphism and hepatocellular carcinoma in Korean patients with chronic hepatitis B viral infection. Hepatogastroenterology. 2013;60:796–798. doi: 10.5754/hge11180. [DOI] [PubMed] [Google Scholar]
- 96.Yan WH. HLA-G expression in cancers: Potential role in diagnosis, prognosis and therapy. Endocr Metab Immune Disord Drug Targets. 2011;11:76–89. doi: 10.2174/187153011794982059. [DOI] [PubMed] [Google Scholar]
- 97.Teng MW, Galon J, Fridman WH, Smyth MJ. From mice to humans: Developments in cancer immunoediting. J Clin Invest. 2015;125:3338–3346. doi: 10.1172/JCI80004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Kochan G, Escors D, Breckpot K, Guerrero-Setas D. Role of non-classical MHC class I molecules in cancer immunosuppression. Oncoimmunology. 2013;2:e26491. doi: 10.4161/onci.26491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Zeng XC, Zhang T, Huang DH, Wang GY, Chen W, Li H, Zhang J, Fang TL, Zhang Q, Chen GH. RNA interfering targeting human leukocyte antigen-G enhanced immune surveillance mediated by the natural killer cells on hepatocellular carcinoma. Ann Clin Lab Sci. 2013;43:135–144. [PubMed] [Google Scholar]
- 100.Lin A, Xu HH, Xu DP, Zhang X, Wang Q, Yan WH. Multiple steps of HLA-G in ovarian carcinoma metastasis: Alter NK cytotoxicity and induce matrix metalloproteinase-15 (MMP-15) expression. Hum Immunol. 2013;74:439–446. doi: 10.1016/j.humimm.2012.11.021. [DOI] [PubMed] [Google Scholar]
- 101.Lesport E, Baudhuin J, LeMaoult J, Sousa S, Doliger C, Carosella ED, Favier B. Human melanoma cell secreting human leukocyte antigen-G5 inhibit natural killer cell cytotoxicity by impairing lytic granules polarization toward target cell. Hum Immunol. 2009;70:1000–1005. doi: 10.1016/j.humimm.2009.07.019. [DOI] [PubMed] [Google Scholar]
- 102.Moreau P, Mouillot G, Rousseau P, Marcou C, Dausset J, Carosella ED. HLA-G gene repression is reversed by demethylation; Proc Natl Acad Sci USA; 2003; pp. 1191–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Zidi I, Guillard C, Marcou C, Krawice-Radanne I, Sangrouber D, Rouas-Freiss N, Carosella ED, Moreau P. Increase in HLA-G1 proteolytic shedding by tumor cells: A regulatory pathway controlled by NF-kappaB inducers. Cell Mol Life Sci. 2006;63:2669–2681. doi: 10.1007/s00018-006-6341-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Rodríguez JA, Galeano L, Palacios DM, Gómez C, Serrano ML, Bravo MM, Combita AL. Altered HLA class I and HLA-G expression is associated with IL-10 expression in patients with cervical cancer. Pathobiology. 2012;79:72–83. doi: 10.1159/000334089. [DOI] [PubMed] [Google Scholar]
- 105.Tao S, He H, Chen Q, Yue W. GPER mediated estradiol reduces miR-148a to promote HLA-G expression in breast cancer. Biochem Biophys Res Commun. 2014;451:74–78. doi: 10.1016/j.bbrc.2014.07.073. [DOI] [PubMed] [Google Scholar]
- 106.Caumartin J, Favier B, Daouya M, Guillard C, Moreau P, Carosella ED, LeMaoult J. Trogocytosis-based generation of suppressive NK cells. Embo J. 2007;26:1423–1433. doi: 10.1038/sj.emboj.7601570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.LeMaoult J, Caumartin J, Daouya M, Favier B, Le Rond S, Gonzalez A, Carosella ED. Immune regulation by pretenders: Cell-to-cell transfers of HLA-G make effector T cells act as regulatory cells. Blood. 2007;109:2040–2048. doi: 10.1182/blood-2006-05-024547. [DOI] [PubMed] [Google Scholar]
- 108.Brown R, Kabani K, Favaloro J, Yang S, Ho PJ, Gibson J, Fromm P, Suen H, Woodland N, Nassif N, et al. CD86+ or HLA-G+ can be transferred via trogocytosis from myeloma cells to T cells and are associated with poor prognosis. Blood. 2012;120:2055–2063. doi: 10.1182/blood-2012-03-416792. [DOI] [PubMed] [Google Scholar]
- 109.Morandi F, Ferretti E, Bocca P, Prigione I, Raffaghello L, Pistoia V. A novel mechanism of soluble HLA-G mediated immune modulation: Downregulation of T cell chemokine receptor expression and impairment of chemotaxis. PLoS One. 2010;5:e11763. doi: 10.1371/journal.pone.0011763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Morandi F, Ferretti E, Castriconi R, Dondero A, Petretto A, Bottino C, Pistoia V. Soluble HLA-G dampens CD94/NKG2A expression and function and differentially modulates chemotaxis and cytokine and chemokine secretion in CD56bright and CD56dim NK cells. Blood. 2011;118:5840–5850. doi: 10.1182/blood-2011-05-352393. [DOI] [PubMed] [Google Scholar]
- 111.Naji A, Menier C, Morandi F, Agaugué S, Maki G, Ferretti E, Bruel S, Pistoia V, Carosella ED, Rouas-Freiss N. Binding of HLA-G to ITIM-bearing Ig-like transcript 2 receptor suppresses B cell responses. J Immunol. 2014;192:1536–1546. doi: 10.4049/jimmunol.1300438. [DOI] [PubMed] [Google Scholar]
- 112.Liu X, Gu W, Li X. HLA-G regulates the invasive properties of JEG-3 choriocarcinoma cells by controlling STAT3 activation. Placenta. 2013;34:1044–1052. doi: 10.1016/j.placenta.2013.07.070. [DOI] [PubMed] [Google Scholar]
- 113.Liang S, Baibakov B, Horuzsko A. HLA-G inhibits the functions of murine dendritic cells via the PIR-B immune inhibitory receptor. Eur J Immunol. 2002;32:2418–2426. doi: 10.1002/1521-4141(200209)32:9<2418::AID-IMMU2418>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 114.Agaugué S, Carosella ED, Rouas-Freiss N. Role of HLA-G in tumor escape through expansion of myeloid-derived suppressor cells and cytokinic balance in favor of Th2 versus Th1/Th17. Blood. 2011;117:7021–7031. doi: 10.1182/blood-2010-07-294389. [DOI] [PubMed] [Google Scholar]
- 115.Loumagne L, Baudhuin J, Favier B, Montespan F, Carosella ED, Rouas-Freiss N. In vivo evidence that secretion of HLA-G by immunogenic tumor cells allows their evasion from immunosurveillance. Int J Cancer. 2014;135:2107–2117. doi: 10.1002/ijc.28845. [DOI] [PubMed] [Google Scholar]
- 116.Dong DD, Yie SM, Li K, Li F, Xu Y, Xu G, Song L, Yang H. Importance of HLA-G expression and tumor infiltrating lymphocytes in molecular subtypes of breast cancer. Hum Immunol. 2012;73:998–1004. doi: 10.1016/j.humimm.2012.07.321. [DOI] [PubMed] [Google Scholar]
- 117.Gallegos CE, Michelin S, Trasci SB, Lobos EA, Dubner D, Carosella ED. HLA-G1 increases the radiosensitivity of human tumoral cells. Cell Immunol. 2014;287:106–111. doi: 10.1016/j.cellimm.2014.01.005. [DOI] [PubMed] [Google Scholar]