Abstract
Background
Burnout is generally perceived a unified disorder with homogeneous symptomatology across people (exhaustion, cynicism, and reduced professional efficacy). However, increasing evidence points to intra-individual patterns of burnout symptoms in non-clinical samples such as students, athletes, healthy, and burned-out employees. Different burnout subtypes might therefore exist. Yet, burnout subtypes based on burnout profiles have hardly been explored in clinical patients, and the samples investigated in previous studies were rather heterogeneous including patients with various physical, psychological, and social limitations, symptoms, and disabilities. Therefore, the aim of this study is to explore burnout subtypes based on burnout profiles in clinically diagnosed burnout patients enrolled in an employee rehabilitation program, and to investigate whether the subtypes differ in depression, recovery/resources-stress balance, and sociodemographic characteristics.
Methods
One hundred three patients (66 women, 37 men) with a clinical burnout diagnosis, who were enrolled in a 5 week employee rehabilitation program in two specialized psychosomatic clinics in Austria, completed a series of questionnaires including the Maslach Burnout Inventory – General Survey (MBI-GS), the Beck Depression Inventory, and the Recovery-Stress-Questionnaire for Work. Cluster analyses with the three MBI-GS subscales as clustering variables were used to identify the burnout subtypes. Subsequent multivariate/univariate analysis of variance and Pearson chi-square tests were performed to investigate differences in depression, recovery/resources-stress balance, and sociodemographic characteristics.
Results
Three different burnout subtypes were discovered: the exhausted subtype, the exhausted/cynical subtype, and the burned-out subtype. The burned-out subtype and the exhausted/cynical subtype showed both more severe depression symptoms and a worse recovery/resources-stress balance than the exhausted subtype. Furthermore, the burned-out subtype was more depressed than the exhausted/cynical subtype, but no difference was observed between these two subtypes with regard to perceived stress, recovery, and resources. Sociodemographic characteristics were not associated with the subtypes.
Conclusions
The present study indicates that there are different subtypes in clinical burnout patients (exhausted, exhausted/cynical, and burned-out), which might represent patients at different developmental stages in the burnout cycle. Future studies need to replicate the current findings, investigate the stability of the symptom patterns, and examine the efficacy of rehabilitation interventions in different subtypes.
Keywords: Burnout, Burnout subtypes, Burnout profiles, Person-oriented approach, Cluster analysis, Depression, Stress-recovery
Background
During the last decade, burnout has become a public health issue affecting between 4% and 7% of the working population [1]. Nevertheless, the diagnosis is not yet included in clinical classification systems such as the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) [2] or the International Statistical Classification of Diseases and Related Health Problems (ICD-10) [3]. To date, there is also no consensus on the definition of burnout and its core symptoms [4–7], and the diagnosis overlaps tremendously in symptomatology with other diagnoses, especially chronic fatigue [8] and depression [9–11].
Despite some conceptual controversies [4–7, 12], the most widely accepted definition of burnout is the one by Maslach, Schaufeli, and Leiter [6], who defined it as a work-related stress syndrome characterized by three main symptoms: exhaustion, cynicism, and reduced professional efficacy. Exhaustion refers to feelings of depletion caused by various work demands; cynicism reflects a distant attitude towards work and the people one is working with; and reduced professional efficacy represents the negative self-evaluation that one is incompetent and no longer able to perform work tasks adequately. However, past research has shown that burnout manifests in different ways. A varying number of burnout profiles [13–15] has been observed across studies, and multifaceted longitudinal trajectories of the burnout symptoms [16–21] indicate different pathways into burnout. Different burnout subtypes might therefore exist.
The person-oriented approach to burnout [15, 22] is one possibility to investigate burnout subtypes. It identifies different groups in a population that are intraindividually homogenous, but interindividually heterogeneous in various aspects such as symptomatology, psychopathology, and job- and person-related factors. In past research, the person-oriented approach has been used to identify typical burnout profiles [15], which might represent people at different developmental stages in the burnout cycle or truly different burnout subtypes [13, 23–27].
The most frequent burnout profiles that emerged in these studies [13–15], predominantly from the analysis of the three dimensions of the Maslach Burnout Inventory (MBI) [28], were the burned-out profile and the healthy or engaged profile representing people with severe or low symptomatology in all three burnout dimensions. Another common symptom profile was the exhausted/cynical profile characterized by high exhaustion and cynicism, but simultaneously high professional efficacy. Typical incongruent scoring patterns included the exhausted or overextended, the cynical or disengaged, and the reduced professional efficacy profile representing people with rather mild symptomatology where only one symptom is pronounced. However, one has to keep in mind that most previous studies have been conducted in non-clinical samples, which consist of people who report symptoms of a burnout but have not been diagnosed by a psychiatrist or clinical psychologist and who are all still working [13–15]. Therefore, the so-called healthy worker effect [29] occurred in these studies, and not all of the prior discussed burnout profiles might genuinely represent clinical burnout subtypes who need or seek treatment in specialized psychosomatic clinics or rehabilitation programs.
To date, only one study [30] has investigated subtypes based on burnout profiles in working-aged adults whose working ability was reduced or threatened by disease, disability or some other disorders, and who were therefore enrolled in an employee rehabilitation program. This study has identified four of the above mentioned subtypes: two subtypes with severe symptoms, namely the burned-out profile and the exhausted/cynical profile, one subtype with milder symptoms, namely the reduced professional efficacy profile, and the healthy profile. However, some of these profiles might have occurred because Hätinen et al. [30] explored a heterogeneous patient sample suffering from various physical, psychological, and social limitations, symptoms, and disabilities.
For that reason, the present study aims to examine whether meaningful burnout subtypes may be found in a more homogeneous group of clinically diagnosed burnout patients treated in a specialized psychosomatic clinic if the three main burnout symptoms suggested by Maslach, Schaufeli and Leiter [6] are considered and explored within a person-oriented approach [15]. Additionally, we will investigate the relationship of these subtypes to depression since an intense discussion has been going on during the last years [9–12, 31–54] whether burnout can be seen as a distinct construct or rather a new label of an already known state.
A growing body of literature has examined the overlap between burnout (subtypes) and depression-level, both in the working population [9, 12, 23, 31, 32, 39–48, 50–52] and in clinical patients [30, 54], but findings are heterogeneous and inconsistent. Several studies in the working population reported strong correlations between burnout and depression [9–11, 31, 32], especially between exhaustion and depression [10, 31, 32], while in clinically diagnosed burnout patients, the strong exhaustion-depression overlap could not be replicated [55]. Low to moderate correlations between burnout and depression were also found by others in the working population [40, 41, 47], whereas Ahola et al. [45] reported that burnout and depression overlapped particularly in severe burnout. These heterogeneous findings may partly result from using different measures of burnout and depression [11, 37] with some measures reflecting a larger concept redundancy between both disorders (for a discussion on this topic, see Maslach & Leiter [37]). Furthermore, longitudinal studies have been used to study the complex relationship between burnout and depression, but yielded inconsistent results as well. Some authors reported reciprocal relations between burnout and depression [42–44], while others found a unidirectional relationship from burnout to depression [46–50] or vice versa [51–53] or no predictive relation [36]. Studies applying a person-oriented approach to explore the burnout-depression overlap [9, 31] detected that burnout and depression were not separable from each other. Moreover, both disorders developed longitudinally in tandem supporting the hypothesis that burnout and depression may be the same disorder. In clinical burnout patients, longitudinal studies are still sparse [55]. Besides, only a few studies have explored the burnout-depression overlap by applying a person-oriented approach in clinical burnout patients [54] or burnout rehabilitation clients [30, 56], respectively. Yet, the overlap between burnout symptoms and depression might differ between burnout subtypes. Boersma and Lindblom [23] found in the working population that subtypes experiencing high exhaustion were more depressed than other burnout subtypes, and van Dam [54] could distinguish a group with mild symptoms from a group with severe symptoms on several measures (burnout, depression, anxiety, and fatigue) in clinically diagnosed burnout patients. In contrast, Hätinen et al. [30] found in working-aged rehabilitation clients that all subtypes were equally depressed, but in this study, a mixed patient sample suffering from various physiological, psychological, and social limitations, symptoms, and disabilities was explored.
Inconsistencies in organizational risk factors have been found in burnout subtypes as well. According to the job demands-resources (JD-R) model [57], burnout develops when job demands (e.g., workload, time pressure, conflict) are high, while resources (e.g., autonomy, social support, positive relationship with supervisor) are limited. Resources are therefore no longer able to buffer the negative impact of high demands on stress reactions [58]. Job demands and resources have also been linked to specific burnout symptoms: exhaustion is caused by high workload and emotional demands, whereas cynicism, reduced professional efficacy, and disengagement have been associated with a lack of resources [59–61]. Previous studies on burnout subtypes in the working population [13, 23, 27] likewise found that workload was high in subtypes experiencing high exhaustion (burned-out, exhausted/cynical, and exhausted), but resources were only low in subtypes with severe burnout symptoms (burned-out and exhausted/cynical), particularly in the burned-out subtype [13]. Yet, in clinical rehabilitation patients, Hätinen et al. [30] did not find any differences in job stressors and resources between three different burnout subtypes (burned-out, exhausted/cynical, and low professional efficacy), although recovery was associated with a decrease in job demands and an increase in job resources [56].
Because most prior research was conducted within the scope of the JD-R model of burnout, recovery has received comparatively less attention in relevant research. The recovery/resources-stress-balance model [62–64] is similar to the JD-R model but focusses additionally on recovery as crucial aspect to prevent burnout. According to the model, burnout develops after prolonged periods of stress without sufficient recovery and resources. More precisely, the homeostatic balance between stress and recovery is impaired because resources that were depleted during phases of stress are not adequately restored in the recovery phase [63]. The role of recovery has, however, not been systematically explored in burnout subtypes, particularly not in clinical burnout patients enrolled in an employee rehabilitation program.
Therefore, the current study aims to explore different burnout subtypes in clinical burnout patients, who are enrolled in an employee rehabilitation program in a psychosomatic clinic, by performing cluster analysis with the three subscales of the Maslach Burnout Inventory – General Survey (MBI-GS) [28] as clustering variables. Furthermore, depression levels will be compared among the subtypes, based on the expectation that the strength of the obviously existing overlap between burnout symptoms and depression might differ between burnout subtypes. Finally, differences between the burnout subtypes in the recovery/resources-stress balance and sociodemographic characteristics will be explored.
Methods
Study design and participants
This study used a person-oriented approach [15] to explore different subtypes based on burnout profiles in clinical burnout patients. A total of 103 patients (64% women) with a clinical burnout diagnosis were recruited from two specialized psychosomatic clinics in Austria. The patients were between 23 and 58 years old (M = 44.82 years, SD = 8.08) and had various educational backgrounds: 31% had a university degree or the A-level (high education), while 69% completed primary education, an apprenticeship or some other type of education or vocational training without the A-level (lower education).
Procedure
Burnout diagnosis was established by a team of psychiatrists and clinical psychologists. Since separate diagnostic codes for burnout are not yet included in clinical classification systems such as DSM-5 or ICD-10 [2, 3], the burnout diagnosis was based on the ICD-10 criteria of work-related neurasthenia, which has been proposed as the psychiatric equivalent of clinical burnout [38]. Similar to previous studies [54, 65], we included only patients that scored ≥2.20 on exhaustion and either ≥2.00 on cynicism or ≤3.67 on professional efficacy in the MBI-GS. Due to their burnout symptoms, all patients were enrolled in a 5 week employee rehabilitation program at the clinics, and they were on sick leave for at least 1 week prior to study admission (M = 106.20 days, SD = 113.46). Data were collected during the first week of the rehabilitation program and informed consent was obtained from all patients prior to participation. The study was in accordance with the 1964 Declaration of Helsinki and was approved by the ethics committee of the University of Graz, Austria.
Psychometric measures
Burnout
Burnout symptom severity was assessed with the German version [66] of the MBI-GS [28]. It has 16 items and consists of three subscales: exhaustion, cynicism, and reduced professional efficacy. The exhaustion subscale consists of five items (e.g., feeling emotionally drained from work), the cynicism subscale includes also five items (e.g., enthusiasm has decreased since work was started), and the professional efficacy subscale consists of six items (e.g., feeling that one gets done things effectively). The items are answered on a frequency rating scale ranging from 0 (never) to 6 (daily). Since all participants were on sick leave, they were instructed to respond to the items of the MBI-GS according to how they would feel if they were working at the moment.
Depression
The German version of the Beck Depression Inventory (BDI) was used to assess depression severity [67]. The BDI is a 21-item self-rating questionnaire that covers a variety of depressive symptoms along a continuum from 0 (absent or mild) to 3 (severe) symptoms. The BDI is widely used in treatment settings. A cut-off score ≥ 18 indicates a clinically relevant level of depression [68]. Additionally, all patients were screened for a past diagnosis of major depression using the Structured Clinical Interview for Axis I DSM-IV Disorders (SCID-I) [69].
Recovery/resources-stress balance
The Recovery-Stress-Questionnaire for Work (RESTQ-Work) is based on the recovery/resources-stress balance model [63] and consists overall of 92 items [62]. On a 7-point frequency rating scale ranging from 0 (never) to 6 (always), it measures the degree of stress and the extent of recovery and resources in the past 7 days/nights. The RESTQ-Work has seven subscales: social-emotional stress (e.g., being mentally stressed, irritated, and frequently in arguments with others), performance (−related) stress (e.g., time pressure, interruptions at work), loss of meaning/burnout (e.g., emotional exhaustion, loss of control, meaninglessness), overall recovery (e.g., physical recovery, relaxation, satisfying sleep), leisure/breaks (e.g., undisturbed leisure time without too many high-duty activities such as household chores, efficient breaks at work), psychosocial resources (e.g., social support from family, friends, and colleagues), and work-related resources (e.g., autonomy, participation, experience of personal growth). The RESTQ-Work displays good internal reliability and validity, and it has been used in burnout research before [58].
Statistical analyses
The burnout-depression overlap for the entire patient sample was analyzed using basic correlations and correlations corrected for attenuation [70] between the three MBI-GS subscales and the BDI score. To explore different burnout subtypes, cluster analyses [71] were performed. The three MBI-GS subscales (exhaustion, cynicism, and professional efficacy) served as the clustering variables and were standardized (z-score; M = 0, SD = 1) prior to the analyses. First, a hierarchical agglomerative cluster analysis with Ward’s method as a linkage method and squared Euclidean distance as a similarity measure was conducted. The optimal number of clusters was determined by the dendrogram, which is a visual illustration of how the individual cases are arranged into the clusters produced by hierarchical clustering. Next, a K-means cluster analysis was conducted to improve the cluster fit [71]. To identify burnout subtypes based on burnout profiles, the same approach has been applied by others as well [23, 30].
To describe the burnout subtypes further, one-way analyses of variance (ANOVAs) with the clusters as independent variable and the three MBI-GS subscales as dependent variables were conducted. Differences in depression between the subtypes were evaluated using Pearson’s chi-square tests (for BDI ≥ 18 and depression diagnosis in the past) and a one-way ANOVA. Differences between the subtypes in recovery/resources-stress balance were evaluated using a one-way MANOVA. In the ANOVAs and MANOVA, the clusters served as the independent variable, while the BDI and the seven RESTQ-Work subscales were the dependent variables, respectively. Sociodemographic differences between the subtypes were investigated with one-way ANOVAs (for age and days on sick leave) and Pearson’s chi-square tests (for gender, education, and rehabilitation clinic). In case of homogeneous variances, post-hoc comparisons were made with the Bonferroni test; in case of inhomogeneous variances, the Games-Howell test was used. Effect sizes are reported as partial eta-square (ηp2) indicating small (0.01 ≤ ηp2 < 0.06), medium (0.06 ≤ ηp2 < 0.14), and large (ηp2 ≥ 0.14) effects, respectively [72]. All statistical procedures were calculated in SPSS 24 and were performed with α = 0.05 (two-tailed).
Results
Burnout-depression overlap in the entire patient sample
To explore the burnout-depression overlap in the entire patient sample, basic correlations and correlations corrected for attenuation [70] between the MBI-GS subscales and the BDI were inspected (see Table 1). The three burnout subscales correlated moderately with depression. The highest correlation emerged between cynicism and depression (r = 0.41; p < 0.01), the lowest correlation occurred between exhaustion and depression (r = 0.30; p < 0.01). Regarding the correlations between the three MBI-GS subscales, both exhaustion and cynicism (r = 0.53; p < 0.01) and cynicism and professional efficacy (r = −0.51; p < 0.01) correlated strongly with each other, whereas a low correlation emerged between exhaustion and professional efficacy (r = −0.16; p = 0.10).
Table 1.
Cronbach’s alpha (α) and correlations (correlations corrected for attenuation are in italics) between the MBI-GS subscales and the BDI
| 1. | 2. | 3. | 4. | α | |
|---|---|---|---|---|---|
| 1. MBI – exhaustion | 1 | 0.53** | −0.16 | 0.30** | 0.86 |
| 2. MBI – cynicism | 0.65** | 1 | −0.51** | 0.41** | 0.77 |
| 3. MBI – professional efficacy | −0.20* | −0.66** | 1 | −0.35** | 0.78 |
| 4. BDI | 0.35** | 0.51** | −0.42** | 1 | 0.88 |
*p < 0.05; **p < 0.01
Burnout subtypes in clinically diagnosed burnout patients
Cluster analysis with the three MBI-GS subscales indicated two to four burnout subtypes in the present sample. In the two-cluster solution, cluster 1 and cluster 2 grouped together although the patients of cluster 2 had more severe burnout symptoms than the patients of cluster 1 (see Table 2). In the four-cluster solution, a cluster of patients with elevated burnout symptoms emerged that lay in between cluster 1 and cluster 2. However, since the four-cluster solution did not provide more conceptual clarity than the three-cluster solution, we considered the three-cluster solution representing three different burnout subtypes the best. Subsequent ANOVAs showed how the three subtypes differed in burnout symptomatology (see Table 2).
Table 2.
Differences between the burnout subtypes in burnout, depression, and recovery/resources-stress balance
| subtype 1 | subtype 2 | subtype 3 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| overall (N = 103) | exhausted (N = 34) | exhausted/ cynical (N = 39) | burned-out (N = 30) | ||||||||
| M | SD | M | SD | M | SD | M | SD | F(2,100) | ηp2 | contrasts | |
| MBI | |||||||||||
| exhaustion | 5.06 | 0.84 | 4.13 | 0.62 | 5.60 | 0.37 | 5.43 | 0.54 | 84.51** | 0.63 | 3,2 > 1 |
| cynicism | 4.13 | 1.01 | 3.28 | 0.71 | 4.17 | 0.85 | 5.03 | 0.63 | 43.84** | 0.47 | 3 > 2 > 1 |
| professional efficacy | 4.56 | 0.80 | 4.83 | 0.55 | 5.05 | 0.43 | 3.60 | 0.54 | 77.73** | 0.61 | 1,2 > 3 |
| BDI | |||||||||||
| depression | 21.46 | 9.65 | 16.41 | 8.68 | 21.31 | 8.74 | 27.39 | 8.69 | 12.70** | 0.20 | 3 > 2 > 1 |
| RESTQ-Work | |||||||||||
| social-emotional stress | 2.58 | 1.12 | 1.88 | 0.79 | 2.69 | 1.18 | 3.22 | 0.95 | 14.85** | 0.23 | 3,2 > 1 |
| performance (−related) stress | 3.08 | 1.10 | 2.32 | 0.92 | 3.32 | 0.94 | 3.63 | 1.03 | 16.96** | 0.25 | 3,2 > 1 |
| loss of meaning/burnout | 3.04 | 1.20 | 2.04 | 0.83 | 3.47 | 0.94 | 3.62 | 1.18 | 26.63** | 0.35 | 3,2 > 1 |
| overall recovery | 2.12 | 0.81 | 2.65 | 0.77 | 1.98 | 0.74 | 1.70 | 0.61 | 15.27** | 0.23 | 1 > 2,3 |
| leisure/breaks | 2.95 | 1.21 | 3.56 | 1.13 | 2.72 | 1.12 | 2.56 | 1.18 | 7.39** | 0.13 | 1 > 2,3 |
| psychosocial resources | 2.88 | 1.28 | 3.34 | 0.98 | 2.75 | 1.37 | 2.51 | 1.34 | 3.84* | 0.07 | 1 > 3 |
| work-related resources | 2.70 | 0.90 | 3.02 | 0.86 | 2.73 | 0.86 | 2.31 | 0.85 | 5.39** | 0.10 | 1 > 3 |
*p < 0.05; **p < 0.01
Figure 1 displays the symptom profile of the burnout subtypes graphically, both in z-scores and in mean scores. Each burnout subtype was described based on its mean score profile and based on which symptoms were most pronounced within the subtype. The three subtypes were labeled as follows: burned-out (subtype 3), exhausted/cynical (subtype 2), and exhausted (subtype 1). The burned-out subtype (n = 30) had the most severe burnout symptomatology. It displayed high exhaustion, high cynicism, and low professional efficacy. The exhausted/cynical subtype (n = 39) had severe burnout symptoms as well. It was characterized by high exhaustion, elevated levels of cynicism, but simultaneously high professional efficacy. Finally, the exhausted subtype (n = 34) showed the least severe burnout symptoms. It displayed elevated levels of exhaustion, the lowest scores on cynicism, and high professional efficacy.
Fig. 1.
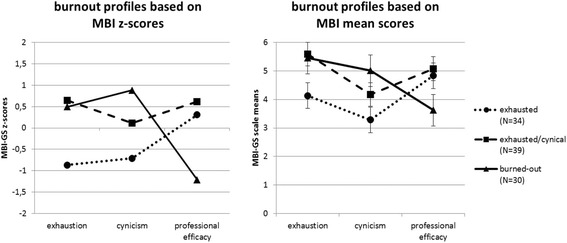
Burnout profiles based on MBI z-scores and based on MBI mean scores. a subtype 1 = exhausted; subtype 2 = exhausted/cynical; subtype 3 = burned-out. b post-hoc tests MBI-GS: exhaustion (burned-out subtype vs. exhausted subtype, p < 0.01; exhausted/cynical subtype vs. exhausted subtype, p < 0.01; burned-out subtype vs. exhausted/cynical subtype, p = 0.30); cynicism (burned-out subtype vs. exhausted subtype, p < 0.01; exhausted/cynical subtype vs. exhausted subtype, p < 0.01; burned-out subtype vs. exhausted/cynical, p < 0.01); professional efficacy (burned-out subtype vs. exhausted subtype, p < 0.01; exhausted/cynical subtype vs. exhausted subtype, p = 0.20; burned-out subtype vs. exhausted/cynical, p < 0.01).
Based on the z-score profile, the three subtypes could have been labeled as burned-out (subtype 3), exhausted (subtype 2), and healthy (subtype 1). However, we decided to label the subtypes based on the means score profile because of the general higher symptom severity in clinical burnout patients. Based on the z-score profile, particularly the label healthy for subtype 1 and the label exhausted for subtype 2 would have been misleading because both subtypes had elevated levels of exhaustion and subtype 2 had additionally elevated levels of cynicism. Hence, subtype 1 did not seem to be healthy and subtype 2 did not seem to be solely exhausted.
Level of depression in the burnout subtypes
Depression score was highest in the burned-out subtype, followed by the exhausted/cynical subtype, and the exhausted subtype (see Table 2; Bonferroni-corrected post-hoc tests: burned-out subtype vs. exhausted/cynical subtype, p = 0.02; burned-out subtype vs. exhausted subtype, p < 0.01; exhausted/cynical subtype vs. exhausted subtype, p = 0.05). Moreover, there were significant differences between the subtypes with regard to how many patients scored above the BDI cut-off score ≥ 18 for clinical depression (burned-out subtype: 27 patients (90%); exhausted/cynical subtype: 27 patients (69%); exhausted subtype: 14 patients (41%); χ2 (2, N = 103) = 17.22, p < 0.01). Concerning previous depression diagnosis, no significant difference was observed between the subtypes, χ2 (2, N = 103) = 0.77, p = 0.68, (see Table 3).
Table 3.
Sociodemographic characteristics of the burnout subtypes
| subtype 1 | subtype 2 | subtype 3 | |||
|---|---|---|---|---|---|
| overall (N = 103) | exhausted (N = 34) | exhausted/ cynical (N = 39) | burned-out (N = 30) | ||
| gender | female | 66 (64%) | 21 (32%) | 24 (36%) | 21 (32%) |
| male | 37 (36%) | 13 (35%) | 15 (41%) | 09 (24%) | |
| education | high | 32 (31%) | 08 (25%) | 12 (38%) | 12 (38%) |
| lower | 71 (69%) | 26 (37%) | 27 (38%) | 18 (25%) | |
| BDI ≥ 18 | yes | 68 (66%) | 14 (21%) | 27 (40%) | 27 (40%) |
| no | 35 (34%) | 20 (57%) | 12 (34%) | 03 (9%) | |
| depression diagnosis in the past | yes | 70 (68%) | 25 (36%) | 25 (36%) | 20 (29%) |
| no | 33 (32%) | 09 (27%) | 14 (42%) | 10 (30%) | |
| rehabilitation clinica | A | 51 (49%) | 15 (29%) | 21 (41%) | 15 (29%) |
| B | 52 (51%) | 19 (37%) | 18 (35%) | 15 (29%) | |
| age | M (SD) | 44.82 (8.08) | 44.96 (9.72) | 45.76 (6.26) | 43.43 (8.22) |
| days sick leave | M (SD) | 106.20 (113.46) | 73.65 (94.66) | 115.56 (104.04) | 130.93 (137.13) |
adata from two different rehabilitation clinics
Level of recovery/resources-stress balance in the burnout subtypes
The MANOVA showed significant differences in recovery/resources-stress balance between the three subtypes (using Pillai’s trace, V = 0.48, F(14, 190) = 4.33, p < 0.01, ηp2 = 0.24). Subsequent ANOVAs indicated significant differences in all seven RESTQ-Work subscales (see Table 2). Post-hoc analyses further revealed that both the burned-out and the exhausted/cynical subtype experienced significantly more social-emotional stress (p < 0.01), performance(−related) stress (p < 0.01), and loss of meaning/burnout (p < 0.01) as well as significantly less overall recovery (p < 0.01) and less leisure/breaks during work (p < 0.01) than the exhausted subtype. Furthermore, the burned-out subtype had significantly less psychosocial resources (p = 0.02) and less work-related resources (p < 0.01) than the exhausted subtype, while the burned-out and the exhausted/cynical subtype did not differ from each other in any of the RESTQ-Work subscales.
Sociodemographic characteristics of the burnout subtypes
Sociodemographic data for the burnout subtypes are presented in Table 3. There were no significant differences between the three subtypes with regard to sociodemographic characteristics. Men and women were equally distributed across the three clusters, χ2 (2, N = 103) = 0.65, p = 0.72, and the subtypes did not differ in age, F(2, 100) = 0.71, p = 0.50, and education, χ2 (2, N = 103) = 2.02, p = 0.36, respectively. The rehabilitation clinic was not significantly associated with the burnout subtype, χ2 (2, N = 103) = 0.69, p = 0.71, and there was no significant difference between the subtypes in how many days the patients had already been on sick leave prior to study admission, F(2, 100) = 2.30, p = 0.10.
Discussion
Burnout subtypes in clinical burnout patients
The present study explored different burnout subtypes based on MBI profiles in clinical burnout patients enrolled in an employee rehabilitation program in a psychosomatic clinic. As increasing evidence points to intra-individual patterns of burnout symptoms in non-clinical samples such as students, athletes, healthy and burned-out employees [13, 15], this study addressed the specific research question of whether different burnout subtypes can also be identified in clinically diagnosed burnout patients and whether these burnout subtypes differ in depression, recovery/resources-stress balance, and sociodemographic characteristics. Previously, van Dam [54] investigated subgroups in clinically diagnosed burnout patients by means of cluster analysis using fatigue (CIS), depression (SCL-90-D), and anxiety (SCL-90-A) as clustering variables and found two clusters that differed from one another in terms of symptom-severity on the three aforementioned measures. To date, only Hätinen et al. [30] have explored MBI burnout profiles in a mixed sample of working-aged rehabilitation clients, in which four different symptom patterns occurred: the burned-out profile, the exhausted/cynical profile, the reduced professional efficacy profile, and the healthy profile. However, some of these profiles might have occurred because Hätinen et al. [30] explored a heterogeneous patient sample suffering from various physical, psychological, and social limitations, symptoms, and disabilities. A study analyzing burnout subtypes in a group of clinically diagnosed burnout patients with the three MBI-GS dimensions (exhaustion, cynicism, professional efficacy) as clustering variables, is to the very best of our knowledge not available yet. Cluster analysis with the three MBI-GS subscales as clustering variables revealed three distinct burnout subtypes in the present study.
In line with Hätinen et al. [30], we found two subtypes with severe burnout symptoms, namely the burned-out and the exhausted/cynical subtype, whereas the reduced professional efficacy subtype and the healthy burnout profile could not be replicated in the present study. Instead, we identified an exhausted subtype representing patients with milder symptomatology. Sociodemographic characteristics were not systematically associated with the subtypes in the present study, but all groups differed in depression severity. The burned-out subtype showed overall the highest level of depression, while the exhausted subtype was the least depressed. Moreover, the burned-out and the exhausted/cynical subtype had a worse recovery/resources-stress balance compared to the exhausted subtype, but they did not differ from each in perceived stress, recovery, and resources. Since neither the depression scale, nor the RESTQ-Work subscales were used for clustering, these differences further support the validity of the cluster solution. Taken together our findings suggest that different burnout subtypes can be identified in clinical patients who were diagnosed with burnout by a professional team of psychiatrists and clinical psychologists working in a specialized psychosomatic clinic.
In line with past research [30, 54], our study indicates that the three subtypes represent patients at different stages in the burnout cycle. The subtypes correspond well with the process model of burnout [18], according to which burnout starts with exhaustion due to prolonged periods of stress, followed by cynicism as an attempt to cope with the intense emotional strain, before finally reduced professional efficacy occurs because a negative attitude towards one’s job precludes achieving work goals. Yet, it cannot be ruled out that the burned-out and the exhausted/cynical subtype might be truly different burnout subtypes, each characterizing the final stage in the burnout cycle. Several researchers have shown that professional efficacy develops rather independently of the other two burnout symptoms [21, 60], and both burnout profiles seem to be relatively stable over time [23]. Moreover, an alternative longitudinal trajectory of the burnout symptoms starting with reduced professional efficacy, followed by cynicism, and ending in emotional exhaustion, has been found as well [21]. The reduced professional efficacy subtype is a common subtype in the general working population [15], and two different pathways into burnout—one starting with exhaustion, the other one starting with reduced professional efficacy—have been addressed [13, 15, 24].
Truly different burnout subtypes might also explain why Hätinen et al. [30] found the reduced professional efficacy subtype, while the present study found the exhausted subtype representing patients with milder symptomatology, although the same methodology was applied in both studies, namely cluster analysis with the three MBI-GS subscales. Nevertheless, one has to keep in mind that our study sample markedly differed from the rehabilitation clients analyzed in the study by Hätinen et al. [30]. The present study solely included clinical burnout patients diagnosed with the ICD-10 criteria of work-related neurasthenia, which has been proposed as the psychiatric equivalent of clinical burnout [38]. In addition, all patients scored high on exhaustion (≥ 2.20) and either high on cynicism (≥ 2.00) or low on professional efficacy (≤ 3.67) in the MBI-GS [54, 65]. In contrast, Hätinen et al. [30] explored a mixed patient sample from an employee rehabilitation clinic suffering from various physical, psychological, and social limitations, symptoms, and disabilities. Patients with physical impairments displayed particularly the healthy burnout profile in their study, but physical impairments can lead to the experience of reduced professional efficacy as well, when one is no longer able to conduct one’s job properly.
Regarding the possible antecedents of burnout, we revealed that the three burnout subtypes in our study differed in their recovery/resources-stress balance. The two subtypes with severe burnout symptoms, namely the burned-out subtype and the exhausted/cynical subtype, experienced more social-emotional stress, performance(−related) stress, and loss of meaning in their job than the exhausted subtype. Both subtypes reported also the lowest overall recovery, leisure, and breaks during work. Furthermore, the burned-out subtype tended to have less psychosocial and work-related resources than the exhausted subtype. According to the JD-R model [57] and the recovery/resources-stress balance model [62–64], burnout develops due to high job demands and simultaneously low resources and recovery. Both would be necessary to buffer the negative effects of high job demands on stress reactions [58]. Our findings are in line with these assumptions, which have also received support in burnout subtypes in the working population [13, 23, 27] and in longitudinal studies in clinical rehabilitation clients [56]. Yet, the burned-out and the exhausted/cynical subtype did not differ in recovery/resources-stress balance from each other in the present study. This is in line with some previous studies [23, 30] but not with others [13] reporting that the burned-out subtype had even less organizational resources than the exhausted/cynical subtype. To clarify, whether the exhausted/cynical subtype and the burned-out subtype represent people at different developmental stages in the burnout cycle or truly different burnout subtypes, future studies should explore longitudinally which characteristics differentiate between these two subtypes.
Burnout-depression overlap
During the last years, an intense discussion has been going on whether burnout can be seen as a distinct construct or rather a new label of an already known state, and much of this debate has focused around the burnout-depression overlap [9–12, 31–54]. Until now, a vast majority of studies confirms that burnout and depression are not independent and especially in severe burnout, both disorders strongly overlap [11, 32, 45, 54]. This was also demonstrated in our own data. In the present study, 90% of the patients in the burned-out subtype scored above the BDI cut-off score ≥ 18 for clinical depression [68], whereas only 69% / 41% of the patients reached this threshold in the exhausted/cynical subtype and the exhausted subtype, respectively. Similarly, Ahola et al. [45] showed that 90% of people with severe burnout reported a physical or mental disease; more specifically, pain and depression. In contrast, Hätinen et al. [30] could not replicate these findings; the authors found that several burnout subtypes in rehabilitation clients were equally depressed. Yet, in their study, a mixed sample of rehabilitation clients suffering from various physiological, psychological, and social limitations, symptoms, and disorders was explored, while other studies [23, 54] using a person-oriented approach to explore burnout subtypes found that subtypes with severe burnout symptoms had higher depression scores than subtypes with milder burnout symptoms, which is in line with our study.
Interestingly, our results differed also from previous findings with regard to the burnout-depression overlap when the correlations between the three MBI-GS subscales and the BDI score were considered [9, 10, 31, 32]. For example, Bianchi et al. [10] found a high correlation between the MBI sum score and the BDI (r = 0.68) in the working population. Importantly, in their study, the correlation between emotional exhaustion and depression was much stronger (r = 0.74) than the correlations between the three dimensions of the MBI. Similar to the study of van Dam [54], the present study could not replicate such a strong correlation between exhaustion and depression (r = 0.30) in clinical burnout patients. For more than half a century [73], researchers have debated about the utility of using non-clinical samples such as students as analogues for patients with clinical diagnosis. Generalizing findings from non-clinical burnout samples to clinical burnout patients might therefore be problematic. However, another explanation for the lower correlation between exhaustion and depression in the present study and in the study of van Dam [54] might be that the range of exhaustion and depression scores is limited in clinical burnout patients, which might have flattened the correlation between both constructs. Furthermore, some of the heterogeneity in study results concerning the burnout-depression overlap may result from using different measures of burnout and depression [11, 12, 31, 32, 37, 40, 41, 47]. Hence, the high correlations between burnout and depression, especially with the burnout dimension emotional exhaustion in some studies, might partly reflect a large level of concept redundancy between specific burnout and depression measures (for a discussion on this topic, please see Maslach & Leiter [37]).
Especially longitudinal studies provide the opportunity to study the complex relationship between burnout and depression. Longitudinal studies focusing on the question whether burnout predicted depression or vice versa, revealed inconsistent results. Some authors [42–44] found a reciprocal relation between burnout and depression, with each predicting subsequent developments in the other, while other authors [46–50] reported a predictive relation from burnout to depression. Furthermore, three longitudinal studies showed a unidirectional relationship from depression to burnout [51–53] and one study failed to find any predictive relation [36]. Bianchi, Schonfeld and Laurent [31] focused on how burnout and depressive symptoms clustered at baseline and follow-up by applying a person-oriented approach. In this study, burnout was measured with a global burnout index (the combination of the MBI subscales emotional exhaustion and cynicism); depression was assessed with the Patient Health Questionnaire (PHQ-9). A similar person-oriented approach by using cluster analysis to study the relationship between burnout and depressive symptoms at baseline and over 7 years in dentists was applied by Ahola et al. [9]. Again, burnout was measured with a global index (more specifically, a weighted sum score of the MBI dimensions was calculated, so that emotional exhaustion, depersonalization, and diminished personal accomplishment had different weights in the syndrome); depressive symptoms were assessed using the short form of the Beck Depression Inventory (BDI-SF). In both studies, similar findings were obtained as both studies could show that the participants formed three clusters with low, intermediate, or high levels of burnout and depressive symptoms at baseline. Additionally, in both studies long-term development occurred in tandem, either remaining stable or changing in synchrony. Therefore, both studies support the hypothesis that burnout and depression overlap or may even be the same disorder.
Up to now, longitudinal studies in clinical burnout patients are still sparse. Oosterholt et al. [55] examined the course of cognitive performance and cortisol level in clinical burnout patients and non-clinical burnout individuals over a time period of 1.5 years. After 1.5 years, clinical burnout patients showed improvement of burnout symptoms and general physical and psychological complaints, but the patients still reported subjective cognitive impairments that were also evident in a cognitive test. In contrast, the non-clinical burnout group expressed the same elevated level of burnout symptoms, general physical and psychological complaints, and cognitive problems, but did not show objective cognitive deficits after 1.5 years.
Hätinen et al. [30] used a person-oriented approach to explore MBI burnout profiles and the changes in burnout 4 months after a rehabilitation intervention in a mixed sample of working-aged rehabilitation clients. In this study, four different burnout profiles (burned-out profile, exhausted/cynical profile, reduced professional efficacy profile, and healthy profile) were found and the burnout changes observed 4-month after the intervention depended on the burnout profile membership. While exhaustion showed a decreasing trend in the burned-out and exhausted/cynical profile, the decreasing trend in cynicism was only evident in the burned-out profile compared to the other profiles. Furthermore, reduced professional efficacy showed an increasing trend in the exhausted/cynical profile, whereas in the reduced professional efficacy profile the trend was decreasing. In a subsequent study, Hätinen et al. [56] investigated burnout trajectories in a one-year rehabilitation program with a six-month follow-up and found inter-individual changes in how clients reacted to the interventions and how these reactions were manifested in burnout symptoms during follow-up. The authors found three burnout patterns: two patterns with high levels of burnout and one pattern with low levels of burnout. However, only in one group with high burnout levels, exhaustion and cynicism were decreased at follow-up. This group was labeled as “high burnout-benefited trajectory” by the authors. For the “low burnout trajectory” and the “high burnout-benefited trajectory”, positive changes were detected in job-related antecedents (e.g., time pressure at work, job control, workplace climate) and consequences (e.g. depressive symptoms, job satisfaction). Thus, preliminary results suggest that in clinical burnout samples distinct symptom profiles exist and that not all burnout profiles benefit equally from rehabilitation in terms of reduction in burnout symptoms, job-related antecedents, and consequences [30, 56].
Practical implications
Burnout prevention/intervention programs in non-clinical burnout employees are either person-directed (individual level interventions), organization-directed or a combination of both [74]. Person-directed interventions usually consist of different kinds of relaxation exercises and/or cognitive behavioral techniques to enhance social support, job competence, and personal coping skills. Organization-directed interventions target on poor workplace climate, dissatisfaction with supervision, and changes in work procedures such as task restructuring. Furthermore, organization-directed interventions aim at decreasing job demand, increasing job control and expanding the level of participation in decision-making. Several reviews in non-clinical populations [74–77] concluded that burnout intervention programs had a beneficial effect on burnout outcome measures, especially when person-directed and organization-directed interventions were combined. Nonetheless, a recent meta-analysis [78] on the effectiveness of controlled interventions to reduce burnout indicated statistically significant effects of interventions only on general burnout scales (d = 0.224) and exhaustion (d = 0.172); no effect was observed on cynicism or professional inefficacy. Moreover, the reported effect sizes were overall rather small. Yet, most studies included in this meta-analysis investigated non-clinical burnout employees who do not necessarily possess a high level of burnout, since the interventions were aimed at decreasing the level of stress.
Studies assessing the efficacy of interventions in burnout patients who are treated in clinical settings are rare [30, 55, 56]. Preliminary results suggest that in clinical burnout samples distinct symptom profiles exist and that not all burnout profiles benefit equally from rehabilitation in terms of reduction in burnout symptoms, job-related antecedents, and consequences [30, 56]. For the burnout subtypes with severe symptomatology such as the exhausted/cynical and the burned-out subtype, the first step in rehabilitation should lie on the alleviation of the burnout and depression symptoms (e.g., psychotherapy and if indicated antidepressants). Additionally, rehabilitation should focus on organization-directed intervention activities in these subtypes, since burnout patients with severe symptomatology reported worse interpersonal relations, poor workplace climate, and dissatisfaction with supervision in previous studies [30]. Similarly, in our own study, the burned-out and the exhausted/cynical subtype experienced high social-emotional stress, performance-related stress and limited (work-related) resources. There is still an ongoing debate about the efficacy of antidepressants and psychotherapies in the treatment of subclinical depression, which is defined as a level of clinically relevant depressive symptoms in the absence of a major depressive disorder [79, 80]. Therefore, the exhausted subtype might profit from a person-directed approach focusing on factors contributing to exhaustion and recovery (e.g., interventions targeting workload, relaxation, and work-life balance [27]. In sum, identifying different subtypes of clinical burnout patients and analyzing the relationship of these subtypes to depression will enable psychiatrists and clinical psychologists to focus their intervention activities more effectively.
Study limitations
Several limitations of the current study need to be addressed. Similar to previous studies [54, 65], in the current paper the term clinical burnout is used to distinguish our study population of clinically diagnosed patients treated in a specialized psychosomatic clinic from non-clinical burnout groups who report symptoms of a burnout but are neither diagnosed by a psychiatrist or clinical psychologist as such and who are all still working. To date, there are no consensual diagnostic criteria for the burnout syndrome and the disorder is not yet included in clinical classification systems such as DSM-5 or ICD-10 [2, 3]. Therefore, in the current study, the burnout diagnosis was based on the ICD-10 criteria of work-related neurasthenia, which has been proposed as the psychiatric equivalent of clinical burnout [38]. Additionally, we included only patients who scored ≥2.20 on exhaustion and either ≥2.00 on cynicism or ≤3.67 on professional efficacy in the MBI-GS. Hence, the findings of our study might not be generalizable to clinical burnout patients who are diagnosed differently. An extensive discussion about the problem of simplification burnout to ICD-10/DSM-5 codes such as neurasthenia, somatic symptom disorder or exhaustion, can be found in a current review by Maslach and Leiter [37].
Furthermore, the patients in the present study were on average three and a half months on sick leave, and hence, a recall bias may have occurred; especially in patients who had been longer on sick leave. However, the burnout subtypes did not differ in how many days the patients had been on sick leave; thus, the distortion bias was at least equally distributed between the subtypes. Additionally, data were collected during the first week of the rehabilitation program. Therefore, it cannot be ruled out that the burnout profiles we found occurred because some patients already started benefiting from the positive effects of the rehabilitation program before they filled in the questionnaires. A further limitation of the present study is that the patients were not screened for comorbid psychiatric disorders using the Structured Clinical Interview for Axis I DSM-IV Disorders (SCID-I) [69] or the Mini-International Neuropsychiatric Interview (MINI) [81]. Therefore, we cannot ensure that comorbid disorder are equally divided over the burnout types. Finally, the analyses were based on cross-sectional report questionnaires. Hence, we were not able to investigate whether the exhausted/cynical and the burned-out subtype represent people at different developmental stages in the burnout cycle or truly different burnout subtypes. Due to the rather small sample size and different interventions in the two rehabilitation clinics, we were also not able to investigate if the three burnout subtypes responded differently to therapy.
Conclusions
In recent years, different burnout subtypes or profiles, based on cluster/profile analysis with the three MBI subscales, have been proposed by several research groups [13, 15]. However, until now, intra-individual patterns of burnout symptoms have primarily been investigated in non-clinical samples such as students, athletes, healthy, and burned-out employees. Therefore, the current study aimed to investigate whether different burnout subtypes can also be identified in a more homogeneous group of clinically diagnosed burnout patients enrolled in an employee rehabilitation program in a psychosomatic clinic. Our results provide evidence that in clinical burnout patients three different burnout subtypes can be revealed: the exhausted subtype, the exhausted/cynical subtype, and the burned-out subtype, which might represent patients at different developmental stages in the burnout cycle. Furthermore, the exhausted subtype displayed the lowest depression level and the best recovery/resources-stress balance, while the burned-out subtype exhibited the most severe depression symptoms and a worse recovery/resources-stress balance than the exhausted subtype. Clearly, the current findings need to be replicated in future studies involving larger, ideally longitudinal data sets to investigate the efficacy of rehabilitation interventions in different burnout subtypes and to track the stability and change patterns between the burnout subtypes over time.
Acknowledgements
We would like to thank two rehabilitation clinics in Austria for support in this research by permitting access to their burnout patients.
Funding
This work was supported by the Austrian Research Promotion Agency (Grant No. 827511/BULT).
Availability of data and materials
The authors confirm that some access restrictions apply to the data underlying the findings. The data set cannot be made publicly available because informed consent from study participants did not cover public deposition of data.
Abbreviations
- ANOVA
Analysis of variance
- BDI
Beck depression inventory
- BDI-SF
Beck depression inventory – short form
- CIS
Checklist individual strength
- DSM-5
Diagnostic and statistical manual of mental disorders
- ICD-10
International statistical classification of diseases and related health problems
- JD-R
Job demands-resources
- MANOVA
Multivariate analysis of variance
- MBI
Maslach burnout inventory
- MBI-GS
Maslach burnout inventory – general survey
- MINI
Mini-international neuropsychiatric interview
- PHQ-9
Patient health questionnaire
- RESTQ-Work
Recovery-stress-questionnaire for work
- SCID-I
Structured clinical interview for Axis I DSM-IV disorders
- SCL-90-A
Symptom checklist – anxiety subscale
- SCL-90-D
Symptom checklist – depression subscale
Authors’ contributions
KB, EW, MC and DB contributed in the conceptualization of the study. DB participated in collecting the data. KB conducted the statistical analyses, supported by MP and IP. KB drafted the manuscript, and EW, PJ, IP and AF contributed to the interpretation of the data. All authors revised the manuscript and gave final approval of the version to be published.
Ethics approval and consent to participate
The study was in accordance with the 1964 Declaration of Helsinki and was approved by the ethics committee of the University of Graz, Austria. Informed consent was obtained from all patients prior to participation. Data confidentiality was guaranteed and the patients were informed that they had the right to withdraw from the study at any time.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Kathrin Bauernhofer, Phone: +43 316-380-5126, Email: kathrin.bauernhofer@uni-graz.at.
Daniela Bassa, Email: daniela.bassa@edu.uni-graz.at.
Markus Canazei, Email: markus.canazei@bartenbach.com.
Paulino Jiménez, Email: paul.jimenez@uni-graz.at.
Manuela Paechter, Email: manuela.paechter@uni-graz.at.
Ilona Papousek, Email: ilona.papousek@uni-graz.at.
Andreas Fink, Email: andreas.fink@uni-graz.at.
Elisabeth M. Weiss, Email: e.weiss@uni-graz.at
References
- 1.Schaufeli W. Past performance and future perspectives of burnout research. SA J Ind Psychol. 2003;29:1–15. doi: 10.4102/sajip.v29i4.127. [DOI] [Google Scholar]
- 2.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 3.World Health Organization . The ICD-10 classification of mental and Behavioural disorders: diagnostic criteria for research. Geneva: World Health Organization; 1993. [Google Scholar]
- 4.Demerouti E, Bakker AB. The Oldenburg burnout inventory: a good alternative to measure burnout and engagement. In: Halbesleben JRB, editor. Handbook of stress and burnout in health care. Hauppauge, NY: Nova Science Publishers; 2008. pp. 65–78. [Google Scholar]
- 5.Kristensen TS, Borritz M, Villadsen E, Christensen KB. The Copenhagen burnout inventory: a new tool for the assessment of burnout. Work Stress. 2005;19:192–207. doi: 10.1080/02678370500297720. [DOI] [Google Scholar]
- 6.Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol. 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 7.Shirom A, Melamed S. A comparison of the construct validity of two burnout measures in two groups of professionals. Int J Stress Manag. 2006;13:176–200. doi: 10.1037/1072-5245.13.2.176. [DOI] [Google Scholar]
- 8.Huibers MJ, Beurskens AJ, Prins JB, Kant IJ, Bazelmans E, van Schayck CP, Knottnerus JA, Bleijenberg G. Fatigue, burnout, and chronic fatigue syndrome among employees on sick leave: do attributions make the difference? Occup Environ Med. 2003;60:26–31. doi: 10.1136/oem.60.suppl_1.i26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ahola K, Hakanen J, Perhoniemi R, Mutanen P. Relationship between burnout and depressive symptoms: a study using the person-centred approach. Burnout Res. 2014;1:29–37. doi: 10.1016/j.burn.2014.03.003. [DOI] [Google Scholar]
- 10.Bianchi R, Boffy C, Hingray C, Truchot D, Laurent E. Comparative symptomatology of burnout and depression. J Health Psychol. 2013;18:782–787. doi: 10.1177/1359105313481079. [DOI] [PubMed] [Google Scholar]
- 11.Bianchi R, Schonfeld IS, Laurent E. Burnout-depression overlap: a review. Clin Psychol Rev. 2015;36:28–41. doi: 10.1016/j.cpr.2015.01.004. [DOI] [PubMed] [Google Scholar]
- 12.Bianchi R, Schonfeld IS, Laurent E. Is burnout a depressive disorder? A reexamination with special focus on atypical depression. Int J Stress Manag. 2014;21:307–324. doi: 10.1037/a0037906. [DOI] [Google Scholar]
- 13.Leiter MP, Maslach C. Latent burnout profiles: a new approach to understanding the burnout experience. Burnout Res. 2016;3:89–100. doi: 10.1016/j.burn.2016.09.001. [DOI] [Google Scholar]
- 14.Maslach C, Leiter M. Early predictors of job burnout and engagement. J Appl Psychol. 2008;93:498–512. doi: 10.1037/0021-9010.93.3.498. [DOI] [PubMed] [Google Scholar]
- 15.Mäkikangas A, Kinnunen U. The person-oriented approach to burnout: a systematic review. Burnout Res. 2016;3:11–23. doi: 10.1016/j.burn.2015.12.002. [DOI] [Google Scholar]
- 16.Golembiewski RT, Munzenrider RF, Stevenson JG. Phases of burnout: developments in concepts and applications. New York: Praeger; 1986. [Google Scholar]
- 17.Friedman IA. Multiple pathways to burnout: cognitive and emotional scenarios in teacher burnout. Anxiety Stress Coping. 1996;9:245–259. doi: 10.1080/10615809608249405. [DOI] [Google Scholar]
- 18.Leiter MP, Maslach C. The impact of interpersonal environment of burnout and organizational commitment. J Organ Behav. 1988;9:297–308. doi: 10.1002/job.4030090402. [DOI] [Google Scholar]
- 19.Taris TW, Le Blanc PM, Schaufeli WB, Schreurs PJ. Are there causal relationships between the dimensions of the Maslach burnout inventory? A review and two longitudinal studies. Work Stress. 2005;19:238–255. doi: 10.1080/02678370500270453. [DOI] [Google Scholar]
- 20.Te Brake H, Smits N, Wicherts JM, Gorter RC, Hoogstraten J. Burnout development among dentists: a longitudinal study. Eur J Oral Sci. 2008;116:545–551. doi: 10.1111/j.1600-0722.2008.00584.x. [DOI] [PubMed] [Google Scholar]
- 21.van Dierendonck R, Schaufeli WB, Buunk BP. Toward a process model of burnout: results from a secondary analysis. Eur J Work Organ Psy. 2001;10:41–52. doi: 10.1080/13594320042000025. [DOI] [Google Scholar]
- 22.Bergman LR, Trost K. The person-oriented versus the variable-oriented approach: are they complementary, opposites, or exploring different worlds? Merrill Palmer Q. 2006;52:601–632. doi: 10.1353/mpq.2006.0023. [DOI] [Google Scholar]
- 23.Boersma K, Lindblom K. Stability and change in burnout profiles over time: a prospective study in the working population. Work Stress. 2009;23:264–283. doi: 10.1080/02678370903265860. [DOI] [Google Scholar]
- 24.Demerouti E, Verbeke WJ, Bakker AB. Exploring the relationship between a multidimensional and multifaceted burnout concept and self-rated performance. J Manage. 2005;31:186–209. [Google Scholar]
- 25.Innanen H, Tolvanen A, Salmela-Aro K. Burnout, work engagement and workaholism among highly educated employees: profiles, antecedents and outcomes. Burnout Res. 2014;1:38–49. doi: 10.1016/j.burn.2014.04.001. [DOI] [Google Scholar]
- 26.Lee SM, Cho SH, Kissinger D, Ogle NT. A typology of burnout in professional counselors. J Couns Dev. 2010;88:131–138. doi: 10.1002/j.1556-6678.2010.tb00001.x. [DOI] [Google Scholar]
- 27.Timms C, Brough P, Graham D. Burnt-out but engaged: the co-existence of psychological burnout and engagement. J Educ Adm. 2012;50:327–345. doi: 10.1108/09578231211223338. [DOI] [Google Scholar]
- 28.Maslach C, Jackson SE, Leiter M. Maslach burnout inventory. Manual. 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996. [Google Scholar]
- 29.Karasek R, Theorell T. Healthy work: stress, productivity and the reconstruction of working life. New York: Basic Books; 1990. [Google Scholar]
- 30.Hätinen M, Kinnunen U, Pekkonen M, Aro A. Burnout patterns in rehabilitation: short-term changes in job conditions, personal resources, and health. J Occup Health Psychol. 2004;9:220–237. doi: 10.1037/1076-8998.9.3.220. [DOI] [PubMed] [Google Scholar]
- 31.Bianchi R, Schonfeld IS, Laurent E. Is burnout separable from depression in cluster analysis? A longitudinal study. Soc Psychiatry Psychiatr Epidemiol. 2015;50:1005–1011. doi: 10.1007/s00127-014-0996-8. [DOI] [PubMed] [Google Scholar]
- 32.Schonfeld IS, Bianchi R. Burnout and depression: two entities or one? J Clin Psychol. 2016;72:22–37. doi: 10.1002/jclp.22229. [DOI] [PubMed] [Google Scholar]
- 33.Bianchi R, Schonfeld IS, Laurent E. Physician burnout is better conceptualised as depression. Lancet. 2017;389:1397–1398. doi: 10.1016/S0140-6736(17)30897-8. [DOI] [PubMed] [Google Scholar]
- 34.Bianchi R, Schonfeld IS, Laurent E. Burnout or depression: both individual and social issue. Lancet. 2017;390:230. doi: 10.1016/S0140-6736(17)31606-9. [DOI] [PubMed] [Google Scholar]
- 35.Bianchi R, Schonfeld IS, Vandel P, Laurent E. On the depressive nature of the “burnout syndrome”: a clarification. Eur Psychiatry. 2017;41:109–110. doi: 10.1016/j.eurpsy.2016.10.008. [DOI] [PubMed] [Google Scholar]
- 36.Bianchi R, Schonfeld IS, Laurent E. Burnout does not help predict depression among French schoolteachers. Scand J Work Environ Health. 2015;41:565–568. doi: 10.5271/sjweh.3522. [DOI] [PubMed] [Google Scholar]
- 37.Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. 2016;15:103–111. doi: 10.1002/wps.20311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schaufeli WB, Bakker AB, Hoogduin K, Schaap C, Kladler A. On the clinical validity of the Maslach burnout inventory and the burnout measure. Psychol Health. 2001;16:565–582. doi: 10.1080/08870440108405527. [DOI] [PubMed] [Google Scholar]
- 39.Schaufeli WB, Enzmann D. The burnout companion to study and practice: a critical analysis. London: Taylor and Francis; 1998. [Google Scholar]
- 40.Leiter MP, Durup J. The discriminant validity of burnout and depression: a confirmatory factor analytic study. Anxiety Stress Coping. 1994;7:357–373. doi: 10.1080/10615809408249357. [DOI] [Google Scholar]
- 41.Raedeke TD, Arce C, De Francisco C, Seoane G, Ferraces MJ. The construct validity of the Spanish version of the ABQ using a multi-trait/multi-method approach. Anales de Psi-cologia. 2012;29:693–700. [Google Scholar]
- 42.Ahola K, Hakanen J. Job strain, burnout, and depressive symptoms: a prospective study among dentists. J Affect Disord. 2007;104:103–110. doi: 10.1016/j.jad.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 43.McKnight JD, Glass DC. Perceptions of control, burnout, and depressive symptomatology: a replication and extension. J Consult Clin Psychol. 1995;63:490–494. doi: 10.1037/0022-006X.63.3.490. [DOI] [PubMed] [Google Scholar]
- 44.Toker S, Biron M. Job burnout and depression: unraveling their temporal relationship and considering the role of physical activity. J Appl Psychol. 2012;97:699–710. doi: 10.1037/a0026914. [DOI] [PubMed] [Google Scholar]
- 45.Ahola K, Honkonen T, Isometsä E, Kalimo R, Nykyri E, Aromaa A, Lönnqvist J. The relationship between job-related burnout and depressive disorders—results from the Finnish health 2000 study. J Affect Disord. 2005;88:55–62. doi: 10.1016/j.jad.2005.06.004. [DOI] [PubMed] [Google Scholar]
- 46.Armon G, Melamed S, Toker S, Berliner S, Shapira I. Joint effect of chronic medical illness and burnout on depressive symptoms among employed adults. Health Psychol. 2014;33:264–272. doi: 10.1037/a0033712. [DOI] [PubMed] [Google Scholar]
- 47.Hakanen JJ, Schaufeli WB. Do burnout and work engagement predict depressive symptoms and life satisfaction? A three-wave seven-year prospective study. J Affect Disord. 2012;141:415–424. doi: 10.1016/j.jad.2012.02.043. [DOI] [PubMed] [Google Scholar]
- 48.Hakanen JJ, Schaufeli WB, Ahola K. The job demands–resources model: a three-year cross-lagged study of burnout, depression, commitment, and work engagement. Work Stress. 2008;22:224–241. doi: 10.1080/02678370802379432. [DOI] [Google Scholar]
- 49.Salmela-Aro K, Savolainen H, Holopainen L. Depressive symptoms and school burnout during adolescence: evidence from two cross-lagged longitudinal studies. J Youth Adolesc. 2009;38:1316–1327. doi: 10.1007/s10964-008-9334-3. [DOI] [PubMed] [Google Scholar]
- 50.Shin H, Noh H, Jang Y, Park YM, Lee SM. A longitudinal examination of the relationship between teacher burnout and depression. J Employ Couns. 2013;50:124–137. doi: 10.1002/j.2161-1920.2013.00031.x. [DOI] [Google Scholar]
- 51.Armon G, Shirom A, Melamed S. The big five personality factors as predictors of changes across time in burnout and its facets. J Pers. 2012;80:403–427. doi: 10.1111/j.1467-6494.2011.00731.x. [DOI] [PubMed] [Google Scholar]
- 52.Campbell J, Prochazka AV, Yamashita T, Gopal R. Predictors of persistent burnout in internal medicine residents: a prospective cohort study. Acad Med. 2010;85:1630–1634. doi: 10.1097/ACM.0b013e3181f0c4e7. [DOI] [PubMed] [Google Scholar]
- 53.Salmela-Aro K, Aunola K, Nurmi JE. Trajectories of depressive symptoms during emerging adulthood: antecedents and consequences. Eur J Dev Psychol. 2008;5:439–465. doi: 10.1080/17405620600867014. [DOI] [Google Scholar]
- 54.van Dam A. Subgroup analysis in burnout: relations between fatigue, anxiety, and depression. Front Psychol. 2016; doi: 10.3389/fpsyg.2016.00090. [DOI] [PMC free article] [PubMed]
- 55.Oosterholt BG, Maes JH, van der Linden D, Verbraak MJ, Kompier MA. Getting better, but not well: a 1.5 year follow-up of cognitive performance and cortisol levels in clinical and non-clinical burnout. Biol Psychol. 2016;117:89–99. doi: 10.1016/j.biopsycho.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 56.Hätinen M, Kinnunen U, Mäkikangas A, Kalimo R, Tolvanen A, Pekkonen M. Burnout during a long-term rehabilitation: comparing low burnout, high burnout – benefited and high burnout – not benefited trajectories. Anxiety Stress Coping. 2009;22:341–360. doi: 10.1080/10615800802567023. [DOI] [PubMed] [Google Scholar]
- 57.Demerouti E, Bakker AB, Nachreiner F, Schaufeli WB. The job demands-resources model of burnout. J Appl Psychol. 2001;86:499–512. doi: 10.1037/0021-9010.86.3.499. [DOI] [PubMed] [Google Scholar]
- 58.Jiménez P, Dunkl A. The buffering effect of workplace resources on the relationship between the areas of worklife and burnout. Front Psychol. 2017; doi:10.3389/fpsyg.2017.00012. [DOI] [PMC free article] [PubMed]
- 59.Bakker AB, Demerouti E, Taris T, Schaufeli WB, Schreurs PJ. A multigroup analysis of the job demands-resources model in four home care organizations. Int J Stress Manag. 2003;10:16–38. doi: 10.1037/1072-5245.10.1.16. [DOI] [Google Scholar]
- 60.Lee RT, Ashforth BE. A meta-analytic examination of the correlates of the three dimensions of job burnout. J Appl Psychol. 1996;2:123–133. doi: 10.1037/0021-9010.81.2.123. [DOI] [PubMed] [Google Scholar]
- 61.Schaufeli WB, Bakker AB. Job demands, job resources, and their relationship with burnout and engagement: a multi-sample study. J Organ Behav. 2004;25:293–315. doi: 10.1002/job.248. [DOI] [Google Scholar]
- 62.Jiménez P, Dunkl A, Kallus KW. Recovery-stress questionnaire for work. In: Kallus KW, Kellmann M, editors. The recovery-stress questionnaire. User manual. Frankfurt/Main: Pearson; 2016. pp. 158–187. [Google Scholar]
- 63.Kallus KW. Stress and recovery: an overview. In: Kallus KW, Kellmann M, editors. The recovery-stress questionnaire. User manual. Frankfurt/Main: Pearson; 2016. pp. 27–48. [Google Scholar]
- 64.Kallus KW, Kellmann M. The recovery-stress questionnaire. User manual. Frankfurt/Main: Pearson; 2016. [Google Scholar]
- 65.Oosterholt BG, van der Linden D, Maes JH, Verbraak MJ, Kompier MA. Burned out cognition – cognitive functioning of burnout patients before and after a period with psychological treatment. Scand J Work Environ Health. 2012;38:358–369. doi: 10.5271/sjweh.3256. [DOI] [PubMed] [Google Scholar]
- 66.Büssing A, Glaser J. Managerial stress und burnout. A collaborative international study (CISMS). Die deutsche Untersuchung. [managerial stress and burnout. The German study]. Bericht nr. 44 aus dem Lehrstuhl für Psychologie. München: Technische Universität, Lehrstuhl für Psychologie; 1998. [Google Scholar]
- 67.Hautzinger M, Bailer M, Worall H, Keller F. Beck-Depressions-Inventar (BDI). Bearbeitung der deutschen Ausgabe. Testhandbuch. Bern, Göttingen, Toronto, Seattle: Huber; 1994. [Google Scholar]
- 68.Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck depression inventory: twenty-five years of evaluation. Clin Psychol Rev. 1988;8:77–100. doi: 10.1016/0272-7358(88)90050-5. [DOI] [Google Scholar]
- 69.First MB, Spitzer RL, Gibbon M, Williams JB. User’s guide for the structured clinical inter-view for DSM-IV interview for DSM-IV Axis I disorders. Washington, DC: Ameri-can Psychiatric Press; 1997. [Google Scholar]
- 70.Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. 3. Mahwah, NJ: Earlbaum; 2003. [Google Scholar]
- 71.Everitt BS, Landau S, Leese M, Stahl D. Cluster analysis. 5. Chichester, West Sussex: Wiley; 2011. [Google Scholar]
- 72.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- 73.Endler NS, Deisoff E, Rutherford A. Anxiety and depression: evidence for the differentiation of commonly cooccurring constructs. J Psychopathol Behav Assess. 1998;20:149–171. doi: 10.1023/A:1023026330644. [DOI] [Google Scholar]
- 74.Awa WL, Plaumann M, Walter U. Burnout prevention: a review of intervention programs. Patient Educ Couns. 2010;78:184–190. doi: 10.1016/j.pec.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 75.Ruotsalainen J, Serra C, Marine A, Verbeek J. Systematic review of interventions for reducing occupational stress in health care workers. Scand J Work Environ Health. 2008;34:169–178. doi: 10.5271/sjweh.1240. [DOI] [PubMed] [Google Scholar]
- 76.Walter U, Krugmann CS, Plaumann M. Preventing burnout? A systematic review of effectiveness of individual and comorbid approaches [German] Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2012;55:172–182. doi: 10.1007/s00103-011-1412-0. [DOI] [PubMed] [Google Scholar]
- 77.Westermann C, Kozak A, Harling M, Nienhaus A. Burnout intervention studies for inpatient elderly care nursing staff: systematic literature review. Int J Nurs Stud. 2014;51:63–71. doi: 10.1016/j.ijnurstu.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 78.Maricutoiu LP, Sava FA, Butta O. The effectiveness of controlled interventions on employees’ burnout: a meta-analysis. J Occup Organ Psychol. 2016;89:1–27.
- 79.Cameron IM, Reid IC, MacGillivray SA. Efficacy and tolerability of antidepressants for sub-threshold depression and for mild major depressive disorder. J Affect Disord. 2014;166:48–58. doi: 10.1016/j.jad.2014.04.078. [DOI] [PubMed] [Google Scholar]
- 80.Cuijpers P, Koole SL, van Dijke A, Roca M, Li J, Reynolds CF. Psychotherapy for subclinical depression: meta-analysis. Br J Psychiatry. 2014;205:268–274. doi: 10.1192/bjp.bp.113.138784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Herqueta T, Baker R, Dunbar GC. The Mini-international neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that some access restrictions apply to the data underlying the findings. The data set cannot be made publicly available because informed consent from study participants did not cover public deposition of data.


