Abstract
Background
Social features of neighborhood environments may influence smoking by creating a stressful environment or by buffering stress through social cohesion. However, the association of the overall neighborhood social environment (NSE) with smoking, and the association of specific neighborhood social factors with change in smoking behavior over time, has rarely been examined.
Methods
This study included 5,856 adults aged 45–84 years from the Multi-Ethnic Study of Atherosclerosis (2000–2012, average follow-up: 7.8 years). Outcomes included current smoking status and smoking intensity (average number of cigarettes smoked per day among baseline smokers). NSE was assessed as a composite score composed of aesthetic quality, safety, and social cohesion scales (derived from neighborhood surveys). Generalized linear mixed models evaluated the association of baseline NSE (composite score and individual scales) with current smoking (modified Poisson models) and smoking intensity (negative binomial models) cross-sectionally and longitudinally.
Results
Each standard deviation increase in baseline NSE composite score was associated with 13% lower prevalence of smoking at baseline (adjusted prevalence ratio (aPR): 0.87 (95% confidence interval: 0.78, 0.98). Neighborhood safety and aesthetic quality were similarly associated with lower smoking prevalence (aPR: 0.87 (0.78, 0.97) and aPR: 0.87 (0.77, 0.99), respectively) but the association with social cohesion was weaker or null. No significant associations were observed for smoking intensity among baseline smokers. Baseline NSE was not associated with changes in smoking risk or intensity over time.
Conclusions
Results suggest that neighborhood social context influences whether older adults smoke, but does not promote smoking cessation or reduction over time.
Keywords: Neighborhoods/place, Social capital, Smoking, Psychosocial factors
INTRODUCTION
Despite declines in smoking prevalence over the past few decades,[1, 2] smoking remains a major cause of preventable death worldwide. In recent years, researchers have increasingly focused on the impact of the neighborhoods in which people live on health behaviors.[3] For example, low neighborhood socioeconomic level has been found to be associated with higher smoking prevalence and decreased likelihood of smoking cessation.[4–8] Additionally, neighborhood social factors including safety and social cohesion have gained increasing attention as potential contextual risk factors for smoking behavior.
Specific aspects of the neighborhood social environment theorized to be relevant to smoking behaviors include psychological stressors such as noise level or poor aesthetic quality [9, 10], perceptions of safety and crime in the neighborhood,[11–13] and perceptions of social cohesion.[11, 14–16] Prior studies have found that individuals living in neighborhoods with higher levels of self-reported neighborhood problems were more likely to smoke,[9, 10, 15] though not all studies found an association.[17] Similarly, studies have shown that people living in high crime areas had higher smoking prevalence[12] and were less likely to quit smoking,[8, 12] likely a result of increased stress due to violence or disorder.[11] Fewer studies have evaluated the effect of neighborhood problems and crime on smoking intensity, defined as the number of cigarettes smoked per day by current smokers. Prior work found no association with neighborhood problems,[9, 17] however, neighborhood violence/crime was associated with higher smoking intensity.[12, 18]
In addition to directly affecting smoking, neighborhood social features may also buffer stress. Neighborhood social cohesion, or how connected people feel with their neighbors,[19] is thought to influence health by promoting supportive neighborhoods that buffer stress and connect residents to shared resources and services; this may in turn lead to adoption of healthy behaviors.[20] Prior research suggests that social cohesion may have a protective effect on smoking prevalence[14–16, 21] although results for smoking intensity have been mixed.[14, 18]
Although a number of studies have examined how neighborhood social factors influence smoking behavior, most prior research has been cross-sectional,[9–12, 14–17] limiting causal inference. The association of neighborhood social environment with smoking over time has been examined in only a few studies.[18, 22, 23] In addition, individual domains of the neighborhood social environment such as social cohesion[14–16] and safety[12] have been examined separately, but studies have not integrated these distinct measures into one composite score to reflect the overall neighborhood social context. In light of these knowledge gaps, this study aims to describe cross-sectional and longitudinal associations of the neighborhood social environment (overall, and for the individual domains of aesthetic quality, safety, and social cohesiveness) with smoking risk and intensity. We hypothesized that a better neighborhood social environment would be associated with lower smoking prevalence and intensity at baseline. Furthermore, a better baseline neighborhood environment would be associated with greater reductions over time in smoking risk and intensity.
METHODS
Study population
This study used data from the Multi-Ethnic Study of Atherosclerosis (MESA), a longitudinal cohort study of 6,814 adults aged 44–84 and free of cardiovascular disease at baseline.[24] MESA participants were sampled from six U.S. sites (Los Angeles, CA, Manhattan and Bronx, NY, St. Paul, MN, Chicago, IL, Baltimore, MD, and Forsyth County, NC). The baseline examination was conducted in 2000–2002, and four follow up exams were conducted between 2002 and 2012, with retention rates of 92.4% at year 2, 89.2% at year 3, 86.8% at year 5, and 75.7% at year 10. The Institutional Review Boards (IRB) at each MESA data collection sites approved the study, and all participants provided informed consent. Drexel University IRB approved secondary analyses of these data under expedited category 7.
MESA participants (N=6,191, 90.9% of the baseline sample) who participated in the MESA Neighborhood Study, an ancillary study to MESA which assessed neighborhood environments and geocoded all residential addresses, were included. In the current study, we excluded those with missing outcome (N=53), exposure (N=108), or covariate data (N=33) and for whom the accuracy of geocoding was low (not at street-level or zip+4 centroid level, N=23). In order to examine longitudinal associations of neighborhood social environment on smoking, we included only participants who had outcome and exposure data from at least two exams (N=5,856, 95% of those in the neighborhood study). Included and excluded participants were similar on most socio-demographic characteristics (Supplemental Table 1).
Smoking Outcomes
The primary outcomes included smoking status and smoking intensity. Both outcomes were assessed at each exam by self-report. Ever smoking was assessed by: “Have you smoked at least 100 cigarettes in your lifetime?” and if the participant answered yes, current smoking status by: “Have you smoked cigarettes in the last 30 days?” In analyses, smoking status was dichotomized as current smoker versus former/never smoker. Smoking intensity was assessed among current and former smokers as follows: “On average, how many cigarettes a day do/did you smoke?” To reflect current habits, the number of cigarettes was recoded to 0 for baseline smokers who quit during follow-up at exams subsequent to quitting.
Neighborhood Social Environment
The neighborhood social environment was characterized using a composite score from subscales reflecting 3 domains: aesthetic quality, safety, and social cohesion (Table 1). Respondents were asked to rate an area within 1 mile of their residence. Questions were asked of MESA Neighborhood Study participants as well as an independent sample of community raters who were recruited from the same census tracts as MESA participants using random digit dialing or list-based sampling (the MESA Community Surveys).[25] MESA participants responded to each scale twice (social cohesion in 2000–2002, safety and aesthetic quality in 2003–2005, and all three scales in 2010–2012). We calculated baseline neighborhood social environment scores for each participant as continuous variables based on the average score reported at first measurement by all respondents (from the Neighborhood Study and Community Surveys) living within 1 mile of their residence, excluding the participant’s own responses (range: 1–738 respondents, mean: 155, standard deviation: 168). This approach avoids the issue of same-source bias, in which individuals self-report both exposure and health outcomes and their health status affects how they report the exposure or vice versa.[26] The scales have good internal consistency (Cronbach’s alphas 0.74–0.77), and test-retest reliability (0.65–0.88).[25] A 1-mile radius (Euclidian distance) was used instead of census tract because the survey defined neighborhood as “the area within about a 20 minute walk (or about a mile) from your home.” In addition, census tracts vary in size across regions, are prone to the modifiable areal unit problem,[27, 28] and may be problematic for assigning neighborhood characteristics to individuals living on the margins of the tract.[29]
Table 1.
Neighborhood Social Environment Survey Questions,a The Multi-Ethnic Study of Atherosclerosis
| Domains and Items |
|---|
| Aesthetic Quality Scale Items |
| There is a lot of trash and litter on the street in my neighborhood |
| There is a lot of noise in my neighborhood |
| My neighborhood is attractive |
|
|
| Safety Scale Items |
| I feel safe walking in my neighborhood, day or night |
| Violence is not a problem in my neighborhood |
|
|
| Social Cohesion Scale Items |
| People around here are willing to help their neighbors |
| People in my neighborhood generally get along with each other |
| People in my neighborhood can be trusted |
| People in my neighborhood share the same values |
Social environment questions were from MESA participants as well as community raters from the same census tracts. MESA participants completed each scale twice (social cohesion in 2000–2002, safety and aesthetic quality in 2003–2005, all three scales in 2010–2011). Community raters completed the scales in 2004 (5,988 participants from the Maryland, New York, and North Carolina study sites) and 2011–2012 (4,212 participants from a subsample of census tracts in all 6 MESA sites). Response options were on a 5-point Likert scale from 1 (strongly agree) to 5 (strongly disagree). Questions were rescaled as needed so a higher score reflected a more favorable neighborhood environment.
Standardized z-scores were constructed for each participant for each subscale by centering at the mean and dividing by the standard deviation (SD) across all time points. In this study, we assessed the effect of both the composite baseline neighborhood social environment score and each of the separate subscales. The composite measure was constructed by summing the three standardized subscales, and then re-standardizing. All regression models report the effect of a standard deviation increase in the neighborhood domain of interest. For descriptive purposes, we calculated tertiles of neighborhood social environment scores at baseline. We focused on baseline neighborhood social environment because there was little change in neighborhood social environment scores over the course of follow-up on average (intraclass correlation coefficients 0.94–0.97).
Covariates
Time-invariant individual-level covariates assessed at the baseline exam included baseline age (in years), gender, race (White, African American, Hispanic, Asian), education (categorized as high school or less, some college/technical school/Associate’s degree, Bachelor’s degree or higher), and study site. Time-varying covariates included marital status (married/living with partner versus not), employment status (employed versus unemployed/retired), alcohol use (current use versus no current use), time since baseline (years), and income. Household income was assessed using a 13-category item with income categories ranging from <$5,000 to >$100,000. A continuous income was constructed by assigning the midpoint of each category to participants who selected that category. This value was divided by the number of people in the household and adjusted for inflation to reflect the inflation-adjusted per capita household income. Sensitivity to alternative income definitions (categorical income or household, rather than per-capita, income) was assessed, and results were found to be similar.
Neighborhood-level socioeconomic status was evaluated using a composite measure that included the following census variables: log median housing value, percent with a high school education, percent with a bachelor’s degree, percent in a managerial occupation, log median household income, and percent with interest/dividend income. Data from the 2000 U.S Census and the 2005–2009 and 2007–2011 American Community Surveys were used. Z-scores for each variable were summed to create the composite measure, with a higher score indicating higher census tract-level socioeconomic status.[30]
Statistical analysis
Characteristics of the study population were described at each exam. We compared the distribution of socio-demographic characteristics between smokers and non-smokers, and by tertiles of baseline neighborhood social environment scores.
We estimated cross-sectional and longitudinal associations of the baseline neighborhood social environment scales with smoking outcomes using generalized linear mixed models (PROC GLIMMIX, SAS 9.3, SAS Institute Inc., Cary, NC). All models included repeated outcome measurements within subjects over time (baseline and at least one additional measurement between Exams 2–5.) We included a random intercept for each subject. The neighborhood social environment domains were highly correlated (r= 0.6 to r=0.9, p<0.0001), thus, when using the disaggregated domains, each domain was modeled separately.
Smoking status was modeled using relative-risk regression (via modified Poisson regression models with robust variance estimates).[31, 32] Smoking intensity was modelled using negative binomial models to evaluate the effect of baseline neighborhood social environment on the number of cigarettes smoked per day. Smoking intensity models included only the subset of the cohort who reported smoking at baseline (N=741). We chose negative binomial models over Poisson as the distribution of the smoking intensity variable suggested over-dispersion (mean across exams: 10.0, variance 162.9) and a likelihood ratio test indicated the negative binomial model was a better fit (p<0.0001). In each model, we included the baseline neighborhood social environment score, time since baseline (modeled continuously with coefficients expressed in 5-year intervals for interpretability), and an interaction between the baseline score and time. The exponentiated coefficient of the neighborhood environment main effect estimated the prevalence ratio of smoking at baseline associated with a 1 SD higher baseline score. The exponentiated coefficient of the interaction term estimated the ratio of the change in risk over a 5-year period associated with a 1 SD higher baseline score. Models were progressively adjusted as follows: Model 1: baseline age (centered at the mean), sex, interaction between baseline age and time since baseline; Model 2: further adjusted for race/ethnicity, education, baseline study site, and the following time-varying characteristics: marital status, income, employment status, and current alcohol use; Model 3: further adjusted for neighborhood socioeconomic status. We tested interactions between time invariant covariates (sex, race, education) and time as prior research suggests trajectories of smoking behavior change may differ in subgroups of the population.[33] We found that smoking intensity trajectories differed significantly by sex, race, and education; these three interaction terms were retained in smoking intensity models. In preliminary cross-sectional analyses, we included a random intercept for census tract to account for neighborhood clustering. As results were unchanged, and models including random intercepts for participants and census tracts did not converge, we did not include census tract random intercepts in final models.
Sensitivity Analyses
In a sensitivity analysis, we repeated analyses after excluding participants who did not live within a 1-mile radius of at least 5 other participants in either the main study or the community survey (N=298, for a total of 5,558 participants). These exclusions were made to test the sensitivity of results to neighborhoods with few participants rating neighborhood social environment.
RESULTS
Among 5,856 participants, 12.7% were current smokers at baseline. Current smokers smoked an average of 13.5 cigarettes per day at baseline. Table 2 presents demographic, behavioral, and neighborhood characteristics at each exam over the follow-up period. Participants had an average of 7.8 years of follow-up. Current smoking prevalence declined over follow-up to 7.3%, and the mean number of cigarettes smoked per day among baseline smokers declined to 7.0. At baseline, overall neighborhood social environment scores ranged from −11.1 to 7.3 (median −0.1). Prior to standardization, the means and standard deviations of the neighborhood subscales were: aesthetic quality: 3.7 (0.4), safety: 3.7 (0.4), social cohesion: 3.5 (0.3) on a scale from 1–5. Slightly more men, black or Hispanic participants, and participants with a high school degree or less were lost to follow-up compared to women, white or Asian participants, and participants with higher educational attainment. The proportion of participants who were married or currently working decreased as participants aged. Alcohol use declined over time while average neighborhood socioeconomic status increased.
Table 2.
Demographic, Behavioral, and Neighborhood Characteristics of the Study Sample, The MultiEthnic Study of Atherosclerosis Exams 1–5 (2000–2012)
| Sample Characteristicsa | Year 0, Exam 1 |
Year 2, Exam 2 |
Year 3, Exam 3 |
Year 5, Exam 4 |
Year 10, Exam 5 |
|---|---|---|---|---|---|
| N | 5,856 | 5,641 | 5,342 | 5,092 | 4,032 |
| Demographic Characteristics | |||||
| Mean age (SD)** | 61.9 (10.1) | 63.6 (10.1) | 65.9 (10.0) | 66.5 (9.9) | 69.9 (9.4) |
| Gender (%) | |||||
| Male | 2,753 (47.0) | 2,648 (46.9) | 2,496 (46.7) | 2,372 (46.6) | 1,848 (45.8) |
| Female | 3,103 (53.0) | 2,993 (53.1) | 2,846 (53.3) | 2,720 (53.4) | 2,184 (54.2) |
| Race (%) | |||||
| White | 2,291 (39.1) | 2,213 (39.2) | 2,121 (39.7) | 2,049 (40.2) | 1,633 (40.5) |
| Black/African American | 1,610 (27.5) | 1,553 (27.5) | 1,475 (27.6) | 1,385 (27.2) | 1,084 (26.9) |
| Hispanic | 1,261 (21.5) | 1,213 (21.5) | 1,121 (21.0) | 1,066 (20.9) | 843 (20.9) |
| Chinese | 694 (11.9) | 662 (11.7) | 625 (11.7) | 592 (11.6) | 472 (11.7) |
| Education (%) | |||||
| High school graduate or less | 2,051 (35.0) | 1,964 (34.8) | 1,842 (34.5) | 1,740 (34.2) | 1,290 (32.0) |
| Some college | 1,660 (28.4) | 1,600 (28.4) | 1,520 (28.4) | 1,438 (28.2) | 1,156 (28.7) |
| Bachelor’s or Graduate degree | 2,145 (36.6) | 2,077 (36.8) | 1,980 (27.1) | 1,914 (37.6) | 1,586 (39.3) |
| Currently employed (%)** | 3,190 (54.5) | 2,938 (52.1) | 2,722 (50.9) | 2,468 (48.5) | 1,764 (43.7) |
| Mean per capita annual household in come adjusted for inflation, in increments of 10,000 (SD)** | |||||
| 2.6 (2.0) | 2.6 (2.1) | 2.5 (2.0) | 2.4 (1.9) | 2.5 (1.8) | |
| Currently married (%)* | 3,610 (61.6) | 3,459 (61.3) | 3,290 (61.6) | 3,175 (62.3) | 2,391 (59.3) |
|
| |||||
| Health Behaviors | |||||
| Current Alcohol Use (%)** | 3,287 (56.1) | 2,867 (50.8) | 2,628 (49.2) | 2,279 (44.8) | 1,724 (42.8) |
| Smoking Status (%)** | |||||
| Never smoker | 2,957 (50.5) | 2,624 (46.5) | 2,435 (45.6) | 2,285 (44.9) | 1,839 (45.6) |
| Former smoker | 2,158 (36.8) | 2,391 (42.4) | 2,347 (43.9) | 2,319 (45.5) | 1,897 (47.1) |
| Current smoker | 741 (12.7) | 626 (11.1) | 560 (10.5) | 488 (9.6) | 296 (7.3) |
| Mean number of cigarettes smoked per day among baseline smokers (SD)** | |||||
| 13.5 (17.7) | 10.1 (9.5) | 9.7 (9.6) | 8.4 (9.2) | 7.0 (14.3) | |
|
| |||||
| Neighborhood Characteristicsb | |||||
| Neighborhood socioeconomic | 0.0 (6.3) | 0.0 (6.3) | 0.6 (5.9) | 1.8 (5.0) | 1.0 (4.6) |
| score, Mean (SD) (range)** | (−19.4–14.7) | (−19.4–14.7) | (−18.2–14.7) | (−8.7–14.8) | (−9.7–14.4) |
| Neighborhood social environment | −0.1 (2.5) | −0.1 (2.5) | −0.1 (2.5) | 0.1 (2.9) | 0.3 (3.0) |
| score, Mean (SD) (range)** | (−11.1–7.3) | (−11.1–7.3) | (−11.1–10.8) | (−12.8–10.8) | (−9.0–10.8) |
| Neighborhood aesthetic quality | 3.7 (0.4) | 3.7 (0.4) | 3.7 (0.4) | 3.7 (0.5) | 3.7 (0.5) |
| score, Mean (SD) (range) ** | (2.0–5.0) | (2.0–5.0) | (2.0–5.0) | (2.0–5.0) | (2.0–5.0) |
| Neighborhood safety score | 3.7 (0.4) | 3.7 (0.4) | 3.7 (0.4) | 3.6 (0.5) | 3.7 (0.5) |
| Mean (SD) (range) | (2.0–5.0) | (2.0–5.0) | (2.0–5.0) | (1.5–5.0) | (1.9–5.0) |
| Neighborhood social cohesion | 3.5 (0.3) | 3.5 (0.3) | 3.5 (0.3) | 3.6 (0.3) | 3.6 (0.3) |
| score, Mean (SD) (range) ** | (2.4–5.0) | (2.4–5.0) | (2.4–5.0) | (2.0–5.0) | (2.0–5.0) |
Sex, race, and education were only measured at baseline. Other variables were time-varying.
Neighborhood socioeconomic status score was calculated by summing z-scores for the following census variables: log median housing value, percent with a high school education, percent with a bachelor’s degree, percent in a managerial occupation, log median household income, and percent with interest/dividend income. Neighborhood social environment score was calculated by summing z-scores of the aesthetic quality, safety, and social cohesion scores. Unstandardized scores for aesthetic quality, safety, and social cohesion are shown in this table and were calculated by taking the average item score for each scale. For each scale, a higher score indicates a better neighborhood environment.
indicates significant at the p<.05 level based on chi-squared tests and analysis of variance
indicates significant at the p<.001 level based on chi-squared tests and analysis of variance
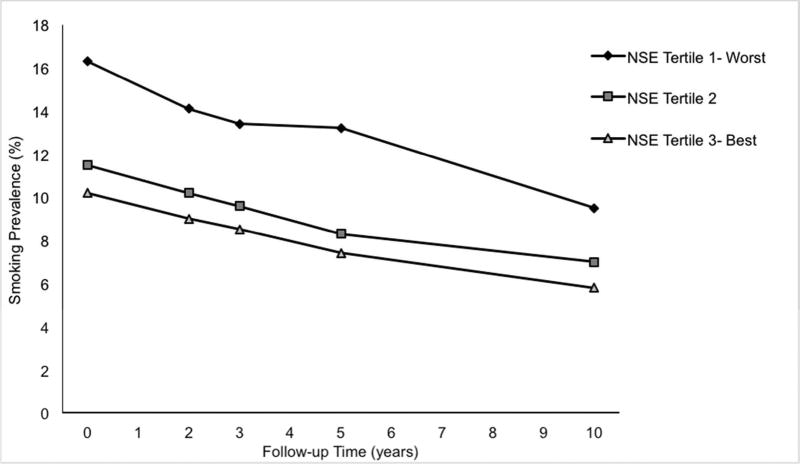
Bivariate analyses found that at higher tertiles of each neighborhood environment domain (reflecting better neighborhood environment), baseline smoking prevalence was lower (p for trends <0.01, Table 3). However, among baseline current smokers, the crude mean number of cigarettes smoked per day was higher in neighborhoods with better social environment scores (p for trends <0.01). Smoking prevalence declined over time across tertiles of baseline neighborhood social environment and the slope of the decline was similar across tertiles (Figure 1).
Table 3.
Bivariate Associations of Baseline Neighborhood Social Environment with Baseline Smoking Status and Intensity, The Multi-Ethnic Study of Atherosclerosis Exam 1 (2000–2002)
| Baseline Neighborhood Scale |
N (Entire Cohort- N=5,856) |
N (%) Current Smokers |
p-valuea | Mean (SD) # cigs smoked per day - current smokers N=741 |
p-valuea |
|---|---|---|---|---|---|
| Neighborhood Social Environment | <0.0001 | <0.0001 | |||
| Tertile 1- Worst | 1932 | 315 (16.3) | 11.6 (9.7) | ||
| Tertile 2 | 1991 | 228 (11.5) | 13.4 (10.2) | ||
| Tertile 3- Best | 1933 | 198 (10.2) | 16.6 (29.9) | ||
|
| |||||
| Aesthetic Quality | <0.0001 | <0.0001 | |||
| Tertile 1- Worst | 1932 | 292 (15.1) | 11.6 (9.5) | ||
| Tertile 2 | 1993 | 252 (12.6) | 13.6 (12.0) | ||
| Tertile 3- Best | 1931 | 1197 (10.2) | 16.3 (29.2) | ||
|
| |||||
| Safety | <0.0001 | <0.0001 | |||
| Tertile 1- Worst | 1932 | 317 (16.4) | 11.5 (9.5) | ||
| Tertile 2 | 1990 | 245 (12.3) | 14.1 (10.2) | ||
| Tertile 3- Best | 1934 | 179 (9.3) | 16.4 (31.4) | ||
|
| |||||
| Social cohesion | 0.003 | 0.002 | |||
| Tertile 1- Worst | 1929 | 279 (14.5) | 11.3 (9.0) | ||
| Tertile 2 | 1994 | 245 (12.3) | 14.6 (12.7) | ||
| Tertile 3- Best | 1933 | 217 (11.2) | 15.1 (27.9) | ||
p-value from test for trend (based on Wald statistic in logistic (current smoking) and negative binomial (smoking intensity) models including an ordinal term for baseline neighborhood social environment tertiles)
Figure 1. Unadjusted Prevalence of Smoking Over Follow-up. by Tertile of Baseline Neighborhood Social (NSE) I Environment. The Multi-Ethnic Study of Atherosclerosis (2000–2012).
In generalized linear mixed models, a 1 SD higher baseline neighborhood social environment score was associated with a 16% lower probability of being a current smoker at baseline [prevalence ratio (PR) 0.84 (95% CI: 0.75, 0.93), Table 4] after adjusting for socio-demographic characteristics. Results were attenuated but still statistically significant after adjustment for neighborhood socioeconomic status [0.87 (0.78, 0.98)]. For aesthetic quality and safety environment domains, the association was similar to the composite score [0.87 (0.77, 0.99); 0.87 (0.78, 0.97)] but for social cohesion there was a non-significant negative association. A higher baseline neighborhood social environment score did not modify changes in smoking risk over time for either the composite score or individual domains, as risk ratios ranged from 0.97–1.00 across models for the interaction term between baseline social environment and follow-up time.
Table 4.
Cross-sectional and Longitudinal Associations of a 1 SD Higher Baseline Neighborhood Social Environment Score with Risk of Current Smoking, The Multi-Ethnic Study of Atherosclerosis (2000–2012)a,b N=5856
| Relative Risk (95% CI) for Current Smoking | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |||||||
| Baseline Score |
Time Trend (5 year interval) |
Baseline Score x Time (5 year interval) |
Baseline Score |
Time Trend (5 year interval) |
Baseline Score x Time (5 year interval) |
Baseline Score |
Time Trend (5 year interval) |
Baseline Score x Time (5 year interval) |
|
| Neighborhood Social Environment | |||||||||
| 0.81 (0.75, 0.87) | 0.72 (0.69, 0.76) | 1.00 (0.96, 1.05) | 0.84 (0.75, 0.93) | 0.74 (0.70, 0.78) | 1.00 (0.95, 1.04) | 0.87 (0.78, 0.98) | 0.74 (0.70, 0.78) | 0.98 (0.94, 1.03) | |
| Aesthetic Quality | |||||||||
| 0.83 (0.78, 0.90) | 0.72 (0.69, 0.76) | 1.01 (0.97, 1.05) | 0.84 (0.75, 0.93) | 0.74 (0.70, 0.78) | 1.00 (0.96, 1.05) | 0.87 (0.77, 0.99) | 0.74 (0.70, 0.78) | 0.99 (0.93, 1.03) | |
| Safety | |||||||||
| 0.76 (0.70, 0.82) | 0.72 (0.69, 0.76) | 1.01 (0.96, 1.05) | 0.84 (0.76, 0.93) | 0.74 (0.70, 0.78) | 1.00 (0.96, 1.05) | 0.87 (0.78, 0.97) | 0.74 (0.70, 0.78) | 0.99 (0.95, 1.04) | |
| Social Cohesion | |||||||||
| 0.88 (0.82, 0.96) | 0.72 (0.69, 0.76) | 0.99 (0.94, 1.03) | 0.89 (0.80, 0.99) | 0.73 (0.70, 0.77) | 0.99 (0.94, 1.03) | 0.94 (0.84, 1.05) | 0.74 (0.70, 0.78) | 0.97 (0.92, 1.02) | |
Relative risks and confidence intervals are from generalized linear mixed Poisson models with robust variance estimates. All models include the baseline neighborhood environment score, time in years since baseline, and an interaction between baseline neighborhood score and time since baseline to test whether neighborhood social environment modifies the change in smoking status over time. All models included repeated measures and a random intercept for each participant.
Model 1 adjusted for baseline age (centered at the mean), sex, and baseline age*time interaction. Model 2 further adjusted for race, education, baseline study site, and the following time-varying covariates: marital status, income, employment, alcohol use. Model 3 further adjusted for neighborhood socioeconomic status (time-varying).
Among current smokers, baseline neighborhood social environment was initially positively associated with baseline smoking intensity; however, adjustment for additional socio-demographic characteristics attenuated this association and all confidence intervals widened to include the null (Table 5). Baseline neighborhood social environment did not modify the rate of change over time in the number of cigarettes consumed per day over time. Results were similar in sensitivity analyses that excluded participants who did not have at least 5 neighbors within a 1-mile radius of their residence (Supplemental Table 4).
Table 5.
Cross-sectional and Longitudinal Associations of a 1 SD Higher Baseline Neighborhood Social Environment Score with the Average Number of Cigarettes Smoked Per Day, The Multi-Ethnic Study of Atherosclerosis (2000–2012)a,b N=741 (restricted to participants who smoked at baseline)
| Rate Ratio (95% CI) for Average Number of Cigarettes Smoked Per Day | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |||||||
| Baseline Score |
Time Trend (5 year interval) |
Baseline Score x Time (5 year interval) |
Baseline Score |
Time Trend (5 year interval) |
Baseline Score x Time (5 year interval) |
Baseline Score |
Time Trend (5 year interval) |
Baseline Score x Time (5 year interval) |
|
| Neighborhood Social Environment | |||||||||
| 1.14 (1.04, 1.24) | 0.51 (0.47, 0.55) | 0.97 (0.92, 1.02) | 1.03 (0.92, 1.15) | 0.43 (0.38, 0.49) | 0.98 (0.93, 1.04) | 1.01 (0.89, 1.14) | 0.43 (0.38, 0.49) | 0.99 (0.93, 1.04) | |
| Aesthetic Quality | |||||||||
| 1.13 (1.03, 1.23) | 0.51 (0.47, 0.55) | 0.99 (0.94, 1.04) | 1.02 (0.90, 1.15) | 0.43 (0.38, 0.49) | 0.99 (0.94, 1.05) | 0.99 (0.87, 1.13) | 0.43 (0.38, 0.49) | 1.00 (0.94, 1.06) | |
| Safety | |||||||||
| 1.11 (1.01, 1.22) | 0.51 (0.47, 0.55) | 0.97 (0.92, 1.03) | 1.03 (0.92, 1.14) | 0.43 (0.38, 0.49) | 0.99 (0.93, 1.05) | 1.01 (0.90, 1.13) | 0.43 (0.38, 0.49) | 0.99 (0.93, 1.05) | |
| Social Cohesion | |||||||||
| 1.14 (1.03, 1.25) | 0.51 (0.47, 0.55) | 0.96 (0.91, 1.02) | 1.03 (0.92, 1.16) | 0.44 (0.39, 0.50) | 0.97 (0.92, 1.03) | 1.02 (0.90, 1.15) | 0.44 (0.38, 0.50) | 0.97 (0.92, 1.03) | |
Results are from generalized linear mixed negative binomial models. All models include the baseline neighborhood environment score, time in years since baseline, and an interaction between baseline neighborhood score and time since baseline to test whether neighborhood social environment modifies the change in smoking status over time. All models included repeated measures and a random intercept for each participant.
Model 1 adjusted for baseline age (centered at the mean), sex, baseline age*time interaction, and sex*time interaction. Model 2 further adjusted for race, education, baseline study site, and the following time-varying covariates: marital status, income, employment, alcohol use, and sex*time, education*time, and race*time interactions. Model 3 further adjusted for neighborhood socioeconomic status (time-varying).
DISCUSSION
In this large longitudinal cohort of middle-aged and older adults, we found that baseline smoking prevalence was lower among participants living in neighborhoods with better neighborhood social environment compared to those in worse neighborhoods. Adjustment for neighborhood socioeconomic status slightly attenuated associations, but the composite score remained statistically significant. However, we found no evidence that neighborhood social environment was associated with a change in smoking risk over time. Finally, we found no association between neighborhood social environment and smoking intensity.
The association of neighborhood social environment with baseline smoking in our study aligns with prior cross-sectional work[8–10, 12, 13, 15, 34] and may reflect an influence of neighborhood context on earlier life smoking patterns. The finding of higher smoking prevalence among participants living in neighborhoods with worse social environment scores, and lack of association with changes over time, suggests that neighborhood social factors may be more relevant for smoking initiation than cessation/reduction. To date, few studies have examined the association of neighborhood context with smoking initiation, and those that have primarily concentrated on neighborhood socioeconomic status[35–37] and racial composition.[37] More research is needed in this area, particularly longitudinal studies examining the impact of social aspects of neighborhood environments on smoking initiation.
Our cross-sectional results indicate that smoking prevalence was negatively associated with domains representing neighborhood stressors (aesthetic quality and safety) but associations were weaker or null for social cohesion. These findings may suggest that environmental stressors play a larger role than social cohesion in smoking behavior among older adults. The former finding is consistent with past cross-sectional studies,[8–10, 12, 13, 15, 34] and the latter finding somewhat aligns with several prior studies that found positive associations between neighborhood social cohesion and smoking prevalence,[14–16, 21] although our results were weaker than seen in previous studies. Our results suggest that neighborhood safety and aesthetic quality may be more promising targets for neighborhood-level interventions than social cohesion.
Our finding that neighborhood social environment was not associated with changes in smoking status or intensity over time can be compared with only a few prior studies using longitudinal data to assess this association. Slopen et al found no association between neighborhood stress, a scale related to both safety and trust in the neighborhood, and smoking behavior change among a cohort of middle-aged U.S. adults.[23] In contrast, Fleisher et al analyzed a cohort of Mexican smokers (mean age: 40 years) and found positive associations between neighborhood social cohesion and both quit attempts and successful quitting.[18] However, the study by Fleisher et al included only 2 years of data and could not evaluate whether smoking behavior changes were sustained over a longer time period.
The MESA population included middle-aged and older adults, and prior studies have found older adults to have lower rates of smoking behavior changes (e.g. cessation, relapse) compared to younger adults,[38–40] suggesting smoking behavior is more stable in older populations. In addition, as our study population had a fairly low baseline smoking rate, and relatively few individuals quit over follow-up, results should be interpreted with caution. Further study is needed to examine whether neighborhood social environment is associated with smoking cessation and reduction in younger populations, where smoking behavior patterns may be less solidly established.
This study had several limitations. Smoking outcomes were based on self-report, which might have led to underreporting due to recall and social desirability biases. However, prior validation work in MESA has indicated that self-reported smoking is a reliable measure consistent with serum and urinary cotinine concentrations.[41] Although we adjusted for a large number of potential confounders, including neighborhood socioeconomic status, it is possible that residual confounding was present from factors such as community/social network smoking norms or individual-level motivation to quit smoking. In addition, we used a 1-mile buffer to calculate neighborhood social environment scores because that was how neighborhoods were defined to participants in the survey. However, it is possible that this scale may be larger than what participants perceived as their actual neighborhood, particularly in more deprived areas.[42] Finally, there was not enough variability in the exposure and outcome to evaluate associations of change in neighborhood social environment with changes in smoking over time.
Strengths of this study include the large, multi-ethnic sample and inclusion of up to twelve years of follow-up. Our measures of neighborhood social environment were based on perceptions of the social environment (derived from neighborhood surveys) and results may be different if objective measures were used instead (such as crime reports or direct observations of aesthetic quality). However, perceptions of the social environment may be the more salient measure as has been found in some work.[8, 11] In addition, the use of multiple neighborhood informants to measure neighborhood social environment is a more valid measurement of neighborhood characteristics than individual self-report.[43]
CONCLUSION
In summary, a better neighborhood social environment was associated with lower smoking prevalence, particularly for the domains of safety and aesthetic quality. Neighborhood social environment was not associated with changes in smoking behavior over time. Further study is needed to determine whether neighborhood social environment is associated with changes to smoking behavior in younger populations.
Supplementary Material
What is already known on this subject?
Social aspects of neighborhood environments such as safety/crime and social cohesion have been cross-sectionally associated with smoking. However, the association of neighborhood social environment with changes in smoking behavior over time, and of the overall neighborhood social context, have rarely been studied.
What this study adds?
Neighborhood social environment was associated with smoking at baseline, but not with changes over time. Results suggest that neighborhood social context influences whether older adults smoke, but not whether they quit smoking or reduce the number of cigarettes smoked per day.
Acknowledgments
The authors thank the other investigators, the staff, and the participants of the MESA study for their valuable contributions. A full list of participating MESA investigators and institutions can be found at http://www.mesa-nhlbi.org.
Funding Information: This research was partially supported by U.S. Department of Health and Human Services. National Institutes of Health (NIH), P60 MD002249-05 (National Institute of Minority Health and Health Disparities) and R01 HL071759 (National Heart, Lung, and Blood Institute [NHLBI]). Funding for the MESA parent study came from NIH NHLBI contracts: HHSN268201500003I, N01-HC-95159 through 95169, UL1-TR-000040 and UL1-TR-001079.
Footnotes
Competing Interests: Competing Interest: None declared.
Licence for Publication: The Corresponding Author has granted, on behalf of all authors, an exclusive licence on a worldwide basis to the BMJ Publishing Group Ltd to permit this article to be published in JECH and any other BMJPGL products and sublicences such use and exploit all subsidiary rights, as set out in BMJ’s licence (http://group.bmj.com/products/journals/instructions-for-authors/licence-forms).
References
- 1.Garrett BE, Dube SR, Trosclair A, et al. Cigarette smoking - United States, 1965–2008. MMWR supplements. 2011;60:109–13. [PubMed] [Google Scholar]
- 2.Agaku IT, King BA, Dube SR. Current cigarette smoking among adults - United States, 2005–2012. MMWR Morbidity and mortality weekly report. 2014;63:29–34. [PMC free article] [PubMed] [Google Scholar]
- 3.Diez Roux AV, Mair C. Neighborhoods and health. Annals of the New York Academy of Sciences. 2010;1186:125–45. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- 4.Cano MA, Wetter DW. Socioeconomic status and smoking cessation: neighborhood context as an underlying mechanism. Texas Heart Institute journal / from the Texas Heart Institute of St Luke’s Episcopal Hospital, Texas Children’s Hospital. 2014;41:309–10. doi: 10.14503/THIJ-14-4096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giskes K, van Lenthe FJ, Turrell G, et al. Smokers living in deprived areas are less likely to quit: a longitudinal follow-up. Tobacco control. 2006;15:485–9. doi: 10.1136/tc.2006.015750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chuang YC, Cubbin C, Ahn D, et al. Effects of neighbourhood socioeconomic status and convenience store concentration on individual level smoking. Journal of epidemiology and community health. 2005;59:568–73. doi: 10.1136/jech.2004.029041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Diez-Roux AV, Nieto FJ, Muntaner C, et al. Neighborhood environments and coronary heart disease: a multilevel analysis. Am J Epidemiol. 1997;146:48–63. doi: 10.1093/oxfordjournals.aje.a009191. [DOI] [PubMed] [Google Scholar]
- 8.Tseng M, Yeatts K, Millikan R, et al. Area-level characteristics and smoking in women. American journal of public health. 2001;91:1847–50. doi: 10.2105/ajph.91.11.1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ellaway A, Macintyre S. Are perceived neighbourhood problems associated with the likelihood of smoking? J Epidemiol Commun H. 2009;63:78–80. doi: 10.1136/jech.2007.068767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gary TL, Safford MM, Gerzoff RB, et al. Perception of neighborhood problems, health behaviors, and diabetes outcomes among adults with diabetes in managed care: the Translating Research Into Action for Diabetes (TRIAD) study. Diabetes care. 2008;31:273–8. doi: 10.2337/dc07-1111. [DOI] [PubMed] [Google Scholar]
- 11.Andrews JO, Mueller M, Newman SD, et al. The Association of Individual and Neighborhood Social Cohesion, Stressors, and Crime on Smoking Status Among African-American Women in Southeastern US Subsidized Housing Neighborhoods. Journal of urban health : bulletin of the New York Academy of Medicine. 2014 doi: 10.1007/s11524-014-9911-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Virtanen M, Kivimaki M, Kouvonen A, et al. Average household income, crime, and smoking behaviour in a local area: the Finnish 10-Town study. Social science & medicine. 2007;64:1904–13. doi: 10.1016/j.socscimed.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 13.Patterson F, Seravalli L, Hanlon A, et al. Neighborhood safety as a correlate of tobacco use in a sample of urban, pregnant women. Addictive behaviors. 2012;37:1132–7. doi: 10.1016/j.addbeh.2012.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin EY, Witten K, Casswell S, et al. Neighbourhood matters: perceptions of neighbourhood cohesiveness and associations with alcohol, cannabis and tobacco use. Drug and alcohol review. 2012;31:402–12. doi: 10.1111/j.1465-3362.2011.00385.x. [DOI] [PubMed] [Google Scholar]
- 15.Echeverria S, Diez-Roux AV, Shea S, et al. Associations of neighborhood problems and neighborhood social cohesion with mental health and health behaviors: the Multi-Ethnic Study of Atherosclerosis. Health Place. 2008;14:853–65. doi: 10.1016/j.healthplace.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Patterson JM, Eberly LE, Ding Y, et al. Associations of smoking prevalence with individual and area level social cohesion. J Epidemiol Community Health. 2004;58:692–7. doi: 10.1136/jech.2003.009167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Steptoe A, Feldman PJ. Neighborhood problems as sources of chronic stress: development of a measure of neighborhood problems, and associations with socioeconomic status and health. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine. 2001;23:177–85. doi: 10.1207/S15324796ABM2303_5. [DOI] [PubMed] [Google Scholar]
- 18.Fleischer NL, Lozano P, Arillo Santillan E, et al. The impact of neighbourhood violence and social cohesion on smoking behaviours among a cohort of smokers in Mexico. Journal of epidemiology and community health. 2015 doi: 10.1136/jech-2014-205115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sampson RJ, Morenoff JD, Gannon-Rowley T. Assessing “neighborhood effects”: Social processes and new directions in research. Annu Rev Sociol. 2002;28:443–78. [Google Scholar]
- 20.Kawachi I, Berkman LF. Social cohesion, social capital and health. In: Berkman LF, Kawachi I, editors. Social Epidemiology. New York: Oxford University Press; 2000. pp. 174–90. [Google Scholar]
- 21.Alcala HE, Sharif MZ, Albert SL. Social cohesion and the smoking behaviors of adults living with children. Addictive behaviors. 2016;53:201–5. doi: 10.1016/j.addbeh.2015.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reitzel LR, Kendzor DE, Castro Y, et al. The Relation between Social Cohesion and Smoking Cessation among Black Smokers, and the Potential Role of Psychosocial Mediators. Ann Behav Med. 2013;45:249–57. doi: 10.1007/s12160-012-9438-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Slopen N, Kontos EZ, Ryff CD, et al. Psychosocial stress and cigarette smoking persistence, cessation, and relapse over 9–10 years: a prospective study of middle-aged adults in the United States. Cancer causes & control : CCC. 2013;24:1849–63. doi: 10.1007/s10552-013-0262-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bild DE, Bluemke DA, Burke GL, et al. Multi-ethnic study of atherosclerosis: Objectives and design. Am J Epidemiol. 2002;156:871–81. doi: 10.1093/aje/kwf113. [DOI] [PubMed] [Google Scholar]
- 25.Mujahid MS, Diez Roux AV, Morenoff JD, et al. Assessing the measurement properties of neighborhood scales: from psychometrics to ecometrics. Am J Epidemiol. 2007;165:858–67. doi: 10.1093/aje/kwm040. [DOI] [PubMed] [Google Scholar]
- 26.Macleod J, Davey Smith G, Heslop P, et al. Psychological stress and cardiovascular disease: empirical demonstration of bias in a prospective observational study of Scottish men. Bmj. 2002;324:1247–51. doi: 10.1136/bmj.324.7348.1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Flowerdew R. How serious is the modifiable areal unit problem for analysis of English census data? Population trends. 2011:102–14. doi: 10.1057/pt.2011.20. [DOI] [PubMed] [Google Scholar]
- 28.Parenteau MP, Sawada MC. The modifiable areal unit problem (MAUP) in the relationship between exposure to NO2 and respiratory health. International journal of health geographics. 2011;10:58. doi: 10.1186/1476-072X-10-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Duncan DT, Piras G, Dunn EC, et al. The built environment and depressive symptoms among urban youth: A spatial regression study. Spat Spatiotemporal Epidemiol. 2013;5:11–25. doi: 10.1016/j.sste.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Diez Roux AV, Merkin SS, Arnett D, et al. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345:99–106. doi: 10.1056/NEJM200107123450205. [DOI] [PubMed] [Google Scholar]
- 31.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159:702–6. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 32.Zou GY, Donner A. Extension of the modified Poisson regression model to prospective studies with correlated binary data. Stat Methods Med Res. 2013;22:661–70. doi: 10.1177/0962280211427759. [DOI] [PubMed] [Google Scholar]
- 33.U.S. Department of Health and Human Services. The Health Consequences of Smoking -- 50 Years of Progress. A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 34.Peretti-Watel P, Seror V, Constance J, et al. Poverty as a smoking trap. International Journal of Drug Policy. 2009;20:230–6. doi: 10.1016/j.drugpo.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 35.Kravitz-Wirtz N. A discrete-time analysis of the effects of more prolonged exposure to neighborhood poverty on the risk of smoking initiation by age 25. Social science & medicine. 2016;148:79–92. doi: 10.1016/j.socscimed.2015.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kuipers MA, Wingen M, Stronks K, et al. Smoking initiation, continuation and prevalence in deprived urban areas compared to non-deprived urban areas in The Netherlands. Social science & medicine. 2013;87:132–7. doi: 10.1016/j.socscimed.2013.03.038. [DOI] [PubMed] [Google Scholar]
- 37.Reardon SF, Brennan RT, Buka SL. Estimating Multi-Level Discrete-Time Hazard Models Using Cross-Sectional Data: Neighborhood Effects on the Onset of Adolescent Cigarette Use. Multivariate behavioral research. 2002;37:297–330. doi: 10.1207/S15327906MBR3703_1. [DOI] [PubMed] [Google Scholar]
- 38.Quitting smoking among adults--United States, 2001–2010. MMWR Morbidity and mortality weekly report. 2011;60:1513–9. [PubMed] [Google Scholar]
- 39.Husten CG, Shelton DM, Chrismon JH, et al. Cigarette smoking and smoking cessation among older adults: United States, 1965–94. Tob Control. 1997;6:175–80. doi: 10.1136/tc.6.3.175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weinberger AH, Pilver CE, Mazure CM, et al. Stability of smoking status in the US population: a longitudinal investigation. Addiction. 2014;109:1541–53. doi: 10.1111/add.12647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hinckley Stukovsky K, Toennis CA, Sammons DL, et al. Measuring tobacco exposure in the Multi-Ethnic Study of Atherosclerosis (MESA). Poster presentation at the International Society for Environmental Epidemiology Annual Meeting; Seattle, WA. 2014. [Google Scholar]
- 42.Vallee J, Le Roux G, Chaix B, et al. The ‘constant size neighbourhood trap’ in accessibility and health studies. Urban Stud. 2015;52:338–57. [Google Scholar]
- 43.Mujahid MS, Diez Roux AV, Shen M, et al. Relation between neighborhood environments and obesity in the Multi-Ethnic Study of Atherosclerosis. Am J Epidemiol. 2008;167:1349–57. doi: 10.1093/aje/kwn047. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.