Prostate cancer (PCa) is the second leading cause of death among men worldwide. Androgen signaling plays key roles in PCa progression [1], and so far available therapeutic agents mainly target androgens or androgen receptor (AR) [2]. However, the patients receiving these treatments often recurs with progression to castration resistant prostate cancer (CRPC) [3]. Metastatic CRPC (mCRPC) is the advanced and lethal stage of PCa [4]. Recent advances in the field show that immune checkpoint blockade (ICB) is the paramount choice for targeting many types of cancers including PCa [4], [5], [6]. ICB generates effective therapeutic response across certain cancers [5], whereas it failed to improve overall survival of patients with mCRPC [7]. To address this challenge, one recent study by Lu and colleagues [8] has demonstrated an ICB approach combined with targeted drugs for myeloid-derived immune suppressive cells (MDSCs), thereby enforcing the T cells to combat mCRPC tumor cells [8]. The authors have shown that, MDSCs are recruited to tumor microenvironment (TME) and exert immune suppressive impact on T cells. MDSCs immune suppression can be prevented using targeted drugs combined with ICB. The landmark strategy introduced by authors is a step towards solving the problem of drug resistance and ICB evasion in PCa and its progression to mCRPC.
Previous studies revealed that ICB improves overall survival in melanoma. In ICB antibodies against cytotoxic-T-lymphocyte-associated protein 4 (CTLA4) and programmed cell death 1/programmed cell death 1 ligand 1 (PD1/PD-L1), target the surface CTLA4 and PD1/PD-L1 receptors thereby stimulating and inhibiting the production of cytokines, interleukin-2 (IL-2) and interferon-γ (IFN-γ) respectively [5], [9]. IL-2 production and IFN-γ inhibition, increase T cell proliferation, restore activated T cell response and reduce immunosuppression, cumulatively activating the immune response against tumor cells [9]. However, mCRPC shows resistance against ICB, due to MDSCs [10] that are major component of TME with immunosuppressive activity [11]. Mouse (Ptenpc−/− and smad4pc−/−) model of PCa tumors indicated that chemokine CXCL5 recruits MDSCs to TME, which enables PCa tumor initiation and progression [10].
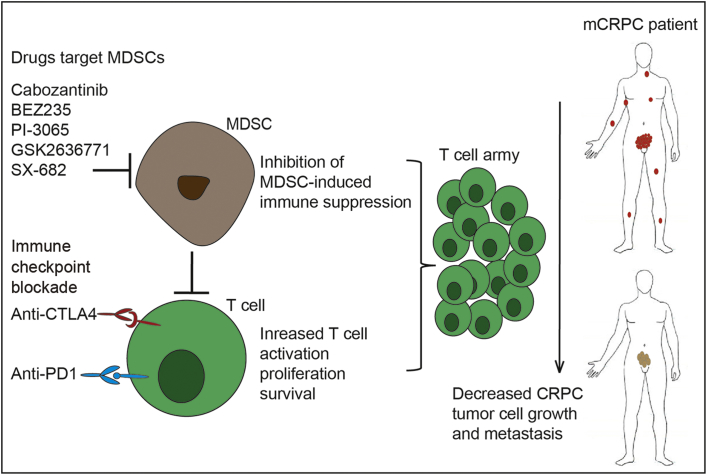
In this current study, Lu and colleagues developed a chimeric mCRPC mouse model (CPPSML) for effective testing of combination immunotherapy. CPPSML chimeric mouse with prostate tumors when subjected to androgen deprivation therapy developed primary CRPC and progressed to mCRPC with metastasis in lymph nodes and lungs. These mCRPC mice were treated with tyrosine kinase inhibitors (dasatinib and cabozantinib) and the phosphoinositide 3-kinase (PI3K)/mTOR dual inhibitor BEZ235 combined with ICB. The cabozantinib and BEZ235 combined with ICB restricted primary and metastatic PCa growth through restricted tumor cell proliferation and apoptosis. Further investigation in CPPSML PCa tumors revealed accumulation of granulocytic MDSCs (Gr-MDSCs), which were significantly reduced upon targeted drug treatment. MDSCs depletion with anti-Gr1 antibody sensitized CPPSML PCa tumors to ICB. Findings suggested that MDSCs generate resistance to ICB, whereas targeted drug treatment enhances ICB through abating MDSCs [8] [Fig. 1, left].
Figure 1.
Targeted drugs for MDSCs combined with ICB help T cells to fight against mCRPC tumors in vivo. Targeted drugs cabozantinib (tyrosine kinase inhibitor), BEZ235 (PI3K/mTOR dual inhibitor), PI-3065 (P110δ-selective inhibitor), GSK2636771 (P110β-selective inhibitor) and SX-682 (CXCR1/2 inhibitor) restrict the immune suppressive activity of MDSCs by inhibiting PI3K signaling pathway and MDSCs recruiting cytokines, and reducing the expression of immune suppressive genes. ICB increases T cell proliferation, restore activated T cell response and reduce immunosuppression thereby activating a strong immune response against mCRPC tumor cells in vivo. ICB combined with targeted drugs have synergistic efficacy on CRPC in chimeric mouse model. The combined immunotherapy strategy may be applied for treating the human mCRPC patients. CRPC, castration resistant prostate cancer; ICB, immune checkpoint blockade; MDSC, myeloid-derived immune suppressive cell; mCRPC, metastatic CRPC.
Mechanistic evaluation in CPPSML PCa tumors revealed that targeted agents reduce suppressive activity of intratumoural MDSCs through various mechanisms. Targeted drugs alleviate suppressive activity of MDSCs on proliferation of CD4+ and CD8+ T cells that are vital in ICB. These agents inhibit PI3K signaling pathway in both MDSCs and tumor cells through reducing phosphorylated MET (pMET) and phosphorylated vascular endothelial growth factor receptor 2 (pVEGFR2) levels. Target drugs plus ICB reduced levels of MDSCs recruiting cytokines such as CCL5, CCL12, CD40 and hepatocyte growth factor (HGF), and increase levels of MDSCs recruitment inhibitors such as IL-1ra, CD142, and vascular endothelial growth factor (VEGF). Previous studies have validated that cytokines production by tumor cells upregulate expression of certain genes such as Arg1, Cybb, Ncf1, and Ncf4 that are responsible for MDSCs induced immune suppression. Those genes were found highly expressed in CPPSML PCa tumors. Target drugs together with ICB treatment significantly downregulated production of 10 cytokines including CCL5. However, when MDSCs isolated from CRPC tumors were treated with each of 10 cytokines upregulated the expression of immunosuppressive genes was significantly upregulated. Additionally, the biopsy samples of PCa tumor analysis showed the frequency of CD8+ T cells inversely correlated with the frequency of Gr-MDSCs, which is consistent with antagonistic activity of Gr-MDSCs on CD8+ T cells in human PCa [8]. Altogether, these findings suggest that one way (ICB) is not enough, a combinatorial (ICB + target drugs) immunotherapy needs to be applied to fight against mCRPC, where targeted agents can empower the T cell army to eliminate tumor cells in the reported mouse models (Fig. 1, left), and potentially in human patients with mCRPC (Fig. 1, right).
For efficient combinatorial immunotherapy testing, the development of a CPPSML chimeric mCRPC model in mice is admirable. However, it is practically unrealistic to have CPPSML-like genotype in PCa patients. The possible solution for this weakness is to test combinatorial therapy (ICB + target drugs) on suitable human mCRPC samples. In addition, patient samples taken at different stages of disease may help in determining the effectiveness of therapy in stage dependent manner. Furthermore, as indicated in original article [8], the combined immunotherapy need clinical trials for its implementation.
Conflicts of interest
The authors declare no conflict of interest.
References
- 1.Stuchbery R., McCoy P.J., Hovens C.M., Corcoran N.M. Androgen synthesis in prostate cancer: do all roads lead to Rome? Nat Rev Urol. 2017;14:49–58. doi: 10.1038/nrurol.2016.221. [DOI] [PubMed] [Google Scholar]
- 2.Miao L., Yang L., Li R., Nava R.D., Crespo M., Hsieh J.T. Disrupting androgen receptor signaling induces snail-mediated epithelial-mesenchymal plasticity in prostate cancer. Cancer Res. 2017 Mar 16 doi: 10.1158/0008-5472.CAN-16-2169. pii: canres.2169.2016. http://dx.doi.org/10.1158/0008-5472.CAN-16-2169. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 3.Watson P.A., Arora V.K., Sawyers C.L. Emerging mechanisms of resistance to androgen receptor inhibitors in prostate cancer. Nat Rev Cancer. 2015;15:701–711. doi: 10.1038/nrc4016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yap T.A., Smith A.D., Ferraldeschi R., Al-Lazikani B., Workman P., de Bono J.S. Drug discovery in advanced prostate cancer: translating biology into therapy. Nat Rev Drug Discov. 2016;15:699–718. doi: 10.1038/nrd.2016.120. [DOI] [PubMed] [Google Scholar]
- 5.Sharma P., Allison J.P. The future of immune checkpoint therapy. Science. 2015;348:56–61. doi: 10.1126/science.aaa8172. [DOI] [PubMed] [Google Scholar]
- 6.Pardoll D.M. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12:252–264. doi: 10.1038/nrc3239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beer T.M., Kwon E.D., Drake C.G., Fizazi K., Logothetis C., Gravis G. Randomized, double-blind, phase III trial of ipilimumab versus placebo in asymptomatic or minimally symptomatic patients with metastatic chemotherapy-naive castration-resistant prostate cancer. J Clin Oncol. 2017;35:40–47. doi: 10.1200/JCO.2016.69.1584. [DOI] [PubMed] [Google Scholar]
- 8.Lu X., Horner J.W., Paul E., Shang X., Troncoso P., Deng P. Effective combinatorial immunotherapy for castration-resistant prostate cancer. Nature. 2017;543:728–732. doi: 10.1038/nature21676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buchbinder E.I., Desai A. CTLA-4 and PD-1 pathways: Similarities, differences, and implications of their inhibition. Am J Clin Oncol. 2016;39:98–106. doi: 10.1097/COC.0000000000000239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang G., Lu X., Dey P., Deng P., Wu C.C., Jiang S. Targeting YAP-dependent MDSC infiltration impairs tumor progression. Cancer Discov. 2016;6:80–95. doi: 10.1158/2159-8290.CD-15-0224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kumar V., Patel S., Tcyganov E., Gabrilovich D.I. The nature of myeloid-derived suppressor cells in the tumor microenvironment. Trends Immunol. 2016;37:208–220. doi: 10.1016/j.it.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]