Abstract
Background
Although collaborative care programs are effective in improving late-life depression, only about half of treated patients achieve clinically meaningful improvement. Thus, we need to examine what characteristics may predict poor late-life depression course. Despite the robust evidence for the negative association between the quality of couple relationships and depression outcomes, few studies have examined these associations in the context of long-term late-life depression course.
Aim
The objective of this study is to examine the relations between the severity of couple conflict, receiving collaborative depression care program, and 24-months depression outcomes.
Methods
Study sample comprised 840 depressed older adults subsample from the improving mood, promoting access to collaborative treatment for late-life depression trial (IMPACT). Depression and couple conflict were assessed at baseline, 12-month, and 24-month follow-up. Descriptive statistics and multivariate regression analyses were performed to examine mean 24-month depression-free days (DFD) and the marginal effects of receiving IMAPCT program over usual care among participants with varying degrees of 24-month couple conflict.
Results
Compared with those who never endorsed frequent couple conflict over the three observation points, those who did twice had 63 fewer DFD (p = 0.01), and those who did three times experienced 148 fewer DFD (p < 0.001). Although the marginal effects of receiving IMPACT program over usual care was greater in overall sample, it was not statistically significant among those who endorsed frequent conflict at two or three times.
Conclusion
Frequent couple conflict is associated with worse long-term late-life depression outcomes among the patients in primary care clinics.
Keywords: late-life depression, marital conflict, IMPACT model
Introduction
Depression is a serious public health problem among older adults, and individuals with depression have greater disability-adjusted life years (DALY) than those without (Murray and Lopez, 1997). DALY is defined as the sum of years of potential life lost because of premature mortality and the years of productive life lost because of disability. It is well established that collaborative care programs in primary care clinics are effective in improving the outcomes associated with late-life depression (Unützer et al., 2002; Bruce et al., 2004). Yet, this evidence-based practice leads to robust improvement in only about half of treated patients. Thus, there is an urgent need to examine what individual characteristics may predict poor depression treatment outcomes in depressed older adults. One such characteristic may be the quality of couple relationships. Literature suggest that, among various social relationships in later life, couples relationships are among the most crucial (Carstensen et al., 1995). In general, older couples report more intimacy, stability, satisfaction, and less conflict than their younger counterparts (Yalom and Carstensen, 2002).
The relation between the quality of couple relationships and depression appears to be bidirectional. Robust evidence suggests that social support may buffer individuals from detrimental effects of life stressors (Kamp Dush et al., 2008; Warner and Kelley-Moore, 2012), decrease the risks for depression(Lee et al., 1996; Martire and Schulz, 2007) and depression relapse (George et al., 1989), increase adherence to depression treatment (Smith et al., 2003; Voils et al., 2005), and improves treatment outcomes (Billings and Moos, 1985; Berkman et al., 2003). Studies have shown depressive symptoms are significantly less prevalent among married or partnered older adults than among never married, divorced, or widowed counterparts (Brown et al., 2005; Choi and Ha, 2011). Spousal supports play important roles in a person’s mental and physical health (Institute of Medicine, 2001), and depression can damage these relationships. Negative emotional experiences, such as arguing or being angry at spouse/partner, can increase the risk for and the severity of depression (Jacobson et al., 1989). On the other hand, depression can increase couple conflict, make individuals perceive the quality of relationship with spouse more negatively, and decrease an individual’s ability to resolve conflict effectively.
A person’s illness and disability may impact older couples more severely than their younger counterparts. Several theoretical frameworks have been presented. First, because the couple relationship becomes more salient to individuals later in life (Carstensen et al., 1995), a person’s illness or relational distress may impact older adults’ emotional health more than younger adults (Bookwala and Franks, 2005; Umberson et al., 2006). Studies have shown a clear connection between poor couple relationship and depression in later life (Choi and Marks, 2008; Wang et al., 2014). Second, as an individual ages, one’s biological vulnerability increases. Thus, the intersection between the psychosocial risk factor, such as couple conflict, and biological vulnerability may create a cumulative effect on individual-health and couple-health (Crystal and Shea, 1990).
Unfortunately, little information is available to conclude if couple conflict has a negative impact on long-term late-life depression outcomes. Few randomized clinical trials on depression treatment collected data on the quality of couple relationship in older adult samples, barring us from examining the effects of couple conflict on depression outcomes. Understanding the association between couple distress on depression outcomes, however, may help us to identify predictors of poor depression outcomes among older adult patients and to formulate strategies to improve quality of care for older adults with depression.
This paper fills this gap by reporting the self-rated couple conflict in cohort of older adults with depression from the improving mood, promoting access to collaborative treatment for late-life depression trial (IMPACT) study, a large trial of collaborative care for late-life depression (Unützer et al., 2002). We tested following two hypotheses: (1) the severity of couple conflict over 24-months would be negatively associated with the 24-month depression-free days (DFD) and (2) receiving IMPACT program would be associated with greater 24-month DFD to usual care.
Methods
The data were derived from the IMPACT study, which compared depression care outcomes between the IMPACT collaborative care program with usual primary care. Participants were recruited from seven study sites in five states, representing eight health care organizations and 18 primary care clinics. Patients were randomly assigned to the IMPACT intervention (n = 906) or to usual care (n = 895). IMPACT intervention was delivered by depression care managers who were supervised by a psychiatrist and a primary care physician. These care managers offered education, care management, and support of depression treatment. Two depression treatments were offered: antidepressant management by the patient’s primary care physician or problem solving treatment in primary care, a brief psychotherapy for depression. Intervention patients had access to an IMPACT care manager for up to 12 months. Usual care patients could use any primary care or specialty mental health services available for them in usual care. After 12 months, all study participants continued with their regular primary care providers as usual. Informed consent was obtained from all participants and the study protocols were approved by the institutional review boards at participating sites and the study coordination center. Rates of item-level missing data at baseline were less than 2% for all variables discussed in this article. Because this was less than the recommended 5% for imputation (Tabachnick and Fidell, 2001), cases with missing values were not included in the analyses, resulting in a slightly reduced number of observations included in the final analyses. Details of design, protocol, and outcomes have been published elsewhere (Unutzer et al., 2001; Unützer et al., 2002).
Sample
The IMAPCT study includes 1801 racially and ethnically diverse depressed older adults (60 years or older). Older adults with severe cognitive impairment, active substance abuse or suicidality, severe mental illness, and current treatment from a psychiatrist were excluded from the study. For the current analyses, we used a subsample of 840 depressed older adults who are cohabiting with their spouse or partner at baseline. Among them, 807 were married or partnered, and 33 were separated or divorced.
Measures
Depression-free days is a summary measure of the severity of depressive symptoms over a period of time (Mallick et al., 2003; Vannoy et al., 2010). In this study, depression severity was measured at baseline, 3, 6, 12, 18, and 24 months using the 20 depression items of the Hopkins symptom checklist (HSCL-20) (Derogatis et al., 1974). We calculated the number of DFD over the 24-month study period based on the HSCL-20 scores following the procedure described by Simon et al.,(Simon et al., 2002) Thompson et al., (Thompson et al., 2008) and Vannoy et al. (Vannoy et al., 2010). First, using HSCL-20 scores from two consecutive outcome assessments (e.g. baseline and 3 moths follow-up), we estimated depression severity for each day during the interval by linear interpolation. Days with an HSCL-90 depression score of 0.50 or less are considered ‘depression free.’ On days with an HSCL-90 depression score of 2.00 or higher, the patient is considered ‘fully symptomatic.’ Days with intermediate severity scores are assigned a value between depression free and fully symptomatic by linear interpolation. For example, days with an SCL-90 score of 1.25 would be considered 50% depression free. Then, values for each follow-up interval are then summed to generate the 24-month DFDs.
Couple conflict was derived based on the question ‘Over the past 2 weeks, have you been angry or argued with your spouse or partner?’ The possible scores ranged from not at all (0), occasionally (1), half the time (2), most of the time (3), and all the time (4). We used the data collected at baseline, 12 and 24 months. To generate the 24-month couple conflict, we first created a binary variable using cut-point of 2 (half the time) because occasional couple conflict is expected in couples’ relationship. Then, we counted the number of times when a respondent indicated having been angry or argued with spouse or partner more than half the time at baseline, 12-month, and 24-month. The possible scores of 24-month couple conflict, hence, ranged between 0 and 3. The greater score indicated increasing degree of perceived couple conflict.
Having a confidante was derived based on the yes/no question ‘do you have a confidante, someone you can talk with, who is a source of support?’
Sharing housework responsibility was derived based on the question ‘over the past 2 weeks, have you and your spouse or partner shared the responsibility of practical matters that have arisen such as household chores or financial matters?’ The possible scores ranged from not at all (0), occasionally (1), half the time (2), most of the time (3), and all the time (4). We generated a binary variable using cut-point of 2 (half the time).
Data analysis
All analyses were performed with Stata MP version 12. Descriptive statistics, t-tests and chi square tests were used to examine the sample distribution. Previous publications have already demonstrated that there were no significant differences in demographic, socioeconomical, and clinical characteristics between these two groups (Unützer et al., 2002).
To examine the association between 24-month couple conflict and DFD (Hypothesis 1), we used multivariate linear regression models with DFD as a dependent variable, adjusted for covariates specified a priori. Using F-test, we tested if there are differences in mean DFD over the 24-month observation period among patients who reported no couple conflict at any of the three survey periods (baseline, 12-months, and 24-months) compared with those who reported couple conflict at one, two, or all three of the surveys.
To examine if receiving IMPACT program would be associated with shorter DFD given same level of couple conflict (Hypothesis 2), we added interaction term between intervention status (IMPACT vs. usual care) and 24-month couple conflict to the multivariate linear regression model mentioned earlier. Based on this regression model, we estimated and compared the marginal effects of two hypothetical conditions (1) when all study sample received IMPACT program and (2) when all study sample received usual care, adjusted for all covariates.
Results
Table 1 summarizes the distribution of demographic, family, and clinical characteristics by baseline couple conflict. Majority of sample were married (n = 809) and only 3% (n = 26) were not married but cohabiting at baseline. The majority of study sample reported having shared household work with spouse more than half the time over the past 2 weeks and having confidante (67.02% vs. 71.16%, respectively). Greater proportion of sample that shared household less than half the time reported frequent couple conflict, compared with their counterparts (28.52% vs. 16.70; p < 0.001). And greater proportion of sample without confidante reported frequent couple conflict than those with confidante (27.27% vs. 17.92 p = 0.002). Compared with non-Hispanic White, greater proportion of minority older adults (Black, Hispanic, and others) reported frequent couple conflict (18.69% vs. 28.31%; p = 0.006). The average number of DFD over 24 months for total sample was 332.2 days (SE ± 7.54). Those with frequent couple conflict had fewer DFD compared to those with low couple conflict (290.45 ± 15.92 vs. 343.07 ± 8.51; p = 0.005).
Table 1.
Distribution of demographic, family and clinical characteristics at baseline
| Couple conflict over the past 2 weeks, have you been angry or argued with each other? | Low less than half the time (N = 667, 79.40%) | High half the time or more (N = 173, 20.60%) | Total (N = 840, 100%) | p-value low vs. high |
|---|---|---|---|---|
| Treatment type (N, %) | 0.976 | |||
| IMPACT | 323 (79.36%) | 84 (20.64%) | 407 (48.45%) | |
| Usual care | 344 (79.45%) | 89 (20.55%) | 433 (51.55%) | |
| Demographic characteristics | ||||
| Age (mean ± SE) | 70.51 ± 0.27 | 69.92 ± 0.50 | 70.39 ± 0.24 | 0.32 |
| Gender (N, %) | 0.90 | |||
| Female | 339 (79.58%) | 87 (20.42%) | 426 (50.71%) | |
| Male | 328 (79.23%) | 86 (20.77%) | 414 (49.29%) | |
| Marital status | 0.58 | |||
| Married | 620 (79.28%) | 162 (20.72%) | 782 (93.10%) | |
| Not married/cohabiting | 219 (76.00%) | 6 (24%) | 25 (2.98%) | |
| Divorced/separated | 28 (84.85%) | 5 (15.15%) | 33 (3.93%) | |
| Education (N, %)* | 0.012 | |||
| Less than high school | 116 (17.39%) | 31 (17.92%) | 147 (17.50%) | |
| High school graduate | 134 (20.09%) | 53 (30.64%) | 187 (22.26%) | |
| Some college | 233 (34.93%) | 56 (32.37%) | 217 (34.40%) | |
| College graduate and above | 184 (27.59%) | 33 (19.08%) | 217 (25.83%) | |
| Race (N, %)* | 0.006 | |||
| White | 548 (81.31%) | 126 (18.69%) | 674 (80.24%) | |
| Non-white | 119 (71.69%) | 47 (28.31%) | 166 (19.76%) | |
| Family characteristics | ||||
| Household size | 2.30 ± 0.03 | 2.38 ± 0.07 | 2.31 ± 0.03 | 0.27 |
| Family wealth (N, %) | 0.10 | |||
| Household asset < $50 000 | 148 (75.51%) | 48 (24.49%) | 196 (25%) | |
| Household asset ≥ $50 000 | 476 (80.95%) | 112 (19.05%) | 588 (75.00%) | |
| Share household work (N, %) | <0.001 | |||
| Less than half the time | 198 (71.48%) | 79 (28.52%) | 277 (32.98) | |
| More than half the time | 469 (83.30%) | 94 (16.70%) | 563 (67.02%) | |
| Have a confidante | 0.002 | |||
| No | 176 (72.73%) | 66 (27.27%) | 242 (28.84%) | |
| Yes | 490 (82.08%) | 107 (17.92%) | 597 (71.16%) | |
| Baseline clinical characteristics (mean, SE) | ||||
| Cognitive screening score | 5.56 ± 0.03 | 5.46 ± 0.06 | 5.54 ± 0.05 | 0.10 |
| Number of chronic disease | 3.74 ± 0.07 | 3.79 ± 0.15 | 3.75 ± 0.07 | 0.79 |
| Quality of life | 5.50 ± 0.07 | 5.23 ± 0.16 | 5.44 ± 0.07 | 0.10 |
| Mental Component Summary (MCS) 12 | 42.41 ± 0.29 | 41.73 ± 0.54 | 42.27 ± 0.25 | 0.28 |
| Physical Component Summary (PCS) 12 | 40.87 ± 0.30 | 40.93 ± 0.56 | 40.88 ± 0.26 | 0.92 |
| General health score | 3.29 ± 0.43 | 3.32 ± 0.89 | 3.30 ± 0.04 | 0.78 |
| Sheehan disability score | 4.59 ± 0.10 | 4.84 ± 0.19 | 4.64 ± 0.09 | 0.26 |
| Baseline HSCL score | 1.63 ± 0.02 | 1.83 ± 0.04 | 1.67 ± 0.02 | <0.001 |
| 24-Month depression-free days | 343.07 ± 8.51 | 290.43 ± 15.92 | 332.2 ± 7.54 | 0.005 |
IMPACT, Improving Mood, Promoting Access to Collaborative Treatment for late-life depression trial; HSCL, Hopkins symptom checklist.
Figure 1 illustrates DFD by couple conflict at baseline and over the 24-month study period with 95% confidence interval (CI). We observed linear trends between DFD and martial conflict measured at baseline and over 24-month period. Although the majority of the sample (58.59%) never endorsed having frequent conflict, approximately 5% of sample endorsed frequent couple conflict at baseline, 12, and 24 months. Another 10% of the sample endorsed having frequent conflict twice out of three surveys over the 24-month observation period.
Figure 1.
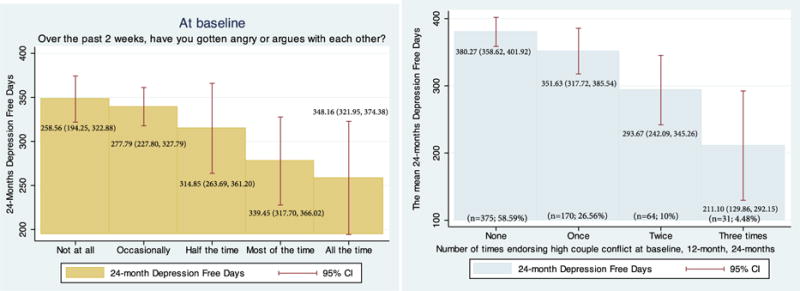
Twenty-four month depression-free days by baseline couple conflict and by 24-month couple conflict.
Table 2 presents the result of multivariate linear regression model. We tested the associations between the mean DFD and 24-month couple conflict adjusted for intervention group, age, education, minority status, having confidante, sharing household work more than half the time, baseline depression severity measured by HSCL-20 scores, baseline Sheehan disability scores, and baseline general health scores. Compared with the older adults who never endorsed couple conflicts, those who endorsed frequent couple conflict on two surveys had 62.51 fewer DFD (p = 0.01). Those who endorsed frequent couple conflict three times experienced 148.15 fewer DFD than those who never endorsed conflict (p < 0.01).
Table 2.
Results from the linear regression examining the association between depression free days and couple conflicts
| Depression-free days and frequency of couple conflicts over 24 months
|
||||||
|---|---|---|---|---|---|---|
| Coefficient | SD | t-statistics | p-values | 95% CI lower | 95% CI upper | |
| Endorsing high couple conflict at baseline, 12 months, 24 months | ||||||
| Never | ref | |||||
| Once | −23.65 | 16.65 | −1.42 | 0.16 | −56.34 | 9.04 |
| Twice | −62.51 | 24.41 | −2.56 | 0.01 | −110.45 | −14.58 |
| All three times | −148.15 | 34.31 | −4.32 | 0.00 | −215.52 | −80.78 |
| Receiving IMPACT (ref: care as usual) | 101.63 | 14.28 | 7.12 | 0.00 | 73.59 | 129.67 |
| Age | −3.61 | 1.07 | −3.37 | 0.00 | −5.71 | −1.50 |
| Education | ||||||
| Less than high school | ref | |||||
| High school Graduate | −24.96 | 24.03 | −1.04 | 0.30 | −72.15 | 22.24 |
| Some college | −24.78 | 22.44 | −1.10 | 0.27 | −68.85 | 19.30 |
| College graduate and above | 45.35 | 23.44 | 1.93 | 0.05 | −0.68 | 91.38 |
| Being minority (ref: non-Hispanic White) | 1.13 | 18.65 | 0.06 | 0.95 | −35.49 | 37.74 |
| Having confidante at baseline | −16.40 | 15.76 | −1.04 | 0.30 | −47.34 | 14.54 |
| Have shared housework more than half the time | −12.31 | 16.07 | −0.77 | 0.44 | −43.87 | 19.25 |
| Baseline HSCL-20 scores | −129.71 | 13.37 | −9.70 | 0.00 | −155.96 | −103.46 |
| Baseline Sheehan disability scores | −7.58 | 3.25 | −2.33 | 0.02 | −13.96 | −1.19 |
| Baseline general health (reverse scores coded) | −36.53 | 6.97 | −5.24 | 0.00 | −50.22 | −22.83 |
| Cons | 967.22 | 89.70 | 10.78 | 0.00 | 791.06 | 1143.37 |
IMPACT, Improving Mood, Promoting Access to Collaborative Treatment for late-life depression trial; HSCL, Hopkins symptom checklist.
Figure 2 presents a graphic representation of the interaction between 24-month couple conflict and receiving IMPACT program. The marginal effect of receiving IMPACT program was consistently greater than receiving usual care across the varying degrees of couple conflict. Among those who endorsed frequent couple conflict never or once at three observation points, the marginal effect of receiving IMPACT program over usual care increased the DFD (329.82 vs. 431.34; 302.50 vs. 412.57) and these differences were statistically significant (p < 0.001). Among those who endorsed frequent couple conflict twice and three times, receiving IMPACT program increased the DFD (293.54 vs. 349.79; 163.02 vs. 317.50), however, these were not statistically significant and 95% CI was wider.
Figure 2.
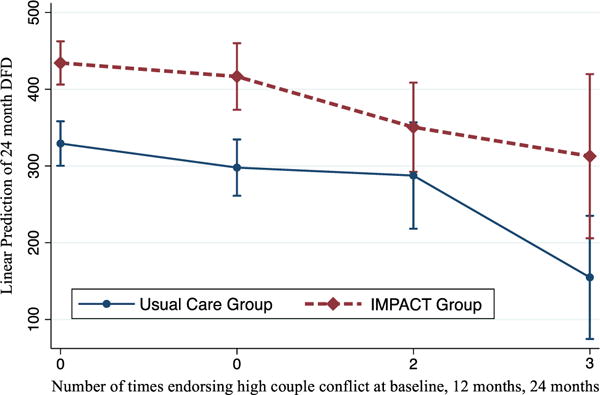
Interaction between 24-month couple conflict and intervention.
Discussion
The major finding of this study is that frequent couple conflict was associated with poor long-term late-life depression outcomes. This burden of couple conflict on long-term depression outcomes persisted in both IMPACT group and the usual primary care group. This finding is consistent with the literature that negative couple experience is unfavorable to the depression outcomes in older adults (Choi and Marks, 2008). This is potentially important because even the most effective evidence-base late-life depression care in primary clinics achieves significant response in only about 50% of those treated. It is possible that closer attention to high couple conflict and addressing such conflict as part of treating older adults with depression might further improve the depression outcomes in both primary care clinics with or without collaborative care program. Couple conflict is modifiable even in later life, and it may be important to identify those who have severe couple conflict and help them improve the quality of couple relationship or ameliorate the negative impact of couple conflict on depression as an important part of treatment.
Our secondary finding is that individuals who received IMPACT program had consistently greater DFD across the varying degrees of couple conflict. Although, those who endorsed frequent couple conflict two and three times, the 95% CI for point estimate of marginal affect of receiving IMPACT program over usual care was wide was not statistically significant.
This may be due to the fact that only small number of older adults reported frequent couple conflict twice (n = 64) or three times (n = 31) over the 24-months, which may have limited a statistical power of the current analyses. Future studies with sufficient statistical power are needed to confirm our findings.
There are few limitations in our study. First, as mentioned earlier, given the bidirectional nature of couple relationship and depression outcomes, we are unable to draw causal relationship in our analysis. Second, couple conflict was measured based on the single self-reported question measuring frequency of arguing or being angry with the partner in the past 2 weeks. It is unknown if the couple conflict at baseline, 12 and 24 months was related to recurring problems or about new problems. We were also unable to examine other important components of couple conflicts, such as the intensity of the conflict or efforts to address such conflict as part of treatment. Collectively, these present limitation in conceptualization and measurement of an important dependent variable. Future studies may consider using a measure that assesses multiple dimensions of couple conflict. Third, data on significant changes in couple status such as divorce, separation, or death of spouse during the 24-month study duration were not collected, thus we were not able to examine how such changes impacted the couple dynamics and, ultimately, long-term depression outcomes.
The vast majority of IMPACT participants received both pharmacotherapy and counseling/psychotherapy. All patients had at least some psychotherapy such as behavioral activation and pleasant events scheduling as part of the care management component of the intervention, and more than 70% had at least some antidepressant management. The assignment of treatments such as psychotherapy or medications was not random (e.g., patients and providers decided on the use of medications, in part based on individual preferences and severity of depression) and these issues make it difficult to try and attribute differences in depression outcomes to various treatment components such as psychotherapy or medications. This is one of the limitations of a multicomponent intervention model such as IMPACT.
Despite aforementioned limitation, this study contributes to the literature significantly. We have identified an important predictor of poor late-life depression outcomes. In this large real world sample of depressed older adults from 18 primary care clinics, approximately 15 % of the participants reported frequent couple conflict more than once. These older adults experienced two or three more months of depression and in this context.
Given the findings of our analyses, it would be a worthwhile endeavor to examine if brief relationship-oriented treatments, such as interpersonal therapies (IPT) might further improve depression outcomes in older adults treatment for depression. Reynolds and colleagues (Reynolds et al., 1999) concluded that combined treatment of nortriptyline and IPT was superior to IPT and placebo. They also suggested that the combined treatment might lead to better efficacy over nortriptyline monotherapy. Recent meta-analyses(Martire and Schulz, 2007; Barbato and D’Avanzo, 2008; Martire et al., 2010) and clinical trials(Jacob et al., 1987; Bodenmann et al., 2008; Cohen et al., 2010) concluded that couples therapy approaches were as effective as individual psychotherapy in alleviating depressive symptoms and more effective than individual therapy in alleviating relationship distress. Providing intensive couples’ therapies in primary a care settings may be challenging, but provider could assess the patient’s preference for such therapies and refer patients with significant couple conflict to therapists experienced in working with couples, especially if patients do not improve with initial treatment in primary care.
Conclusions
Couple relationship quality is an important aspect of patients’ ecological and social context. A failure to consider this important aspect of a patient’s life can lead to poor depression outcomes. When treating late-life depression, providers should assess conflict with the spouse or partner, especially when there is no improvement after a period of evidence-based treatment.
Key points.
Approximately 15 % of depressed older adults in primary care report having high-conflict couple conflict.
Prolonged couple conflict is detrimental to depression outcomes among older adults
Footnotes
Conflict of interest
None declared.
References
- Murray C, Lopez A. Alternative projections of mortality by cause 1990–2020: global burden of disease study. Lancet. 1997;349:1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- Unützer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting. JAMA. 2002;288(22):2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- Bruce M, Ten Have T, Reynolds C, Katz I, Schulberg H. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291(9):1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- Carstensen LL, Gottman JM, Levenson RW. Emotional behavior in long-term marriage. Psychol Aging. 1995;10(1):140–149. doi: 10.1037//0882-7974.10.1.140. [DOI] [PubMed] [Google Scholar]
- Yalom M, Carstensen LL. Inside the American Couple: new Thinking, New Challenges. University of California Pr; Berkeley, CA: 2002. [Google Scholar]
- Warner DF, Kelley-Moore J. The social context of disablement among older adults does marital quality matter for loneliness? J Health Soc Behav. 2012;53(1):50–66. doi: 10.1177/0022146512439540. [DOI] [PubMed] [Google Scholar]
- Kamp Dush CM, Taylor MG, Kroeger RA. Marital happiness and psychological well-being across the life course*. Fam Relat. 2008;57(2):211–226. doi: 10.1111/j.1741-3729.2008.00495.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martire LM, Schulz R. Involving family in psychosocial interventions for chronic illness. Curr Dir Psychol Sci. 2007;16(2):90–94. [Google Scholar]
- Lee MS, Crittenden KS, Yu E. Social support and depression among elderly Korean immigrants in the United States. Int J Aging Hum Dev. 1996;42(4):313–327. doi: 10.2190/2VHH-JLXY-EBVG-Y8JB. [DOI] [PubMed] [Google Scholar]
- George LK, Blazer DG, Hughes DC, Fowler N. Social support and the outcome of major depression. Br J Psychiatry. 1989;154(4):478–485. doi: 10.1192/bjp.154.4.478. [DOI] [PubMed] [Google Scholar]
- Smith F, Francis S-A, Gray N, Denham M, Graffy J. A multi-centre survey among informal carers who manage medication for older care recipients: problems experienced and development of services. Health Soc Care Community. 2003;11(2):138–145. doi: 10.1046/j.1365-2524.2003.00415.x. [DOI] [PubMed] [Google Scholar]
- Voils CI, Steffens DC, Flint EP, Bosworth HB. Social support and locus of control as predictors of adherence to antidepressant medication in an elderly population. Am J Geriatr Psychiatry. 2005;13(2):157–165. doi: 10.1176/appi.ajgp.13.2.157. [DOI] [PubMed] [Google Scholar]
- Berkman LF, Blumenthal J, Burg M, et al. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the enhancing recovery in coronary heart disease patients (ENRICHD) randomized trial. JAMA. 2003;289(23):3106–3116. doi: 10.1001/jama.289.23.3106. [DOI] [PubMed] [Google Scholar]
- Billings AG, Moos RH. Life stressors and social resources affect posttreatment outcomes among depressed patients. J Abnorm Psychol. 1985;94(2):140–153. doi: 10.1037//0021-843x.94.2.140. [DOI] [PubMed] [Google Scholar]
- Choi NG, Ha J-H. Relationship between spouse/partner support and depressive symptoms in older adults: gender difference. Aging Ment Health. 2011;15(3):307–317. doi: 10.1080/13607863.2010.513042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SL, Bulanda JR, Lee GR. The significance of nonmarital cohabitation: Marital status and mental health benefits among middle-aged and older adults. J Gerontol B Psychol Sci Soc Sci. 2005;60(1):S21–S29. doi: 10.1093/geronb/60.1.s21. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Health and Behavior: The Interplay of Biological, Behavioral, and Social Influence. The national Academied Press; Washington D.C.: 2001. [Google Scholar]
- Jacobson NS, Holtzworth-Munroe A, Schmaling KB. Marital therapy and spouse involvement in the treatment of depression, agoraphobia, and alcoholism. J Consult Clin Psychol. 1989;57(1):5–10. doi: 10.1037//0022-006x.57.1.5. [DOI] [PubMed] [Google Scholar]
- Umberson D, Williams K, Powers DA, Liu H, Needham B. You make me sick: marital quality and health over the life course. J Health Soc Behav. 2006;47(1):1–16. doi: 10.1177/002214650604700101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bookwala J, Franks MM. Moderating role of marital quality in older adults’ depressed affect: beyond the main-effects model. J Gerontol B Psychol Sci Soc Sci. 2005;60(6):P338–P341. doi: 10.1093/geronb/60.6.p338. [DOI] [PubMed] [Google Scholar]
- Choi H, Marks NF. Marital conflict, depressive symptoms, and functional impairment. J Marriage Fam. 2008;70(2):377–390. doi: 10.1111/j.1741-3737.2008.00488.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q, Wang D, Li C, Miller RB. Marital satisfaction and depressive symptoms among Chinese older couples. Aging Ment Health. 2014;18(1):11–18. doi: 10.1080/13607863.2013.805730. [DOI] [PubMed] [Google Scholar]
- Crystal S, Shea D. Cumulative advantage, cumulative disadvantage, and inequality among elderly people. Gerontologist. 1990;30(4):437–443. doi: 10.1093/geront/30.4.437. [DOI] [PubMed] [Google Scholar]
- Tabachnick B, Fidell L. Using Multivariatestatistics. 4th. Harper & Row; NewYork: 2001. [Google Scholar]
- Unutzer J, Katon W, Williams JW, Jr, et al. Improving primary care for depression in late life: the design of a multicenter randomized trial. Med Care. 2001;39(8):785–799. doi: 10.1097/00005650-200108000-00005. [DOI] [PubMed] [Google Scholar]
- Mallick R, Jieling C, Entsuah AR, Schatzberg AF. Depression-free days as a summary measure of the temporal pattern of response and remission in the treatment of major depression: a comparison of venlafaxine, selective serotonin reuptake inhibitors, and placebo. J Clin Psychiatry. 2003;64(3):321–330. doi: 10.4088/jcp.v64n0315. [DOI] [PubMed] [Google Scholar]
- Vannoy SD, Arean P, Unutzer J. Advantages of using estimated depression-free days for evaluating treatment efficacy. Psychiatr Serv. 2010;61(2):160–163. doi: 10.1176/appi.ps.61.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR, Lipman RS, Rickels K, Uhlenhuth EH, Covi L. The Hopkins symptom checklist (HSCL): a self-report symptom inventory. Behav Sci. 1974;19(1):1–15. doi: 10.1002/bs.3830190102. [DOI] [PubMed] [Google Scholar]
- Simon GE, Von Korff M, Ludman EJ, et al. Cost-effectiveness of a program to prevent depression relapse in primary care. Med Care. 2002;40(10):941–950. doi: 10.1097/00005650-200210000-00011. [DOI] [PubMed] [Google Scholar]
- Thompson A, Fan MY, Unutzer J, Katon W. One extra month of depression: the effects of caregiving on depression outcomes in the IMPACT trial. Int J Geriatr Psychiatry. 2008;23(5):511–516. doi: 10.1002/gps.1929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbato A, D’Avanzo B. Efficacy of couple therapy as a treatment for depression: a meta-analysis. Psychiatry Q. 2008;79(2):121–132. doi: 10.1007/s11126-008-9068-0. [DOI] [PubMed] [Google Scholar]
- Reynolds CF, Frank E, Perel JM, et al. Nortriptyline and Interpersonal Psychotherapy as Maintenance Therapies for Recurrent Major Depression. JAMA: The Journal of the American Medical Association. 1999;281(1):39–45. doi: 10.1001/jama.281.1.39. [DOI] [PubMed] [Google Scholar]
- Martire LM, Schulz R, Helgeson VS, Small BJ. Review and meta-analysis of couple-oriented interventions for chronic illness. Ann Behav Med. 2010;40(3):325–342. doi: 10.1007/s12160-010-9216-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodenmann G, Plancherel B, Beach SRH, et al. Effects of coping-oriented couples therapy on depression: a randomized clinical trial. J Consult Clin Psychol. 2008;76(6):944–954. doi: 10.1037/a0013467. [DOI] [PubMed] [Google Scholar]
- Cohen S, O’Leary KD, Foran H. A randomized clinical trial of a brief, problem-focused couple therapy for depression. Behav Ther. 2010;41(4):433–446. doi: 10.1016/j.beth.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob M, Frank E, Kupfer DJ, Comes C, Carpenter LL. A psychoeducational workshop for depressed patients, family, and friends: description and evaluation. Hosp Community Psychiatry. 1987;38(9):968–972. doi: 10.1176/ps.38.9.968. [DOI] [PubMed] [Google Scholar]


