Abstract
It is increasingly recognized that mental disorders are affected by both personal characteristics and environmental exposures. The built, natural, and social environments can either contribute to or buffer against metal disorders. Environmental exposure assessments related to mental health typically rely on neighborhoods within which people currently live. In this article, I call into question such neighborhood-based exposure assessments at one point in time, because human life unfolds over space and across time. To circumvent inappropriate exposure assessments and to better grasp the etiologies of mental disease, I argue that people are exposed to multiple health-supporting and harmful exposures not only during their daily lives, but also over the course of their lives. This article aims to lay a theoretical foundation elucidating the impact of dynamic environmental exposures on mental health outcomes. I examine, first, the possibilities and challenges for mental health research to integrate people's environmental exposures along their daily paths and, second, how exposures over people's residential history might affect mental health later in life. To push the borders of scientific inquiries, I stress that only such mobility-based approaches facilitate an exploration of exposure duration, exposure sequences, and exposure accumulation.
Keywords: Mental health, Spatial context, Exposure assessments, Dynamic exposures, Daily path, Residential life course, Geographic information system, Global positioning system, Register data
Graphical abstract
Highlights
-
•
The environmental context affects people's mental health.
-
•
Environmental exposure assessments are frequently restricted to the neighborhoods in which people currently live.
-
•
Dynamic exposures along people's daily paths may trigger mental disorders.
-
•
Exposures over people's residential history might affect mental health later in life.
-
•
Only dynamic exposure assessments enable the inclusion of the duration and sequence of exposures and risk accumulation over time.
1. Urban environments and mental health
Mental health is an integral aspect of people's capacity to live a fulfilling life (World Health Organization, 2013). However, mental disorders (e.g., anxiety, depression) are exceedingly prevalent (Wittchen et al., 2011): On a global scale, one out of five adults suffered from a mental disorder within the past year (Steel et al., 2014). With a lifetime prevalence of two out of seven adults, mental disorders make a significant contribution to the number of healthy years lost due to mental ill-health (Steel et al., 2014). Mental disorders not only have devastating consequences for people's quality of life, but also present striking challenges for health systems and cause significant economic losses (Bloom et al., 2011). Both research and policymakers have therefore identified the reduction of mental disorders as a key priority (World Health Organization, 2013, Wittchen et al., 2011).
Public concerns about mental health have prompted a large number of researchers to disentangle the underlying risk and protective factors. It seems that the predisposition of people toward mental disorders consists of genetic factors, demographic characteristics, socioeconomic conditions, traumatic events, lifestyle habits, etc. (Cairns et al., 2014, Franklin et al., 2017, Hawton et al., 2013, Lorant et al., 2003, Meng et al., 2017). It turns out that these individual factors are not the sole health influencing factors (Kestens et al., 2017). According to the socio-ecological model of health (Sallis et al., 2008), people's mental health behavior also shapes, and is shaped by, the socio-environmental context in which they live and/or are born and raised (Riva et al., 2007, Diez Roux and Mair, 2010, Mair et al., 2008, Blair et al., 2014; Tost et al., 2015). The socio-ecological model furthermore suggests that the environment – subsuming built, natural, and social environments – serves as a background factor that can trigger, reduce, or amplify the risk of suffering from a mental disorder. More recently, significant conceptual and methodological progress has been made concerning the role of place in general (Riva et al., 2007, Diez Roux and Mair, 2010, Blair et al., 2014), and how the urban environment affects the brain in particular (Tost et al., 2015). Along with this renewed interest in the urban environment, a differentiated understanding of environmental exposures emerged, namely that places constitute different physical environments while being shaped by social interaction (Kestens et al., 2017).
Whereas the aforementioned risk and protective factors are relatively well understood, how the built, natural, and social environments together affect mental disorders remains less clear (Tost et al., 2015, Stickley et al., 2017, Adli et al., 2017, Heinz et al., 2013, Peen et al., 2010, Prüss-Üstün and Corvalán, 2006, Nieuwenhuijsen, 2016). There is increasing evidence that the built environment (e.g., urban morphology, land use, and street layout) might be a determinant of mental health (Rao et al., 2007, Sarkar and Webster, 2017). Although the existing knowledge is inconclusive, and the individual environments were frequently studied in isolation (Mair et al., 2008, Weich et al., 2002, Evans, 2003, Saarloos et al., 2011, James et al., 2017), it seems that, for example, higher urban densities increase social interactions that may decrease the risk of psychotic disorders (Kawachi and Berkman, 2001). Neighborhoods with well-connected streets benefit from good neighborliness, thus increasing community ties and enhancing the degree of acquaintanceship (Duncan et al., 2013). Similarly, land-use diversity ensures that there are more destinations nearby (Miles et al., 2012). Both factors encourage active travel, which has antidepressant effects (Teychenne et al., 2008). Others have reported the opposite effect, namely that, for example, walkable neighborhoods increase depression risk, but variations across population groups are possible (James et al., 2017). The natural environment (i.e., green space and blue space) has received attention in the mental health literature, and accumulated findings suggest that greenness reduces stress and has restorative effects (Gascon et al., 2015, Hartig et al., 2014, Völker and Kistemann, 2011). There is evidence that strong social ties, a close family, etc. reduce the risk of mood disorders at the individual level (Mair et al., 2008, Hawton and van Heeringen, 2009), and that overcrowded places characterized by stressful urban living contribute to psychological stress (Tost et al., 2015, Berry, 2008).
Although these explanations seem intuitively plausible, empirical models utilizing either cross-sectional or longitudinal study designs are still controversial. The partly contradictory results might be traced back to the static conceptualizations of how place and environmental exposures are integrated, which is primarily done by means of administrative units thought to represent neighborhoods (Kwan, 2012, Kwan, 2013, Van Ham and Manley, 2012). Such static environmental exposure assessments are undoubtedly inappropriate, however, as they misleadingly assume that people do not move in space–time throughout a day or over their life course.
In this article, I therefore argue for a dynamic conceptualization of environmental exposures when exploring environment–mental health relations. Further, I stress the significance of advances in geotechnologies as well as the availability of register data with respect to the implementation of dynamic exposure assessments. As health policies are increasingly grounded in evidence-based research, dynamic exposure assessments that focus on people's daily mobility and residential trajectory are necessary as they may prevent a misspecification of the health-influencing context across space and over time (Park and Kwan, 2017).
The rest of the article is structured as follows. Section 2 promotes a switch from neighborhood-based conceptualizations of environmental exposures to mobility-based exposure assessments; Section 3 deals with the benefits of dynamic context specifications; Section 4 outlines challenges related to space–time exposure assessments; and Section 5 presents the conclusions.
2. From static to dynamic exposure assessments
2.1. Area-based exposure assessments
Although not consistently confirmed, urban living seems to affect mental health (Tost et al., 2015, Heinz et al., 2013, Gruebner et al., 2017a). For example, a meta-analysis confirmed that urbanization is a risk factor for several psychiatric disorders (e.g., mood and anxiety disorders) (Peen et al., 2010). However, research (Blüml et al., 2017, Helbich et al., 2015) remains on a coarse analytical scale focusing on intra-regional differences, which is too crude to explore how area-level urban environmental exposures correlate with mental health. As residential neighborhoods matter for health outcomes (Diez Roux and Mair, 2010, Macintyre and Ellaway, 2000, Sampson et al., 2002), it is reasonable to analyze mental health within cities on a detailed scale beyond the crude urban–rural dichotomy (Peen et al., 2010, Helbich et al., 2017, Liu et al., 2015). Inter-urban study designs markedly increase the conceptual and methodological complexity of analyses, as environmental exposures not only directly affect people's mental health, but also moderate other risk and protective factors.
Methodological advances in spatial analytics within the field of statistics and geographic information science have created new possibilities to link health data with environmental exposures by means of people's residential location. Here, it is traditionally assumed that the residential location and the surroundings affect people's mental health (Kwan, 2013). Administrative units thought to represent neighborhoods are frequently used to define the influential neighborhood by attaching aggregated environmental conditions to individuals (Riva et al., 2007, Diez Roux and Mair, 2010, Mair et al., 2008, Blair et al., 2014, Owen et al., 2016). Through the correlations between people nested within the same spatial unit, multilevel models are the gold standard when simultaneously examining the association between individual and area-based exposures on health outcomes, otherwise resulting in biased inference (Owen et al., 2016, Diez-Roux, 2000). Despite this progress in modeling, the area-level approach misleadingly indicates that the environmental context is static following a well-defined spatial extent. At least the following criticisms have been put forward concerning such a procedure: a) Administrative units are not intended to capture health exposures meaningfully (Flowerdew et al., 2008, Wheeler et al., 2012); b) it is assumed that people in a neighborhood have similar exposures, independent of their daily mobility patterns (Kwan, 2012, Chaix et al., 2013); and c) people living close to a neighborhood boundary are possibly more exposed to the neighboring context than to their own (Van Ham and Manley, 2012).
To circumvent the rigidity of administrative units, more individualized or eco-centered representations of environmental exposures have been proposed (Meng et al., 2017, Kestens et al., 2017, Berke et al., 2007). The geocoding capabilities of geographic information systems (GIS) can be used to pinpoint people's exact residential locations. Well-established procedures to delineate the health-influencing spatial environmental contexts are circular buffers centered on people's actual place of residence, or on accessibility measures reflecting areas that can be reached within a given walking or driving time along the street network (Helbich et al., 2017). Although this context operationalization added important details compared to neighborhoods, ignoring exposures beyond the residential location is regarded as problematic, as short- or long-term locational immobilities of people are still postulated (Cummins, 2007). This probably induces inaccuracies and a systematic bias in exposure assessments (Kwan, 2012, Hurvitz and Moudon, 2012).
Whereas area-based research was insightful in addressing the role of place within the constellation of health, static approaches gave impetus for dynamic individual assessment methods that consider exposures during people's day-to-day traveling (Kestens et al., 2017, Chaix et al., 2013, Perchoux et al., 2013, Sarkar et al., 2013) and changing exposures over their life course (Ben-Shlomo and Kuh, 2002, Lynch and Smith, 2005) due to residential moves (Leyland and Næss, 2009, Miltenburg and van der Meer, 2016, Musterd et al., 2012, Sharkey and Faber, 2014, Browning et al., 2016).
2.2. Exposures along people's daily activity places and their mobility path
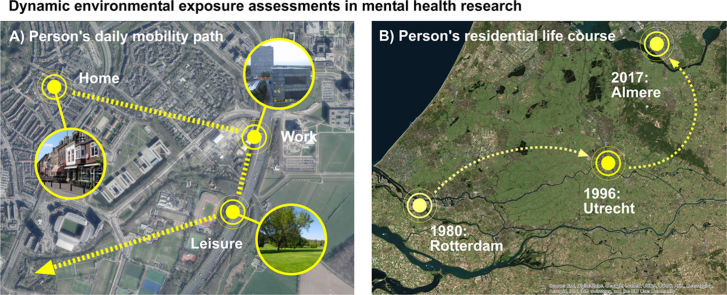
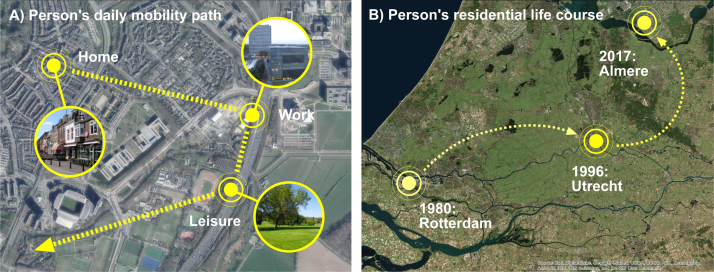
As most of daily life takes place at different places outside the home, people experience numerous exposures during their daily trajectories (Fig. 1A). From a theoretical view point, thinking of people's activity spaces – namely the multiple places people visit for their daily activities (e.g., work, leisure) (Schönfelder and Axhausen, 2003) and their daily paths connecting these activity places – offers a comprehensive framework to assess the mobility of individuals and their spatiotemporal exposure to environments (Dijst, 2009). The latter approach is rooted in time geography (Hägerstraand, 1970). It has been shown, for example, that 80% of people's daily activity space is outside their perceived neighborhood (Vallée et al., 2010), which emphasizes the incapacity of such a static approach to represent exposures that are etiologically meaningful (Basta et al., 2010). It is this visited and traversed environment that might increase people's vulnerability to mental disease. For example, it might be that people living in a less green area are more exposed to greenery on their daily paths and at activity locations, resulting in positive psychological effects (e.g., stress restoration) and thus a lower depression risk.
Fig. 1.
: Dynamic exposure assessments based on people's daily path (A) and people's residential trajectory (B).
Whereas data on the severity of people's mental health disorders can be collected relatively easily by means of self-complete, multiple-choice screeners such as the Patient Health Questionnaire (Spitzer et al., 1999), capturing precise spatiotemporal trajectories of the subjects is more challenging. Although travel and activity diaries (Axhausen et al., 2002) describe people's mobility in sufficient detail, their utilization is time consuming and labor intensive, particularly when a large sample is involved, as is common in epidemiology. As an alternative, global positioning system (GPS) tracking enables the automatic retrieval of precise and fine-grained geolocations and time information tracing people's space–time mobility without any human effort and in an objective manner (Richardson et al., 2013). GPS technology has at least the following advantages compared to traditional travel and activity diaries: a) The data captured through GPS are more accurate; b) GPS tracking provides information about route choice, travel speed, activity places, etc.; and c) it allows the tracking of a larger number of people without the need to conduct cost-intensive surveys and it reduces the burden on participants (Shen and Stopher, 2014). As a consequence, GPS tracking devices are receiving increased attention in both the mobility (Helbich et al., 2016) and the health field (Glasgow et al., 2016).
Due to the rapid diffusion of GPS in tandem with mobile technologies, GPS-enabled smartphones enable the capturing of massive amounts of people-related data in a noninvasive and near-real time manner under real-word conditions (Birenboim and Shoval, 2016). Due to high population penetration rates and the fact that people carry their smartphones during their daily lives, subjects do not need to wear additional GPS devices, which can affect their mobility behavior. Smartphones are not only communication devices: They are high-end technological platforms with computing power and they are equipped with rich in-built sensors (e.g., Bluetooth, Wi-Fi, microphone, motion, and ambient air temperature sensors) (Gravenhorst et al., 2015). Through passive sensing, an app can collect individual types of data (e.g., mobility data, accelerometer data, Bluetooth signals, and noise levels) in the background without any user interaction.
Three examples illustrate the utility of smartphones for mental health research. First, the integrated Bluetooth technology can be used to sense the crowdedness in the vicinity of people along their daily paths (Miluzzo et al., 2008, Eskes et al., 2016). Crowded public places are known to cause psychological distress (Evans, 2003, Berry, 2008). Compared to alternative approaches (e.g., cellphone handovers), Bluetooth technology allows real-time sensing and the development of indoor measures of crowdedness (e.g., on public transportation), and researchers do not have to rely on cellphone providers.
Second, place, social processes, and mental health are interlinked. As people's social networks and social interactions affect in which environments activities take place, most recent research argues that they should be considered jointly (Kestens et al., 2017). Although people's activity spaces might be constrained and spatiotemporally distinct from others, subjects can still be linked through sharing similar virtual social networks. In turn, the embeddedness in social networks can have health supporting effects while affecting people's spatial behavior (e.g., location choice) (Kawachi and Berkman, 2001, Larsen et al., 2006). Detailed data on where, with whom, and when people spatially and socially interact (e.g., phone usage, social media activities) are rarely collected, but smartphones offer a valuable source of such data. While enhancing social support and promoting the maintenance of personal relationships (Rettie, 2008), the frequency of incoming and outgoing calls was found to be, for example, a behavioral marker correlating with depression severity (Saeb et al., 2015, Thomée et al., 2011). In addition, online socializing has partly replaced face-to-face contacts and social interactions progressively occur on social media platforms (Hobbs et al., 2016). Logging social media behavior (e.g., Facebook check-ins, Tweets, WhatsApp messages) during daily life seems a promising way to record information about people's social connectedness and to explore how social networks dynamically change with place (Eagle et al., 2009). Furthermore, the social media content itself or the networks arising from followers provide a valuable source to contextualize place when analyzed through machine learning (Gruebner et al., 2017b, Conway and O’Connor, 2016).
Finally, although asking people about their subjective experiences (e.g., happiness) through an app-based a spatially or temporally triggered questionnaire, which is also referred to ecological momentary assessment (Shiffman et al., 2008), is widespread, continuous measurements are feasible by integrating wearable sensors with smartphones. Now that they have been miniaturized and embedded in wrist bands, skin patches, etc., these sensors are ideally suited to acquire, possibly georeferenced, bio-signals from the autonomic nervous system to investigate people's bodily reactions and mental states (e.g., electroencephalography) while they are moving (Kumari et al., 2017). Although the research possibilities for exposure assessments are rich, this technology is still in its infancy for mental health.
2.3. Exposures over people's residential life course
Aspects of the environmental context over people's residential history recently became a major research frontier potentially helping to explain mental health outcomes. The majority of studies, however, still consider environmental exposures only once at the actual place of residence as exposure source serving as a surrogate for all experienced exposures over time. However, as people move in to and out of different residential places (e.g., from Rotterdam to Utrecht, Fig. 1B) their living environment changes, as do the experienced environmental conditions that evolve and change dynamically over space–time (Sharkey and Faber, 2014, Brazil and Clark, 2017). This makes analyses at a single point in time problematic, as the history of exposures remains omitted; as a consequence, a substantial over- or underestimation of the true exposures may occur (Wheeler et al., 2012).
Therefore, the consideration of people's residential trajectory is an important element when studying long-term mental health outcomes (Leyland and Næss, 2009, Brazil and Clark, 2017, Meliker and Jacquez, 2007, Sabel et al., 2009). Suicide, for instance, has a long latency and develops over the lifetime (Hawton and van Heeringen, 2009). It might be that exposures at previous residential locations are more impactful than those at the current residential location. For example, moving from a high-poverty to a lower poverty neighborhood seems to improve long-term mental health (Brazil and Clark, 2017, Ludwig et al., 2012), but the short-term effects are minor (Tunstall et al., 2014). Consequently, there is ample need for dynamic exposure conceptualizations in mental health research.
Life course epidemiology (Ben-Shlomo and Kuh, 2002, Lynch and Smith, 2005, Niedzwiedz et al., 2012) explicitly recognizes the role of time in long-term exposure effects, and that different exposures operate over people's lives and their residential history. Within the life course approach, it is assumed, first, that exposures during a critical period of people's lives (e.g., during childhood) influence their vulnerability to psychotic disorders (Lynch and Smith, 2005). Second, it is emphasized that past exposures might have long-lasting consequences that are critical for people's health trajectory later in life (Pearce, 2014). Third, the life course approach facilitates the evaluation of how early and later risk factors accumulate over people's lives and how the sequence of different exposures affect mental health later in life (Pearce, 2014).
Although theoretically sound, there has been little transfer of the residential life course perspective to empirical studies (notable exceptions are, for example, Pearce et al. (2016), Veldman et al. (2017), Brazil and Clark (2017), and Brokamp et al. (2016)). One reason might be that studying earlier life exposures jointly over time is highly data intensive, calling not only for people's relocation history but also for precise time-varying environmental data to reconstruct past exposures. Given their quality and availability, register data offer vast resources for spatiotemporal epidemiological research (Erlangsen et al., 2017, Termorshuizen et al., 2014, Kunst et al., 2013) concerning the life course of people at a nationwide level. Key advantages of register-based data are their availability at a population level – which increases their statistical power and their availability over time – and that they reduce the potential for ecological fallacy in ecological study designs (Lyons et al., 2014). In the Netherlands, for example, the death register can be linked with the population register on an individual basis. The latter contains precise data on all residents since the mid 1990s, and includes people's residential locations. This ability to trace people's address history back in time in combination with the analytical power of GIS and the increasing availability of all kinds of high resolution environmental data, offers great potential for life course studies (Lyons et al., 2014) in general, and for reconstructing people's bio-geographical history as well as actual and past environmental exposures in particular.
A second reason why only a fraction of studies implement a life course approach, is that moving from models for a single point in time to models that take into account multiple time points while people are nested in multiple and changing spatial contexts, increases analytical complexity considerably (Owen et al., 2016). Leyland and Næss (2009) propose a) multiple membership models (i.e., exposures are constant over time), b) cross-classified modes (i.e., exposures are allowed to vary over time while assuming temporal independence), and c) correlated cross-classified models (i.e., adjusting for correlations over time to explore the contributions of accumulated effects) to address exposures over people's residential life courses. These life course oriented models can push health research forward.
3. What can be gained from dynamic exposure assessments?
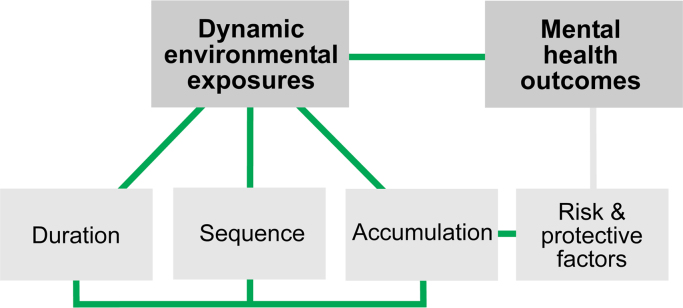
The reduction of mental disorders is recognized as a grand challenge for both research and health policy (World Health Organization, 2013). Despite extensive research on health–place relations, we have a limited understanding of the mechanisms that explain the role of dynamic environments in this constellation on a daily basis and over the life course. It seems rational that dynamic environments not only influence, but also mediate mental health outcomes. Fig. 2 illustrates the key mechanisms that can be explored through a dynamic conceptualization of place. Such mobility-based research designs put a strong emphasis on exposure duration, the exposure sequences, and the exposure accumulation.
Fig. 2.
: General mechanisms that explain dynamic environment–health associations.
A set of new hypotheses emerged as a consequence of rethinking space–time exposures. For example, studies can address the hypothesis that the daily environmental context to which people are exposed is associated with their mental health. It is expected that traversed environments, unlike static neighborhood-based exposures, have either beneficial or harmful effects on mental health outcomes, and that these exposures interact in a complex manner with each other as well as with people's individual characteristics. Given this premise, it seems certain that exposure sequences also matter. For example, people who are exposed to several health damaging exposures simultaneously at one place in time, or sequentially across several places over a longer period of time, might face an increased risk for mental disorders such as depression, as risk factors accumulate over time. Beyond a certain tipping point, people might not be able to cope with these exposures and depression symptoms are expected to be triggered. In contrast, people who are exposed alternately to health supporting and health deteriorating factors, might be able to recover from the latter and thus have a reduced disorder risk.
Considering multiple environmental conditions of the neighborhood in which a person lives at the time of diagnosis disregards movements between residential home locations, and a mental disorder develops over the life course. It is thus hypothesized that environmental exposures accumulate over time. Exposures around the actual home location are interrelated with past ones and moderate each other. For example, a lack of green space in previous residential neighborhoods might impede psychological stress reduction and increase depression risk. Besides the temporal order of exposures, it is assumed that abrupt changes in exposures have more pronounced effects on mental health outcomes later in life compared with gradual changes. Congruent with life course epidemiology, it is possible to assess how exposures arise throughout life. I posit that there are critical periods during which people are particularly vulnerable, resulting in pronounced mental health risk later in life.
Hypotheses such as these cannot be addressed without focusing on people's mobility over their residential histories and throughout their days. It is therefore vital for future research to add this temporal dimension comprising exposure duration, the sequence of exposures, and risk accumulation when analyzing environment–mental health associations. As the realization of dynamic environment–health research is a non-trivial task, it calls for combined transdisciplinary efforts between, for example, geographers, psychiatrist, computer scientists, and statisticians.
4. Challenges related to space–time exposures
Despite potential progress in dealing with environment–mental health associations, dynamic exposure assessments are not a panacea. Conducting such spatiotemporal health research is complex, and at least the following challenges warrant careful consideration.
First, since individual trips and exposures are not gathered directly though GPS, post-processing by means of GIS is required to distinguish between stationary activity places and conducted trips (Helbich et al., 2016, Maas et al., 2013). To determine the health-influencing exposures on a trip or around residential locations requires some GIS-based buffering. While decisions about buffer types (i.e., geometric or street network-based) and sizes are not supported by any theory, ad hoc approaches are widespread, even though comparative studies have highlighted significant differences across operationalizations (Burgoine et al., 2014, Wong et al., 2011).
Second, whereas life course studies are based on retrospective or prospective cohorts, studies that investigate day-to-day exposures are often cross-sectional, cannot address causality, and have limited ability to deal with residential self-selection issues; that is, people's individual characteristics influence their residential area choice (Riva et al., 2007, Mokhtarian and Cao, 2008, Galster and Hedman, 2013). However, individual-level variables can partly control for such confounding arising from residential self-selection (Riva et al., 2007). In any case, to support longitudinal research designs, repeated measures of the outcome variable over time are advised. Nevertheless, the retests with mental health screeners may introduce a measurement bias (Longwell and Truax, 2005). Closely related to the residential self-selection when utilizing GPS data is the selective daily mobility bias (Chaix et al., 2013): Environment–health associations could theoretically be confounded due to unobserved factors influencing health outcomes and the visiting of activity places (see Chaix et al. (2013) on how to mitigate the bias).
Third, to consider urban environmental exposures in an objective and transferable manner, dynamic exposure assessments are extremely data intensive and demand multi-temporal, high-resolution geodata, which is particularly challenging for long-term residential history analyses. Although some countries (e.g., the Netherlands) are pioneering in the availability of high-quality environmental data longitudinally, some retrospective data need to be restricted to specific timestamps. This means, for example, that environmental changes due to people's residential moves, but not the temporal changes per variable itself, are considered. Still, realizing dynamic exposures results in tons of data having different spatial and temporal granularities. This calls for longitudinal analytical approaches grounded in latent growth modeling (Jung and Wickrama, 2008), machine learning (Witten et al., 2016), etc. to efficiently process, mine, and draw inferences.
Fourth, a major, but predicted, challenge, as in any GPS study, could be a low participation rate. Given the involvement of mentally-ill people, the risk of dropouts is high. It is advised to start with a large sample and, when a priori knowledge about the expected effect sizes is available, conduct power calculations. Additionally, monetary incentives, apps and questionnaires originating from well-known institutions, etc. support higher participation rates (Edwards et al., 2002). Such strategies provide the increased statistical power necessary to conduct advanced statistical modeling while controlling for confounding factors.
Finally, as such studies involve sensitive personal information and mobility data, privacy protection is paramount. Data storing and processing needs to be done within a secure IT environment that has effective protection conditions. To safeguard subjects’ privacy (including their location privacy) and to ensure secure and confidential data management, information security specialists should periodically monitor and audit studies. Ethical approval must, of course, be obtained; however, the above safeguards allow research to be carried out in an ethically sound way.
5. Conclusions
There is renewed interest in how place shapes people's mental health, and the conceptual and methodological focus has shifted from static toward dynamic exposures assessments. Exposures at people's daily activity places and along their daily paths, as well as over their residential histories, are increasingly recognized as determinants of mental health. Through the former it is possible to address whether the traversed environment may serve as trigger for an onset of mental disorder. A residential life course perspective greatly facilitates addressing whether past environmental exposures may contribute to mental health disorders later in life. Such refinements toward dynamic exposure assessments provide much needed answers to several pressing questions, such as how people's mental health is affected by the duration, sequences, and accumulation of environmental exposures across space and over time. As I argued in this article, it is vital to add this temporal dimension, because such questions cannot be answered without focusing on people's mobility.
Methodological progress in dynamic exposure assessment can be made through nationwide register linkages at an individual level, and the application of cutting-edge smartphone-based GPS tracking, GIS analytics, and environmental sensing. Future studies are encouraged to implement dynamic exposures assessments; simply going beyond static exposures may prevent exposure misspecifications. The foundations laid in such research will likely reveal comprehensive insights into etiologies of mental disease that may lead, in turn, to alternative health policy supporting healthier urban living.
Acknowledgements
I thank all my colleagues for their constructive comments on earlier drafts of this article. Their remarks greatly improved the research protocol. In memoriam of Rudi.
Acknowledgments
Funding
This project has received funding from the European Research Council (ERC) under the European Union's Horizon 2020 research and innovation program (Grant agreement no 714993).
References
- World Health Organization . WHO; Switzerland: 2013. Investing in Mental Health: Evidence for Action. [Google Scholar]
- Wittchen H.-U., Jacobi F., Rehm J. The size and burden of mental disorders and other disorders of the brain in Europe 2010. Eur Neuropsychopharmacology. 2011;21:655–679. doi: 10.1016/j.euroneuro.2011.07.018. [DOI] [PubMed] [Google Scholar]
- Steel Z., Marnane C., Iranpour C. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-−2013. Int. J. Epidemiol. 2014;43:476–493. doi: 10.1093/ije/dyu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloom D., Chisholm D., Llopis E., 2011. et al. From burden to ‘best buys': reducing the economic impact of non-communicable disease in low-and middle-income countries.
- Cairns K.E., Yap M.B.H., Pilkington P.D. Risk and protective factors for depression that adolescents can modify: a systematic review and meta-analysis of longitudinal studies. J. Affect. Disord. 2014;169:61–75. doi: 10.1016/j.jad.2014.08.006. [DOI] [PubMed] [Google Scholar]
- Franklin J.C., Ribeiro J.D., Fox K.R. Risk factors for suicidal thoughts and behaviors: a meta-analysis of 50 years of research. Psychol. Bull. 2017;143:187–232. doi: 10.1037/bul0000084. [DOI] [PubMed] [Google Scholar]
- Hawton K., Casañas Comabella C., Haw C. Risk factors for suicide in individuals with depression: a systematic review. J. Affect. Disord. 2013;147:17–28. doi: 10.1016/j.jad.2013.01.004. [DOI] [PubMed] [Google Scholar]
- Lorant V., Deliège D., Eaton W. Socioeconomic inequalities in depression: a meta-analysis. Am. J. Epidemiol. 2003;157:98–112. doi: 10.1093/aje/kwf182. [DOI] [PubMed] [Google Scholar]
- Meng X., Brunet A., Turecki G. Risk factor modifications and depression incidence: a 4-year longitudinal Canadian cohort of the Montreal Catchment Area Study. BMJ Open. 2017;7:e015156. doi: 10.1136/bmjopen-2016-015156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kestens Y., Wasfi R., Naud A. ‘Contextualizing context’: reconciling environmental exposures, social networks, and location preferences in health research. Curr. Environ. Health Rep. 2017;4:51–60. doi: 10.1007/s40572-017-0121-8. [DOI] [PubMed] [Google Scholar]
- Sallis J.F., Owen N., Fisher E.B. Ecological models of health behavior. In: Glanz K., Rimer B., Viswanath K., editors. 4th. Jossey-Bass; United States: 2008. pp. 465–486. (Health Behavior and Health Education: Theory, Research, and Practice). [Google Scholar]
- Riva M., Gauvin L., Barnett T.A. Toward the next generation of research into small area effects on health: a synthesis of multilevel investigations published since July 1998. J. Epidemiol. Community Health. 2007;61:853–861. doi: 10.1136/jech.2006.050740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux A.V., Mair C. Neighborhoods and health. Ann. N.Y. Acad. Sci. 2010;1186:125–145. doi: 10.1111/j.1749-6632.2009.05333.x. [DOI] [PubMed] [Google Scholar]
- Mair C.F., Roux A.V.D., Galea S. Are neighborhood characteristics associated with depressive symptoms? A critical review. J. Epidemiol. Community Health. 2008 doi: 10.1136/jech.2007.066605. (jech--2007) [DOI] [PubMed] [Google Scholar]
- Blair A., Ross N.A., Gariepy G. How do neighborhoods affect depression outcomes? A realist review and a call for the examination of causal pathways. Soc. Psychiatry Psychiatr. Epidemiol. 2014;49:873–887. doi: 10.1007/s00127-013-0810-z. [DOI] [PubMed] [Google Scholar]
- Tost H., Champagne F.A., Meyer-Lindenberg A. Environmental influence in the brain, human welfare and mental health. Nat. Neurosci. 2015;18:1421–1431. doi: 10.1038/nn.4108. [DOI] [PubMed] [Google Scholar]
- Stickley A., Ng C.F.S., Konishi S. Airborne pollen and suicide mortality in Tokyo, 2001–2011. Environ. Res. 2017;155:134–140. doi: 10.1016/j.envres.2017.02.008. [DOI] [PubMed] [Google Scholar]
- Adli M., Berger M., Brakemeier E.-L. Neurourbanism: towards a new discipline. Lancet Psychiatry. 2017;4:183–185. doi: 10.1016/S2215-0366(16)30371-6. [DOI] [PubMed] [Google Scholar]
- Heinz A., Deserno L., Reininghaus U. Urbanicity, social adversity and psychosis. World Psychiatry. 2013;12:187–197. doi: 10.1002/wps.20056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peen J., Schoevers R.A., Beekman A.T. The current status of urban-rural differences in psychiatric disorders. Acta Psychiatr. Scand. 2010;121:84–93. doi: 10.1111/j.1600-0447.2009.01438.x. [DOI] [PubMed] [Google Scholar]
- Prüss-Üstün A., Corvalán C. World Health Organization; 2006. Preventing Disease Through Healthy Environments: Towards an Estimate of the Environmental Burden of Disease.〈http://www.who.int/quantifying_ehimpacts/publications/preventingdisease/en/〉 [Google Scholar]
- Nieuwenhuijsen M.J. Urban and transport planning, environmental exposures and health-new concepts, methods and tools to improve health in cities. Environ. Health. 2016;15:S38. doi: 10.1186/s12940-016-0108-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rao M., Prasad S., Adshead F. The built environment and health. Lancet. 2007;370:1111–1113. doi: 10.1016/S0140-6736(07)61260-4. [DOI] [PubMed] [Google Scholar]
- Sarkar C., Webster C. Healthy cities of tomorrow: the case for large scale built environment--health studies. J. Urban Health. 2017;94:4–19. doi: 10.1007/s11524-016-0122-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weich S., Blanchard M., Prince M. Mental health and the built environment: cross-sectional survey of individual and contextual risk factors for depression. Br. J. Psychiatry. 2002;180:428–433. doi: 10.1192/bjp.180.5.428. [DOI] [PubMed] [Google Scholar]
- Evans G.W. The built environment and mental health. J. Urban Health. 2003;80:536–555. doi: 10.1093/jurban/jtg063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saarloos D., Alfonso H., Giles-Corti B. The built environment and depression in later life: the health in men study. Am. J. Geriatr. Psychiatry. 2011;19:461–470. doi: 10.1097/JGP.0b013e3181e9b9bf. [DOI] [PubMed] [Google Scholar]
- James P., Hart J.E., Banay R.F. Built environment and depression in low-income African Americans and Whites. Am. J. Prev. Med. 2017;52:74–84. doi: 10.1016/j.amepre.2016.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I., Berkman L.F. Social ties and mental health. J. Urban Health. 2001;78:458–467. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan D.T., Piras G., Dunn E.C. The built environment and depressive symptoms among urban youth: a spatial regression study. Spat. Spat. Epidemiol. Epidemiol. 2013;5:11–25. doi: 10.1016/j.sste.2013.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles R., Coutts C., Mohamadi A. Neighborhood urban form, social environment, and depression. J. Urban Health. 2012;89:1–18. doi: 10.1007/s11524-011-9621-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teychenne M., Ball K., Salmon J. Physical activity and likelihood of depression in adults: a review. Prev. Med. (Baltim.) 2008;46:397–411. doi: 10.1016/j.ypmed.2008.01.009. [DOI] [PubMed] [Google Scholar]
- Gascon M., Triguero-Mas M., Martinez D. Mental health benefits of long-term exposure to residential green and blue spaces: a systematic review. Int. J. Environ. Res. Public Health. 2015;12:4354–4379. doi: 10.3390/ijerph120404354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartig T., Mitchell R., De Vries S. Nature and health. Annu. Rev. Public Health. 2014;35:207–228. doi: 10.1146/annurev-publhealth-032013-182443. [DOI] [PubMed] [Google Scholar]
- Völker S., Kistemann T. The impact of blue space on human health and well-being - salutogenetic health effects of inland surface waters: a review. Int. J. Hyg. Environ. Health. 2011;214:449–460. doi: 10.1016/j.ijheh.2011.05.001. [DOI] [PubMed] [Google Scholar]
- Hawton K., van Heeringen K. Suicide. Lancet. 2009;373:1372–1381. doi: 10.1016/S0140-6736(09)60372-X. [DOI] [PubMed] [Google Scholar]
- Berry H.L. ‘Crowded suburbs’ and ‘killer cities’: a brief review of the relationship between urban environments and mental health. N. SW Public Health Bull. 2008;18:222–227. doi: 10.1071/nb07024. [DOI] [PubMed] [Google Scholar]
- Kwan M.-P. The uncertain geographic context problem. Ann. Assoc. Am. Geogr. 2012;102:958–968. [Google Scholar]
- Kwan M.-P. Beyond space (as we knew it): toward temporally integrated geographies of segregation, health, and accessibility. Ann. Assoc. Am. Geogr. 2013;103:1078–1086. [Google Scholar]
- Van Ham M., Manley D. Neighbourhood effects research at a crossroads: ten challenges for future research introduction. Environ. Plan A. 2012;44:2787–2793. [Google Scholar]
- Park Y.M., Kwan M.-P. Individual exposure estimates may be erroneous when spatiotemporal variability of air pollution and human mobility are ignored. Health Place. 2017;43:85–94. doi: 10.1016/j.healthplace.2016.10.002. [DOI] [PubMed] [Google Scholar]
- Gruebner O., Rapp M.A., Adli M. Cities and mental health. Dtsch. Arztebl. Int. 2017;114:121. doi: 10.3238/arztebl.2017.0121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blüml V., Helbich M., Mayr M. Antidepressant sales and regional variations of suicide mortality in Germany. J. Psychiatr. Res. 2017;87:88–94. doi: 10.1016/j.jpsychires.2016.12.013. [DOI] [PubMed] [Google Scholar]
- Helbich M., Blüml V., de Jong T., Plener P., Kwan M.-P., Kapusta N. Urban-rural inequalities in suicide mortality: A comparison of urbanicity indicators. International Journal of Health Geographics. 2017;19:39. doi: 10.1186/s12942-017-0112-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helbich M., Leitner M., Kapusta N.D. Lithium in drinking water and suicide mortality: interplay with lithium prescriptions. Br. J. Psychiatry. 2015;207:64–71. doi: 10.1192/bjp.bp.114.152991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macintyre S., Ellaway A. Ecological approaches: rediscovering the role of the physical and social environment. Soc. Epidemiol. 2000;9:332–348. [Google Scholar]
- Sampson R.J., Morenoff J.D., Gannon-Rowley T. Assessing ‘neighborhood effects': social processes and new directions in research. Annu. Rev. Sociol. 2002;28:443–478. [Google Scholar]
- Liu S., Page A., Yin P. Spatiotemporal variation and social determinants of suicide in China, 2006–2012: findings from a nationally representative mortality surveillance system. Psychol. Med. 2015;45:3259–3268. doi: 10.1017/S0033291715001269. [DOI] [PubMed] [Google Scholar]
- Owen G., Harris R., Jones K. Under examination: multilevel models, geography and health research. Prog. Hum. Geogr. 2016;40:394–412. [Google Scholar]
- Diez-Roux A.V. Multilevel analysis in public health research. Annu. Rev. Public Health. 2000;21:171–192. doi: 10.1146/annurev.publhealth.21.1.171. [DOI] [PubMed] [Google Scholar]
- Flowerdew R., Manley D.J., Sabel C.E. Neighbourhood effects on health: does it matter where you draw the boundaries? Soc. Sci. Med. 2008;66:1241–1255. doi: 10.1016/j.socscimed.2007.11.042. [DOI] [PubMed] [Google Scholar]
- Wheeler D.C., Ward M.H., Waller L.A. Spatial-temporal analysis of cancer risk in epidemiologic studies with residential histories. Ann. Assoc. Am. Geogr. 2012;102:1049–1057. doi: 10.1080/00045608.2012.671131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaix B., Meline J., Duncan S. GPS tracking in neighborhood and health studies: a step forward for environmental exposure assessment, a step backward for causal inference? Health Place. 2013;21:46–51. doi: 10.1016/j.healthplace.2013.01.003. [DOI] [PubMed] [Google Scholar]
- Berke E.M., Gottlieb L.M., Moudon A.V. Protective association between neighborhood walkability and depression in older men. J. Am. Geriatr. Soc. 2007;55:526–533. doi: 10.1111/j.1532-5415.2007.01108.x. [DOI] [PubMed] [Google Scholar]
- Helbich M., Schadenberg B., Hagenauer J. Food deserts? Healthy food access in Amsterdam. Appl. Geogr. 2017;83:1–12. [Google Scholar]
- Cummins S. Commentary: investigating neighbourhood effects on health—avoiding the ‘local trap’. Int. J. Epidemiol. 2007;36:355–357. doi: 10.1093/ije/dym033. [DOI] [PubMed] [Google Scholar]
- Hurvitz P.M., Moudon A.V. Home versus nonhome neighborhood: quantifying differences in exposure to the built environment. Am. J. Prev. Med. 2012;42:411–417. doi: 10.1016/j.amepre.2011.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perchoux C., Chaix B., Cummins S. Conceptualization and measurement of environmental exposure in epidemiology: accounting for activity space related to daily mobility. Health Place. 2013;21:86–93. doi: 10.1016/j.healthplace.2013.01.005. [DOI] [PubMed] [Google Scholar]
- Sarkar C., Gallacher J., Webster C. Urban built environment configuration and psychological distress in older men: results from the Caerphilly study. BMC Public Health. 2013;13:695. doi: 10.1186/1471-2458-13-695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben-Shlomo Y., Kuh D. A life course approach to chronic disease epidemiology: conceptual models, empirical challenges and interdisciplinary perspectives. Int. J. Epidemiol. 2002;31:285–293. [PubMed] [Google Scholar]
- Lynch J., Smith G.D. A life course approach to chronic disease epidemiology. Annu. Rev. Public Health. 2005;26:1–35. doi: 10.1146/annurev.publhealth.26.021304.144505. [DOI] [PubMed] [Google Scholar]
- Leyland A.H., Næss Ø. The effect of area of residence over the life course on subsequent mortality. J. R. Stat. Soc. Ser. A (Stat. Soc. 2009;172:555–578. doi: 10.1111/j.1467-985X.2008.00581.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miltenburg E.M., van der Meer T.W.G. Lingering neighbourhood effects: a framework to account for residential histories and temporal dynamics. Urban Stud. 2016 (42098016639012) [Google Scholar]
- Musterd S., Galster G., Andersson R. Temporal dimensions and measurement of neighbourhood effects. Environ. Plan A. 2012;44:605–627. [Google Scholar]
- Sharkey P., Faber J.W. Where, when, why, and for whom do residential contexts matter? Moving away from the dichotomous understanding of neighborhood effects. Annu. Rev. Sociol. 2014;40:559–579. [Google Scholar]
- Browning C.R., Cagney K.A., Boettner B. Handbook of the Life Course. Springer; 2016. Neighborhood, place, and the life course; pp. 597–620. [Google Scholar]
- Schönfelder S., Axhausen K.W. Activity spaces: measures of social exclusion? Transp. Policy. 2003;10:273–286. [Google Scholar]
- Dijst M. Time geographic analysis. In: Kitchin R., Thrift N., editors. International Encyclopedia of Human Geography. Oxford; 2009. pp. 266–278. [Google Scholar]
- Hägerstraand T. What about people in regional science? Pap. Reg. Sci. 1970;24:7–24. [Google Scholar]
- Vallée J., Cadot E., Grillo F. The combined effects of activity space and neighbourhood of residence on participation in preventive health-care activities: the case of cervical screening in the Paris metropolitan area (France) Health Place. 2010;16:838–852. doi: 10.1016/j.healthplace.2010.04.009. [DOI] [PubMed] [Google Scholar]
- Basta L.A., Richmond T.S., Wiebe D.J. Neighborhoods, daily activities, and measuring health risks experienced in urban environments. Soc. Sci. Med. 2010;71:1943–1950. doi: 10.1016/j.socscimed.2010.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Axhausen K.W., Zimmermann A., Schönfelder S. Observing the rhythms of daily life: a six-week travel diary. Transportation (Amst.) 2002;29:95–124. [Google Scholar]
- Richardson D.B., Volkow N.D., Kwan M.-P. Spatial turn in health research. Science. 2013;80(339):1390–1392. doi: 10.1126/science.1232257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen L., Stopher P.R. Review of GPS travel survey and GPS data-processing methods. Transp. Rev. 2014;34:316–334. [Google Scholar]
- Helbich M., Emmichoven M.J.Z., van, Dijst M.J. Natural and built environmental exposures on children's active school travel: a Dutch global positioning system-based cross-sectional study. Health Place. 2016;39:101–109. doi: 10.1016/j.healthplace.2016.03.003. [DOI] [PubMed] [Google Scholar]
- Glasgow M.L., Rudra C.B., Yoo E.-H. Using smartphones to collect time-activity data for long-term personal-level air pollution exposure assessment. J. Expo. Sci. Environ. Epidemiol. 2016;26:356–364. doi: 10.1038/jes.2014.78. [DOI] [PubMed] [Google Scholar]
- Birenboim A., Shoval N. Mobility research in the age of the smartphone. Ann. Am. Assoc. Geogr. 2016;106:283–291. [Google Scholar]
- Gravenhorst F., Muaremi A., Bardram J. Mobile phones as medical devices in mental disorder treatment: an overview. Pers. Ubiquitous Comput. 2015;19:335–353. [Google Scholar]
- Miluzzo E., Lane N.D., Fodor K., 2008. et al. Sensing meets mobile social networks: the design, implementation and evaluation of the cenceme application. In: Proceedings of the 6th ACM Conference on Embedded Network Sensor Systems. pp. 337–350.
- Eskes P., Spruit M., Brinkkemper S. The sociability score: app-based social profiling from a healthcare perspective. Comput. Human. Behav. 2016;59:39–48. [Google Scholar]
- Larsen J., Axhausen K.W., Urry J. Geographies of social networks: meetings, travel and communications. Mobilities. 2006;1:261–283. [Google Scholar]
- Rettie R. Mobile phones as network capital: facilitating connections. Mobilities. 2008;3:291–311. [Google Scholar]
- Saeb S., Zhang M., Karr C.J. Mobile phone sensor correlates of depressive symptom severity in daily-life behavior: an exploratory study. J. Med. Internet Res. 2015;17:e175. doi: 10.2196/jmir.4273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomée S., Härenstam A., Hagberg M. Mobile phone use and stress, sleep disturbances, and symptoms of depression among young adults-a prospective cohort study. BMC Public Health. 2011;11:66. doi: 10.1186/1471-2458-11-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hobbs W.R., Burke M., Christakis N.A. Online social integration is associated with reduced mortality risk. Proc. Natl. Acad. Sci. 2016;113:12980–12984. doi: 10.1073/pnas.1605554113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eagle N., Pentland A.S., Lazer D. Inferring friendship network structure by using mobile phone data. Proc. Natl. Acad. Sci. 2009;106:15274–15278. doi: 10.1073/pnas.0900282106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruebner O., Sykora M., Lowe S.R. Big data opportunities for social behavioral and mental health research. Soc. Sci. Med. 2017;189:167. doi: 10.1016/j.socscimed.2017.07.018. [DOI] [PubMed] [Google Scholar]
- Conway M., O’Connor D. Social media, big data, and mental health: current advances and ethical implications. Curr. Opin. Psychol. 2016;9:77–82. doi: 10.1016/j.copsyc.2016.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S., Stone A.A., Hufford M.R. Ecological momentary assessment. Annu. Rev. Clin. Psychol. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- Kumari P., Mathew L., Syal P. Increasing trend of wearables and multimodal interface for human activity monitoring: a review. Biosens. Bioelectron. 2017;90:298–307. doi: 10.1016/j.bios.2016.12.001. [DOI] [PubMed] [Google Scholar]
- Brazil N., Clark W.A.V. Individual mental health, life course events and dynamic neighbourhood change during the transition to adulthood. Health Place. 2017;45:99–109. doi: 10.1016/j.healthplace.2017.03.007. [DOI] [PubMed] [Google Scholar]
- Meliker J.R., Jacquez G.M. Space-time clustering of case-control data with residential histories: insights into empirical induction periods, age-specific susceptibility, and calendar year-specific effects. Stoch. Environ. Res. Risk Assess. 2007;21:625–634. doi: 10.1007/s00477-007-0140-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabel C.E., Boyle P., Raab G. Modelling individual space-time exposure opportunities: a novel approach to unravelling the genetic or environment disease causation debate. Spat. Spatiotemporal Epidemiol. 2009;1:85–94. doi: 10.1016/j.sste.2009.07.002. [DOI] [PubMed] [Google Scholar]
- Ludwig J., Duncan G.J., Gennetian L.A. Neighborhood effects on the long-term well-being of low-income adults. Science (80-) 2012;337:1505–1510. doi: 10.1126/science.1224648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tunstall H., Pearce J.R., Shortt N.K. Residential mobility and the association between physical environment disadvantage and general and mental health. J. Public Health (Bangk.) 2014;37:563–572. doi: 10.1093/pubmed/fdu058. [DOI] [PubMed] [Google Scholar]
- Niedzwiedz C.L., Katikireddi S.V., Pell J.P. Life course socio-economic position and quality of life in adulthood: a systematic review of life course models. BMC Public Health. 2012;12:628. doi: 10.1186/1471-2458-12-628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce J. Invited commentary: history of place, life course, and health inequalities—historical geographic information systems and epidemiologic research. Am. J. Epidemiol. 2014;181:26–29. doi: 10.1093/aje/kwu312. [DOI] [PubMed] [Google Scholar]
- Pearce J., Shortt N., Rind E. Life course, green space and health: incorporating place into life course epidemiology. Int. J. Environ. Res. Public Health. 2016;13:331. doi: 10.3390/ijerph13030331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veldman K., Reijneveld S.A., Verhulst F.C. A life course perspective on mental health problems, employment, and work outcomes. Scand. J. Work Environ. Health. 2017;43:316–325. doi: 10.5271/sjweh.3651. [DOI] [PubMed] [Google Scholar]
- Brokamp C., LeMasters G.K., Ryan P.H. Residential mobility impacts exposure assessment and community socioeconomic characteristics in longitudinal epidemiology studies. J. Expo. Sci. Environ. Epidemiol. 2016;26:428. doi: 10.1038/jes.2016.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erlangsen A., Runeson B., Bolton J.M. Association between spousal suicide and mental, physical, and social health outcomes: a longitudinal and nationwide register-based study. JAMA Psychiatry. 2017;74:456–464. doi: 10.1001/jamapsychiatry.2017.0226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Termorshuizen F., Smeets H.M., Braam A.W. Neighborhood ethnic density and psychotic disorders among ethnic minority groups in Utrecht City. Soc. Psychiatry Psychiatr. Epidemiol. 2014;49:1093–1102. doi: 10.1007/s00127-014-0842-z. [DOI] [PubMed] [Google Scholar]
- Kunst A.E., van Hooijdonk C., Droomers M. Community social capital and suicide mortality in the Netherlands: a cross-sectional registry-based study. BMC Public Health. 2013;13:969. doi: 10.1186/1471-2458-13-969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyons R.A., Ford D.V., Moore L. Use of data linkage to measure the population health effect of non-health-care interventions. Lancet. 2014;383:1517–1519. doi: 10.1016/S0140-6736(13)61750-X. [DOI] [PubMed] [Google Scholar]
- Maas J., Sterkenburg R.P., de Vries S.I. Neighbourhood Structure and Health Promotion. Springer; 2013. Using GPS to measure the interaction between individuals and their neighbourhood; pp. 153–175. [Google Scholar]
- Burgoine T., Forouhi N.G., Griffin S.J. Associations between exposure to takeaway food outlets, takeaway food consumption, and body weight in Cambridgeshire, UK: population based, cross sectional study. BMJ. 2014;348:g1464. doi: 10.1136/bmj.g1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong B.Y.-M., Faulkner G., Buliung R. GIS measured environmental correlates of active school transport: a systematic review of 14 studies. Int J. Behav. Nutr. Phys. Act. 2011;8:39. doi: 10.1186/1479-5868-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokhtarian P.L., Cao X. Examining the impacts of residential self-selection on travel behavior: a focus on methodologies. Transp. Res. Part B Methodol. 2008;42:204–228. [Google Scholar]
- Galster G., Hedman L. Measuring neighbourhood effects non-experimentally: how much do alternative methods matter? Hous. Stud. 2013;28:473–498. [Google Scholar]
- Longwell B.T., Truax P. The differential effects of weekly, monthly, and bimonthly administrations of the Beck Depression Inventory-II: psychometric properties and clinical implications. Behav. Ther. 2005;36:265–275. [Google Scholar]
- Jung T., Wickrama K.A.S. An introduction to latent class growth analysis and growth mixture modeling. Soc. Personal. Psychol. Compass. 2008;2:302–317. [Google Scholar]
- Witten I.H., Frank E., Hall M.A., 2016. et al. Data mining: practical machine learning tools and techniques.
- Edwards P., Roberts I., Clarke M. Increasing response rates to postal questionnaires: systematic review. BMJ. 2002;324:1183. doi: 10.1136/bmj.324.7347.1183. [DOI] [PMC free article] [PubMed] [Google Scholar]