Abstract
Objective
To evaluate the association of salt consumption with blood pressure in Viet Nam, a developing country with a high level of salt consumption.
Design and setting
Analysis of a nationally representative sample of Vietnamese adults 25–65 years of age who were surveyed using the World Health Organization STEPwise approach to Surveillance protocol. Participants who reported acute illness, pregnancy, or current use of antihypertensive medications were excluded. Daily salt consumption was estimated from fasting mid-morning spot urine samples. Associations of salt consumption with systolic blood pressure and prevalent hypertension were assessed using adjusted linear and generalized linear models. Interaction terms were tested to assess differences by age, smoking, alcohol consumption, and rural/urban status.
Results
The analysis included 2,333 participants (mean age: 37 years, 46% male, 33% urban). The average estimated salt consumption was 10g/day. No associations of salt consumption with blood pressure or prevalent hypertension were observed at a national scale in men or women. The associations did not differ in subgroups defined by age, smoking, or alcohol consumption; however, associations differed between urban and rural participants (p-value for interaction of urban/rural status with salt consumption, p = 0.02), suggesting that higher salt consumption may be associated with higher systolic blood pressure in urban residents but lower systolic blood pressure in rural residents.
Conclusions
Although there was no evidence of an association at a national level, associations of salt consumption with blood pressure differed between urban and rural residents in Viet Nam. The reasons for this differential association are not clear, and given the large rate of rural to urban migration experienced in Viet Nam, this topic warrants further investigation.
Introduction
While numerous epidemiological studies have reported an association between dietary salt intake and blood pressure, the majority of this evidence has come from developed countries.[1–3] Few studies on this topic have been conducted in developing countries, and those studies were focused on unique, geographically isolated populations with low levels of salt consumption.[2, 4–6] The impact of salt on blood pressure in developing countries with a high level of salt intake, such as those of South-east Asia, is unclear.[7, 8]
Viet Nam has undergone a period of rapid economic growth in the past 10–20 years, during which the country also experienced substantial rural to urban migration, increased tobacco use, the adoption of unhealthier diets, and decreased levels of physical activity.[8–12] These changes align with the “epidemiological transition,” the concept that as countries become more developed, the burden of disease shifts to chronic non-communicable diseases as the number of deaths from communicable diseases decreases and the average life expectancy increases.[13] Evidence from urban areas strongly suggests that the Vietnamese urban population is growing older and more obese, and that the prevalence of hypertension and diabetes is on the rise.[11, 12, 14, 15]
As a modifiable risk factor, salt consumption may be an appropriate target for public health interventions to lower population-wide blood pressure, which is hypothesized to lead to major improvements in public health.[1, 3, 16, 17] Although the cost of antihypertensive medications for an individual can be as little as pennies a day, salt reduction interventions are often cited as the most cost-effective means by which to lower population-wide blood pressure.[16, 18–20] Before any nation-wide salt reduction efforts are considered in Viet Nam, it is important to understand whether the effect of salt on blood pressure among Vietnamese is similar to that previously observed in developed countries.
Salt consumption is notoriously difficult to measure accurately, which has inhibited its investigation in resource-limited settings and developing countries.[3, 21] However, recent research has shown that a single spot urine collection can be used to provide useful estimates of salt intake in settings where multiple spot or 24-hour urine collections are not feasible.[22–27] We used spot urine sample data from a nationally representative population in Viet Nam to evaluate the association of salt intake with blood pressure and prevalent hypertension. We also assessed whether this association differed by age, smoking, alcohol consumption, or rural/urban residence.
Methods
Study population
The 2009 Viet Nam STEPwise approach to Surveillance (STEPS) survey is a cross-sectional study designed in accordance with World Health Organization (WHO) protocols to estimate the prevalence of key risk factors for non-communicable diseases among Vietnamese adults.[28] The 2009 Viet Nam STEPS design and recruitment are described in detail elsewhere.[29] Briefly, probability proportional to size sampling was used to select a nationally representative sample of 22,940 individuals aged 25–64 years from eight provinces, with each province representing a unique ecological region within Viet Nam. Between June and October 2009, trained interviewers conducted in-person interviews, and participants were invited to a clinic for a physical exam and blood and urine collection. A total of 14,706 Vietnamese adults completed an interview, physical examination, and blood collection; a spot urine sample was collected from a random subsample of 2,551 participants. Participants were excluded from this analysis if they reported acute illnesses or pregnancy, or if they reported current use of antihypertensive medications. This study was approved by the Viet Nam Ministry of Health Institutional Review Board, and participants provided written informed consent before participating.
Data collection
Each province recruited a data collection team of approximately 20 local medical personnel who were trained by staff from the WHO, the Viet Nam Non-Communicable Disease office, and consultants from the Menzies Research Institute. Survey clinics were set up at each commune in a location convenient to participants, such as the People’s Committee Office (the local government administration office) or health center. The times that clinics opened were adjusted for each area based on the activities of local participants, and varied between 6 and 7AM. Participants attended the clinic after overnight fasting.
Urine and blood samples were collected before participants ate breakfast. Samples were collected in standard containers, and were refrigerated as they were transported to the Viet Nam National Institute of Nutrition, where they were kept at -20 degrees Celsius until analyzed. The concentrations of sodium and creatinine in the urine were measured using an ion selective electrode method. Fasting blood glucose and total cholesterol were measured from capillary whole blood using Roche Diagnostics Accutrend Plus glucometers.
At the clinic visit, participants were administered an in-person questionnaire by a study interviewer. The questionnaire was adapted from the WHO STEPS instrument (version 2.1) that was translated into Vietnamese.[28] Topics covered included demographic information, tobacco and alcohol use, physical activity, and medical history (self-reported history of hypertension, diabetes, and medication use).
Height, weight, and waist and hip circumference measurements were taken with the participant in bare feet without headwear or heavy clothing. Blood pressure was measured using an Omron HEM 907 digital automatic blood pressure monitor after the participants had rested for at least 15 minutes. Two blood pressure measurements were taken; if they differed by more than 25/15mmHg then a third measurement was taken. The average of the last two blood pressure measurements was used in the analysis. Once per week measurement tools and equipment were inspected by study staff and recalibrated if needed.
Daily salt consumption estimation
Daily salt consumption was estimated from a fasting, mid-morning spot urine sample using a formula derived by Tanaka:[22]
eNa: Estimated 24-hour sodium excretion (mmol/day)
NaS: Sodium concentration in spot urine (mEq/L)
CrS: Creatinine concentration in spot urine (mg/L)
Pr.Cr24: estimated 24hr urinary Cr excretion (mg/day)
A validation study was conducted on a subsample of 154 participants between November and December 2010. Using the same collection protocol as described above, participants attended a study clinic after overnight fasting to provide mid-morning spot urine samples. At this point the participants began their 24-hour urine collections, and returned to the study clinic at the same time the following day to complete the 24-hour urine collection. After excluding eight incomplete or biologically implausible 24-hour urine samples (24-hour creatinine to body weight ratios that exceeded two standard deviations of the mean), spot urine based estimates of daily salt consumption were conservative (-12%; S1 Fig), but moderately correlated with 24-hour measured salt consumption (rho = 0.35).[30–32] In a sensitivity analysis, use of the Kawasaki formula had similar validity (rho = 0.34), but yielded higher estimated daily salt consumption than the Tanaka formula in this population (+15%; S2 Fig).[23]
Results are presented in terms of grams of salt intake (1 gram salt (sodium chloride) = 17.1mmol sodium). We excluded participants with estimated salt consumption levels that exceeded 3 standard deviations from the mean (less than 3 or more than 17 grams of salt per day).
Statistical methods
Associations of daily salt consumption with systolic blood pressure were assessed using adjusted linear regression models. Relative risk regression was used to directly estimate the relative risk of hypertension associated with daily salt consumption, using generalized linear models with a Poisson distribution and robust standard errors.[33] Models included adjustment terms for age, sex, height, weight, smoking, total cholesterol, diabetes, and physical inactivity. Prevalent hypertension was defined as systolic blood pressure ≥140mmHg or diastolic blood pressure ≥90mmHg, and diabetes was defined as fasting glucose ≥126mg/dL or use of diabetes medication in the previous two weeks. Smoking was defined as current use of tobacco products; alcohol use was defined as five or more alcoholic drinks per week. Physical inactivity was defined as not meeting any of the following three criteria: 30 minutes of moderate-intensity physical activity on at least 5 days every week, 20 minutes of vigorous-intensity physical activity on at least 3 days every week, or a combination of vigorous- and moderate-intensity physical activity that exceeds 600 metabolic equivalent (MET)-minutes per week.[34] Rural and urban classification was based on the commune’s rural/urban designation in the 2009 national census.
To evaluate differences in the association of salt intake with blood pressure and prevalent hypertension by age (<45 years vs. ≥45 years), smoking (non-current vs. current), alcohol use (<5 drinks/week vs. ≥5 drinks/week), and rural/urban status, we tested interaction terms between salt intake and each of these risk factors in separate models. Interaction models included the primary set of adjustment covariates, except the age interaction model, which did not include a continuous term for age. Interaction models for smoking and alcohol consumption models were restricted to men due to the infrequency of reported smoking (2%) and alcohol use (<1%) among women. As a sensitivity analysis, we repeated analyses of salt intake with blood pressure and hypertension using Kawasaki and INTERSALT estimated salt consumption. [23, 35]
Analyses were conducted with STATA version 11.2 using the svy procedure. All analyses used STEPS sample weights that adjust for non-coverage and unequal probabilities of selection; sample weights incorporated post-stratification weights, which were calculated for each age (25–34, 35–44, 45–54, and 55–65 years) and sex stratum within each province using data from the 2009 Viet Nam national census.[36] Standard errors were computed using a robust variance estimator to take into account the complex sample design.
Of the 2,551 participants who provided spot urine samples, 7 were pregnant, 133 reported use of antihypertensive medications in the previous two weeks, 54 had missing body size or blood pressure measurements, and 24 had implausible salt intake levels and were excluded, leaving data from 2,333 participants available for analysis.
Results
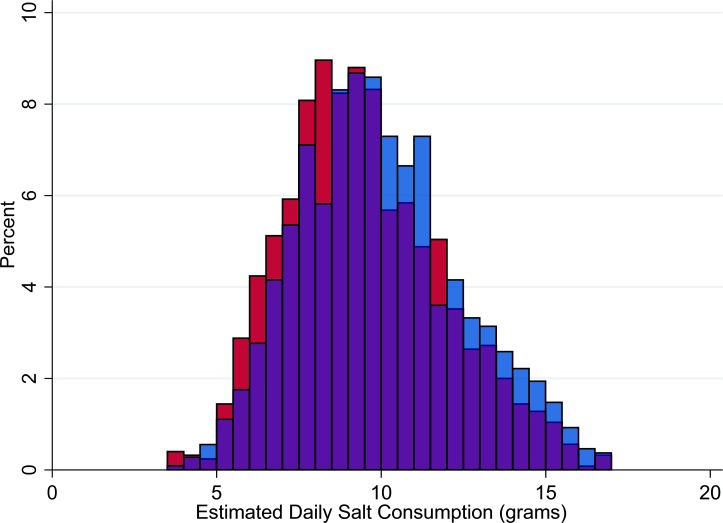
Characteristics of the 1,083 male and 1,250 female participants in the study are reported in Table 1. The average age of participants was 37 years and 11% had prevalent hypertension. On average, women were shorter, lighter, had lower blood pressure, and were less likely to smoke or drink alcohol than men. Participants consumed an average of 9.9 grams of salt per day, the distribution of which was relatively normal (Fig 1); 99% consumed more than the WHO recommended limit of 5 grams of salt per day.[37]
Table 1. Characteristics of 1,083 male and 1,250 female 25–64 year old participants in the 2009 Viet Nam STEPS survey.*.
| Men | Women | |||
|---|---|---|---|---|
| Mean or % | SE | Mean or % | SE | |
| Age (years) | 37 | 0.34 | 37 | 0.45 |
| Height (cm) | 163 | 0.38 | 153 | 0.31 |
| Weight (kg) | 59 | 1.06 | 50 | 0.46 |
| BMI (kg/m2) | 22 | 0.36 | 21 | 0.15 |
| Current smoker | 59% | 0.04 | 2% | 0.01 |
| ≥ 5 Alcoholic drinks/week | 15% | 0.02 | <1% | 0.00 |
| Physically inactive | 32% | 0.03 | 39% | 0.04 |
| Urban residence | 31% | 0.02 | 34% | 0.02 |
| Kinh ethnicity | 97% | 0.01 | 98% | 0.00 |
| Systolic BP (mmHg) | 123 | 0.95 | 113 | 0.88 |
| Diastolic BP (mmHg) | 75 | 0.80 | 70 | 0.67 |
| Hypertension | 15% | 0.02 | 5% | 0.01 |
| Fasting Glucose (mmol/L) | 4.2 | 0.11 | 3.9 | 0.05 |
| Diabetes | 12% | 0.03 | 9% | 0.02 |
| Total Cholesterol (mmol/L) | 4.7 | 0.05 | 4.7 | 0.05 |
| Estimated salt intake (g/day) | 10.2 | 0.19 | 9.5 | 0.15 |
*Nationally representative; weighted with sampling and post-stratification weights
Fig 1. Daily salt intake.
Blue = men. Red = women.
In sex-stratified models adjusted for age, height, weight, smoking, total cholesterol, diabetes, and physical inactivity, there was no evidence of an association of salt consumption with systolic blood pressure or prevalent hypertension (Table 2).
Table 2. Sex-stratified regression models of salt intake (g/day) with systolic blood pressure and prevalent hypertension.
| Minimally Adjusted Model* | Primary Model** | |||
|---|---|---|---|---|
| 95% CI | 95% CI | |||
| Systolic Blood Pressure (mmHg) | ||||
| Men | β = -0.20 | -1.03, 0.63 | β = -0.12 | -0.83, 0.58 |
| Women | β = 0.29 | -0.26, 0.84 | β = -0.06 | -0.73, 0.61 |
| Hypertension*** | ||||
| Men | RR = 0.94 | 0.79, 1.12 | RR = 0.97 | 0.87, 1.09 |
| Women | RR = 0.98 | 0.88, 1.09 | RR = 0.92 | 0.83, 1.02 |
*Includes age and body mass index as adjustment covariates
**Includes age, height, weight, smoking, total cholesterol, diabetes, and physical inactivity as adjustment covariates
***Systolic blood pressure ≥ 140mmHg or diastolic blood pressure ≥ 90mmHg
There was no evidence of an association of salt consumption with systolic blood pressure or prevalent hypertension in subgroups defined by age, smoking, alcohol consumption, or urban/rural residence (Table 3). Although we did not observe statistically significant associations of salt consumption with blood pressure within either urban or rural subgroups, there was evidence that these associations differed (p-value for interaction of urban/rural status with salt consumption, p = 0.02), which suggested that higher salt consumption may be associated with higher systolic blood pressure in urban participants but lower blood pressure in rural participants. While the mean systolic blood pressure was similar in urban and rural participants (119 vs. 118 mmHg, p = 0.79), salt consumption levels were slightly lower in urban residents than in rural residents (9.5 vs 10.1 g/day, p = 0.01). Restricting analyses to Kinh participants, using the Kawasaki or INTERSALT formulas to estimate salt intake, and including salt consumption levels that exceeded three standard deviations from the mean did not alter any of these findings (S3 Fig; S1, S2 and S3 Tables).
Table 3. Age-, smoking-, alcohol-, and rural/urban-stratified adjusted* regression models of salt intake (g/day) with systolic blood pressure and prevalent hypertension.
| Systolic Blood Pressure | Hypertension | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean Salt Intake (g/day) |
Mean (mmHg) |
β | 95% CI | p** | Prevalence | RR | 95% CI | p** | |
| Age*** | |||||||||
| <45 years | 10.0 | 117 | -0.08 | -0.67, 0.50 | 9% | 0.96 | 0.85, 1.10 | ||
| ≥45 years | 9.6 | 124 | 0.15 | -0.52, 0.81 | 0.58 | 18% | 0.97 | 0.89, 1.06 | 0.94 |
| Current smoker**** | |||||||||
| No | 10.3 | 124 | -0.04 | -0.85, 0.77 | 15% | 0.99 | 0.82, 1.20 | ||
| Yes | 10.2 | 123 | -0.30 | -1.26, 0.66 | 0.76 | 16% | 0.97 | 0.85, 1.11 | 0.95 |
| Alcohol consumption**** | |||||||||
| <5 drinks/week | 10.3 | 122 | 0.18 | -0.56, 0.93 | 14% | 1.00 | 0.88, 1.14 | ||
| ≥5 drinks/week | 9.7 | 129 | -0.49 | -1.46, 0.48 | 0.46 | 23% | 1.07 | 0.92, 1.24 | 0.71 |
| Place of residence | |||||||||
| Rural | 10.1 | 118 | -0.41 | -0.99, 0.17 | 10% | 0.92 | 0.82, 1.02 | ||
| Urban | 9.5 | 119 | 0.59 | -0.29, 1.46 | 0.02 | 12% | 1.01 | 0.86, 1.18 | 0.29 |
*Includes adjustment terms for age, sex, height, weight, smoking, total cholesterol, diabetes, and physical inactivity
**p-value for interaction
***Continuous age not included as an adjustment term
****Analyses restricted to men-only
Discussion
We observed that salt consumption was not associated with systolic blood pressure or the risk of prevalent hypertension at a national level in Viet Nam. We also observed that associations with systolic blood pressure differed between urban and rural participants, suggesting that higher salt consumption may be associated higher systolic blood pressure in urban residents but lower systolic blood pressure in rural residents in Viet Nam. However, associations in each subgroup were not statistically significant and may be due to chance.
To the best of our knowledge, this is the first study to examine the association of salt consumption with blood pressure at a national level in South-east Asia.[3, 7, 8] The national average estimated salt consumption level we observed (9.9g/day) was in line with levels recently reported in rural areas near Hanoi (8.5g/day to 10.8g/day).[38, 39] Our finding of no association of salt consumption with blood pressure at a national level contrasts with a recent meta-analysis of thirty-four trials in developed countries, which observed a positive association of salt intake with blood pressure (difference in systolic blood pressure (mmHg) per one-gram higher level of salt consumption; β = 0.95, 95%CI: 0.72, 1.18).[1] A recent South Korean national survey estimated daily sodium excretion from spot urine samples and reported an association of salt consumption with higher blood pressure; however, this study did not collect information on antihypertensive medication use and was not able to account for this in its analysis.[40] We did not observe the differential association of salt consumption with systolic blood pressure or hypertension by smoking status, alcohol consumption, or age that has been observed elsewhere.[2]
Reasons that salt consumption may have a different impact on the blood pressure of urban participants than of rural participants are not clear. The varying degree to which an individual’s blood pressure responds to changes in salt intake (“salt-sensitivity”) is largely driven by renal function.[41] A number of genetic factors have been found to impair renal function and are associated with salt-sensitivity.[42–45] Both rural and urban residents were predominantly Kinh ethnicity (98% and 96%, respectively; p = 0.23), and restricting analyses to Kinh participants did not alter our findings. Given that the rate of rural to urban migration from 1999 to 2010 increased by an average of 9.2% per year, and one-sixth of the urban population in 2009 had moved from rural areas in the past five years,[46] it would seem unlikely that genetic differences between rural and urban participants fully explain the stronger association of salt consumption with blood pressure in urban residents.
Apart from genetics, a number of other factors are associated with salt-sensitivity, including old age and diets low in potassium or calcium. [41, 42, 47–49] While we were able to adjust for age as a confounding variable, we were not able to adjust for dietary potassium or calcium, or for markers of renal function, as they were not measured in this survey. If these factors were more common among urban participants than rural participants, they could impair renal function (thereby increasing the salt-sensitivity) of urban residents more than rural residents, which could help explain the differential association of salt consumption with blood pressure by urban/rural status that we observed.
It is also possible that because rural participants were more likely to work in agriculture, they would lose more salt in sweat than urban participants due to the physical nature of their work and the hot climate of Viet Nam. Although there is a common perception that extra salt should be consumed to replace electrolytes lost due to perspiration, the amount of salt needed to maintain electrolyte balance in most conditions is actually quite low (approximately 0.6–1.2 grams per day for an average adult), so the amount consumed in this population far exceeded physiological need.[3, 50, 51] While some sodium is indeed secreted through perspiration, the amount is relatively small (0.6–4.1 grams per liter of sweat), with heat acclimated people on the low end of that spectrum.[21] Because the study population would be well acclimated to the heat and humidity, and because we adjusted for physical activity in our analyses, we do not have reason to believe that differential perspiration loss by rural/urban status influenced our findings.
Although many studies have documented a rise in blood pressure corresponding with rural to urban migration, few have examined the influence of salt on this association.[52, 53] A 1991 study of the Yi, an ethnic minority in southwestern China, collected blood pressure measurements and 24-hour urine samples from Yi farmers who lived in the rural mountains and Yi who had migrated to nearby urban centers.[4] Rural Yi farmers had low levels of salt consumption (5.6g/day) and one of the lowest average blood pressures in the world (98/60mmHg); both of which were lower than those of Yi urban migrants (9.3g/day, 107/69mmHg).[2] The study authors concluded that, due to the ethnic similarity of the urban migrants to the rural farmers, the higher blood pressure observed in the urban migrants was largely due lifestyle changes, including increased salt intake. A 1984 study of Kenyan rural to urban migrants provided similar findings.[5] In our population, rural participants had a slightly higher average level of salt consumption than urban participants, but the mean systolic blood pressure was similar in the two groups.
The cross-sectional nature of the study is a limitation of this analysis. Because we cannot assess whether salt consumption levels predated systolic blood pressure levels, we are only able to assess the correlation of salt consumption with blood pressure and prevalent hypertension, rather than causality. Another limitation is our use of an imperfect measure of salt consumption. Although 24-hour urine collection is the gold standard for estimating salt consumption in epidemiological studies, spot urine sample-derived estimates are a useful measure of salt consumption and are gaining popularity in large-scale epidemiological studies.[24, 26] Further, the levels of estimated daily salt consumption we observed were similar to those reported in region-specific studies of salt consumption in Viet Nam.[38, 39] However, deriving daily salt consumption from a single spot urine often results in overestimates among those at lower salt consumption levels and underestimates among those at higher salt consumption levels.[25, 30, 54] In our population where 99% consumed more than the WHO recommended limit of salt per day, use of spot urine may have underestimated daily salt consumption and impaired our ability to detect associations with blood pressure and hypertension, resulting in conservative estimates of the association of salt consumption with blood pressure and prevalent hypertension or an apparent lack of association where one may truly be present.[55] Finally, the relatively young upper age (64 years) of included participants inhibited our ability to assess associations among those at greatest risk of high blood pressure.
Conclusions
There was no evidence of an association of salt consumption with elevated systolic blood pressure at a national level in Viet Nam; however, the association of salt consumption with blood pressure differed in urban versus rural residents. The reasons for this differential association are not clear, and given the large rate of rural to urban migration experienced in Viet Nam, this topic warrants further investigation.
Supporting information
(TIF)
(TIF)
Blue = men. Red = women.
(TIF)
(DOCX)
(DOCX)
(DOCX)
(CSV)
(CSV)
Acknowledgments
The authors thank the study participants and staff, and the Viet Nam Ministry of Health for their important contributions.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
Funding to support data collection (TQB, TTTH, TLVN) was provided by The Atlantic Philanthropies Inc.; the sponsor had no role in the study design, data analysis, writing or preparation of the article, or decision to have it submitted for publication. Study authors had no association with the funding organization. http://www.atlanticphilanthropies.org/
References
- 1.He FJ, Li J, Macgregor GA. Effect of longer term modest salt reduction on blood pressure: Cochrane systematic review and meta-analysis of randomised trials. Bmj. 2013;346:f1325 Epub 2013/04/06. doi: 10.1136/bmj.f1325 . [DOI] [PubMed] [Google Scholar]
- 2.Intersalt: an international study of electrolyte excretion and blood pressure. Results for 24 hour urinary sodium and potassium excretion. Intersalt Cooperative Research Group. Bmj. 1988;297(6644):319–28. Epub 1988/07/30. ; PubMed Central PMCID: PMC1834069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown IJ, Tzoulaki I, Candeias V, Elliott P. Salt intakes around the world: implications for public health. Int J Epidemiol. 2009;38(3):791–813. Epub 2009/04/09. doi: 10.1093/ije/dyp139 . [DOI] [PubMed] [Google Scholar]
- 4.He J, Klag MJ, Whelton PK, Chen JY, Mo JP, Qian MC, et al. Migration, blood pressure pattern, and hypertension: the Yi Migrant Study. Am J Epidemiol. 1991;134(10):1085–101. Epub 1991/11/15. . [DOI] [PubMed] [Google Scholar]
- 5.Poulter N, Khaw KT, Hopwood BE, Mugambi M, Peart WS, Rose G, et al. Blood pressure and its correlates in an African tribe in urban and rural environments. J Epidemiol Community Health. 1984;38(3):181–5. Epub 1984/09/01. ; PubMed Central PMCID: PMC1052349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carvalho JJ, Baruzzi RG, Howard PF, Poulter N, Alpers MP, Franco LJ, et al. Blood pressure in four remote populations in the INTERSALT Study. Hypertension. 1989;14(3):238–46. Epub 1989/09/01. . [DOI] [PubMed] [Google Scholar]
- 7.Mohani S, Prabhakaranii D, Krishnaniii A, editors. Promoting populationwide salt reduction in the South-East Asia Region: current status and future directions. Regional Health Forum; 2013. [Google Scholar]
- 8.Dans A, Ng N, Varghese C, Tai ES, Firestone R, Bonita R. The rise of chronic non-communicable diseases in southeast Asia: time for action. Lancet. 2011;377(9766):680–9. Epub 2011/01/29. doi: 10.1016/S0140-6736(10)61506-1 . [DOI] [PubMed] [Google Scholar]
- 9.Thanh VT. Vietnam's trade liberalization and international economic integration: evolution, problems, and challenges. ASEAN Economic Bulletin; 2005:75–91. [Google Scholar]
- 10.Huyen DNTN, Tuan DBA. Vietnam's economic development: Opportunities and challenges towards the integration tendency.
- 11.Trinh OT, Nguyen ND, Dibley MJ, Phongsavan P, Bauman AE. The prevalence and correlates of physical inactivity among adults in Ho Chi Minh City. BMC Public Health. 2008;8:204 Epub 2008/06/11. doi: 10.1186/1471-2458-8-204 ; PubMed Central PMCID: PMC2435539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nguyen QN, Pham ST, Nguyen VL, Weinehall L, Bonita R, Byass P, et al. Time trends in blood pressure, body mass index and smoking in the Vietnamese population: a meta-analysis from multiple cross-sectional surveys. PLoS One. 2012;7(8):e42825 Epub 2012/08/23. doi: 10.1371/journal.pone.0042825 ; PubMed Central PMCID: PMC3415402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Omran AR. The epidemiologic transition. A theory of the epidemiology of population change. Milbank Mem Fund Q. 1971;49(4):509–38. Epub 1971/10/01. . [PubMed] [Google Scholar]
- 14.Trang NH, Hong TK, Dibley MJ. Cohort profile: Ho Chi Minh City Youth Cohort—changes in diet, physical activity, sedentary behaviour and relationship with overweight/obesity in adolescents. BMJ Open. 2012;2(1):e000362 Epub 2012/02/18. doi: 10.1136/bmjopen-2011-000362 ; PubMed Central PMCID: PMC3282290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cuong TQ, Dibley MJ, Bowe S, Hanh TT, Loan TT. Obesity in adults: an emerging problem in urban areas of Ho Chi Minh City, Vietnam. Eur J Clin Nutr. 2007;61(5):673–81. Epub 2006/12/14. doi: 10.1038/sj.ejcn.1602563 . [DOI] [PubMed] [Google Scholar]
- 16.Murray CJ, Lauer JA, Hutubessy RC, Niessen L, Tomijima N, Rodgers A, et al. Effectiveness and costs of interventions to lower systolic blood pressure and cholesterol: a global and regional analysis on reduction of cardiovascular-disease risk. Lancet. 2003;361(9359):717–25. Epub 2003/03/07. doi: 10.1016/S0140-6736(03)12655-4 . [DOI] [PubMed] [Google Scholar]
- 17.He FJ, MacGregor GA. Reducing population salt intake worldwide: from evidence to implementation. Prog Cardiovasc Dis. 2010;52(5):363–82. Epub 2010/03/17. doi: 10.1016/j.pcad.2009.12.006 . [DOI] [PubMed] [Google Scholar]
- 18.Wang G, Labarthe D. The cost-effectiveness of interventions designed to reduce sodium intake. J Hypertens. 2011;29(9):1693–9. Epub 2011/07/26. doi: 10.1097/HJH.0b013e328349ba18 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rubinstein A, Garcia Marti S, Souto A, Ferrante D, Augustovski F. Generalized cost-effectiveness analysis of a package of interventions to reduce cardiovascular disease in Buenos Aires, Argentina. Cost Eff Resour Alloc. 2009;7:10 Epub 2009/05/08. doi: 10.1186/1478-7547-7-10 ; PubMed Central PMCID: PMC2684068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Asaria P, Chisholm D, Mathers C, Ezzati M, Beaglehole R. Chronic disease prevention: health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet. 2007;370(9604):2044–53. Epub 2007/12/08. doi: 10.1016/S0140-6736(07)61698-5 . [DOI] [PubMed] [Google Scholar]
- 21.Ji C, Sykes L, Paul C, Dary O, Legetic B, Campbell NR, et al. Systematic review of studies comparing 24-hour and spot urine collections for estimating population salt intake. Rev Panam Salud Publica. 2012;32(4):307–15. Epub 2013/01/10. . [DOI] [PubMed] [Google Scholar]
- 22.Tanaka T, Okamura T, Miura K, Kadowaki T, Ueshima H, Nakagawa H, et al. A simple method to estimate populational 24-h urinary sodium and potassium excretion using a casual urine specimen. J Hum Hypertens. 2002;16(2):97–103. Epub 2002/02/19. doi: 10.1038/sj.jhh.1001307 . [DOI] [PubMed] [Google Scholar]
- 23.Kawasaki T, Itoh K, Uezono K, Sasaki H. A simple method for estimating 24 h urinary sodium and potassium excretion from second morning voiding urine specimen in adults. Clin Exp Pharmacol Physiol. 1993;20(1):7–14. . [DOI] [PubMed] [Google Scholar]
- 24.O'Donnell M, Mente A, Rangarajan S, McQueen MJ, Wang X, Liu L, et al. Urinary sodium and potassium excretion, mortality, and cardiovascular events. N Engl J Med. 2014;371(7):612–23. doi: 10.1056/NEJMoa1311889 . [DOI] [PubMed] [Google Scholar]
- 25.Huang L, Crino M, Wu JH, Woodward M, Barzi F, Land MA, et al. Mean population salt intake estimated from 24-h urine samples and spot urine samples: a systematic review and meta-analysis. Int J Epidemiol. 2016;45(1):239–50. Epub 2016/01/23. doi: 10.1093/ije/dyv313 . [DOI] [PubMed] [Google Scholar]
- 26.Mente A, O'Donnell MJ, Dagenais G, Wielgosz A, Lear SA, McQueen MJ, et al. Validation and comparison of three formulae to estimate sodium and potassium excretion from a single morning fasting urine compared to 24-h measures in 11 countries. J Hypertens. 2014;32(5):1005–14; discussion 15. doi: 10.1097/HJH.0000000000000122 . [DOI] [PubMed] [Google Scholar]
- 27.Mill JG, Rodrigues SL, Baldo MP, Malta DC, Szwarcwald CL. Validation study of the Tanaka and Kawasaki equations to estimate the daily sodium excretion by a spot urine sample. Rev Bras Epidemiol. 2015;18 Suppl 2:224–37. Epub 2016/03/24. doi: 10.1590/1980-5497201500060020 . [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. STEPwise approach to surveillance (STEPS) Geneva, Switzerland2012 [cited 2012 October 1]. Available from: http://www.who.int/chp/steps/en/.
- 29.Bui TV, Blizzard L, Luong KN, Truong Nle V, Tran BQ, Ha ST, et al. Declining Prevalence of Tobacco Smoking in Vietnam. Nicotine Tob Res. 2015;17(7):831–8. Epub 2014/10/22. doi: 10.1093/ntr/ntu202 . [DOI] [PubMed] [Google Scholar]
- 30.Mann SJ, Gerber LM. Estimation of 24-hour sodium excretion from spot urine samples. J Clin Hypertens (Greenwich). 2010;12(3):174–80. doi: 10.1111/j.1751-7176.2009.00241.x . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Liu K, Stamler J. Assessment of sodium intake in epidemiological studies on blood pressure. Ann Clin Res. 1984;16 Suppl 43:49–54. . [PubMed] [Google Scholar]
- 32.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1(8476):307–10. . [PubMed] [Google Scholar]
- 33.Lumley T, Kronmal R, Ma S. Relative risk regression in medical research: models, contrasts, estimators, and algorithms. Working Paper 293, UW Biostatistics Working Paper Series2006.
- 34.Hallal PC, Andersen LB, Bull FC, Guthold R, Haskell W, Ekelund U. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380(9838):247–57. Epub 2012/07/24. doi: 10.1016/S0140-6736(12)60646-1 . [DOI] [PubMed] [Google Scholar]
- 35.Elliott P, Brown IJ, Dyer AR, Chan Q, Ueshima H, Stamler J. Elliott et al. Respond to “Quantifying Urine Sodium Excretion”. American Journal of Epidemiology. 2013;177(11):1196–8. doi: 10.1093/aje/kwt065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Viet Nam Population and Housing Census 2009 [Internet]. 2009.
- 37.World Health Organization. Salt Reduction—Fact Sheet 2016. Available from: http://www.who.int/mediacentre/factsheets/fs393/en/.
- 38.Do HT, Santos JA, Trieu K, Petersen K, Le MB, Lai DT, et al. Effectiveness of a Communication for Behavioral Impact (COMBI) Intervention to Reduce Salt Intake in a Vietnamese Province Based on Estimations From Spot Urine Samples. J Clin Hypertens (Greenwich). 2016;18(11):1135–42. doi: 10.1111/jch.12884 ; PubMed Central PMCID: PMCPMC5129579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Do HTP. Hypertension in Vietnam: prevalence, risk groups and effects of salt substitution [PhD Thesis]: Wageningen University; 2014.
- 40.Oh J, Lee J, Koo HS, Kim S, Chin HJ. Estimated 24-hour urine sodium excretion is correlated with blood pressure in Korean population: 2009–2011 Korean National Health and Nutritional Examination Survey. J Korean Med Sci. 2014;29 Suppl 2:S109–16. doi: 10.3346/jkms.2014.29.S2.S109 ; PubMed Central PMCID: PMCPMC4194280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Weinberger MH. Salt sensitivity of blood pressure in humans. Hypertension. 1996;27(3 Pt 2):481–90. Epub 1996/03/01. . [DOI] [PubMed] [Google Scholar]
- 42.Sanada H, Jones JE, Jose PA. Genetics of salt-sensitive hypertension. Curr Hypertens Rep. 2011;13(1):55–66. Epub 2010/11/09. doi: 10.1007/s11906-010-0167-6 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Svetkey LP, McKeown SP, Wilson AF. Heritability of salt sensitivity in black Americans. Hypertension. 1996;28(5):854–8. Epub 1996/11/01. . [DOI] [PubMed] [Google Scholar]
- 44.Miller JZ, Weinberger MH, Christian JC, Daugherty SA. Familial resemblance in the blood pressure response to sodium restriction. Am J Epidemiol. 1987;126(5):822–30. Epub 1987/11/01. . [DOI] [PubMed] [Google Scholar]
- 45.Luft FC, Rankin LI, Bloch R, Weyman AE, Willis LR, Murray RH, et al. Cardiovascular and humoral responses to extremes of sodium intake in normal black and white men. Circulation. 1979;60(3):697–706. Epub 1979/09/01. . [DOI] [PubMed] [Google Scholar]
- 46.United Nations Population Fund. Vietnam Population and Housing Census 2009—Migration and Urbanization in Vietnam: Patterns, Trends and Differentials. 2011.
- 47.Kotchen TA, McCarron DA. Dietary electrolytes and blood pressure: a statement for healthcare professionals from the American Heart Association Nutrition Committee. Circulation. 1998;98(6):613–7. Epub 1998/08/26. . [DOI] [PubMed] [Google Scholar]
- 48.Sanders PW. Dietary salt intake, salt sensitivity, and cardiovascular health. Hypertension. 2009;53(3):442–5. Epub 2009/01/21. doi: 10.1161/HYPERTENSIONAHA.108.120303 ; PubMed Central PMCID: PMC2678240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mattson DL, Dwinell MR, Greene AS, Kwitek AE, Roman RJ, Jacob HJ, et al. Chromosome substitution reveals the genetic basis of Dahl salt-sensitive hypertension and renal disease. Am J Physiol Renal Physiol. 2008;295(3):F837–42. Epub 2008/07/26. doi: 10.1152/ajprenal.90341.2008 ; PubMed Central PMCID: PMC2536867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Meneely GR, Battarbee HD. High sodium-low potassium environment and hypertension. Am J Cardiol. 1976;38(6):768–85. Epub 1976/11/23. . [DOI] [PubMed] [Google Scholar]
- 51.Holbrook JT, Patterson KY, Bodner JE, Douglas LW, Veillon C, Kelsay JL, et al. Sodium and potassium intake and balance in adults consuming self-selected diets. Am J Clin Nutr. 1984;40(4):786–93. Epub 1984/10/01. [DOI] [PubMed] [Google Scholar]
- 52.Nadim A, Amini H, Malek-Afzali H. Blood pressure and rural—urban migration in Iran. Int J Epidemiol. 1978;7(2):131–8. Epub 1978/06/01. . [DOI] [PubMed] [Google Scholar]
- 53.Steffen PR, Smith TB, Larson M, Butler L. Acculturation to Western society as a risk factor for high blood pressure: a meta-analytic review. Psychosom Med. 2006;68(3):386–97. Epub 2006/06/02. doi: 10.1097/01.psy.0000221255.48190.32 . [DOI] [PubMed] [Google Scholar]
- 54.Cogswell ME, Wang CY, Chen TC, Pfeiffer CM, Elliott P, Gillespie CD, et al. Validity of predictive equations for 24-h urinary sodium excretion in adults aged 18–39 y. Am J Clin Nutr. 2013;98(6):1502–13. Epub 2013/09/21. doi: 10.3945/ajcn.113.059436 ; PubMed Central PMCID: PMCPMC3831536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.White E, Armstrong BK, Saracci R. Principles of exposure measurement in epidemiology: collecting, evaluating, and improving measures of disease risk factors. 2nd ed. Oxford; New York: Oxford University Press; 2008. xi, 428 p. p. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(TIF)
(TIF)
Blue = men. Red = women.
(TIF)
(DOCX)
(DOCX)
(DOCX)
(CSV)
(CSV)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.