Abstract
Conjunctivitis is the most common ocular condition diagnosed in US emergency departments (EDs), accounting for almost one-third of all eye-related encounters.1 Because of its generally nonemergent nature, understanding the burden and timing of conjunctivitis may allow preemptive triage to a less expensive health care setting.
Methods
The National Emergency Department Sample (NEDS) is a population-based data set consisting of a stratified sample of 20% of US hospital-based EDs. National estimates are extrapolated using poststratification weights.2 We calculated national estimates of encounters with a primary diagnosis of acute conjunctivitis from January 1, 2010, through December 31, 2013, stratified by age, sex, and calendar month. Analysis of this public de-identified data set did not meet the institutional review board at University of California, San Francisco’s definition of human subject research and therefore did not require ethical approval or informed consent. We estimated the incidence of conjunctivitis diagnosed in the ED by using population figures obtained from the 2010 US decennial census as the denominator. We implemented the Kolmogorov-Smirnov test and the Edwards test3 to compare age-incidence curves and seasonality, respectively, with P < .05 indicating statistical significance. We used R software, version 3.3.1 (survey and zoo packages; https://cran.r-project.org) for analyses performed from January 15 to March 30, 2017.
Results
We found a total of 555 740 encounters in US EDs that resulted in a primary diagnosis of conjunctivitis in the NEDS data set from 2010 through 2013. The distribution of conjunctivitis diagnosed in the ED was bimodal, with the highest rates among children younger than 7 years and a minor mode in early adulthood (Figure 1A). Conjunctivitis was more common among women than men when we restricted the analysis to persons 18 years or older (maximum difference of 36.2 per 100 000 cases; P = .03, Kolmogorov-Smirnov test), with a minor mode at 22 years in women and 28 years of age in men. Conjunctivitis cases among all ages had significant seasonality (peak of 3.5 per 100 000 population; nadir of 2.4 per 100 000 population; P < .001, Edwards test) (Figure 2A). When stratified by age group, children aged 0 to 4 years demonstrated a peak in conjunctivitis presentations in March, whereas all other age groups showed a peak in May. The peak in age incidence (Figure 1B) and seasonality pattern (Figure 2B) did not differ using more granular conjunctivitis codes. Similar seasonal patterns were observed for geographic regions.
Figure 1. Age-Incidence Curve for Acute Conjunctivitis Diagnosed at US Emergency Departments.
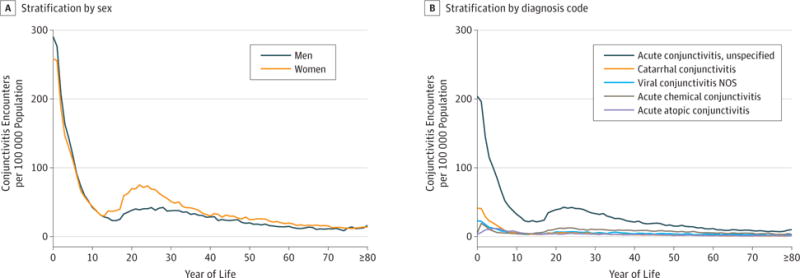
Cases were calculated using the total number of cases at each year of age divided by the total census population for that same age, with the mean calculated from January 1, 2010, through December 31, 2013. NOS indicates not otherwise specified.
Figure 2. Seasonality of Acute Conjunctivitis by Age Group in US Emergency Departments.
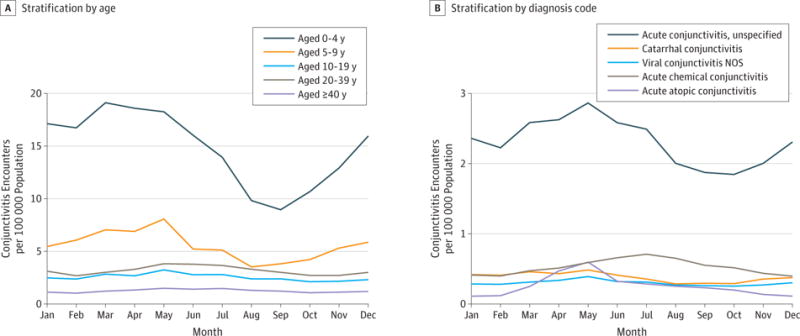
Cases were calculated using the total number of cases in each month divided by the total census population for that same month, with the mean calculated from January 1, 2010, through December 31, 2013. NOS indicates not otherwise specified.
Discussion
This study provides several insights into the epidemiology of conjunctivitis diagnosed in the ED. We found a higher prevalence among adult women than men, a bimodal age distribution, and a predictable surge of cases during the spring. We believe caregiver proximity to young children likely explains the peak of conjunctivitis in early adulthood but cannot prove this hypothesis from our data. Our theory is supported by increased childcare responsibility for women compared with men.4 In addition, women and men first become parents at a mean age of 23 and 25 years, respectively, roughly corresponding to the minor peaks we observed. We speculate that inexperience may cause first-time parents to bring their children to the ED for nonemergent conditions, such as conjunctivitis.
Conjunctivitis was consistently seasonal. Increases in allergic conjunctivitis may explain this finding because atopic conjunctivitis diagnosed in the ED spiked during this time; however, this theory represents speculation on our part. Bacterial or viral conjunctivitis may also contribute to the increase in cases during the spring, although investigations into the seasonality of similar infectious agents, such as those causing otitis media and viral illnesses in children, demonstrated peaks in the winter months.5
A major limitation of this analysis is its inclusion of only cases diagnosed in the ED. This exclusion criterion underestimates the true incidence of conjunctivitis and could lead to spurious associations if the likelihood of an ED visit for conjunctivitis varied with age or season. Furthermore, diagnostic code misclassification can occur with an administrative data set. However, in 1 study,6 92% of clinicians in general practice were confident in diagnosing acute infective conjunctivitis despite uncertainty in differentiating between bacterial and viral conjunctivitis. Moreover, our large sample size reduces statistical noise from misclassification error.
Conclusions
Conjunctivitis in US EDs demonstrated a peak during early childhood and a smaller peak in early adulthood. Diagnoses were seasonal, with more cases in spring. Educational efforts targeted to new parents about the timing and nonemergent nature of conjunctivitis may help shift the burden of conjunctivitis care away from EDs, which could ultimately reserve ED resources for patients requiring more urgent attention.
Acknowledgments
Funding/Support: This study was supported by Core Grant for Vision Research EY002162 and grant R01EY024608 from the National Eye Institute, National Institutes of Health (NIH) (Drs Lietman and Porco); grant U01-GM087728 from the National Institute of General Medical Sciences Models of Infectious Disease Agent Study Program, NIH (Dr Porco); grant R25MD006832 from the National Institute on Minority Health and Health Disparities, NIH (Mr Ramirez); and Research to Prevent Blindness.
Role of the Funder/Sponsor: The sponsors had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review or approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
Author Contributions: Mr Ramirez and Dr Keenan had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Ramirez, Lietman, Keenan.
Acquisition, analysis, or interpretation of data: Ramirez, Porco.
Drafting of the manuscript: Ramirez, Keenan.
Critical revision of the manuscript for important intellectual content: Ramirez, Porco, Lietman.
Statistical analysis: Ramirez, Porco, Keenan.
Obtained funding: Ramirez.
Administrative, technical, or material support: Ramirez, Keenan.
Study supervision: Lietman, Keenan.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and none were reported.
Contributor Information
David A. Ramirez, Currently a medical student, School of Medicine, University of California, San Francisco; Francis I. Proctor Foundation, University of California, San Francisco.
Travis C. Porco, Francis I. Proctor Foundation, University of California, San Francisco; Department of Ophthalmology, University of California, San Francisco; Department of Epidemiology and Biostatistics, University of California, San Francisco.
Thomas M. Lietman, Francis I. Proctor Foundation, University of California, San Francisco; Department of Ophthalmology, University of California, San Francisco; Department of Epidemiology and Biostatistics, University of California, San Francisco.
Jeremy D. Keenan, Francis I. Proctor Foundation, University of California, San Francisco; Department of Ophthalmology, University of California, San Francisco.
References
- 1.Channa R, Zafar SN, Canner JK, Haring RS, Schneider EB, Friedman DS. Epidemiology of eye-related emergency department visits. JAMA Ophthalmol. 2016;134(3):312–319. doi: 10.1001/jamaophthalmol.2015.5778. [DOI] [PubMed] [Google Scholar]
- 2.Health Cost and Utilization Project. Introduction to the HCUP Nationwide Emergency Department Sample (NEDS) 2013 https://www.hcup-us.ahrq.gov/db/nation/neds/NEDS_Introduction_2013.jsp#sampledesign. November 2015, Accessed December 8, 2016.
- 3.Edwards JH. The recognition and estimation of cyclic trends. Ann Hum Genet. 1961;25:83–87. doi: 10.1111/j.1469-1809.1961.tb01501.x. [DOI] [PubMed] [Google Scholar]
- 4.Laughlin L. Who’s minding the kids? child care arrangements. US Census Bureau; Spring. 2011. https://www.census.gov/library/publications/2013/demo/p70-135.html. April 2013. Accessed March 31, 2017. [Google Scholar]
- 5.Stockmann C, Ampofo K, Hersh AL, et al. Seasonality of acute otitis media and the role of respiratory viral activity in children. Pediatr Infect Dis J. 2013;32(4):314–319. doi: 10.1097/INF.0b013e31827d104e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Everitt H, Little P. How do GPs diagnose and manage acute infective conjunctivitis? a GP survey. Fam Pract. 2002;19(6):658–660. doi: 10.1093/fampra/19.6.658. [DOI] [PubMed] [Google Scholar]


